Coronavirus
Commission on Safety
and Quality in
Nursing Homes
Commission Final Report
September 2020

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
NOTICE
This document was produced for the U. S. Government under Contract Number
75FCMC19F0012, and is subject to Federal Acquisition Regulation Clause 52.227-14, Rights in
Data-General.
No other use other than that granted to the U. S. Government, or to those acting on behalf of the
U. S. Government under that Clause is authorized without the express written permission of The
MITRE Corporation.
For further information, please contact The MITRE Corporation, Contracts Management Office,
7515 Colshire Drive, McLean, VA 22102-7539, (703) 983-6000.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Coronavirus Commission on Safety
and Quality in Nursing Homes
Commission Members
Roya Agahi, RN, MS HCM, WCC
Chief Nursing Officer, CareRite, New York
Lisa M. Brown, PhD, ABPP
Professor of Psychology,
Palo Alto University, California
Mark Burket
CEO, Platte Health Center Avera, South Dakota
Eric M. Carlson, JD
Directing Attorney, Justice in Aging, California
(does not endorse this report)
Michelle Dionne-Vahalik, DNP, RN
Associate Commissioner, State Health and Human
Services Commission, Texas
Debra Fournier, MSB, BSN, RN-BC,
LNHA, CHC, CPHQ
Chief Operations Officer, Veterans’ Homes, Maine
Terry T. Fulmer, PhD, RN, FAAN
President, The John A. Hartford Foundation,
New York
Candace S. Goehring, MN, RN
Director, State Department of Social and Health
Services, Aging and Long-Term Support
Administration, Washington
David C. Grabowski, PhD
Professor of Healthcare Policy, Harvard University,
Massachusetts
Camille Rochelle Jordan, RN, BSN, MSN,
APRN, FNP-C, CDP
Senior Vice President of Clinical Operations &
Innovations, Signature Healthcare, Kentucky
Jessica Kalender-Rich, MD, CMD, AGSF,
FAAHPM, FACP
Medical Director, Post-Acute Care, University of
Kansas Health System, Kansas
Marshall Barry Kapp, JD, MPH
Professor Emeritus of Law, Florida State University,
Florida
Morgan Jane Katz, MD, MHS
Assistant Professor of Medicine, Johns Hopkins
University, Maryland
Beverley L. Laubert, MA
State Long-Term Care Ombudsman, State
Department of Aging, Ohio
Rosie D. Lyles, MD, MHA, MSc, FACA
Director of Clinical Affairs, Medline Industries,
Illinois
Jeannee Parker Martin, MPH, BSN, RN
President and CEO, LeadingAge California
G. Adam Mayle, CHFM, CHC, CHE
Administrative Director of Facilities, Memorial
Healthcare System, Florida
David A. Nace, MD, MPH, CMD
President, AMDA –The Society for Post-Acute and
Long-Term Care Medicine, Pennsylvania
Lori Porter, LNHA, CNA
CEO, National Association of Health Care
Assistants, Missouri
Neil Pruitt, Jr., MBA, MHA, LNHA
Chairman and CEO, PruittHealth, Inc., Georgia
Penelope Ann Shaw, PhD
Nursing Home Resident and Advocate, Braintree
Manor Healthcare, Massachusetts
Lori O. Smetanka, JD
Executive Director, National Consumer Voice for
Quality Long-Term Care, Maryland
Janet Snipes, LNHA
Executive Director, Holly Heights Nursing Home,
Colorado
Patricia W. Stone, PhD, MPH, FAAN, RN,
CIC
Professor of Health Policy in Nursing, Columbia
University, New York
Dallas Taylor, BSN, RN
Director of Nursing, Eliza Bryant Village, Ohio

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
i
Table of Contents
Executive Summary ........................................................................................................ iii
Principal Recommendations ............................................................................................... vii
1 Introduction .................................................................................................... 1
2 Background .................................................................................................... 6
2.1 CMS and State Regulation of Nursing Homes .................................................... 6
2.2 SARS-CoV-2 Exposure, Spread, and Mitigation in Nursing Homes ...................... 8
2.3 COVID-19 and Nursing Home Data .................................................................. 9
2.4 Systemic Problems in Long-Term Care ............................................................ 11
2.5 Guiding Principles in Relation to Safety and Quality of
Nursing Home Residents ................................................................................ 12
3 Themes, Recommendations, Action Steps, and Analysis .................................... 18
3.1 Testing and Screening .................................................................................... 19
3.2 Equipment and PPE ....................................................................................... 24
3.3 Cohorting ..................................................................................................... 28
3.4 Visitation ...................................................................................................... 32
3.5 Communication ............................................................................................. 38
3.6 Workforce Ecosystem: Stopgaps for Resident Safety ........................................ 41
3.7 Workforce Ecosystem: Strategic Reinforcement .............................................. 48
3.8 Technical Assistance and Quality Improvement ............................................... 53
3.9 Facilities ....................................................................................................... 56
3.10 Nursing Home Data ....................................................................................... 60
4 Securing the Future of Long-Term Care ........................................................... 65
4.1 Strategic Workforce Planning ......................................................................... 65
4.2 Interoperable Data, Real-Time Predictive Modeling, and
Communications Technology ......................................................................... 65
4.3 Facility Planning and Renovations ................................................................... 66
4.4 Payment Reform ............................................................................................ 66
4.5 Overall: Resident-Driven Care and Shared Decision-Making ............................. 67
Appendix A: Definition of Acronyms and Terms in Report ...................................... A-1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
ii
Appendix B: Selection of Commission Members .................................................... B-1
Appendix C: Findings and Evidence for Recommendations and Action Steps ........... C-1
Appendix D: List of CMS Actions to Date ............................................................ D-1
Appendix E: Public Input Summary ...................................................................... E-1
Appendix F: Commission Charter ......................................................................... F-1
Appendix G: Commission Memorandum of Short-Term Recommendations –
July 17, 2020 ................................................................................. G-1
Appendix H: Nursing Home COVID-19 Data Limitations ...................................... H-1
Appendix I: Commission Recommendations Overview Presentation –
August 14, 2020 ............................................................................. I-1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
iii
Executive Summary
The global outbreak of the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
constitutes a public health emergency unlike any in living memory. The transmission
characteristics of COVID-19—the disease the virus causes in the human body—result in brisk
community spread. Moreover, the recovery trajectory for those who survive the initial acute
attack of the virus remains to be seen. The scientific community’s understanding of the virus and
development of effective treatments for COVID-19 is nascent.
Nursing homes have emerged as prime hotspots for COVID-19 outbreaks. In the United States,
nursing-home residents and staff represent only 8% of COVID-19 cases, yet bear 41% of
COVID-19 deaths based on data reported August 13.
1
Beyond experiencing the ravages of the
disease itself, residents have been traumatized by the impact of nursing homes restricting visitors
and curtailing group activities in an effort to mitigate spread of this virus. The resulting physical
and mental harm—and increased vulnerabilities—to residents is common knowledge and
troubling. Furthermore, the pandemic’s spread in these institutions has exposed and exacerbated
long-standing, underlying challenges in this care setting. For example, dynamics of the U.S.
federal system—where public health, emergency management, health services, and long-term
care authorities function at federal, state, and local levels—have resulted in a patchwork
approach to infection prevention and control that many believe has contributed to our nation’s
inability to contain the spread of the virus.
Purpose of the Commission and This Report
The Centers for Medicare & Medicaid Services (CMS) tasked MITRE, the operator of the CMS
Alliance to Modernize Healthcare (Health FFRDC), with an urgent assignment: Convene a
commission of experts to address safety and quality in nursing homes in relation to the public
health emergency. The main purpose of the independent Coronavirus Commission on Safety and
Quality in Nursing Homes (Commission) was to solicit lessons learned from the early days of the
pandemic and recommendations for future actions to improve infection prevention and control
measures, safety procedures, and the quality of life of residents within nursing homes. CMS
outlined four objectives for the Commission.
1. Identify best practices
2
for facilities to enable rapid and effective identification and
mitigation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
transmission (and other infectious diseases) in nursing homes.
2. Recommend best practices as exemplars of rigorous infection control practices and
facility resiliency that can serve as a framework for enhanced oversight and quality
monitoring activities.
3. Identify best practices for improved care delivery and responsiveness to the needs of all
nursing home residents in preparation for, during, and following an emergency.
4. Leverage new data sources to improve upon existing infection control policies, and
enable coordinated actions across federal surveyors and contractors (as well as state and
local entities) to mitigate the effects of SARS-CoV-2 and future emergencies.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
iv
Likewise, CMS asked for the Commission to focus its recommendations on actions within
CMS’s authority and that could be undertaken immediately or within the six months following
this report’s delivery. This final report, prepared by MITRE, documents the Commission’s
output.
Organization, Perspectives, and Process
The 25 Commission members hailed from around the country with diverse expertise and
viewpoints ranging from nursing home resident, consumer advocates, and nursing home owners
and administrators to infectious disease experts, academicians, state authorities, and others. The
Commission convened nine times between June 23 and August 19. The Commission used the
four objectives provided by CMS and its collective knowledge of the nursing home system, to
frame its discussions. Analysis of public input solicited via the Commission’s website and
discussion of relevant CMS and other federal actions to date also informed the Commission’s
work. Figure 1 illustrates the Commission process and outputs.
Figure 1. Commission Process and Outputs
The Commission emerged from its convenings with 27 recommendations and accompanying
action steps organized into 10 themes. These themes intersect with the Commission’s four
objectives, and reflect responses to:
• Ongoing supply and affordability dilemmas related to testing, screening, and personal
protective equipment (PPE)
• Tension between rigorous infection control measures and quality of life issues that exist
in cohorting and visitation policies
• A call for transparent and accessible communications with residents, their representatives
and loved ones, and the public
• Urgent need to train, support, protect, and respect direct-care providers

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
v
• Outdated infrastructure of many nursing-home facilities
• Opportunities to create and organize guidance to owners and administrators that is more
actionable and to obtain data from nursing homes that is more meaningful for action and
research
• Insufficient funding for quality nursing home operations, workforce performance, and
resident safety.
Each of the 27 Principal Recommendations are deliberately paired with specific action steps. The
intent is that CMS would implement each principal recommendation in conjunction with its
associated action steps to understand and realize the Commission’s vision.
A Call to Further Action
To reduce suffering and to save the lives of residents and staff, CMS can implement or initiate
the Commission’s actionable recommendations in relatively short order. In some cases, CMS
will need to assume a greater leadership role working with its federal partners and state, local,
tribal and territorial (SLTT) authorities to determine which entity has authority to accomplish the
Commission’s recommendations and action steps. Even so, with the nation’s attention on
COVID-19 in nursing homes and the devastating consequences of leaving long-standing
systemic issues unaddressed, the Commission urges CMS, as the lead federal agency with
nursing home quality and safety oversight, to lead, to advocate, and to ensure accountability for
nursing homes and their residents and staff in the national pandemic response. The time has
come for a turning point in nursing home care. The Commission envisions a person-centered,
resilient system of care that is better for the next generation—one that more deeply values and
respects older adults and people with disabilities as vital to the fabric of American society.
Figure 2 presents this framework.
Figure 2. Commission Recommendation Framework

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
vi
The Commission is confident CMS has the tools and can leverage its influence to make this
vision a reality in partnership with government, academia, the private sector, nursing home
owners, administrators, staff, residents, families, essential care partners, legal surrogates, and
advocates.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
vii
Principal Recommendations
Please navigate to each theme’s analysis (using the provided links) for an overview of relevant
findings and evidence, the specific action steps to implement each recommendation, and
information about the Commission’s endorsement.
#
Theme
Recommendation
1A
Testing and
Screening
Immediately develop and execute a national strategy, coordinating
with federal partners and SLTT authorities, for testing and
delivering rapid turnaround of results (i.e., results in less than 24
hours) in nursing homes, in combination with CDC-recommended
screening protocols. Allow nursing home owners and
administrators to tailor the strategy based on community
prevalence and resource availability in partnership with federal
and SLTT authorities.
[See associated action steps for this recommendation]
2A
Equipment and
PPE
Assume responsibility for a collaborative process with federal and
SLTT partners to ensure nursing home owners and administrators
can procure and sustain a three-month supply of high-quality
supplies of PPE. This process must provide accountability and
oversight.
[See associated action steps for this recommendation]
2B
Equipment and
PPE
Provide specific guidance on the use, decontamination, and reuse
of PPE, working with federal partners, including CDC, FDA, and
OSHA.
[See associated action steps for this recommendation]
2C
Equipment and
PPE
As needed, collaborate with other federal and state agencies to
provide guidance on training to all clinical and nonclinical facility
staff on proper use of PPE and equipment, according to available
manufacturer specifications. (See also recommendation on
Infection Preventionist under Workforce Ecosystem.)
[See associated action steps for this recommendation]
3A Cohorting
Update cohorting guidance to balance resident and staff
psychological safety and well-being with infection prevention and
control.
[See associated action steps for this recommendation]
3B Cohorting
Update cohorting guidance and reimbursement policy to address
differences in nursing home resources (e.g., facility, infrastructure,
staff).
[See associated action steps for this recommendation]

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
viii
#
Theme
Recommendation
4A Visitation
Emphasize that visitation is a vital resident right. Update and
release consolidated, evidence-based guidance on safely
increasing controlled, in-person visitation prior to federal Phase 3
reopening.
[See associated action steps for this recommendation]
4B Visitation
Update and release consolidated, evidence-based guidance on
effectively planning for and implementing virtual visitation tools
and techniques.
[See associated action steps for this recommendation]
4C Visitation
Provide resources to help nursing home staff assess and improve
the mental health and psychosocial well-being of residents during
and after the pandemic.
[See associated action steps for this recommendation]
4D Visitation
Assess, streamline, and increase the accessibility of COVID-19-
related directives, guidance, and resources on visitation into a
single source.
[See associated action steps for this recommendation]
5A Communication
Increase specificity and expand breadth of guidance on
communications between nursing home staff, residents, and
families.
[See associated action steps for this recommendation]
6A
Workforce
Ecosystem:
Stopgaps for
Resident Safety
Mobilize resources to support a fatigued nursing home workforce
and assess minimum care standards.
[See associated action steps for this recommendation]
6B
Workforce
Ecosystem:
Stopgaps for
Resident Safety
Provide equity-oriented guidance that allows nursing home
workforce members to safely continue to work in multiple nursing
homes while adhering to infection prevention and control
practices.
[See associated action steps for this recommendation]
6C
Workforce
Ecosystem:
Stopgaps for
Resident Safety
Support 24/7 RN staffing resources at nursing homes in the event
of a positive SARS-CoV-2 test within that facility.
[See associated action steps for this recommendation]

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
ix
#
Theme
Recommendation
6D
Workforce
Ecosystem:
Stopgaps for
Resident Safety
Identify and immediately leverage certified infection
preventionists to support nursing homes’ infection prevention
needs.
[See associated action steps for this recommendation]
6E
Workforce
Ecosystem:
Stopgaps for
Resident Safety
Require nursing homes to employ infection preventionist(s) with
educator capabilities.
[See associated action steps for this recommendation]
7A
Workforce
System: Strategic
Reinforcement
Catalyze interest in the CNA profession through diverse
recruitment vehicles; issue guidance for on-the-job CNA training,
testing, and certification; and create a national CNA registry.
[See associated action steps for this recommendation]
7B
Workforce
System: Strategic
Reinforcement
Professionalize infection prevention positions in nursing homes by
updating regulations at 42 CFR § 483.80 so more fully qualified
infection preventionists are available to serve in nursing homes.
[See associated action steps for this recommendation]
7C
Workforce
System: Strategic
Reinforcement
Catalyze the overhaul of the workforce ecosystem in partnership
with federal, SLTT, other public, private, and academic partners.
[See associated action steps for this recommendation]
7D
Workforce
System: Strategic
Reinforcement
Convene a Long-Term Care Workforce Commission to assess,
advise on, and provide independent oversight for modernization of
workforce ecosystem.
3
[See associated action step for this recommendation]
8A
Technical
Assistance and
Quality
Improvement
Identify and work to achieve funding mechanisms for—or
reprioritize activities of—technical assistance providers and other
contractors to increase the availability of collaborative, on-site,
data-driven, and outcomes-oriented support prior to, during, and
after a public health emergency.
[See associated action steps for this recommendation]
9A Facilities
Identify and share with nursing homes short-term facility design
enhancements to address immediate pandemic-related risks that
can be implemented at minimal cost.
[See associated action steps for this recommendation]

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
x
#
Theme
Recommendation
9B Facilities
Establish a collaborative national forum to identify and share best
practices and recommendations; facilitate real-time learning on
how to best use existing physical spaces. (Please refer to action
steps following 9C.)
[See associated action steps for this recommendation]
9C Facilities
Collaboratively establish long-term priorities and seek appropriate
funding streams for nursing homes to redesign and/or strengthen
facilities against infectious diseases.
[See associated action steps for this recommendation]
10A
Nursing Home
Data
Standardize COVID-19 data elements, improve data collection,
and identify supportive actions that CMS and federal partners will
take in response to key COVID-19 indicators based on nursing
home-reported data.
[See associated action steps for this recommendation]
10B
Nursing Home
Data
Create an easy-to-use, intuitive, and interactive technical
infrastructure for nursing homes that streamlines the process of
data reporting and consolidates dissemination of essential policy
guidance, information about updated regulations, and other
communications.
[See associated action steps for this recommendation]
10C
Nursing Home
Data
Enhance HIT interoperability to facilitate better communication,
improve quality measurement standards, and coordinate
integration of nursing home data with data from other health
organizations.
[See associated action steps for this recommendation]
1
Conten, M., et. al. (2020, August 13). More Than 40% of U.S. Coronavirus Deaths Are Linked to Nursing Homes.
The New York Times. https://nyti.ms/31mkr1B
.
2
Given the novel nature of the virus and rapidly evolving state of understanding of the virus, the Commission was in
the realm of “emerging evidence” and “emerging practices” with respect to some areas discussed.
3
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
1
1 Introduction
As the novel coronavirus 2019 (COVID-19) pandemic swept the globe in 2020, the Centers for
Medicare & Medicaid Services (CMS) tasked MITRE, the operator of the CMS Alliance to
Modernize Healthcare (Health FFRDC), with an urgent assignment: Convene an independent
commission of experts to address safety and quality in nursing homes in relation to the public
health emergency.
4, 5
The main purpose of the independent Coronavirus Commission on Safety
and Quality in Nursing Homes (Commission) was to solicit lessons learned from the early days
of the pandemic and recommendations for future actions to improve infection prevention and
control measures, safety procedures, and the quality of life of residents within nursing homes.
6
CMS outlined four objectives for the Commission:
1. Identify best practices
7
for facilities to enable rapid and effective identification and
mitigation of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2)
transmission (and other infectious diseases) in nursing homes.
2. Recommend best practices as exemplars of rigorous infection control practices and
facility resiliency that can serve as a framework for enhanced oversight and quality
monitoring activities.
3. Identify best practices for improved care delivery and responsiveness to the needs of all
nursing home residents in preparation for, during, and following an emergency.
4. Leverage new data sources to improve upon existing infection control policies, and
enable coordinated actions across federal surveyors and contractors (as well as state and
local entities) to mitigate the effects of SARS-CoV-2 and future emergencies.
Commission Membership. On May 14, MITRE announced an open call for Commission
nominations. MITRE selected 25 Commission members from a pool of more than 800
nominations and through a rigorous selection process. (The selection process is summarized in
Appendix B in this report.) The Commission members hailed from around the country with
diverse expertise and viewpoints ranging from nursing home resident, consumer advocates, and
nursing home owners and administrators to infectious disease experts, academicians, state
authorities, and others. CMS provided technical input to MITRE during the selection process.
Commission membership was announced by MITRE and CMS on June 19.
8
Timely convening
was critical to enable CMS to leverage insights from the Commission as quickly as possible for
the benefit of nursing home residents and staff.
Commission Convenings. The Commission met almost weekly between June 23 and August 7;
they discussed the CMS objectives, the long-standing problems faced by nursing homes that
were exacerbated by the pandemic, and recommendations to the agency and its federal partners
to support residents and families as well as owners and administrators as they continue
combating the pandemic on behalf of their residents and workforce. At CMS’s request, the
Commission sought to focus its recommendations on actions within CMS’s authority and that
could be undertaken in the short term, defined for this purpose as immediately or within the six
months following this report’s delivery (i.e., between September 1, 2020, and March 1, 2021).
The Commission discussed immediate system stabilization actions for improving infection

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
2
control, safety, and quality of life, as well as system-recovery pursuits leading to sustainable
improvement over time.
CMS Role. CMS leaders and staff joined the Commission’s meetings as guest speakers and
invited guests during full-group discussions. CMS provided technical input to this report as
further described in this section.
MITRE and Health FFRDC Roles. MITRE and two of its Health FFRDC Alliance partners, Atlas
Research and Ripple Effect, filled several roles supporting the Commission.
• Dr. Jay Schnitzer, MITRE’s chief medical officer, served as the Commission’s
moderator; Ms. Meg Kabat, Atlas senior director, served as the facilitator. All three
organizations provided planning, research, and technical support.
• MITRE maintained communications with Commission members and the public through
the Commission website and email account.
• On behalf of the Commission, MITRE sought public input to align with the four
Commission objectives, and to allow the public to formally note their support of nursing
home residents and staff.
9
Atlas Research and MITRE analyzed and presented to the
Commission and CMS the public input submissions received.
• MITRE prepared each of the three major deliverables presenting the interim, preliminary,
and final recommendations of the Commission.
Public Input. The Commission received 632 responses from a multitude of stakeholders through
its website-based feedback form announced publicly by press release. These responses took the
form of checkbox indications of interest in the well-being of nursing home residents and staff;
500-character open-ended comments wherein contributors provided their perspective as it
aligned to one of the four Commission objectives; and attachments up to five pages long (e.g.,
formal letters, publications, or other resources). Commission members had the opportunity to
review these public inputs, categorized first by objectives and broken down into discussion
themes, in a detailed summary report. This summary was later synthesized into a formal briefing
to guide the second half of the Commission’s convening schedule. These public inputs urged
coordinated federal action to support the enhanced operation of nursing homes; called for the re-
prioritization of resident and staff quality of life and safety; and demanded transparent
communications and the re-engagement of essential care partners. The Commission used these
public inputs to refine their development of actionable recommendations, and to drive the
identification of additional relevant actions CMS and its federal partners should take to improve
the ongoing COVID-19 response and support of nursing homes. (An analysis of this public input
appears in Appendix E in this report.)
Final Report and Other Deliverables. This final report is based on the Commission’s discussions
and recommendations; analysis of public inputs; MITRE’s analysis and clarification of the
foregoing; and CMS’s actions to date. MITRE completed most of its research in support of the
report as of August 11, in advance of delivering preliminary draft recommendations and action
steps to CMS on August 14, noting areas still under Commission discussion. (See Appendix I.)
Text and/or endnotes throughout this report reflect where more-recent research or updated

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
3
information resulted from input from Commission members or CMS. MITRE notes that CMS
and other federal agencies have varied authorities that they have been exercising in a rapidly
evolving legislative environment. CMS must work with its federal partners to determine which
agency has authority to implement the Commission’s recommendations and action steps.
As MITRE prepared this report, both Commission members and CMS experts had the
opportunity to review it in draft form. Commission members were able to comment on any
aspect of the report. CMS experts provided technical input by providing comments to MITRE on
the following: 1) items that were demonstrated to be factually incorrect or reflect incorrect data,
or were objectively wrong based on data and evidence, 2) incomplete or incorrect description of
CMS actions, 3) unclear, missing, or incorrect reference to a regulatory provision, 4) incorrect
reference to CMS authority, and 5) identification of federal and SLTT government partners
necessary to CMS’s implementation of a recommendation or action step.
In addition to this report, as the Commission’s work progressed, CMS Administrator Seema
Verma requested that the Commission develop and provide a set of interim, short-term
recommendations to inform CMS’s immediate and continuing response to the pandemic. The
Commission focused its July 14 convening specifically on this request, and MITRE delivered
those short-term recommendations, endorsed by nearly all Commission members, to CMS on
July 17. (The text of this memorandum appears as Appendix G in this report.) CMS noted that
some of these interim recommendations reinforced actions CMS already had underway, and that
others provided impetus to explore new actions. CMS and its federal partners continued to act as
this final report was being prepared.
10, 11, 12
Commission Endorsement Matrix
Thirteen members of the Commission endorse this report in full:
• Roya Agahi
• Lisa M. Brown
• Debra Fournier
• Terry T. Fulmer
• Candace S. Goehring
• David C. Grabowski
• Jessica Kalender-Rich
• Marshall Barry Kapp
• Morgan Jane Katz
• Rosie D. Lyles
• G. Adam Mayle
• David A. Nace
• Patricia W. Stone
One member—Eric M. Carlson—does not endorse this report.
Eleven members of the Commission endorse this report with the reservations included on the
following table.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
4
Commission Member
Reservations about some specifics for the
following theme(s)
Mark Burket
Workforce Ecosystem – Stopgaps for Resident Safety
Michelle Dionne-Vahalik
General reservation (wished for more recommendations
framed as “requirements” for nursing home owners and
administrators, rather than as “guidance”)
Camille Rochelle Jordan
Workforce Ecosystem – Stopgaps for Resident Safety
Beverley L. Laubert
Testing and Screening
Cohorting
Workforce Ecosystem – Stopgaps for Resident Safety
Jeannee Parker Martin
Visitation
Workforce Ecosystem – Stopgaps for Resident Safety
Lori Porter
Workforce Ecosystem – Stopgaps for Resident Safety
Workforce Ecosystem – Strategic Reinforcement
Neil Pruitt, Jr.
Workforce Ecosystem – Stopgaps for Resident Safety
Penelope Ann Shaw
General reservation (opposed to any infringement on resident
rights; wished for more accountability for providers to meet
standards and to be good stewards of federal dollars)
Lori O. Smetanka
General reservation (wished for more accountability for
providers to meet standards and to be good stewards of
federal dollars)
Workforce Ecosystem – Stopgaps for Resident Safety
Workforce Ecosystem – Strategic Reinforcement
Technical Assistance and Quality Improvement
Janet Snipes
Workforce Ecosystem – Stopgaps for Resident Safety
Dallas Taylor
Workforce Ecosystem – Stopgaps for Resident Safety
4
World Health Organization. (n.d.). Naming the coronavirus disease (COVID-19) and the virus that causes it.
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-
disease-(covid-2019)-and-the-virus-that-causes-it
5
Centers for Medicare & Medicaid Services. (2020, April 30). CMS announces independent commission to address
safety and quality in nursing homes [Press release].
https://www.cms.gov/newsroom/press-releases/cms-announces-
independent-commission-address-safety-and-quality-nursing-homes
6
For this report and the Commission’s work, the term “nursing homes” includes facilities under the purview of CMS,
specifically skilled nursing facilities (SNF) that participate in the Medicare program and nursing facilities that
participate in the Medicaid program. Many facilities have SNF and Medicaid beds alike. The Commission’s focus did
not include nursing facilities under the purview of the Veterans Health Administration.
7
Given the novel nature of the virus and rapidly evolving state of understanding of the virus, the Commission was in
the realm of “emerging evidence” and “emerging practices” with respect to some areas discussed.
8
Centers for Medicare & Medicaid Services. (2020, June 19). CMS announces membership of independent
coronavirus commission on safety and quality in nursing homes [Press release].

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
5
https://www.cms.gov/newsroom/press-releases/cms-announces-membership-independent-coronavirus-commission-
safety-and-quality-nursing-homes
9
MITRE. (2020, July 10). Independent coronavirus commission for safety and quality in nursing homes launches
additional public input option [Press release].
https://www.mitre.org/news/press-releases/independent-coronavirus-
commission-for-safety-and-quality-in-nursing-homes
10
Centers for Medicare & Medicaid Services. (2020, Aug. 25). Trump Administration Strengthens COVID-19
Surveillance with New Reporting and Testing Requirements for Nursing Homes, Other Providers [Press release].
https://www.cms.gov/newsroom/press-releases/trump-administration-strengthens-covid-19-surveillance-new-
reporting-and-testing-requirements
11
Centers for Medicare & Medicaid Services. (2020, Aug. 26). CMS posts guidance for implementing new testing
requirements in nursing homes and labs [Press release]. https://www.cms.gov/newsroom/press-releases/cms-posts-
guidance-implementing-new-testing-requirements-nursing-homes-and-labs
12
Food and Drug Administration. (2020, Aug. 26). COVID-19 Update: FDA Authorizes First Diagnostic Test Where
Results Can Be Read Directly From Testing Card [Press release].
https://www.fda.gov/news-events/press-
announcements/covid-19-update-fda-authorizes-first-diagnostic-test-where-results-can-be-read-directly-testing-card

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
6
2 Background
2.1 CMS and State Regulation of Nursing Homes
The United States has more than 15,000 nursing homes that care for approximately 1.2 million
residents.
13
Annual spending in 2018 on nursing homes
14
was approximately $170 billion, with
Medicare spending approximately $38 billion and Medicaid spending approximately $50
billion.
15
Nursing homes provide skilled nursing care and related services for residents who
require medical or nursing care and rehabilitation services for people with injuries, disabilities,
and illnesses.
16
For this report and the Commission’s work, the term “nursing homes” includes
facilities certified to participate under the Medicare and Medicaid programs, specifically skilled
nursing facilities (SNF)
17
that participate in Medicare and nursing facilities (NF)
18
that
participate in Medicaid only, but not assisted living facilities. Although some may use the terms
“skilled nursing facility” and “nursing facility” interchangeably (along with “long-term care
facility”), and some facilities are certified/participate as both NFs and SNFs,
19
clinical and
coverage differences exist between the two.
20, 21
Nursing homes span in size and organizational
structure from small, single-facility nonprofits to facilities that are part of regional or national
chains to nursing homes that are integrated into their local or regional health system. Nursing
homes are additionally subject to state regulation, as further discussed in this section. The
Commission focused on CMS actions, which includes actions that could affect both SNFs and
NFs; state actions were beyond its scope.
Since nursing homes are subject to both state and federal authorities, they must navigate a
patchwork of regulations and guidance. Federal statutory authority for CMS oversight of long-
term care facilities and requirements for participation reside in sections 1819 and 1919 of the
Social Security Act (the Act) for Medicare- and Medicaid-participating nursing homes,
respectively.
22
These authorities work in tandem to ensure the safety and quality of care; provide
a comprehensive plan of care, training, licensure, and competency of staff; and protect residents’
rights, such as freedom of choice and freedom from restraints, in Medicare- and/or Medicaid-
participating facilities. These sections also permit the Department of Health and Human Services
(HHS) to establish any additional requirements relating to the health, safety, and well-being of
SNFs and NFs as its Secretary finds necessary. CMS has the authority to penalize facilities that
are in violation of these requirements. Although state nursing home regulations vary, and some
states may establish more stringent requirements than those imposed nationally, CMS’s role as a
national regulator places it in an important position to ensure safety and quality in nursing home
care around the country.
In addition to federal laws and regulations, each state adopts its own legislative requirements for
the operations, governance, and quality assurance in nursing homes and assisted living facilities
alike.
23
States have the authority to license healthcare practitioners and facilities.
24
States may
also have separate laws and regulations governing all nursing homes in the state (i.e., not just
those participating in Medicare and Medicaid) that may exceed federal requirements, including
state enforcement actions.
25
State surveys/site visits serve a key monitoring function in the
nursing home ecosystem.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
7
To prepare for public health emergencies, CMS has acted to ensure that Medicare and Medicaid
providers and suppliers of all types adhere to certain emergency preparedness requirements. For
example, CMS issued a final rule outlining a “comprehensive, consistent, flexible, and dynamic
regulatory approach to emergency preparedness and response”
26
for a wide variety of healthcare
providers and suppliers that participate in Medicare and Medicaid, including nursing homes.
That final rule specified emergency-preparedness requirements for long-term care facilities,
which it codified at 42 CFR § 483.73 (Emergency Preparedness regulation). These regulations
generally align with those emergency preparedness requirements that CMS has adopted for
hospitals, with an additional requirement for long-term care facilities to track the locations of
residents and staff during and after emergencies. These requirements ensure that long-term care
facilities develop and implement emergency-preparedness policies and procedures on topics such
as providing sufficient food, water, medical, and pharmaceutical supplies for staff and resident
during an emergency; communication plans with contact information for staff, vendors,
residents’ physicians, other facilities, and volunteers; and training and testing programs provided
at least annually. Other requirements ensure that facilities implement emergency and standby
power systems and allow facilities that are part of integrated healthcare systems to participate in
unified and integrated emergency-preparedness policies developed by their healthcare systems.
Long-term care facilities must establish and maintain these plans in order to participate in the
Medicare and Medicaid programs. CMS works closely with state surveyors to enforce these
regulations and to ensure that long-term care facilities maintain appropriate emergency-
preparedness plans.
The interaction of federal and state authorities within the Medicaid program often involve
requests for Medicaid waivers under section 1915, 1932, and 1115 of the Act. Medicaid State
Plan Amendments also provide important state-driven activities subject to federal approval.
These authorities are intended to allow flexibility in the delivery of Medicaid benefits at the state
level, including changes to eligibility, delivery system (managed care), benefits, and value-based
payments beyond what is normally permitted (or for costs not otherwise matchable) under the
Medicaid statute.
27
In relation to public health emergencies, the Secretary is authorized under section 1135 of the
Act to temporarily waive or modify Medicare, Medicaid, and Children’s Health Insurance
Program (CHIP) requirements to meet the needs of a natural disaster or public health
emergency.
28
Ordinarily, providers in each state are responsible for submitting a formal request
in writing to a dedicated inbox, and for notifying their CMS Location of the pending request;
CMS may also implement specific waivers or modifications under the 1135 authority on a
“blanket” basis, upon a determination that all similarly situated providers in the emergency area
need such a waiver or modification.
29
On March 13, CMS announced that in addition to reviewing specific provider requests for 1135
waivers, it would activate blanket waivers nationwide to ease requirements for providers
impacted by the COVID-19 national emergency.
30
CMS announced the blanket waivers were to
take effect retroactively from March 1 through the end of the emergency declaration. Although
Section 1135 blanket waivers apply to a broad spectrum of providers, CMS enacted blanket
waivers specifically for nursing homes, including but not limited to waiver of Pre-Admission
Screening and Annual Resident Review; waiver of residents’ rights to participate in person in

