
1
Medical Policy
Joint Medical Policies are a source for BCBSM and BCN medical policy information only. These documents
are not to be used to determine benefits or reimbursement. Please reference the appropriate certificate or
contract for benefit information. This policy may be updated and is therefore subject to change.
*Current Policy Effective Date: 5/1/24
(See policy history boxes for previous effective dates)
Title:
Dry Needling of Trigger Points for Myofascial Pain
Description/Background
Dry Needling
Dry needling refers to a procedure in which a fine needle is inserted into the skin and muscle at
a site of myofascial pain. The needle may be moved in an up-and-down motion, rotated, and/or
left in place for as long as 30 minutes. The intent is to stimulate underlying myofascial trigger
points, muscles, and connective tissues to manage myofascial pain. Dry needling may be
performed with acupuncture needles or standard hypodermic needles but is performed without
the injection of medications (e.g., anesthetics, corticosteroids). Dry needling is proposed to treat
dysfunctions in skeletal muscle, fascia, and connective tissue; diminish persistent peripheral
pain, and reduce impairments of body structure and function.
The physiologic basis for dry needling depends on the targeted tissue and treatment objectives.
The most studied targets are trigger points. Trigger points are discrete, focal, hyperirritable
spots within a taut band of skeletal muscle fibers that produce local and/or referred pain when
stimulated. Trigger points are associated with local ischemia and hypoxia, a significantly
lowered pH, local and referred pain and altered muscle activation patterns.
1
Trigger points can
be visualized by magnetic resonance imaging and elastography. The reliability of manual
identification of trigger points has not been established.
Deep dry needling is believed to inactivate trigger points by eliciting contraction and subsequent
relaxation of the taut band via a spinal cord reflex. This local twitch response is defined as a
transient visible or palpable contraction or dimpling of the muscle, and has been associated
with alleviation of spontaneous electrical activity; reduction of numerous nociceptive,
inflammatory, and immune system related chemicals; and relaxation of the taut band.
1
Deep dry
needling of trigger points is believed to reduce local and referred pain, improve range of motion,
and decrease trigger point irritability.

2
Superficial dry needling is thought to activate mechanoreceptors and have an indirect effect on
pain by inhibiting C-fiber pain impulses. The physiologic basis for dry needling treatment of
excessive muscle tension, scar tissue, fascia, and connective tissues is not as well described in
the literature.
1
Regulatory Status
Dry needling is considered a procedure and, as such, is not subject to regulation by the U.S.
Food and Drug Administration.
Medical Policy Statement
Dry needling of myofascial trigger points is experimental/investigational. It has not been
scientifically demonstrated to improve patient clinical outcomes.
Inclusionary and Exclusionary Guidelines
N/A
CPT/HCPCS Level II Codes (Note: The inclusion of a code in this list is not a guarantee of
coverage. Please refer to the medical policy statement to determine the status of a given procedure.)
Established codes:
N/A
Other codes (investigational, not medically necessary, etc.):
20560 20561 20999
Note: Codes 97810-97814 are not appropriate since this is not the same as acupuncture
Note: Individual policy criteria determine the coverage status of the CPT/HCPCS code(s) on this
policy. Codes listed in this policy may have different coverage positions (such as established or
experimental/investigational) in other medical policies.
Rationale
Evidence reviews assess the clinical evidence to determine whether the use of technology
improves the net health outcome. Broadly defined, health outcomes are the length of life,
quality of life (QOL), and ability to function-including benefits and harms. Every clinical
condition has specific outcomes that are important to patients and managing the course of that
condition. Validated outcome measures are necessary to ascertain whether a condition
improves or worsens; and whether the magnitude of that change is clinically significant. The
net health outcome is a balance of benefits and harms.
3
To assess whether the evidence is sufficient to draw conclusions about the net health outcome
of technology, two domains are examined: the relevance, and quality and credibility. To be
relevant, studies must represent one or more intended clinical use of the technology in the
intended population and compare an effective and appropriate alternative at a comparable
intensity. For some conditions, the alternative will be supportive care or surveillance. The
quality and credibility of the evidence depend on study design and conduct, minimizing bias
and confounding that can generate incorrect findings. The randomized controlled trial (RCT) is
preferred to assess efficacy; however, in some circumstances, nonrandomized studies may be
adequate. RCTs are rarely large enough or long enough to capture less common adverse
events and long-term effects. Other types of studies can be used for these purposes and to
assess generalizability to broader clinical populations and settings of clinical practice.
