
1
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
To download a clean version of the SCAT tools please visit the journal online (http://dx.doi.org/10.1136/bjsports-2017-097506SCAT5)
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017
SCAT5©
WHAT IS THE SCAT5?
The SCAT5 is a standardized tool for evaluating concussions
designed for use by physicians and licensed healthcare
professionals
1
. The SCAT5 cannot be performed correctly
in less than 10 minutes.
If you are not a physician or licensed healthcare professional,
please use the Concussion Recognition Tool 5 (CRT5). The
SCAT5 is to be used for evaluating athletes aged 13 years
and older. For children aged 12 years or younger, please
use the Child SCAT5.
Preseason SCAT5 baseline testing can be useful for
interpreting post-injury test scores, but is not required for
that purpose.Detailed instructions for use of the SCAT5 are
provided on page 7. Please read through these instructions
carefully before testing the athlete. Brief verbal instructions
for each test are given in italics. The only equipment required
for the tester is a watch or timer.
This tool may be freely copied in its current form for dis-
tribution to individuals, teams, groups and organizations.
It should not be altered in any way, re-branded or sold for
commercial gain. Any revision, translation or reproduction
in a digital form requires specic approval by the Concus-
sion in Sport Group.
Recognise and Remove
A head impact by either a direct blow or indirect transmission
of force can be associated with a serious and potentially fatal
brain injury. If there are signicant concerns, including any
of the red ags listed in Box 1, then activation of emergency
procedures and urgent transport to the nearest hospital
should be arranged.
Patient details
Name:
DOB:
Address:
ID number:
Examiner:
Date of Injury: Time:
Key points
•
Any athlete with suspected concussion should be REMOVED
FROM PLAY, medically assessed and monitored for
deterioration. No athlete diagnosed with concussion
should be returned to play on the day of injury.
•
If an athlete is suspected of having a concussion and
medical personnel are not immediately available, the
athlete should be referred to a medical facility for urgent
assessment.
•
Athletes with suspected concussion should not drink
alcohol, use recreational drugs and should not drive a motor
vehicle until cleared to do so by a medical professional.
• Concussion signs and symptoms evolve over time and it
is important to consider repeat evaluation in the assess-
ment of concussion.
•
The diagnosis of a concussion is a clinical judgment,
made by a medical professional. The SCAT5 should NOT
be used by itself to make, or exclude, the diagnosis of
concussion. An athlete may have a concussion even if
their SCAT5 is “normal”.
Remember:
•
The basic principles of rst aid (danger, response, airway,
breathing, circulation) should be followed.
•
Do not attempt to move the athlete (other than that required
for airway management) unless trained to do so.
•
Assessment for a spinal cord injury is a critical part of the
initial on-eld assessment.
•
Do not remove a helmet or any other equipment unless
trained to do so safely.
SPORT CONCUSSION ASSESSMENT TOOL — 5TH EDITION
DEVELOPED BY THE CONCUSSION IN SPORT GROUP
FOR USE BY MEDICAL PROFESSIONALS ONLY
supported by
1
BJSM Online First, published on April 26, 2017 as 10.1136/bjsports-2017-097506SCAT5
Copyright Article author (or their employer) 2017. Produced by BMJ Publishing Group Ltd under licence.
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from

2
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017 2
IMMEDIATE OR ON-FIELD ASSESSMENT
The following elements should be assessed for all athletes who
are suspected of having a concussion prior to proceeding to the
neurocognitive assessment and ideally should be done on-eld after
the rst rst aid / emergency care priorities are completed.
If any of the “Red Flags“ or observable signs are noted after a direct
or indirect blow to the head, the athlete should be immediately and
safely removed from participation and evaluated by a physician or
licensed healthcare professional.
Consideration of transportation to a medical facility should be at
the discretion of the physician or licensed healthcare professional.
The GCS is important as a standard measure for all patients and can
be done serially if necessary in the event of deterioration in conscious
state. The Maddocks questions and cervical spine exam are critical
steps of the immediate assessment; however, these do not need to
be done serially.
STEP 1: RED FLAGS
STEP 2: OBSERVABLE SIGNS
Witnessed Observed on Video
Lying motionless on the playing surface Y N
Balance / gait difculties / motor incoordination: stumbling, slow /
laboured movements
Y N
Disorientation or confusion, or an inability to respond appropriately
to questions
Y N
Blank or vacant look Y N
Facial injury after head trauma Y N
STEP 3: MEMORY ASSESSMENT
MADDOCKS QUESTIONS
2
“I am going to ask you a few questions, please listen carefully and
give your best effort. First, tell me what happened?”