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
8
resident group activities; modification to the nurse aide training requirements; waiver of
discharge planning requirements, and modifications to the scope of Quality Assurance and
Performance Improvement (QAPI) reporting requirements.
31
As of August 19, CMS has also
approved 118 state-specific requests (with several states having multiple approved requests) for
1135 waivers for various flexibilities to ease challenges with healthcare delivery for providers
during the pandemic.
32
Generally, these state waiver approvals are retroactively effective to
March 1, and will terminate upon termination of the public health emergency.
33
2.2 SARS-CoV-2 Exposure, Spread, and Mitigation in Nursing Homes
According to the Centers for Disease Control and Prevention (CDC), the risk for severe illness
from SARS-CoV-2 infection increases with age; adults aged 85 or older are at highest risk.
34
Additionally, people with some underlying medical conditions (e.g., cancer, chronic kidney
disease, chronic obstructive pulmonary disease, immunocompromised state, obesity, serious
heart conditions, sickle cell disease, or Type 2 diabetes mellitus) face increased risk of severe
illness when infected with the virus.
35
These risks are heightened by the congregate nature and
relatively frequent infections among residents in long-term care facilities, estimated between 1
and 3 million serious infections per year in nursing homes, SNFs, and assisted living facilities.
36,
37
The virus’s disproportionate effect on nursing home resident and staff populations is due in part
to the way that the virus spreads. Similar to other human coronaviruses and respiratory viruses,
SARS-CoV-2 appears to transmit between humans through expulsion of respiratory droplets
from an infected individual.
38
Talking, coughing, singing, exercising, and other activities can
cause respiratory droplets with viral particles to be shed into the immediate proximity of the
infected person.
39, 40, 41
The most effective way to prevent the spread of the virus is to limit the
frequency and duration of close physical contact between an infected individual and an
uninfected individual.
42
As a result, effective methods to reduce this spread include physical
distancing at a community level and physical separation within nursing homes to limit contact
among individuals.
43
This strategy, however, is problematic in care facilities where vulnerable
people are kept in close quarters—and are not only permitted, but also encouraged, to socially
interact with one another. When physical distancing is not entirely possible, cohorting presents
another mitigation strategy.
44, 45
Cohorting is the process of locating individuals with the same
condition in the same space, with the intent of reducing or eliminating interaction between
infected persons with uninfected persons.
46
Cohorting could help reduce the spread of the virus;
it has shown to be effective both historically and during recent infectious outbreaks.
47
As discussed in this report, however, cohorting is often problematic for residents’ social and
emotional health. Preventing the spread of this virus through physical distancing may lead to
unintended consequences for residents. For example, limiting potential exposure to the virus
through physical isolation has left family members, legal surrogates, and others unable to
observe the status of residents due to restrictive visitation policies. Public input submitted to the
Commission expressed fears about, and examples of, abuse and neglect—and missed
opportunities to identify or intervene. State survey data in the period leading up to the pandemic
showed that “most facilities (80%) received a deficiency related to resident quality of life or care,
and 37% received an abuse/neglect/exploitation deficiency.”
48
Visitation restrictions

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
9
implemented for infection control have elevated
demand on state ombudsman programs and placed
attention on the reduced scale and scope of state
inspection and survey activity during this time.
49, 50
As discussed in this report, assisting nursing homes,
residents, and families to find an avenue for safe
visitation is a high priority that is contingent on the
availability of rapid testing and results and PPE for
visitors.
2.3 COVID-19 and Nursing Home Data
Since SARS-CoV-2 was first detected in Washington
State on January 20,
51
nursing homes have endured high rates of infection, and related morbidity
and mortality among residents.
52
As of August 9, almost 12,000 facilities nationwide have
reported COVID-19 disease cases among their residents and staff—including 188,954 resident
cases—which have led to more than 48,215 COVID-19 related deaths among residents. The
virus has affected nursing homes disproportionately: reported data through August 13 show that
8% of COVID-19 cases and 41% of COVID-19 deaths in the United States have occurred among
residents and staff.
53
CMS and other federal and SLTT agencies have taken steps to address this crisis. For example,
CMS released a series of guidelines targeted at reducing the impact of COVID-19 on nursing
homes and other long-term care facilities, including guidance related to visitor restrictions,
infection control guidelines, and designating separate facilities for COVID-positive residents and
COVID-negative residents. (See Appendix D for a list of CMS actions taken to date.)
Additionally, on April 19, CMS announced new reporting requirements requiring nursing homes
to report cases of COVID-19 directly to the CDC.
54
Figure 1 shows the location of nursing homes with identified COVID-19 resident cases.
55
As of August 13,
8% of all U.S.
COVID-19 disease
cases and 41% of
all U.S. COVID-19
disease deaths
are linked to
nursing homes.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
10
Figure 1:Nursing Home COVID-19 Resident Confirmed Cases Heat Map developed from CMS Nursing Home
COVID-19 Public File, Submitted Data as of Week Ending 8/9/2020
A variety of data sources are available to describe and assess the impact of COVID-19 on
nursing homes. At the federal level, CMS and CDC use the National Healthcare Safety Network
(NHSN) to collect standardized COVID-19 data from owners and administrators across the
county. CMS finalized new reporting requirements to collect this data starting in May.
56
Because
reporting COVID-19 cases and deaths prior to this time was optional, counts from January 1
through May 24 are likely to be inconsistent across states. Nevertheless, this approach
established a central repository for ongoing collection of data about facility characteristics,
occupied beds, number of residents and staff with suspected and confirmed COVID-19, number
of residents and staff deaths due to COVID-19, staff shortages, supply of PPE, and other details.
At the state level, the scope and availability of nursing home data related to COVID-19 is varied
and often not directly comparable to the federal data.
57
Some states made detailed data on cases
and deaths publicly available early on; others did not.
58
Various entities have also summarized or
analyzed state-level data on nursing homes (or long-term care facilities), such as AARP,
59
the
Kaiser Family Foundation,
60
and the New York Times.
61
Although the variability in these data is challenging, it is nonetheless important to consider how
to best use the available state data, in conjunction with the federal data, to gain the greatest
insights. Each data source must be evaluated individually to understand how the individual
elements derived from that source are defined; for example, CMS provided a data dictionary for
the Nursing Home COVID-19 Public Use File (PUF) based on the NHSN data that describes
each of the variables in the dataset.
62
A rapid consultation guide created by the National
Academies of Sciences, Engineering, and Medicine Societal Experts Action Network (NASEM
SEAN) that summarizes benefits and drawbacks of selected measurements is an example of

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
11
efforts to develop standard guidance in this area.
63
Appendix H provides additional information
about data limitations related to nursing homes.
2.4 Systemic Problems in Long-Term Care
Several long-term, systemic problems underline the difficulties of preventing and treating
COVID-19 in nursing homes. In exchanges about current and future responses to COVID-19
(and future infectious disease outbreaks), Commission members discussed at length the systemic
issues exacerbated by the pandemic. Prior reports have documented these issues; chief among
these challenges are related to financing, fiscal accountability, facility design, workforce,
governance/management, technology, data, and research.
64
Short-term solutions cannot be found
in isolation from the pressing need for systemic improvements in the long-term care sector; these
long-standing systemic issues thus became the lens through which the Commission approached
its work.
Delivery Systems
In its 2013 Report to Congress, the Commission on Long-Term Care (2013 Commission)
described fragmented care delivery models for individuals in nursing homes, with little
coordination between care settings.
65
The needs of individuals and families are subordinated to
the systems in which those individuals and families engage. Funding streams and setting
specifications (e.g., SNF, rehabilitation, long-term care) may encumber person-centered and
person-driven care, and can deprioritize residents’ individual choices.
In addition, owners and administrators are paid under several different systems (i.e., private and
public; and federal, state, and local governments). These fragmented funding streams, featuring
widely varying rates and myriad regulations, further exacerbate the currently fragmented
delivery system. Thus, even experts in nursing homes experience difficulty when striving to
understand which payer is responsible for which services and solutions.
Workforce and Other Limited Resources
The 2013 Commission emphasized a recurring issue in most discussions of nursing homes:
Homes are hampered by too few staff, who are paid too little for physically and emotionally
taxing work. Additionally, little room exists for these professionals to advance in their careers,
and they suffer from a lack of meaningful benefits.
66
As a result, challenges in workforce
recruitment and retention are compounded year-over-year, as workforce shortages persist with
the older population increasing. Without qualified staff, nursing homes find it difficult to meet
residents’ regular needs—let alone those that arise in times of crisis.
Along with shortages in the workforce, some nursing home owners and administrators are
limited in the resources at their disposal—hampering responses to emergencies regardless of
whether they are natural disasters or infectious disease outbreaks. When crises arise, owners and
administrators frequently do not have necessary training, equipment, or staff to respond. Often,
nursing homes may be deemed lower-priority facilities for assistance from government sources
in comparison to acute care settings.
67
As a result, emergencies stress an already precarious care
system.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
12
In the Wake of a Pandemic, Balancing Resident and Staff Safety and Well-Being
These systemic issues have become especially pointed during the COVID-19 pandemic.
Rigorous infection-control practice and treatment needs require that residents that test positive
for COVID-19 may need to be transferred to new locations within their nursing home, to other
sites, and in and out of hospitals. In the early days of the pandemic, transitions at times were
abrupt, and the resident and family had no prior awareness that such a transition might occur.
68
In the future, when a nursing home contends with a widespread outbreak, rapid transitions may
still be indicated.
69
When transitions are not well-communicated, the result may be that care is
not coordinated or handoffs are missed. The resident and family suffer from the trauma that
relocation and/or isolation may cause—from the possible decline in care quality, as well as from
missed opportunities for resident-centered shared decision-making.
Furthermore, different funding streams and oversight authorities complicate matters for owners
and administrators trying to understand to whom they should go for additional help. Well-
intentioned incentives may inadvertently create unintended consequences, such as care
paradigms that are not person-centered or person-driven. Because reimbursement rates are higher
for placing residents with COVID-19 in a room alone (as compared to placing residents with a
COVID-19 positive group), nursing homes administrators may be more likely to isolate residents
prematurely, contrary to resident-expressed desires to remain with other residents with the same
infection status. During an outbreak, there may be insufficient time and funding for additional
staff training on COVID-19 and other infectious-disease protocols. And, with limited staff
available on a day-to-day basis, surge support often is unavailable to nursing homes in times of
crisis. Staff members, already stretched thin, become more taxed while working on the front
lines of the crisis—and subjecting themselves and their families to increased risk of contracting
the disease. Nursing home staff have been asked to deploy themselves and their limited resources
in new ways and with Herculean effort—a scenario likely to exacerbate turnover and staff
shortages in the long term.
The Commission members offered expertise as seen through these lenses of systemic challenges
in delivery, workforce, and resources; these fundamental and long-standing challenges informed
their recommendations and lessons learned. As one Commission member pointed out, “Nursing
homes were not designed with infectious disease control in mind.” Many members noted that
stopping the spread of infectious diseases in nursing homes cannot be accomplished without
immediately addressing these long-standing issues.
2.5 Guiding Principles in Relation to Safety and Quality of
Nursing Home Residents
These long-standing, systemic issues informed not only the development of the Commission’s
recommendations, but also shaped guiding principles for their implementation. Commission
members were aligned in their belief that CMS would be most effective in implementation of the
recommendations and associated action steps if guided by two overarching principles: elevating
person-centered and person-driven care; and increasing organizational capacity to improve safety
and quality.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
13
Elevating Person-Centered and Person-Driven Care
Despite regulatory recognition of person-centeredness, resident goals, values, and needs often are
treated as important—but not central—considerations.
70
Elevating person-centered care requires
that care providers first ask what is best for the resident, and ensures they are active participants
in decision-making about their care. Where residents are unable to actively participate in these
decision-making processes, and/or when they would like additional support, legal surrogates
should likewise be assured of an equal place on the care team. These considerations remain of
paramount importance, even during a pandemic and when planning for future emergencies.
Further, person-driven care means empowering residents to take the lead in decision-making
about their care, and to identify their desired health outcomes. As nursing home administrators
implement policies impacting residents, they should do so in consultation with the resident and,
ideally, driven by the resident (or their legal surrogate in situations when residents are unable to
drive these decisions). Given that the nursing home is many residents’ home—not a temporary
care setting—their inclusion, at least on a representative level, in emergency plan creation, and
their engagement at an individual level during implementation is pragmatic and reasonable. As
owners and administrators consider how to best implement rigorous infection prevention and
control practices within their facilities in the months to come, they must empower residents as
partners in finding person-centered solutions that ensure connections with their essential care
partners, legal surrogates, families, and advocates.
Increasing Organizational Capacity to Improve Safety and Quality
During the pandemic and everyday, nursing home staff are responsible for the care and
protection of some of the most vulnerable populations in the nation. The safety and quality of life
needs of residents are complex and diverse, and require mindful decision-making and effective
processes in order to be met.
Mindful decision-making is only possible when the workforce feels safe, prepared, and respected
for the meaningful work they do. They need to work in facilities compliant with Occupational
Safety and Health Administration (OSHA) regulations; they need timely access to the right
training, equipment, and technology; and they need to be compensated at a level commensurate
with the intensity of the care they provide. These needs must be accompanied by a multi-faceted
financing approach that involves securing and distributing federal emergency funding relief and
longer-term appropriations, reforming Medicaid and Medicare reimbursement rates, and
allocating wage pass-throughs.
Employing effective processes requires that oversight bodies at federal and SLTT levels deliver
clear, concise, timely, transparent, and evidence-based guidance and instruction for compliance,
as well as streamline reporting requirements. Moreover, nursing home owners and
administrators, along with their oversight bodies, share responsibility for ensuring that required
processes for operation are implemented and continuously improved as new learnings emerge
about the pandemic.
As such, CMS actions in response to the pandemic should have the intention of increasing
organizational capacity so that nursing home staff fulfill their responsibilities related to the care
and protection of residents. Increasing organizational capacity can involve both effective

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
14
oversight and enforcement but also leveraging the resources and insights gleaned from a national
level perspective of the pandemic and disseminating them to others at the ground level.
Other Principles at Play – Providing Funding and Ensuring Accountability
The Commission discussed other principles, as reflected directly in some of the
recommendations and associated actions. Some members voiced strongly that CMS should make
no unfunded mandates: if CMS implements the recommendations and actions steps in this report,
it must do so in a way that ensures funding mechanisms are in place to support them.
Other members stressed the criticality of CMS and its federal partners in ensuring accountability
and appropriateness for how emergency and other funds are spent, now and in the future, by
owners and administrators. These members underscored CMS’s oversight and enforcement role
and voiced concerns if CMS implemented recommendations without plans in place to monitor
and ensure funds were applied for their intended purpose.
13
Kaiser Family Foundation analysis of 2019 Certification and Survey Provider Enhanced Reports (CASPER) data.
https://www.kff.org/state-category/providers-service-use/nursing-facilities/
Centers for Disease Control and Prevention. (2019). Nursing home care.
https://www.cdc.gov/nchs/fastats/nursing-home-care.htm
; Not forgotten: Protecting Americans from abuse and
neglect in nursing homes: Hearings before the Senate Committee on Finance, 116
th
Cong. (2019) (testimony of David
C. Grabowski).
https://www.finance.senate.gov/imo/media/doc/Grabowski%20Senate%20Finance%20testimony%20FINAL.pdf;
Homeland Infrastructure Foundation-Level Data- Public Health. (2020). Nursing homes [Map]. https://hifld-
geoplatform.opendata.arcgis.com/
14
In this instance, nursing homes refers to nursing homes and continuing care requirement communities alike, as is
the case with the CDC data from which the datapoint is drawn.
15
Centers for Medicare & Medicaid Services. (2019, November 26). National health expenditures data [Data set].
https://www.cms.gov/files/zip/national-health-expenditures-type-service-and-source-funds-cy-1960-2018.zip
. See also
Grabowski cited at note 3.
16
Nursing Homes. (n.d.). in Nursing Home Compare Glossary.
https://www.medicare.gov/NursingHomeCompare/Resources/Glossary.html
17
Section 1819(a) of the Social Security Act [42 U.S.C. 1395i-3(a)] defines skilled nursing facilities (SNFs) as “…an
institution (or distinct part of an institution) which (1) is primarily engaged in providing to residents (A) skilled nursing
care and related services for residents who require medical or nursing care, or (B) rehabilitation services for the
rehabilitation of injured, disabled, or sick persons, and is not primarily for the care and treatment of mental disease;
has in effect a transfer agreement…”; and meets other SNF requirements described therein.
18
Section 1919(a) of the Social Security Act [42 U.S.C. 1396r(a)] defines nursing facilities as ” “…an institution (or a
distinct part of an institution) which (1) is primarily engaged in providing residents (A) skilled nursing care and related
services for residents who require medical or nursing care, (B) rehabilitation services for the rehabilitation of injured,
disabled, or sick persons, or (C) on a regular basis, health-related care and services to individuals who because of
their mental or physical condition require care and services (above the level of room and board) which can be made
available to them only through institutional facilities, and is not primarily for the care and treatment of mental
diseases; (2) has in effect a transfer agreement…with one or more hospitals…” and (3) meets other NF requirements
described therein.
19
Most SNFs (more than 90 percent) are dually certified as SNFs and nursing homes. Medicare Payment Advisory
Commission. (2020). Chapter 8, skilled nursing facility services (Report to the Congress: Medicare Payment Policy).
http://www.medpac.gov/docs/default-source/reports/mar20_medpac_ch8_sec.pdf?sfvrsn=0
20
SNFs provide short-term skilled nursing or rehabilitation care after an individual is discharged from the hospital,
also known as post-acute care. Medicare covers skilled nursing care in a SNF for up to 100 days per spell of illness,
after a medically necessary inpatient hospital stay of at least three days. (A spell of illness begins with the first day of

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
15
a hospital or SNF stay and ends when there has been 60 consecutive days during which an individual was not in a
hospital or a SNF). For beneficiaries who qualify for a covered stay, Medicare pays 100 percent of the payment for
the first 20 days of the spell of illness. Beginning with day 21, beneficiaries are responsible for copayments through
day 100 of the covered stay. Medicare does not cover custodial care if that is the only type of care needed. Custodial
care is care that helps the resident with usual daily activities, like getting in and out of bed, eating, bathing, dressing,
and using the bathroom. It may also include care that most people do themselves, like using eye drops, oxygen, and
taking care of colostomy or bladder catheters. See Centers for Medicare and Medicaid Services. (2019). Medicare
coverage of skilled nursing facility care.
https://www.medicare.gov/Pubs/pdf/10153-Medicare-Skilled-Nursing-Facility-
Care.pdf. The Medicare SNF benefit covers skilled nursing care, rehabilitation services, and other goods and
services. Medicare Payment Advisory Commission. (2019). Skilled nursing facility services payment system.
http://medpac.gov/docs/default-source/payment-basics/medpac_payment_basics_19_snf_final_sec.pdf?sfvrsn=0
21
NFs provide 24-hour long-term medical and skilled nursing care, rehabilitation, or health-related services to
residents. That care is intended to sustain the wellness level of a person who does not require hospital level care but
does require nursing care due to a mental or physical condition and cannot remain at home. Medicaid is the primary
payer of long-term care including 55 billion in 2015 for nursing homes covering approximately 60 percent of NF
residents in the United States. Eiken et. al. (2017, April 14). Medicaid expenditures for long-term services and
supports (LTSS) in FY 2015. https://www.medicaid.gov/sites/default/files/2019-12/ltssexpendituresffy2015final.pdf
.
See also Centers for Disease Control and Prevention. (2016). Long-term care providers and services users in the
United States: data from the national study of long-term care providers, 2013–2014.
https://www.cdc.gov/nchs/data/series/sr_03/sr03_038.pdf. Medicaid coverage of NF services is available only for
services provided in a nursing home licensed and certified by the state survey agency as a Medicaid NF. Centers for
Medicare and Medicaid Services. (n.d.). Nursing facilities.
https://www.medicaid.gov/medicaid/long-term-services-
supports/institutional-long-term-care/nursing-facilities/index.html. NF services are required to be provided by state
Medicaid programs for individuals age 21 or older who need them; services for individuals under age 21 is a
separate, optional, Medicaid service. However, in practice there is no distinction between the services because all
states provide both services. States define the parameters of NF services and NF level of care criteria in their
Medicaid state plan, which may also specify limitations to each service.
22
Sections 1819 and 1919 of the Social Security Act. For the most part, these statutes mirror each other for
consistency across Medicare- and Medicaid-participating facilities with a few special considerations for the scope of
services for SNFs under Medicare.
23
University of Minnesota School of Public Health, Division of Health Policy Management. (2012, March 19). Nursing
home state regulations by state. http://www.hpm.umn.edu/nhregsplus/NHRegs_by_State/By%20State%20Main.html
24
Walsh, K. (2001, December). HEALTH AFFAIRS VOL. 20, NO. 6: CHRONIC CARE IN AMERICA Regulating U.S.
Nursing Homes: Are We Learning From Experience? https://www.healthaffairs.org/doi/full/10.1377/hlthaff.20.6.128
25
Id.
26
Medicare and Medicaid Programs; Emergency Preparedness requirements for Medicare and Medicaid
Participating Providers and Suppliers. 81 Fed. Reg. 63860 (September 16, 2016).
https://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/
27
Artiga, S., Hinton, E., Rudowitz, R., & Musmumeci, M. (2017, January 31). Current flexibility in Medicaid: An
overview of federal standards and state options. Kaiser Family Foundation.
https://www.kff.org/report-section/current-
flexibility-in-medicaid-issue-brief/
28
42 U.S.C. § 1320b–5 (2010).
29
Medicaid and CHIP Payment and Access Commission (MACPAC). (2020, March). Section 1135 Waivers.
https://www.macpac.gov/subtopic/section-1135-waivers/
30
Centers for Medicare & Medicaid Services. (2020, March 13). CMS takes action nationwide to aggressively
respond to coronavirus national emergency [Press release].
https://www.cms.gov/newsroom/press-releases/cms-
takes-action-nationwide-aggressively-respond-coronavirus-national-emergency
31
Centers for Medicare & Medicaid Services. (2020, July 7). Long Term Care Facilities (Skilled Nursing Facilities
and/or Nursing Facilities): CMS Flexibilities to Fight COVID-19
https://www.cms.gov/files/document/covid-long-term-
care-facilities.pdf
32
Centers for Medicare & Medicaid Services. (Updated 2020, August 19) Federal Disaster Resources (Waiver List)
https://www.medicaid.gov/state-resource-center/disaster-response-toolkit/federal-disaster-resources/101346
33
Id.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
16
34
Centers for Disease Control and Prevention. (2020, August 16). Coronavirus disease 2019 (COVID-19), older
adults. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/older-adults.html
35
Centers for Disease Control and Prevention. (2020, August 14). Coronavirus disease 2019 (COVID-19), people
with certain medical conditions.
https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-
medical-conditions.html
36
Centers for Disease Control and Prevention. (2020, June 22). Nursing homes and assisted living (long-term care
facilities [LTCFs]). https://www.cdc.gov/longtermcare/index.html
37
Centers for Disease Control and Prevention. (2020, June 25). Nursing homes & long-term care facilities.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
38
Centers for Disease Control and Prevention. (2020, June 16). How COVID-19 spreads.
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/how-covid-spreads.html
39
Ibid.
40
Hamner, L., Dubbel, P., Capron, I., Ross, A., Jordan, A., Lee, J., Lynn, J., Ball, A., Narwal, S., Russel, S., Patrick,
D., & Leibrand, H. (2020). High SARS-CoV-2 attack rate following exposure at a choir practice — Skagit County,
Washington, March 2020 (Report 2020; 69:606–610). Center for Disease Control and
Prevention. https://www.cdc.gov/mmwr/volumes/69/wr/mm6919e6.htm
41
Jang, S., Han, S., & Rhee, J. (2020). Cluster of coronavirus disease associated with fitness dance classes, South
Korea. Emerging Infectious Diseases, 26(8), 1917-1920. https://dx.doi.org/10.3201/eid2608.200633
42
Centers for Disease Control and Prevention. (2020, July 31). How to protect yourself & others.
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
43
Centers for Disease Control and Prevention. (2020, July 15). Social distancing.
https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/social-distancing.html
44
Rosenberger, L. H., Hranjec, T., Politano, A. D., Swenson, B. R., Metzger, R., Bonatti, H., & Sawyer, R. G. (2011).
Effective cohorting and "superisolation" in a single intensive care unit in response to an outbreak of diverse multi-
drug-resistant organisms. Surgical Infections, 12(5), 345–350. https://doi.org/10.1089/sur.2010.076
45
Uyeki, T. M., Bernstein, H. H., Bradley, J. S., Englund, J. A., File, T. M., Fry, A. M., Gravenstein, S., Hayden, F. G.,
Harper, S. A., Hirshon, J. M., Ison, M. G., Johnston, B. L., Knight, S. L., McGeer, A., Riley, L. E., Wolfe, C. R.,
Alexander, P. E., & Pavia, A. T. (2019). Clinical practice guidelines by the Infectious Diseases Society of America:
2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal
influenza. Clinical Infectious Diseases: An Official Publication of the Infectious Diseases Society of America, 68(6),
e1–e47. https://doi.org/10.1093/cid/ciy866
46
American Health Care Association/National Center for Assisted Living. (2020, April 4). Cohorting residents to
prevent the spread of COVID-19. https://www.ohca.org/docs/documents/5963/Cohorting.pdf
47
Such as “MRSA, VRE, ESBL-producing K. pneumoniae, S. marcescens, Acinetobacter baumannii, and P.
aeruginosa.” Rosenberger, L. H., Riccio, L. M., Campbell, K. T., Politano, A. D., & Sawyer, R. G. (2012). Quarantine,
isolation, and cohorting: From cholera to Klebsiella. Surgical Infections, 13(2), 69–73.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4845677/
48
Musumeci, M & Chidambaram, P. (2020, August 3). Key Questions About Nursing Home Regulation and Oversight
in the Wake of COVID-19. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/key-
questions-about-nursing-home-regulation-and-oversight-in-the-wake-of-covid-19/
49
See for example Whitlock, J. Confirmed Nursing Home Complaints Plummet During Pandemic (2020, Aug. 25)
https://www.voiceofsandiego.org/topics/nonprofits/confirmed-nursing-home-complaints-plummet-during-pandemic/
50
Musumeci, M & Chidambaram, P. (2020, August 3). Key Questions About Nursing Home Regulation and Oversight
in the Wake of COVID-19. Kaiser Family Foundation. https://www.kff.org/coronavirus-covid-19/issue-brief/key-
questions-about-nursing-home-regulation-and-oversight-in-the-wake-of-covid-19/
51
Toblowsky, F. A., Gonzales, E., Self J. L., Rao, C.Y., Keating, R., Marx, G.E., McMichael, T.M., Lukoff, M.D.,
Duchin, J.S., Huster, K., Rauch, J., McLendon, H., Hanson, M., Nichols, D., Pogosjans, S., Fagalde, M., Lenahan, J.,
Maier, E., Whitney, H., … (2020, April 22). COVID-19 outbreak among three affiliated homeless service sites – King
County, Washington, 2020. Centers for Disease Control and Prevention.
https://www.cdc.gov/mmwr/volumes/69/wr/mm6917e2.htm
52
Government Accountability Office. (2020, May 20). Infection control deficiencies were widespread and persistent in
nursing homes prior to COVID-19 Pandemic. https://www.gao.gov/assets/710/707069.pdf
53
Conten, M., et. al. (2020, August 13). More Than 40% of U.S. Coronavirus Deaths Are Linked to Nursing Homes.
The New York Times. https://nyti.ms/31mkr1B
.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
17
54
See Centers for Medicare & Medicaid Services. (2020, April 19). Trump administration announces new nursing
homes COVID-19 transparency effort [Press release].
https://www.cms.gov/newsroom/press-releases/trump-
administration-announces-new-nursing-homes-covid-19-transparency-effort or memo:
https://www.cms.gov/files/document/qso-20-26-nh.pdf). The requirement was established at 42 C.F.R. § 483.80(g) as
published at 85 Fed. Reg. 27550 (May 8, 2020).
55
This heat map was developed from CMS Nursing Home COVID-19 Public File, Submitted Data as of Week Ending
8/9/2020.
56
Centers for Medicare & Medicaid Services. (2020, May 6). Memo to state survey agency directors on interim final
rule updating requirements for notification of confirmed and suspected COVID-19 cases among residents and staff in
nursing homes. https://www.cms.gov/medicareprovider-enrollment-and-certificationsurveycertificationgeninfopolicy-
and-memos-states-and/interim-final-rule-updating-requirements-notification-confirmed-and-suspected-covid-19-
cases-among
57
Chidambaram, P., & Garfield, R. (2020, June 15). Limits and opportunities for federal reporting on COVID-19 in
nursing facilities. Kaiser Family Foundation.
https://www.kff.org/coronavirus-covid-19/issue-brief/limits-and-
opportunities-of-federal-reporting-on-covid-19-in-nursing-facilities/
58
Paulin, E. (2020, June 11). How to track COVID-19 nursing home cases and deaths in your state. AARP.
https://www.aarp.org/caregiving/health/info-2020/coronavirus-nursing-home-cases-deaths.html
59
Ibid.
60
Kaiser Family Foundation. (2020, August 12). State data and policy actions to address coronavirus [Data set].
https://www.kff.org/health-costs/issue-brief/state-data-and-policy-actions-to-address-coronavirus/#long-term-care-
cases-deaths
61
More than 40% of U.S. coronavirus deaths are linked to nursing homes. (2020, July 30). The New York Times.
https://www.nytimes.com/interactive/2020/us/coronavirus-nursing-homes.html
62
Centers for Medicare & Medicaid Services. (2020). COVID-19 nursing home data dictionary [Data set].
https://data.cms.gov/Special-Programs-Initiatives-COVID-19-Nursing-Home/COVID-19-Nursing-Home-Data-
Dictionary/6bgw-jr58
63
National Academies of Sciences, Engineering, and Medicine. (2020, June 11). National academies release COVID-
19 data guide for decision-makers [Press release].
https://www.nationalacademies.org/news/2020/06/national-
academies-release-covid-19-data-guide-for-decision-makers
64
Chernof, B. A., & Mann, C. (2020, July 31). Of the future: will the Covid-19 nursing home tragedies lead to real
change? Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200729.267815/full/
65
Commission on Long-Term Care. (2013, September 30). Report to the Congress.
http://ltccommission.org/ltccommission/wp-content/uploads/2013/12/Commission-on-Long-Term-Care-Final-Report-9-
26-13.pdf
66
Id. at 20-21.
67
Seattle & King County Public Health. (2020, July 10). Personal protective equipment (PPE) prioritization and
distribution for COVID-19 in King County.
https://www.kingcounty.gov/depts/health/covid-
19/~/media/depts/health/communicable-diseases/documents/C19/PPE-prioritization-factsheet.ashx,
68
Goodman, C. K. (2020, May 13). Florida transferring nursing home residents with coronavirus into hospitals. South
Florida Sun Sentinel.
https://www.sun-sentinel.com/coronavirus/fl-ne-coronavirus-nursing-homes-mass-transfers-
20200513-vdpc2txp7jeztepngt3dsk3eve-story.html
69
MITRE-developed, derived from Commission discussion and/or public input.
70
Although current CMS regulations (42 C.F.R. § 483.10) state that “person-centered care means to focus on the
resident as the locus of control and support the resident in making their own choices and having control over their
daily lives,” and recognize the resident’s right to participate in the development and implementation of a person-
centered plan of care as a resident right, resident advocates argue these regulations are vague and difficult to
enforce.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
18
3 Themes, Recommendations, Action Steps, and Analysis
The Commission emerged from its convenings with 27 recommendations, with accompanying
action steps, and organized into ten themes. These themes intersect the Commission’s four
objectives, and reflect responses to the:
• Ongoing supply and affordability dilemmas related to testing, screening, and personal
protective equipment (PPE)
• Tension between rigorous infection control measures and quality of life issues that exist
in cohorting and visitation policies
• Call for transparent and accessible communications with residents, their representatives,
and loved ones, and the public
• Urgent need to train, support, protect, and respect direct-care providers
• Stressed and outdated infrastructure of many nursing-home facilities
• Opportunities to create and organize guidance to owners and administrators that is more
actionable (and data from nursing homes more meaningful for action and research)
• Insufficient funding for quality nursing home operations, workforce performance, and
resident safety.
Organized by theme, this section presents the primary problems identified by the Commission,
outlines CMS responses as of early August (unless otherwise noted) and emerging evidence
related to the theme; and presents the Commission’s principal recommendations and related
action steps. Each theme section closes by documenting the Commission’s endorsements. The
intent is that CMS would implement each principal recommendation in conjunction with its
associated action steps.
The icons, as provided as a sample in Figure 2, respectively, provide a visual indication of the
association between each theme and the four objectives of the Commission, and between the
theme and the volume of public input received on that theme. The icons appear on the first page
of each Theme subsection.
Figure 2. Sample Icons Aligning Themes to Objectives and Public Input Volume.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
19
3.1 Testing and Screening
The Commission identified five primary problems associated with testing and screening.
71
1. National and regional testing and screening supply shortages continue, and nursing homes
have not been prioritized.
2. Extended wait times for testing results prevent meaningful infection control.
72
3. Funding gaps prevent owners and administrators from implementing staff screening and
testing in accordance with existing CMS and CDC guidance.
73
4. Healthcare personnel may lack adequate training to administer tests properly, as well as
sufficient resources and time to screen visitors and staff in accordance with CDC
recommendations.
5. A national strategy that specifically prioritizes nursing home test accessibility with rapid
turnaround time does not yet exist, which contributes to a backlog of screening tests and
hampered nursing homes in responding to outbreaks in real-time.
Response to Date and Emerging Evidence
CMS Actions to Date. Starting in March, CMS and CDC released iterative guidance about
screening and testing residents, staff, and visitors.
74, 75
On July 22, CMS announced an additional
$5 billion from the Provider Relief Fund (including 15,000 testing devices) to support testing,
and that it would begin requiring (rather than recommending) weekly staff testing in states with a
5% positivity rate or greater.
76
The Office of the Assistant Secretary for Health (OASH) oversees
test distribution.
Commission Member Discussions. Commission members focused on this theme during their first
convening on July 1, returning to it throughout their convenings. When asked to prioritize
immediate, short-term actions, this theme was
among the Commission’s top priorities.
Discussion noted challenges that owners and
administrators face with paying for and
acquiring testing and screening supplies.
77, 78
They stressed the need for rapid and
appropriate testing of staff, residents, and
visitors, to mitigate potential spread, leading
them to recommend a targeted approach to
ensure adequate supplies are available.
79
The
Commission focused on the importance of
funding for staff screening and testing in
response to the exclusion of funding for frontline worker return-to-work testing from the CARES
Act.
80
Members also noted the importance of visitor testing. They noted that access to testing
supplies alone was insufficient when unaccompanied by the ability to rapidly receive results.
Some Commission members observed the risks and issues raised by error rates in the rapid
"Major issue is that testing
[and rapid results are] not
readily available. There is a
shortage and laboratories are
redirecting priorities out of the
state, leading to a turnaround
time of more than a week."
-Commission Member

