
CENTER FOR DRUG EVALUATION AND
RESEARCH
APPLICATION NUMBER:
211243Orig1s000
NON-CLINICAL REVIEW(S)

Secondary Pharmacology/Toxicology Review:
By: Ikram M. Elayan, PhD, Pharmacology/Toxicology Supervisor, Division of Psychiatry Products
NDA: 211243
Submission date: September 4, 2018
PDUFA goal date: March 4, 2019
Drug: SPRAVATO® (esketamine)
Applicant: Janssen Pharmaceuticals, Inc.
Indication: Treatment-resistant depression in adults
Background: This is a 505(b)1 application for esketamine (SPRAVATO®) for the treatment of adults with
treatment-resistant depression (TRD) to be administered intranasally. The proposed clinical treatment
paradigm is twice weekly for four weeks as an induction phase followed by a maintenance phase of once
weekly for four weeks and then once a week or every other week for continued maintenance. The
maximum recommended human dose (MRHD) is 84 mg.
Esketamine is a non-competitive antagonist to the glutamate N-methyl-D-aspartate (NMDA) receptor. The
sponsor conducted a comprehensive non-clinical program to address the safety of the product including:
safety pharmacology studies, chronic general toxicity studies in rats and dogs, reproductive toxicity
studies (including embryofetal studies in rats and rabbits that were conducted using racemic ketamine,
), genotoxicity studies, acute/short-term neurotoxicity studies, and carcinogenicity
studies (2-year study in rats and 6-month study in transgenic mice).
The non-clinical studies submitted by the sponsor were thoroughly and critically reviewed by Dr. Shiny
Mathew as the primary non-clinical reviewer. Dr. Mathew found the submitted data to be adequate to
support the approval of the application as indicated for adults with TRD, and I agree with her assessment.
However, Dr. Mathew expressed concerns about the long-term neurotoxicity evaluation in the studies
conducted by the sponsor. Her concern stems from the observation that the plasma levels at the highest
dose in animal studies were at or lower than the human plasma levels and did not provide multiple-fold
safety margins to the human exposures. In addition, a thorough evaluation of the brain was not conducted
in the long-term studies, including lack of additional endpoints for detecting neuronal apoptosis or
markers for other neurological diseases (e.g. Alzheimer’s). Dr. Mathew recommended in her review that
a post marketing requirement (PMR) for the assessment of higher exposures of esketamine in chronic
animal studies would be needed to evaluate the long-term neurotoxic effect of esketamine on the brain
(see her review in DARRTS dated 2/28/2019).
Supervisor’s comments on the issues raised by the reviewer:
Even though I understand Dr. Mathew’s concerns about the long-term neurotoxicity potential for
esketamine based on findings in the literature for racemic ketamine, I believe that the data submitted by
the sponsor for esketamine provide evidence about the safety of the doses and dosing paradigm proposed
for its use under this application. Therefore, I don’t agree that there is a need for a PMR to further
investigate the long-term neurotoxic effects of esketamine for this application.
In addition, I acknowledge Dr. Mathew’s reservations about the plasma levels obtained in animal studies
conducted with this program and I agree that they were not optimal; however, the data can still be useful
to establish safety for human use of esketamine as indicated in this application. The plasma levels in rats
were 1.8 (C
max
) and 0.6 (AUC) fold and in dogs 6.5 (C
max
) and 1.3 (AUC) fold the levels obtained in humans.
Reference ID: 4397715
(b) (4)
2
These studies were conducted at the maximum feasible dose due the insolubility of the drug in solution
and the limitation of the volume that can be administered intranasally in animals. It should be pointed
out that dosing was conducted on a daily basis in these animal studies while humans will be dosed
intermittently (twice a week for four weeks, once a week for another four weeks, and once every other
week for maintenance). As such, the plasma levels seen in animals at steady state based on chronic daily
exposures might be an exaggerated effect of what is predicted in human dosing where the drug does not
accumulate due to the short half-life (7-12h) and the intermittent dosing. It is worth noting that the drug
is to be administered under the supervision of a medical doctor, therefore patients’ misuse of the
administration of the drug as described in the label is not expected.
In addition, plasma levels in animals might not reflect brain levels. It was evident from a study conducted
by the sponsor (Study #FK12091) with orally administered esketamine that the brain levels were almost
twice those in the plasma in rats. While the sponsor did not conduct a similar study with the intranasal
(IN) route, IN administration is considered a route that could result in higher levels of administered drugs
in the brain compared to the plasma due to the direct nose-to-brain route via olfactory and respiratory
epithelium that might involve paracellular, transcellular, and neuronal transport (Erdo et al., 2018).
Therefore, the brain of animals treated with IN route might have been exposed to even higher drug levels
than those reported in plasma. The fact that no neurotoxicity was detected in rat brains using the more
expansive method of brain dissection (7 sections as per Bolon et al. 2013) used in the 6-month general
toxicity study might be reassuring even though only H&E staining was used. Bolon et al. (2013) indicated
that CNS and PNS tissues from general toxicity studies maybe surveyed effectively using the standard
H&E-stained sections. At the time when the 6-month rat study was conducted, the sponsor used the more
expansive sectioning of the brain proposed by Bolon et al. (2013), even though this has been only recently
recommended (Draft FDA Guidance for Industry: Developing Drugs for Treatment of Major Depressive
Disorder, 2018), therefore, the sponsor did due diligence to investigate the effect on the brain. While
additional staining and further investigations might be informative, these are typically needed as a
second-tier approach where there is a signal from general toxicity studies that there is an observed or
possible neurotoxic effect. At the doses used in this study, there does not seem to be any
neuropathological findings with esketamine to warrant this second-tier approach. As I discussed earlier,
even though the plasma levels in the chronic toxicity studies were not of multiple folds compared to the
human plasma, the animal dosing paradigm provides assurance that it is an exaggerated effect that
humans are not expected to experience based on the intermittent dosing in humans.
Dr. Mathew referred to published data in which ketamine has been reported to be associated with
apoptosis in the brain of adolescent mice and monkeys (Sun et al., 2012, Yeung et al., 2010, and Li et al.,
2017). However, it could be argued that such findings with ketamine might not be related to this product
for two reasons:
1) the indication for this product currently is for adults and not for adolescents or children and an
adult brain might be different from an adolescent brain that is still undergoing development, and
2) esketamine was negative when tested in adult brain for its neurotoxic effect by a single IN dose
administration (Olney lesion study) even at very high concentrations suggesting that esketamine
is different from ketamine as far as the short-term toxicity profile.
It is possible that the long-term neurotoxicity with ketamine might be stemming from its acute
neurotoxicity (Olney lesion) or it could be unrelated as a different mechanism of toxicity. The studies that
are described in the literature with ketamine did not address the relation between the acute and the long-
term neurotoxicity. The data that the sponsor provided for their drug from acute neurotoxicity in rats and
long-term studies in rats and dogs did not indicate neurotoxicity signals. I acknowledge that in the long-
term studies brain histopathology evaluation was based on H&E staining only; however, this is a procedure
Reference ID: 4397715
3
that is the standard for evaluations conducted in long-term general toxicity studies for any product. As
mentioned earlier and based on the paper by Bolon et al., H&E is still capable of detecting neurotoxic
effects if such findings are present in brain sections that are used in the general toxicity studies.
Some studies in the literature in which adult mice or rats were treated with ketamine exhibited learning
and memory and/or sensorimotor gating deficits resembling those in schizophrenia (Ding et al, 2016,
Sabbagh et al., 2012). Similar effects are reported in ketamine abusers and are probably expected to be
seen at higher levels of esketamine. Clinical trials conducted by the sponsor assessed cognitive functions
and these functions will be further assessed in an ongoing 3-year study as a PMR that the clinical team is
recommending. Therefore, addressing the neurobehavioral effects of higher doses of esketamine in
animals might not be needed at this time.
Finally, treatment-resistant depression is a serious and debilitating condition, and the risk-benefit ratio
for this condition might be different from other less serious and debilitating conditions. Therefore, under
the current circumstances and with the available data from the studies conducted with this program, it is
reasonable to conclude that esketamine is adequately safe to use as indicated for this submission and for
this population. If esketamine is to be used at higher doses or with more frequent administration, then
future studies might be needed to provide assurance that these higher doses or more frequent dosing will
not pose any safety concerns for humans. In addition, the use of esketamine in adolescents or children
will require thorough evaluation at relevant doses to be used in this population to make sure that the
findings reported in the literature with ketamine use are addressed and to provide ample evidence about
the long-term safety of the brain in this population.
References
Bolon B, Garman RH, Pardo ID, Jensen K, Sills RC, Roulois A, Radovsky A, Bradley A, Andrews-Jones L,
Butt M, and Gumprecht L. Toxicol Pathol. 41:1028-1048, 2013.
Ding R, Li Y, Du A, YuH He B, Shen R, Zhou J, Li L, Cui W, Zhang G, Lu Y and Wu X. Sci Rep. 6: 38771, 2016.
Erdo F, Bors LA, Farkas D, Bajza A, and Gizurarson S. Brain Res Bull 143: 155-170, 2018.
Li Q, Shi L, Lu G, Yu HL, Yeung FK, Wong NK, Sun L, Liu K, Yew D, Pan F, Wang DF and Sham PC. Front
Neurosci. 11:1-9, 2017.
Sabbagh JJ, Heaney CF, Bolton MM, Murtishaw AS, Kinney JW, Physiol. Behav. 107 (3): (2012) 355–363,
2012
Sun L, Li Q, Li Q, Zhang Y, Liu D, Jiang H, Pan F, and Yew D. Add Bio, 19:185-194, 2012
Yeung LY, Wai MS, Fan M, Mak YT Lam WP, Li Z, Lu G, and Yew DT. Toxicol Lett. 193:189-193, 2010.
Reference ID: 4397715
--------------------------------------------------------------------------------------------
This is a representation of an electronic record that was signed
electronically. Following this are manifestations of any and all
electronic signatures for this electronic record.
--------------------------------------------------------------------------------------------
/s/
------------------------------------------------------------
IKRAM M ELAYAN
03/01/2019 10:20:28 AM
Signature Page 1 of 1
Reference ID: 4397715
1
DEPARTMENT OF HEALTH AND HUMAN SERVICES
PUBLIC HEALTH SERVICE
FOOD AND DRUG ADMINISTRATION
CENTER FOR DRUG EVALUATION AND RESEARCH
PHARMACOLOGY/TOXICOLOGY NDA REVIEW AND EVALUATION
Application number: 211243
Supporting document/s: SDN1/SN0001
Applicant’s letter date: September 4, 2018
CDER stamp date: September 4, 2018
Product:
SPRAVATO (esketamine)
Indication: Treatment Resistant Depression
Applicant: Janssen Research & Development
Review Division: Division of Psychiatry Products
Reviewer: Shiny V. Mathew, PhD, DABT
Supervisor/Team Leader: Ikram Elayan, PhD
Division Director: Tiffany Farchione, MD (Acting Director)
Project Manager: Hiren Patel, PharmD
Template Version: September 1, 2010
Disclaimer
Except as specifically identified, all data and information discussed below and necessary for
approval of NDA 211243 are owned by Janssen or are data for which Janssen has obtained a
written right of reference. Any information or data necessary for approval of NDA 211243 that
Janssen does not own or have a written right to reference constitutes one of the following: (1)
published literature, or (2) a prior FDA finding of safety or effectiveness for a listed drug, as
reflected in the drug’s approved labeling. Any data or information described or referenced
below from reviews or publicly available summaries of a previously approved application is for
descriptive purposes only and is not relied upon for approval of NDA 211243.
Reference ID: 4395937
2
TABLE OF CONTENTS
1 EXECUTIVE SUMMARY ................................................................................................... 7
1.1 INTRODUCTION .................................................................................................................... 7
1.2 BRIEF DISCUSSION OF NONCLINICAL FINDINGS ........................................................................... 7
1.3 RECOMMENDATIONS .......................................................................................................... 10
2 DRUG INFORMATION ................................................................................................... 14
2.1 DRUG .............................................................................................................................. 14
2.2 RELEVANT INDS, NDAS, BLAS AND DMFS ............................................................................ 15
2.3 DRUG FORMULATION .......................................................................................................... 15
2.4 COMMENTS ON NOVEL EXCIPIENTS........................................................................................ 15
2.5 COMMENTS ON IMPURITIES/DEGRADANTS OF CONCERN ........................................................... 15
2.6 PROPOSED CLINICAL POPULATION AND DOSING REGIMEN ......................................................... 17
2.7 REGULATORY BACKGROUND ................................................................................................. 17
3 STUDIES SUBMITTED .................................................................................................... 17
3.1 STUDIES REVIEWED ............................................................................................................ 17
3.2 STUDIES NOT REVIEWED...................................................................................................... 17
3.3 PREVIOUS REVIEWS REFERENCED .......................................................................................... 18
4 PHARMACOLOGY ......................................................................................................... 18
4.1 PRIMARY PHARMACOLOGY................................................................................................... 18
4.2 SECONDARY PHARMACOLOGY ............................................................................................... 19
4.3 SAFETY PHARMACOLOGY ..................................................................................................... 20
5 PHARMACOKINETICS/ADME/TOXICOKINETICS ............................................................. 21
5.1 PK/ADM E ....................................................................................................................... 21
5.2 TOXICOKINETICS ................................................................................................................. 24
6 GENERAL TOXICOLOGY ................................................................................................. 28
6.1 SINGLE-DOSE TOXICITY ....................................................................................................... 28
6.2 REPEAT-DOSE TOXICITY ....................................................................................................... 29
6.2.1 RAT REPEAT-DOSE TOXICITY USING ESKETAMINE .................................................................. 29
6.2.2 DOG REPEAT-DOSE TOXICITY USING ESKETAMINE ................................................................. 38
6.3 GENERAL TOXICOLOGY STUDIES USING PMI-100 .................................................................... 42
7 GENETIC TOXICOLOGY .................................................................................................. 43
7.1 IN VITRO REVERSE MUTATION ASSAY IN BACTERIAL CELLS (AMES) .............................................. 43
7.2 IN VITRO ASSAYS IN MAMMALIAN CELLS ................................................................................ 44
7.3 IN VIVO CLASTOGENICITY ASSAY IN RODENT (MICRONUCLEUS ASSAY).......................................... 45
7.4 OTHER GENETIC TOXICITY STUDIES ........................................................................................ 45
8 CARCINOGENICITY ....................................................................................................... 46
Reference ID: 4395937
3
8.1
RAT CARCINOGENICITY ........................................................................................................ 46
8.2 TRANSGENIC MOUSE CARCINOGENICITY ................................................................................. 46
9 REPRODUCTIVE AND DEVELOPMENTAL TOXICOLOGY ................................................... 47
9.1 FERTILITY AND EARLY EMBRYONIC DEVELOPMENT .................................................................... 47
9.2 EMBRYONIC FETAL DEVELOPMENT ........................................................................................ 50
9.2.1 RAT EMBRYONIC FETAL DEVELOPMENT .............................................................................. 50
9.2.2 RABBIT EMBRYONIC FETAL DEVELOPMENT .......................................................................... 53
9.3 PRENATAL AND POSTNATAL DEVELOPMENT ............................................................................. 5 6
10 SPECIAL TOXICOLOGY STUDIES ................................................................................. 59
11 APPENDIX/ATTACHMENTS ....................................................................................... 63
Reference ID: 4395937
4
Table of Tables
Table 1: Potential impurities in drug substance and their calculated amounts. .......................... 16
Table 2: In vitro binding data for esketamine, arketamine, and selected esketamine metabolites
at the PCP binding site of NMDAR. ............................................................................................... 18
Table 3: Esketamine, arketamine, and metabolites in an in vitro receptor binding screen ........ 19
Table 4: PK of ketamine in mice, rats, and rabbits following single bolus IV administration ........ 21
Table 5: PK of esketamine in rats administered aqueous vs. clinical formulation ....................... 21
Table 6: TK of esketamine in rats from the 6-month toxicity study (week 26). ........................... 24
Table 7: TK of esketamine in dogs from the 9-month toxicity study (week 39)........................... 25
Table 8: TK of racemic ketamine from pregnant rats in the embryofetal toxicity study (GD17)
following IN PMI-100 administration............................................................................................ 25
Table 9: Bridging study conducted in pregnant rats on GD17 after IV dosing of 90 mg/kg of
racemic ketamine.......................................................................................................................... 25
Table 10: TK of racemic ketamine from pregnant rabbits in the embryofetal toxicity study (GD
18) following IN PMI-100 administration. .................................................................................... 25
Table 11: Bridging study conducted in pregnant rabbits on GD19 after IV dosing of 8 mg/kg of
racemic ketamine.......................................................................................................................... 26
Table 12: TK of esketamine in rats in the 2-year carcinogenicity assay after 6 months of dosing
....................................................................................................................................................... 26
Table 13: TK of esketamine after subcutaneous administration in transgenic mice (week 25/26)
....................................................................................................................................................... 26
Table 14: TK of racemic ketamine after subcutaneous administration of PMI-100 in rats on D1 of
neurotoxicity study ....................................................................................................................... 27
Table 15: TK of IN esketamine in female rats on D1 of neurotoxicity study ................................ 27
Table 16: TK of IN esketamine in female rats on D1 of neurotoxicity study ................................ 27
Table 17: Summary of histopathology findings in the nasal turbinates of rats from the 6-month
toxicity study. ................................................................................................................................ 34
Table 18 : Summary of histopathology findings in the respiratory epithelium of rats from the 6-
month toxicity study. .................................................................................................................... 34
Table 19: Mean activity count in rats from the 6-month toxicity study. ...................................... 35
Table 20: Mean trial times on various test days (D1-4) in the Morris water maze test in rats from
the 6-month toxicity study. .......................................................................................................... 35
dĂďůĞ Ϯϭ͗ DĞĂŶ й ŽĨ ƌĂƚƐ ƚŚĂƚ ĨĂŝůĞĚ ƚƌŝĂůƐ ;шϵϬ ƐĞĐͿ ŝŶ ƚŚĞ DŽƌƌŝƐ ǁĂƚĞƌ ŵĂnjĞ ĨƌŽŵ ƚŚĞ ϲ-month
toxicity study. ................................................................................................................................ 36
Table 22: Reproductive toxicity endpoints examined in male rats from the 6-month toxicity
stud y. ............................................................................................................................................. 36
Table 23: Reproductive toxicity endpoints examined in female rats from the 6-month toxicity
stud y. ............................................................................................................................................. 37
Table 24: Summary of histopathology findings in dogs from the 9-month toxicity study ........... 42
Table 25: Mating and fertility parameters in male rats in the fertility and early embryonic
development study ....................................................................................................................... 49
Table 26: Mating and fertility parameters in female rats in the fertility and early embryonic
development study ....................................................................................................................... 49
Reference ID: 4395937
5
Table 27: Cesarean section findings from rat embryo-fetal development study with PMI-100 .. 52
Table 28: Offspring necropsy findings from rat embryo-fetal development study ..................... 52
Table 29: Caesarian section findings from rabbit embryo-fetal development study with PMI-100
....................................................................................................................................................... 55
Table 30: Offspring necropsy findings from rabbit embryofetal development study with PMI-100
....................................................................................................................................................... 55
Table 31: Effects of esketamine administration on parameters examined in the pre- and post-
natal development study in rats. .................................................................................................. 59
Table 32: TK of noresketamine in rats from the 6-month toxicity study. .................................... 65
Table 33: TK of noresketamine in dogs from the 9-month toxicity study. .................................. 65
Table 34: TK of noresketamine in transgenic mice following 26-weeks of dosing. ..................... 65
Table 35: TK of noresketamine in rats in the 2-year carcinogenicity assay after 6 months of IN
dosing. ....................................................................................................................... .................... 65
Table 36: TK data from bridging studies after IV administration of racemic ketamine in non-
pregnant rats. ................................................................................................................................ 67
Table 37: TK data from bridging studies after IV administration of racemic ketamine in dogs. .. 67
Table 38: TK parameters from F1 offsprings in the pre- and postnatal development study on
PND 4 and PND12. ........................................................................................................................ 68
Reference ID: 4395937
NDA211243 Shiny V. Mathew, PhD, DABT
6
Table of Figures
Figure 1: Proposed in vitro metabolic pathways of esketamine in liver microsomes and S9
fractions of various species. .......................................................................................................... 63
Figure 2: Esketamine (above) and noresketamine (below) exposure in nonclinical species
relative to humans. ....................................................................................................................... 64
Figure 3: Nasal cavity, brain and larynx dissections in the rat from the 6-month toxicity study. 66
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
7
1 Executive Summary
1.1 Introduction
This application is a 505(b)(1) NDA submitted by Janssen Research & Development (JRD) for
SPRAVATO (esketamine). All toxicology studies reviewed under this NDA are currently
owned by the applicant, regardless of who sponsored the original studies. The proposed
indication is treatment-resistant depression (TRD). Esketamine is a proprietary formulation of
the S-enantiomer of ketamine, which is approved only for acute use as an anesthetic agent.