Mark Y for correct answer / N for incorrect
What venue are we at today? Y N
Which half is it now? Y N
Who scored last in this match? Y N
What team did you play last week / game? Y N
Did your team win the last game? Y N
Note: Appropriate sport-specific questions may be substituted.
STEP 4: EXAMINATION
GLASGOW COMA SCALE (GCS)
3
Time of assessment
Date of assessment
Best eye response (E)
No eye opening 1 1 1
Eye opening in response to pain 2 2 2
Eye opening to speech 3 3 3
Eyes opening spontaneously 4 4 4
Best verbal response (V)
No verbal response 1 1 1
Incomprehensible sounds 2 2 2
Inappropriate words 3 3 3
Confused 4 4 4
Oriented 5 5 5
Best motor response (M)
No motor response 1 1 1
Extension to pain 2 2 2
Abnormal exion to pain 3 3 3
Flexion / Withdrawal to pain 4 4 4
Localizes to pain 5 5 5
Obeys commands 6 6 6
Glasgow Coma score (E + V + M)
CERVICAL SPINE ASSESSMENT
Does the athlete report that their neck is pain free at rest?
Y N
If there is NO neck pain at rest, does the athlete have a full
range of ACTIVE pain free movement?
Y N
Is the limb strength and sensation normal? Y N
In a patient who is not lucid or fully
conscious, a cervical spine injury should
be assumed until proven otherwise.
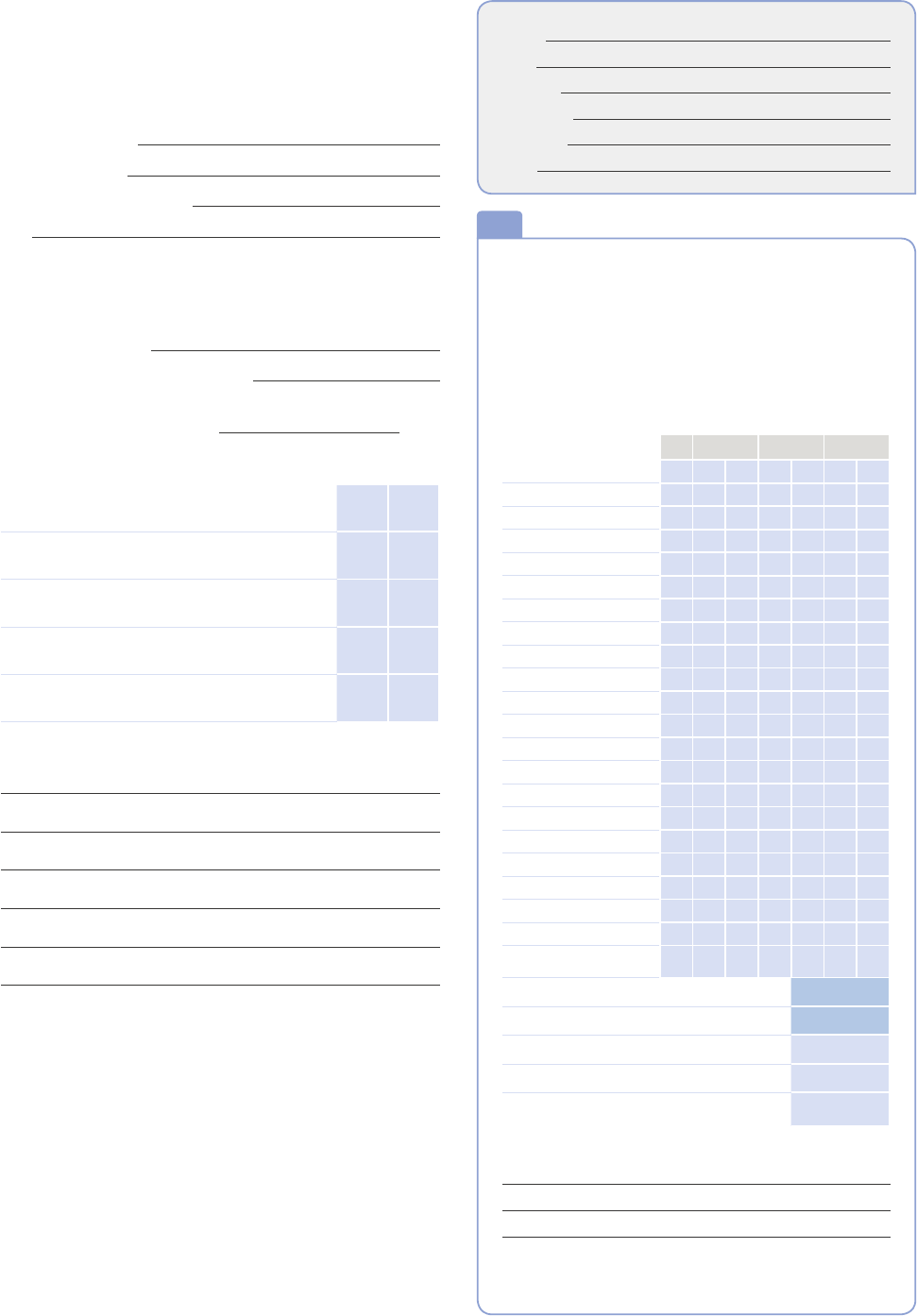
RED FLAGS:
• Neck pain or
tenderness
• Double vision
• Weakness or tingling/
burning in arms or legs
• Severe or increasing
headache
• Seizure or convulsion
• Loss of consciousness
• Deteriorating
conscious state
• Vomiting
• Increasingly restless,
agitated or combative
1
Name:
DOB:
Address:
ID number:
Examiner:
Date:
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from
3
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
Name:
DOB:
Address:
ID number:
Examiner:
Date:
SCAT5 © Concussion in Sport Group 2017 3
OFFICE OR OFF-FIELD ASSESSMENT
Please note that the neurocognitive assessment should be done in a
distraction-free environment with the athlete in a resting state.