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
20
antigen test results, as well as additional issues arising in some states where state public health
authorities may require nursing homes to use more-sensitive tests than the test technology
provided by CMS and other HHS components.
81
Other members underscored that CMS must not
enforce testing requirements unless all facilities have the testing equipment they need, as well as
sufficient and sustained access to supplies to use the equipment. Further, these members asserted
that in any enforcement scheme, CMS must not punish providers for issues beyond their control
(e.g., lack of available supplies or lab capacity in delivering timely test results). Other members
emphasized the need for CMS to establish clear requirements related to testing according to best
practices, and a mechanism to ensure that those requirements are being followed. With respect to
the provision of testing supplies, a member noted that all testing supplies should be paired with
clear guidance regarding protocols for implementing both surveillance and outbreak response.
(For example, point of care antigen tests may be used for screening staff and visitors on a weekly
basis in a non-outbreak setting. Antigen tests may be used to rapidly identify positive residents
with symptoms; in an outbreak setting all negative antigen tests should be followed by a
confirmatory molecular (PCR) test due to the high potential false negative rates of antigen tests.)
Public Input. Public comments expressed the need for more widely available and rapid testing
and screening to support cohorting, along with visitation policies that can enhance social and
emotional health as well as critical workforce availability. Submitters also noted the importance
of increasing the protection of existing workforce members, as many facilities are already
understaffed and struggle to recruit. Enhanced testing and screening were widely mentioned as
the best solution to ensure the efficient use of staff across facilities, especially in the case of staff
supporting multiple sites.
Emerging Evidence. See Appendix C for discussion of the emerging evidence and regulatory
background.
Principal Recommendation and Action Steps
Principal Recommendation 1A: Immediately develop and execute a national strategy,
coordinating with federal partners and SLTT authorities, for testing and delivering rapid
turnaround of results (i.e., results in less than 24 hours) in nursing homes, in combination with
CDC-recommended screening protocols. Allow nursing home owners and administrators to
tailor the strategy based on community prevalence and resource availability in partnership with
federal and SLTT authorities.
Action Steps
Testing:
• Ensure that nursing homes are prioritized to receive testing and screening supplies, and
rapid turnaround of test results, based on the prevalence of COVID-19 in facilities and in
the surrounding community.
[Collaborate with federal partners; SLTT]
• Develop a central point for coordinating distribution among federal partners of testing
kits (including molecular point-of-care testing) and adequate supplies. Ensure that testing
with sufficient supplies is made available, based on the prevalence of COVID-19 in the

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
21
area, in one quarter, one half, three quarters, and all of the nation’s nursing homes—by
Oct. 1, Nov. 1, Dec. 1, and Jan. 1, 2021, respectively.
[Collaborate with federal partners; SLTT]
• Identify and work to achieve funding mechanisms for nursing home staff to ensure
nursing home capability to conduct baseline and iterative testing of staff and residents
alike. In the interim, seek access to additional funding from the HHS Public Health and
Social Services Emergency Fund to ensure that nursing homes are able to support the
scale of screening and testing required for effective operations.
• Ensure approved rapid tests (e.g., those approved under the NIH RADx initiative) are
providing accurate results.
[Partner with CDC, the Food and Drug Administration (FDA), the National Institutes of
Health (NIH), the Agency for Healthcare Research and Quality (AHRQ), and other
federal agencies as needed]
• Provide a list of recommended tests for nursing home use.
[Collaborate with FDA]
• Provide, with federal partners, training for all rapid testing machines and, as appropriate,
waive current Clinical Laboratory Improvement Amendments (CLIA) limitations to
permit on-site testing.
82
Accompanying instructions should note limitations of rapid tests
in terms of reliability and accuracy.
[Collaborate with federal partners]
• Develop a decision tree that incorporates recommendations from Nursing Home
Reopening Recommendations for State and Local Officials, QSO-20-30-NH (May 18,
2020)
83
and that communicates the most appropriate testing strategy for residents, staff,
and visitors for baseline and iterative testing. This decision tree must be tailored for
community prevalence and other risk factors (e.g., staff travelling between nursing
homes, residents receiving offsite care including dialysis) to encourage effective planning
and intervention. It should explain what to do (e.g., cohorting, observation, transfer,
additional testing) when a resident or staff member: (1) is exposed to an individual(s)
known to have COVID-19; (2) is presumptively positive; (3) confirmed positive; or (4)
refuses testing.
84
If a resident refuses testing under 42 CFR § 483.10(c)(6),
85
require
quarantine of the resident for up to 14 days pursuant to the waiver of 42 CFR §483.10
(e)(6)
86
and (7),
87
and document the reasoning and action in the resident’s record.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
22
Screening:
• Recommend, with support of CDC and FDA, and provide funding for, technology-based
solutions that can improve daily screening processes and allow staff to focus on direct
resident care. Include recommendations for web and phone-based applications that can
quickly capture and assess screening questions for each person entering a nursing home
without the use of staff input or assistance. Develop recommendations for physical
screening technologies (e.g., touchless temperature devices). Update recommendations as
new technologies and evidence emerge.
[Collaborate with CDC and FDA]
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 23 members of the
Commission; 1 member does not endorse Principal Recommendation 1A; 1 member does not
endorse the report.
71
Arons, M. M., Hatfield, K. M., Reddy, S. C., Kimball, A., James, A., Jacobs, J. R., Taylor, J., Spicer, K., Bardossy,
A. C., Oakley, L. P., Tanwar, S., & Dyal, J. W. (2020). Presymptomatic SARS-CoV-2 infections and transmission in a
skilled nursing facility. New England Journal of Medicine, 382, 2081-2090.
https://www.nejm.org/doi/full/10.1056/NEJMoa2008457#article_citing_articles
72
Van Ness, L. (2020, July 15). COVID-19 testing falls short in long-term care facilities. The Pew Charitable Trusts.
https://www.pewtrusts.org/en/research-and-analysis/blogs/stateline/2020/07/15/covid-19-testing-falls-short-in-long-
term-care-facilities
73
Keith, K. (2020, June 25). Feds carve out workplace COVID-19 testing from guaranteed coverage and more.
Health Affairs Blog. DOI: https://www.healthaffairs.org/do/10.1377/hblog20200625.139207/full/
74
Centers for Medicare & Medicaid Services. (2020, March 13). CMS announces new measures to protect nursing
home residents from COVID-19 [Press release]. https://www.cms.gov/newsroom/press-releases/cms-announces-
new-measures-protect-nursing-home-residents-covid-19
75
National Center for Immunization and Respiratory Diseases (NCIRD), Division of Viral Diseases. (2020, February
11). Testing guidelines for nursing homes. Centers for Disease Control and Prevention.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/nursing-homes-testing.html
76
Centers for Medicare & Medicaid Services. (2020, July 22). Trump administration announces new resources to
protect nursing home residents against COVID-19 [Press release]. https://www.cms.gov/newsroom/press-
releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19.
77
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
78
American Health Care Association, National Center Assisted Living. (2020, June 29). Survey shows processing
time of Covid tests for long term care residents and staff a major concern. American Health Care Association
Network. https://www.ahcancal.org/News-and-Communications/Fact-Sheets/FactSheets/AHCA-NCAL-Survey-
Testing-Results.pdf
79
Keith, K. (2020, June 25). Feds carve out workplace COVID-19 testing from guaranteed coverage and more.
Health Affairs Blog. DOI:
https://www.healthaffairs.org/do/10.1377/hblog20200625.139207/full/
10.1377/hblog20200625.139207
80
Ibid.
81
Commission member communications with MITRE, Aug. 24, 2020.
82
Centers for Medicare & Medicaid Services (2020, March 26). Clinical Laboratory Improvement Amendments (CLIA)
Laboratory Guidance During COVID-19 Public Health Emergency. Ref: QSO-20-21-CLIA.
https://www.cms.gov/files/document/qso-20-21-clia.pdf-0.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
23
83
Centers for Medicare & Medicaid Services. (2020, May 18). Nursing home reopening recommendations for state
and local officials. http://www.cms.gov/files/document/qso-20-30-nh.pdf
84
MITRE-developed, derived from Commission discussion and/or public input.
85
Resident rights, 42 CFR § 483.10(c)(6) (2017).
86
Resident rights, 42 CFR §483.10 (e)(6) (2017).
87
Resident rights, 42 CFR §483.10 (e)(7) (2017).

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
24
3.2 Equipment and PPE
The Commission identified the following primary problems associated with equipment and PPE.
1. Nursing home owners and administrators do not have consistent access to an adequate
quantity and quality of PPE,
88
and traditional nursing home supply chains have been
overwhelmed. A recent study found that a fifth of nursing homes had reported a PPE
shortage in June and July.
89
2. Nursing home staff may have gaps in their understanding of best practices for PPE training,
use, and reuse, and thus may not be consistently applying best practices.
Response to Date and Emerging Evidence
CMS Actions to Date. In late April, the Federal Emergency Management Agency (FEMA) issued
a 14-day supply of PPE to all nursing homes;
90
at the end of May, CMS and CDC introduced
national COVID-19 training modules to provide guidance to healthcare personnel. CMS also
issued guidance on April 2 encouraging nursing homes to ensure that all staff were using
appropriate PPE when interacting with patients and residents, as well as conserving that
equipment when necessary in accordance with CDC guidelines (which have been updated
iteratively).
91
Nursing homes report to NHSN on whether they have a seven-day supply of PPE
(i.e., N95 masks, surgical masks, eye protection, gowns, gloves, and hand sanitizer),
92
which
enables federal awareness about specific those nursing homes that may be experiencing supply
shortfalls. CDC’s data is showing that PPE supply is no longer an issue for 90% of nursing
homes, per 7-day reported supply. For example, for the week ending August 16, just 1,354
nursing homes of 14,450 (9.4%) reporting did not have a one-week supply of surgical masks.
93
“PPE varies a lot in quality.
‘PPE is PPE is PPE,’ just
isn’t true!"
-Commission Member
Commission Member Discussions. Commission
members are adamant that CMS has the
responsibility to work with its federal and SLTT
partners to ensure that every nursing home in the
country has a continuous and adequate supply of
high-quality and properly fitting PPE, and that their
staff do not have to provide their own PPE.
Commission members also underscored as the importance of properly training staff on PPE
use.
94
Public Input. Public comments primarily focused on the need to prioritize PPE supply to nursing
home facilities for staff and residents. Many comments also underscored the need for local,
statewide, and regional tracking to prepare for a future surge.
Emerging Evidence. See Appendix C for detailed discussion of the emerging evidence and
regulatory background.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
25
Principal Recommendations and Action Steps
The Commission made three principal recommendations for procurement, use, and training of
adequate and quality PPE in nursing homes.
Principal Recommendation 2A: Assume responsibility for a collaborative process with federal
and SLTT partners to ensure nursing home owners and administrators can procure and sustain a
three-month supply of high-quality supplies of PPE. This process must provide accountability
and oversight.
(Note: Some members support this recommendation only if this process provides accountability,
funding, and oversight; others support it only if this process provides funding and shared
accountability.)
Action Steps
• Develop a process, working with federal partners including CDC, FDA, the Assistant
Secretary for Preparedness and Response (ASPR) and FEMA, for procurement of PPE
that includes:
o Coordinated joint purchasing procurement and distribution of PPE with federal
and SLTT agencies to ensure adequate availability and quality for nursing homes.
o Ability to identify status of PPE inventory, procurement pipeline, and projected
demand at facility, state, and national levels.
o Established quality standards and requirements for commercial use of PPE.
o Ability for CMS to exercise its enforcement authority to ensure compliance and
accountability for procurement of recommended supplies of PPE. (Note: Some
members would amend this recommendation to apply in facilities that can procure
and sustain PPE; for facilities that cannot,
95
CMS will provide support to ensure
those facilities can procure and sustain PPE.)
o Development of standardized, integrated tools to monitor inventory, rotate
stockpiles, manage burn rates, and maintain the federally recommended level of
supplies.
• Add a requirement in the Emergency Preparedness regulation (42 C.F.R. § 483.73) to
include PPE utilization in emergency preparedness and infection control protocols.
96
• Enhance established federal reporting sites (e.g., NHSN and the Payroll-Based Journal
[PBJ]) to capture detailed COVID-19 case reporting, specific staffing information, and
status of PPE availability.
97
(See related Nursing Home Data recommendations.)
[Collaborate with federal partners including the CDC]
• Develop guidelines for nursing home owners and administrators for addressing
equipment and PPE shortages (i.e., procurement options when normal supply chains are
unavailable or protocols for reallocation of supplies currently stored by states, facilities,
and other entities).

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
26
Principal Recommendation 2B: Provide specific guidance on the use, decontamination, and
reuse of PPE, working with federal partners, including CDC, FDA, and OSHA.
Action Steps
• Develop and provide guidance for when to use different PPE such as face shields,
surgical or cloth facemasks, gloves, gowns, and National Institute for Occupational
Safety and Health (NIOSH)-approved N95 respirators. This guidance must be specific to
nursing home staff residents, contractors, essential care partners, and visitors (including
ombudsmen and surveyors). It must also identify expectations during outbreaks, followed
by ramping down when appropriate. The guidance should incorporate decision-making
based on the level of infection severity within the facility itself and geographic location
alike.
• Release guidance for FDA-approved reuse of PPE and other essential equipment,
prioritizing the use of N95 masks for high-risk staff. Include a framework for facility
medical directors to implement practices most appropriate on a case-by-case basis. (Note:
some Commission members recommend that CMS promote coordination with state and
local authorities to offer fit testing and other training for nursing homes. Other members
emphasized the need for a clear process, adequate funding, and an achievable procedure
for facilities to meet these standards.) [Collaborate with OSHA]
• Release guidance on fit testing for NIOSH-approved N95 respirators and other tight-
fitting respirators (according to available manufacturer specifications).
• Establish requirements and guidance on decontamination of N95 respirators.
• Provide guidelines for equipment and PPE shortages (i.e., refresh/reuse protocols,
strategies for extending limited supplies, and use of alternative products where
applicable).
• Centralize communications about
98
and provide training on methods for refresh and reuse
of PPE by healthcare personnel in situations when shortages require optimizing and
extending the supply and use of PPE. Increase the visibility of CDC Crisis Capacity
strategies. [Collaborate with CDC.] (See also Principal Recommendation 10B .)
Principal Recommendation 2C: As needed, collaborate with other federal and state agencies to
provide guidance on training to all clinical and nonclinical facility staff on proper use of PPE and
equipment, according to available manufacturer specifications. (See also recommendation on
Infection Preventionist under Workforce Ecosystem.)
Action Steps
• Establish national training requirements for infection control and use of PPE for all
healthcare personnel, as well as other individuals with direct and indirect contact with
residents. This should be incorporated into the training requirements set forth in 42 CFR
483.80 and 42 CFR 483.95.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
27
• Tailor training modules for PPE utilization for administrators, residents, staff,
contractors, essential care partners, and visitors.
• Incorporate PPE training modules into the Nursing Home Preventionist Training course
and the Infection Prevention and Control Program (IPCP).
• Establish national training standards for staff based on existing core competency
standards or other model standards/certifications developed by states.
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 24 members of the
Commission; 1 member does not endorse the report.
88
McGarry, B. E., Grabowski, D. C., & Barnett, M. L. (2020, August 20). Severe Staffing And Personal Protective
Equipment Shortages Faced By Nursing Homes During The COVID-19 Pandemic. Health Affairs (Project Hope),
101377hlthaff202001269. Advance online publication.
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.01269
89
McGarry, B. E., Grabowski, D. C., & Barnett, M. L. (2020). Severe Staffing And Personal Protective Equipment
Shortages Faced By Nursing Homes During The COVID-19 Pandemic. Health Affairs (Project Hope),
101377hlthaff202001269. Advance online publication.
https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2020.01269
90
FEMA. (2020, April 30). Personal protective equipment for Medicare and Medicaid nursing homes [Press release].
https://www.fema.gov/news-release/20200727/personal-protective-equipment-medicare-and-medicaid-nursing-
homes
91
Centers for Medicare and Medicaid Services. (2020, April 2). COVID-19 long-term care facility guidance.
https://www.cms.gov/files/document/4220-covid-19-long-term-care-facility-guidance.pdf
92
Centers for Medicare and Medicaid Services. (2020). COVID-19 Data Dictionary.
https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data-Data-Dictionary/8rzn-j9yt/
93
Centers for Medicare and Medicaid Services. (2020). COVID-19 Nursing Home Dataset.
https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/
94
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
95
MITRE suggests perhaps CMS could assess this by NHSN reporting on 7-day supply.
96
MITRE-developed, derived from Commission discussion and/or public input.
97
Elizaitis, B. (2020, April 25) CMS Publishes List of Nursing Home Staffing Levels. CMS Compliance Group, INC.
https://cmscompliancegroup.com/2020/04/25/cms-publishes-list-of-nursing-home-staffing-levels/
.
98
Centers for Disease Control and Prevention. (2020, July 16). Optimizing Supply of PPE and Other Equipment
during Shortages. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
28
3.3 Cohorting
The Commission identified two primary problems associated with cohorting.
1. Cohorting is considered a common infection prevention and control technique
99
and a core
response tool against COVID-19.
100, 101
It has been effective historically, as well as during
recent outbreaks of infectious diseases.
102, 103
Nevertheless, isolation associated with
cohorting can instill loneliness and increase the risk for a number of health conditions in
residents (e.g., cognitive decline, stroke, high blood pressure, and other complications).
104
Cohorting practices based on COVID-19 status may negatively affect their social and
emotional health, contributing to increased anxiety and/or depression among residents.
105
2. Owners and Administrators may not be able to implement existing cohorting guidance
because of staffing, equipment, and/or environmental limitations (e.g., cleaning, tight space,
lack of physical barriers, inadequate ventilation systems), and may be inappropriately
incentivized to isolate residents.
106, 107
Response to Date and Emerging Evidence
CMS Actions to Date. CMS issued blanket waivers of certain requirements (e.g., physical
environment, transfer, and discharge) to ease cohorting implementation in nursing homes. In
conjunction with CDC, it also issued a series of related recommendations.
108
The CDC also
issued iterative guidance to help owners and administrators with cohorting-related decisions.
109
Commission Member Discussions. Commission members stressed that, although cohorting is a
critical infection prevention and control tool, it has a detrimental effect on residents. They
expressed concern that the use of blanket waivers to ease cohorting implementation exacerbates
tension between the need to protect residents and staff from COVID-19 and the need to ensure
resident rights and quality of life.
110
Public Input. The public noted the
importance of social and emotional
health, along with the need for
evidence-based policies regarding
cohorting, nursing home design, and
visitation. The public noted that
significant work remains to be done to
balance the costs and benefits of
restrictive policies against the
consequences of minimal care and
decreased socialization.
Emerging Evidence. No additional
evidence has been identified at this
time.
"Being told you are moving with very
little notice and no choice is disturbing
but these are unusual circumstances. ....
The mortality rate of nursing home
residents in my state .... is] 31% .... I
think most would choose to cohort
quickly if they understood what is at
stake. ... Conversations [ahead of time]
with the residents about why they need
to relocate and resolving their concerns
would certainly be the correct way to
proceed."
-Commission Member

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
29
Principal Recommendations and Action Steps
Principal Recommendation 3A: Update cohorting guidance to balance resident and staff
psychological safety and well-being with infection prevention and control.
Action Steps
• Develop clear and concise guidance for cohorting using the Tuberculosis (TB)
111
Training Module 12B in the CDC’s Infection Preventionist training course
112
and the
Recommended Nursing Home Phased Reopening for States.
113, 114
Ensure CMS cohorting guidance:
o Prioritizes resident social and emotional health and minimizes disruption of
resident daily routines
o Includes instructions for determining, monitoring, and adapting staffing
assignments that maintain cohorts while minimizing inequity of staff workload
(see Principal Recommendation 6B and associated action steps for more details)
o Is adaptable based on community COVID-19 prevalence
o Reflects resident rights to return to original room (within original facility, if they
are moved outside the facility) once transmission risk has been mitigated
115
• Modify 42 C.F.R. § 483.10 and § 483.15 waivers to:
o Require nursing homes to proactively communicate via advance written notice
(e.g., in email and/or in print) with residents and residents’ representatives
specifically about facility cohorting protocols, including protocols specific to the
possibility of in-facility and extra-facility transfer.
o Require that when COVID-19 tests are administered, nursing homes notify
residents and residents’ representatives specifically how the facility’s cohorting
protocol will be applied upon the receipt of the COVID-19 test results, including
whether a positive or negative test will require an in-facility transfer or extra-
facility transfer (and, for extra-facility transfers, the options available to the
resident).
o Require that when a test result is received and/or symptoms emerge that require a
resident to be isolated and/or transferred in-facility or outside the facility,
residents and residents’ representatives are notified about the intent to isolate or
transfer and provided additional, case-specific details about that process while
maintaining compliance with the Health Insurance Portability and Accountability
Act (HIPAA). For transfers outside the facility, require facilities to speak with
residents or representatives to choose an alternate facility, unless such
conversations would cause a delay presenting a clear danger to residents’ health
or safety. Require a minimum of two documented attempts to comply, including
method(s), date(s), and time(s).

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
30
• Commission a study to identify the effects of cohorting for prolonged periods of
indefinite duration, methods for nursing home owners and administrators to address those
effects, requirements for implementing isolation, and strategies for adapting practices
when a vaccine emerges.
116
[Collaborate with the National Academy of Sciences, Engineering, and Medicine
(NASEM)]
Principal Recommendation 3B: Update cohorting guidance and reimbursement policy to
address differences in nursing home resources (e.g., facility, infrastructure, staff).
Action Steps
• Recommend nursing homes have an observation unit or separate area for new admission
or transfer residents. For nursing homes without the ability to create this infrastructure,
continue to allow the nursing home to cohort new admissions in another facility for the
purpose of observation by waiving requirements in 42 CFR 483.10(c)(5);
483.15(c)(4)(ii), (c)(5)(i) and (iv), (c)(9), and (d); and §483.21(a)(1)(i), (a)(2)(i), and (b)
(2)(i). Ensure residents and residents’ representatives receive ongoing communications
about observation plans and actions.
• Modify the Resident Assessment Instrument/Minimum Coding Set (RAI/MDS) coding
instructions (Chapter, MDS 3.0 RAI Manual O0100M2) to eliminate the possibility of a
higher reimbursement rate for residents placed in a room alone (i.e., isolated/quarantined)
than that paid for residents who have been cohorted with a group in accordance with
CDC and/or CMS COVID-19 cohorting guidelines.
• Redirect and prepare Quality Improvement Network (QIN)-Quality Improvement
Organizations (QIO) to assist nursing home providers with development of effective
cohorting plans (see Principal Recommendation 8A and associated action steps for more
details).
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 23 members of the
Commission; 1 member does not endorse Principal Recommendation 3B; 1 member does not
endorse the report.
99
Lee, T., Jordan, N. N., Sanchez MD, J. L., Gaydos MD, J. C. (2005). Selected nonvaccine interventions to prevent
infectious acute respiratory disease. American Journal of Preventive Medicine, 28(3), 305-316.
https://doi.org/10.1016/j.amepre.2004.12.010
100
Centers for Disease Control and Prevention. (2020, June 25). Preparing for COVID-19 in nursing homes.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
101
Sanchez, G. V., Biedron, C., Fink, L. R., Hatfield, K. M., Polistico, J. M. F., Meyer, M. P., Noe, R. S., Copen, C. E.,
Lyons, A. K., Gonzalez, G., Kiama, K., Lebednick, M., Czander, B. K., Agbonze, A., Surma, A. R., Sandhu, A., Mika,

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
31
V. H., Prentiss, T., Zervos, J., … (2020, July 10). Initial and repeated point prevalence surveys to inform SARS-CoV-2
infection prevention in 26 skilled nursing facilities – Detroit, Michigan, March-May 2020. Centers for Disease Control
and Prevention. https://www.cdc.gov/mmwr/volumes/69/wr/mm6927e1.htm?s_cid=mm6927e1_w
102
Such as “MRSA, VRE, ESBL-producing K. pneumoniae, S. marcescens, Acinetobacter baumannii, and P.
aeruginosa.” Rosenberger, L. H., Riccio, L. M., Campbell, K. T., Politano, A. D., & Sawyer, R. G. (2012). Quarantine,
isolation, and cohorting: From Cholera to Klebsiella. Surgical Infections, 3(2), 69–73.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4845677/
103
Cohorting is the process of locating individuals with the same condition in the same space with the intent of
reducing or eliminating interaction between infected persons with uninfected persons.
104
Simard, J., & Ladislav V. (2020, May 2). Loneliness and isolation in long-term care and the COVID-19 pandemic.
Journal of the American Medical Directors Association, 21(7), 966-967. https://doi.org/10.1016/j.jamda.2020.05.006
105
Simard, J., & Ladislav V. (2020, May 2). Loneliness and isolation in long-term care and the COVID-19 pandemic.
Journal of the American Medical Directors Association, 21(7), 966-967. https://doi.org/10.1016/j.jamda.2020.05.006
106
Iaboni, A., Cockburn, A., Marcil, M., Rodrigues, K., Marshall, C., Garcia, M. A., Quirt, H., Reynolds, K. B., Keren,
R., & Flint, A. J. (2020). Achieving safe, effective, and compassionate quarantine or isolation of older adults with
dementia in nursing homes. The American Journal of Geriatric Psychiatry: Official Journal of the American
Association for Geriatric Psychiatry, 28(8), 835–838. https://doi.org/10.1016/j.jagp.2020.04.025
107
Cohen, C. C., Pogorzelska-Maziarz, M., Herzig, C. T., Carter, E. J., Bjarnadottir, R., Semeraro, P., Travers, J. L.,
& Stone, P. W. (2015). Infection prevention and control in nursing homes: A qualitative study of decision-making
regarding isolation-based practices. BMJ Quality & Safety, 24(10), 630–636. https://doi.org/10.1136/bmjqs-2015-
003952
108
Centers for Medicare & Medicaid Services. (2020, April 13). 2019 Novel Coronavirus (COVID-19) long term care
facility transfer scenarios. https://www.cms.gov/files/document/qso-20-25-nh.pdf; Centers for Medicare and Medicaid
Services. (2020, July 9). Long term care facilities (skilled nursing facilities and/or nursing facilities): CMS flexibilities to
fight COVID-19. https://www.cms.gov/files/document/covid-long-term-care-facilities.pdf; Centers for Disease Control
and Prevention. (2020, June 25). Preparing for COVID-19 in nursing homes. https://www.cdc.gov/coronavirus/2019-
ncov/hcp/long-term-care.html; Centers for Medicare and Medicaid Services. (2020, April 2). COVID-19 long-term care
facility guidance. https://www.cms.gov/files/document/4220-covid-19-long-term-care-facility-guidance.pdf
109
Centers for Disease Control and Prevention. (2020, April 30). Responding to Coronavirus (COVID-19) in nursing
homes. https://www.cdc.gov/coronavirus/2019-ncov/hcp/nursing-homes-responding.html
110
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
111
Tuberculosis in general, and the TB training specifically, is considered analogous to COVID because both are
respiratory infections that are spread by a person who releases droplets into the air when breathing out. Secondly,
the presence of comorbidities can result in poor outcomes for both diseases. In addition, CDC provided respiratory
infection control measures for both COVID-19 and TB, including the following:
• Triage, early identification, and separation of symptomatic patients
• Fast tracking or expedited service
• Implementation of droplet and contact precautions
• Frequent handwashing
• Implement environmental engineering controls, for example, physical barriers and dedicated pathways to guide
symptomatic patients through triage areas, remote or outdoor triage stations for patients with respiratory
symptoms
• Use of personal protective equipment (PPE)
Centers for Disease Control and Prevention. (2020, August 17). Operational considerations for maintaining
essential services and providing prevention, care, and treatment for Tuberculosis (TB) in low-resource non-US
settings during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/TB-non-
us-settings.html
112
Centers for Disease Control and Prevention. (n.d.). Nursing home infection preventionist training course.
http://www.train.org/cdctrain/course/1081820/
113
Centers for Medicare and Medicaid Services. (2020, May 18). Nursing home reopening recommendations for state
and local officials. http://www.cms.gov/files/document/qso-20-30-nh.pdf
114
MITRE-developed, derived from Commission discussion and/or public input.
115
MITRE-developed, derived from Commission discussion and/or public input.
116
MITRE-developed, derived from Commission discussion and/or public input.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
32
3.4 Visitation
The Commission identified four primary problems associated with visitation.
1. Although visitation restrictions have partially protected the physical health of residents, the
practice also has resulted in unintended harm. Residents experience loneliness, anxiety, and
depression due to prolonged separation from families and loved ones.
117, 118
These measures
also compromise the ability of families and guardians to validate resident well-being and
safety, and caused significant distress for families.
119
2. Virtual visitation often provides an insufficient substitute to address resident needs. The gap
between in-person and virtual visitation is even more acute when combined with limitations
due to differing physical and cognitive abilities; resident, family, and/or staff unfamiliarity
with proper equipment use and functionality; and equipment and internet availability.
120
3. The extent of this unintended harm has not been adequately assessed; nursing home staff also
have under-prioritized the continuation of routine daily activities to address infectious
disease protocols, thus exacerbating the unintended harm caused by overly restrictive
visitation policies.
121
4. Visitation guidance is currently unclear. CMS and its federal partners have issued directives
and guidance pertaining to visitation during the pandemic in multiple documents, making it
challenging for nursing homes to meet (and CMS to enforce) federal expectations or leverage
evolving flexibility.
Response to Date and Emerging Evidence
CMS Actions to Date. After initially advising nursing home owners and administrators to adopt
restrictive visitation policies, CMS subsequently clarified its guidance, expanded visitation
guidelines in compassionate care and other situations, and provided suggestions to help residents
connect with their families.
122
Commission Member Discussions. Throughout their convenings,
123
many members expressed
serious concerns about the effect restrictions have on residents’ mental health and well-being;
they supported finding ways to increase visitation without compromising infection prevention
and control. Other members questioned whether relaxing restrictions—especially in areas with
high community prevalence—would increase the risk of COVID-19 transmission. Commission
members also discussed the need to monitor for and prevent the misuse of antipsychotic and
antidepressant medication, especially among isolated residents.
Public Input. Public commenters overwhelmingly supported policies grounded in person-
centered care practices, viewed improving visitation as vital to support nursing home residents,
and expressed the importance of maintaining communication with family and essential care
partners. These issues received the greatest volume of public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
33
Emerging Evidence: The most effective way to prevent spreading of SARS-CoV-2 at the
population level is to limit the frequency and duration of contact between an infected individual
and an uninfected individual.
124
SARS-CoV-2’s incubation period (estimated by CDC to extend
up to 14 days),
125
coupled with emerging evidence of spreading by asymptomatic carriers of the
virus, means that visitors without observable symptoms can infect nursing home residents and
staff. Physical separation of visitors and
residents is an effective way to reduce spread
of the virus;
126
nevertheless, residents rely on
visits with loved ones and caregivers outside
of the nursing home (e.g., family members,
friends) for care and critical emotional
support, and those visitors in turn rely on
visitation to ensure resident safety and
quality of care.
127, 128, 129
Maintaining those
relationships in the absence of in-person
visitation has posed a challenge due to
limited supply of technology,
130
lack of staff
training on that technology, and difficulty
tracking evolving CMS expectations.
“The decision has been made for
Mom and thousands of her peers
to choose longevity over quality
of life. This includes many folks
on hospice…they are simply
robbed of their quality. For
people with dementia like my
mother, today is their best day.
Tomorrow will be a little worse
and who knows if there will be a
six-months from now… We are
losing precious time.”
-Public Input
Principal Recommendations and
Action Steps
Principal Recommendation 4A: Emphasize that visitation is a vital resident right. Update and
release consolidated, evidence-based guidance on safely increasing controlled, in-person
visitation prior to federal Phase 3
131
reopening.
Action Steps
• Provide updated guidance on in-person visitation that immediately enables nursing home
owners and administrators to adjust protocols and safely increase in-person visitation by
essential care partners, compassionate care visitors, and ombudsmen based on emerging
and established evidence. This CMS in-person visitation guidance should:
o Restate the existing right to visitation and clarify modifications to this right for each
phase of the pandemic.
o Describe or restate minimum standards for visitor testing, training on and use of facial
coverings and other PPE, temperature checks, physical distancing, visitor movement
restrictions (e.g., separate visitor rooms, indoor/outdoor options, staggered visitation
schedules), post-visit disinfection, instructional signage, supervision and assistance
from staff, and SARS-CoV-2 positive visits.
o Outline how to adapt visitation policies based on local prevalence of COVID-19 cases
internal and external to nursing homes.
o Require nursing home owners and administrators to encourage residents to designate
an Essential Care Partner that can visit in person when other visitors may not be