The maximum recommended human dose (MRHD) is 84 mg/day for an adult with a proposed
dosing regimen of twice weekly during the induction phase (week 1-4), followed by a once
weekly maintenance phase (weeks 5-6), and a once biweekly maintenance phase (week 9-
lifetime). Esketamine has not been approved outside the U.S.
1.2 Brief Discussion of Nonclinical Findings
Esketamine, like racemic ketamine, is a noncompetitive glutamate N-methyl-D-Aspartate
(NMDA) receptor antagonist. It has a higher potency at this receptor compared to the
racemate, R-enantiomer, or any of its metabolites. Noresketamine (M10), the major
metabolite, has a 6-fold lower affinity to the NMDA receptor compared to esketamine. In vitro
studies demonstrated that the parent and/or noresketamine have a weak affinity (<50%) for
the serotonin (5HT) transporter, opioid (mu and kappa), ɶ-amino butyric acid (GABA), and
nicotinic acetylcholine receptors (nAChRs). Therefore, the Sponsor is suggesting that the
antidepressant activity is unlikely to be mediated through these transporters/receptors.
The Intranasal (IN) route of administration was chosen for esketamine due to its low oral
bioavailability in both humans and nonclinical species. It is quickly absorbed from the nasal
cavity with a Tmax of 5-30 minutes in all adult nonclinical species. Due to its high lipophilicity,
esketamine distributes quickly to well-perfused tissues including the brain in mice and rats.
After oral esketamine administration, the distribution of polar metabolites (M10, M4, and M9)
into the brain was lower compared to the parent. Esketamine is rapidly and extensively
metabolized in rat and dog liver microsomes and there are species differences in its metabolic
profile. Based on human mass balance studies using radiolabeled esketamine administered
orally and intravenously, the major human metabolite (i.e. >10% total circulating) is
noresketamine, which was quantified in all nonclinical species. There are no unique human
metabolites. In rats and humans, the major excretion pathway is through urine.
General toxicology studies with esketamine of up to 6 months in rats and 9 months in dogs
were conducted to support chronic administration in humans. All pivotal toxicology studies,
except the single dose acute neurotoxicity study in rats and carcinogenicity study in transgenic
mice, were conducted at a maximum feasible dose (MFD) due to both the inability to achieve
higher concentrations of esketamine in the test formulation and the inability to administer
higher IN volumes in laboratory animals. Therefore, exposures in all toxicology studies, except
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
8
the two mentioned above, are generally at or lower than the clinical exposure. Furthermore, in
chronic toxicity, reproductive toxicity, and carcinogenicity studies, where there is a large
increase in body weight over the duration of dosing, the estimated dose (mg/kg/day) and
exposures were substantially decreased, potentially affecting the endpoints evaluated.
The 6-month chronic toxicity study in rats was conducted using juvenile animals with dosing
initiated at postnatal day (PND) 35 and with reproductive and neurobehavioral parameters
evaluated as part of the study design. It should be noted that a MFD was used in this study and
thus the development of tolerance to some of the clinical signs observed might be due to a
decrease in dose that occurs with an increase in body weight. Minimal to slight hyperplasia of
the olfactory epithelium and estrous cycle irregularities were observed in this study at an AUC
exposure 0.3 times that was achieved at the MRHD of 84 mg. Reproductive function was
assessed after a recovery period and showed no effect on time to mating or mating/fertility
indices. In this study, learning delays were observed at all doses suggesting that there is no No
Observed Adverse Effect Level (NOAEL) for this finding.
In addition to the routine parameters in a general toxicity study, the Sponsor conducted
subjective gross neurological examinations in the 9-month dog study. Dose dependent
increases in clinical signs such as salivation, increased activity, and incoordination were
observed lasting up to 1 hour post dose and persisting throughout the study at the highest
dose. Minimal to moderate olfactory epithelial atrophy and changes to the nasal cavity were
observed in this study after 9 months of daily dosing, at AUC exposures that were similar to
those at the MRHD of 84 mg/day. In shorter toxicity studies in dogs conducted using
esketamine in aqueous vehicle, and not the clinical vehicle, clinical signs such as head shaking,
vomiting, salivation, ataxia, and tremors were observed at exposures similar to or lower than
the MRHD.
Based on an overall weight of evidence, esketamine was determined to be negative for
genotoxicity. In a 2-year carcinogenicity study in rats (IN) and a 6-month transgenic study in
mice (subcutaneous), there was no evidence of carcinogenicity observed at exposures (AUC)
0.6-times in rat and 6-times in transgenic mice compared with MRHD. Additionally, a low
incidence of non-neoplastic lesions of the submucosa of the bladder was observed in males at
clinical exposures after daily dosing for two years in rats. With IN administered PMI-100
[100mg/mL (10% w/v) aqueous racemic ketamine solution containing 0.002% benzalkonium
chloride as an antimicrobial preservative], bladder toxicity findings had a safety margin of 1.5-
times the estimated esketamine AUC exposure at MRHD after 3-months in rats while there was
no safety margin for these findings in dogs after 1 month of administration.
In a fertility and early embryonic development (Segment I) study, estrous cycle irregularities
were observed at an esketamine dose of 45 mg/kg/day and a delay in mating ǁĂƐ ŽďƐĞƌǀĞĚ шϭϱ
mg/kg/day. Due to the lack of overall changes to mating and fertility indices, the NOAEL in this
study was considered 45 mg/kg/day which produce AUC exposure that was 0.6 times the AUC
exposure at MRHD.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
9
NMDA receptor antagonists are known to cause neuronal apoptosis in the young, developing
brain in animals. These findings are well-established in literature for mice, rats, and non-human
primates treated with acute anesthetic doses of racemic ketamine. Predicting that similar
findings would occur with esketamine and that appropriate drug label warning will be issued for
use during pregnancy and lactation, a dedicated neurotoxicity study after in utero drug
administration was not requested from the Sponsor for esketamine. The Sponsor submitted
embryofetal developmental (Segment II) studies conducted with PMI-100 in both rats and
rabbits (originally sponsored by Javelin Pharmaceuticals reaching
nominal doses through varied IN volumes for different treatment groups. In rats, there were
no adverse fetal findings up to 12-fold the MRHD for the estimated esketamine AUC exposure
in this study. In rabbits administered PMI-100, skeletal malformations were observed at
maternally toxic doses. The estimated esketamine AUC exposure at NOAEL for these findings is
0.3 times the AUC exposure at MRHD.
In a pre- and postnatal development (Segment III) study in rats, a sensorimotor delay (i.e.
Preyer response reflex) was observed at all doses of esketamine during the preweaning period
without an observed effect on fetal body weight. During the postweaning period, motor
activity was decreased but there was no effect on learning, habituation, sexual development, or
mating and fertility in F1 offsprings. These findings were observed at exposures comparable to
or lower than the MRHD.
Due to the known effect of NMDA receptor antagonists in causing neuronal vacuolation and
necrosis in the sexually mature adult brain, commonly referred to as Olney lesions, several
dedicated neurotoxicity studies were conducted in rats. Because of the time-sensitive nature of
these findings, only those GLP studies where a 4-6 hour and 3-day sacrifice time points were
utilized for the examination of neuronal vacuolation and necrosis, respectively, were
considered adequate. In general, neuronal vacuolation is considered reversible while neuronal
necrosis is irreversible. When a single dose of PMI-100 was administered subcutaneously to
rats, neuronal vacuoles but not necrosis was observed at the highest dose. Estimating 50% of
the exposure to be from esketamine, the NOAEL for neuronal vacuolation is 1.6-times and 4.5
times and the NOAEL for necrosis was 10-times and 16-times, respectively, for AUC and Cmax
exposures at MRHD. In a single dose neurotoxicity study conducted with IN esketamine,
exposures up to 17-fold and 23-fold the AUC and Cmax at the MRHD, respectively, did not
produce neuronal necrosis.
In conclusion, even though JRD has generated substantial amount of
nonclinical data with either IN racemic ketamine or IN esketamine, these studies have not been
ideal since exposures in the nonclinical species were either less than or equal to human
exposures. The AUC exposures at the highest dose in the chronic dog and rat studies were 1.3
times and 0.6 times, respectively, when compared with AUC exposure at MRHD. Through
multiple dosing, it was possible to increase exposures even if the drug was IN instilled as
evident by the high exposures in the pivotal single dose neurotoxicity study in rats. Therefore,
the major outstanding concern for esketamine in nonclinical studies is an understanding of
toxicities at higher exposures, particularly those related to the brain, after chronic-intermittent
Reference ID: 4395937
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
10
dosing. Specifically, the Sponsor’s current chronic toxicity studies only conducted routine
histopathology and were not designed to address other neurotoxicity concerns such as
neuronal apoptosis or protein changes that are reported after 6 months of daily administration
of IV racemic ketamine in adolescent nonclinical species (Yeung et al., 2010, Sun et al., 2012
and Li et al., 2017). The estimated esketamine exposure where the positive findings occur in
these studies is near the clinical exposure with IN esketamine. Having no safety margin for
these potentially unmonitorable and irreversible findings is highly concerning. Considering the
clinical need for this product for a life-threatening condition, the best way to characterize these
toxicities is through adequate animal toxicity studies conducted at a maximum tolerated dose
(MTD) in an appropriate adult species under a Post Marketing Requirement (PMR).
To reiterate, while carcinogenicity and embryofetal toxicity concerns can be adequately
communicated through the drug label, we currently do not have sufficient safety information
on the chronic-intermittent effect of esketamine on the brain to alleviate concerns from the
published literature on racemic ketamine. Clinical studies to examine cognitive deficits after a
lifetime exposure to the drug are not practical and may have multiple confounders. The
current chronic nonclinical toxicity studies conducted by the Sponsor were not designed to
understand if neuronal changes or cognitive deficits occur with chronic-intermittent
administration. The 6-month rat toxicity study examined seven brain sections as per Bolon et
al., 2013 but in the dog, sectioning did not include appropriate nuclei noted for nonrodents in
the same paper. Histopathology in both species used only routine H&E staining without the use
of specific markers to detect neuronal loss or changes in implicated proteins. Chronic toxicity
study in rats included neurobehavioral battery which showed nonstatistically significant delays
in learning but were underpowered and used juvenile rats. Chronic toxicity study in dogs
included gross neurological examinations which were uninformative to understand if cognitive
deficits occur. Therefore, this Reviewer believes that the Sponsor will need to commit to an
adequate chronic toxicity study conducted at MTD, but following clinical frequency in an
appropriate nonclinical species, chosen based on similar metabolite profile as in the human.
The highest dose in this proposed study should reach several multiples of the clinical exposure
and should be a dedicated neurotoxicity study to examine neuronal markers of apoptosis,
necrosis, and possibly Alzheimer’s disease. Additionally, this study conducted to satisfy PMR,
should include a head-to-head comparison with racemic ketamine and examine functional
endpoints such as locomotor activity, learning and memory, and auditory startle habituation.
1.3 Recommendations
1.3.1 Approvability
The nonclinical information submitted by the Sponsor is adequate to support approval of the
product as indicated for adults with TRD, which is a life-threatening condition. However, the
long-term effects on the brain will need to be explored with a designated nonclinical
neurotoxicity study under a PMR.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
11
1.3.2 Additional Nonclinical Recommendations
None
1.3.3 Labeling
Below are the recommendations for the drug label. The Warning and Precaution section and sections
5.10, 8.1, 8.2, 8.3 and 8.4 were written, in collaboration with the review team from the Division of
Pediatric and Maternal Health, to express the neuronal apoptosis concerns in nonclinical species with
racemic ketamine. Sections 12.1, 12.2, 13.1, and 13.2 were also edited/written by the Pharm/Tox team.
Labeling is under negotiation with the Sponsor therefore, the following may not be the final version of
the labeling.
Section 8: Use in specific populations
8.1 Pregnancy
Risk Summary
use in pregnant women to drug-associated risk
o
f major birth defects, miscarriage, or adverse maternal or fetal outcomes. Based on findings from
published animal reproduction studies with ketamine, SPRAVATO may cause fetal
harm (see Data).
advise pregnant women of the potential risk to a
There are risks to the mother associated with untreated depression in pregnancy (see Clinical
Considerations).
Published studies in pregnant primates demonstrate that the administration of drugs that block N-
methyl-D-aspartate (NMDA) receptors during the period of peak brain development increases neuronal
apoptosis in the developing brain of the offspring. There are no data on pregnancy exposures in
primates corresponding to periods prior to the third trimester in humans [See Use in Specific Populations
(8.2)].
In embryofetal reproduction studies in rabbits, skeletal malformations were noted at maternally toxic
doses when ketamine was IN administered with a No Observed Adverse Effect Level (NOAEL) at an
estimated esketamine exposures 0.3 times the exposures at the maximum recommended human dose
(MRHD) of 84 mg/day. In addition, IN administration of esketamine to pregnant rats during pregnancy
and lactation at exposures that were similar to those at the MRHD resulted in a delay in sensorimotor
development in pups during the preweaning period and a decrease in motor activity in the post-weaning
period. The estimated background risk of major birth defects and miscarriage for the indicated
population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse
outcomes. In the U.S. general population, the estimated background risk of major birth defects and
miscarriage in clinically recognized pregnancies is 2 to 4% and 15 to 20%, respectively.
Clinical Considerations
Disease-associated maternal and/or embryo/fetal risk
A prospective, longitudinal study followed 201 pregnant women with a history of major depressive
disorder who were euthymic and taking antidepressants at the beginning of pregnancy. The women who
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
12
discontinued antidepressants during pregnancy were more likely to experience a relapse of major
depression than women who continued antidepressants. Consider the risk of untreated depression
when discontinuing or changing treatment with antidepressant medication during pregnancy and
postpartum.
Data
Animal Data
When female monkeys were treated intravenously with ketamine at anesthetic
dose levels in the third trimester of pregnancy, neuronal cell death was observed in the brains of their
fetuses.
This period of brain
development translates into the third trimester of human pregnancy. The clinical significance of these
findings is not clear; however, studies in juvenile animals suggest neuroapoptosis correlates with long-
term cognitive deficits.
Racemic ketamine was administered IN to pregnant rats during the period of organogenesis at doses of
15, 50, and 150 mg/kg/day and in pregnant rabbits at doses of 10, 30, and 100/50 mg/kg/day. The No
Observed Adverse Effect level (NOAEL) for embryofetal toxicity in rats was the highest dose of 150
mg/kg/day.
the NOAEL associated with
esketamine plasma exposure (AUC) is 12-times the AUC exposure at the MRHD of 84 mg/day. In
rabbits, the high dose was lowered from 100 to 50 mg/kg due to excessive mortality
in maternal does. Skeletal malformations were observed at doses ш 30mg/kg/day, which were
maternally toxic. The NOAEL for skeletal malformations was associated with a plasma esketamine
exposure (AUC) that was 0.3 times the AUC exposure at MRHD of 84 mg/day.
Administration of esketamine HCl to pregnant rats during pregnancy and lactation at IN doses
equivalent to 4.5, 15, and 45 mg/kg/day (based on a 200 gram rat) produced AUC exposures 0.07, 0.5,
and 0.7 times the MRHD of 84 mg/day, respectively. Maternal toxicity was observed at doses ш 15
mg/kg/day. In addition, a dose response delay in the age of attainment of Preyer response reflex was
observed in pups at all doses during the preweaning period This sensory/motor
developmental measure was tested starting on postnatal day (PND) 9, and the effect normalized by PND
19 in treatment groups as compared with PND14 for the majority of the controls. There is no NOAEL for
this delay in sensory/motor response observed in pups during the preweaning period. During the
postweaning period, a decrease in motor activity was observed at doses ш 15 mg/kg which is 0.5-times
the human exposure at the MRHD of 84 mg/day. The NOAEL for maternal toxicity and decreased motor
activity during the postweaning period was 4.5 mg/kg/day which was associated with plasma exposure
(AUC) that was 0.07-times the AUC exposure at MRHD of 84 mg/day.