STEP 1: ATHLETE BACKGROUND
Sport / team / school:
Date / time of injury:
Years of education completed:
Age:
Gender: M / F / Other
Dominant hand: left / neither / right
How many diagnosed concussions has the
athlete had in the past?:
When was the most recent concussion?:
How long was the recovery (time to being cleared to play)
from the most recent concussion?: (days)
Has the athlete ever been:
Hospitalized for a head injury? Yes No
Diagnosed / treated for headache disorder or migraines? Yes No
Diagnosed with a learning disability / dyslexia? Yes No
Diagnosed with ADD / ADHD? Yes No
Diagnosed with depression, anxiety
or other psychiatric disorder?
Yes No
Current medications? If yes, please list:
STEP 2: SYMPTOM EVALUATION
The athlete should be given the symptom form and asked to read this instruction
paragraph out loud then complete the symptom scale. For the baseline assessment,
the athlete should rate his/her symptoms based on how he/she typically feels and for
the post injury assessment the athlete should rate their symptoms at this point in time.
Please Check: Baseline Post-Injury
Please hand the form to the athlete
none mild moderate severe
Headache
0 1 2 3 4 5 6
“Pressure in head” 0 1 2 3 4 5 6
Neck Pain 0 1 2 3 4 5 6
Nausea or vomiting 0 1 2 3 4 5 6
Dizziness 0 1 2 3 4 5 6
Blurred vision 0 1 2 3 4 5 6
Balance problems 0 1 2 3 4 5 6
Sensitivity to light 0 1 2 3 4 5 6
Sensitivity to noise 0 1 2 3 4 5 6
Feeling slowed down 0 1 2 3 4 5 6
Feeling like “in a fog“ 0 1 2 3 4 5 6
“Don’t feel right” 0 1 2 3 4 5 6
Difculty concentrating 0 1 2 3 4 5 6
Difculty remembering 0 1 2 3 4 5 6
Fatigue or low energy 0 1 2 3 4 5 6
Confusion 0 1 2 3 4 5 6
Drowsiness 0 1 2 3 4 5 6
More emotional 0 1 2 3 4 5 6
Irritability 0 1 2 3 4 5 6
Sadness 0 1 2 3 4 5 6
Nervous or Anxious 0 1 2 3 4 5 6
Trouble falling asleep
(if applicable)
0 1 2 3 4 5 6
Total number of symptoms:
of 22
Symptom severity score: of 132
Do your symptoms get worse with physical activity? Y N
Do your symptoms get worse with mental activity? Y N
If 100% is feeling perfectly normal, what
percent of normal do you feel?
If not 100%, why?
Please hand form back to examiner
2
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from

4
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017 4
STEP 3: COGNITIVE SCREENING
Standardised Assessment of Concussion (SAC)
4
ORIENTATION
What month is it? 0 1
What is the date today? 0 1
What is the day of the week? 0 1
What year is it? 0 1
What time is it right now? (within 1 hour) 0 1
Orientation score of 5
IMMEDIATE MEMORY
The Immediate Memory component can be completed using the
traditional 5-word per trial list or optionally using 10-words per trial
to minimise any ceiling effect. All 3 trials must be administered irre-
spective of the number correct on the rst trial. Administer at the rate
of one word per second.
Please choose EITHER the 5 or 10 word list groups and circle the specic word list chosen
for this test.
I am going to test your memory. I will read you a list of words and when I am done, repeat
back as many words as you can remember, in any order. For Trials 2 & 3: I am going to repeat
the same list again. Repeat back as many words as you can remember in any order, even if
you said the word before.