Dry Needling of Trigger Points Associated with Neck and/or Shoulder Pain
Clinical Context and Therapy Purpose
The purpose of dry needling in patients who have myofascial neck and/or shoulder pain is to
provide a treatment option that is an alternative to or an improvement on existing therapies.
The following PICO was used to select literature to inform this review.
Populations
The relevant population of interest are individuals with myofascial trigger points associated
with neck, shoulder pain. Trigger points are discrete, focal, hyperirritable spots within a taut
band of skeletal muscle fibers that produce local and/or referred pain when stimulated.
Interventions
The therapy being considered is dry needling.
Dry needling refers to a procedure whereby a fine needle is inserted into the trigger point to
induce a twitch response and relieve the pain. The needle may be moved in an up-and-down
motion, rotated, and/or left in place for as long as 30 minutes. The physiologic basis for dry
needling depends on the targeted tissue and treatment objectives. Deep dry needling is
believed to inactivate trigger points by eliciting contraction and subsequent relaxation of the
taut band via a spinal cord reflex. Superficial dry needling is thought to activate
mechanoreceptors and have an indirect effect on pain by inhibiting C-fiber pain impulses.
Comparators
Alternative nonpharmacologic treatment modalities for trigger point pain include manual
techniques, massage, acupressure, ultrasonography, application of heat or ice, diathermy,
transcutaneous electrical nerve stimulation, and spray cooling with manual stretch.
2
Outcomes
The outcomes of interest are symptoms, functional outcomes, QOL, and treatment-related
morbidity.
4
Review of Evidence
Systemic Reviews
Numerous, primarily small, RCTs involving dry needling techniques in neck or shoulder pain
have been evaluated in several systematic reviews and meta-analyses.
Charles et al (2019) conducted a systematic review of different techniques for treatment of
myofascial pain.
3
A total of 23 studies of dry needling were included. Of these, 15 assessed
the technique for neck or shoulder pain. The quality of evidence for dry needling in the
management of myofascial pain and trigger points ranged from very low to moderate
compared with control groups, sham interventions, or other treatments for changes in pain,
pressure point threshold, and functional outcomes. Multiple limitations in the body of the
evidence were identified, including high risk of bias, small sample sizes, unclear randomization
and concealment procedures, inappropriate blinding, imbalanced baseline characteristics, lack
of standardized methodologies, unreliable outcome measures, high attrition rates, unknown
long-term treatment effects, lack of effective sham methods, and lack of standardized
guidelines in the location of trigger points. The reviewers concluded that the evidence for dry
needling was not greater than placebo.
Navarro-Santana et al (2020) conducted a systematic review and meta-analysis of dry
needling of myofascial trigger points associated with neck pain compared to sham needling, no
intervention, or other physical interventions.
4
A total of28 RCTs were included. Dry needling
reduced pain immediately after the intervention (mean difference [MD] in pain score-1.53; 95%
confidence interval [CI] -2.29 to -0.76) and at the short-term (up to 1 month) (MD -2.31, 95% CI
-3.64 to -0.99)when compared with sham, placebo, waiting list, or other forms of dry needling,
and at the short-term compared with manual therapy (MD -0.51, 95% CI -0.95 to -0.06). No
differences in comparison with other physical therapy interventions were observed. An effect
on pain-related disability at the short-term was found when comparing dry needling with sham,
placebo, waiting list, or other form of dry needling, but not with manual therapy or other
physical therapy interventions.
Navarro-Santana et al (2020) also conducted a systematic review and meta-analysis of dry
needling for shoulder pain.
5
The meta-analysis found moderate quality evidence for a small
effect (MD -0.49 points; 95% CI -0.84 to -0.13;standardized mean difference [SMD] -0.25; 95%
CI -0.42 to -0.09) for decreasing shoulder pain intensity, and low quality evidence for a large
effect (MD -9.99 points; 95% CI -15.97 to -4.01; SMD -1.14; 95% CI -1.81 to -0.47) for
reducing related disability. The effects on pain intensity were found only in the short term (up to
1 month) and did not reach the minimal clinically important difference of 1.1 points for the
numerical pain rating scale (0 to 10) determined for patients with shoulder pain. Confidence
intervals of the main effects of dry needling on pain intensity and related disability were wide.