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
34
allowed; when a resident is unable to do so, the legal surrogate could serve as an
Essential Care Partner or appoint an alternate, such as a loved one.
o Include a person-centered, consumer-driven definition of compassionate care
situations (e.g., not limited to hospice care or last days or hours of life), along with
criteria for assessing when compassionate care and extended end-of-life visitation by
at least one visitor is appropriate.
o Stress that ombudsmen may visit residents, and relay information to families and
guardians, prior to federal Phase 3
132
reopening when they are able to observe
infection prevention and control standards.
Principal Recommendation 4B: Update and release consolidated, evidence-based guidance on
effectively planning for and implementing virtual visitation tools and techniques.
Action Steps
• Provide guidance on virtual visitation that specifies evidence-based protocols for
acquiring, using, and safely sharing technology and communicative devices (e.g., cell
phones, tablets, webcams, other web applications/platforms) to safely facilitate virtual
visitation. This CMS virtual visitation guidance should:
o Encourage safe sharing of sanitized technology that is readily accessible (e.g., large
button phones) and available to residents (e.g., at the closest nursing station).
o Provide learning resources about various technology tools that nursing home staff can
use to communicate with residents, families, and staff (see Principal
Recommendation 8A and associated action steps for more details).
o Include information on accessing and using low-cost, creative methods for
maintaining contact between residents and their loved ones (e.g., messages through
windows, Jitterbug flip phone, postcards).
133, 134
• Continue to facilitate the sharing of ideas about virtual visitation options among nursing
home owners and administrators.
• Encourage state agencies to approve applications for the use of civil money penalty
(CMP) funds for the purpose of providing communicative devices for virtual visitation.
135
Principal Recommendation 4C: Provide resources to help nursing home staff assess and
improve the mental health and psychosocial well-being of residents during and after the
pandemic.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
35
Action Steps
• Develop and distribute a mental health supplemental assessment to help nursing home
staff assess and improve the psychosocial well-being of residents exhibiting a mental
health status change. The supplemental assessment should:
o Contain assessment items separate from the current RAI/MDS questions on mood and
behavior that would identify when a resident is suffering emotionally due to isolation
and lack of family contact
o Include adaptation options so nursing home staff can tailor items to enhance their
current resident assessments and meet unique needs of residents
136
o Outline instruction for implementation by staff with training in behavioral health
137
o Inform resident care, recognizing that residents continue to have the right to shape
their own care plans
• Monitor a subset of data generated from mental health supplemental assessment use and
resultant care changes to assess impact; consider formally integrating this supplemental
assessment into the RAI required at 42 C.F.R. § 483.20 in place of outdated or less-
comprehensive mental health assessment components.
• Issue guidance that promotes regular socialization within facilities and outside of resident
rooms; prohibits unnecessary isolation within resident rooms; reinforces the prohibition
of the misuse of antipsychotic and antidepressant medications; and emphasizes the
importance of routine daily activities (e.g., showering and personal hygiene, communal
meals, meditation, exercise).
• Distribute guidance for accessing and integrating telehealth-based mental health services
for nursing home residents.
138
• Provide training at no cost to direct-care providers about psychological first aid and
trauma-informed care. See also Principal Recommendation 8A and associated action
steps for more details.
[Collaborate with CDC and/or FEMA]
• Amend 42 CFR § 483.10 to include differentiated reference to compassionate care and
hospice care under the residents’ rights provision; define contingencies for emergencies.
Principal Recommendation 4D: Assess, streamline, and increase the accessibility of COVID-
19-related directives, guidance, and resources on visitation into a single source.
Action Steps
• Identify all of CMS’s COVID-19 ideas, suggestions, guidance, frequently asked
questions (FAQ), and directives to date regarding visitation (“visitation information”).
139
• Analyze CMS visitation information released to date for accuracy and actionability.
140

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
36
• Synthesize visitation information into a single, user-friendly source accessible to all
stakeholder groups.
• Add a single, user-friendly visitation information source to dynamic multi-user interface
enabling nursing home staff to exchange updated information with CMS and its federal
partners, as well as make evidence-based decisions about visitation policies and
procedures (see Data Principal Recommendation 10B and associated action steps for
more details).
• Establish an operating procedure to ensure timely updates on visitation based on
emerging evidence.
141
• Update regularly new single visitation source based on emerging evidence.
• Harmonize federal, state, and local visitation guidance, ideally through single, user-
friendly, dynamic multi-user interface (see Data Principal Recommendation 10B and
associated action steps for more details).
[Collaborate with federal partners; SLTT]
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 23 members of the
Commission; 1 member does not endorse Principal Recommendation 4A; 1 member does not
endorse the report.
117
Abbasi, J. (2020, July 16). Social Isolation—the Other COVID-19 Threat in Nursing Homes. JAMA 324(7):619-
620. doi:10.1001/jama.2020.13484 https://jamanetwork.com/journals/jama/article-abstract/2768640
118
Chidambaram, P. (2020, March 13). Data Note: How might Coronavirus Affect Residents in Nursing Facilities?
Kaiser Family Foundation.
https://www.kff.org/coronavirus-covid-19/issue-brief/data-note-how-might-coronavirus-
affect-residents-in-nursing-facilities/
119
Hado, E., & Feinberg, L.F. (2020, May 22). Amid the COVID-19 pandemic, meaningful communication between
family caregivers and residents of long-term care facilities is imperative. Journal of Aging and Social Policy, 32(4-5),
410-415. https://doi.org/10.1080/08959420.2020.1765684; Grabowski, D. C., & Mitchell, S. L. (2009). Family
oversight and the quality of nursing home care for residents with advanced dementia. Medical Care, 47(5), 568-574.
https://dx.doi.org/10.1097%2FMLR.0b013e318195fce7; Simard, J., Volicer, L. (2020). Loneliness and isolation in
long-term care and the covid-19 pandemic. The Journal of Post-Acute and Long-Term Care Medicine, 21(7), 966-
967.
https://doi.org/10.1016/j.jamda.2020.05.006
120
Soregel, A. (2020, June 11). Nursing homes receive tech devices thanks to government-nonprofit funding. AARP.
https://www.aarp.org/caregiving/health/info-2020/more-nursing-home-virtual-visits.html
121
Simard, J., & Volicer, L. (2020). Loneliness and isolation in long-term care and the Covid-19 pandemic. The
Journal of Post-Acute and Long-Term Care Medicine, 21(7), 966-967.
https://www.jamda.com/article/S1525-
8610(20)30373-X/fulltext
122
Center for Clinical Standards and Quality. (2020, March 13). Guidance for infection control and prevention of
Coronavirus disease 2019 (COVID-19) in nursing homes (revised). Centers for Medicare and Medicaid Services.
https://www.cms.gov/files/document/3-13-2020-nursing-home-guidance-covid-19.pdf; Centers for Medicare and
Medicaid Services. (2020, June 23). Frequently asked questions on nursing home visitation.
https://www.cms.gov/files/document/covid-visitation-nursing-home-residents.pdf; Center for Clinical Standards and
Quality. (2020, April 24). Nursing home five star quality rating system updates, nursing home staff counts, and
frequently asked questions. Centers for Medicare and Medicaid Services.
https://www.cms.gov/files/document/qso-
20-28-nh.pdf; Center for Clinical Standards and Quality. (2020, May 6). Interim final rule updating requirements for

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
37
notification of confirmed and suspected COVID-19 cases among residents of staff in nursing homes. Centers for
Medicare and Medicaid Services. https://www.cms.gov/files/document/qso-20-29-nh.pdf
123
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
124
Qualls, N., Levitt, A., Kanade, N., Wright-Jegede, N., Dopson, S., & Biggerstaff, M. (2017). Community mitigation
guidelines to prevent pandemic influenza - United States, 2017. MMWR. Recommendations and reports: Morbidity
and mortality weekly report. Recommendations and reports, 66(1), 1-34.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5837128/
125
Centers for Disease Control and Prevention. (2020, June 30). Interim clinical guidance for management of patients
with confirmed coronavirus disease (COVID-19).
https://www.cdc.gov/coronavirus/2019-ncov/hcp/clinical-guidance-
management-patients.html
126
Arons, M. M, Hatfield, K. M, Reddy, S. C., Kimball, A., et al. (2020). Presymptomatic SARS-CoV-2 infections and
transmission in a skilled nursing facility. New England Journal of Medicine, 382, 2081-2090.
https://www.nejm.org/doi/full/10.1056/NEJMoa2008457#article_citing_articles
127
Frampton, S, Agrawal, S Guastello, S. (2020, July 6). Guidelines for Family Presence Policies During the COVID-
19 Pandemic. JAMA. https://jamanetwork.com/channels/health-forum/fullarticle/2768108
128
Hado E. & Feinberg L. F. (2020, April 30). Amid the COVID-19 pandemic, meaningful communication between
family caregivers and residents of long-term care facilities is imperative. Families and Caregivers of Older Adults,
32(4-5), 410-415. doi: https://doi.org/10.1080/08959420.2020.1765684
129
Grabowski, D. C., Mitchell, S. L. (2009). Family oversight and the quality of nursing home care for residents with
advanced dementia. Medical Care, 47(5), 568-574. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2709799/
130
Soergel A. (2020, June 11). Nursing homes receive tech devices thanks to government-nonprofit funding. AARP.
https://www.aarp.org/caregiving/health/info-2020/more-nursing-home-virtual-visits.html
131
Centers for Disease Control and Prevention (2020). CDC Activities and Initiatives Supporting the COVID-19
Response and the President’s Plan for Opening America Up Again.
https://www.cdc.gov/coronavirus/2019-
ncov/downloads/php/CDC-Activities-Initiatives-for-COVID-19-Response.pdf
132
Centers for Disease Control and Prevention (2020). CDC Activities and Initiatives Supporting the COVID-19
Response and the President's Plan for Opening America Up Again.
https://www.cdc.gov/coronavirus/2019-
ncov/downloads/php/CDC-Activities-Initiatives-for-COVID-19-Response.pdf
133
Simard, J., Volicer, L. (2020). Loneliness and isolation in long-term care and the Covid-19 pandemic. The Journal
of Post-Acute and Long-Term Care Medicine, 21(7), 966-967. https://doi.org/10.1016/j.jamda.2020.05.006
134
MITRE-developed, derived from Commission discussion and/or public input.
135
MITRE-developed, derived from Commission discussion and/or public input.
136
MITRE-developed, derived from Commission discussion and/or public input.
137
MITRE-developed, derived from Commission discussion and/or public input.
138
Verma, S. (2020, July 15). Early impact of CMS expansion of Medicare telehealth during COVID-19. Health
Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200715.454789/full/
139
MITRE-developed, derived from Commission discussion and/or public input.
140
MITRE-developed, derived from Commission discussion and/or public input.
141
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
38
3.5 Communication
The Commission identified the following primary problem associated with communication.
1. Knowledge about COVID-19—including incidence, prevalence, virulence, symptoms,
prevention, control, treatment, and recovery—is rapidly evolving. Nursing homes are
challenged in keeping nursing home residents and their loved ones informed about the most
up-to-date information on COVID-19, related protocols, and polices.
Response to Date and Emerging Evidence
CMS Actions to Date: CMS updated regulations
142
and provided guidelines
143
to nursing home
owners and administrators regarding communications with residents and caregivers during the
COVID-19 pandemic. These measures generally recommend nursing home staff maintain a
person-centered approach to communications and to seek alternatives for communication (e.g.,
emails, letters, and signage). CMS also provided examples of nursing home communication from
various states.
144
The guidance and follow-up examples do not address existing regulatory
compliance framework for providing notice where it is required, and do not establish nationwide
minimum standards for level and type of communication.
Commission Member Discussions: Throughout their convenings,
145
several Commission
members shared approaches to communication with residents, essential care partners, and
families.
146
Commission members noted ambiguity in CMS’s guidance, citing the need for more
detail related to message type, recipients, and
accessibility. Additionally, members expressed
concerns about issues involving affordability of
technology, privacy, meeting family member
expectations, and inconsistencies in staff
availability to manage communications.
Public Input: Public comments expressed interest
in keeping essential care partners, resident
representatives, family members, and loved ones
informed about resident well-being and nursing
home policies and practices in a unified,
accessible, consistent, and transparent manner.
Emerging Evidence: Over the course of the
pandemic, communications strategies have varied
widely across states and facilities. Additionally, the
pace of information flow during the pandemic has sparked leading long-term care stakeholders to
encourage nursing home owners and administrators to hasten their communication processes:
“Because information about the outbreak is evolving rapidly, often on a daily basis, facilities
should be prepared to update their messaging quickly to ensure [residents] and family members
have the most current information they need to stay safe and healthy.”
147
“[Facilities are obligated]…
to notify residents, family
members of infections or
likely infections within the
facility. But the sense…[is]
there's still too much
ambiguity there, that there
needs to be more detail to
make sure that that
information is presented in a
way that's understandable.”
-Commission Member

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
39
See Appendix C for additional detailed discussion of the emerging evidence and regulatory
background.
Principal Recommendation and Action Steps
Principal Recommendation 5A: Increase specificity and expand breadth of guidance on
communications between nursing home staff, residents, and families.
Action Steps
• Provide standardized templates for email blasts, newsletters, bulletins, town hall discussion
guides, and the like to be used when issuing regular updates. Allow nursing home staff to
tailor their communication to the literacy and cultural needs of recipients (including
residents, essential care partners, resident representatives, family members, loved ones, and
advocates).
• Define the type of information that nursing home staff are expected to communicate (e.g.,
specifics about a cohorting plan; transfer and discharge rights during phases of an
emergency; visitation and/or connection options; options for residents to share feedback;
screening/testing protocols and policies; COVID-19 cases and deaths).
• Define time-sensitivity of key messages (e.g., about transfers, discharge, hospitalization).
148
• Require an individualized communication plan as part of each nursing home resident’s
individual care plan, documenting preferred mode (e.g., recordings, letters, phone, video, in-
person) and frequency of communications; with whom to engage (e.g., residents, providers,
loved ones; one-on-one, small groups, or large groups); and action steps for missed
communications.
• Assess and advise nursing home owners and administrators on how federal COVID-19 relief
funds can support adoption of multimedia communication systems (e.g., text, phone, email,
virtual townhalls, websites, applications, cameras).
• Amend federal requirements for nursing homes to create and implement protocols for the
adoption of multimedia communication systems.
149
• Consider long-term regulations requiring nursing home owners and administrators to
integrate these specific details in communications.
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 24 members of the
Commission; 1 member does not endorse the report.
142
The requirement was established at 42 C.F.R. § 483.80(g)(3) as published at 85 Fed. Reg. 27550 (May 8, 2020).
143
Centers for Medicare & Medicaid Services Center for Clinical Standards and Quality/Quality, Safety & Oversight
Group. (2020, March 13). Memorandum to state survey agency directors: guidance for infection control and

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
40
prevention of coronavirus disease 2019 (COVID-19) in nursing homes (REVISED). Centers for Medicare & Medicaid
Services. https://www.cms.gov/files/document/qso-20-14-nh-revised.pdf
.
144
Center for Medicare & Medicaid Services. (2020). Toolkit on state actions to mitigate COVID-19 prevalence in
nursing homes. https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-homes.pdf
.
145
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
146
Commission members cited communications methods like having 24-hour communication hotlines, granting every
press interview to convey information to the public, and hosting up to 20,000 video chats in one facility.
147
Feldman, V. (2020, March 31). Communicating with patients and families during COVID-19: Five messages to
consider. McKnight’s Long-Term Care News.
https://www.mcknights.com/marketplace/communicating-with-patients-
and-families-during-covid-19-five-messages-to-consider/.
148
MITRE-developed, derived from Commission discussion and/or public input.
149
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
41
3.6 Workforce Ecosystem:
Stopgaps for Resident Safety
The Commission identified five primary problems associated with workforce ecosystem
stopgaps for resident safety.
1. The pandemic has exacerbated long-standing workforce ecosystem (education,
certification/licensure, recruitment, training, retention) challenges.
150,
151
Low wages, high
resident-to-staff ratios,
152
increased pressure to deliver care for residents with complex needs
under difficult conditions, and a dearth of systemic support significantly contribute to current
gaps in care for nursing home residents.
153
2. Direct-providers who work across multiple facilities face an increased risk of SARS-CoV-2
infection; nonetheless, systemic workforce ecosystem problems essentially necessitate
working for multiple employers. A preliminary analysis from CDC concluded that these
professionals—along with direct-care providers continuing to work while sick—helped
hasten the spread of SARS-CoV-2.
154
3. SARS-CoV-2 infection can cause sudden clinical changes that require astute triage,
assessment, intervention, and stabilization and/or transfer of the resident to a higher level of
care. These capabilities fall within the scope of practice of a Registered Nurse (RN),
155
but
they are insufficiently present in nursing homes,
156, 157
especially during overnight and
weekend hours. As a result, Licensed Practical Nurses (LPNs)
158
and Certified Nursing
Assistants (CNAs) are called upon to complete tasks that may fall beyond their scope of
practice.
4. Current regulations require nursing home owners and administrators to designate a part-time,
minimally qualified infection preventionist.
159
This position is traditionally assigned to a
supervisor, nursing manager, or provider as an added (rather than a core) responsibility,
yielding insufficient response to the demands of the current pandemic.
160
5. Workforce educators with expertise in infection prevention and control are insufficiently
used in nursing homes. When employed, nursing home owners and administrators often
contract part-time infection preventionists without educator training and lacking insight into
local nursing home context. This underutilization and insufficient integration of infection
prevention education professionals (IP Educators) has yielded knowledge and skills deficits
among the nursing home workforce—deficiencies that have been compounded by the
pandemic.
161
Maintaining updated standards of care requires dedicated, on-site IP
Educators.
162
Response to Date and Emerging Evidence
CMS Actions to Date. CMS’s distribution of $5 billion for nursing homes from the Provider
Relief Fund authorized by the CARES Act
163
is a potential funding source to hire additional staff
and support existing staff. CMS also issued several informational bulletins to help nursing home

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
42
owners and administrators address resident safety concerns stemming from inadequate infection
prevention and control practices.
164, 165, 166, 167
CMS deployed “strike teams” to assess nursing
homes on infection prevention and control;
168
in practice, however, these strike teams have
focused on verifying competency, rather than providing instruction.
169
Commission Member Discussions. Commission members emphasized at every convening
170
that
CMS must do more to address emergency staffing shortages, including providing hazard pay.
Commission members also highlighted the need for more robust on-site infection prevention and
control oversight, training, and interventions, but added that nursing home owners and
administrators require additional support to implement such measures.
Public Input. Comments frequently
mentioned ensuring the ability to maintain
critical staffing levels during emergencies.
Submitted materials included scholarly
articles reviewing studies from multiple
geographic areas that tied resident outcomes
and infection rates to the staffing levels of
various facilities. The public also noted the
need for enhanced workforce training—
especially in infection prevention and
control—to ensure a constant state of
readiness to respond to outbreaks.
Emerging Evidence. The CDC underscored
that maintaining appropriate staffing levels
is essential to providing a safe working
environment and proper care; it developed guidelines for healthcare facilities to address potential
staffing shortfalls during the pandemic.
171, 172
See Appendix C for additional detailed discussion of the emerging evidence and regulatory
background.
“The direct care staff need
targeted training, adequate
equipment and supplies, stress
and grief support, and access
to paid leave and other
benefits. Addressing these
needs is necessary to ensure
this workforce can provide
continuous, quality care for
nursing home residents in
emergencies and in general.”
-Public Input
Principal Recommendations and Action Steps
The Commission made five principal recommendations related to workforce stopgaps for
resident safety.
Principal Recommendation 6A: Mobilize resources to support a fatigued nursing home
workforce and assess minimum care standards.
Action Steps
• Assess federal relief funds for hazard pay options; advise nursing home owners and
administrators how to access and distribute hazard pay.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
43
• Urge nursing home owners and administrators to incorporate increased
break/recuperation time, as well as time for proper PPE donning and doffing for direct-
care providers as part of emergency-management planning to minimize the physiological
stress of prolonged use of PPE (see Principal Recommendation 8A and associated action
steps for more details).
173
• Reinforce the importance of medical director engagement in nursing home emergency
management planning and execution.
• Assess and adapt existing COVID-19 data collection and analysis to anticipate hotspots,
along with workforce surge needs (see Principal Recommendation 10A and associated
action steps for more details).
• Update existing emergency management plans to reflect emerging workforce shortages
and surge-support resources.
[Collaborate with FEMA and State Departments of Health]
• Update interstate compact language addressing public health emergencies to include
licensed and certified individuals (e.g., CNAs) to support a surge-staffing pool in
hotspots.
[Collaborate with state governments]
• Issue guidance based on recent research
174
that defines updated, acuity-adjusted,
evidence-based, person-centered minimum care standards. These standards should
specify hours of care per resident per day during normal and emergency operations alike,
and require nursing homes to adhere to these standards.
Principal Recommendation 6B: Provide equity-oriented guidance that allows nursing home
workforce members to safely continue to work in multiple nursing homes while adhering to
infection prevention and control practices.
Action Steps
• Develop and distribute guidance for direct care staffing assignment patterns that require
direct care providers to work only with residents testing negative for SARS-CoV-2 or
only with residents testing positive for SARS-CoV-2 across nursing homes within a given
week.
175
This guidance should include the following specifications:
o Diagnostically test direct-care providers before rotating them from caring for
residents with SARS-CoV-2 infection to caring for residents without SARS-CoV-2
infection.
o Direct-care providers should work at no more than two nursing homes during the
pandemic to allow for accurate contact tracing and monitoring.
• Identify federal relief funds to provide paid quarantine-leave options to direct-care
providers testing positive for SARS-CoV-2. Advise nursing homes how to access and
distribute paid leave to those providers during their quarantine.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
44
• Catalyze adoption of evidence-based, equitable, infection prevention and control-oriented
assignment patterns by nursing home administrators and direct-care providers.
176
[Collaborate with national professional associations and organizations representing
nursing homes and/or their staff]
• Develop regulations requiring integration of multi-employer staffing assignment patterns
for into emergency planning.
• Support increased wages for nursing home staff through Medicaid and Medicare payment
reform to disincentivize working for multiple employers.
Principal Recommendation 6C: Support 24/7 RN staffing resources at nursing homes in the
event of a positive SARS-CoV-2 test within that facility.
Action Steps
• Leverage federal relief funds, and coordinate the use of regional health system
resources, to provide 24/7 RN staff augmentation in nursing homes with SARS-CoV-2
incidence among residents.
[Collaborate with state and local authorities]
• Monitor and evaluate mortality and transfer rates of residents who have tested positive
for SARS-CoV-2 when an RN has been consistently present during their care.
• Commission a study to establish an evidence-based standard for specific, competency-
based care requirements during times of normal and emergency operations alike.
Principal Recommendation 6D: Identify and immediately leverage certified infection
preventionists to support nursing homes’ infection prevention needs.
Action Steps
• Identify and deploy infection-preventionist resources to provide immediate assistance to
nursing homes without full-time infection prevention support, prioritizing those nursing
homes in current or anticipated hotspots.
[Collaborate with FEMA, the National Guard, the Public Health Service Corps (USPHC),
infection prevention recruiting companies, and infection prevention professional
organizations (e.g., Association for Professionals in Infection Control (APIC) and/or
Society for Healthcare Epidemiology of America (SHEA)]
Principal Recommendation 6E: Require nursing homes to employ infection preventionist(s)
with educator capabilities.
Action Steps
• Require infection preventionists to have educator capabilities (IP Educators). Require
these IP Educators to provide and document competency-driven, experiential training on
core practice; crisis standards of care, including fit testing of N95 masks and PPE

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
45
donning and doffing; and crisis recovery. Also require regular assessments and
competency achievement of all direct and contract staff (e.g., administrators, nurses,
CNAs, environmental services, maintenance, food service, ancillary staff). Encourage IP
Educators to include residents in this training and counsel.
• Provide templates for IP Educators to track infection prevention and control onboarding
introduction, continuous training, and competency achievement for all staff.
• Develop and distribute to IP Educators competency and self-efficacy measurements for
proper PPE use and reuse.
[Collaborate with CDC]
• Endorse individual infection prevention and control competency assessment and
achievement by all nursing home staff at an 80% threshold or higher.
• Encourage the provision of collaborative technical assistance from infection control and
prevention experts for on-site IP Educators, including support for N95 mask fit testing
(see Recommendation 8A and associated actions steps for more details).
[[Collaborate with state health departments and QIOs]
• Develop partnerships with acute-care and academic facilities to share simulation
resources with nursing homes.
[Collaborate with state and local authorities]
• Encourage state agencies to approve nursing home owners’ and administrators’
applications to use CMP funds for infection prevention and control training costs.
177, 178
• Include audits of IP education provision and participation, and related IP emergency
management protocols, in QAPI programs.
179
• Establish an evidence-based standard for an IP Educator full-time equivalent (FTE) to
bed ratio, including considerations for Health Professional Shortage Areas (HPSA).
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 14 members of the
Commission; 5 members do not endorse Principal Recommendation 6A; 4 members do not
endorse Principal Recommendation 6C; 2 members do not endorse Principal Recommendation
6D; 4 members do not endorse Principal Recommendation 6E; 1 member does not endorse the
report.
150
United States Senate Commission on Long Term Care. (2013). Commission on long-term care: Report to the
Congress. https://catalog.archives.gov/id/7741376
.; Quality Improvement Organizations. (2019, June). Resources to
support staff stability in post-acute and long-term care settings.
https://qioprogram.org/sites/default/files/editors/141/Resources_To_Support_Staff_Stability_20190626_508.pdf;

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
46
Wofford, P. (2019, July 11). Nurses say staffing ratios in long term care facilities are unsafe. Nurse.org.
https://nurse.org/articles/nurse-staffing-unsafe-long-care-facilities/
151
Grabowski, D. & Mor, V. (2020). Nursing home care in crisis in the wake of COVID-19. JAMA. 324(1), 23–24.
doi:10.1001/jama.2020.8524
152
Wofford, P. (2019, July 11). Nurses say staffing ratios in long term care facilities are unsafe. Nurse.org.
https://nurse.org/articles/nurse-staffing-unsafe-long-care-facilities/
153
Coronavirus Commission on Safety and Quality in Nursing Homes. (2020, July 7).
154
McMichael, T. M., Clark, S., Pogosjans, S., Kay, M., Lewis, J., Baer, A., Kawakami, V., Lukoff, M. D., Ferro, J.,
Brostrom-Smith, C., Riedo, F. X., Russell, D., Hiatt, B. Montgomery, P., Rao, A. K., Currie, D. W., Chow, E. J.,
Tobolowsky, F., Bardossy, A. C., … (2020, March 18). COVID-19 in a long-term care facility — King County,
Washington, February 27–March 9, 2020. MMWR Morb Mortal Wkly (Report 2020;69:339-342).
https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e1.htm
155
Registered Nurse (RN) vs. Licensed Practical Nurse (LPN). (2020, August 13). RegisteredNursing.org.
https://www.registerednursing.org/rn-vs-lpn/
156
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 1).
157
ANA nursing staffing requirements to meet the demands of today’s long term care consumer. (2014, November
12). American Nurses Association.
https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-
statements/id/nursing-staffing-requirements-to-meet-the-demands-of-todays-long-term-care-consumer/
158
In a few states, workforce members with equivalent competencies are Licensed Vocational Nurses (LVNs).
Anywhere LPN appears in this document, LVN is implied.
159
42 CFR 483.80 (b)(3) “The facility must designate one or more individual(s) as the infection preventionist(s) (IPs)
who are responsible for the facility's IPCP. The IP must: [ . . .] (3) Work at least part-time at the facility . . .”
160
Flynn, M. (2020, May 26). How nursing homes can bolster infection control – for COVID-19 and beyond. Skilled
Nursing News.
https://skillednursingnews.com/2020/05/how-nursing-homes-can-bolster-infection-control-for-covid-19-
and-beyond/
161
U.S. Government Accountability Office. (2020, May 20). Infection control deficiencies were widespread and
persistent in nursing homes prior to COVID-19 pandemic. https://www.gao.gov/assets/710/707069.pdf
162
Nursing home staff will need to be trained and supported in good infection control. Grabowski, D. C., & Mor, V.
(2020). Nursing Home Care in Crisis in the Wake of COVID-19. JAMA 324(1), 23–24. doi: 10.1001/jama.2020.8524
163
Centers for Medicare & Medicaid Services. (2020, July 22). Trump administration announces new resources to
protect nursing home residents against COVID-19 [Press release].
https://www.cms.gov/newsroom/press-
releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
164
Centers for Medicare & Medicaid Services. (2020, February 6). Information for healthcare facilities concerning
2019 novel coronavirus illness (2019-nCoV). https://www.cms.gov/files/document/qso-20-09-all.pdf
165
Centers for Medicare & Medicaid Services. (2020, March 4). Guidance for infection control and prevention of
coronavirus disease 2019 (COVID-19) in nursing homes.
https://www.cms.gov/medicareprovider-enrollment-and-
certificationsurveycertificationgeninfopolicy-and/qso-20-14-nh.pdf
166
Centers for Medicare & Medicaid Services. (2020, April 2). COVID-19 long-term care facility guidance.
https://www.cms.gov/files/document/4220-covid-19-long-term-care-facility-guidance.pdf
167
Centers for Medicare and Medicaid Services. (2020, May 13). Toolkit on state actions to mitigate covid-19
prevalence in nursing homes.
https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-
homes.pdf
168
Centers for Medicare & Medicaid Services. (2020, July 22). Trump administration announces new resources to
protect nursing home residents against COVID-19 [Press release].
https://www.cms.gov/newsroom/press-
releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
169
Centers for Medicare & Medicaid Services. (2020, August 14). Trump administration has issued more than $15
million in fines to nursing homes during Covid-19 pandemic [Press release].
https://www.cms.gov/newsroom/press-
releases/trump-administration-has-issued-more-15-million-fines-nursing-homes-during-covid-19-pandemic
170
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
171
Centers for Disease Control and Prevention. (2019, July 17). Strategies to mitigate healthcare personnel staffing
shortages. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html
172
Additional pay and support for staff, along with short-term programs to supplement this workforce, will be
necessary. Grabowski, D. C., & Mor, V. (2020). Nursing home care in crisis in the wake of COVID-19. JAMA, 324(1),
23–24. doi:10.1001/jama.2020.8524

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
47
173
Centers for Disease Control and Prevention. (2020, June 10). The physiological burden of prolonged PPE use on
healthcare workers during long shifts [Blog]. https://blogs.cdc.gov/niosh-science-blog/2020/06/10/ppe-burden/
174
If recent research does not exist, commission a study to establish this evidence base.
175
MITRE-developed, derived from Commission discussion and/or public input.
176
MITRE-developed, derived from Commission discussion and/or public input.
177
State CMP funds may be reinvested to support activities that benefit nursing home residents and that protect or
improve their quality of care or quality of life. Centers for Medicare & Medicaid Services. (2020, August 7). Civil
money penalty reinvestment program. https://www.cms.gove/Medicare/Provider-Enrollment-and-
Certification/SurveyCertificationGenInfo/LTC-CMP-Reinvestment
178
MITRE-developed, derived from Commission discussion and/or public input.
179
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
48
3.7 Workforce Ecosystem:
Strategic Reinforcement
The Commission identified three primary problems associated with workforce ecosystem
strategic reinforcement.
1. CNAs spend more time with nursing home residents—including residents with additional
COVID-19 care needs—than other members of the workforce, yet they earn the lowest
wages among direct-care providers and receive few (if any) benefits.
180
CNA turnover rates
can also be close to 100% in some cases.
181
Moreover, the pandemic has disrupted CNA
training critical for reinforcing the nursing home workforce, leading to serious CNA
workforce deficits.
182
2. There are no national standards for training and licensure requirements of infection
preventionists that nursing homes are mandated to employ.
3. Efforts to address workforce ecosystem challenges have been delayed, further jeopardizing
an already fragile nursing home system. In addition to low pay and limited benefits, the
potential of an emerging workforce is restrained by the combination of a lack of educational
support (e.g., limited assistance in progressing into LPN/RN training), insufficient
competency standards, low- to no exposure to geriatrics in formal education programs, and
limited opportunities for professional advancement (e.g., no clinical ladder or lattice).
183
“There should be more
standardization of the
curriculum across the
country to make sure that
the infection preventionist
had (sic) adequate
competency in this really
important job.”
-Commission Member
Response to Date and Emerging Evidence
CMS Actions to Date. CMS issued two blanket waivers addressing nursing assistant training and
certification to reduce barriers for hiring and retaining CNAs.
184
The waivers provide flexibility
at the federal level, but state occupational licensing and state regulatory agencies have to approve
the temporary hiring of nursing assistants—and only certain states have done so.
Commission Member Discussions. Commission
members highlighted throughout their convenings
185
that CMS must immediately launch a multi-faceted
approach to strengthen the entire nursing home
workforce pipeline in order to meet staffing-
reinforcement needs in the near term.
Public Input. Public comments supported unified
national training for nursing home staff, and called for
additional funding to incentivize people to join and
stay in the nursing home workforce.
Emerging Evidence. Deaths among nursing home staff
during the pandemic illustrate how dangerous these
jobs have become.
186
Future nursing home professionals must be equipped with knowledge,