List Alternate 5 word lists
Score (of 5)
Trial 1 Trial 2 Trial 3
A Finger Penny Blanket Lemon Insect
B Candle Paper Sugar Sandwich Wagon
C Baby Monkey Perfume Sunset Iron
D Elbow Apple Carpet Saddle Bubble
E Jacket Arrow Pepper Cotton Movie
F Dollar Honey Mirror Saddle Anchor
Immediate Memory Score of 15
Time that last trial was completed
List Alternate 10 word lists
Score (of 10)
Trial 1 Trial 2 Trial 3
G
Finger
Candle
Penny
Paper
Blanket
Sugar
Lemon
Sandwich
Insect
Wagon
H
Baby
Elbow
Monkey
Apple
Perfume
Carpet
Sunset
Saddle
Iron
Bubble
I
Jacket
Dollar
Arrow
Honey
Pepper
Mirror
Cotton
Saddle
Movie
Anchor
Immediate Memory Score of 30
Time that last trial was completed
CONCENTRATION
DIGITS BACKWARDS
Please circle the Digit list chosen (A, B, C, D, E, F). Administer at the
rate of one digit per second reading DOWN the selected column.
I am going to read a string of numbers and when I am done, you repeat them back to me
in reverse order of how I read them to you. For example, if I say 7-1-9, you would say 9-1-7.
Concentration Number Lists (circle one)
List A List B List C
4-9-3 5-2-6 1-4-2 Y N
0
1
6-2-9 4-1-5 6-5-8 Y N
3-8-1-4 1-7-9-5 6-8-3-1 Y N
0
1
3-2-7-9 4-9-6-8 3-4-8-1 Y N
6-2-9-7-1 4-8-5-2-7 4-9-1-5-3 Y N
0
1
1-5-2-8-6 6-1-8-4-3 6-8-2-5-1 Y N
7-1-8-4-6-2 8-3-1-9-6-4 3-7-6-5-1-9 Y N
0
1
5-3-9-1-4-8 7-2-4-8-5-6 9-2-6-5-1-4 Y N
List D List E List F
7-8-2 3-8-2 2-7-1 Y N
0
1
9-2-6 5-1-8 4-7-9 Y N
4-1-8-3 2-7-9-3 1-6-8-3 Y N
0
1
9-7-2-3 2-1-6-9 3-9-2-4 Y N
1-7-9-2-6 4-1-8-6-9 2-4-7-5-8 Y N
0
1
4-1-7-5-2 9-4-1-7-5 8-3-9-6-4 Y N
2-6-4-8-1-7 6-9-7-3-8-2 5-8-6-2-4-9 Y N
0
1
8-4-1-9-3-5 4-2-7-9-3-8 3-1-7-8-2-6 Y N
Digits Score: of 4
MONTHS IN REVERSE ORDER
Now tell me the months of the year in reverse order. Start with the last month and go backward.
So you’ll say December, November. Go ahead.
Dec - Nov - Oct - Sept - Aug - Jul - Jun - May - Apr - Mar - Feb - Jan 0 1
Months Score of 1
Concentration Total Score (Digits + Months) of 5
3
Name:
DOB:
Address:
ID number:
Examiner:
Date:
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from

5
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
Name:
DOB:
Address:
ID number:
Examiner:
Date:
SCAT5 © Concussion in Sport Group 2017 5
STEP 4: NEUROLOGICAL SCREEN
See the instruction sheet (page 7) for details of
test administration and scoring of the tests.
Can the patient read aloud (e.g. symptom check-
list) and follow instructions without difculty?
Y N
Does the patient have a full range of pain-
free PASSIVE cervical spine movement?
Y N
Without moving their head or neck, can the patient look
side-to-side and up-and-down without double vision?
Y N
Can the patient perform the nger nose
coordination test normally?
Y N
Can the patient perform tandem gait normally? Y N
BALANCE EXAMINATION
Modified Balance Error Scoring System (mBESS) testing
5
Which foot was tested
(i.e. which is the non-dominant foot)
Left
Right
Testing surface (hard oor, eld, etc.)
Footwear (shoes, barefoot, braces, tape, etc.)
Condition Errors
Double leg stance of 10
Single leg stance (non-dominant foot) of 10
Tandem stance (non-dominant foot at the back) of 10
Total Errors of 30
STEP 5: DELAYED RECALL:
The delayed recall should be performed after 5 minutes have
elapsed since the end of the Immediate Recall section. Score 1
pt. for each correct response.
Do you remember that list of words I read a few times earlier? Tell me as many words
from the list as you can remember in any order.