8.2 Lactation
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
13
Risk Summary
Esketamine is present in human milk. There are no data on the effects of esketamine on the breastfed
infant or on milk production. Published studies in juvenile animals report neurotoxicity (see Data).
Because of the potential for neurotoxicity, advise patients that breast-feeding is not recommended
during treatment with SPRAVATO
™
.
Data
Published juvenile animal studies demonstrate that the administration of drugs that block NMDA
receptors, such as ketamine, during the period of rapid brain growth or synaptogenesis, results in
widespread neuronal and oligodendrocyte cell loss in the developing brain and alterations in synaptic
morphology and neurogenesis. Based on comparisons across species, the window of vulnerability to
these changes is believed to correlate with exposures in the third trimester of gestation through the first
several months of life, but may extend out to approximately 3 years of age in humans.
8.3 Females and Males of Reproductive Potential
Contraception
Based on published animal reproduction studies, SPRAVATO
™
may cause embryofetal harm when
administered to a pregnant woman [see Warnings and Precautions (5.x) and Use in Specific Populations
(8.1)]. However, it is not clear how these animal findings relate to females of reproductive potential
treated with the recommended clinical dose. Consider pregnancy planning and prevention for females
of reproductive potential.
8.4 Pediatric Use
The safety and effectiveness of SPRAVATO
™
in pediatric patients have not been evaluated.
Section 12: Clinical Pharmacology
12.1 Mechanism of Action
Esketamine, the S-enantiomer of racemic ketamine, is a nonselective, noncompetitive antagonist of the
N-methyl-D-aspartate (NMDA) receptor. The mechanism by which esketamine exerts its antidepressant
effect is unknown. The major circulating metabolite of esketamine (noresketamine) demonstrated
activity at the same receptor with less affinity.
Section 13: Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis
Once-daily IN administration of esketamine at doses equivalent to 4.5, 15, and 45 mg/kg/day (based on
a 200 gram rat) did not increase the incidence of tumors in a 2-year rat carcinogenicity study. At the
highest dose, the AUC exposure to esketamine was lower than the human exposure (AUC) at the
maximum recommended human dose (MRHD) of 84 mg. Once-daily subcutaneous administration of
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
14
esketamine up to 75/40 mg/kg/day did not increase the incidence of tumors in a 6-month study in
transgenic (Tg.rasH2) mice.
Mutagenesis
Racemic ketamine was not mutagenic with or without metabolic activation in the Ames test, but was
positive in an in vitro mouse lymphoma test in the presence of metabolic activation. Intraperitoneally-
injected ketamine in an in vivo bone marrow micronucleus test in mice.
Genotoxicity with esketamine was seen in a screening in vitro micronucleus test in the presence of
metabolic activation. However, esketamine was in an in vivo Comet assay in rat liver cells.
Impairment of Fertility
Esketamine was administered IN to both male and female rats before mating, throughout the mating
period, and up to day 7 of gestation at doses equivalent to 4.5, 15, and 45 mg/kg/day (based on a 200
gram rat), which are approximately 0.05, 0.3, and 0.6-times the maximum recommended human dose
(MRHD) of 84 mg/day based on mean AUC exposures, respectively. estrous cyclicity at
the high dose of 45 mg/kg/day and increased time to mate at doses ш 15 mg/kg/day were observed
without an overall effect on mating or fertility indices. The No Observed Adverse Effect Level (NOAEL)
for mating and fertility is 45 mg/kg/day which is 0.6-times the esketamine exposures at MRHD of 84
mg/day.
13.2 Animal Toxicology and/or Pharmacology
Neurotoxicity
In a single-dose neuronal toxicity study where esketamine was administered IN to adult female rats,
there were no findings of neuronal vacuolation up to an estimated dose equivalent of 45 mg/kg for a
200 gram rat with an exposure difference of 1.8 and 4.5 times the clinical exposures for AUC and Cmax,
respectively, to the MRHD of 84 mg/day. In a second single dose neurotoxicity study conducted with
nasally administered esketamine to adult female rats, there were no findings of neuronal necrosis up to
a dose equivalent of 270 mg/kg for a 200 gram rat which has an exposure difference of 18-fold and 23-
fold, respectively, to AUC and Cmax exposures at the MRHD of 84 mg/day.
In a single-dose neuronal toxicity study in adult rats, subcutaneously administered racemic ketamine
caused neuronal vacuolation in layer I of the retrosplenial cortex without neuronal necrosis at a dose of
60 mg/kg. The NOAEL for vacuolation in this study was 15 mg/kg. Estimating 50% of the exposure to be
from esketamine, the NOAEL for neuronal necrosis is times and 16-times exposures and the NOAEL for
neuronal vacuolation is 1 times and times, respectively, for AUC and Cmax to the clinical exposure
at the MRHD of 84 mg/day. The relevance of these findings to humans is unknown.
2 Drug Information
2.1 Drug
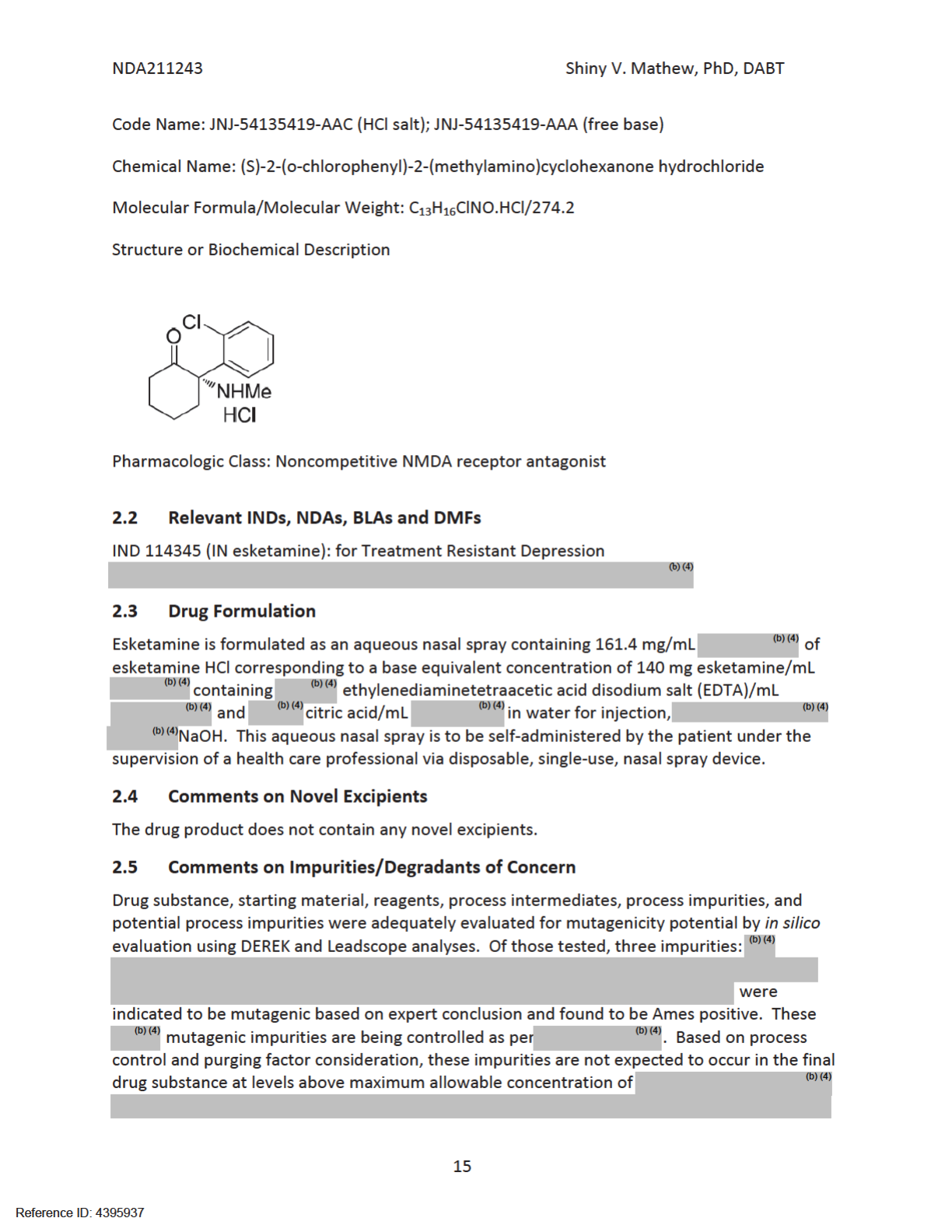
CAS Registry Number: 33643-47-9
Generic Name: esketamine
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b)
(4)
(b)
(4)
(b)
(4)

NDA211243 Shiny V. Mathew, PhD, DABT
16
Therefore, the Sponsor has not specified any limits for
these three mutagenic impurities and it is acceptable based on the CMC review.
The following table lists the specified organic impurities of esketamine HCl in the European
Pharmacopeia. None of the impurities (A, B, C, or D) have structural alerts or concerns for
mutagenicity based on FDA internal CMC assessment. Despite having no structural alerts, the
Sponsor evaluated impurity
Based on that legislation, the Sponsor tested
impurity in an acute oral toxicity test in rats, Ames assay, in vitro bovine corneal opacity
and permeability (BCOP) test, in vitro skin corrosion and skin irritation tests, and an in vivo local
lymph node assay in mice. All tests were negative except a positive signal in the BCOP test.
Table 1: Potential impurities in drug substance and their calculated amounts.
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
17
substance, the threshold for qualification is % or mg per day intake, whichever is lower.
The level of these impurities in the carcinogenicity studies, 6-month chronic toxicity studies,
and neurotoxicity studies (batches A12BD0277 and A12LD4238) are % and calculated to be
in a rat based on surface area calculation. The fourth impurity (impurity D in the
table
above), the R-enantiomer of the drug is present at higher levels (i.e. %) in the clinical
batch but it is also qualified in the rat (see table above). Therefore, all of the nongenotoxic
organic impurities are adequately covered in toxicology studies.
The CMC reviewer, Rohit Tiwari, PhD, alerted the Pharm/Tox Reviewer to the presence of an
not listed under ICHQ3C: for which risk assessment was
requested from the Sponsor. The Sponsor’s risk assessment notes that
induced chromosomal aberrations in some in vitro and in vivo animal studies but it is negative
in a rat and mouse carcinogenicity studies conducted by ATSDR, EPA, NTP and others.
Therefore, based on a weight of evidence, it is considered to be non-genotoxic. Based on the
principles outlined in the Sponsor calculated the permitted daily exposure (PDE)
for the mg/day or approximately mg/kg/day in a 60-kg subject. The
reporting threshold for which translates to ug/day for a 84
mg/day, if given daily. This ug/day is calculated as ug/kg/day in a 60-kg weighing patient,
which is -fold below the tentative PDE value of mg/kg/day. Therefore, the Sponsor’s
conclusion that the risk of adverse impact in patients is low is reasonable.
2.6 Proposed Clinical Population and Dosing Regimen
The proposed indication is TRD. The proposed starting dose is 56 mg/day in adults with a
proposed dosing regimen of twice weekly during the induction phase (week 1-4), followed by a
once weekly maintenance phase (weeks 5-6), and a once biweekly maintenance phase (week 9-
lifetime). Subsequent doses after Day 1 of dosing may be either 56 or 84 mg/day.
2.7 Regulatory Background
JRD is the original developer of IN esketamine.
3 Studies Submitted
3.1 Studies Reviewed
All submitted pivotal studies, in various species were reviewed in detail, except the
neurotoxicity studies in juvenile animals.
3.2 Studies Not Reviewed
Preliminary dose range finding studies and non-pivotal studies for deciding nonclinical safety of
esketamine and ketamine were not reviewed in detail. In addition, because the approval of
TRD will be based on clinical trials in adults, juvenile animal toxicity studies were not reviewed.
Reference ID: 4395937
(b)
(4)
(b) (4)
(b)
(4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b)
(4)
(b)
(4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)



NDA211243 Shiny V. Mathew, PhD, DABT
20
Published data report that ketamine, esketamine, and arketamine block the nicotine-induced current at
a low micromolar concentration range in transfected rat nicotinic acetylcholine receptors (nAChRs)
(Moaddel et al, 2013). In a study (DD17053) conducted by the Sponsor using cells transfected with
human nAChR ɲ7, (R,S) DHNK failed to inhibit these receptors whereas Moaddel, et al., 2013 reported
that the same metabolite blocked rat nAChR ɲ7 current with an IC
50
of 50 nM. The Sponsor
hypothesizes that the discrepancy between published data and in-house data may be attributed to
species-specific sensitivity. However, a head-to-head comparison of the human and rat nAChRs would
be needed to resolve this discrepancy. In study No. DD17063 examining functional activity of racemic
ketamine, esketamine, arketamine, and esketamine metabolites at human nAChR ɲ7, none of the
compounds exhibited significant antagonist activity, except for 2S-5,6 DHNK (M9) which reduced activity
by 36% when tested at 100uM.
Overall, the pharmacology studies conducted by JRD conclude that esketamine is a nonselective and a
noncompetitive antagonist of NMDARs. Of the various phase 1 metabolites generated in humans, only
noresketamine (M10), but not others (i.e. M4, M5, M9, and M19), is confirmed to have activity at
NMDARs.
Established Pharmacologic Class
The current list of established pharmacological class (EPC) has two listings for N-methyl-D-Aspartate
(NMDA) receptor antagonists: 1. Dextromethorphan; which is described as an “uncompetitive NMDAR
antagonist” and 2. Memantine; which is described as “NMDA receptor antagonist”. The KETALAR® label
refers to the racemate as nonbarbiturate general anesthetic with the statement “mechanism of action is
primarily due to antagonism of NMDA receptors in the central nervous system.” In the current
proposed label, the Sponsor is referring to the drug as “glutamate receptor modulator” in the highlights
and in the mechanism of action section 12.1 as “a non-competitive, subtype non-selective, activity-
dependent glutamate receptor modulator”. However, to keep simplicity of EPC class, it was determined
that the EPC of esketamine should be referred to as a “noncompetitive NMDA receptor antagonist.”
4.3 Safety Pharmacology
CNS safety pharmacology was evaluated as part of the 6-month toxicology study in rats using Functional
Observational Battery (FOB), Morris Water Maze, and locomotor activity (refer to the 6-month study
under section 6.2.1). Cardiovascular pharmacology was evaluated as part of the 9-month dog study
using electrocardiography (refer to the 9-month dog study under section 6.2.2). Additionally, the
following cardiovascular and respiratory studies were conducted under Safety Pharmacology.
Study/Study No. Finding
hERG Assay/ JRD,
TOX11340 (GLP)
IC
50
= 214 μM (58.7 μg/mL). IC
50
based safety margin is approximately 337-fold the
plasma concentration of esketamine at MRHD (174 ng/mL).
Cardiovascular and
Respiratory (Conscious
non-telemetered Beagle
Dog)/TOX11501 (GLP)
Single escalating doses of 0.3, 1 or 3 mg /kg of esketamine was IV administered to
male beagle dogs resulting in increases in heart rate, blood pressure (systolic,
diastolic, and mean), and heart related shortening of QT-interval in a dose-
dependent manner. The effects on heart rate, blood pressure, and QT-interval were
noted in all dose levels, whereas heart rate related shortening of the PQ-interval and
an increase in respiration rate was only observed at 3 mg eq/kg. No drug related
arrythmias were noted throughout the study.
Reference ID: 4395937


NDA211243 Shiny V. Mathew, PhD, DABT
22
Type of Study Major Findings
Distribution
Study No. FK12091
The Sponsor did not conduct radiolabeled tissue distribution or quantitative
whole body autoradiography studies in animal species using esketamine. After
oral dosing of esketamine in rats, brain:plasma concentration ratios were 3-4 for
M19, 1.8 for esketamine, 1.2 for M4, and 0.3-0.4 for both M10 and M9.
From literature, after 5 min IV dose of ketamine, the highest esketamine
concentration was observed in kidney, lung, fat, and heart at 3 h post infusion
(Edwards and Mather, 2001). Esketamine and ketamine are known to cross the
placental barrier and it is rapidly distributed to fetal tissues including the brain
(Chang et al., 1974 ) .
Metabolism
In vitro study:
Study No. FK10473
Esketamine was rapidly and extensively metabolized in rat and dog liver
microsomes and S9 fractions and in human liver microsomes. Much slower
and less extensive metabolism was observed in mouse microsomes. In rat
induced liver S9 fraction, high turnover was observed. A total of 12 metabolites
were observed in vitro, 7 of which are present in humans.
The major metabolic pathway in all species was N-demethylation at the
secondary amine (M10; noresketamine). Other pathways involved are
oxidation on the cyclohexanone moiety (M2, M4, and M5), oxidative
deamination (M11), and keto reduction (M12) of M10. Additionally, further
oxidation of the cyclohexanone moiety of esketamine (M6), was observed. In
mice and human microsomes, the major metabolite was M10 and in rat and
dog microsomes, the major metabolite was M2. In dog and rat microsomes,
additional oxidation of M10 to M1 was observed. (See Figure 1 in the
Appendix for in vitro metabolic pathways of esketamine).
In humans, noresketamine (N-demethylation) was the major circulating
metabolite in plasma (i.e. 12-14% of total circulating drug material). This was
followed by M19 (keto-reduction of M4), M4 (N-demethylation and
hydroxylation at the 6-position), M5 (2S, 6S-HNK), and M17 (O-glucuronidation
of M4), which were present at >25% of parent AUC. Noresketamine is
accepted to be generally qualified in nonclinical species as its exposure levels in
rat general toxicity, Segment I, Segment III, and carcinogenicity study are near
the MRHD (0.5 fold) in humans (see Figure 2 in the Appendix for Sponsor’s
safety margin estimation). Segment II studies were not conducted with
esketamine, but rather with PMI-100. Norketamine, of which 50% is
noresketamine, is formed when ketamine is administered; however, the
exposure of level of neither norketamine nor noresketamine was directly
quantified in those studies. Nevertheless, the label for this drug indicates that
the drug is not recommended for pregnant and lactating women.
The Sponsor did not conduct in vivo metabolism studies in nonclinical species
with unlabeled esketamine.
In vitro, CYP2B6 and CYP3A4 play major roles in esketamine metabolism
whereas CYP2A6 and CYP2B6 play a major role in noresketamine metabolism.
In vitro, esketamine was not a major CYP inhibitor; M10 weakly inhibits CYP3A4
(IC
50
=1.9 uM with testosterone as substrate).