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
49
skills, and resources to protect themselves and the residents for whom they will care, and
immediate and ongoing systemic efforts must bolster workplace safety.
See Appendix C for additional detailed discussion of the emerging evidence and regulatory
background.
Principal Recommendations and Action Steps
The Commission made four principal recommendations related to strategic reinforcements for
the workforce.
Principal Recommendation 7A: Catalyze interest in the CNA profession through diverse
recruitment vehicles; issue guidance for on-the-job CNA training, testing, and certification; and
create a national CNA registry.
Action Steps
• Include content and relevant links related to CNA careers and certification in the
administration’s “Find Something New” campaign website.
187
• Develop and implement a National CNA Community of Excellence recruitment
campaign.
[Collaborate with CNA professional associations (e.g., National Association of Health
Care Assistants (NAHCA))]
• Develop a public/private partnership with relevant industry partners and academia to
promote and amplify the CNA Community of Excellence campaign.
• Permit nursing homes to hire personnel that are qualified to attend and complete CNA
on-site, continuous training; and provide them with rigorous, on-site, developmentally
and linguistically appropriate,
188
culturally mindful,
189
literacy-oriented
190, 191
CNA
training, testing, and certification using current (i.e., pre-waiver) state education
standards and testing for nursing assistant certification. Involve residents, essential care
partners, and family members as user experts complementing on-site instruction for
CNAs in training.
• Require that nursing homes training CNAs on-site have these staff members work under
supervision during their probationary period (i.e., until completion of their on-site
training, testing, and certification); require nursing homes to track the progress of these
staff members; and require nursing homes to recognize (e.g., graduation ceremony with
residents in attendance) when CNAs have officially completed their on-site training,
testing, and certification requirements.
• Assess targeted federal funds for on-site CNA training facilitation and materials; advise
nursing homes how to access and distribute these funds.
• Monitor on-site training programs for CNAs and their subsequent performance to verify
effectiveness (e.g., standard of care, retention rates, continued education).
[Collaborate with academia and foundations]

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
50
• Accurately track CNA workforce retention growth (e.g., individual continuing education
and CNA profession growth).
192
[Collaborate with academia and the Bureau of Labor Statistics]
Principal Recommendation 7B: Professionalize infection prevention positions in nursing
homes by updating regulations at 42 CFR § 483.80 so more fully qualified infection
preventionists are available to serve in nursing homes.
Action Steps
• Leverage current training programs to develop and provide a standardized, required,
regularly updated training curriculum and certification for infection preventionists in
nursing homes at no cost to nursing homes. Consider using the following established
programs:
o CDC’s Nursing Home Infection Prevention Training Course
o APIC materials, including:
EPI in Long-Term Care Certificate Program
EPI Intensive Certificate Program
Certified Infection Control (CIC) certification preparation materials, including the
Infection Preventionist Certification Review Online Course
Basics of Infection Prevention and Control for Non-Clinicians Training Course
o SHEA’s Podcast Series: Infection Control in Long-Term Care Facilities
o SHEA/CDC Outbreak Response Training Program (ORTP)
o Certification Board of Infection Control and Epidemiology’s (CBIC) CIC process
o American Health Care Association’s (AHCA) Infection Preventionist Specialized
Training
• Create a national registry of infection preventionists certified by this program to identify
emergency reinforcement support for nursing homes without full-time infection
prevention support.
Principal Recommendation 7C: Catalyze the overhaul of the workforce ecosystem in
partnership with federal, SLTT, other public, private, and academic partners.
Action Steps
• Establish a competitive grant program and/or national scholarship to fund entry into
practice education for aspiring CNAs.
[Collaborate with AHRQ]
• Identify and work to achieve funding mechanisms that defer/reimburse CNA and LPN
education costs after three years of service in nursing homes.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
51
• Identify and/or re-examine core competencies for long-term care direct-care providers;
use these competencies to develop and/or update national training programs and
standards (e.g., Nurse Aid National Training and Competency Evaluation Program).
[Collaborate with CDC and OSHA]
• Modify RN, LPN, and CNA clinical training standards for certification and licensure;
include a clinical rotation in a long-term care setting in order to supplement staffing and
provide immersion into geriatric care and care for other specialty populations.
[Collaborate with ANA, NAHCA, trade schools, universities, and state
certification/licensure authorities]
• Develop a meaningful national clinical ladder and lattice for long-term direct care
providers—including CNAs, LPNs, and RNs—that includes access to career
advancement opportunities and improved compensation.
[Collaborate with professional nursing associations and organizations]
Principal Recommendation 7D: Convene a Long-Term Care Workforce Commission to assess,
advise on, and provide independent oversight for modernization of workforce ecosystem.
193
Action Step
• Develop a charter and criteria for identifying potential stakeholders to participate in the
Long-Term Care Workforce Commission and/or Advisory Board.
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 22 members of the
Commission; 2 members do not endorse Principal Recommendation 7A; 1 member does not
endorse the report.
180
PHI. (2019, September 3). U.S. nursing assistants employed in nursing homes. https://phinational.org/resource/u-
s-nursing-assistants-employed-in-nursing-homes-key-facts-2019/
181
Quality Improvement Organizations. (2019, June). Resources to support staff stability in post-acute and long-term
care settings.
https://qioprogram.org/sites/default/files/editors/141/Resources_To_Support_Staff_Stability_20190626_508.pdf
182
Coronavirus Commission on Safety and Quality in Nursing Homes. (2020, July 14).
183
Long-Term Care Commission Report; PHI. (2019, September 3). U.S. nursing assistants employed in nursing
homes. https://phinational.org/resource/u-s-nursing-assistants-employed-in-nursing-homes-key-facts-2019/
184
Centers for Medicare & Medicaid Services. (2020, March 6). COVID-19 emergency declaration blanket waivers for
health care providers. https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-waivers.pdf
185
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
186
McGarry, B., Porter, L., & Grabowski, D. (2020, July 28). Nursing home workers now have the most dangerous
jobs in America. They deserve better. Washington Post.
https://www.washingtonpost.com/opinions/2020/07/28/nursing-home-workers-now-have-most-dangerous-jobs-
america-they-deserve-better/
187
MITRE-developed, derived from Commission discussion and/or public input.
188
Gentry, R., Sallie, A., & Sanders, C. (2013). Differentiated instructional strategies to accommodate students with
varying needs and learning styles. The Urban Education Conference. https://files.eric.ed.gov/fulltext/ED545458.pdf
.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
52
189
Velott, D., Forte, K., S. (2019, March 5). Toward health equity: Mindfulness and cultural humility as adult
education. New Directions for Adult and Continuing Education, 161, 57-66.
https://onlinelibrary.wiley.com/doi/full/10.1002/ace.20311
190
Baur, C. (2011). Calling the nation to act: Implementing the national action plan to improve health literacy. Nursing
Outlook, 59(2), 63-69. https://www.sciencedirect.com/science/article/pii/S0029655410004793?viewFullText=true
191
Egbert, N. & Nanna, K. (2009, September 30). Health literacy: Challenges and strategies. OJIN, 14(3).
https://ojin.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/OJIN/TableofContents/Vol14200
9/No3Sept09/Health-Literacy-Challenges.html
192
MITRE-developed, derived from Commission discussion and/or public input.
193
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
53
3.8 Technical Assistance and
Quality Improvement
The Commission identified the following primary problem associated with technical assistance
and quality improvement.
1. To date, QIOs have begun assisting 9,000 of the 15,400 certified nursing homes in the
country.
194, 195
However, technical assistance and quality improvement support have not been
sufficiently available at nursing homes during the pandemic. QIOs provide toolkits,
information guides, and online learning options; nevertheless, nursing homes need proactive,
tailored, timely, and on-the-ground support in emergency management, infection prevention
and control, and workforce capability development.
196,
197
Response to Date and
Emerging Evidence
CMS Actions to Date. Nursing homes with
COVID-19 outbreaks receive on-site and
online technical assistance and education.
198,
199
Commission Member Discussion.
Commission members recommended calling
on QIOs to provide more on-site training and
assistance to nursing homes—specifically
those in infection hotspots—to improve
resident care and outcomes. One commission
member recommended increasing the
number of QIOs so that each could serve a
smaller segment of the country (and thus increase services to the smaller number of nursing
homes).
200
In addition, the Commission recommended creating COVID-19 QAPI tools for
nursing homes.
Public Input. Public comments noted the lack of data reporting in some areas due to
disincentives to report. Suggestions included a call for additional federal and state guidance with
regard to ratings and survey processes for nursing homes to increase consistency and
comparability.
Emerging Evidence. See Appendix C for additional detailed discussion of the emerging evidence
and regulatory background.
“CMS should continue to hold
routine discipline specific
COVID-19 calls. These calls
have provided a great
opportunity for providers to
hear directly from CMS as well
as ask questions and raise
pertinent issues, concerns or
points of clarifications and
receive responses in real time.”
-Public Input

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
54
Principal Recommendation and Action Steps
Principal Recommendation 8A: Identify and work to achieve funding mechanisms for—or
reprioritize activities of—technical assistance providers and other contractors to increase the
availability of collaborative, on-site, data-driven, and outcomes-oriented support prior to, during,
and after a public health emergency.
"In this pandemic
situation, we all have
to take responsibility
to collaborate and
share learnings to get
through this."
-Commission Member
Action Steps
• Redirect, prepare, and coordinate with regional
strike teams, QIN-QIOs, and other technical
assistance contractors to offer expanded, outcomes-
oriented, on-the-ground technical assistance with
organizational diagnosis, strategic direction,
organizational resilience, resource prioritization,
emergency-management assistance, data-
management assistance, and workforce capability
development in infection prevention and control, trauma-informed care, person-centered and
person-directed care, visitation, and/or family communications and engagement.
• Research and provide examples of federal and regional strike teams providing technical
assistance and quality improvement support.
• Support QIN-QIO technical assistance work with nursing homes and reinforce a culture of
learning by grounding information about citations and penalties in QAPI methods.
• Create and distribute an organizational-level QAPI tool on how to effectively respond to
COVID-19 and future pandemics.
• Remind nursing home administrators to use QAPI tools, data, and methods to improve their
performance.
• Provide instruction to state surveyors on Focused Infection Control (FIC) rules and survey
process, including information about when surveyors should provide nursing homes with
immediate feedback.
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 23 members of the
Commission; 1 member does not endorse Principal Recommendation 8A; 1 member does not
endorse the report.
194
Centers for Medicare and Medicaid Services. (2020, July 20). Trump Administration Announces New Resources
to Protect Nursing Home Residents Against COVID-19.
https://www.cms.gov/newsroom/press-releases/trump-
administration-announces-new-resources-protect-nursing-home-residents-against-covid-19

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
55
195
Centers for Medicare and Medicaid Services. (2020, August 25). Trump Administration Launches National
Training Program to Strengthen Nursing Home Infection Control Practices.
https://www.cms.gov/newsroom/press-
releases/trump-administration-launches-national-training-program-strengthen-nursing-home-infection-control
196
Coronavirus Commission for Safety and Quality in Nursing Homes. (July 7, 2020).
197
Coronavirus Commission for Safety and Quality in Nursing Homes. (July 21, 2020).
198
Centers for Disease Control and Prevention (2019). Nursing Home Infection Preventionist Training Course.
www.cdc.gov/longtermcare/training.html
199
Quality Improvement Organizations (2020). CMS-CDC Fundamentals of COVID-19 Prevention for Nursing Home
Management. https://qioporgram.org/demand-trainings-nursing-home-resources
200
Coronavirus Commission for Safety and Quality in Nursing Homes. (July 7, 2020).

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
56
3.9 Facilities
The Commission identified two primary problems associated with nursing home facilities.
1. The physical environment (e.g., structure of resident rooms; architecture and layout of
nursing homes; heating, ventilation, and air conditioning [HVAC] systems) of many nursing
homes is not optimally designed to limit spread of transmissible diseases.
201
2. Fundamental design changes are costly and may take longer to implement. but are necessary
due to the prolonged risks to residents from COVID-19 and the need to position facilities to
manage future epidemics.
As the fall season approaches, design adaptation
will take on increased importance and urgency
with respect to physical-distancing practices that
depend on use of outdoor space. Outdoor
visitation, for example, will be neither safe nor
practical in colder weather.
“When nursing homes are built,
the ideal is private rooms with
three fixture bathrooms. Of
course, the expense of building
that model is often prohibitive,
so the infrastructure we have in
place is often buildings from the
70’s with long institutional
corridors and mostly semi-
private rooms. Newer homes
that are built try to include more
privacy and a homelike
character, but financing is
difficult for this level of care, so
compromises are made in order
to build or renovate at all...”
-Public Input
Response to Date and Emerging Evidence
CMS Actions to Date. CDC has issued iterative
recommendations that nursing homes identify
space in their facilities that could be dedicated to
preventing and controlling COVID-19.
202
On
July 9, CMS waived requirements under 42 CFR
§483.90 to allow alternate facilities to be
certified as SNFs in order to facilitate isolation of
residents with COVID-19 disease.
203
CMS
guidance notes that the Medicare Conditions of
Participation and interpretive guidance with
respect to the Life Safety Code provide
information regarding modifications to the
physical plant to reduce infection risk.
204
Commission Member Discussions. During the Commission convenings,
205
members spoke at
length about the need for long-term solutions to improve the physical layout of nursing homes to
better control the spread of communicable diseases. The Commission and public input alike
highlighted the priority of single-occupancy rooms,
206
but the current financial model does not
support this. In the near term, the Commission noted the lack of physical space as a limitation to
making changes to the physical layout. Additionally, the Commission noted that modifications or
upgrades to HVAC systems and other adaptations are costly and would require supplemental
funding in many cases.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
57
Public Input. Public comments noted how design can support cohorting practices while
maintaining the social and emotional health of residents.
Emerging Evidence. In a previous outbreak of a respiratory virus in a long-term care facility,
lack of available space within the facility was identified as one of the challenges associated with
cohorting symptomatic residents.
207
Furthermore, a study of an influenza outbreak in a four-
building nursing home suggested that current architectural design and HVAC systems may
increase disease transmission.
208
Out of four buildings, the influenza rate was lowest in the
building with more space (square feet) per resident and featuring a unique HVAC system.
Nursing home architecture and layout often prioritizes quality of life (e.g., establishing family
units
209
) and resident safety (preventing falls
210
or wayfinding
211
) rather than infection
prevention and control (e.g., single-occupancy rooms, improved HVAC systems). Designs
should take into consideration psychosocial factors, physical safety, and infection prevention
needs for residents. Design modifications made in response to COVID-19 ideally would not
degrade or disrupt layout elements that promote quality of life and safety.
Principal Recommendations and Action Steps
The Commission made three principal recommendations in this area.
Principal Recommendation 9A: Identify and share with nursing homes short-term facility
design enhancements to address immediate pandemic-related risks that can be implemented at
minimal cost.
Action Steps
• Close information gaps on how to modify the physical plant by gathering best practices and
issuing guidance on design enhancements.
[Collaborate with the CDC, the Environmental Protection Agency (EPA), and other federal
partners]
Examples include:
o Resident rooms: The ability to physically separate residents is greatly enhanced when
rooms are occupied by only a single resident.
o HVAC and air flow: modification and upgrades to HVAC systems further harden the
infrastructure and potentially limit transmission.
• Work with CDC to supplement its guidance for the manipulation of HVAC systems that can
reduce risk of transmission by:
o Adjusting existing systems to support infection control (e.g., creating negative
pressure, replacing filters)

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
58
o Supplementing systems with equipment that can further purify air (e.g., air ionization,
air scrubbers)
o Setting standards for HVAC system performance as part of the long-term plan to
upgrade systems and redesign nursing homes
• Encourage nursing homes to assign residents to single-occupancy rooms in facilities that can
accommodate this approach without detrimental reduction in census. Examine changes to the
CMS reimbursement that would promote single occupancy (temporarily during pandemic as
well as in the long term).
Principal Recommendation 9B: Establish a collaborative national forum to identify and share
best practices and recommendations; facilitate real-time learning on how to best use existing
physical spaces. (Please refer to action steps following 9C.)
Principal Recommendation 9C: Collaboratively establish long-term priorities and seek
appropriate funding streams for nursing homes to redesign and/or strengthen facilities against
infectious diseases.
212
Action Steps
• Establish a commission or task force, jointly led by industry, safety and consumer
organizations, to identify long-term priorities for nursing care with emphasis on the design,
redesign, retrofitting, and reconfiguration of nursing homes to be resilient to infectious
disease threats.
213
Topics to be considered include, but are not limited to:
o The ability to designate separate wings for cohorting
o Separate entrances and exits
o Separate restrooms and break areas for staff
o Separate areas to don and doff PPE
o Ultraviolet light systems for decontamination
o HVAC upgrades and retrofitting
o Design considerations that take resident quality of life and leisure into consideration
• Consider forming a public/private partnership that issues a challenge for nursing home
redesign.
214
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 24 members of the
Commission; 1 member does not endorse the report.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
59
201
Harrison, S. (2020, May 25). Some nursing homes escaped COVID-19—Here's what they did right. Wired.
https://www.wired.com/story/some-nursing-homes-escaped-covid-19-heres-what-they-did-right/
202
Centers for Disease Control and Prevention. (2020, June 25). Preparing for COVID-19 in nursing homes.
https://www.cdc.gov/coronavirus/2019-ncov/hcp/long-term-care.html
203
Centers for Medicare & Medicaid Services. (2020, July 9). Long term care facilities (skilled nursing facilities and/or
nursing facilities): CMS flexibilities to fight COVID-19.
https://www.cms.gov/files/document/covid-long-term-care-
facilities.pdf
204
CMS technical input, August 26, 2020.
205
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 7).
206
Plucinski, M.M., Wallace, M., Uehara, A., Kurbatova, E. V., Tobolowsky, F. A., Schneider, Z. D., Ishizumi, A.,
Bozio, C.H., Koboyashi, M., Toda, M., Stewart, A., Wagner, R. L., Moriarty, L. F., Murray, R., Queen, K., Tao, Y.,
Paden, C., Mauldin, M. R., Zhang, J., … . (2020, August 12). COVID-19 in Americans aboard the Diamond Princess
cruise ship [Accepted manuscript]. Clinical Infectious Diseases.
https://academic.oup.com/cid/advance-
article/doi/10.1093/cid/ciaa1180/5891779#.XzmzSCFyVfg.twitter
207
Spires, S. S., Talbot, H. K., Pope, C. A., & Talbot, T. R. (2017). Paramyxovirus outbreak in a long-term care
facility: The challenges of implementing infection control practices in a congregate setting. Infection Control and
Hospital Epidemiology, 38(4), 399-404. doi: https://10.1017/ice.2016.316
208
Drinka, P. J., Krause, P., Schilling, M., Miller, B. A., Shult, P., & Gravenstein, S. (1996). Report of an outbreak:
Nursing home architecture and influenza-A attack rates. Journal of the American Geriatrics Society, 44(8), 910-30.
https://pubmed.ncbi.nlm.nih.gov/8708299/
209
Chang, Y. P., Li, J., & Porock, D. . (2013). The effect on nursing home resident outcomes of creating a household
within a traditional structure. Journal of the American Medical Directors Association, 14(4), 293-99.
https://pubmed.ncbi.nlm.nih.gov/23434319/
210
Hill, E. E., Nguyen, T. H., Shaha, M., Wenzel, J. A., DeForge, B. R., & Spellbring, A. M. . (2009 October). Person-
environment interactions contributing to nursing home resident falls. Research in Gerontological Nursing, 2(4), 287-
96. https://pubmed.ncbi.nlm.nih.gov/20077985/
211
Marquadt, G. (2011). Wayfinding for people with dementia: a review of the role of architectural design. HERD 4(2),
75-90. https://pubmed.ncbi.nlm.nih.gov/21465436/
212
MITRE-developed, derived from Commission discussion and/or public input.
213
MITRE-developed, derived from Commission discussion and/or public input.
214
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
60
3.10 Nursing Home Data
The Commission identified three primary problems associated with nursing home data.
1. The time and cost required for nursing homes to report COVID-19-related data to the federal
government is not consistently offset by benefits to nursing home residents, families, or staff.
For example, nursing homes continue to lack sufficient PPE despite reporting these shortages
to CMS.
215
2. Nursing homes are required to report multiple types of data to various federal and state
authorities, which is complex and time-consuming. In addition, data and information released
to nursing homes by CMS and its federal partners has been at times inconsistent, and released
and accessible via multiple websites. These issues make it challenging for nursing homes to
comply with reporting requirements, and difficult for staff to be sure they are accessing the
most relevant, trustworthy, and up-to-date data and guidance. The situation continues to
rapidly evolve, and some initial efforts have been made by CMS and its federal partners to
consolidate information. Nevertheless, a more cohesive approach is needed to streamline data
collection and information dissemination.
216
3. The lack of consistent nursing home data standards and interoperability can hinder data
management and data sharing between providers and payers, delay effective care delivery,
and result in poor data integration across care settings.
217, 218
Further discussion of data
limitations related to nursing homes appears at Appendix H.
Response to Date and Emerging Evidence
CMS Actions to Date. Findings from a Government Accountability Office report noted the need
for CMS to make ongoing improvements in how nursing home data are collected, compiled, and
reported publicly.
219
CMS has taken some steps to address these issues, including updating the
CMS Nursing Home Compare website and Five-Star Quality Rating System.
220, 221
CMS and
CDC are refining and creating greater specificity for certain COVID-19 NHSN data elements,
such as gathering more details related to testing.
222
Furthermore, CMS and its federal partners
are taking action based on data that nursing homes report to the NHSN system. Between July 18
– 20, CMS and federal partners began deploying Task Force Strike Teams to provide technical
assistance to select nursing homes with increased cases.
223
CMS is also using this data as part of
the weekly “Governor’s report” so that states can direct support to the highest-risk nursing
homes.
224
Data from state and local health departments will continue to be important as well.
CMS and CDC established a resource that provides access to the COVID-19 Public File
containing data reported by nursing homes to NHSN, as well as related resources and
statistics.
225
CMS has released iterative guidance requiring facilities to report information about
communicable diseases, healthcare-associated infections, and potential outbreaks to CDC in a
standardized format.
226, 227
CMS also requires nursing homes to report COVID-19 facility data to
the CDC as well as residents, their representatives, and their families. Further, CMS updated
several surveys and related tools to reflect COVID-19 reporting requirements.
228

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
61
Commission Member Discussions. Commission members
229
supported obtaining data from, and
releasing information to, nursing homes that can be acted upon in a meaningful way, while also
considering the associated time and costs of data collection.
During a Commission convening on July 29, CMS reported that it has begun developing a new
consolidated source of guidance and other relevant information.
230
Commission members
generally supported efforts to develop a central location for nursing homes to submit COVID-19
data, and to find essential information from CMS and its federal partners.
Public Input. Public comments noted the importance of providing a centralized collection and
reporting hub for easy access by stakeholders looking to make informed and coordinated
decisions. Other input focused on the importance of providing additional data context to enhance
predictive ability of nursing homes for planning and coordination with other health facilities.
Emerging Evidence. See Appendix C for additional discussion of the emerging evidence and
regulatory background.
Principal Recommendations and Action Steps
The Commission made three principal
recommendations to improve the availability and
usefulness of nursing home data.
Principal Recommendation 10A: Standardize
COVID-19 data elements, improve data collection,
and identify supportive actions that CMS and
federal partners will take in response to key
COVID-19 indicators based on nursing home-
reported data.
“[We need] streamlining
of multiple guidance on
state and federal level, as
well as reporting. And if
we can achieve this, that
would free up resources
to really do some of the
other items that have
been identified throughout
[this commission].”
-Commission Member
Action Steps
• Further standardize existing data elements,
improve current survey questions,
231
and incorporate additional elements into the NHSN
dataset that are essential for improved clinical outcomes and quality care delivery but not
yet adequately captured in other existing reporting systems (e.g., MDS and PBJ). This
data may include turnaround times on diagnostic tests, infection-control measures, and
detailed staffing data (e.g., staff providing housekeeping services).
[Collaborate with CDC]
• Capture more-targeted data and identify corresponding actions related to the experiences,
perspectives, and other issues shared by residents, families, and staff. Focus on data
related to demographics, visitation, satisfaction, quality of life, depression, and basic
behavioral needs (e.g., resident access to a phone).
• Develop threshold criteria for key data indicators (e.g., positive COVID-19 test results,
deaths, low PPE supplies, staffing requirements) that will trigger coordinated responses
by CMS, state and federal partners, and nursing homes. These indicator thresholds should

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
62
be integrated into relevant policies and updated based on evolving evidence.
232
[Collaborate with state and local authorities]
• Leverage actionable NHSN data about equipment and supplies to assist with coordination
of available resources and support for screening, testing, cohorting, training, and
equipment needs at a national level.
• Provide clear guidance on appropriate uses of data to support facilities while recognizing
the need to ensure quality and safety standards.
• Collect and analyze COVID-19 data that was reported by nursing homes to state and
local authorities during the period from the beginning of the pandemic until the nationally
required reporting of these data to the NHSN system was formally mandated on May 8.
Establish a national data clearinghouse to make this data and its analysis available to the
research community and general public. As feasible, include in this clearinghouse
additional data for this timeframe that nursing home owners and administrators may
voluntarily share directly with the clearinghouse.
233
[Collaborate with CDC and other federal partners]
Principal Recommendation 10B: Create an easy-to-use, intuitive, and interactive technical
infrastructure for nursing homes that streamlines the process of data reporting and consolidates
dissemination of essential policy guidance, information about updated regulations, and other
communications.
Action Steps
• Define and prioritize features and capabilities of the new streamlined technical
infrastructure.
234
[Collaborate with health information technology (HIT) resources, vendors, and nursing
home owners and administrators]
• Develop a secure method for nursing homes to enter new data and correct previously
submitted data.
• Provide dynamic, real-time, mobile-friendly, HIPAA-compliant, and actionable feedback
reports to nursing homes and federal partners based on the data entered or queried. The
reporting elements should include, but are not limited to, clinical and performance
metrics, resource utilization, survey responses, inspection data, and information related
to the well-being of residents.
• Integrate a COVID-19 toolkit into the technical infrastructure to include an interactive
map of states with the current applicable metrics, mandates, and guidance.
Principal Recommendation 10C: Enhance HIT interoperability to facilitate better
communication, improve quality measurement standards, and coordinate integration of nursing
home data with data from other health organizations.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
63
Action Steps
• Develop interoperability and communication standards to integrate nursing home data
with data from other health organizations, as demonstrated by ONC’s Health IT
Certification Program in the electronic health record (EHR) market.
235
[Collaborate with the Office of the National Coordinators for Health Information
Technology (ONC)]
• Incentivize nursing homes to adopt health information technology (HIT) to standardize
data collection, transmission, and management to support health information exchange
and access to comprehensive EHRs by care providers across settings. (Note: A
Commission member does not support incentives for the use of HIT; since it is not new,
its adoption should be a business decision on the part of the owners and administrators.)
• Promote interoperability standards across nursing homes.
• Assess data needs and leverage data assets.
[Collaborate with state and local authorities]
• Foster collaboration, data transparency, and information-sharing across health
organizations and information technology vendors. (Note: Some Commission members
feel strongly that if nursing homes are encouraged to contribute to data transparency,
CMS should ensure protection of the facilities and healthcare providers through federal
rules.)
Statement on Commission Endorsement
The recommendations and action steps of this theme have been endorsed by 24 members of the
Commission; 1 member does not endorse the report.
215
Rau, J. (2020, June 11). Nursing homes run short of covid-19 protective gear as federal response falters. NPR.
https://www.npr.org/sections/health-shots/2020/06/11/875335588/nursing-homes-run-short-of-covid-19-protective-
gear-as-federal-response-falters
216
Coronavirus Commission for Safety and Quality in Nursing Homes. (2020, July 21).
217
Mohamoud, S., Byrne, C., & Samarth, A. (2009, October). Implementation of health information technology in
long-term care settings: Findings from the health it portfolio. Agency for Healthcare Research and Quality.
https://digital.ahrq.gov/sites/default/files/docs/page/08-0087-EF.pdf
218
Heny, J., Pylpchuk. Y., & Patel, V. (2018, November). Electronic health record adoption and interoperability
among U.S. skilled nursing facilities and home health agencies in 2017 (Report No. 41). The Office of the National
Coordinator for Health Information Technology. https://www.healthit.gov/sites/default/files/page/2018-11/Electronic-
Health-Record-Adoption-and-Interoperability-among-U.S.-Skilled-Nursing-Facilities-and-Home-Health-Agencies-in-
2017.pdf?platform=hootsuite
219
Dicken, J. E. (2018, September 6). Nursing home quality: Continued improvements needed in CMS’s data and
oversight. Government Accountability Office. https://www.gao.gov/assets/700/694324.pdf
220
Centers for Medicare & Medicaid Services. (2019, March 5). CMS improving nursing home compare in April 2019
[Press release]. https://www.cms.gov/newsroom/press-releases/cms-improving-nursing-home-compare-april-2019

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
64
221
Wright, D. (2019, October 7). Consumer alerts added to the Nursing Home Compare website and the Five Star
Quality Rating System. Centers for Medicare and Medicaid Services.
https://www.cms.gov/Medicare/Provider-
Enrollment-and-Certification/SurveyCertificationGenInfo/Downloads/QSO-20-01-NH.pdf
222
Wisconsin Health Care Association. (2020, August 14). NHSN updates instructions and adds testing to resident
impact and facility capacity pathway.
https://www.whcawical.org/publications/care-connection/august-14-2020/nhsn-
updates-instructions-and-adds-testing-to-resident-impact-and-facility-capacity-pathway/
223
Centers for Medicare & Medicaid Services. (2020, July 22). Trump administration announces new resources to
protect nursing home residents against COVID-19 [Press release].
https://www.cms.gov/newsroom/press-
releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
224
Ibid.
225
Ibid.
226
Wright, D. R. (2020, March 13). Guidance for infection control and prevention of coronavirus disease 2019
(COVID-19) in nursing homes (REVISED). Centers for Medicare & Medicaid Services.
https://www.cms.gov/files/document/3-13-2020-nursing-home-guidance-covid-19.pdf
227
Wright, D. R. (2020, April 19). Upcoming requirements for notification of confirmed COVID-19 (or COVID-19
persons under investigation) among residents and staff in nursing homes. Centers for Medicare & Medicaid Services.
https://www.cms.gov/files/document/qso-20-26-nh.pdf
228
Wright, D. R. (2020, May 6). Interim final rule updating requirements for notification of confirmed and suspected
covid-19 cases among residents and staff in nursing homes. Centers for Medicare and Medicaid Services.
https://www.cms.gov/files/document/qso-20-29-nh.pdf
229
Coronavirus Commission on Safety and Quality in Nursing Homes (2020, July 21).
230
Coronavirus Commission for Safety and Quality in Nursing Homes. (2020, July 29).
231
An example of an improvement offered by a Commission member would be to the NHSN survey of facilities
around testing, PPE, and staffing. The PPE and staffing questions only measure extreme shortages. Commission
member feedback to draft report, August 24, 2020.
232
MITRE-developed, derived from Commission discussion and/or public input.
233
Emergency Support for Nursing Homes and Elder Justice Reform Act of 2020, S. 4182, 116 Cong., 2d Sess.
(2020).
https://www.finance.senate.gov/imo/media/doc/116.S.4182%20-
%20Emergency%20Nursing%20Home%20Relief%20and%20Elder%20Justice%20Reform%20Act%20of%202020%
20bill%20text.pdf
234
MITRE-developed, derived from Commission discussion and/or public input.
235
MITRE-developed, derived from Commission discussion and/or public input.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
65
4 Securing the Future of Long-Term Care
The Commission based its work on lessons learned from the early days of the pandemic, and it
envisions future actions by CMS and its federal partners to improve infection prevention and
control, safety, and quality within nursing homes. Unless accompanied by sustainable, systems-
level change addressing the issues discussed in the report (Background), however, these
recommendations will likely be inadequate to enable nursing homes to prevent the next crisis.
Nursing homes (and long-term care in general) need to be reimagined to ensure they can protect
the safety and foster the well-being of some of the most vulnerable members of our population—
older adults and people with disabilities. This conclusion discusses five key areas for long-term
improvement.
4.1 Strategic Workforce Planning
It is impossible to ensure quality care for and safety of residents without first supporting their
direct-care providers. Strengthening the nursing home workforce and supporting other resident
care partners involves many dimensions, but a primary area of focus must be CNAs. These
professionals serving on the front lines of care delivery are generally underpaid, receive few if
any benefits, and have little to no opportunity for career advancement.
The Commission recommends that CMS partner with experts across government components
(federal and SLTT), private leaders, and academic experts to convene a Strategic CNA
Workforce Planning Council that will realize the promise of the data-driven, CNA-oriented
advice that may emerge from the proposed Long-Term Care Commission (Section 3.7). This
new council should work to articulate the present and future projections for CNAs, and develop a
plan for training, recruitment, retention, and growth for these professionals. The council should
also assess the cultural aspects that disincentivize and devalue the prospect of working in a
nursing home. Commission members often remarked that the outside world does not value the
labor and investment of CNAs and other providers, thus contributing to their turnover. Therefore,
this strategic CNA workforce planning should encompass extrinsic and intrinsic benefits alike,
especially within the context of the entire workforce system.
With CMS leading these actions, the CNA workforce of the future will be more competent, more
capable of providing high-quality care, and encouraged to remain in these roles or to grow along
a career track, actualized by the satisfaction they derive from the meaningful work they
contribute to residents, their families, and our society.
4.2 Interoperable Data, Real-Time Predictive Modeling, and
Communications Technology
The United States needs to develop a national strategy to improve the data available within and
across nursing homes. Data about residents and facilities is often siloed and incomplete. Nursing
homes (especially independent ones) are often under-resourced to address these issues.
Technology within nursing homes is often outdated and insufficient, hindering not only data-
related activities of staff but also communications that may provide vital linkages between
residents and the larger community. Many nursing homes will need coordinated federal and