Time Started
Please record each word correctly recalled. Total score equals number of words recalled.
Total number of words recalled accurately: of 5 or of 10
4
5
STEP 6: DECISION
Domain
Date & time of assessment:
Symptom
number (of 22)
Symptom severity
score (of 132)
Orientation (of 5)
Immediate memory
of 15
of 30
of 15
of 30
of 15
of 30
Concentration (of 5)
Neuro exam
Normal
Abnormal
Normal
Abnormal
Normal
Abnormal
Balance errors (of 30)
Delayed Recall
of 5
of 10
of 5
of 10
of 5
of 10
Date and time of injury:
If the athlete is known to you prior to their injury, are they different from their usual self?
Yes No Unsure Not Applicable
(If different, describe why in the clinical notes section)
Concussion Diagnosed?
Yes No Unsure Not Applicable
If re-testing, has the athlete improved?
Yes No Unsure Not Applicable
I am a physician or licensed healthcare professional and I have personally
administered or supervised the administration of this SCAT5.
Signature:
Name:
Title:
Registration number (if applicable):
Date:
6
SCORING ON THE SCAT5 SHOULD NOT BE USED AS A STAND-ALONE
METHOD TO DIAGNOSE CONCUSSION, MEASURE RECOVERY OR
MAKE DECISIONS ABOUT AN ATHLETE’S READINESS TO RETURN TO
COMPETITION AFTER CONCUSSION.
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from
6
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017 6
CLINICAL NOTES:
Name:
DOB:
Address:
ID number:
Examiner:
Date:
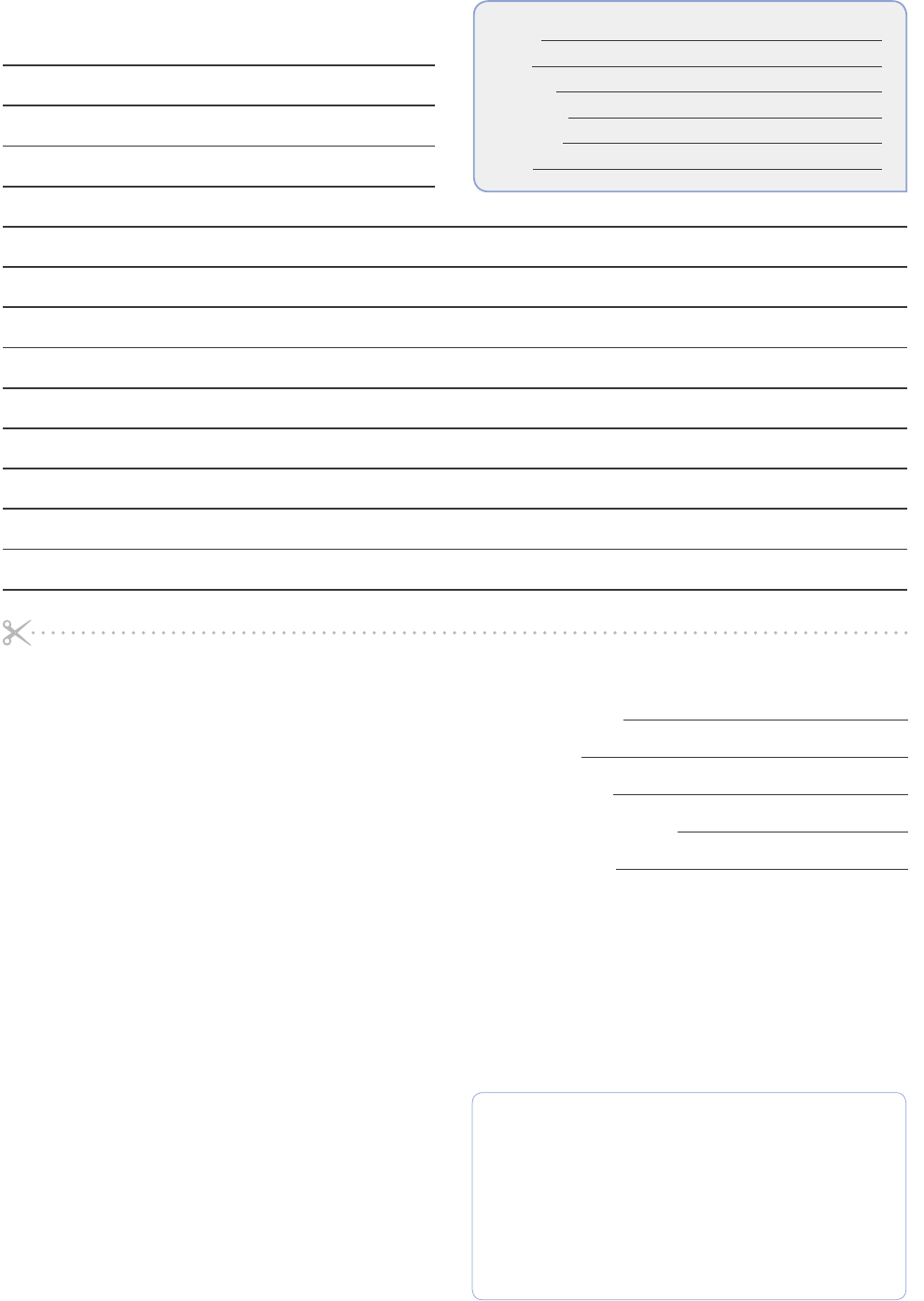
CONCUSSION INJURY ADVICE
(To be given to the person monitoring the concussed athlete)
This patient has received an injury to the head. A careful medical
examination has been carried out and no sign of any serious
complications has been found. Recovery time is variable across
individuals and the patient will need monitoring for a further pe-
riod by a responsible adult. Your treating physician will provide
guidance as to this timeframe.