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
23
Type of Study Major Findings
Excretion
Study No. FK10757
After a single IV dose of 5 mg/kg
3
H-esketamine to male rats, 30-41%
radioactivity was excreted in the urine. No biliary excretion study for
esketamine was performed in animals.
There is literature evidence that esketamine is excreted in human breast milk
therefore animal studies were not conducted.
Other PK studies
Study No.: FK10602 , FK10995,
FK12057, FK12092, FK 12099,
FK12111, FK12229
The Sponsor conducted additional studies to characterize other metabolites
which represented >25% of esketamine AUC, such as M4, M5, M9, M10, and
M19. Of these, M19 and M4 are present at 3-4 fold higher levels in humans
when esketamine was administered IN than PO or IV. In nonclinical species
(rats and dogs) M4, but not M19, had adequate coverage after IN
administration. Similarly, M19 was not adequately covered in the Sponsor’s
transgenic mice carcinogenicity study. However, it was shown that M19 forms
under experimental conditions in the presence of S9 in an Ames assay and
mouse lymphoma assay when incubated with both ketamine and esketamine.
Therefore, it can be concluded that M19 has been qualified in routine
genotoxic studies.
Published data suggest that tertiary amines can react with nitrous acid to form
N-nitrosocompounds which are potentially genotoxic (Brambilla and Martelli,
2007; Mensinga, et al., 2003). However, there was no measurable
concentration of N-nitrosoesketamine formed in simulated gastric fluid under
fasted or fed conditions.
Reference ID: 4395937





NDA211243 Shiny V. Mathew, PhD, DABT
28
6 General Toxicology
6.1 Single-Dose Toxicity
Rat
Three non-GLP studies were conducted to determine esketamine exposure when ketamine was
administered. In study No. TOX 10457, all rats (3/sex) died within 15 minutes during an IV
infusion of 30 minutes with 150 mg/kg/day racemic ketamine (aqueous solution, pH 4.5, NaCl
until isotonic) after exhibiting signs such as severe sedation and decreased activity. At 120
mg/kg/day, 2/3 males died shortly at the end of infusion but the females survived. A dose of 30
mg/kg by a 30 min IV infusion was well-tolerated with abnormal respiration and ataxia lasting
up to 2 hours postdose. See the Table 36 in the Appendix for exposure data in rats from these
bridging studies.
A single dose oral study at doses ч 160 mg/kg/day followed by a 14-day repeated dose toxicity
study at doses ч 160 mg/kg/day (non-GLP; Study No. TOX 12233) were conducted with
esketamine HCl in S-D rats (8-9 weeks of age). In the single dose phase, the dose was lowered
to ч120mg/kg/day and in the repeated dose, the dose was lowered to ч 40mg/kg/day in
females due to severity of the clinical signs. Ataxia was observed immediately after dosing
followed by decreased generĂů ĂĐƚŝǀŝƚLJ шϴϬŵŐͬŬŐͬĚĂLJ ĂŶĚ шϰϬ ŵŐͬŬŐͬĚĂLJ ŝŶ ĨĞŵĂůĞƐ͘ ĂƚĂůĞƉƐLJ
ǁĂƐ ŽďƐĞƌǀĞĚ шϭϲϬ ŵŐͬŬŐͬĚĂLJ ŝŶ ŵĂůĞƐ ĂŶĚ шϰϬ ŵŐͬŬŐͬĚĂLJ ŝŶ ĨĞŵĂůĞƐ͘ ĨƚĞƌ ƚŚĞƐĞ E^ ƐŝŐŶƐ
resolved, the animals showed excitation. With repeated dosing, severity and duration of CNS
signs decreased. There was a minimal increase in calcium and inorganic phosphate in males at
160 mg/kg/day. Minimal centrilobular hypertrophy was observed at 160 mg/kg/day correlating
with increased liver weights. Dose-related accumulation of hyaline droplets in the
corticotubular epithelium in the kidney was observed in males ш ϰϬ ŵŐͬŬŐͬĚĂLJ͘ dŚĞ EK> ŝŶ
the 14-day study was 40 mg/kg/day for males (Cmax 314 ng/mL and AUC
0-24h
was 425
ng.hr/mL) and 10 mg/kg/day for females (Cmax 203 ng/mL and AUC
0-24h
was 262 ng.hr/mL).
Dog
A non-GLP study (TOX 13114) was conducted in the beagle dog to explore various formulations
of esketamine (IV, IN, oral, sublingual). Clinical signs such as decubitus, moderate to severe
decreased activity, tremors, excitation and/or hemorrhagic vomit were observed ш 28mg/dog,
depending on the route of administration. Best bioavailability was observed via the oral dose
using an oral thin film. A bridging study (TOX10458) was conducted in the dog to determine
esketamine exposures after a single IV ketamine (aqueous solution, pH 4.5, NaCl until isotonic)
administration to correlate findings from shorter studies conducted with PMI-100 (see Table 37
in the Appendix showing the PK bridging data in dogs). In this study, ataxia, decubitus,
decreased general activity, salivation, and licking were observed after a single IV dose ш0.3
mg/kg, lasting up to 2 hrs.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
29
6.2 Repeat-Dose Toxicity
6.2.1 Rat Repeat-Dose Toxicity using Esketamine
Summary of studies shorter than 6 months in duration in rat:
A 3-month repeat dose IN toxicity study in SPF SD rats followed by a 1-month recovery period
(6-7 weeks 10/sex/group for main study; 5/sex/group for recovery) was conducted (GLP; TOX
10517). Doses of esketamine HCl (batch no. A12BD0277) were IN instilled (0.5 ml/rat) at doses
of 0.9, 3, or 9 mg equivalent/rat once daily or 9 mg eq/rat once a day for three days per week
for 3 months. This study had two controls: one to complement daily dosing and the second to
complement intermittent dosing. The vehicle in this study was not the clinical vehicle but rather
demineralized water adjusted to pH 4.5 ± 0.1 with NaOH or HCl. Slight salivation and increased
ŐĞŶĞƌĂů ĂĐƚŝǀŝƚLJ ǁĞƌĞ ŽďƐĞƌǀĞĚ ϯϬ ŵŝŶƵƚĞƐ ƉŽƐƚ ĚŽƐŝŶŐ ƚŚƌŽƵŐŚŽƵƚ ƚŚĞ ĚƵƌĂƚŝŽŶ ŽĨ ƚŚĞ ƐƚƵĚLJ ш ϯ
mg eq/rat. After daily dosing, ataxia ǁĂƐ ƐĞĞŶ ш ϯ ŵŐ ĞƋͬƌĂƚ ƵŶƚŝů ĚĂLJ ϰ ĂŶĚ ŽĐĐĂƐŝŽŶĂůůLJ
afterwards. With intermittent dosing, similar CNS signs were observed except that ataxia was
seen until 4
th
treatment (D7). There were no clinical observations on treatment free days and
severity and frequency decreased over time. Histopathology showed a minimal decrease in
mucus content of goblet cells in the respiratory epithelium, noted particularly in the epithelium
lining the nasal septum at level 1 at 9 mg eq/rat. Morphologically, this change appeared as
hypercellularity in this localized area due to the disappearance of large quantities of cytoplasm
(mucus vacuoles). In the daily dose group, the frequency was increased as compared with
intermittent dosing (i.e. all or nearly all rats affected in the daily dosing group compared with
2M and 4F affected in the intermittent group). There were no histopathology findings in the
recovery group. The NOAEL in this study is the mid dose of 3mg/eq (Cmax is 172 ng/mL and
AUC
0-24h
is 176 ng.hr/mL).
Study title: Esketamine hydrochloride (JNJ-54135419-AAC): Toxicity study by IN
administration to Crl:CD (SD) rats for 26 weeks with a reproductive phase
Study no.: TOX 10768
Study report location:
Conducting laboratory and location:
Date of study initiation: December 4, 2013
GLP compliance: Yes
QA statement: Yes
Drug, lot #, and % purity: JNJ-54135419-AAC, 2 batches used:
A12BD0277 (from weeks 1-10; purity 99.7%);
A12LD4238 (from weeks 11 to termination,
purity: 100.3%)
Reference ID: 4395937
(b) (4)
(b) (4)
NDA211243 Shiny V. Mathew, PhD, DABT
30
Key Study Findings
x This rat toxicity study was conducted as a combination of chronic and juvenile toxicity studies
with dosing initiated on postnatal day (PND) 35 and included evaluation of neurobehavioral and
reproductive toxicity endpoints. In general, CNS clinical signs reflected the anesthetic properties
of the drug with apparent tolerance developing over time. Unexpected to the predicted
anesthetic properties, there ǁĂƐ Ă ĚŽƐĞ ƌĞƐƉŽŶƐĞ ŝŶĐƌĞĂƐĞ ŝŶ ĂĐƚŝǀŝƚLJ Ăƚ шϭϱŵŐͬŬŐͬĚĂLJ ŝŶ ƚŚĞ
open field test which often reached statistical significance. The NOAEL for this finding was 4.5
mg/kg/day.
x A drug effect was observed on spatial learning in Morris Water maze. An increase in latency to
reach platform and higher failure rate were observed at week 13/14 of dosing (but not at week
5/6) with statistical significance observed on D2 of that week in males at 45 mg/kg/day. A
similar trend was seen without reaching statistical significance at other time points. After
repeated drug administration of nearly 6 months, the learning delay was observed at all doses.
x A drug effect on estrous cycle was not observed at weeks 6-7 of dosing but rather after 1 week
ŽĨ ƌĞĐŽǀĞƌLJ Ăƚ шϰϱ ŵŐͬŬŐͬĚĂy. At that time point, 25% of HDF compared to 15% of controls had
irregular estrous cycles. Reproductive capacity was assessed only after 3 weeks of recovery but
not in the presence of drug. No mating delay or effect on mating/fertility indices was observed
in this study in the absence of drug.
x Minimal to slight hyperplasia of the olfactory epithelium was observed in both males and
ĨĞŵĂůĞƐ шϰϱ ŵŐͬŬŐͬĚĂLJ͘
x The appearance of tolerance to clinical signs and the lack of consistent findings for other
endpoints in this study may be due to the lack of body weight correction for dosing over the
course of the study (see the dose section below).
x NOAEL in this study is the mid dose of 15 mg/kg/day for nasal findings and estrous cycle delays
but there is no NOAEL for the learning deficits observed in this study. The rat NOAEL is 0.3
*
-
times for AUC and 0.8-times for Cmax as compared to the esketamine exposures at the MRHD
of 84 mg/day (530 ng.h/mL for AUC and 174 ng/mL for Cmax for esketamine).
*
Esketamine exposures used here to calculate safety margins were from the carcinogenicity study in rats
because of contamination of PK samples in this study.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
31
Methods
Doses: 0, 0.9, 3, 9 mg eq/rat/day (estimated to be 4.5, 15,
and 45 mg/kg/day for a 200 gram rat; To note: at the
end of 26 weeks, male rats weighed as much as 600
gram which means that the highest dose received
was 15 mg/kg/day)
Frequency of dosing: Once daily for 26 weeks.
Route of administration: IN instillation
Dose volume: All treatment groups received the same volume
(50uL/day; 25ul/nare) with varying drug
concentration in vehicle.
Formulation/Vehicle: Pyrogenic free water/water for injection with
citric acid and EDTA, pH4.5
Species/Strain: Rat/Crl:CD (SD)
Number/Sex/Group: 20/sex/dose for main study group
Age: PND 35 at the start of dosing
Weight: 108-199g (M); 93-157g (F)
Satellite groups: TK group: 6/sex/dose for all doses except vehicle
control which had 3/sex/dose; reproductive phase
group: 20/sex/dose
Unique study design: The Sponsor integrated endpoints similar to a
juvenile toxicity study into this chronic toxicity study
using PND 35 rats at the start of dosing. After 13
weeks of dosing, the reproductive phase group rats
were given a 6-week dose free period during which
mating and fertility parameters were assessed.
Neurobehavioral endpoints were assessed on week 5
(first 10 main study rats), week 13 (reproductive
phase animals), and week 21 (last 10 main study
rats). Dosed females were checked for estrous cycle
phases using vaginal smears for 15 days during
treatment (weeks 6 and 7 of treatment) and for 15
days prior to pairing (starting after at least one week
of recovery). Animals were paired at approximately
20 weeks of age for up to 2 weeks. Following
pairing, mating was confirmed using pipette lavage.
Reproductive phase females were killed on D14 after
mating, or on D10 after last day of pairing for the
females which failed to mate. Reproductive phase
males were killed after the majority of the
reproductive phase females, which was after six
weeks of recovery. In the reproductive phase
females, each ovary/uterine horn, number of
corpora lutea, implantation sites, resorption sites
Reference ID: 4395937
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
32
and embryos were assessed. (See appendix Figure 3
for brain and nasal histopathology sectioning)
Deviation from study protocol: None affecting the interpretation of study results
Observations and Results: Changes from Control
Parameters Major findings
Mortality No test article related mortality. Three deaths/early termination in main/reproductive phase
groups [1CM (repro), 1CM (main), 1MDF (main)]. Two TK deaths due to failure to revive from
anesthesia.
Clinical Signs Dose-dependent increase in the incidence of unsteady gait (all animals affected at the
highest dose), overactive and underactive behavior in all dosed males and females. The
clinical signs started within 5-10 minutes of drug administration and lasted for 20-30 minutes
post dose. These findings decreased in frequency and magnitude with repeat dosing with no
signs observed after week 16 of dosing in main study animals.
Body Weights unremarkable
Ophthalmoscopy unremarkable
Hematology unremarkable
Clinical Chemistry unremarkable
Urinalysis unremarkable
Gross Pathology unremarkable
Organ Weights A decrease in absolute and relative ovarian weight was observed in females at the end of 26
weeks. This finding was slight (i.e. <20%) but statistically significant at all doses. The relative
weights were 0.093g, 0.078g, 0.076g, and 0.083g for all C, LD, MD, and HD respectively. This
decrease in ovarian weight occurred in the absence of correlating histopathology findings.
Histopathology
Adequate battery:
Yes; Brain
sectioning
conducted as per
Bolon et al., 2013
Nasal turbinates
Minimal to slight hyperplasia of the olfactory epithelium was observed in 12/20 HDM and
10/20 HDF, and in a single MDF (see Table 17 below).
Respiratory epithelium
There was an increase in globlet cells in the respiratory epithelium of the septum in all
animals, including vehicle controls. While a dose-dependent relationship is not clear in
males, mid and high dose females have twice as many incidences of this finding compared
with controls (see Table 18 below for the Sponsor’s summary). This may be the result of IN
route of administration but a test article relationship cannot be excluded due to increased
frequency in females.
Special Evaluation:
Locomotor activity
FOB was conducted at the time of anticipated peak plasma concentration (5-15 minutes after
dosing). In FOB, total mean activity count in an open field showed a dose related increase
(18-90%) which reached statistical significance at the mid and high doses on weeks 5 and 21
(see Table 19).
There were no dose related effects for total locomotor activity (home cage) which was
performed 1 hr prior to dose administration (i.e. 20-22 hrs post dose). Considering the drug’s
short half-life, it may have been completely excreted at the time when this endpoint was
measured.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
33
Special
Evaluation:
Continued
Functional
Observational
battery
Other FOB findings were consistent with that for an anesthetic. These included the following:
dose related incidences of salivation and cold paws in all dosed animals; a dose dependent
increase in the incidence of abnormal gait
(unsteady/uncoordinated/elevated/flattened/unstable) during the 2-minute observation
assessment in weeks 5, 13, and 21. Slow or poorly coordinated righting reflex, increased
distance in landing footsplay and reduced forelimb/hindlimb grip strength (~30%) was
observed at all three time points at the HD compared with controls. For most of the
anesthetic related findings, there was a reduction in magnitude and/or incidence over time.
Special
Evaluation:
Continued;
Morris Water
maze
There was a drug effect on spacial learning (i.e. mean trial times) observed starting on week
13/14 (see Table 20). Due to the high variability in data and small sample size (only
10/sex/group), statistics cannot be fully relied on in this study (i.e. 11.3 sec, 12.9 sec, 17.2 sec
and 27.3 sec in CM, LDM, MDM and HDM, respectively) but there seems to be a trend effect.
On week 13/14, day 2, there was a clear dose response delay in reaching the platform in all
drug treated males, which was statistically significant at the HD. HDM had a delay of 2.4 fold
compared with controls at this time point (p<0.01). On the later test dates in week 21/22,
this initial delay is still observed but at a smaller magnitude and not reaching statistical
significance.
Additionally, a drug effect was observed on the % of animals that failed the test on D1 (i.e.
ƚŚŽƐĞ ĂŶŝŵĂůƐ ƚŚĂƚ ŚĂĚ ш ϵϬ ƐĞĐ ƚŽ ƌĞĂĐŚ ƚŚĞ ƉůĂƚĨŽƌŵͿ (seeTable 21). For this parameter, a
dose response is clear in both sexes by week 21/22 reaching a 20-30% increase in failure rate
at the HD compared with controls. Based on the fewer number of rats failing by D4, it is clear
that they are able to learn after repeated trials (i.e. no apparent effect of drug on memory
retention in this study).
Special
Evaluation:
Continued;
Reproductive
Toxicity
During the treatment period, there were statistically significant variations in body weight in
reproductive phase males. However, overall, the body weight gain in dosed animals was
similar to controls. In recovery, MDM and HDM had a 17% and 25% increase in body weight
gain that reached statistical significance at high dose. See Table 22 for reproductive toxicity
endpoints tabulated from Sponsor’s data.
During the gestational period, body weights were not different over days 0-6, but between
days 6-14, all dosed females had a 16% decrease in body weight gain, which reached
statistical significance at MD and HD. During the 13-weeks of drug dosing, there were no
significant differences in absolute body weights or body weight gains between treated rats
and controls (see Table 23).
Vaginal smears were done for two weeks on weeks 6-7 and on week 14 (1 week after
recovery) (see methods for details). Whereas there was no drug effect on estrous cycling in
weeks 6-7, an effect on estrous cycles was observed at the second time point (i.e. recovery).
At this time point, slightly less number of HDF (75%) had normal 4 day cycles as compared
with 85% in Controls. Unlike the observed mating delays in the Segment I study, this study
did not show a delay in mating because mating was conducted after 3 weeks of recovery and
not in the presence of drug. Overall, similar to Segment I study, there was no effect on
mating and fertility indices. It is likely that effect on estrous cycle in this study may be age-
related.