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
66
SLTT support (including funding) to bring their systems and capabilities in line with the 21st
century.
Assessing quality and outcomes in any healthcare setting depends on accurate and
comprehensive data. During the pandemic, some stakeholders proposed collecting additional
data, such as leveraging the existing MDS for SNF residents to capture data specific to COVID-
19.
236
COVID-19 highlighted the immediate need for better and more timely data related to care
processes, staffing, infection rates, deaths, and other issues; nevertheless, nursing homes are also
lagging in use of EHRs and interoperability of data. SNFs were not eligible to participate in the
Medicare and Medicaid Promoting Interoperability Programs; in 2017, 66% of SNFs had
adopted EHRs, and only 18% of SNFs had the ability to integrate resident health information
received from outside facilities.
237
A more complete picture of the health and well-being of residents at a population level across the
varied sites where care and services are received would assist with rapid identification of insights
and evidence for improvements that help prevent and treat infections more effectively and
efficiently - now and in the future. Such data could also be used to predict hotspots, resource
needs, and other interventions in the future, thus protecting residents before threats occur. Data
could also be used to further research in long-term care.
With CMS taking a lead, in collaboration with its federal partners, to drive these changes,
nursing home owners and administrators will be able to more fully leverage modern technology
to: 1) integrate with the larger healthcare data network, yielding an enrichment of the big data
analytics needed to formulate systems-level, data-driven decisions, and 2) engage in user-
centered communications with their staff, residents, residents’ representatives and families, and
the public, yielding a greater sense of transparency, accountability, and partnership.
4.3 Facility Planning and Renovations
Throughout the pandemic, outdated facilities have complicated the challenges that nursing
homes face to meet the needs of residents while protecting them from infectious diseases.
Facilities cannot easily be retrofitted for cohorting or creating separate visitor entrances. CMS
needs to examine how nursing homes are financed; fixed costs may prevent owners and
administrators from investing in infrastructure stabilization and modernization. CMS is
positioned to elicit recommendations for the redesign, retrofitting, and reconfiguration of nursing
homes that incorporate lessons learned about disease prevention and control; technological best
practices; financing requirements; and the health and well-being of residents and staff. These
recommendations could be collected by a sub-committee of the proposed Long-Term Care
Commission (Section 3.7).
By catalyzing this change, CMS will help ensure that nursing home stakeholders of the future
will feel safe, secure, and supported in the environments where they live and work.
4.4 Payment Reform
Across the care continuum, payment drives care. Payment in the long-term care setting is split
across payers and systems—too often incentivizing the type of care received, rather than
coordinated best practices for quality and safety. CMS, together with its partners, must undertake

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
67
payment reform, specifically clarifying coverage for resident hand-offs across a wide variety of
care settings. CMS, with its government, private, and academic partners, can recommend
concrete payment-reform options that incentivize coordinated, personalized care that prioritizes
safety and quality.
238
These recommendations could be collected by a sub-committee of the
proposed Long-Term Care Commission (Section 3.7).
By CMS leading these actions, nursing home residents of the future will feel they are actually at
the center of and driving decision-making about their care and well-being.
4.5 Overall: Resident-Driven Care and Shared Decision-Making
These system reforms must be made in a resident-centered and, if possible, resident-driven
manner. Resident-driven care prioritizes not only clinical care received, but also the lifestyle
goals of the resident—where they live, with whom they live, their quality of life, their visitor
preferences, their desires, and ability to leave, and so on. It recognizes residents for who they
are—human beings who should be treated with dignity and respect; who deserve to not only be a
part of those decisions but to be armed with information to help drive those decisions.
CMS should take every recommended action—and all of its work on behalf of nursing homes—
with this resident-centered and resident-directed focus in mind. The nation’s attention has landed
squarely on nursing homes during this pandemic. America is witnessing the devastating
consequences of having ignored or underfunded systemic issues in long-term care settings. We
envision a system of care that is better for our children than it is and was for our grandparents—
one that values and respects older adults and people with disabilities as vital to the fabric of our
society.
236
Fogel, B. S. (2020, July 27). Data Driven Solutions For COVID-19 in Skilled Nursing Facilities: MDS ‘Section Y’.
Health Affairs. https://www.healthaffairs.org/do/10.1377/hblog20200723.64590/full/
237
Heny, J., Pylpchuk, Y., & Patel, V. (2018, November). Electronic Health Record Adoption and Interoperability
among U.S. Skilled Nursing Facilities and Home Health Agencies in 2017. The Office of the National Coordinator for
Health Information Technology. https://www.healthit.gov/sites/default/files/page/2018-11/Electronic-Health-Record-
Adoption-and-Interoperability-among-U.S.-Skilled-Nursing-Facilities-and-Home-Health-Agencies-in-2017.pdf
238
See Commission on Long-Term Care (September 30, 2013). “Report to the Congress.”
http://ltccommission.org/ltccommission/wp-content/uploads/2013/12/Commission-on-Long-Term-Care-Final-Report-9-
26-13.pdf

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-1
Appendix A:
Definition of Acronyms and Terms in Report
1. Acronyms
Acronym Definition
AHCA American Health Care Association
AHRQ Agency for Healthcare Research and Quality
APIC Association for Professionals in Infection Control
ASPR Assistant Secretary for Preparedness and Response
CARES Act Coronavirus Aid, Relief, and Economic Security Act
CBIC Certification Board of Infection Control and Epidemiology
CDC Centers for Disease Control and Prevention
CFR Code of Federal Regulations
CGNO Coalition of Geriatric Nursing Organizations
CHIP Children's Health Insurance Program
CIC Certified Infection Control
CLIA Clinical Laboratory Improvement Amendments
CMP Civil Monetary Penalty
CMS Centers for Medicare & Medicaid Services
CNA Certified Nursing Assistant
COVID Coronavirus Disease
COVID-19 Coronavirus Disease-2019
ECP Essential Care Partner
EHR Electronic Health Record
EPA Environmental Protection Agency
ESBL Extended Spectrum Beta-Lactamase
FAQ Frequently Asked Question
FDA Food and Drug Administration
FEMA Federal Emergency Management Agency
FFRDC Federally Funded Research and Development Center
FIC Focused Infection Control

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-2
Acronym Definition
HHS Department of Health and Human Services
HIPAA Health Insurance Portability and Accountability Act
HIT Health Information Technology
HPSA Health Professional Shortage Area
HVAC Heating, Ventilation, and Air Conditioning
IP Infection Prevention
IPC Infection Prevention and Control
IPCP Infection Prevention and Control Program
LPN Licensed Practical Nurse
LTC Long-Term Care
LTCCR Long Term Care Commission Report to Congress
LTSS Long-Term Services and Supports
MDS Minimum Data Set
MITRE The MITRE Corporation
MMWR Morbidity and Mortality Weekly Report
MRSA Methicillin-resistant Staphylococcus aureus
NAHCA National Association of Health Care Assistants
NASEM National Academy of Sciences, Engineering, and Medicine
NCAL National Center for Assisted Living
NCIRD National Center for Immunization and Respiratory Diseases
NF Nursing Facility
NHSN National Healthcare Safety Network
NIH National Institutes of Health
NIOSH National Institute for Occupational Safety and Health
NPI Non-Pharmaceutical Interventions
OASH Office of the Assistant Secretary for Health
PPE Personal Protective Equipment
PUF Public Use File
QAPI Quality Assurance and Performance Improvement
QIN Quality Improvement Network
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-3
Acronym Definition
QIO Quality Improvement Organization
RAI/MDS Resident Assessment Instrument/Minimum Data Set
RN Registered Nurse
SARS Severe Acute Respiratory Syndrome
SARS-CoV-2 Severe Acute Respiratory Syndrome Coronavirus 2
SEAN National Academies of Sciences, Engineering, and Medicine
Societal Experts Action Network
SHEA Society for Healthcare Epidemiology of America
SLTT State, Local, Territorial, and Tribal
SNF Skilled Nursing Facility
TB tuberculosis
USC United States Code
USPHC United States Public Health Service Corps
VRE Vancomycin-resistant Enterococci
WHO World Health Organization
2. Glossary of Terms
Term
Definition
The Act
The Social Security Act
Amendment
In the final privacy rule, an amendment to a record would
indicate that the data is in dispute while retaining the original
information (CMS).
Office of the
Assistant Secretary
for Preparedness and
Response (ASPR)
From phe.gov: ASPR was established to create a focal point
or a “unity of command” by consolidating all Federal
nonmilitary public health and medical preparedness and
response functions in one office. ASPR leads the public
health and medical, preparedness, response and recovery
to disasters and public health emergencies.
Assessments
The gathering of information to rate or evaluate your health
and needs, such as in a nursing home.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-4
Term
Definition
Asymptomatic Carrier
From CDC.gov: An individual who tests positive for COVID-
19 but does not exhibit the known symptoms of the disease.
Blanket waiver
Under Section 1135 or 1812(f) of the Social Security Act,
CMS can issue several blanket waivers when there is a
disaster or emergency. When a blanket waiver is issued,
providers are not required to apply for an individual waiver.
Blanket waivers prevent access to care gaps for
beneficiaries affected by the emergency. If a blanket waiver
is not issued, providers can ask for an individual Section
1135 waiver.
Center for Disease
Control and
Prevention (CDC)
From CDC.gov: The Centers for Disease Control and
Prevention (CDC) serves as the national focus for
developing and applying disease prevention and control,
environmental health, and health promotion and health
education activities designed to improve the health of the
people of the United States.
Certified Nursing
Assistant (CNA)
From bls.gov: Nursing assistants provide basic care and
help residents with activities of daily living.
Civil Money Penalty
(CMP)
A CMP is a monetary penalty the Centers for Medicare &
Medicaid Services (CMS) may impose against nursing
homes for either the number of days or for each instance a
nursing home is not in substantial compliance with one or
more Medicare and Medicaid participation requirements for
long-term care facilities. A portion of CMPs collected from
nursing homes are returned to the states in which CMPs are
imposed. State CMP funds may be reinvested to support
activities that benefit nursing home residents and that
protect or improve their quality of care or quality of life.
Clinical Laboratory
Improvement
Amendments (CLIA)
The Centers for Medicare & Medicaid Services (CMS)
regulates all laboratory testing (except research) performed
on humans in the U.S. through the Clinical Laboratory
Improvement Amendments (CLIA). In total, CLIA covers
approximately 260,000 laboratory entities. The objective of
the CLIA program is to ensure quality laboratory testing.
Although all clinical laboratories must be properly certified to
receive Medicare or Medicaid payments, CLIA has no direct
Medicare or Medicaid program responsibilities.
CMS Locations
CMS sites formerly referred to as Regional Offices.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-5
Term
Definition
Cohorting
Cohorting is the process of locating individuals with the
same condition in the same space with the intent of
reducing or eliminating interaction between infected persons
with uninfected persons.
Commission
members
The people selected by MITRE to serve on the Commission.
Contact tracing
From CDC.gov: Case investigation and contact tracing are
fundamental activities that involve working with a person
(symptomatic and asymptomatic) who has been diagnosed
with an infectious disease to identify and provide support to
people (contacts) who may have been infected through
exposure to the person.
Convenings
Meetings of The Coronavirus Commission on Safety and
Quality in Nursing Homes
Coronavirus Aid,
Relief, and Economic
Security Act
(CARES Act)
From treasury.gov: The Coronavirus Aid, Relief, and
Economic Security (CARES) Act was signed into law by
President Trump on March 27th, 2020. The CARES Act
provides for payments to State, Local, and Tribal
governments navigating the impact of the COVID-19
outbreak. CMS received $5 billion from the Provider Relief
Fund authorized by the CARES Act for nursing homes’ use.
Coronavirus Disease
2019 (COVID-19)
The disease caused by SARS-CoV-2
Decontamination
From CDC.gov: Decontamination of N95 Filtering Facepiece
Respirators (FFRs) may be considered as part of limited
reuse strategies. Extended use may also be considered as
part of limited reuse strategies whereby an N95 FFR is worn
for multiple person contacts then stored or decontaminated
before being reused.
Diagnostic test
Diagnostic testing is used to identify infected individuals
based on the ability to detect the presence of the genetic
signature of the SARS-CoV-2 virus in respiratory secretions.
Don and Doff
From CDC.gov: Don is the process of how to put on PPE
gear while Doff is the process of how to take off PPE.
Emergency
Preparedness Rule,
42 C.F.R. § 483.73
The long-term care facility must comply with all applicable
Federal, State and local emergency preparedness
requirements. The long-term care facility must establish and
maintain an emergency preparedness program that meets
the requirements of this section.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-6
Term
Definition
Family
For the purposes of this report, anyone the resident defines
as their family, individuals who are related to them, as well
as friends.
Federal Emergency
Management Agency
(FEMA)
From FEMA.gov: FEMA’s mission is to help people before,
during and after disasters.
Federally Funded
Research and
Development Center
(FFRDC)
The FFRDC works with federal government sponsors as a
technical collaborator and advisor on critical research and
development programs and technology acquisitions.
Focused Infection
Controls (FIC) Survey
The Focused Infection Control Survey is a CMS
Assessment tool used by federal and state surveyors to
assess compliance with the minimum health and safety
requirements as it relates to the COVID-19 pandemic. It is
available to every provider in the country to make them
aware of Infection Control priorities during this time of crisis,
and providers and suppliers may perform a voluntary self-
assessment of their ability to meet these priorities.
Food and Drug
Administration (FDA)
From FDA.gov: The FDA is responsible for ensuring that
human drugs, and vaccines and other biological products
and medical devices intended for human use are safe and
effective.
Hazard Pay
From DOL.gov: Hazard pay means additional pay for
performing hazardous duty or work involving physical
hardship. Work duty that causes extreme physical
discomfort and distress which is not adequately alleviated
by protective devices is deemed to impose a physical
hardship. The Fair Labor Standards Act (FLSA) does not
address the subject of hazard pay, except to require that it
be included as part of a federal employee's regular rate of
pay in computing the employee's overtime pay.
Healthcare Personnel
From CDC.gov: Healthcare personnel (HCP) refers to all
paid and unpaid persons serving in healthcare settings who
have the potential for direct or indirect exposure to
clients/residents/patients or infectious materials
Health Information
Technology (HIT)
From HealthIT.gov: The application of information
processing involving both computer hardware and software
that deals with the storage, retrieval, sharing, and use of
healthcare information, data, and knowledge for
communication and decision making.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-7
Term
Definition
Health Professional
Shortage Areas
(HPSA)
From HRSA.gov: Health Professional Shortage Areas
(HPSAs) are designations that indicate healthcare provider
shortages in primary care, dental health; or mental health.
These shortages may be geographic-, population-, or
facility-based.
HIPAA compliant
A regulation to guarantee people’s rights and protections
against the misuse or disclosure of their health records.
COVID-19 Hotspot
From CDC.gov: Counties meeting specified criteria relating
to temporal increases in number of cases and incidence.
Infection Prevention
and Control
Programs (IPCP)
42 CFR § 483.80
The long-term care facility must establish an infection
prevention and control program (IPCP).
Infection Prevention
Educators
Provide and document competency-driven, experiential
training on core practice; crisis standards of care, including
fit testing of N95 masks and PPE donning and doffing; and
crisis recovery; and regularly assess competency
achievement of all direct and contract staff (e.g.,
administrators, nurses, CNAs, environmental services,
maintenance, food service, and ancillary staff).
Long-Term Care
Health-related care and services (above the level of room
and board) not available in the community, needed regularly
due to a mental or physical condition
Long-term care
facilities
Used when referring collectively to skilled nursing facilities,
nursing facilities, assisted living facilities, and other facilities
that provide long-term care.
Long-Term Services
and Supports
The Centers for Medicare & Medicaid Services (CMS) is
working in partnership with states, consumers and
advocates, providers and other stakeholders to create a
sustainable, person-driven long-term support system in
which people with disabilities and chronic conditions have
choice, control and access to a full array of quality services
that assure optimal outcomes, such as independence,
health and quality of life.
Medicaid
Beneficiaries
Individuals eligible to receive healthcare services paid by
Medicaid; 10.9 million individuals are dually eligible for
Medicare and Medicaid.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-8
Term
Definition
Medicare
Beneficiaries
58 million individuals who are eligible to receive Medicare
benefits from CMS; individuals ages 65 and older,
individuals under age 65 who are receiving disability
benefits from Social Security or the Railroad Retirement
Board, and those having End Stage Renal Disease.
National Healthcare
and Safety Network
(NHSN)
From CDC.gov: CDC’s National Healthcare Safety Network
is the nation’s most widely used healthcare-associated
infection (HAI) tracking system. NHSN provides facilities,
states, regions, and the nation with data needed to identify
problem areas, measure progress of prevention efforts, and
ultimately eliminate healthcare-associated infections.
Non-pharmaceutical
intervention (NPI)
Interventions to slow the spread of SARS-CoV-2, excluding
medication (e.g., mandatory stay at home orders; non-
essential business closures; social distancing; large
gathering bans; school closures; mandatory isolation of the
sick; mandatory quarantine of travelers; and restrictions on
bars, restaurants, and other public places
Nursing facility (NF)
A facility that provides long-term medical and skilled nursing
care, rehabilitation, or health-related services; Medicaid is
the dominant payer
Nursing home
The type of facility that is the focus of the Commission’s
work; including both skilled nursing facilities and nursing
facilities.
Nursing home
residents
People who reside in nursing homes.
Observation Unit
A separate area in a nursing home for newly admitted or
transferred residents
Ombudsman
From acl.gov: States’ Long-Term Care Ombudsman
programs work to resolve problems related to the health,
safety, welfare, and rights of individuals who live in long-
term care facilities, such as nursing homes, board and care
and assisted living facilities, and other residential care
communities. Ombudsman programs promote policies and
consumer protections to improve long-term services and
supports at the facility, local, state, and national levels.
Outbreak
From apic.org: An outbreak is a sudden rise in the number
of cases of a disease. An outbreak may occur in a
community or geographical area or may affect several
countries. It may last for a few days or weeks, or even for
several years. Some outbreaks are expected each year,
such as influenza.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-9
Term
Definition
Personal Protective
Equipment (PPE)
Equipment worn to minimize exposure to hazards that
cause serious workplace injuries and illnesses.
Pandemic
From CDC.gov: Pandemic refers to an epidemic that has
spread over several countries or continents, usually
affecting a large number of people. Epidemics occur when
an agent and susceptible hosts are present in adequate
numbers, and the agent can be effectively conveyed from a
source to the susceptible hosts.
Patients Over
Paperwork
CMS established an internal process to evaluate and
streamline regulations with a goal to reduce unnecessary
burden, to increase efficiencies, and to improve the
beneficiary experience.
Post-acute care
Rehabilitation or palliative care services that beneficiaries
receive after, or in some cases instead of, a stay in an acute
care hospital. Depending on the intensity of care the person
requires, treatment may include a stay in a facility (e.g., a
SNF), ongoing outpatient therapy, or care provided at home.
Medicare is a major payer.
Provider Relief Fund
From HHS.gov: Provider Relief Fund payments are being
disbursed via both "General" and "Targeted" Distributions.
To be eligible for the General Distribution, a provider must
have billed Medicare fee-for-service in 2019, be a known
Medicaid and CHIP or dental provider and provide or
provided after January 31, 2020 diagnoses, testing, or care
for individuals with possible or actual cases of COVID-19, or
prevented in the spread of SARS-CoV-2. HHS broadly
views every person as a possible case of COVID-19.
Targeted Distributions: HHS is allocating targeted
distribution funding to providers in areas particularly
impacted by the COVID-19 outbreak, rural providers, and
providers requesting reimbursement for the treatment of
uninsured Americans.
Quality Assurance
and Performance
Improvement (QAPI)
§ 483.75
Each long-term care facility, including a facility that is part of
a multi-unit chain, must develop, implement, and maintain
an effective, comprehensive, data-driven QAPI program that
focuses on indicators of the outcomes of care and quality of
life.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
A-10
Term
Definition
Quality Improvement
Network (QIN)-
Quality Improvement
Organization (QIO)
From QIOProgram.org: The 12 regional Quality Innovation
Network-Quality Improvement Organizations work with
providers, community partners, beneficiaries and caregivers
on data-driven quality improvement initiatives designed to
improve the quality of care for people with specific health
conditions.
Severe Acute
Respiratory
Syndrome
Coronavirus 2
(SARS-CoV-2)
The most recent coronavirus known to transmit from
animals to humans, first detected in China in December
2019, and causes a disease now referred to as “coronavirus
disease 2019” (“COVID-19”)
Skilled nursing
facility (SNF)
A facility that provides short-term recuperative and
rehabilitative services (often referred to as post-acute care);
Medicare is the dominant payer.
Social Security Act
P.L. 74-271, approved
August 14, 1935, 49
Stat. 620
From ssa.gov: Social Security provides replacement income
for qualified retirees and their families. Social Security
enrolls you in Original Medicare Part A (hospital insurance)
and Part B (medical insurance). Individuals who are within
three months of age 65 or older and not ready to start
receiving monthly Social Security benefits can apply just for
Medicare and wait to apply for retirement or spouses
benefits.:
Strike Team
From training.fema.gov: A set number of resources of the
same kind and type that have an established minimum
number of personnel, common communications, and a
designated leader.
Symptomatic Carrier
An individual who tests positive for COVID-19 and exhibits
the known symptoms of the disease
Triage
The assignment of degrees of urgency to wounds or
illnesses to decide the order of treatment of a large number
of people or casualties.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
B-1
Appendix B: Selection of Commission Members
This appendix summarizes the process MITRE used to select the members of the Commission.
Step 1: Nominations
MITRE launched a Commission website on May 14, announcing an open call for a cross-section
of thought leaders from various stakeholder groups to serve on the Commission. Interested and
qualified individuals were invited to nominate themselves or others to serve as Commission
members by submitting a nomination form, responding to a series of questions, and uploading
their resume or curriculum vitae prior to 5 p.m. EDT May 22. MITRE received more than 800
nominations.
The nomination form specified that desired membership would consist of a cross-section of
thought leaders from stakeholder groups including, but not limited to, the following categories:
academic researcher, clinician (various types), director and/or administrator of nursing home,
electronic medical records expert, family member, industry professional, infection control and
prevention expert, infectious disease expert, medical ethicist, nursing home resident, resident
advocate, and state or local authority.
Step 2: Initial Review Process: Coding and Evaluating Nominations
MITRE composed a team of project members and subject matter experts to participate in the
selection process (MITRE Review Team). The MITRE Review Team developed categories of
pre-determined objective criteria applicable to the evaluation of potential Commission members
from academia, industry, and administration. In addition, the MITRE Review Team established
objective criteria applicable to the evaluation of potential nursing home resident/family
member/resident advocates. Information from each application was reviewed and coded to
ensure minimal applicant requirements were met.
The MITRE Review Team then used the appropriate unique category of objective criteria to
conduct an initial evaluation of each applicant. In the instance where a nominees had expertise in
more than one of the stakeholder categories, the MITRE Review Team considered the nominees
under the most appropriate primary category based on the resume and the nominees’ self-
designated category assignment.
Step 3: Inter-Rater Reliability Analysis
When the initial review process was complete, the MITRE Review Team conducted an inter-rater
reliability analysis to quantitatively assess consistency and replicability of the review process and to
ensure the selection results met standards for acceptability.
Step 4: Secondary Review Process
Remaining candidates were distributed to reviewers from the MITRE Review Team based on
nomination category and reviewer expertise. The MITRE Review Team considered a set of
variables including scores, team notes, and observations to determine if each nominee was
recommended for further consideration.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
B-2
Step 5: Consensus-Seeking Discussion
A subset of the MITRE Review Team collaboratively considered the secondary reviewers’
recommendations to achieve an initial list of potential candidates and a set of alternates. The
result was shared for review and feedback with representatives from Atlas (an Alliance Partner),
members of MITRE’s senior leadership, and representatives of CMS.
Step 6: Announcement of Commission Members
MITRE invited selected nominees to serve on the Commission on June 12. Following
acceptances, MITRE announced the 25 members of the Commission on June 19.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-1
Appendix C:
Findings and Evidence for Recommendations and
Action Steps
Theme 3.1 – Testing and Screening
CMS and CDC have released iterative guidance recommending screening and testing of
residents, staff and visitors. On July 22, CMS announced HHS would provide an additional $5B
from Provider Relief Fund, as well as 15,000 testing devices, to support testing and that CMS
would begin requiring (rather than recommending) weekly staff testing in states with a 5%
positivity rate or greater. Commission members stressed the importance of testing and screening
and specifically noted challenges with funding and acquisition of testing and screening supplies.
They further underscored the need for rapid and appropriate testing to mitigate the potential
spread of SARS-CoV-2.The commission members recommended a targeted approach to ensure
adequate supplies are available in one quarter, one half, and three quarters and all of the nation’s
nursing facilities by October 1, November 1, December 1, 2020, and January 1, 2021,
respectively. Public input similarly supported the importance of testing and screening and urged
additional funding to support a robust testing and screening regime. Effective screening and
testing protocols and policies are critically necessary to reduce the risk of entry of SARS-CoV-2
within a facility and to control the virus’s spread, particularly in the context of significant
proportion of asymptomatic individuals.
239, 240
Screening, testing, and surveillance activities play a pivotal role in detecting and responding to
infectious disease outbreaks. Without a viable vaccine, identifying and isolating people infected
with SARS-CoV-2 is the only mechanism to prevent its spread.
241
Diagnostic testing is used to
identify infected individuals based on the ability to detect the presence of the genetic signature of
the SARS-CoV-2 virus in respiratory secretions. Testing of symptomatic individuals rapidly is
critical to subsequent isolation of those individuals away from susceptible and vulnerable
residents and staff, as well as the need to provide immediate medical care to those individuals if
necessary. Furthermore, targeted testing of staff and residents to capture asymptomatic or pre-
symptomatic individuals would enhance the ability of nursing homes to prevent or control the
spread of infection. Key to effective testing strategies is accuracy of tests, availability of tests,
and rapid turnaround times to receive and report results.
Screening attempts to prevent individuals with a recent positive test result, SARS-CoV-2 like
symptoms, or recent exposure risk from entering into a nursing home or interacting with staff
and residents. As more information is learned about the disease presentation, screening protocols
should be adapted to capture the common symptoms of infected individuals. However, while
screening can be an effective way to limit exposures within a nursing home, the substantial
percentage of individuals that remain asymptomatic after exposure means that nursing homes
cannot rely on screening alone to prevent and mitigate the spread of SARS-CoV-2 within their
facilities.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-2
Theme 3.2 – Equipment and PPE
Following the initial announcement of the COVID-19 pandemic outbreak, CMS has issued
guidance on the use of PPE March 10 and April 2. This guidance included updated CDC
recommendations for essential care workers to address PPE use when working with known or
suspected COVID-19 residents. PPE is “specialized clothing or equipment, worn by an employee
for protection against hazard.”
242
PPE has been demonstrated to be critically important in
protecting staff from the spread of SARS-CoV-2 and in turn, the residents whom they support.
OSHA released guidance that supports CDC recommendations for adequate supply and use of
PPE to protect nursing home workers.
243
PPE use, along with a combination of other infectious
disease mitigation strategies, have been shown to reduce spread of illness.
244
Along with this
guidance, CMS collaborated with the CDC in the development and release of National COVID-
19 training modules to provide guidance to nursing home staff.
These training modules covered
important infection control and PPE information vital to the successful containment or reduction
of SARS-CoV-2 within nursing homes. This release of these modules on March 11 was at the
beginning of this pandemic.
As concerns and cases of the virus grew, the supplies of PPE diminished. Many nursing homes
across the country were tasked with finding and securing PPE on their own during this crisis.
Most facilities had trouble securing quality PPE for staff and residents which resulted in
increased cases of people who tested COVID-19 positive within a nursing home. In response to
the national PPE shortage, FEMA issued 14-day supply of PPE to all nursing homes. There was
widespread press coverage of the inadequacy of supply in terms of volume and quality.
245
Commission members have been adamant about CMS responsibility to ensure that every nursing
home in the country has an adequate supply of high-quality PPE. Commission members
requested federally funded PPE for equal allocation while having the ability to reallocate when
surges occur. The Commission further emphasized the importance of the supplies being
appropriately fitted and the staff being properly trained on use.
246
The public input on this topic
primarily focused on the need to provide direct priority access of adequate PPE supply to nursing
home facilities for staff and visitors. The public also mentioned the importance of local,
statewide and regionally tracking of PPE to prepare for a future surge.
Theme 3.5 – Communication
Pursuant to the CMS final rule Reform of Requirements for Long-Term Care Facilities at 81 FR
68688 in 2016,
247
CMS imposes minimum standards on nursing homes that ensure timely and
adequate advance notice for family and caregivers on resident status at least 30 days prior to such
critical care transitions as transfer (whether to another part of the facility or another facility such
as a hospital) and discharge. If immediate transfer is required or the individual’s safety is in
jeopardy, nursing homes are required to notify the resident and caregivers as soon as practicable
before transfer or discharge. Nursing homes are also required to have written policies and
procedures on resident visitation rights, including any clinically necessary or reasonable
restriction or safety limitations the nursing home may place on such rights.
248
However, many of
these provisions did not prescribe a manner, timeframe, or frequency for which communication
about these events is to occur in the event of an ongoing state or nationwide public health
emergency, or specify acceptable alternatives or adaptive methods of communication when a

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-3
nursing home has to operate under such restrictions and make decisions rapidly pursuant to state
and federal guidelines on cohorting and restrictions on visitation. It is unlikely, for example, that
nursing homes would also be able to ensure the written policies and procedures on visitation
rights are updated frequently enough to reflect such restrictions, but there is currently no
nationwide CMS-endorsed standards for an alternative. It is also unclear whether CMS would
allow flexibilities for notice after the fact. To date, CMS has provided the following relief or
guidelines to nursing homes on communications with residents and caregivers during the
COVID-19 pandemic:
• March 4, 20202 Suspension of Survey Activities: CMS limited survey activity to
immediate jeopardy complaints (likely to result in harm) and some other special
circumstances only.
249
• March 13, 2020 Guidance for Infection Control and Prevention of Coronavirus Disease
2019 (COVID-19) in Nursing Homes: CMS stated that 1) facilities should maintain a
person-centered approach to…communicating effectively with residents, resident
representatives and/or their family, and understanding their individual needs and goals of
care; and 2) facilities should communicate through multiple means to inform individuals and
nonessential healthcare personnel of the visitation restrictions, such as through signage at
entrances/exits, letters, emails, phone calls, and recorded messages for receiving calls
250
• Updated July 2020 Toolkit on State Actions to Mitigate COVID-19 Prevalence in
Nursing Homes:
251
CMS included a disclaimer that this information did not constitute
agency guidance, but provided these Nursing Home Communications examples from states.
A few examples of state innovations are as follows:
o Arizona: Nursing homes are leveraging social media to increase morale, optimism,
and to reassure its community about loved ones in the nursing home.
o Delaware: Nursing home facilitates one-on-one electronic communication with
facility ombudsman to ensure families are connected to staff on important
information. Nursing home placed large signs with room numbers on long-term care
facility windows so families could easily identify their loved ones.
o Indiana: State Department of Health released communication guidelines for long-
term care facilities and set up outreach emails for communicating with concerned
loved ones. State also issued guidance for designating essential family caregivers to
participate more in care.
o Pennsylvania: Due to concerns that family and friends emergency may struggle with
changes in protocol, rights, and policies during COVID-19, state set up the
Pennsylvania Long-Term Care Ombudsman Program to help with a new statewide
resource called Virtual Family Council, offering weekly online meetings with a local
ombudsman and a team of 10 local experts. The weekly online meetings participants

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-4
can ask questions, share concerns, or listen to learn and gather information and
receive updates to resources and policies will be provided as well.
One recent opinion echoed the need for effective communication with families of nursing home
residents during the pandemic after state and CMS restrictions, stating that “Because information
about the outbreak is evolving rapidly, often on a daily basis, facilities should be prepared to
update their messaging quickly to ensure residents and family members have the most current
information they need to stay safe and healthy.” The opinion issued the following
recommendations on communication from providers on their challenges with communicating
with families of long-term care residents, stating that communication with families must: 1)
provide a clear purpose for calling; 2) express empathy for emotions of family members and
loved ones; 3) specify the nursing home’s protocols for helping families stay educated; 4)
reassure recipient that care of their loved one is the highest priority; and 5) instill a message of
togetherness and cooperation.
252
Communication guidelines from Indiana cited earlier also agree
that it is critical to calm concerns when communicating with family representatives and
suggested methods such as establishing a facility listserv or chat room where staff members
provide a daily “briefing” to residents, designated representatives, and other family members
about what is happening in the facility, and any updated to the facility's restricted visitation
policy and how the facility will be implementing it.
253
Given the varied approaches across these
several states, CMS’ recently issued statements about the nursing home’s responsibility to
communicate care-planning with residents and families in a person-centered manner may benefit
from additional detail and guidance to maintain consistency and effectiveness for the long-term
across states and clarify how nursing homes might still meet requirements for participation if
normal survey activities resume, but restrictions are still in effect in their state.
Theme 3.6 – Workforce Ecosystem: Stopgaps for Resident Safety
Surge Support: The CDC also developed guidelines for healthcare facilities to address potential
staffing shortfalls “Strategies to Mitigate Healthcare Personnel Staffing Shortages.”
254
CDC
highlights that as the pandemic progresses, staffing shortages will increase due to direct-care
worker exposures, illness, or need to care for family members at home. As maintaining
appropriate staffing levels is essential to providing a safe working environment and proper
resident care, the CDC guidance offers both contingency capacity strategies and crisis capacity
strategies for nursing homes that experience staffing shortages. Once a facility identifies its
minimum staffing needs, the CDC recommends the facility reach out to local, state, and federal
public health partners for assistance in identifying additional direct care workers who are
available for hire. For healthcare facilities with existing staffing shortages, the CDC recommends
developing regional strategies to send residents to alternate healthcare facilities/ care sites.
Multi-employer Direct Care Providers: Studies indicate an increased risk of COVID-19
infection of staff working across different nursing facilities.
255
Additionally, a preliminary
analysis from the CDC concluded that the sharing of staff members among multiple nursing
homes — along with employees continuing to work while sick — helped to hasten the spread of
SARS-CoV-2 in Washington state and other states.
256
Working in multiple facilities, however, is
the economic reality for many nursing home staff.
257