Additionally, the trials were heterogeneous with regard to the number and/or frequency of
needling sessions and the type of comparator.
Para-Garcia et al (2022) conducted a systematic review and meta-analysis of dry-needling
compared with other interventions in patients with subacromial pain syndrome.
16
Five RCTs
(N=315) published between 2012 and 2022 were included. The intervention group included 3
studies with dry needling in combination with exercise and 2 studies with dry needling alone
while the control group had a wide range of interventions including exercise, stretching,
massage, heat, and electrotherapy. Dry needling was generally performed for 2 sessions over
5
3 or 4 weeks, but 1 study had all sessions in 1 week. Minimal information was available on
session duration. Short-term pain was reduced with dry needling either alone or when
combined with exercise compared with other interventions (SMD, -0.27; 95% CI, -0.49 to -0.05;
I2=0.00%; p<.02; low quality evidence), but the difference between groups was small and
clinical relevance is questionable. Pain intensity was also reduced at mid-term (1 to 12
months) based on low-quality evidence; however, there was no difference in disability between
groups. The quality of evidence was low to very-low due to lack of blinding and imprecision.
Section Summary: Neck and/or Shoulder Pain
A number of RCTs and systematic reviews of these studies have evaluated dry needling of
myofascial trigger points for neck and/or shoulder pain. A systematic review of techniques for
myofascial pain included 15 studies of dry needling for neck or shoulder pain published
through 2017. Studies had multiple methodological limitations, and the reviewers concluded
that the evidence for dry needling was not greater than placebo. In more recent systematic
reviews and meta-analyses, dry needling was not associated with clinically important
reductions in shoulder or neck pain when compared toother physical therapy modalities.
Dry Needling of Myofascial Trigger Points Associated with Plantar Heel Pain
Review of Evidence
Systemic Review
Llurda-Almuzara et al (2021) published a systematic review of 6 randomized trials (N=395)
evaluating dry needling for the treatment of plantar fasciitis (Tables 1 to 3).
6,
None of the
included trials were double-blind and, although the authors did find some positive effects of dry
needling, the heterogeneity, lack of blinding, and small number of patients in the trials limits
applicability.
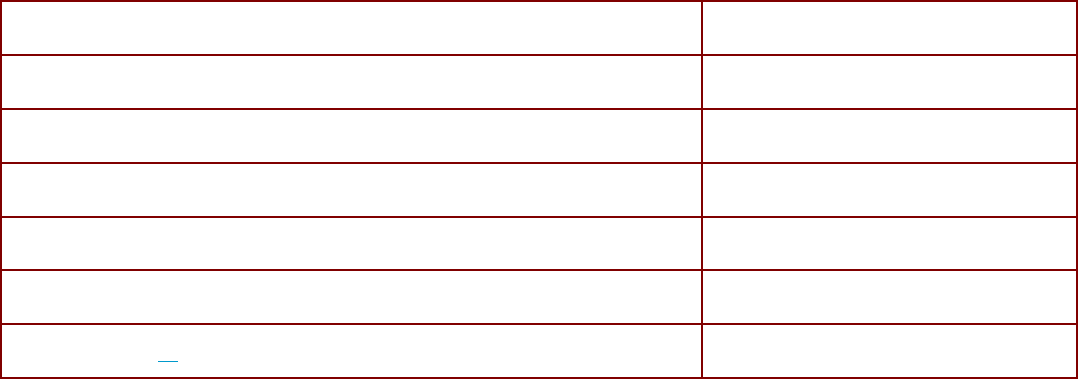
Table 1. Trials Included in Systematic Review
Study
Llurda-Almuzara et al (2021)
6,
Bagcier et al (2020)
7,
⚫
Cotchett et al (2014)
8,
⚫
Eftekharsadat et al (2016)
9,
⚫
Rahbar et al (2018)
10,
⚫
Rastegar et al (2017)
11,
⚫
Uygur et al (2019)
12,
⚫

6
Table 2. Systematic Review Characteristics
Study
Dates
Trials
Participants
N (Range)
Design
Duration
Llurda-
Almuzara
et
al (2021)
6,
Inception-
2020
6
Patients with heel pain
receiving dry needling
or comparator (placebo,
no intervention, or active
comparator)
395 (10 to
49)
RCT
1 to 6 sessions (mean,
4 sessions)
RCT: randomized controlled trial.