The post implantation loss was 62% and 38% higher in LDF and HDF compared with controls
but not following a clear dose response. There were no other salient findings in other litter
data parameters (Table 23). HCD was not provided for reproductive and neurobehavioral
parameters from 6-month chronic toxicity studies.
LD: low dose; MD: mid dose; HD: high dose; HCD: historical control data.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
34
Reviewer’s Comments: The dosing scheme (mg/rat) in this study is skewing the data, particularly those related to
learning and behavior. Since there is no body weight correction for dosing, the animals are receiving more dose of
the drug earlier in the study than towards the end of six months when they gain weight (i.e. 45 mg/kg/day when
200 gram vs. 15 mg/kg/day when 600 gram).
Table 17: Summary of histopathology findings in the nasal turbinates of rats from the 6-
month toxicity study.
The table below is excerpted from TOX 10678, P.67. Esketamine doses were 0, 0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45
mg/kg/day for a 200 gram rat).
Table 18 : Summary of histopathology findings in the respiratory epithelium of rats from the
6-month toxicity study.
The table below is excerpted from TOX 10678, P.67. Esketamine doses were 0, 0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45
mg/kg/day for a 200 gram rat).
Reference ID: 4395937
NDA211243 Shiny V. Mathew, PhD, DABT
35
Table 19: Mean activity count in rats from the 6-month toxicity study.
The table below is created from data from TOX 10678. Esketamine doses were 0, 0.9, 3 and 9 mg/rat (0, 4.5, 9 and
45 mg/kg/day for a 200 gram rat); N=10/sex/dose.
Mean Activity count in open arena
Males Females
Doses;
estimated
Week 5 Week 13 Week 21 Week 5 Week 13 Week 21
0 21.5 22 17.3 27.7 26.5 24.2
4.5 mg/kg/day 24.1 20.9 20.4 28.7 28.1 27.2
15 mg/kg/day 28.9** 20.7 24.2* 36.7* 32 26.6
45 mg/kg/day 37.9** 28.0 40.4** 51.6** 31.6 43.9**
Table 20: Mean trial times on various test days (D1-4) in the Morris water maze test in rats
from the 6-month toxicity study.
Tables are created from data taken from the Sponsor’s submission (Study No. TOX10768, P. 167-172). Esketamine
doses were 0, 0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45 mg/kg/day for a 200 gram rat); N=10/sex/dose.
Mean Trial times (Seconds) on Week 5/6
Doses; estimated Males Females
D1 D2 D3 D4 D1 D2 D3 D4
0 52.1 21.8 11 12.6 40 17.3 15.6 12.4
4.5 mg/kg/day 44.1 22 19 15.8 56.9 19.8 17.7 12
15 mg/kg/day 42.3 22.5 13.7 8.3 48.9 14.6 15.1 9.2
45 mg/kg/day 41.4 28.1 15 16.5 38.9 16.8 9.4 9.1
Mean Trial times (Seconds) on Week 13/14
Doses; estimated Males Females
D1 D2 D3 D4 D1 D2 D3 D4
0 42.6 11.3 8.2 6.9 48 18.9 11.5 11.4
4.5 mg/kg/day 40 12.9 8.2 9.4 60.3 22 13.3 11.6
15 mg/kg/day 45.5 17.2 13.0 10.8 49.2 22.7 15.3 8.6
45 mg/kg/day 56.5 27.3** 14.6 7.4 56.9 17 11.5 9.5
Mean Trial times (Seconds) on Week 21/22
Doses; estimated Males Females
D1 D2 D3 D4 D1 D2 D3 D4
0 53.8 13.3 10 8.5 47.6 31.3 14.2 9
4.5 mg/kg/day 54.5 24.7 6.6 10.2 49.3 30.4 15 13.6
15 mg/kg/day 51.3 24 10.2 7.7 57.9 30 15.9 11.4
45 mg/kg/day 62 21.6 9.5 5.9 55.7 22 19.6 10.6
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
36
Table 21: Mean % of ƌĂƚƐ ƚŚĂƚ ĨĂŝůĞĚ ƚƌŝĂůƐ ;шϵϬ ƐĞĐͿ ŝŶ ƚŚĞ DŽrris water maze from the 6-
month toxicity study.
Tables are created from data taken from the Sponsor’s submission (Study No. TOX10768, P. 167-172). Esketamine
doses were 0, 0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45 mg/kg/day for a 200 gram rat); N=10/sex/dose.
Day 1 of testing on respective weeks
Doses; estimated % of Males with at least 1 failed trial (90
sec)
% of Females with at least 1 failed
trial (90 sec)
Week 5/6 Week 13/14 Week 21/22 Week 5/6 Week
13/14
Week
21/22
0 50 70 55.6 50 50 50
4.5 mg/kg/day 70 60 70 60 70 60
15 mg/kg/day 40 60 60 50 50 70
45 mg/kg/day 70 70 80 40 80 70
Day 4 of testing on respective weeks
Doses; estimated % of Males with at least 1 failed trial (90
sec)
% of Females with at least 1 failed
trial (90sec)
Week 5/6 Week 13/14 Week 21/22 Week 5/6 Week
13/14
Week
21/22
0 0 0 0 0 0 0
4.5 mg/kg/day 0 0 0 0 0 0
15 mg/kg/day 0 10 0 0 0 0
45 mg/kg/day 20 0 0 0 10 0
Table 22: Reproductive toxicity endpoints examined in male rats from the 6-month toxicity
study.
Table is created from data taken from the Sponsor’s submission (Study No. TOX10768). Esketamine doses were 0,
0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45 mg/kg/day for a 200 gram rat); N=20/dose.
Parameter Estimated Dose, mg/kg/day
0 4.5 9 45
Body weight gain Week 0-13 (g) 347 375 364 363
Body weight gain Recovery 0-6
(g)
52 55 61 65*
No. males paired 19 20 20 20
No. males mated 18 20 20 20
Fertility index (%) 89 95 100 90
Relative testes weight (g) 3.86 3.888 3.963 3.788
Relative Epididymis weight (g) 1.503 1.503 1.521 1.457
Epididymal sperm concentration Not examined
% motile sperm Not examined
% abnormal sperm Not examined
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
37
Table 23: Reproductive toxicity endpoints examined in female rats from the 6-month toxicity
study.
Table is created from data taken from the Sponsor’s submission (Study No. TOX10768). Esketamine doses were 0,
0.9, 3 and 9 mg/rat (0, 4.5, 9 and 45 mg/kg/day for a 200 gram rat); N=20/dose.
Parameter Estimated Dose, mg/kg/day
0 4.5 15 45
Absolute Body weight 300 298 296 304
Week 0-13 (dosing period) 173 174 171 181
Recovery period 0-3 weeks (g) -1 -5 -3 -4
Absolute body weight on GD 14 355 350 349 357
Body weight gain GD 0-6 (g) 19 23 22 23
Body weight gain GD 6-14 (g) 37 31 31* 31*
% Regular estrous cycle of 4 days (wks 6-7) 95 100 100 95
% regular estrous cycle during recovery 85 90 100 75
Mating index for F (%) 95 100 100 100
Fertility index for F (%) 90 95 100 90
Corpora lutea (mean no. per animal) 16.6 15.7 15.8 16.7
Implantations (mean no. per animal) 15.8 14.2 14.8 15.9
Early Resorptions (mean no. per animal) 1.3 1.8 1.4 1.8
Live embryo 14.6 12.4 13.4 14.1
Preimplantation loss (%) 5.4 10.5 6.9 5.4
Postimplantation loss (%) 8.6 14.0 8.7 11.9
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
38
6.2.2 Dog Repeat-Dose Toxicity using Esketamine
Summary of studies shorter than 9 months in duration in dog:
A 3-month repeated dose IN toxicity study of JNJ-54135419-AAC in the beagle dog with a 1-
month recovery period/Study No. 10524 (GLP). Male and female beagle dogs (4/sex/group)
were administered esketamine HCl (Batch no. A12BD0277) doses of 0, 24, 48 or 72 mg
equivalent/dog/day twice daily (7 days a week) for 3 months or at 72 mg equivalent/dog/day
for 3 days each week for three months. The volume administered in this study was 0.4
mL/dog/day and given twice daily with 15 minutes in between dosing. This study had two
controls: one to complement daily dosing and a second to complement intermittent dosing.
The vehicle in this study was not the clinical vehicle but rather demineralized water adjusted to
pH 4.5 ± 0.1 with NaOH or HCl. A 1-month recovery period was conducted in this study where
2/sex/group served as recovery animals for the two control and two high dose groups. Clinical
signs were as expected for an anesthetic and included head shaking, transient vomiting,
salivation, ataxia (up to 1 hr post dosing), slight tremors (on a few occasions for approximately
the first 3 weeks of dosing), and/or increased/decreased activity following a dose response.
InĐƌĞĂƐĞĚ ŚĞĂƌƚ ƌĂƚĞ ;јϮϬ ďƉŵͿ͕ ǁŝƚŚŽƵƚ ĐŚĂŶŐĞƐ ƚŽ ŽƚŚĞƌ <' ƉĂƌĂŵĞƚĞƌƐ͕ ǁĂƐ ŽďƐĞƌǀĞĚ Ăƚ Ăůů
doses (including intermittent dosing) starting at 1 month of dosing into three months of dosing
and the effect did not fully recover. Decreased (6%) potassium levels were observed starting at
the MD after 1 month of dosing. There were no histopathological changes (signed path report
is present). The NOAEL in this study is the high dose of 72 mg eq/dog/day (Cmax=791ng/mL,
AUC 550 ng.hr/mL).
Reviewer’s Comments: This study is not conducted at MTD but rather at MFD. The high dose tested in this study
has no exposure difference to the clinical dose and the vehicle tested here is not the clinical vehicle. Brain sectioning
for nonrodents was not done as per Bolon et al., 2013 since this study was conducted prior to the publication of the
position paper.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
39
Study title: JNJ-54135419-AAC: A 9-month toxicity study by the IN route in dogs
Study no.: TOX 10701
Study report location:
Conducting laboratory and location:
Date of study initiation: Oct 23, 2013
GLP compliance: Yes
QA statement: Yes
Drug, lot #, and % purity: JNJ-54135419-AAC, Batch No. A12LD4238,
100.3%
Key Study Findings
x Clinical signs were transient and included salivation, increased activity, uncoordination
characterized by unsteady gait, head drop and collision with the pen furniture, in a dose
responsive manner within 15 minutes of drug administration for up to 1 hr post dose;
lasting up to 2 hours at the high dose of 12 mg/kg/day. Increased activity and
uncoordination persisted throughout the study at 12 mg/kg/day.
x DŝŶŝŵĂů ƚŽ ŵŽĚĞƌĂƚĞ ŽůĨĂĐƚŽƌLJ ĞƉŝƚŚĞůŝĂů ĂƚƌŽƉŚLJ ŝŶ ŵĂůĞƐ ш ϴ ŵŐͬŬŐͬĚĂLJ ďƵƚ ŶŽƚ ŝŶ
females. Focal minimal intra-epithelial accumulation of pale eosinophilic material in the
dorsal meatus at level III of the nasal cavity was observed at all doses in males and at ш8
mg/kg/day in females.
x The NOAEL in this study is 8 mg/kg/day based on clinical signs and nasal histopathology
changes. At this dose the mean Cmax and AUC at NOAEL are 1102 ng/mL and 576
ng.hr/mL for Cmax and AUC, respectively. This is 6.3 times and 1.08 times the
esketamine exposure for Cmax and AUC at the MRHD of 84 mg/day (174 ng/mL for
Cmax and 530 ng.h/mL for AUC for esketamine).
Reference ID: 4395937
(b) (4)
NDA211243 Shiny V. Mathew, PhD, DABT
40
Methods
Doses: 0, 24, 48, and 72 mg eq/dog/day (estimated to be 4
mg/kg/day, 8 mg/kg/day, and 12 mg/kg/day for a
male dog that is about 6 kg; to note, at the end of 9
months, male dogs weighed as much as 10 kg which
means that the highest dose received was 7.2
mg/kg/day)
Frequency of dosing: Twice daily dosing for 39 weeks
Route of administration: IN instillation
Dose volume: Each animal received 2 instillations in each nostril
(100 ul/nostril) on each treatment day. Both daily
instillations were given at 15 ±5 min interval (total
dosing volume 200 uL per nostril or 400 uL per
animal) on each day. Doses were given using a
pipette syringe with attached approximately sized
plastic tip.
Formulation/Vehicle: Water for irrigation, citric acid, EDTA, pH 4.5 via
NaOH and/or HCl
Species/Strain: Beagle Dog
Number/Sex/Group: 4/sex/dose
Age: 5-6 months at initiation
Weight: At the initiation of dosing, 5.3-7.6 kg for M and 5.5-
7.2 kg for F.
Satellite groups: TK was conducted in main study animals
Unique study design: Neurological examination was conducted on all
animals once during pretrial period then prior to the
first dose on D1, and during weeks 14, 27, and 38.
Neurological exam included a subjective observation
of animal in its home pen of the functions controlled
by the cranial nerves comprising: vision, eye
movements, mastication, swallowing, facial
expression, breathing, tongue, neck and head
movement. Animals were removed from home
pens to examine head movement/symmetry, head
muscle tone and eye reaction (menace reflex). Also,
proprioception and postural reaction tests such as
proprioceptive position, hopping and visual and
tactile placing reactions.
Deviation from study protocol: None affecting the overall interpretation of results.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
41
Observations and Results: Changes from Control
Parameters Major findings
Mortality No premature mortalities
Clinical Signs Drug related clinical signs included salivation, increased activity, incoordination (unsteady
gait, head drop, collision with pen furniture and/or tentative placement of limbs) occurring
in a dose responsive manner within 15 minutes postdose lasting up to 1 hr post dose. At
higher doses, the effects were seen up to 2 hours post dose. Increased activity and
incoordination was observed for the first 6 weeks, 15/16 weeks and up to 34 weeks
respectively at the LD, MD, and HD.
Body Weights Unremarkable
Ophthalmoscopy Unremarkable
ECG Unremarkable
Hematology No drug related findings
Clinical Chemistry Changes were noted but none were clearly drug related or of large magnitude.
Urinalysis Unremarkable
Gross Pathology Unremarkable
Organ Weights Unremarkable
Histopathology
Adequate
battery: Yes, for
most tissues but
not for the brain
since sectioning
was not
conducted as per
Bolon et al., 2013.
Minimal to moderate olfactory epithelial atrophy was observed in 1/4 males at MD and 3/4
males at the HD. Additionally, there was a dose response finding of focal minimal intra-
epithelial accumulation of pale eosinophilic material in the dorsal meatus at level III of the
nasal cavity at all doses in males and at MDF (see Table 24).
The pathology summary and the Sponsor’s summary notes vacuolation in the sub-
ependymal neuropil around the third ventricle in 1 MDM. Since this finding was not present
in the HDM, the pathologist concludes that this is unrelated to drug administration. Peer
review, by the Sponsor’s pathologist, notes general agreement with overall interpretation
and conclusion of the study. Peer review mentions “brain sections from all dogs were
evaluated.” But does not discuss any brain finding concerns.
Additionally, cellular debris consisting of multinuclear cells and swollen spermatogenic cells
present in the tubular lumen were seen in the testes and epididymides of 2 LDM and 2
HDM. The pathologist considers this finding to be part of normal background in young adult
male dogs. This conclusion sounds reasonable. Individual animal observations showed
minimal to mild congestion/inflammation of the urinary bladder in 1 HDM, 1MDF, and
1HDF. However, these were not noted in the pathology report suggesting that the
pathologist considered these findings within background.
Special
Evaluation: Neuro
exam
No drug related abnormalities were noted.
LD: low dose; MD: mid dose; HD: high dose.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
42
Table 24: Summary of histopathology findings in dogs from the 9-month toxicity study
Table is excerpted from Study No. TOX10768, P. 904.
Reviewer’s Comments: This study is not conducted at MTD but rather MFD. Brain sectioning was not conducted as
per nonrodent sampling mentioned in Bolon et al., 2013 therefore, fewer brain sections than noted in the current
draft Major Depressive Disorder guidance. The finding of neuropil vacuolation around the third ventricle in 1 male
at the mid dose is a concern due to the nature of its location which may have been missed at higher doses due to
the lack of adequate brain sections. At the same time, the pathologist’s evaluation of this case as incidental since it
was not seen at HD, may be reasonable. The neurological exams conducted in this study were routine subjective
observations and not a dedicated specialized exam.
6.3 General Toxicology Studies Using PMI-100
The general toxicity studies with PMI-100 have been reviewed by Dr. Baishali Kanjilal.
Toxicology studies of up to 3 months were conducted by the previous owner, Javelin
Pharmaceuticals in which PMI-100 (100mg/mL (10% w/v) aqueous
racemic ketamine solution containing 0.002% benzalkonium chloride as an antimicrobial
preservative) was administered via IN route. These studies were conducted with varying
volumes of the drug to reach nominal doses. JRD performed several tolerability/TK studies with
IV racemic ketamine (aqueous solution, pH 4.5, NaCl until isotonic; without benzalkonium
chloride) in nonpregnant and pregnant rats, pregnant rabbits, and dogs to be used as bridging
studies to estimate exposure to esketamine from studies conducted with PMI-100. When IV
racemic ketamine was administered, circulating esketamine exposures were approximately
40%, 50%, and 30% in nonpregnant rats, dogs, and pregnant rats, respectively (see Appendix
Table 36, Table 37 and section 5.2). It is important to note that different vehicles and different
routes of administration were pursued in the bridging studies as compared with Javelin’s
toxicology studies.
Reference ID: 4395937
(b) (4)
NDA211243 Shiny V. Mathew, PhD, DABT
43
IN administration of ш 75 mg/kg/day and SC administration ŽĨ ш40 mg/kg/day in rats and IN
administration of шϳϱŵŐͬŬŐͬĚĂLJ of PMI-100 in CD-1 mice produced transient clinical signs that
were consistent with anesthetic doses of the drug such as wobbly gait, decreased activity,
impaired mobility, circling, prostration, labored breathing, and ataxia. MTD was reached at an
IN dose of 250 mg/kg/day and >80 mg/kg/day when administered subcutaneously in rats and at
>250 mg/kg/day IN for mice. Three months of IN administration of PMI-100 in mice produced
minimal to mild squamous metaplasia and acute inflammation of the nasal cavity at 90
mg/kg/day with NOAEL at 60 mg/kg/day (AUC=2,646 ng.hr/mL for racemic ketamine). A 3-
month study in SD rats showed test article related minimal squamous metaplasia and
hyperplasia of the nasal cavity and bladder/kidney calculi and/or minimal
inflammation/mucosal hyperplasia of the urinary bladder at ш 60 mg/kg/day (AUC at
LOAEL=9,489ng.hr/mL and AUC at NOAEL=1,711 ng.hr/mL for racemic ketamine). After 28-day
dosing in dogs, gross necropsy showed the following findings in the bladder: multiple red foci
and reddened mucosa, minimal chronic inflammation, hyperplasia of the transitional
epithelium, and hemorrhage at ш20 mg/kg/day. The NOAEL for the findings in the bladder in
this study is 4 mg/kg/day (AUC at NOAEL=64 ng.hr/mL for racemic ketamine). These findings
did not fully reverse after 2 weeks of recovery.