If you notice any change in behaviour, vomiting, worsening head-
ache, double vision or excessive drowsiness, please telephone
your doctor or the nearest hospital emergency department
immediately.
Other important points:
Initial rest: Limit physical activity to routine daily activities (avoid
exercise, training, sports) and limit activities such as school,
work, and screen time to a level that does not worsen symptoms.
1) Avoid alcohol
2) Avoid prescription or non-prescription drugs
without medical supervision. Specically:
a) Avoid sleeping tablets
b) Do not use aspirin, anti-inammatory medication
or stronger pain medications such as narcotics
3) Do not drive until cleared by a healthcare professional.
4) Return to play/sport requires clearance
by a healthcare professional.
Clinic phone number:
Patient’s name:
Date / time of injury:
Date / time of medical review:
Healthcare Provider:
Contact details or stamp
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from
7
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017 7
INSTRUCTIONS
Words in Italics throughout the SCAT5 are the instructions given to the athlete by the clinician
Symptom Scale
The time frame for symptoms should be based on the type of test being admin-
istered. At baseline it is advantageous to assess how an athlete “typically” feels
whereas during the acute/post-acute stage it is best to ask how the athlete feels
at the time of testing.
The symptom scale should be completed by the athlete, not by the examiner. In
situations where the symptom scale is being completed after exercise, it should
be done in a resting state, generally by approximating his/her resting heart rate.
For total number of symptoms, maximum possible is 22 except immediately post
injury, if sleep item is omitted, which then creates a maximum of 21.
For Symptom severity score, add all scores in table, maximum possible is 22 x 6
= 132, except immediately post injury if sleep item is omitted, which then creates
a maximum of 21x6=126.
Immediate Memory
The Immediate Memory component can be completed using the traditional 5-word
per trial list or, optionally, using 10-words per trial. The literature suggests that
the Immediate Memory has a notable ceiling effect when a 5-word list is used. In
settings where this ceiling is prominent, the examiner may wish to make the task
more difcult by incorporating two 5–word groups for a total of 10 words per trial.
In this case, the maximum score per trial is 10 with a total trial maximum of 30.
Choose one of the word lists (either 5 or 10). Then perform 3 trials of immediate
memory using this list.
Complete all 3 trials regardless of score on previous trials.
“I am going to test your memory. I will read you a list of words and when I am done,
repeat back as many words as you can remember, in any order.” The words must be
read at a rate of one word per second.
Trials 2 & 3 MUST be completed regardless of score on trial 1 & 2.
Trials 2 & 3:
“I am going to repeat the same list again. Repeat back as many words as you can
remember in any order, even if you said the word before.“
Score 1 pt. for each correct response. Total score equals sum across all 3 trials.
Do NOT inform the athlete that delayed recall will be tested.
Concentration
Digits backward
Choose one column of digits from lists A, B, C, D, E or F and administer those digits
as follows:
Say: “I am going to read a string of numbers and when I am done, you repeat them
back to me in reverse order of how I read them to you. For example, if I say 7-1-9,
you would say 9-1-7.”
Begin with rst 3 digit string.
If correct, circle “Y” for correct and go to next string length. If incorrect, circle “N” for
the rst string length and read trial 2 in the same string length. One point possible
for each string length. Stop after incorrect on both trials (2 N’s) in a string length.
The digits should be read at the rate of one per second.
Months in reverse order
“Now tell me the months of the year in reverse order. Start with the last month and
go backward. So you’ll say December, November ... Go ahead”
1 pt. for entire sequence correct
Delayed Recall
The delayed recall should be performed after 5 minutes have elapsed since the end
of the Immediate Recall section.