Table 3. Systematic Review Results
Study
Overall
Pain
Intensity
Pain Intensity
(at least 3 Sessions)
Long-term Pain Intensity
Pain-related Disability
Llurda-Almuzara et al (2021)
6,
Trials (n)
6
4
2
5
SMD (95% CI)
-0.5 (-1.13 to
0.13)
-1.28 (-2.11 to -0.44)
-1.45 (-2.19 to -0.70)
-0.46 (-0.90 to -0.01)
I
2
94%
>85%
67% to 78%
84%
CI: confidence interval; SMD: standardized mean difference.
Section Summary: Plantar Heel Pain
The evidence base consists of a systematic review of RCTs. The authors included 6
randomized trials enrolling 395 patients and found no overall difference in pain intensity in
those treated with dry needling compared with active control, placebo, or no intervention.
However, pain intensity after at least 3 sessions, long-term pain intensity, and pain-related
disability were improved. The systematic review rated the quality of the studies it assessed as
low to moderate. The evidence is limited by small patient populations and lack of blinding;
therefore, additional RCTs are needed to strengthen the evidence base.
Dry Needling of Myofascial Trigger Points Associated with Temporomandibular Pain
Review of Evidence
Randomized Controlled Trials
A double-blind, sham-controlled trial of dry needling for the treatment of temporomandibular
myofascial pain was reported by Diracoglu et al (2012).
13
Patients (N=52) with symptoms for at
least 6 weeks with 2 or more myofascial trigger points in the temporomandibular muscles were
included in the trial. Trigger points were stimulated once weekly over three weeks. The sham
condition involved dry needling in areas away from the trigger points. Patients were evaluated
one week after the last needling. At follow-up, there was no significant difference between
groups in pain scores assessed by a 10-point VAS. Mean VAS scores were 3.88 in the
treatment group and 3.80 in the control group (p=.478). Also, the difference in unassisted jaw
opening without pain did not differ significantly between the treatment group (40.1 mm) and the
7
control group (39.6 mm; p=.411). The mean pain pressure threshold was significantly higher in
the treatment group (3.21 kg/cm
2
) than in the control group (2.75 kg/cm
2
; p<.001).
Section Summary: Temporomandibular Myofascial Pain
One RCT evaluating dry needling for the treatment of temporomandibular myofascial pain was
identified; this trial was double-blind and sham-controlled. One week after completing the
intervention, there were no statistically significant differences between groups in pain scores or
function (unassisted jaw opening without pain). There was a significantly higher pain pressure
threshold in the treatment group. This single RCT does not provide sufficient evidence on
which to draw conclusions about the impact of dry needling on health outcomes in patients
with temporomandibular myofascial pain.
Adverse Events
A prospective survey (2014) of 39 physical therapists, providing 7629 dry needling treatments,
reported 1463 (19.18%) mild adverse events (bruising, bleeding, pain) and no serious adverse
events.
14
Summary of Evidence
For individuals who have myofascial trigger points associated with neck and/or shoulder pain
who receive dry needling of trigger points, the evidence includes randomized controlled trials
(RCTs) and systematic reviews. The relevant outcomes are symptoms, functional outcomes,
QOL, and treatment-related morbidity. A systematic review of techniques to treat myofascial
pain included 15 studies of dry needling for neck or shoulder pain published through 2017.
Studies had multiple methodological limitations, and the reviewers concluded that the evidence
for dry needling was not greater than placebo. In more recent systematic reviews and meta-
analyses, dry needling was not associated with clinically important reductions in shoulder or
neck pain when compared to other physical therapy modalities. The evidence is insufficient to
determine that the technology results in an improvement in the net health outcome.
For individuals who have myofascial trigger points associated with plantar heel pain who
receive dry needling of trigger points, the evidence includes a systematic review of randomized
trials. Relevant outcomes are symptoms, functional outcomes, quality of life, and treatment-
related morbidity. The systematic review included 6 randomized trials enrolling 395 patients
and found no overall difference in pain intensity in those treated with dry needling compared
with active control, placebo, or no intervention. However, pain intensity after at least 3
sessions, long-term pain intensity, and pain-related disability were improved. The systematic
review rated the evidence as low to moderate. The evidence for dry needling in patients with
plantar heel pain is limited by small patient populations and lack of blinding; therefore,
additional RCTs are needed to strengthen the evidence base. The evidence is insufficient to
determine that the technology results in the net health outcome.