Estimating 50% esketamine exposure at NOAEL, nasal cavity findings in mice and rats have a
1.5-2.5-fold safety margin to the clinical exposure at MRHD of 84mg/day. For bladder findings,
there is a 1.5-fold safety margin in rats, however, in dogs there is no safety margin to the
clinical AUC exposure at the MRHD.
7 Genetic Toxicology
7.1 In Vitro Reverse Mutation Assay in Bacterial Cells (Ames)
Study title/Number: Bacterial Reverse mutation assay using racemic ketamine (PMI-
100)*/Study No. AA34UN.503.BTL
Key Study Findings:
x PMI-100 (racemic ketamine; batch No. 46855) was negative for mutagenicity in bacterial
cells in a valid Ames test.
GLP compliance: Yes
Test system: Salmonella typhimurium strains TA98, TA100, TA1535 and TA1537 and Escherichia
ĐŽůŝ ƐƚƌĂŝŶ tWϮ Ƶǀƌ ;Ɖ<DϭϬϭͿ͖ ĚŽƐĞƐ ч ϱϬϬϬ μg/plate in water with Benzalkonium chloride; +/-
S9.
Study is valid: Yes
*Reviewer’s Comments: Esketamine was never tested in an Ames assay but by definition, 50% of the racemate
should be the S-enantiomer. Genotoxic studies were accepted as valid and negative during the IND phase of this
drug.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
44
Study title/Number: Bacterial Reverse Mutation Assay of (Impurity
A; )/Study No. TOX 12465
Key Study Findings:
x JNJ (batch No. I16KB4361) was negative for mutagenicity in bacterial
cells in a valid Ames test.
GLP compliance: Yes
Test system: Salmonella typhimurium strains TA98, TA100, TA1535 and TA1537 and Escherichia
coůŝ ƐƚƌĂŝŶ tWϮ Ƶǀƌ ;Ɖ<DϭϬϭͿ͖ ĚŽƐĞƐ ч ϱϬϬϬ μg/plate in DMSO; +/- S9.
Study is valid: Yes
Reviewer’s Comments: is an impurity in the of
esketamine. Based on the Sponsor’s CMC section (2.3.S.3, table 4), there is no structural alert for this substance in
silico and since it is negative in an Ames assay, its levels are controlled as a nonmutagenic impurity.
7.2 In Vitro Assays in Mammalian Cells
Study title/Number: In vitro mammalian cell gene mutation test (L5178Y/TK=/-
Mouse Lymphoma assay)/Study No. AA34UN.704.BTL
Key Study Findings:
x PMI-100 (racemic ketamine; batch no. 46855) was negative for clastogenicity in mouse
lymphoma cells without activation in both a 4-hr and 24-hr exposure and positive with
S9 with a 4-hour exposure in a valid in vitro mammalian cell gene mutation test.
GLP compliance: Yes
Test system: L5178Y mouse lymphoma cells; doses ч ϭϮϱ μŐͬŵ> ŝŶ ǁĂƚĞƌ н^ϵ ĂŶĚ ч ϳϱ μg/mL in
water.
Study is valid: Yes
Study title/Number: JNJ-54135419: In vitro micronucleus test in human TK6 cells/TOX10413
Key Study Findings:
x Esketamine HCl (batch no. 0142911P) was negative for clastogenicity in human
lymphocytes in the absence of S9 activation in both a 4-hr and 24hr exposure and
positive with S9 with a 4-hour exposure in a valid in vitro micronucleus assay.
GLP compliance: No
Test system: Human TK5 lymphoblastoid cell line; doses ч ϱϰ͘ϲ μŐͬŵ> ŝŶ D^K н^ϵ ĂŶĚ ч
500ug/mL μg/mL in DMSO -S9
Study is valid: Yes
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
45
7.3 In Vivo Clastogenicity Assay in Rodent (Micronucleus Assay)
Study title/Number: PMI-100: Mammalian Erythrocyte Micronucleus test/
AA34UN.123.BTL
Key Study Findings:
x PMI-100 (batch No. 46855) was not clastogenic in a valid in vivo micronucleus assay
after IP injections of ч150 mg/kg plasma concentrations 34-times clinical exposure.
x Mortality occurred at 400 mg/kg. Convulsions observed at 150 mg/kg.
GLP compliance: Yes
Test system: rat, bone marrow micronuclei; single intraperitoneal injections of 37.5, 75 or 150
mg/kg; bone marrow was collected at 24 and 48 hrs after treatment.
Study is valid: Yes
7.4 Other Genetic Toxicity Studies
In Vivo Comet Assay in Rodent (DNA damage)
Study title/ number: In vivo Comet assay in liver cells following intravenous infusion of JNJ-
54135419-AAC in rats/Study No. TOX10530
Key Study Findings:
x Esketamine HCl (batch no. A12BD0277) was not genotoxic in a valid in vivo Comet assay
after IV infusions of ч50 mg/kg which is 11 times the AUC exposure at MRHD of 84 mg.
GLP compliance: Yes
Test system: rat (7-13 weeks old) liver samples; 30 minute IV infusions of 10, 30 or 50 mg/kg for
3 consecutive days in water, pH 4.5.
Study is valid: Yes
Reviewer’s Comments: This study did not test the clinical vehicle containing citric acid and EDTA. The TK data were
determined in a separate study (TOX 12321 (non-GLP) using batch no A12LD4238 of esketamine HCl). AUC for the
esketamine was 5860 ng.hr/mL but Cmax was not determined. For the metabolite(JNJ64115922) AUC
0-t
was 548
ng.hr/mL and Cmax 74.5 ng/mL.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
46
8 Carcinogenicity
8.1 Rat Carcinogenicity
Study title: JNJ-54135419-AAC: A 104-week carcinogenicity study by the IN
route in rats/ Study No.673195
Male and female S-D rats (65/sex/group) were IN administered (via instillation; 50ul/rat)
mg/rat dose of esketamine HCl [in water for irrigation with citric acid and
EDTA (pH 4.5)] estimated at 0 (saline), 0 (vehicle), 4.5, 15, and 45
mg/kg/day for a 200 gram rat. Males were terminated at 104 weeks and females were
terminated at 105 weeks after a drug holiday from 102-105 weeks. Numerical incidence
for Leydig cell adenoma was 1, 0, 1, 1, and 3, respectively, for saline, vehicle, LD, MD,
and HD. However, the p value (p=0.04) did not reach Executive Carcinogenicity
Assessment Committee’s (E-CAC) criteria for statistical significance for common tumors.
Even in the absence of statistical significance, this Reviewer had considered this tumor
finding to be relevant considering the distribution of NMDARs in the male reproductive
system and delays in mating observed in the Segment I study. The administration of
drug in this study (mg/rat) where dosing was done without body weight correction and
the observed body weight decreases at the HD may have impacted tumor formation.
There were no other treatment related increases in tumor incidence in either sex
according to E-CAC criteria for statistical significance. Two HDM in this study had non-
neoplastic lesions of the submucosa of the bladder which could be drug-related
considering ketamine’s known effect on this organ in rats and dogs from Javelin’s
toxicity studies and in humans (Skeldon and Goldenberg, 2014). The mean AUC
exposure at the highest dose of 45 mg/kg/day is 309 ng/mL which is 0.58-times the
clinical exposure at the MRHD of 84 mg.
8.2 Transgenic Mouse Carcinogenicity
Study title: JNJ-54135419: 26 week repeated dose subcutaneous
carcinogenicity study in Tg.rasH2 mice/Study No. AD64VG.7S8R.BTL
Male and female Tg. ras H2 mice (25/sex/dose) were subcutaneously injected doses of
esketamine HCl [in water with citric acid and EDTA (pH 4.5)] at 0
(saline), 0 (vehicle), 10, 25, and 75 mg/kg/day for 26-weeks. Due to high mortality, ECAC
advised the Sponsor to provide a drug holiday of 1-week at the high dose and lower all
doses to 5, 10, and 30 mg/kg/day during the interim phase of the study. The Sponsor
implemented the drug holiday and lowered the high dose to 40 mg/kg/day but did not
lower doses in the other two dose groups. FDA statistical analysis showed a statistically
significant increase in mortality at the mid and high doses in male mice. The overall
number of male mice surviving until the end of the study was adequate. There were no
treatment related increases in tumor incidence in either sex per the E-CAC criteria for
statistical significance. The mean AUC exposure at 40 mg/kg/day is 3,095 ng/mL which is
Reference ID: 4395937
(b) (4)
(b) (4)
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
47
5.8-times the clinical exposure at the MRHD of 84 mg/day.
Reviewer’s Comments: The full review of the carcinogenicity studies and E-CAC meeting minutes can be
found under the IND 114345.
9 Reproductive and Developmental Toxicology
9.1 Fertility and Early Embryonic Development
Study title: JNJ-54135419-AAC: IN Fertility study in the rat
Study no.: TOX 10529
Study report location: Archives of JRD
Conducting laboratory and location:
Date of study initiation: January 23, 2013
GLP compliance: Yes
QA statement: Yes
Drug, lot #, and % purity: JNJ-54135419-AAC, A12BD0277, 99.7%
Key Study Findings
x ĚŽƐĞ ĚĞƉĞŶĚĞŶƚ ĚĞĐƌĞĂƐĞ ŝŶ ďŽĚLJ ǁĞŝŐŚƚ ŐĂŝŶ ;ϭϱйͿ ǁĂƐ ƐĞĞŶ ŝŶ ŵĂůĞƐ Ăƚ ĚŽƐĞƐ ш ϭϱ
mg/kg/day while a dose dependent increase (10-16 %) was seen in females prior to
ŵĂƚŝŶŐ Ăƚ ĚŽƐĞƐ ш ϰ͘ϱ ŵŐͬŬŐͬĚĂLJ͘ dŚŝƐ ŝŶĐƌĞĂƐĞ ƌĞǀĞƌƐĞĚ ĚƵƌŝŶŐ ƚŚĞ ŐĞƐƚĂƚŝŽŶĂů ƉĞƌŝŽĚ
(GD1-7).
x Estrous cycle irregularities were observed at the high dose of 45 mg/kg/day and an
increase in tiŵĞ ƚŽ ŵĂƚĞ ǁĂƐ ŽďƐĞƌǀĞĚ Ăƚ шϭϱ ŵŐͬŬŐͬĚĂLJ͘ dŚŝƐ ĚĞůĂLJ ĚŝĚ ŶŽƚ ĂĨĨĞĐƚ
overall mating and fertility indices.
x The overall NOAEL in this study (based on no change in mating and fertility indices) is 45
mg/kg/day which is 0.6* times the esketamine exposure for clinical AUC at the MRHD of
84 mg/day (530 ng.h/mL for AUC for esketamine).
*Exposure data is the average of male and female rats based on week 26 of the 6-month
chronic study.
Reference ID: 4395937
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
48
Methods
Doses: 0, 0.9, 3, and 9 mg eq/rat/day (estimated to be 0,
4.5, 15, and 45 mg/kg/day of esketamine for a 200
gram rat)
Frequency of dosing: Once daily
Dose volume: All treatment groups received the same volume
(50uL/day; 25ul/nare) with varying drug
concentration in vehicle.
Route of administration: IN instillation
Formulation/Vehicle: Demineralized water adjusted to pH 4.5 ± 0.1 with
NaOH or HCl
Species/Strain: Rat/SPF Sprague Dawley (Crl: CD)
Number/Sex/Group: 22/sex/dose; M rats were 53-70 days old at dosing; F
rats were 49-63 days old at dosing
Satellite groups: None
Study design: Males were dosed for 4 weeks prior to pairing,
during pairing and up to termination. Females were
dosed for 14 days prior to pairing, during pairing and
up to Day 7 of pregnancy.
Deviation from study protocol: None affecting interpretation of study results
Observations and Results
Parameters Major findings
Mortality None
Clinical
Signs
Transient ataxia observed in 2/22 MDM&F and 11/22 HDM and 21/22 HDF in the early part of
the dosing period. Salivation was also observed in most MD and HD rats. No clinical signs at
the LD.
Body
Weights
Premating period: A significant decrease in body weight gain of 15% was observed in males
at the MD and HD during the dosing period prior to mating (see Table 25). A statistically
significant increase of >70% in body weight gain was observed in all dosed females weeks 2-
4. Body weight changes were independent of food consumption.
Mating/Gestation: A decrease in body weight gain of 18% was observed in males at MD and
HD during the mating period. A dose dependent decrease in body weight gain (10-16%) was
observed in all treated females from GD 1-7, reaching statistical significance in MD and HD.
This finding reversed on GD 8-13 with an observed increase in body weight gain (>10%) in
treated females. These changes were independent of food consumption (see Table 26).
Necropsy
Findings
No drug related effects.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
49
Mating and
Fertility and
Pregnancy
parameters
Estrous cycle: A drug effect on estrous cycles was observed at all doses in this study. While
all the CF had cycles of ч 4 days, 2/22, 3/22, and 6/22 females at LD, MD, and HD,
respectively, were either acyclic or had irregular estrous cycles (i.e. some longer and some
shorter than 4-5 days) (see Table 26). Percent of females with regular cycles were 100%,
90%, 86%, and 73% in controls, LD, MD, and HD respectively. Of those that had irregular
cycles, 7%, 6%, and 15% had cycles of greater than 5 days at LD, MD, and HD, respectively
(see Table 26).
Mating and Fertility: Compared with concurrent (2.23) and HCD (2.58), MD and HD had an
increase in mean days to mate of 2.82 and 2.82, respectively. Specifically, a total of 5 pairs
(3/22 in MD and 2/22 in HD) failed to mate in this study within the first 5 days. Three of
these pairs (2 at the MD and 1 at the HD) mated within a 10-day period and were pregnant
at necropsy. In the other two cases (one from each dose), the pairs were separated and the
females were paired with a male from the same group which had previously mated, finally
resulting in successful mating on day 13 and day 17. There was no drug effect on overall
copulation or fertility rate.
Pregnancy: Pre-implantation loss was higher in all treatment groups compared to
concurrent controls (2.8%, 12.35%, 6.02%, 8.95% in Control, LD, MD, HD, respectively). The
values in LD and HD are higher than mean HCD values (6.56%). However, examining
individual data, it appears that this difference is driven by a few dams. The
postimplantation loss and resorptions at the HD was higher than HCD but not from
concurrent control. There were no other notable changes to fertility or litter parameters.
C: Control; LD: low dose; MD: mid dose; HD: high dose; HCD: historical control data
Table 25: Mating and fertility parameters in male rats in the fertility and early embryonic
development study
Estimated doses (mg/kg/day)
Parameter 0 4.5 15 45 HCD
Body weight gain (Week 1-4) (g) 78.5 75.4 65.9* 67*
Body weight gain (Week 4-8) (g) 127.7 124.0 107.5* 109.2*
No. of males that were paired 22 22 22 22
No. of males mated 22 22 21 21
Copulation index (%) 100 100 95.5 95.5 100
Mean number of days prior to mating 2.23 1.95 2.82 2.82 2.58
No. of fertile males 22 22 21 21
Fertility index 100 100 95.5 95.5 96.3
HCD: historical control data,
*
P<0.05
Table 26: Mating and fertility parameters in female rats in the fertility and early embryonic
development study
Estimated doses (mg/kg/day)
0 4.5 15 45 HCD
Body weight gain (Week 2-4) (g) 8.9 15.2* 16.6* 15.1*
Body weight gain (GD 1-7) (g) 37.3 33.7 31.2* 32.2*
Body weight gain (GD8-13) (g) 29.4 32.4 34.2* 32.4
# of rats (regular estrous cycles) 22 20 19 16
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
50
# of rats (Irregular estrous cycles i.e. other
than 4-5 day cycles)
0 0 0 3
# of rats (Acyclic) 0 2 3 3
% of F with < 4 days 0 0 0 1
% of F with 4 days
$
100 93 94 84
% of F with 5 days 0 4 2 6
% of F with 6-10 days 0 0 0 6
% F with >10 days 0 3 4 3
Embryo-fetal parameters
Corpora lutea (mean no. per animal) 15.7 16.2 16.5 17.6* 16.81
Implantations (mean no. per animal) 15.6 14.7 16 16.2 15.6
Resorptions (mean no. per animal 1.27 0.50* 0.95 1.14 0.83
Preimplantation loss (%) 2.8 12.35 6.02 8.95 6.56
Postimplantation loss (%) 8.04 3.44 5.93 7.12 5.64
HCD: historical control data
$
This % of rats does not include those that were acyclic.
*
P<0.05
Reviewer’s comments: Effect of vehicle on fertility was not tested in this study. The Sponsor attributes increase in
time to mate in this study to female estrous cycle irregularities. However, due to mating of treated rats (i.e. both
males and females were treated), this mating delay could be mediated by an effect of drug on one sex or both
sexes. However, overall mating and fertility indices (i.e. total number of rats mated and found pregnant) are not
affected. The Sponsor notes that estrous cycle irregularities observed in this study is consistent with published
literature on ketamine’s known effect on suppression of circulating progesteƌŽŶĞ͕ ƚĞƐƚŽƐƚĞƌŽŶĞ͕ ĂŶĚ ϭϳɴ ĞƐƚƌĂĚŝŽů͘
9.2 Embryonic Fetal Development
9.2.1 Rat Embryonic Fetal Development
Study title.: A developmental toxicity (Segment II) study in Sprague-Dawley
rats with PMI-100
Study no.: 3542.11
Study report location:
Conducting laboratory and location:
Date of study initiation: October 11, 2001
GLP compliance: Yes; except for mating conducted in a non-
GLP lab
QA statement: Yes
Drug, lot #, and % purity: Ketamine HCl, Lot No. 42727, 100.6%
Reference ID: 4395937
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
51
Key Study Findings
x Maternal toxicity NOAEL is the 50 mg/kg/day based on the severity of clinical signs
related to anesthetic properties of the drug at 150 mg/kg/day. A drug related
embryofetal toxicity is not evident in this study.
x Deviation in concurrent control data as compared to HCD is attributed to large and
varying volumes of instillation used in this study.
x Assuming that 50% of circulating drug species is esketamine when PMI-100 is
administered, there is no evidence of teratogenicity in rats at a dose of up to 12-fold the
MRHD (Cmax=174 ng/mL and AUC=530 ng.h/mL for esketamine in the clinic) of 84
mg/day.