“Do you remember that list of words I read a few times earlier? Tell me as many words
from the list as you can remember in any order.“
Score 1 pt. for each correct response
Modied Balance Error Scoring System (mBESS)
5
testing
This balance testing is based on a modied version of the Balance Error Scoring
System (BESS)
5
. A timing device is required for this testing.
Each of 20-second trial/stance is scored by counting the number of errors. The
examiner will begin counting errors only after the athlete has assumed the proper
start position. The modied BESS is calculated by adding one error point for each
error during the three 20-second tests. The maximum number of errors for any
single condition is 10. If the athlete commits multiple errors simultaneously, only
one error is recorded but the athlete should quickly return to the testing position, and
counting should resume once the athlete is set. Athletes that are unable to maintain
the testing procedure for a minimum of ve seconds at the start are assigned the
highest possible score, ten, for that testing condition.
OPTION: For further assessment, the same 3 stances can be performed on a surface
of medium density foam (e.g., approximately 50cm x 40cm x 6cm).
Balance testing – types of errors
1. Hands lifted off
iliac crest
2. Opening eyes
3. Step, stumble, or fall
4. Moving hip into > 30
degrees abduction
5. Lifting forefoot or heel
6. Remaining out of test
position > 5 sec
“I am now going to test your balance. Please take your shoes off (if applicable), roll up
your pant legs above ankle (if applicable), and remove any ankle taping (if applicable).
This test will consist of three twenty second tests with different stances.“
(a) Double leg stance:
“The rst stance is standing with your feet together with your hands on your hips
and with your eyes closed. You should try to maintain stability in that position for 20
seconds. I will be counting the number of times you move out of this position. I will
start timing when you are set and have closed your eyes.“
(b) Single leg stance:
“If you were to kick a ball, which foot would you use? [This will be the dominant
foot] Now stand on your non-dominant foot. The dominant leg should be held in
approximately 30 degrees of hip exion and 45 degrees of knee exion. Again, you
should try to maintain stability for 20 seconds with your hands on your hips and your
eyes closed. I will be counting the number of times you move out of this position. If
you stumble out of this position, open your eyes and return to the start position and
continue balancing. I will start timing when you are set and have closed your eyes.“
(c) Tandem stance:
“Now stand heel-to-toe with your non-dominant foot in back. Your weight should be
evenly distributed across both feet. Again, you should try to maintain stability for 20
seconds with your hands on your hips and your eyes closed. I will be counting the
number of times you move out of this position. If you stumble out of this position,
open your eyes and return to the start position and continue balancing. I will start
timing when you are set and have closed your eyes.”
Tandem Gait
Participants are instructed to stand with their feet together behind a starting line
(the test is best done with footwear removed). Then, they walk in a forward direction
as quickly and as accurately as possible along a 38mm wide (sports tape), 3 metre
line with an alternate foot heel-to-toe gait ensuring that they approximate their heel
and toe on each step. Once they cross the end of the 3m line, they turn 180 degrees
and return to the starting point using the same gait. Athletes fail the test if they
step off the line, have a separation between their heel and toe, or if they touch or
grab the examiner or an object.
Finger to Nose
“I am going to test your coordination now. Please sit comfortably on the chair with
your eyes open and your arm (either right or left) outstretched (shoulder exed to
90 degrees and elbow and ngers extended), pointing in front of you. When I give
a start signal, I would like you to perform ve successive nger to nose repetitions
using your index nger to touch the tip of the nose, and then return to the starting
position, as quickly and as accurately as possible.”
References
1.
McCrory et al. Consensus Statement On Concussion In Sport – The 5th
International Conference On Concussion In Sport Held In Berlin, October 2016.
British Journal of Sports Medicine 2017 (available at www.bjsm.bmj.com)
2.
Maddocks, DL; Dicker, GD; Saling, MM. The assessment of orientation following
concussion in athletes. Clinical Journal of Sport Medicine 1995; 5: 32-33
3. Jennett, B., Bond, M. Assessment of outcome after severe brain damage: a
practical scale. Lancet 1975; i: 480-484
4.
McCrea M. Standardized mental status testing of acute concussion. Clinical
Journal of Sport Medicine. 2001; 11: 176-181
5.
Guskiewicz KM. Assessment of postural stability following sport-related
concussion. Current Sports Medicine Reports. 2003; 2: 24-30
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from

8
Davis GA, et al. Br J Sports Med 2017;0:1–8. doi:10.1136/bjsports-2017-097506SCAT5
© Concussion in Sport Group 2017
SCAT5 © Concussion in Sport Group 2017 8
CONCUSSION INFORMATION
Any athlete suspected of having a concussion should be removed from
play and seek medical evaluation.