For individuals who have myofascial trigger points associated with temporomandibular
myofascial pain who receive dry needling of trigger points, the evidence includes an RCT. The
relevant outcomes are symptoms, functional outcomes, QOL, and treatment-related morbidity.
One double-blind, sham-controlled randomized trial was identified; it found that one week after
completing the intervention, there were no statistically significant differences between groups
in pain scores or function (unassisted jaw opening without pain). There was a significantly
higher pain pressure threshold in the treatment group. Additional RCTs, especially those with a

8
sham-control group, are needed. The evidence is insufficient to determine that the technology
results in the net health outcome.
SUPPLEMENTAL INFORMATION
Practice Guidelines and Position Statements
Guidelines or position statements will be considered for inclusion in ‘Supplemental Information'
if they were issued by, or jointly by, a US professional society, an international society with US
representation, or National Institute for Health and Care Excellence (NICE). Priority will be
given to guidelines that are informed by a systematic review, include strength of evidence
ratings, and include a description of management of conflict of interest.
American Academy of Orthopaedic Manual Physical Therapists
The American Academy of Orthopaedic Physical Therapists (2009) issued a statement that dry
needling fell within the scope of physical therapist practice.
15
In support of this position, the
Academy stated that “dry needling is a neurophysiological evidence-based treatment
technique that requires effective manual assessment of the neuromuscular system….
Research supports that dry needling improves pain control, reduces muscle tension,
normalizes biochemical and electrical dysfunction of motor endplates, and facilitates an
accelerated return to active rehabilitation.”
Ongoing and Unpublished Clinical Trials
Some currently unpublished trials that might influence this review are listed in Table 4.
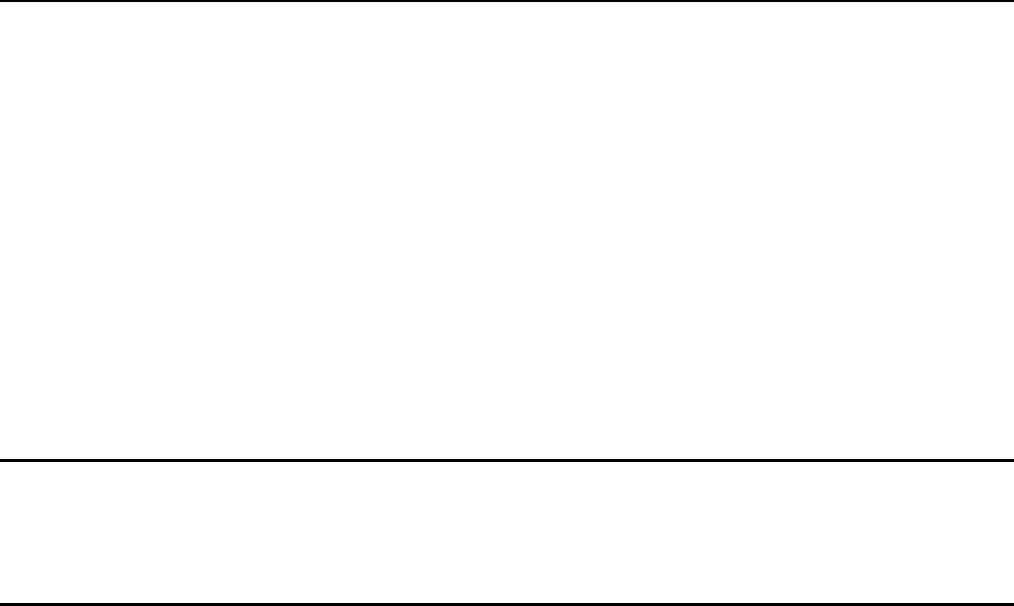
Table 4. Summary of Key Trials
NCT No.