Methods
Doses: 0, 15, 50, and 150 mg/kg/day
Frequency of dosing: Once daily
Dose volume: Varying dosage volumes of 1500, 150, 500, and 1500
uL/kg/day, respectively for doses of 0, 15, 50 and
150 mg/kg/day.
Route of administration: IN instillation
Formulation/Vehicle: Water for injection
Species/Strain: Crl:CD (SD)IGS BR rats
Number/Sex/Group: 25F/group
Satellite groups: 6F/dose were assigned for TK
Study design: Time mated female rats were dosed from GD6
through GD17. Fetuses were delivered by C-section
on GD20 and examined.
Deviation from study protocol: None affecting the interpretation of results
Observations and Results
Parameters Major findings
Mortality No drug related effect.
Clinical Signs Drug related anesthetic effects such as salivation, wobbly gait and impaired mobility, and/or
decreased activity were observed at the MD and HD. In addition, ocular discharge, dark
material around nose, rough coat, and nystagmus were also observed in MD and HD.
Body Weights Absolute body weight (uncorrected) was not significantly different between control and
ƚƌĞĂƚĞĚ ƌĂƚƐ ;ŝ͘Ğ͘ ŶŽƚ хϭϬйͿ͘ ŽĚLJ ǁĞŝŐŚƚ ŐĂŝŶ ;љϭϮйͿ Ăƚ ƚŚĞ , ďĞƚǁĞĞŶ ' ϲ-17 and
rĞĂĐŚĞĚ ƐƚĂƚŝƐƚŝĐĂů ƐŝŐŶŝĨŝĐĂŶĐĞ͘ ŽƌƌĞĐƚĞĚ ŵĂƚĞƌŶĂů ďŽĚLJ ǁĞŝŐŚƚ ĐŚĂŶŐĞ ǁĂƐ љϭϰй ĂŶĚ
љϵ͘ϲй ĨŽƌ D ĂŶĚ ,͕ ƌĞƐƉĞĐƚŝǀĞůLJ͘
Necropsy
findings
Cesarean Section
Data
Corpora lutea, implantation sites, live fetuses, # of male and female pups, and
postimplantation loss were lower in this study compared with HCD (See
Table 27). There was a drug effect following a dose response in the mean number of male
and female pups (53% M in C vs. 48.5% in HD; 46.7% F in C vs. 51.5% in HD). These numbers
were out of the range for the HCD of the lab. Fetal body weight on the other hand was higher
in concurrent control than HCD.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
52
Necropsy
findings
Offspring
A tabular summary of malformations and variations that appear to change with treatment
provided in Table 28 below. For many of the endpoints, concurrent control appears to have
an increased incidence compared with treatment and HCD.
Toxicokinetic See tabular summary of TK data in section 5.2. Tmax was reached within 15 minutes. Drug
accumulation appeared to have occurred based on the doubling of AUC exposure by GD 17.
LD: low dose; MD: mid dose; HD: high dose; HCD: historical control data
Table 27: Cesarean section findings from rat embryo-fetal development study with PMI-100
Segment 2 study parameters (PMI-100) (varying volumes)
Dose (mg/kg/day) 0 15 50 150 HCD range
Body weight gain in g (GD 6-17) F0 67 72 61 59*
Corrected body weight change in g 73 74 63* 66
Corpora lutea (per animal) 13 14.2 14.3 13.7 16.3-19.3
Implantation sites (# per animal) 11.6 13 13.2 12.3 15.1-18.2
Pre implantation loss (# per animal) 1.4 1.2 1.1 1.5 0.7-2.3
Live fetuses (per animal) 11.2 12.5 12.5 11.7 13.9-17.3
Males (mean %) 53 51 46.7 48.5 44-49
Females (mean %) 46.7 48.9 53.3 51.5 49-51
Postimplantation loss(# per animal) 0.4 0.5 0.7 0.5 0.6-1.6
Fetal body weight (g) 4 3.8 3.8 3.7 3.5-3.8
Table 28: Offspring necropsy findings from rat embryo-fetal development study
with PMI-100
Segment 2 study parameters (PMI-100) malformations (varying volumes)
Dose (mg/kg/day) 0 15 50 150 HCD range
% with visceral malformations fetal (litter) 10 (26) 4 (20) 3 (12) 3 (8) 0-0.6 (0-
4.5)
Total % with malformations fetal (litter) 10 (30) 4 (20) 3 (16) 4 (12) 0-1 (0-8)
Seg 2 study parameters (PMI-100) variations
% with Sternebrae malaligned slight/moderate
fetal (litter)
16 (48) 15 (56) 17 (56) 22 (54) 11-44 (42-
96)
% with Reduced ossification of the 13
th
rib
fetal (litter)
0.7 (4) 0 (0) 0.6 (4) 1.4 (8) 0-8 (0-4)
Reviewer’s comments: This study did not test the effect of the commercial drug substance or vehicle on
embryofetal parameters. The methodology used in this study (i.e. the large amounts and varying instillation
volumes) adds additional stress on the maternal dams and makes the interpretation of the results difficult.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
53
9.2.2 Rabbit Embryonic Fetal Development
Study title.: A developmental toxicity (Segment II) study in New Zealand white
rabbits with PMI-100
Study no.: 3542.13
Study report location:
Conducting laboratory and location:
Date of study initiation: December 14, 2001
GLP compliance: Yes; except for mating conducted in a non-
GLP lab
QA statement: Yes
Drug, lot #, and % purity: Ketamine HCl, Lot No 42727, 100.6%
Key Study Findings
x Maternal toxicity characterized by decreased body weight gain and feed consumption
occurring at ш30 mg/kg/day.
x Developmental toxicity characterized by skeletal malformations and observed at ш30
mg/kg/day.
x The NOAEL for maternal and embryofetal toxicities is 10 mg/kg/day which is estimated
to be 0.3* times the AUC exposure at MRHD.
*Ketamine exposures could not be determined at IN 10 mg/kg/day dose in the Segment II
study in rabbits. The esketamine estimate here is derived from PK bridging data with
8mg/kg/day IV ketamine assuming linearity of exposure (at 10 mg/kg/day of ketamine
administration, AUC exposure for esketamine is 148 ng.hr/mL). Therefore, the esketamine
exposure here may be overestimated.
Methods
Doses: 0, 10, 30 and 100/50 mg/kg/day
Frequency of dosing: Daily
Dose volume: varying IN volumes of 1000/500, 100, 300 and
1000/500 uL/kg/day respectively for 0, 10, 30 and
100/50 mg/kg/day
Route of administration: IN instillation
Formulation/Vehicle: Sterile water for injection
Species/Strain: New Zealand white rabbits
Number/Sex/Group: 20F/group
Satellite groups: TK: 3F/group
Study design: Pregnant rabbits were dosed from GD6-GD18. The
fetuses were delivered by C-section on GD29 and
Reference ID: 4395937
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
54
examined.
Deviation from study protocol: Yes. Due to unexpected mortality, the high dose was
lowered to 50 mg/kg/day by lowering volume to
500ul/kg/day (in both HD and control groups) after
the first 5 days of dosing. Therefore, the does
received the lower dose starting on GD 11 until the
remainder of the dosing period.
Observations and Results
Parameters Major findings
Mortality Five HDF were found dead on GD 7/8. Two HDF from the TK group was added to the main
study to meet the minimum requirement for the study.
Clinical Signs One MDF aborted on GD25 and 1 HDF delivered early on GD 28. Dose dependent clinical signs
as expected for an anesthetic drug such as wobbly gait and decreased activity were observed
at both MD and HD. In addition, wetness around nares, salivation, dilated pupils, and ocular
discharge were noted in these F. Lateral recumbency, shallow breathing, eyes dark in color
were all noted in HDF. One LDF had wetness around nares. In premature decedents or those
that aborted early, the clinical signs included decreased activity, decreased food
consumption, lateral recumbency, wobbly gait, shallow breathing, eyes dark in color, reddish
nasal discharge, and/or soft/mucoid stools.
Body Weights At the end of the dosing period, HD dams had a 4% decrease in absolute body weight which
ƌĞĂĐŚĞĚ Ă ƐƚĂƚŝƐƚŝĐĂů ƐŝŐŶŝĨŝĐĂŶĐĞ͘ љ ŝŶ ŵĞĂŶ ďŽĚLJ ǁĞŝŐŚƚ ŐĂŝŶ ŽĨ ϭϮй͕ ϱϬй͕ ĂŶĚ ϱϳй ǁĂƐ
observed in LD, MD, and HD; respectively, compared to control, during the dosing period
(GD 6-18). This difference reached statistical significance at both the MD and HD. When
dosing was stopped (GD 18-29) this effect reversed for LD and MD but not for the HD dams
(see Table 27). Gravid uterine weights were not significantly different from one another.
When corrected maternal body weight (maternal body weight change-gravid uterine weight)
was evaluated, a significant effect of drug on maternal body weight was also observed for
ƚŚĞ D ŐƌŽƵƉ ;ŝ͘Ğ͘ љϯϯйͿ ĂŶĚ Ăůů ƚŚĞ ǁĞŝŐŚƚ ŐĂŝŶ Ăƚ ƚŚĞ , ǁĂƐ ĨƌŽŵ ŐƌĂǀŝĚ ƵƚĞƌŝŶĞ ǁĞŝŐŚƚ
(see Table 27) .
Necropsy findings
Cesarean
Section Data
Mean number of post implantation loss was >2x in all dose groups compared with control but
not strictly dose-dependent (i.e. 0.2, 0.4, 1, and 0.7 for C, LD, MD, and HD, respectively) and
within HCD (see Table 29).
Necropsy findings
Offspring
External malformations such as anal atresia and/or short tail were present in a total of 3
fetuses in 2 litters at the HD. Fused kidney, a visceral malformation was present in 1 HDF.
The litter incidences for skeletal malformations at the high dose were as follows:
intraparietal bipartite (1/15), jugals misshapen (1/15), cervical vertebral anomaly (2/15),
vertebral anomaly with/without rib anomaly (3/15), thoracic centrum anomaly (1/15), fused
ribs (1/15), and costal cartilage anomaly (1/15). Total skeletal malformations, were
increased based on fetus and litter number at the MD and HD from concurrent controls (see
Table 30). Total number of malformations was increased at all doses and above the HCD for
the lab.
Toxicokinetic See tabular summary of TK data in section 5.2. Tmax was reached within 15 minutes. There
was no drug accumulation in this study.
LD: low dose; MD: mid dose; HD: high dose
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
55
Table 29: Caesarian section findings from rabbit embryo-fetal development study with PMI-
100
Segment 2 study parameters (PMI-100) (varying volumes) rabbit
Dose (mg/kg/day) 0 10 30 100/50 HCD range
Body weight gain (D 6-D18) (g) 233 204 116* 100* ___
Body weight gain (D18-29) 241 237 299 209 ___
Gravid uterine weight (g) 507 502 526 515 ___
Corrected maternal body weight change
(g)
124 129 82 -1 ___
Pregnancy rate (%) 95 100 85 75 70-100%
Corpora lutea (mean#/animal) 9.5 9.7 10.4 10 8.6-10.4
Implantation site (mean #/animal) 8.3 8.8 9.8 9.3 5.7-10
Preimplantation loss (mean number per
animal)
1.2 0.9 0.6 0.7 0.4-2.9
Postimplantation loss (mean number per
animal)
0.2 0.4 1.0 0.7 0.2-1.1
Early resorption mean # per animal) 0.1 0.2 0.6 0.3 0.2-0.9
Late resorptions mean# per animal) 0.1 0.3 0.4 0.3 0-0.4
*=p<0.05
Table 30: Offspring necropsy findings from rabbit embryofetal development study with PMI-
100
Segment 2 study parameters (PMI-100) (varying volumes) rabbit
Dose (mg/kg/day) 0 10 30 100/50 HCD range
Short tail (fetal) (%) 0 0 0 2% ___
Short tail (litter) (%) 0 0 0 13% ___
Cervical vertebral anomaly (fetal) (%) 0 0 0 3% 0-1.91%
Cervical vertebral anomaly (litter) % 0 0 0 13% 0-11.76%
Vertebral anomaly with/without rib
anomaly (fetal) (%)
1.2% 0.6% 2% 3% 0-2.33%
Vertebral anomaly with/without rib
anomaly (litter) (%)
5% 5% 12% 20% 0-15%
Fetus with skeletal malformations (%) 3% 3% 8% 8% 0-6%
Litters with skeletal malformations (%) 16% 25% 47% 40% 0-31%
Total malformations (fetal) 4.5% 4.2% 11% 9% 0-6.38%
Total malformation (litter) 26% 35% 58% 46% 0-31%
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
56
9.3 Prenatal and Postnatal Development
Study title: Esketamine hydrochloride (JNJ-54135419): study for effects on pre-
and postnatal development in the Crl: CD (SD) rat by IN administration
Study no.: TOX10766
Study report location:
Conducting laboratory and location:
Date of study initiation: December 23, 2013
GLP compliance: Yes
QA statement: Yes
Drug, lot #, and % purity: JNJ-54135419-AAC, A12LD4238, 100.3%
Key Study Findings
x DĂƚĞƌŶĂů ƚŽdžŝĐŝƚLJ ;&Ϭ ĚĂŵƐͿ ŽĐĐƵƌƌĞĚ Ăƚ шϭϱ ŵŐͬŬŐͬĚĂLJ ďĂƐĞĚ ŽŶ Ă ƚƌĂŶƐŝĞŶƚ ĚĞĐƌĞĂƐĞ ŝŶ
body weight gain and decrease in food consumption from GD 6-10 but reaching control
levels at the end of the gestation period. Adverse clinical signs were observed in
ŵĂƚĞƌŶĂů ĚĂŵƐ ƚŚƌŽƵŐŚŽƵƚ ŐĞƐƚĂƚŝŽŶ ĂŶĚ ůĂĐƚĂƚŝŽŶ Ăƚ шϰϱ ŵŐͬŬŐͬĚĂLJ͘
x A dose response delay in Preyer response reflex was observed independent of a drug
effect on body weight in this study. On D14, only 69.4%, 66.1%, and 52.8% at LD, MD,
and HD reached this development milestone compared with 84.3% in controls. This
effect normalized by PND19.
x /Ŷ ƚŚĞ ƉŽƐƚǁĞĂŶŝŶŐ ƉĞƌŝŽĚ͕ ŵŽƚŽƌ ĂĐƚŝǀŝƚLJ ǁĂƐ ĚĞĐƌĞĂƐĞĚ Ăƚ ш ϭϱ ŵŐͬŬŐͬĚĂLJ ǁŝƚŚŽƵƚ ĂŶ
effect on learning, habituation, sexual development, mating, and fertility.
x The NOAEL for maternal toxicity is 4.5 mg/kg/day, no NOAEL for pup physical
development during the pre-weaning period and 4.5 mg/kg/day for post weaning
development which is 0.07-times
†
, <0.09-times
‡
, and 0.09-times
‡
times; respectively,
the human exposure (Cmax=174 ng/mL and AUC=530 ng.h/mL for esketamine) at the
MRHD of 84 mg/day.
†
There were no TK data from maternal dams available in this study. Exposure data were taken from female
animals in the2-year carcinogenicity study in rats.
‡
PND 4 AUC values are used for exposure margin calculation in F1 offspring (see table 38 in the Appendix).
Reference ID: 4395937
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
57
Methods
Doses: 0, 0.9, 3, and 9 mg eq/rat/day (estimated to be 0,
4.5, 15 and 45 mg/kg/day of esketamine for a 200
gram rat).
Frequency of dosing: daily
Dose volume: All treatment groups received the same volume
(50uL/day; 25ul/nare) with varying drug
concentration in vehicle.
Route of administration: IN instillation
Formulation/Vehicle: Pyrogen free water/water for injection with
citric acid and EDTA (pH 4.5)
Species/Strain: Crl: CD (SD) rat
Number/Sex/Group: 22/sex/dose
Satellite groups: No satellite group; TK was conducted in F1 offspring
on PND4 and PND12
Study design: Pregnant rats (F0 dams) were dosed from
gestational day (GD) 6 to day 20 of lactation,
inclusive. Blood was collected from 4 F1 pup culls on
PND 4 and 12 but not from F0 dams.
In addition to routine parameters, Preyer response
reflex was assessed daily from D9 of age until
achieved or D19 of age in the F1 offsprings. Brain
weights were taken for F0 dams and F1 offsprings.
Brain histopathology, targeting cingulate
gyrus/retrosplenial cortices, was done on 5
randomly selected F0 dams, pups on PND4, PND12,
and PND21, and adults from F1. Preyer response
testing was done as follows: individual pups were
gently restrained in the hand of the observer. With
background noise kept to a minimum, a dog clicker
was used to generate a sound of (75-85dB)
approximately 8cm behind the pup and assessed for
response. Reactions such as ear or head twitching
or jumping were deemed a positive response and
the pup was considered to have passed the test.
Deviation from study protocol: None affecting interpretation of study results
Observations and Results
Generation Major Findings
F0 Dams Mortality: Two deaths: 1CF found dead after parturition; 1LDF euthanized humanely on D23 due
to difficulties in parturition.
Clinical signs: At the HD, unsteady gait, salivation, and decreased activity were observed from first
day of dosing (GD6) until D18 of lactation in nearly all animals; one female had circling behavior
Reference ID: 4395937
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
58
on D4 of lactation. These signs were observed 5-15 min after dosing and were not observed at
the end of the working day, except for salivation. These signs decreased in incidence and severity
at lower doses.
Body weight: There were no changes to absolute body weights in this study but there were
statistically significant decreases in body weight gain at MD and HD (35% and 41% lower than
control, respectively) initially from GD 6-10. This decrease was accompanied by a decrease in
food consumption at the MD and HD during the same time period. The decrease in body weight
returned to control levels by the end of gestation. Absolute body weight and body weight gain
were less than 10% from D1 to D 21 of lactation.