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-5
24/7 RN Coverage: While staffing in long-term care facilities has been a chronic issue, there is
little consideration for acuity when developing staffing patterns on a daily basis. Given the high
acuity and labile nature of COVID-19 positive residents’ status, RN oversight is recommended
around the clock when the resident population experiences a COVID-19 positive test. RNs assess
and manage all resident populations with appropriate interventions, admit and discharge
residents, and develop plans of care and wellness for all residents in the facility. The rapid
intervention of an RN may reduce unnecessary hospitalizations.
In 2014, the Coalition of Geriatric Nursing Organizations (CGNO) recommended that an RN be
present in nursing homes at all times for oversight of resident care, resident assessment,
supervision of licensed nursing staff and delegation to certified nursing assistants. This position
statement was endorsed by the ANA.
258
Infection Preventionists and Infection Prevention Educators: Deficiencies in infection
prevention and control in nursing homes were prevalent prior to the COVID-19 pandemic.
259
As
COVID-19 cases and deaths in nursing homes increased, CMS issued an informational bulletin
in February 2020 advising healthcare facilities to review the Centers for Disease Control (CDC)
COVID-19 advisory and recommendations as well as their own infection control policies.
260
In
April 2020, CMS issued guidance directing facilities to screen staff, residents, and visitors for
symptoms, ensure staff use PPE “to the extent available,” and designate separate staff and
facilities or units for COVID-19 cases.
261
In May 2020, CMS issued an informational toolkit
with best practices for states to mitigate COVID-19 in nursing homes.
262
WHO says: “Infection prevention and control (IPC) is a scientific approach and practical
solution designed to prevent harm caused by infection to patients and health workers. It is
grounded in infectious diseases, epidemiology, social science and health system strengthening.
IPC occupies a unique position in the field of patient safety and quality universal health coverage
since it is relevant to health workers and patients at every single health-care encounter. No
country, no health-care facility, even within the most advanced and sophisticated health-care
systems, can claim to be free of the problem of healthcare-associated infections. The need for
having IPC programs nationally and at the facility level is clearly reinforced within the WHO
100 Core Health Indicators list.”
263
Theme 3.7 – Workforce Ecosystem: Strategic Reinforcement
CNA On-the-job Training and Recruitment: Direct care worker positions are often viewed as
low-wage, entry-level jobs with little to no opportunity for advancement and
thus workers choose or move on to other professions. High turnover and workforce shortages
have an impact on care quality.
264
The pandemic has exacerbated staffing challenges because
of the increased resident acuity and risks of providing direct care residents with COVID-19.
To assist in addressing potential nursing home staffing shortages during the COVID-19
pandemic and to reduce barriers for SNFs and NFs to hire staff, CMS provided two waivers
related to workforce staffing as part of its long-term care blanket waivers.
265
First, CMS waived
the requirement at 42 CFR 483.35(d) that a facility may not employ anyone for longer than four
months unless they meet certain training and certification requirements, provided nursing homes
utilize competency assessments to ensure that these nurse aides are competent to provide

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-6
relevant nursing and nursing-related services. While the waiver provides flexibility at the federal
level, state occupational licensing and state regulatory agencies must approve the waiver for this
temporary hiring of nursing assistants, and only certain states have done so. AHCA/NCAL
developed an 8-hour, free, online “Temporary Nurse Aide”
266
training course to provide a
pathway for providers to utilize the waiver once they received state regulatory approval. Second,
CMS modified the nurse aide training requirements at 42 CFR 483.95(g)(1) by postponing the
deadline for nursing assistants to receive at least 12 hours of in-service training annually
throughout the COVID-19 PHE until the end of the first full quarter after the declaration of the
PHE concludes.
CNAs spend more time than any other nursing staff assisting residents, providing a median of
2.1 hours of hands-on care per resident per day.
267
Wages for nursing assistants have not kept up
with inflation over the past 10 years, and there is a high rate of poverty among CNAs.
268
In the
wake of the pandemic, CNA education has been interrupted. Private CNA schools are closed,
and it is not possible to conduct the necessary hands-on training of CNAs. Moreover, the stigma
associated with being a CNA and competition from other industries that employ workers with
similar education and experience (e.g., service workers, warehouse fulfillment) makes it difficult
to fill these positions. CNA shortages is a serious, complex problem.
Longstanding Issues: Chronic long-term care workforce challenges were documented in the
2013 Long Term Care Commission report to Congress (LTCCR) and continues today due to: low
levels of compensation; lack of benefits; limited opportunities for professional advancement
(e.g., no clinical ladder, no assistance in progressing into LPN/RN training); and high resident-
to-staff ratios.
Federal law has few requirements for nurse staffing in long-term care facilities and haven’t been
updated since the Nursing Home Reform Act was implemented in 1987.
269
A 2019 poll
270
of
nurse-to resident ratios of long-term care and SNF nurses in a private Facebook group found
unsafe nurse-resident staffing ratios pre-dated the COVID-19 pandemic:
• 32:1 nurse and 16:1 CNA- Ohio
• 44:1 nurse and 44:2 CNA- Tennessee
• 50:2 nurse and 15:3 CNA- New York
• 66:2 nurse and 66:4 CNA- Illinois
• 50:1 nurse and 30:1 CNA- Georgia
• 60:1 nurse and 60:3-4 CNA- Nebraska
Theme 3.8 – Technical Assistance and Quality Improvement
Nursing homes with COVID-19 outbreaks are receiving on-site technical assistance and
education from QIN-QIOs
271, 272, 273
and Federal Task Force Strike Teams.
274
Other training is
available online: weekly infection control webinars for nursing homes through the QIO
program,
275
COVID-19 Prevention in Long-term Care Facilities,
276
Nursing Home Infection
Preventionist Training Course,
277
and Infection Preventionist Specialized Training - IPCO

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-7
Version 2.
278
Several commission members recommended leveraging QIOs to provide on-site
training and assistance to nursing homes, specifically nursing homes in COVID-19 “hot spots,”
to improve resident care and residents’ healthcare outcomes.
279
One commission member
recommended increasing the number of QIOs, which would enable all QIOs to serve a smaller
segment of the country and, thus, fewer nursing homes, giving QIOs the ability to provide more
assistance. In addition to providing on-site training, the Commission recommended creating
COVID-19 QAPI tools for nursing homes.
Theme 3.10 – Nursing Home Data
Principal Recommendation 10A:
CMS and federal partners have initiated actions on some of these issues. During the July 21,
2020 Commission meeting, CMS and CDC representatives described how they are working
together to refine and create more specificity for certain COVID-19 NHSN data elements. Based
on nursing home data reported to CDC, CMS and federal partners have provided staff for Task
Force Strike Teams to provide technical assistance and training to select nursing homes with
increased COVID-19 cases. CMS announced that they will also use the data to provide states
with a list of nursing homes with increased cases each week as part of the weekly Governor’s
report to assist states with targeting support to high-risk nursing homes.
280
Commission members
and public comments supported a continued focus on obtaining data from nursing homes that can
be acted upon in a meaningful way while considering the associated costs of data collection.
Principal Recommendation 10B:
When CMS initiated a joint effort with CDC to collect COVID-19 data from nursing homes
nationwide, it was announced that CDC would be providing a reporting tool to collect the data
and that there were plans to make the data publicly available.
281
CMS subsequently established
the COVID-19 Nursing Home Data website, which provides access to the COVID-19 Public File
containing data reported by nursing homes to CDC’s NHSN system, along with related resources
and statistics.
282
During the July 29 Commission meeting, CMS also indicated that work on a
new consolidated source of relevant guidance and regulations had been initiated. Commission
members and public comments were generally quite supportive of continued efforts to develop a
central location for nursing homes to submit COVID-19 data and to find essential information
from CMS and partners.
Principal Recommendation 10C:
CMS has released guidance requiring facilities to report to the CDC communicable diseases,
healthcare-associated infections, and potential outbreaks in a standardized format and frequency
defined by CMS and CDC. According to requirements at 42 CFR 483.80 and CDC guidance,
nursing homes must notify state or local health department about residents or staff with
suspected or confirmed COVID-19, residents with severe respiratory infection resulting in
hospitalization or death, or ≥ 3 residents or staff with new-onset respiratory symptoms within 72
hours of each other.
283, 284
CMS also requires nursing homes to report COVID-19 facility data to
the CDC, residents, their representatives and families of residents in facilities and updated the
COVID-19 Focused Survey for Nursing Homes, Entrance Conference Worksheet, COVID-19

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-8
Focused Survey Protocol, and Summary of the COVID-19 Focused Survey for Nursing Homes
to reflect COVID-19 reporting requirements.
285
239
Gao, Z., Xu, Y., Sun, C., Wang, X., Guo, Y., Qiu, S., & Ma, K. (2020). A systematic review of asymptomatic
infections with COVID-19 [Advance online publication]. Journal of Microbiology, Immunology, and Infection.
https://doi.org/10.1016/j.jmii.2020.05.001
240
Kimball, A., Hatfield, K. M., Arons, M., James, A., Taylor, J., Spicer, K., & Bell, J. M. (2020, March 20).
Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a long-term care skilled nursing facility—
King County, Washington. Morbidity and Mortality Weekly Report, 69(13), 377.
http://dx.doi.org/10.15585/mmwr.mm6913e1
241
Cheng M. P., Papenburg, J., Desjardins, M., Kanjilal, S., Quach, C., Libman, M., Dittrich, S., & Yansouni, C. P.
(2020). Diagnostic testing for severe acute respiratory syndrome-related Coronavirus 2: A narrative review. Ann
Intern Med, 172(11), 726-734. https://www.acpjournals.org/doi/10.7326/M20-1301
242
Bloodborne pathogen. 29 CFR 1910.1030(b). https://www.law.cornell.edu/cfr/text/29/1910.1030
243
Occupational Safety and Health Administration. (n.d.). COVID-19 Guidance for Nursing Home and Long-Term
Care Facility Workers. https://www.osha.gov/Publications/OSHA4025.pdf
244
Chou, R., Dana, T., Buckley, D. I., Selph, S., Fu, R., & Totten, A. M.. (2020). Epidemiology of and risk factors for
coronavirus infection in health workers. Annals of Internal Medicine, 173(2), 120-136.
https://www.acpjournals.org/doi/10.7326/M20-1632
245
Rau, J. (2020, June 11). Nursing homes run short of COVID-19 protective gear as federal response falters. NPR.
https://www.npr.org/sections/health-shots/2020/06/11/875335588/nursing-homes-run-short-of-covid-19-protective-
gear-as-federal-response-falters
246
Kimball, A., Hatfield, K. M., Arons, M., James, A., Taylor, J., Spicer, K., Bardossy, A. C., Oakley, L.P., Tanwar, S.,
Chisty, Z., Bell, J. M., Methner, M., Harney, J., Jacobs, J.R., Carlson, C. M., McLaughlin, H.P., Stone, N., Clark, S.,
Bronstrom-Smith, C., … . (2020, April 3). Asymptomatic and presymptomatic SARS-CoV-2 infections in residents of a
long-term care skilled nursing facility — King County, Washington, March 2020. Morbidity and Mortality Weekly
Report, 69(13), 377-381. https://www.cdc.gov/mmwr/volumes/69/wr/mm6913e1.htm?s_cid=mm6913e1_w
247
Medicare and Medicaid Programs. (2016, October 4). Reform of Requirements for Long-Term Care Facilities. 81
Fed. Reg. 68688 (2016). https://www.govinfo.gov/content/pkg/FR-2016-10-04/pdf/2016-23503.pdf
248
Id.
249
Centers for Medicare & Medicaid Services Center for Clinical Standards and Quality/Quality, Safety & Oversight
Group. (2020, March 4). Memorandum to State Survey Agency Directors: Suspension of Survey Activities.
https://www.cms.gov/files/document/qso-20-12-all.pdf
250
Centers for Medicare & Medicaid Services Center for Clinical Standards and Quality/Quality, Safety & Oversight
Group. (2020, March 13). Memorandum to State Survey Agency Directors: Guidance for Infection Control and
Prevention of Coronavirus Disease 2019 (COVID-19) in Nursing Homes
(REVISED).https://www.cms.gov/files/document/qso-20-14-nh-revised.pdf
251
Centers for Medicare & Medicaid Services. (2020, August). Toolkit on State Actions to Mitigate COVID-19
Prevalence in Nursing Homes.
https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-
homes.pdf
252
Id.
253
Indiana State Department of Health. (2020, May 5). Long-term Care Facility Communication Guidelines: Informing
Family Members during COVID-19.
https://www.coronavirus.in.gov/files/IN_COVID-
19_comm%20guidelines%205.3.20.pdf
254
Centers for Disease Control and Prevention (2019, July 17) Strategies to Mitigate Healthcare Personnel Staffing
Shortages https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html
255
SARS-CoV-2 positivity was 4-fold higher in staff working across different care homes. Ladhani, S. N. et al. London
Care Home Investigation Team (2020). Increased risk of SARS-CoV-2 infection in staff working across different care
homes enhanced CoVID-19 outbreak investigations in London care Homes. The Journal of infection, S0163-
4453(20)30508-9. Advance online publication. https://doi.org/10.1016/j.jinf.2020.07.027

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-9
256
McMichael, T. M. et al. (2020, March 18). COVID-19 in a Long-Term Care Facility — King County, Washington,
February 27–March 9, 2020. MMWR Morb Mortal Wkly Rep 2020;69:339-342.
https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e1.htm
257
Reported by Commission members; “Some certified nursing assistants need to work jobs at more than one home
to earn enough to support their families.”Romero, L., Mosk, M., Freger, H., & Pecorin, A. (2020, May 5) With millions
out of work, nursing homes under siege from coronavirus plead for more staff.
https://abcnews.go.com/Health/millions-work-nursing-homes-siege-coronavirus-plead-staff/story?id=70513441
258
Nursing World. (2014, November 12). ANA Nursing Staffing Requirements to Meet the Demands of Today’s Long
Term Care Consumer.
https://www.nursingworld.org/practice-policy/nursing-excellence/official-position-
statements/id/nursing-staffing-requirements-to-meet-the-demands-of-todays-long-term-care-consumer/
259
U.S. Government Accountability Office. (2020, May 20) Infection Control Deficiencies Were Widespread and
Persistent in Nursing Homes Prior to COVID-19 Pandemic. https://www.gao.gov/assets/710/707069.pdf
260
Centers for Medicare & Medicaid Services. (2020, February 6). Information for Healthcare Facilities Concerning
2019 Novel Coronavirus Illness (2019-nCoV).
https://www.cms.gov/medicareprovider-enrollment-and-
certificationsurveycertificationgeninfopolicy-and-memos-states-and/information-healthcare-facilities-concerning-2019-
novel-coronavirus-illness-2019-ncov
261
Centers for Medicare & Medicaid Services. (2020, April 2). COVID-19 Long-Term Care Facility Guidance.
https://www.cms.gov/files/document/4220-covid-19-long-term-care-facility-guidance.pdf
;
262
Centers for Medicare and Medicaid Services. (2020, May 13). Toolkit on State Actions to Mitigate COVID-19
Prevalence in Nursing Homes.
https://www.cms.gov/files/document/covid-toolkit-states-mitigate-covid-19-nursing-
homes.pdf
263
World Health Organization. (2020). Infection Prevention and Control. https://www.who.int/infection-
prevention/about/ipc/en/
264
Quality Improvement Organizations. (2019 June). Resources to Support Staff Stability in Post-Acute and Long-
Term Care Settings.
https://qioprogram.org/sites/default/files/editors/141/Resources_To_Support_Staff_Stability_20190626_508.pdf
265
Centers for Medicare & Medicaid Services. (2020, March 6). COVID-19 Emergency Declaration Blanket Waivers
for Health Care Providers.
https://www.cms.gov/files/document/summary-covid-19-emergency-declaration-
waivers.pdf
266
American Healthcare Association Education. (2020). Temporary Nurse Aide Course.
https://educate.ahcancal.org/products/temporary-nurse-aide
. As of 8/11, nine states (Delaware, Indiana, Iowa,
Maryland, Nebraska, New Jersey, New York, Texas, and West Virginia) have permitted facilities to use the
AHCA/NCAL temporary training, and 13 states (Alabama, Connecticut, District of Columbia, Georgia, Illinois, Kansas,
Mississippi, North Carolina, New Hampshire, Pennsylvania, South Carolina, Tennessee, and Virginia) have included
the AHCA/NCAL training as part of a broader set of requirements for temporary CNAs.
267
PHI (2019, September 3). U.S. Nursing Assistants Employed in Nursing Homes. https://phinational.org/resource/u-
s-nursing-assistants-employed-in-nursing-homes-key-facts-2019/ RNs provide .4 staff hours per resident per day,
and LPNs provide .8 staff hours per resident per day.
268
CNAs working in nursing homes earn a median income of $22,200 per year. Low annual earnings result in a
relatively high rate of poverty among nursing assistants: 13 percent live below the federal poverty line.
269
Omnibus Budget Reconciliation Act of 1987, Pub. L. No. 100-203, Subtitle C: Nursing Home Reform (1987). The
Nursing Home Reform Law of 1987 (passed as part of the Omnibus Budget Reconciliation Act) requires these
facilities to have:
• A registered nurse eight consecutive hours, seven days a week
• Licensed nurses 24 hours a day re
• Otherwise “sufficient” nursing staff to meet residents’ needs
See 42 USC 1395i-3(b)(4)(C)(i)
270
Wofford, P. (2019, July 11). Nurses Say Staffing Ratios In Long Term Care Facilities Are Unsafe. Nurse.org.
https://nurse.org/articles/nurse-staffing-unsafe-long-care-facilities/
271
Centers for Medicare & Medicaid Services. Quality Improvement Organizations. (2020, July 13). CMS Directs
Additional Resources to Nursing Homes in COVID-19 Hotspot Areas.
https://qi.ipro.org/2020/07/13/cms-directs-
additional-resources-to-nursing-homes-in-covid-19-hotspot-areas/

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
C-10
272
In FY 2019, CMS proposed to revise 42 CFR § 483. 75 to permit facilities to more flexibily design their QAPI
programs to meet their facility needs. Medicare and Medicaid Programs; Requirements for Long-Term Care Facilities:
Regulatory Provisions To Promote Efficiency, and Transparency (85 FR 34737, 34738) available at
https://www.govinfo.gov/content/pkg/FR-2019-07-18/pdf/2019-14946.pdf
(page 34738).
273
In June 2020, CMS announced new state requirements to perform on-site surveys at nursing homes that have
experienced COVID-19 outbreaks or cases and starting in FY 2021 perform annual infection control surveys of 20
percent of nursing homes. The guidance also authorizes expanded survey activities related to additional aspects of
care once a facility enters Phase 3 (e.g., complaint investigations that do not involve immediate jeopardy);
https://www.cms.gov/files/document/qso-20-31-all.pdf
274
Centers for Medicare & Medicaid Services. (2020, July 22). Trump Administration Announces New Resources to
Protect Nursing Home Residents Against COVID-19.
https://www.cms.gov/newsroom/press-releases/trump-
administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
275
Centers for Medicare & Medicaid Services. Quality Improvement Organizations. (2020, August 13). National
CMS/CDC Nursing Home COVID-19 Training. https://qioprogram.org/nursing-home-trainings
276
Center for Disease Control and Prevention. Healthcare Workers. Training for Healthcare Professionals. (2020,
July 20). COVID-19 Prevention in Long-term Care Facilities.
https://www.cdc.gov/coronavirus/2019-
ncov/hcp/training.html
277
Center for Disease Control and Prevention. Healthcare Workers. Training for Healthcare Professionals. (2020,
July 20). Nursing Home Infection Preventionist Training Course.
https://www.cdc.gov/coronavirus/2019-
ncov/hcp/training.html
278
ahcancalED. (n.d.) Infection Preventionist Specialized Training - IPCO Version 2.
https://educate.ahcancal.org/p/ipcov2
279
Coronavirus Commission for Safety and Quality in Nursing Homes. (2020, July 7).
280
Centers for Medicare & Medicaid Services. (2020, July 22). Trump Administration Announces New Resources to
Protect Nursing Home Residents Against COVID-19 [Press release].
https://www.cms.gov/newsroom/press-
releases/trump-administration-announces-new-resources-protect-nursing-home-residents-against-covid-19
281
Center for Medicare & Medicaid Services. (2020, April 19). Trump Administration Announces New Nursing Homes
COVID-19 Transparency Effort [Press release].
https://www.cms.gov/newsroom/press-releases/trump-administration-
announces-new-nursing-homes-covid-19-transparency-effort
282
Centers for Medicare & Medicaid Services. (2020, August 16). COVID-19 Nursing Home Data.
https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/
283
Wright, D. R. (2020, March 13). Guidance for Infection Control and Prevention of Coronavirus Disease 2019
(COVID-19) in Nursing Homes (REVISED). Department of Health & Human Services. Centers for Medicare &
Medicaid Services. https://www.cms.gov/files/document/3-13-2020-nursing-home-guidance-covid-19.pdf
284
Wright, D. R. (2020, April 19). Upcoming Requirements for Notification of Confirmed COVID-19 (or COVID-19
Persons under Investigation) Among Residents and Staff in Nursing Homes. Department of Health & Human
Services. Centers for Medicare & Medicaid Services. https://www.cms.gov/files/document/qso-20-26-nh.pdf
285
Wright, D. R. (2020, May 6). Interim Final Rule Updating Requirements for Notification of Confirmed and
Suspected COVID-19 Cases Among Residents and Staff in Nursing Homes. Department of Health & Human
Services. Centers for Medicare & Medicaid Services.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
D-1
Appendix D: List of CMS Actions to Date
This list captures the actions that CMS has taken through August 6, 2020, to respond to the
COVID-19 pandemic in the United States.
(1) Initial Action to Prepare Healthcare Facilities (February 6, 2020)
(2) Screening of entrants into nursing homes (March 4, 2020)
(3) The use of PPE (March 10, 2020)
(4) Restriction of staff and visitors (March 13, 2020)
(5) Inspections and immediate jeopardy (March 23, 2020)
(6) COVID-19 Survey for Nursing Homes Webinar Series (March 23, 2020)
(7) Hospitals/laboratories can test for COVID-19 (March 30, 2020)
(8) Infection control responsibilities (April 2, 2020)
(8a) Emergency Declaration Blanket Waivers (April 9, 2020) (same as 23)
(9) Payment for COVID-19 testing doubles (April 15, 2020)
(10) Nursing homes must report cases to residents/families (April 19, 2020)
(11) Notification of Confirmed COVID-19 ... Residents/Staff (April 19, 2020)
(12) Independent COVID-19 Commission (April 30, 2020)
(13) Details to State Survey Agency directors (May 6, 2020)
(14) COVID-19 toolkit for Nursing Homes (May 13, 2020)
(15) Guidance on the reopening of nursing homes and related FAQs (May 18, 2020)
(16) COVID-19 survey activities (June 1, 2020)
(17) COVID-19 nursing home results from inspections (June 4, 2020)
(18) Coronavirus Commission membership (June 19, 2020)
(19) FAQs on nursing home visitation (June 23, 2020)
(20) The end of the emergency blanket waiver (June 25, 2020)
(21) Assistance from QIOs to hotspot nursing homes (July 10, 2020)

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
D-2
(22) Rapid point-of-care diagnostic devices and tests (July 14, 2020)
(23) New resources to protect nursing home residents (July 22, 2020)
(23a) Emergency Declaration Blanket Waivers (July 28, 2020)
(24) Reimbursement for counseling isolated residents (July 30, 2020)
(25) CMS Flexibilities to Fight COVID-19 (July 30, 2020)
(26) COVID-19 Nursing Home Data (Aug. 2, 2020)
(27) Nursing Home Data - Point of Care Device Allocation (Aug. 6, 2020)

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-1
Appendix E: Public Input Summary
1. Background
On behalf of the Coronavirus Commission for Safety and Quality in Nursing Homes (the
Commission), MITRE sought public input to align with the four Commission objectives and to
allow the public to formally note their support of nursing home residents and staff.
2. Purpose
Public feedback was sought as input for the Commission’s development of actionable
recommendations to CMS to evaluate and improve the ongoing novel Coronavirus (COVID-19)
response and support of nursing homes. Public input comments and resources were categorized
against the four Commission objectives:
• Objective 1: Identify best practices for facilities to enable rapid and effective
identification and mitigation of transmission of COVID-19 and other infectious diseases
in nursing homes.
• Objective 2: Recommend best practices as exemplars of rigorous infection control
practices and facility resiliency that can serve as a framework for enhanced oversight and
quality monitoring activities.
• Objective 3: Endeavor to identify best practices for improved care delivery and
responsiveness to the needs of all nursing home residents in preparation for, during, and
following an emergency.
• Objective 4: Leverage new sources of data to improve existing infection control policies
and enable coordination across federal surveyors, contractors, and state and local entities
to mitigate coronavirus infection and future emergencies.
Commission members had the opportunity to review public inputs categorized by objectives and
further into discussion themes during the second half of their convening schedule. Public input
was used to drive the identification of additional relevant, actionable interventions for CMS to
improve quality and safety in nursing homes.
3. Scope and Approach
Public input was received from a multitude of nursing home stakeholders: nursing home staff
and residents, essential care partners, family, friends, members of the long-term care industry,
and additional stakeholders or affiliated organizations. Minimal public input was received
through a public-facing email address; robust public input was received via a website-based
feedback form. MITRE published a press release to promote the website-based feedback form
option, noting the Commission’s objectives and intention to review and incorporate public
feedback into their recommendations.
The public input form was made live via the Commission website on July 6. MITRE formally
published the website-based public input press release on July 10, and accepted inputs via the
website-based form through July 18.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-2
Through the public input form, individuals and organizations had the opportunity to: express
their interest in the well-being of nursing home residents without providing additional comment;
express their interest in the well-being of nursing home staff without providing additional
comment; submit a 500-character open-ended comment providing their perspective as it aligned
to one of the four (4) Commission objectives; and/or provide an attachment up to five pages long
(e.g., formal letters, publications, or other resources).
In total, the Commission received 632 responses via the website-based feedback form.
• 214 entries focused on the well-being of nursing home residents without further
comment
• 29 entries focused on the well-being of nursing home staff without further comment
• 301 open-response entries addressed at least one Commission objective
• 87 entries included an attachment
• 1 empty open-response entry
These open-ended comments and attachments were assigned to one of the four (4) Commission
objectives; then, they were further categorized into (1) established themes derived from
Commission discussions during the first half of their convening schedule, (2) emerging
Commission discussion themes, and (3) new themes that emerged from the public input content.
The full list of themes includes: Testing/Screening, Equipment/Supplies/Personal Protective
Equipment (PPE), Cohorting, Social/Emotional Health, Essential Care Partner Support,
Communications, Workforce, Shared Accountability for Quality Management and Improvement,
Reporting, Survey/Assessment, Quality Control Policies and Practices, General Policy Guidance
and/or Requirements, Nursing Home Policies and Practices, Funding, and Other.
A summary of the public input was provided to Commission members. Commission members
had the opportunity to utilize the summary to refine their recommendations and action steps
associated with each recommendation. Specifically, public input commonly highlighted the need
for urgent coordinated action to support the continued operations of nursing homes. Many
comments also called for enhanced operational and support practices to create a more robust
environment of care that prioritizes resident, essential care partner, and staff quality of life and
safety. These comments largely aligned with and augmented the recommendations of the
Commission. This alignment is made clear in the tables that follow.
4. Alignment with Commission Objectives and Themes
The Commission received 301 open-ended comments from the public through the website-based
form. Each comment was first assigned to one of the four (4) Commission objectives to which it
primarily applied. These assignments displayed a primary focus on policy and process
recommendations in direct support of the health and well-being of nursing home residents,
essential care partners, and the nursing home workforce.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-3
Table 1: Number of Open-Ended Comments on Each Commission Objective
Commission Objective
Count of Open-
Ended
Comments
Objective 1: Identify best practices for facilities to enable rapid and effective
identification and mitigation of transmission of COVID-19 and other
infectious diseases in nursing homes.
39
Objective 2:
Recommend best practices as exemplars of rigorous infection
control practices and facility resiliency that can serve as a framework for
enhanced oversight and quality monitoring activities.
71
Objective 3: Endeavor to identify best practices for improved care delivery
and responsiveness to the needs of all nursing home residents in
preparation for, during, and following an emergency.
185
Objective 4
: Leverage new sources of data to improve existing infection
control policies and enable coordination across federal surveyors,
contractors, and state and local entities to mitigate coronavirus infection and
future emergencies.
6
Open-ended responses were then organized by theme. Comments were coded to multiple themes,
as appropriate. These assignments more specifically showed the public’s focus on social and
emotional health needs, workforce concerns, and essential care partner support. The following
table is a count of open-ended comments by theme.
Table 2: Number of Open-Ended Comments on Each Emerging Theme
Established or Emerging Theme Count of Open-Ended
Comments
Social and Emotional Health
72
Workforce
66
Essential Care Partner Support 55
Nursing Home Policies and Practices 51
Shared Accountability for Quality Monitoring and
Improvement
48
Cohorting Residents and/or Nursing Home Design 46
Testing and Screening 39
Equipment, Supplies, and PPE
33
Funding 27
General Policy Guidance and/or Requirements 24
Communications 23
Quality Control Policies and Practices 20
Other 17

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-4
Established or Emerging Theme Count of Open-Ended
Comments
Data Reporting 11
Surveys and Assessments 5
Further analysis by Commission objective and theme is provided in the following tables.
Commission discussion of the public input focused on identification and integration of actionable
proposals put forward by the public; therefore, priority actions that emerged from these
discussions are outlined in successive paragraphs.
Objective 1: Identify best practices for facilities to enable rapid and effective identification and
mitigation of transmission of COVID-19 and other infectious diseases in nursing homes.
Many open-ended comments corresponding with Objective 1 focused on direct provision of PPE
and robust testing and screening supplies to allow for near universal testing of staff and residents
in nursing homes. Responses also noted the need for direct support of the workforce through
expanded hazard pay and training, as well as enhanced workforce monitoring and coordination
across facilities to provide redundancy and support for facilities and communities facing staffing
constraints due to community outbreaks.
Table 3: Number of Open-Ended Comments on Objective 1 Themes
Themes
Count
Testing and Screening 20
Equipment, Supplies, and PPE 9
Funding 8
Data Reporting 6
Workforce 5
Quality Control Policies and Practices 4
General Policy Guidance and/or Requirements
3
Nursing Home Policies and Practices 3
Shared Accountability for Quality Monitoring and Improvement 3
Cohorting and/or Nursing Home Design 2
Communications 1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-5
Quoted and Summarized Open-Ended Comments:
• “As the first case of COVID-19 was announced … we locked down all long-term care
facilities and assisted living communities. We did that as a collective on March 8, 2020.
We began meeting daily via phone conference with nursing homes, assisted livings, and
independent living senior housing, public health, and emergency management. We
discussed protocols and practices to identify and isolate unwell residents, PPE and
testing. We have had zero cases.”
• “The residents are in jeopardy of infection from poor cleaning standards …”
• Provide (at no cost to nursing homes) all equipment and swabs necessary for rapid results
testing on-site in nursing homes, as well as an ongoing supply of PPE including gowns,
masks, N95s and face shields. The profit margin is too low for individual facilities to be
able to purchase these items
• Eliminate the practice of targeted testing and instead implement continual, thorough, &
mandated testing for all residents and staff
• There should be a registry of workers available when many nurses and CNAs are sick,
similar to hospital systems
• Provide funding for hero pay for staff during outbreaks and additional funding for
ongoing staff supports; count training and time worked as temporary nurse aide in
nursing homes towards CMS minimum 75 hours training requirement for long term
workforce support
• When the first cases were detected, staff trained in infection control should have been
hired to train and monitor staff, help them isolate individuals, disinfect the environment,
and monitor residents
• Create a standardized reporting tool to report infection spread accurately and
transparently to residents, family members, and community members
The following priority actions emerged from Commission members’ discussion of this public
input:
• Provide (at no cost to nursing homes) all supplies necessary for rapid results testing
on-site in nursing homes, as well as an ongoing supply of PPE. Low profit margins
prohibit adequate procurement of these items.
• Support continual, thorough, and mandated testing for all residents, staff,
and visitors.
• Identify workers available to provide surge support; provide funding for hazard pay
for staff during outbreaks; count on-the-job training toward training requirements for
direct care providers.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-6
• Standardize reporting tools to maximize accuracy and transparency of virus tracking
for residents, family members, and community members.
Objective 2: Recommend best practices as exemplars of rigorous infection control practices and
facility resiliency that can serve as a framework for enhanced oversight and quality monitoring
activities.
Open-ended comments corresponding with Objective 2 had a primary focus on the need for
additional coordination and planning at the state, regional, and federal level on reporting and data
requirements as well as for reimbursement and other payment planning. Responses noted the
burden of reporting to multiple systems from both a cost and time standpoint, as well as the lack
of perceived value from reporting, as analysis received back was not presented cohesively and in
an easy to access format. Additionally, responses associated with Objective 2 had a similar
secondary focus as Objective 1, focusing on policies that could be implemented that would
support a more robust and reliable workforce. Suggestions included enhanced testing and
screening availability and reliability, additional funding, and training and preparation of the
workforce.
Table 4: Number of Open-Ended Comments on Objective 2 Themes
Themes
Count
Shared Accountability for Quality Monitoring and Improvement 33
Workforce 26
Nursing Home Policies and Practices 13
General Policy Guidance and/or Requirements 12
Funding
10
Cohorting and/or Nursing Home Design 9
Testing and Screening 8
Equipment, Supplies, and PPE 7
Quality Control Policies and Practices 6
Essential Care Partner Support 5
Social and Emotional Health 5
Communications 4
Other
4
Data Reporting
2
Surveys and Assessments 2