Trial Name
Planned
Enrollment
Completion Date
NCT04851067
Dry Needling Versus Manual Therapy in Patients With Mechanical
Neck
Pain: A Randomized Control Trial
75
Mar 2022
NCT04726683
Trigger Point Dry Needling vs Injection in Patients With
Temporomandibular Disorders: A Randomized Placebo-controlled
Trial
80
Dec 2021
NCT03844802
Effectiveness of Real or Placebo Dry Needling Combined
With Therapeutic Exercise in Adults With Chronic Neck Pain
60
Mar 2022
NCT05624515
Efficacy of Dry Needling and Ischaemic Compression of the
Scapula Angularis Muscle in Patients With Cervicalgia.
Randomised Clinical Trial
80 Jan 2023
NCT05532098
Comparative Efficacy of Platelet Rich Plasma and Dry
Needling in Management of Anterior Disc Displacement of
Temporomandibular Joint
78 Mar 2023
NCT: national clinical trial.
9
Government Regulations
National:
There is no national coverage determination on dry needling of trigger points for myofascial
pain.
Local:
There is no local coverage determination on dry needling of trigger points for myofascial pain.
There is a LCD on Trigger Points, Local Injections (L34588, for services on or after
08/31/2023) which addresses only injections and not dry needling.
(The above Medicare information is current as of the review date for this policy. However, the coverage issues
and policies maintained by the Centers for Medicare & Medicare Services [CMS, formerly HCFA] are updated
and/or revised periodically. Therefore, the most current CMS information may not be contained in this
document. For the most current information, the reader should contact an official Medicare source.)
Related Policies
• Myofascial Trigger Point Injections-Dry Needling. Retired 07/01/15.
References
1. American Physical Therapy Association (APTA). Dry Needling. n.d.;
https://www.apta.org/patient-care/interventions/dry-needling. Accessed December 7, 2021.
2. Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician.
Feb 15 2002; 65(4):653-60. PMID 11871683
3. Charles D, Hudgins T, MacNaughton J, et al. A systematic review of manual therapy
techniques, dry cupping and dry needling in the reduction of myofascial pain and myofascial
trigger points. J Bodyw Mov Ther. Jul 2019; 23(3):539-546. PMID 31563367
4. Navarro-Santana MJ, Sanchez-Infante J, Fernandez-de-Las-Penas C, et al. Effectiveness
of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An
Updated Systematic Review and Meta-Analysis. J Clin Med. Oct 14 2020; 9(10). PMID
33066556
5. Navarro-Santana MJ, Gomez-Chiguano GF, Cleland JA, et al. Effects of Trigger Point Dry
Needling for Nontraumatic Shoulder Pain of Musculoskeletal Origin: A Systematic Review
and Meta-Analysis. Phys Ther. Feb04 2021; 101(2). PMID 33340405
6. Llurda-Almuzara L, Labata-Lezaun N, Meca-Rivera T, et al. Is Dry Needling Effective for the
Management of Plantar Heel Pain or Plantar Fasciitis? An Updated Systematic Review and
Meta-Analysis. Pain Med. Jul 25 2021; 22(7): 1630-1641. PMID 33760098
7. Bagcier F, Yilmaz N. The Impact of Extracorporeal Shock Wave Therapy and Dry Needling
Combination on Pain and Functionality in the Patients Diagnosed with Plantar Fasciitis. J
Foot Ankle Surg. Jul 2020; 59(4): 689-693. PMID 32340838
8. Cotchett MP, Munteanu SE, Landorf KB. Effectiveness of trigger point dry needling for
plantar heel pain: a randomized controlled trial. Phys Ther. Aug 2014; 94(8): 1083-94. PMID
24700136
9. Eftekharsadat B, Babaei-Ghazani A, Zeinolabedinzadeh V. Dry needling in patients with

10
chronic heel pain due to plantar fasciitis: A single-blinded randomized clinical trial. Med J
Islam Repub Iran. 2016; 30: 401. PMID 27683642
10. Rahbar M, Kargar A, Eslamian F, Dolatkhah N. Comparing the efficacy of dry needling and
extracorporeal shock wave therapy in treatment of plantar fasciitis. J Mazandaran Univ
Med Sci. 2018;28(164):53-62.
11. Rastegar S, Baradaran Mahdavi S, Hoseinzadeh B, et al. Comparison of dry needling and
steroid injection in the treatment of plantar fasciitis: a single-blind randomized clinical trial.