Uterine content: A slight increase in gestational length is observed at the HD (i.e. 64% of control
animals delivered by GD22 in comparison to only 50% at the HD). However, all F had delivered by
GD 23 (No HCD provided for gestational length). There were also no significant differences in
pup sex ratios, pup birth weight, or pup body weight gain.
Necropsy/Histopathology: H&E staining in brain sections at three levels targeting the cingulate
gyrus/cores of the retrosplenial cortices showed no salient changes.
F1
Generation
Survival: No drug effect
Clinical signs: No drug effect
Body weight: No drug effect
Physical development: There was a dose-dependent delay in age of attainment of Preyer response
reflex where it was tested from PND9-19. By D14 (M&F combined), 84.3% of control vs. 69.4, 66.1,
and 52.8% had attained this reflex at LD, MD, and HD (no HCD provided for this parameter) (Table
31). The mean age for this reflex reached a statistical significance at the HD (14.5 days vs. 13.8
days in control). This delay was not correlated with a concurrent decrease in body weight at the
same age. All pups attained Preyer reflex by D19. There was no drug effect on other preweaning
examinations like pupil reflex, auditory startle response or air righting day.
Neurological assessment: After weaning, pups (N=20/sex/dose) were tested on motor activity
(PND 22), prepulse inhibition of auditory startle response (PND24/25), and Morris Water (MW)
maze (PND 31). High beam breaks (rearing activity) was nonstatistically decreased in F1 offspring
by 22% in both MDM and HDM and low beam break (ambulatory activity) was decreased by 12% at
HDM. Effect is not clear in F. In MW maze, dose dependent decreased number of sector entries
(30%) and decreased trial time (30%) in HDF, reaching statistical significance for the former on D2.
No HCD provided for postweaning neurological assessment.
Reproduction: There was no esketamine effect on balanopreputial separation or vaginal opening.
No effect on precoital interval, mating performance and fertility in F1 rats.
Organ weight: Brain weights were measured in F1 pups. There were decreases in absolute brain
weight but not when corrected for body weight.
Necropsy/Histopathology: No brain histopathological changes were noted in 5 randomly selected
pups on PND 4, 12, 21, and adults from F1 generation with H&E stain.
Toxicokinetics: See Table 41 in the Appendix for exposure data from the F1 pups on PND 4 and
PND 12.
F2
Generation
Litter data: No effect on drug treatment on F0 generation observed in F2 litter parameters such as
mean corpora lutea, implantations, resorptions, live embryos, and pre/post implantation losses.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
59
Table 31: Effects of esketamine administration on parameters examined in the pre- and post-
natal development study in rats.
PPND study parameters
Dose (mg/kg/day; estimated) 0 4.5 15 45 HCD
(mean)
Body weight gain (GD 6-10)F0 17 14 11** 10** ___
Body weight gain (GD 6-20) F0 114 118 113 112 ___
% passed Preyer reflex on D14 F1 84.3 69.4 66.1 52.8 ___
Total Locomotor activity (high
beam) (males)F1
182.9 172.5 142.8 141.8 ___
Total Locomotor activity (low
beam) (males)F1
626.6 611 614 545.7 ___
Total Locomotor activity (high
beam) (females) F1
177.7 153.8 141.5 171.2 ___
Total Locomotor activity (low
beam)(females) F1
617 550 517.6 599.4 __
Preimplantation loss F2 (%) 5 6.7 4.8 6.2 7.2
Postimplantation loss F2 (%) 8.3 7 4.5 6.3 6.2
Reviewer’s comments: The drug administration as conducted in this study (mg/rat) would suggest that maternal
dams received less exposure to esketamine as their body weight increased. Even in the presence of less than
optimal dosing paradigm, there was a dose dependent delay in Preyer response reflex (sound-induced movement of
the external part of the ear) suggesting that the drug causes an initial delay in sensorimotor development which
normalizes over time. Preyer reflex is the elicitation of startle response to auditory stimuli and has been widely used
for hearing in rodent. This test is effective for identifying profound sensorineural hearing loss and effect on
brainstem response in experimental animals. It is well known that NMDA receptor antagonists like ketamine and
MK-801 impair EEG/ERG readout and therefore mimic the EEG deficits observed in patients with schizophrenia. The
finding of normalization of the delay by PND 19 and lack of drug effect on PPI when tested on PND24/25 would
suggest that the drug does not have a long-lasting consequence on sensory gating in F1 offspring.
10 Special Toxicology Studies
Other Toxicology Studies
The Sponsor of this NDA has submitted a total of 10 neurotoxicity studies including dose range
finding studies, those for PMI-100, those for IN esketamine, and those examining neuronal
apoptosis in juvenile animals. These studies are: TOX 10820: tolerability study for dose
selection for the pivotal 2-week neurotox study, TOX 10950: 2-week repeat dose IN
neurotoxicity study using esketamine, TOX12438: range finding study in juvenile rats,
TOX13050: 2-week intermittent dosing neurotoxicity study using esketamine in juvenile rats,
TOX11374: single dose neurotoxicity study in female rat using esketamine, TOX 11334: single
dose TK study using esketamine, Study No. 3542.9A: acute neurotoxicity study in rats using
PMI-100, Study No. 3542.9B: 28-day neurotoxicity study using PMI-100, TOX JIR00009: PMI-100
vehicle effect on neurotoxicity, and TOX10415: single dose neurotoxicity study using IN
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
60
esketamine in rats. The neurotoxicity studies in juvenile rats will not be reviewed under this
NDA since the indication here is not relevant for pediatric population. For Olney lesion toxicity
evaluation, the appropriate sacrifice time points are 2-4 hours after the Tmax and 3-days after a
single dose for neuronal vacuolation and necrosis, respectively, for most drugs. Of the studies
conducted in adult rats, only valid studies are summarized below.
Esketamine HCl (JNJ 54135419-AAC): Single dose neurotoxicity study by IN
administration to female rats/ Tox 10415 (GLP; signed pathology report)
Adult female Crl:CD (SD) rats (12-14 weeks of age; 10F/dose/timepoint) were administered
esketamine hydrochloride (Batch No. 0142911P) doses of 0 (pyrogen free water pH 4.5), 0.9, 3,
and 9 mg/rat (0, 4.5, 15 and 45 mg/kg/day of esketamine for a 200 gram rat) via IN instillation
(50 ul/rat). The sacrifice time points in this study were 4 hours and 7 days post dose. The MK-
801 positive controls showed minimal to moderate neuronal vacuolation at the 4-hr time point
but were euthanized prematurely due to humane reasons on D2. Therefore, the 4-hr time
point is valid and negative for neuronal vacuolation but not the 7-day time point for necrosis.
The AUC
0-ь
exposure is 936 ng.h/mL and Cmax is 791ng.h/mL which is 1.8 and 4.5 times clinical
exposures (AUC=530 ng.h/mL and Cmax=174 ng/mL for esketamine) at the MRHD of 84
mg/day.
JNJ54135419: A single dose IN neurotoxicity study in the female rat/Tox11374: (GLP;
signed path report).
Sprague-Dawley (Crl:CD) rats (12-14 weeks; 12-15F/group/time point) were IN administered
esketamine HCl (batch No. 0142911P) at doses of 0 (citric acid , EDTA
and NaOH to PH 4.5), 36, 54 or 72 mg eq/rat (100ul/rat/instillation) via twice, thrice or 4-times
in one day. These doses are estimated to be 180, 270 and 360 mg/kg for a 200 gram rat.
Sacrifice time points were 48 and 96 hours post dose. There were a total of 4 deaths at the
highest dose (2 main and 2 TK). Premature decedents showed ataxia, bradypnea, severely
decreased activity, decubitus, catalepsy, salivation, and/or narrowed palpebral fissures. At
necropsy, 2 main study animals showed discoloration in lungs and/or hemmorrahge in the
pleural cavity. Rats that survived also showed decreased activity, ataxia, audible respiration
with the first two occurring for 1.5 hrs, <3 hr, and >3 hrs postdose at LD, MD, and HD. This
study did not examine the appropriate sacrifice time point for neuronal vacuolation. However,
this is a valid and negative study for the observation of necrosis at a dose of 72 mg/eq (lower
doses were not histopathologically analyzed). Exposure at 72 mg eq had a Cmax of 10,245
ng/mL and AUC of 45,800 (only N=2 TK). Due to the high variability of TK between these two
animals, comparison to the next lower dose of 54 mg eq/rat (270 mg/kg) where Cmax is 4070
ng/mL and AUC is 9430 ng.hr/mL (N=4) may be appropriate. A dose of 54 mg eq/day has a
safety margin of 23-and 17-fold to clinical exposures to Cmax and AUC, respectively (Cmax=174
ng/mL and AUC=530 ng.h/mL for esketamine) to the MRHD of 84 mg/day.
Reference ID: 4395937
(b) (4)
(b) (4)

NDA211243 Shiny V. Mathew, PhD, DABT
61
An acute subcutaneous neurotoxicity study in rats with PMI-100/Study No. 3542.9A
(GLP; signed pathology report)
Sprague-Dawley (Crl:CD(SD)IGS BR rats (11-12 weeks old; 4/sex/group/sacrifice timepoint) were
subcutaneously administered a single dose of PMI-100 (batch No. 46855) at 0, 4, 15, and 60
mg/kg. This study used sacrifice time points of 6 hrs, 24 hrs, 72 hrs, and 2 weeks post dosing
and stains such as H&E, Fluoro-Jade/DAPI, and amino cupric silver (de Olmos method).
Functional Observation Battery (FOB) and Biel water maze learning/memory testing was done
in this study. The Biel water maze study design was: day 5 (swimming trial), 6-9 (learning trial),
10-11 (rest days), and day 12 (memory trial). Clinical signs were as expected for anesthetic drug
ůĂƐƚŝŶŐ ϭ Śƌ ƉŽƐƚĚŽƐĞ Ăƚ ш ϭϱ ŵŐͬŬŐ͘ Minimal neuronal vacuolation was observed in layer 1 of
the retrosplenial cortex of females at 60 mg/kg at the 6 hr sacrifice time point with H&E
staining. Minimal neuronal degeneration observed in 2/4 F at 60 mg/kg with amino cupric
silver staining was noted to be within background considering the increased sensitivity of the
stain. A subcutaneous dose of 0.5 mg/kg of MK-801 produced mild to moderate vacuolation in
layers 2 and 3 of the retrosplenial cortex of females and minimal to mild degree of neuronal
necrosis with H&E again only in females. The ketamine exposures in female rats at NOAEL for
vacuolation in this study are 1,577 ng/mL for Cmax and 1,686 ng.hr/ml for AUC
0-ь
. NOAEL for
neuronal degeneration is 60 mg/kg which provides exposures in female rats of 5,523 ng/mL for
Cmax and 10,781 ng.hr/ml for AUC
0-ь͘
Presuming that 50% of the circulating species is
esketamine when ketamine is administered, the exposure in females for esketamine at the
NOAEL for vacuolation is 788 ng/mL for Cmax and 843 ng.hr/mL for AUC. Similarly, the
presumed esketamine exposure in females at the NOAEL for neuronal degeneration (e.g. the
HD used in this study) is 2,761 ng/mL for Cmax and 5,390 ng.hr/mL for AUC. Therefore, the
NOAEL for vacuolation provides a safety margin of 4.5-fold for Cmax and 1.6-fold for AUC to
clinical exposures at the MRHD of 84 mg/day. The NOAEL for degeneration provides a safety
margin of 16-fold for Cmax and 10-fold for AUC to clinical exposures at the MRHD of 84
mg/day.
There was also a 28-day repeat-dose neurotoxicity study (Study No. 3542-9b) with sacrifice time
points at 6 hrs, 24hrs, 48 hrs, and 14 days after the last dose. Doses of PMI-100 were exactly
the same as that used in the single dose study. The results of a Biel water memory test showed
a non-statistically significant but a dose dependent increase in trial time on D3&4 (learning
delay) and on memory recall trial (memory delay) (nonstatistically significant) in males but no
effect was observed in females. In this study, MK-801 positive control rats did not show
vacuolation nor neuronal necrosis with H&E staining. With amino cupric silver stain, minimal to
moderate late stage neuronal and axonal degeneration was observed in 2/4 females but not
males. Occasional minimal necrosis in a HDM treated with 60 mg/kg PMI-100 was noted as
background by the pathologist.
Reviewer’s Comments: The single dose study (study No. 3542.9A) using PMI-100 was not conducted at MTD based
on the transient clinical signs observed. The sacrifice time point for neuronal vacuolation was appropriate and
valid, however, the sample size was small. The sacrifice time point in the 28-day study (Study No. 3542.9B) was
not appropriate to detect vacuolation/degeneration as seen by the lack of findings in positive control females and
the sample size was too small to be considered an adequate Olney study. The single dose acute toxicity study with
Reference ID: 4395937
NDA211243 Shiny V. Mathew, PhD, DABT
62
PMI-100 is a well conducted study based on histopathology, time points of sacrifice, and tissue sectioning although
only a small sample size was used; therefore, the results from the single dose study are accepted.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
63
11 Appendix/Attachments
Figure 1: Proposed in vitro metabolic pathways of esketamine in liver microsomes and S9
fractions of various species.
(Excerpted from the Sponsor’s Nonclinical overview, P.33)
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
64
Figure 2: Esketamine (above) and noresketamine (below) exposure in nonclinical species
relative to humans.
(Excerpted from the Sponsor’s nonclinical overview, P. 45-46).
Reference ID: 4395937


NDA211243 Shiny V. Mathew, PhD, DABT
66
Figure 3: Nasal cavity, brain and larynx dissections in the rat from the 6-month toxicity study.
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
67
Table 36: TK data from bridging studies after IV administration of racemic ketamine in non-
pregnant rats.
Table is excerpted from TOX 10457, P.2
Table 37: TK data from bridging studies after IV administration of racemic ketamine in dogs.
Table is excerpted from TOX 10458, P.8
Reference ID: 4395937

NDA211243 Shiny V. Mathew, PhD, DABT
68
Table 38: TK parameters from F1 offsprings in the pre- and postnatal development study on
PND 4 and PND12.
Table is excerpted from TOX 10766, P.57
References
Bolon B, Garman RH, Pardo ID, Jensen K, Sills RC, Roulois A, Radovsky A, Bradley A, Andrews-
Jones L, Butt M, and Gumprecht L. (2013) STP Position paper: recommended practices
for sampling and processing the nervous system (brain, spinal cord, nerve and eye)
during nonclinical general toxicity studies. Toxicol Pathol. 41:1028-1048.
Brambilla G, and Martelli A. (2007) Genotoxic and carcinogenic risk to humans of drug-nitrite
interaction products. Mutat Res, 635:17-52.
Chang T, and Glazko AJ. (1974) Biotransformation and disposition of ketamine. Int Anesthesiol
Clin, 12:157-177.
Edwards SR, and Mather LE. (2001) Tissue uptake of ketamine and norketamine enantiomers in
the rat: indirect evidence for extrahepatic metabolic inversion. Life Sci, 69:2051-66.
Li Q, Shi L, Lu G, Yu HL, Yeung FK, Wong NK, Sun L, Liu K, Yew D, Pan F, Wang DF and Sham PC.
(2017) Chronic ketamine exposure causes white matter microstructural abnormalities in
adolescent cynomolgus monkeys. Front Neurosci. 11:1-9.
Mensinga TT, Speijers GJ, and Meulenbelt J. (2003) Health implications of exposures to
environmental nitrogenous compounds. Toxicol Rev, 22: 41-51.
Moaddel R, Abdrakhmanova G, Kozak J, Jozwiak K, Toll L, Jimenez L, Rensberg A, Tran T, Xiao Y,
Zarate CA, and Wainer IW. (2013) Subanesthetic concentration of (R,S)-ketamine
metabolites inhibit acetylcholine-evoked currents in ɲ7 nicotinic acetylcholine
receptors. Eur J Pharmacol, 698:228-34.
Newcomer JW, Farber NB and Olney JW. (2000) NMDA receptor function, memory and brain
aging. Dialogues Clin Neurosci, 2:219-232.
Reference ID: 4395937
NDA211243 Shiny V. Mathew, PhD, DABT
69
Sun L, Li Q, Li Q, Zhang Y, Liu D, Jiang H, Pan F and Yew D. (2012) Chronic ketamine exposure
induces permanent impairment of brain functions in adolescent cynomolgus monkeys.
Add Bio, 19:185-194.
Van Dongen AM, editor. Biology of the NMDA receptor. Boca Raton (FL): CRC Press/Taylor &
Francis; 2009.
Yang C, Shirayama Y, Zhang JC, Ren Q, Yao W, Ma M, Dong C and Hashimoto K. (2015) R-
ketamine: a rapid onset and sustained antidepressant without psychomimetic side
effects. Transl Psychiatry, 5:e6321; doi:10.1038/tp.2015.136.
Yeung LY, Wai MS, Fan M, Mak YT Lam WP, Li Z, Lu G, and Yew DT. (2010) Hyperphosphorylated
tau in the brains of mice and monkeys with long term administration of ketamine.
Toxicol Lett. 193:189-193.
Zanos P, Moaddel R, Morris PJ, Georgiou P, Fischell J, Elmer GI, Alkondon M, Yuan P, Pribut HJ,
Singh NS, Dossou KS, Fang Y, Huan XP, Mayo CL, Wainer IW, Albuquerque EX,
Thompson SM, Thomas CJ, Zarate CA Jr, and Gould TD. (2016) NMDAR inhibition-
independent actions of ketamine metabolites. Nature, 533: 481-486.
Zhang J-C, Li Su-x, and Hashimoto, K. (2014) R(-) ketamine shows greater potency and longer
lasting antidepressant effects than S(+)-ketamine. Pharmacol Biochem Behav. 137-141.
Signatures
Shiny V. Mathew, PhD, DABT, Pharmacologist {see appended electronic signature page}
Ikram Elayan, PhD, Supervisory Pharmacologist {see appended electronic signature page}
Reference ID: 4395937
--------------------------------------------------------------------------------------------
This is a representation of an electronic record that was signed
electronically. Following this are manifestations of any and all
electronic signatures for this electronic record.
--------------------------------------------------------------------------------------------
/s/
------------------------------------------------------------
SHINY V MATHEW
02/28/2019 08:57:04 AM
IKRAM M ELAYAN
02/28/2019 10:20:26 AM
Please see the secondary reviewer memo in DARRTS
Signature Page 1 of 1
Reference ID: 4395937