Signs to watch for
Problems could arise over the rst 24-48 hours. The athlete should not be
left alone and must go to a hospital at once if they experience:
• Worsening
headache
• Drowsiness or
inability to be
awakened
• Inability to
recognize people
or places
• Repeated vomiting
• Unusual behaviour
or confusion
or irritable
• Seizures (arms
and legs jerk
uncontrollably)
• Weakness or
numbness in
arms or legs
• Unsteadiness
on their feet.
• Slurred speech
Consult your physician or licensed healthcare professional after a sus-
pected concussion. Remember, it is better to be safe.
Rest & Rehabilitation
After a concussion, the athlete should have physical rest and relative
cognitive rest for a few days to allow their symptoms to improve. In most
cases, after no more than a few days of rest, the athlete should gradually
increase their daily activity level as long as their symptoms do not worsen.
Once the athlete is able to complete their usual daily activities without
concussion-related symptoms, the second step of the return to play/sport
progression can be started. The athlete should not return to play/sport
until their concussion-related symptoms have resolved and the athlete
has successfully returned to full school/learning activities.
When returning to play/sport, the athlete should follow a stepwise,
medically managed exercise progression, with increasing amounts of
exercise. For example:
Graduated Return to Sport Strategy
Exercise step
Functional exercise
at each step
Goal of each step
1. Symptom-
limited activity
Daily activities that do
not provoke symptoms.
Gradual reintroduc-
tion of work/school
activities.
2. Light aerobic
exercise
Walking or stationary
cycling at slow to medium
pace. No resistance
training.
Increase heart rate.
3. Sport-specic
exercise
Running or skating drills.
No head impact activities.
Add movement.
4. Non-contact
training drills
Harder training drills, e.g.,
passing drills. May start
progressive resistance
training.
Exercise, coor-
dination, and
increased thinking.
5. Full contact
practice
Following medical clear-
ance, participate in normal
training activities.
Restore con-
dence and assess
functional skills by
coaching staff.
6. Return to
play/sport
Normal game play.
In this example, it would be typical to have 24 hours (or longer) for each
step of the progression. If any symptoms worsen while exercising, the
athlete should go back to the previous step. Resistance training should
be added only in the later stages (Stage 3 or 4 at the earliest).
Written clearance should be provided by a healthcare professional before
return to play/sport as directed by local laws and regulations.
Graduated Return to School Strategy
Concussion may affect the ability to learn at school. The athlete may
need to miss a few days of school after a concussion. When going back
to school, some athletes may need to go back gradually and may need to
have some changes made to their schedule so that concussion symptoms
do not get worse. If a particular activity makes symptoms worse, then the
athlete should stop that activity and rest until symptoms get better. To
make sure that the athlete can get back to school without problems, it is
important that the healthcare provider, parents, caregivers and teachers
talk to each other so that everyone knows what the plan is for the athlete
to go back to school.
Note: If mental activity does not cause any symptoms, the athlete may
be able to skip step 2 and return to school part-time before doing school
activities at home rst.
Mental Activity Activity at each step
Goal of
each step
1. Daily activities
that do
not give
the athlete
symptoms
Typical activities that the athlete
does during the day as long as
they do not increase symptoms
(e.g. reading, texting, screen
time). Start with 5-15 minutes at
a time and gradually build up.
Gradual
return to
typical
activities.
2. School
activities
Homework, reading or other
cognitive activities outside of
the classroom.
Increase
tolerance
to cognitive
work.
3. Return to
school
part-time
Gradual introduction of school-
work. May need to start with
a partial school day or with
increased breaks during the day.
Increase
academic
activities.
4. Return to
school
full-time
Gradually progress school
activities until a full day can be
tolerated.
Return to full
academic
activities and
catch up on
missed work.
If the athlete continues to have symptoms with mental activity, some
other accomodations that can help with return to school may include:
• Starting school later, only
going for half days, or going
only to certain classes
• More time to nish
assignments/tests
• Quiet room to nish
assignments/tests
• Not going to noisy areas
like the cafeteria, assembly
halls, sporting events, music
class, shop class, etc.
• Taking lots of breaks during
class, homework, tests
• No more than one exam/day
• Shorter assignments
• Repetition/memory cues
• Use of a student helper/tutor
• Reassurance from teachers
that the child will be supported
while getting better
The athlete should not go back to sports until they are back to school/
learning, without symptoms getting signicantly worse and no longer
needing any changes to their schedule.
on September 17, 2024 by guest. Protected by copyright.http://bjsm.bmj.com/Br J Sports Med: first published as 10.1136/bjsports-2017-097506SCAT5 on 26 April 2017. Downloaded from