Int Orthop. Jan 2018; 42(1): 109-116. PMID 29119296
12. Uygur E, Aktas B, Eceviz E, et al. Preliminary Report on the Role of Dry Needling Versus
Corticosteroid Injection, an Effective Treatment Method for Plantar Fasciitis: A Randomized
Controlled Trial. J Foot Ankle Surg. Mar 2019; 58(2): 301-305. PMID 30850099
13. Diracoglu D, Vural M, Karan A, et al. Effectiveness of dry needling for the treatment of
temporomandibular myofascial pain: a double-blind, randomized, placebo controlled study.
J Back Musculoskelet Rehabil. 2012; 25(4):285-90. PMID 23220812
14. Brady S, McEvoy J, Dommerholt J, et al. Adverse events following trigger point dry
needling: a prospective survey of chartered physiotherapists. J Man Manip Ther. Aug
2014; 22(3): 134-40. PMID 25125935
15. American Academy of Orthopaedic Physical Therapists. AAOMPT position statement on
dry needling. 2009;
http://aaompt.org/Main/About_Us/Position_Statements/Main/About_Us/Position_Statement
s.aspx?hkey=03f5a333-f28d-4715-b355-cb25fa9bac2c. Accessed January 6, 2023.
16. Para-García G, García-Muñoz AM, López-Gil JF, et al. Dry Needling Alone or in
Combination with Exercise Therapy versus Other Interventions for Reducing Pain and
Disability in Subacromial Pain Syndrome: A Systematic Review and Meta-Analysis. Int J
Environ Res Public Health. Sep 02 2022; 19(17). PMID 36078676
The articles reviewed in this research include those obtained in an Internet based literature search
for relevant medical references through December 6, 2023, the date the research was completed.

11
Joint BCBSM/BCN Medical Policy History
Policy
Effective Date
BCBSM
Signature Date
BCN
Signature Date
Comments
02/24/03 02/24/03 02/14/03 Joint policy established titled
Myofascial Trigger Points
03/21/05 03/21/05 02/28/05 Routine maintenance; policy retired.
07/01/15 04/21/15 05/08/15 Policy taken out of retirement, added
information on dry needling, also
added to title. Policy re-retired.
5/1/20 2/18/20 Unretired, completely rewritten with
focus on dry needling. Remains as
E/I service.
5/1/21 2/16/21 Routine maintenance. Reference 4
added. Policy statement unchanged.
Title changed from “Dry Needling of
Myofascial Trigger Points” to “Dry
Needling of Trigger Points for
Myofascial Pain”.
5/1/22 2/15/22 Routine maintenance. References
added; some references removed.
Policy statement unchanged.
5/1/23 2/21/23 Routine maintenance. Policy
statement unchanged. Vendor
Review: NA. (ky)
5/1/24 2/20/24 Routine maintenance. Policy
statement unchanged. Vendor
Review: NA. (ky)
Next Review Date: 1
st
Qtr. 2025
Pre-Consolidation Medical Policy History
Original Policy Date Comments
BCN: Revised:
BCBSM: Revised:

12
BLUE CARE NETWORK BENEFIT COVERAGE
P
OLICY: DRY NEEDLING OF TRIGGER POINTS FOR MYOFASCIAL PAIN
I. Coverage Determination:
Commercial HMO
(includes Self-Funded
groups unless otherwise
specified)
Not covered
BCNA (Medicare
Advantage)
See government section
BCN65 (Medicare
Complementary)
Coinsurance covered if primary Medicare covers the
service.
II. Administrative Guidelines:
• The member's contract must be active at the time the service is rendered.
• Coverage is based on each member’s certificate and is not guaranteed. Please
consult the individual member’s certificate for details. Additional information regarding
coverage or benefits may also be obtained through customer or provider inquiry
services at BCN.
• The service must be authorized by the member's PCP except for Self-Referral Option
(SRO) members seeking Tier 2 coverage.
• Services must be performed by a BCN-contracted provider, if available, except for
Self-Referral Option (SRO) members seeking Tier 2 coverage.
• Payment is based on BCN payment rules, individual certificate and certificate riders.
• Appropriate copayments will apply. Refer to certificate and applicable riders for
detailed information.
• CPT - HCPCS codes are used for descriptive purposes only and are not a guarantee
of coverage.
• Duplicate (back-up) equipment is not a covered benefit.