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-7
Quoted and Summarized Open-Ended Comments:
• “Wh
at I’ve seen over and over again is the issue of unfunded mandates. CMS in D.C.
issues new regulatory requirements for all to follow and the 50 individual states that
control the payments do not increase the payments.”
• “As with every emergency, having a plan in place is imperative. The education,
preparedness and training of your staff will determine survival rates of both patients and
staff. The example is set by the leaders.”
• “As front-line staff must be out of work due to illness or positive test results, there must
be back-up staff who can commit to assignments of 4-6 weeks or longer.”
• “The risk to those individuals is from the virus coming into the facility from the outside,
either a staff member or once visitations are allowed, from a family member. Either
source can break infection control protocols. For either party, education and information
on using social distancing and masking while in the outside community is critical. This is
essential.”
• “Unfortunately, each home is doing things differently to try to control the situation. A
clear AMDA recommendation for prevention/isolation that I could point to would help -
each home is doing a mix of CDC, state Health Dept, and in-house ideas, some working
better, some not at all.”
• Focus on finance reform of nursing homes and their stakeholders in US politics
• Ensure equity in the quality of care and outcomes for nursing home residents and staff of
color
• Offer alternatives to nursing home services for elder care
• Prioritize advanced care planning and hospice care for residents
The following priority actions emerged from Commission members’ discussion of this public
input:
• Attach additional funding to regulatory requirements to facilitate their
implementation.
• Have an emergency plan in place and make sure that nursing homes continuously
educate and prepare their staff and residents to implement that plan.
• Identify back-up staff who can provide direct care when the regular staff is out
sick or in quarantine.
• Provide equipment, testing, and infection control resources to nursing home staff
and visitors.
• Create a clear single-source set of recommendations for nursing homes and their
families.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-8
• Offer alternatives to nursing home services for elder care. Prioritize advanced care
planning and hospice care for residents.
Objective 3: Endeavor to identify best practices for improved care delivery and responsiveness
to the needs of all nursing home residents in preparation for, during, and following an
emergency.
Open-ended comments corresponding with Objective 3 were most numerous. The public was
especially pointed in their remarks on the social and emotional health of residents, and the ability
of essential care partners to provide meaningful support to residents during the COVID-19
outbreak. Additionally, workforce training and enhancement of staffing levels, facility
infrastructure, policy modifications for cohorting, and improved communication of policies for
essential care partners were noted as essential.
Table 5: Number of Open-Ended Comments on Objective 3 Themes
Themes Count
Social and Emotional Health 61
Essential Care Partner Support 55
Workforce 43
Cohorting and/or Nursing Home Design 36
Nursing Home Policies and Practices
35
Communications 12
Shared Accountability for Quality Monitoring and Improvement 12
Funding
9
General Policy Guidance and/or Requirements 9
Quality Control Policies and Practices 9
Equipment, Supplies, and PPE 7
Other 7
Testing and Screening 7
Data Reporting 6
Surveys and Assessments
1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-9
Quoted and Summarized Open-Ended Comments:
• “My 94-year old mother is in a long-term care facility… I’m sure the intentions were
good when the nursing home lockdown went into effect and probably most of us did not
expect the COVID-19 crisis to go on indefinitely. Well, it has and this isolation that was
intended to protect seniors is ironically killing them. Mom has dementia and cannot
comprehend the situation. I go to the window every morning to let her know she is not
forgotten but it’s not always a pleasant start to the day. In fact, sometimes it’s very
upsetting to see the sadness and desperation on her face. The decision has been made for
Mom and thousands of her peers to choose longevity over quality of life. This includes
many folks on hospice for whom longevity is out of the question – they are simply
robbed of their quality. For people with dementia like my mother, today is their best day.
Tomorrow will be a little worse and who knows if there will be a six-months from now…
We are losing precious time.”
• “It is hard to imagine an infection control scheme working well if staff is underpaid and
forced to make difficult decisions for child and dependent care.”
• “While keeping loved ones safe from COVID-19 there needs to be methods to support
their emotional and mental health as well with in person family/collateral contact.”
• “When nursing homes are built, the ideal is private rooms with three fixture bathrooms.
Of course, the expense of building that model is often prohibitive, so the infrastructure
we have in place is often buildings from the 70’s with long institutional corridors and
mostly semi-private rooms. Newer homes that are built try to include more privacy and a
homelike character, but financing is difficult for this level of care, so compromises are
made in order to build or renovate at all...”
• “My Mom contracted COVID-19 in a skilled nursing facility and subsequently died from
it. The lack of communication and transparency from the skilled nursing home is
inexcusable. I was not directly informed that the nursing home was closed to visitors, nor
was I provided any communication or information regarding the protocols put into place
to protect staff and residents from the coronavirus. We were never given the option to
make the best decision about her placement during this pandemic.”
• “The care for nursing home consumers is costly, and now the cost remains the same
while the services that are paid for with that hefty fee are non-existent. Older adults are
losing their cognitive capabilities, losing their physical capabilities and morale is low. “
• “CMS should continue to hold routine discipline specific COVID-19 calls. These calls
have provided a great opportunity for providers to hear directly from CMS as well as ask
questions and raise pertinent issues, concerns or points of clarifications and receive
responses in real time. CMS should continue to provide tools such as the Focused
Infection Control Self-Assessment. This tool was valuable asset in navigating COVID-19
in the long-term care and skilled nursing setting.”
• “I want to go on record as saying that I will submit to COVID testing, I will wrap up in
PPE and be very diligent in sanitizing my hands etc. in order to have physical contact

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-10
with my only parent. If those guidelines are appropriate for nursing home staff, they
should be more than appropriate for immediate family members.”
• The direct care staff need targeted training, adequate equipment and supplies, stress and
grief support, and access to paid leave and other benefits. Addressing these needs is
necessary to ensure this workforce can provide continuous, quality care for nursing home
residents in emergencies and in general
• Allow hospice workers to be considered essential, work with facilities and hospice on
testing to gain entry to the facility, facilitate telecommunication communication for
hospice residents, and consider the unintended consequences of the 3-day qualifying stay
waiver for residents on hospice who are required to revoke to get their SNF benefit
• Ensure that nursing homes have access to up-to-date treatment options for COVID-19
• End nursing homes in favor of another option for elder care
The following priority actions emerged from Commission members’ discussion of this public
input:
• Provide targeted training, adequate equipment and supplies, stress and grief
support, and access to paid leave and health benefits to direct care providers.
• Identify alternative methods to get the physical and emotional support to
residents while their essential care support teams are unable to provide care in person
• Ensure that residents and their family members have considered advanced care
planning, hospice care, and other care options.
• Ensure that nursing homes have access to up-to-date treatment options for COVID-19
• Consider the unintended consequences of the 3-day qualifying stay waiver for
residents on hospice who are required to revoke to get their SNF benefit
Objective 4: Leverage new sources of data to improve existing infection control policies and
enable coordination across federal surveyors, contractors, and state and local entities to mitigate
coronavirus infection and future emergencies.
Open-ended comments corresponding with Objective 4 were by far the least numerous; however,
it was noted these adjustments would be critical for intervention support. Input focused on
suggestions and recommendations to streamline and make data collection less burdensome;
moreover, there was a call for metrics that specifically support targeted measures for infection
and quality control.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-11
Table 6: Number of Open-Ended Comments on Objective 4 Themes
Themes
Count
Other
3
Quality Control Policies and Practices
2
Shared Accountability for Quality Monitoring and Improvement
2
Cohorting and/or Nursing Home Design 1
Data Reporting
1
Equipment, Supplies, and PPE
1
Surveys and Assessments
1
Summarized Open-Ended Comments:
• Leverage the 9/26/19 CMS Final Rule on Discharge Planning as a tool to improve the control
of Coronavirus in nursing homes (local, state, federal levels), supporting facilities to address
problems and ensuring funds go to nursing home needs, not enforcement
• Align data collection efforts (local, state, and federal levels) to provide reliable, actionable
data and clear and consistent information for the public.
• Use data to support identification of resources needed by nursing homes (including enhanced
funding, PPE, testing, workforce)
The following priority actions emerged from Commission members’ discussion of this public
input:
• Leverage tools from the local, state, and federal levels to improve defenses against and
responses to COVID-19.
• Align data collection efforts to provide reliable, actionable data and clear and consistent
information for the public.
• Use data to identify resources needed by nursing homes (including enhanced funding,
personal protective equipment, testing, workforce, etc.).
The Commission received 87 attachments in the form of scholarly publications, organizational
briefs and memos, organizational and personal letters, news articles, and additional resources via
the website-based form. These documents or websites were prioritized for review using the
following matrix.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-12
Table 7: Number of Attachments by Rating
Score Rating Count Description
5
Outstanding
15
Focal point is uniquely displayed and developed;
Closely aligned to the Commission objectives;
Publication includes analysis, synthesis, and
interpretation of ideas— leads to a sense that the piece
could withstand critical analysis by experts in the
discipline.
4 Very
Satisfactory
22 Displays clear, well-developed focal point; Aligned to the
Commission objectives; Publication includes analysis,
synthesis, and interpretation of ideas throughout.
3 Satisfactory 28 Displays adequately developed focal point; Somewhat
aligned to the Commission objectives; Includes analysis,
synthesis, and interpretation of ideas in most parts of
the publication.
2 Unsatisfactory 16 Displays a focal point, although not clearly developed;
Loosely aligned to the Commission objectives;
Publication includes little analysis, synthesis, and
interpretation of ideas.
1
Poor
6
Assignment lacks a clear and concise point; Not aligned
to the Commission objectives; Publication includes no
analysis, synthesis, and interpretation of ideas.
The Commission received a summary, which included origin, key points, and score.
Attachments included multiple formats including:
• Scholarly Articles:
o Past non-COVID-19 related scholarly articles on process and program
improvement for nursing homes and long-term care facilities.
o COVID-19 related scholarly articles on process and program improvement for
nursing homes and long-term care facilities.
• Grey Literature:
o Position Briefs, Letters, and Memos from practice groups and network
organizations representing nursing home and long-term care providers and
facilities.
o Industry reports and white papers.
o Investigative reports.
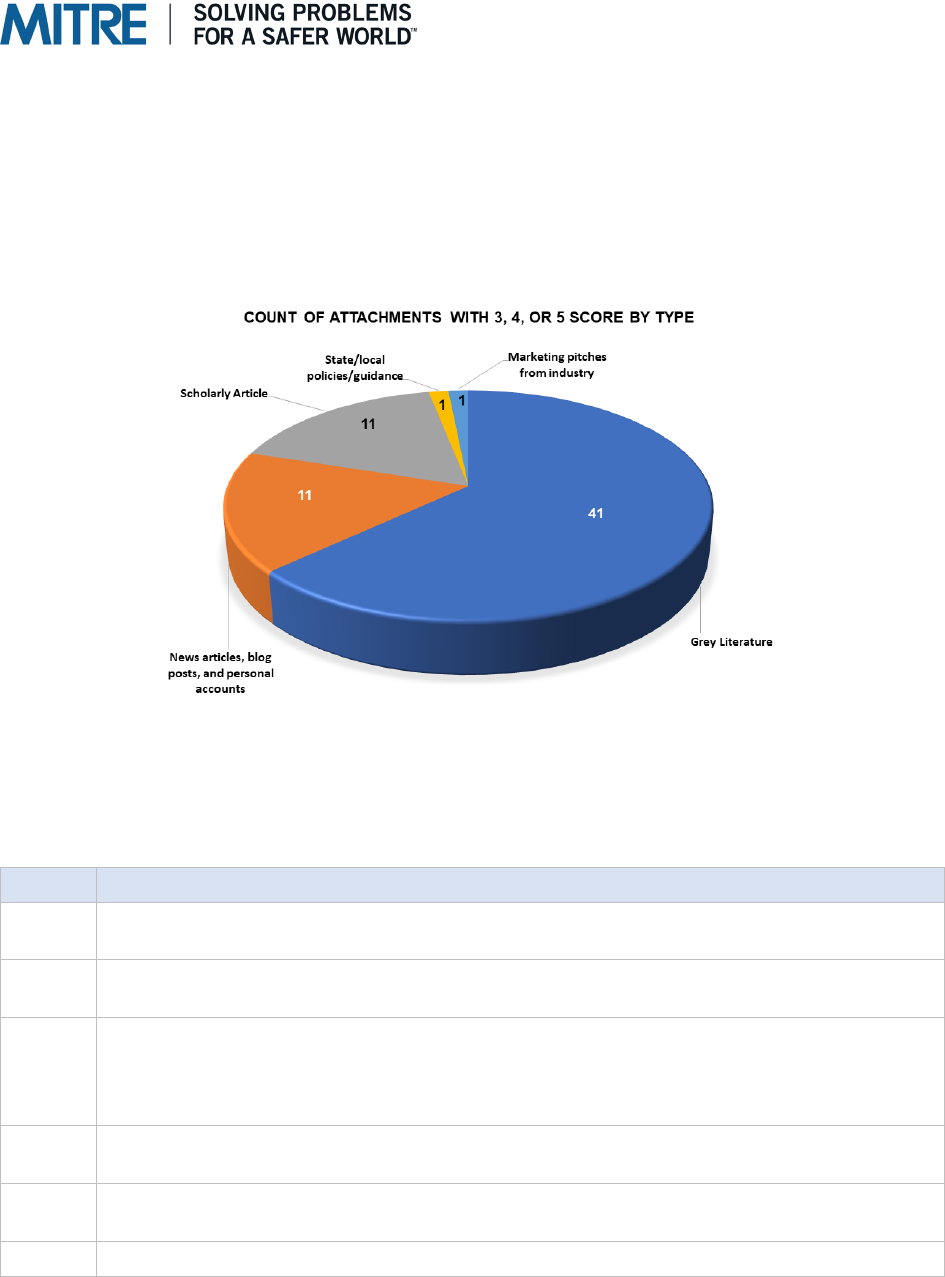
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-13
• State and local policies and guidance
• News articles, blog posts, and personal accounts
• Marketing pitches from industry stakeholders for specific equipment/tools.
Attachments with scores of 3, 4, or 5 were mapped to these categories, and the results are noted
in the following chart:
Figure 3: Distribution of Content Types for Attachments Scoring 3 – 5
The following table lists the identification numbers and attachment summaries.
Table 8: Attachment Summaries
ID
Attachment Summary
1
Article: NH fought federal emergency plan requirements for years and how to rectify
it for the future
4
Scottish Article: Scotland move to national care homes and the recommendation that
US also move to that model
10
2020 Letter from Congress: A clinician list would be of enormous value for public
health agencies to address preparedness for influenza, norovirus, and other
seasonal outbreaks as well as another emergency uses during the COVID-19
pandemic
11
2018 Letter submission about adequate medical oversight and establishing and
maintaining a national database of Nursing Home medical directors
12
Submitted Public Comment on Examining the COVID-19 Nursing Home Crisis – The
Society for Post-Acute and Long-Term Care (PALTC)
13
Article on 5 Keys to Solving COVID-19 Crisis
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-14
ID
Attachment Summary
14
Whitepaper about reopening America and managing COVID risk for nursing home
population in six parts
41
Article on the impact of peer mentoring of loneliness, depression, and social
engagement in long-term care from cohorting/grouping residents
46
Investigative report focused on performance data between for-profit nursing homes
and not-for-profit nursing homes
48
NY State Senate letter to Gov. Cuomo: Recommendations to address adult care
facilities vulnerabilities exposed during the COVID-19 crisis at nursing homes, adult
homes, and assisted living facilities
79
Resource letter: Social Workers working in Nursing Homes - Support System/Group
93
Whitepaper: Behavioral Healthcare in Long Term Care Facilities under COVID-19
Restrictions: A Blueprint for Mental Health Crisis
95
NYT Article: Nursing homes legal protections/provisions included in the NY budget
bill to protect against lawsuits that are COVID-19 related
96
Policy: Indiana State Department of Health Essential Family Caregivers in Long
Term Care Facilities
97
Article outlining the importance of implementing guidance for the need of having "an
essential family caregiver" program to support residents during uncertain times
98
Excerpt subchapter from the Assisted Living Facility Regulation: 8:36-18.1-2 -
Infection Control Program. Excerpt copied and pasted without any
explanation/recommendation
99
Article outlining the symptoms of dementia affecting resident needs and behavior
impacting staff workload. A Cognitive acuity assessment tool developed to list out
the symptoms of dementia
102
Individual Contributor: Highlighting the need for a stronger presence of RNs in
nursing homes and request CMS reforms to RN staffing levels
117
Visual picture highlighting Antifungal and Antibacterial Medical Textiles to interrupt
pathogen transfer to corroborate the Stay Fresh Technology
133
Corporation for supportive Housing Website highlighting their integrated and
supportive housing models
134
Blog post about COVID-19 nursing home conditions focused on residents' rights and
provides instructions for resident empowerment during restrictions and strategies for
visitation
173
Personal account - in-depth overview of experience of individual with mother in long-
term care facility in Oregon, Ohio
216
Part of American Academy article on the effects of social isolation on older adults
219
Promotion of Macy Catheter for non-IV medication and fluid delivery to patients
224
Proposal to test communities through wastewater testing for COVID-19 to detect
problem areas
226
Letter from Pro Senior nonprofit organization advocating for enhanced family
visitation policies at national level
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-15
ID
Attachment Summary
231
The Center for Medicare Advocacy recommendations for a coordinated national
solution and suspension of waivers for federal law and regulation governing nursing
facilities
233
Scholarly article noting recommended strategies for overall improvement of
conditions in US nursing homes based on analysis of international and domestic
policy as well as site conditions in US
235
Leading Age PA making wide ranging suggestions for approach to improvement of
operations and support of nursing homes in US specific to COVID-19 challenges
237
Kaiser Family Foundation report- "Improving the Financial Accountability of Nursing
Facilities". (Published 2013, not COVID specific but relevant)
238
Proposed policy brief advocating for an at-home model for care versus congregate
settings by the Roads to Freedom Center for Independent
239
Blog post from 7/8/20 from McKnight's Long-Term Care News site "Delaying death
not enough for nursing home residents"
241
Letter from American Association of Post-Acute Care Nursing (AAPACN) suggesting
two short term actions and longer-term actions to support each of the four
commission areas specific to Skilled Nursing Facilities
242
Briefing from Nursing Home National Association for Home Care & Hospice (NAHC)
on multiple observations of developments in the relationship of hospice providers
and facilities during the COVID-19 pandemic. Focuses on access to care to hospice
services in facilities
252
Personal account as article on being a caregiver for aunt pre-COVID-19, references
benefits from non-visitation policies with harm caused by them and advocates for
revisit of policies
255
Policy brief from American Geriatrics Society specific to COVID-19 and Nursing
Homes based on information available as of 4/4/2020
258
Scholarly article highlighting best practice strategies for Geriatric providers to
respond to the emergent COVID-19 pandemic within their patient bases.
Recommends strategies to identify infection, manage COVID-19 cases within and
outside of long-term care environments, and identify and implement national,
regional, and local policies
259
American Geriatrics Society policy statement on Resource Allocation and COVID 19
- companion article to item 260. Focuses on urgent need for advance care planning,
achieving justice in resource allocation, and legal considerations - companion article
to item 260
260
American Geriatrics Society policy statement on Rationing Limited Healthcare
Resources in the COVID-19 Era and Beyond: Ethical Considerations Regarding
Older Adults - companion article to item 259
261
News article titled "Social Isolation - the Other COVID-19 Threat in Nursing Homes"
262
American Geriatrics Society policy statement on Coronavirus Disease19 in Geriatrics
and Long-Term Care: An Update. Presents wide-ranging suggestions for long-term
care facility management and policy including

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-16
ID
Attachment Summary
267
Letter by US Against Alzheimer's specific to COVID-19 and effect on Alzheimer’s
residents in long-term care facilities
270
Scholarly article highlighting results of study comparing the level of nursing staffing
levels and COVID-19 cases in long-term care facilities in California
277
Letter from the Association for Linen, Uniform, and Facility Services (TRSA)
highlighting proposed strategies to enhance infection prevention and employee
safety while reducing costs through the outsourcing of linen management
279
Article by The American Geriatrics Society overviewing results from review of
COVID-19 Infections and Deaths among Connecticut Nursing Home Residents:
Facility Correlates
285
Memo from Continuing Care Leadership Coalition (CCLC), representing member
long-term care facilities, highlighting best practices observed/identified by the
organization to inform safety and quality improvement in nursing homes and other
long-term care facilities
288
Memo from the American Health Care Association (AHCA), National Center for
Assisted Living (NCAL), and the National Hospice and Palliative Care Organization
(NHPCO) on Guidance on the Role of Hospice Services in LTC Facilities During the
COVID-19 pandemic
291
This is a sales pitch from a software company. There are some considerations when
implementing training for example, but it’s an invitation to work with this company to
leverage data to combat infections
293
Suggestions/Recommendations to the Coronavirus Commission for Safety and
Quality in Nursing Homes from the Patients’ Rights Help Line of the New York
Statewide Senior Action Council
295
The Partnership for Inclusive Disaster Strategies recommendations on including
Centers for Independent Living in emergency response, enforcing the Olmstead
decision and pursing cohorting design of one person per room
296
The Partnership for Inclusive Disaster Strategies recommendations to reduce
staffing shortages
297
The Partnership for Inclusive Disaster Strategies request for Attorney Generals to
investigate allegations at nursing homes
300
National Governor's Association call for emergency relocation of residents in
congregate settings
302
Letter from the Service Employees International Union (SEIU) that advocates for
updating staffing levels in nursing homes, providing staff with appropriate PPE and
COVID-Testing, offering hazard pay and wages, and ensuring paid sick leave
305
Families for Better Care recommendation to use nursing home fines to enable
molecule point-of-care rapid testing machine in every facility
306
Disability Rights of North America appeal to NC health department to study COVID
rates and respond appropriately
307
Information for a hospice and palliative care company

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-17
ID
Attachment Summary
308
American Occupational Therapy Association appeal to provide access to PPE for
therapy practitioners, extend telehealth flexibilities, and continued resident access
309
Individual contributor suggestions on changes in nursing home policies and practices
including molecular POC rapid testing at every facility, one essential care
partner/resident, and improving infection prevention measures
311
Neighbors to Save Rivington House recommendations on infection control,
government oversight, and long-term care
315
Editorial on a staged approach to optimizing medication management during this
pandemic
316
Alzheimer’s Association Policy recommendations in the areas of providing testing,
reporting, PPE, communications for residents and families, and surge support
318
Medicaring.org editorial about the increase in nursing home deaths due to COVID. It
is a passionate appeal to minimize the number of deaths while also addressing
those residents
319
Medicaring.org recommendations on resident-centered preferences in advance of
illness, treatment of respiratory failure, testing, regional planning process, and
removal of bodies in a timely manner
320
Medicaring.org editorial on rethinking facility-based long-term care (the aims,
financing, and place in society)
323
Unfinished tool to organize testing and interventions for residents suspected with
COVID-19
324
#VisitationSavesLives This entry is an infographic
327
AARP urges action on a five-point plan to slow the spread and save lives
329
Massachusetts Advocates for Nursing Home Reform recommendations on infection
control, communications, testing, workforce and cohorting
331
Consortium for Citizens with Disabilities requests the commission to provide
recommendations in addressing the needs of people with disabilities and older
adults in all types of congregate facilities, not just nursing homes
333
Care for Advocacy and the Rights and Interests of the Elderly recommendations to
mitigate crisis of prolonged isolation in long-term care facilitates
338
Individual contributor focused on raising awareness of wound care and common to
COVID 19 occurrences
341
National Governor's Association call for emergency relocation of residents in
congregate settings
347
Letter from the Avila Institute of Gerontology with several recommendations for the
Commission for how nursing homes can better prepare for emergencies or
pandemics
348
Detailed petition from the American Civil Liberties Union (ACLU) advocating for
better care for staff and residents that includes multiple data sources for each of their
recommendations

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-18
ID
Attachment Summary
349
Journal of Geriatric Emergency Medicine article that describes the challenges of
how to safely transfer to and from hospital and nursing home settings and offers
recommendations
352
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
355
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
356
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
358
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
361
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
362
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
369
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
370
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
381
Letter to provide the Commission with a narrative of how challenging it has been to
keep COVID-19 out of their nursing home
385
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
388
Journal of Geriatric Emergency Medicine article that describes the challenges of how
to safely transfer to and from hospital and nursing home settings and offers
recommendations
5. Alignment with Principal Recommendations
Open-ended comments and attachments are associated with many final Commission
recommendations. Many open-ended comments and attachments align to Commission
recommendations by relationship of a stated problem in the comment and solution provided by
the Commission recommendation(s). Some open-ended comments and attachments provided
specific recommendations in direct alignment with the Commission recommendations; those are
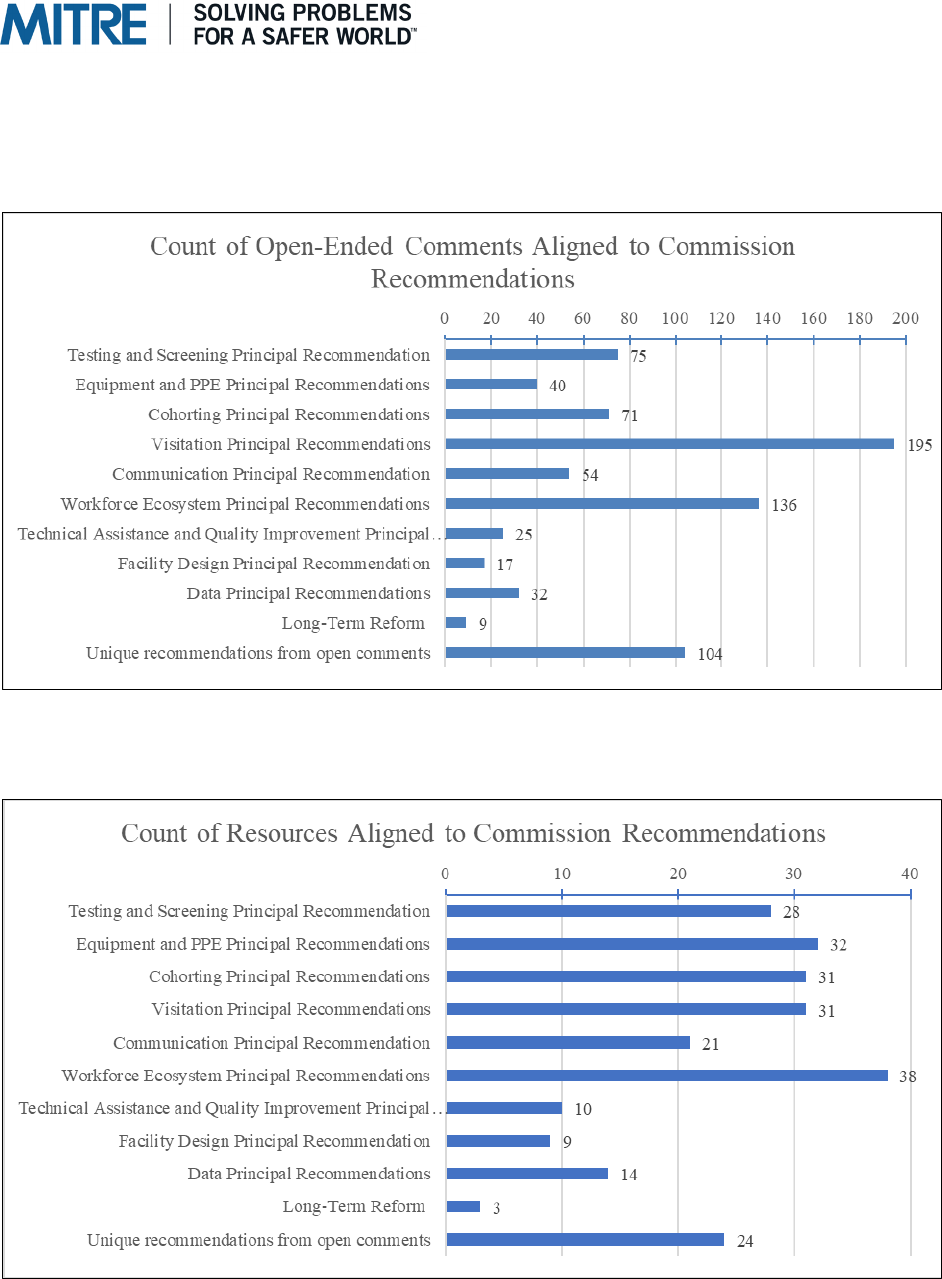
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-19
noted in the following tables. Open-ended comments and attachments that provided
recommendations unique from Commission recommendations are noted as “Unique
recommendations from open comments/resources.” The following charts show the total number
of associations by recommendations for open-ended comments and attachments.
Figure 4: Aligning Open-Ended Comments to Commission Recommendations
Figure 5: Aligning Resources to Commission Recommendations

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-20
5.1. Infection Prevention and Control
Six principal recommendations were developed by the Commission in the infection prevention
and control category grouping. The Commission was influenced by public input from essential
care partners, nursing home staff and administrators, and industry representatives, especially in
consideration of the balance between infection prevention and control policies (e.g., cohorting
and restricted visitation) and emotional health and well-being of residents. To support an
adjustment of policies to lessen the impact and allow for some measure of visitation and support,
the Commission noted that enhanced training of staff, provision of PPE, and availability of rapid
testing would be crucial to do so without opening the door to increases in infection.
Testing and Screening Principal Recommendation:
• Principal Recommendation 1A: Immediately develop and execute a national strategy,
coordinating with federal partners and SLTT authorities, for testing and delivering rapid
turnaround of results (i.e., results in less than 24 hours) in nursing homes, in combination
with CDC-recommended screening protocols. Allow nursing home owners and
administrators to tailor the strategy based on community prevalence and resource availability
in partnership with federal and SLTT authorities.
Summary: Addresses public input noting the need for more widely available and rapid
testing and screening to support cohorting and visitation policies that can enhance social and
emotional health and critical workforce availability. Notes the importance of increasing the
protection of existing workforce members as many facilities are already understaffed and
struggle to recruit. Enhanced testing and screening was widely noted as the best solution to
ensure the efficient use of staff across facilities, especially considering staff supporting
multiple sites.
Count of Aligned Open Comments: 75
Specific Recommendation(s) from Open Comments:
• Require more robust testing and screening of residents (not just those with high fever) to
capture additional infectious residents before they are contagious
• Require testing for staff traveling between facilities
• Implement and support widespread, continual, and mandated testing for all nursing home
staff
• Complete testing prior to admission or transfer from outside facilities
• Provide a direct provision of tests to nursing homes
• Prioritize nursing homes in first tier testing and test processing
• Guarantee by federal order sufficient testing materials and resources for nursing homes
Count of Aligned Attachments: 28

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-21
Specific Recommendation(s) from Attachments:
• Begin immediate and repeated rapid-result testing of all residents and staff of nursing
homes
• Require facilities to test all nursing home workers and residents at least weekly
• Provide nursing homes with priority access to rapid response point of care testing, make
more tests and related supplies available, and expand capacity of testing labs to expedite
result times
• Implement a molecular point-of care rapid testing machine at every nursing home
• Review measures to ease the challenge of testing costs borne by facilities
• Ensure funding and support for actions required to meet new guidelines by facilities
• Institute cost-based reimbursement
Equipment and PPE Principal Recommendations:
• Principal Recommendation 2A: Assume responsibility for a collaborative process with
federal and SLTT partners to ensure nursing home owners and administrators can procure
and sustain a three-month supply of high-quality supplies of PPE. This process must provide
accountability and oversight.
• Principal Recommendation 2B: Provide specific guidance on the use, decontamination, and
reuse of PPE, working with federal partners, including CDC, FDA, and OSHA.
• Principal Recommendation 2C: As needed, collaborate with other federal and state agencies
to provide guidance on training to all clinical and nonclinical facility staff on proper use of
PPE and equipment, according to available manufacturer specifications.
Summary: Addresses public input noting the need for enhancement of PPE supply chain to
ensure safety of residents and nursing home workforce.
Count of Aligned Open Comments: 40
Specific Recommendation(s) from Open Comments:
• Provide a direct provision of PPE to nursing homes
• Ensure adequate PPE is provided to all nursing homes for staff and visitors
• Track PPE locally, statewide, and regionally
• Build stockpile to prepare for a surge/ensure access to resupply
• Prioritize nursing homes with or higher than hospitals
Count of Aligned Attachments: 32
Specific Recommendation from Attachments:
• Provide nursing homes with priority access to PPE

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-22
Cohorting Principal Recommendations:
• Principal Recommendation 3A: Update cohorting guidance to balance resident and staff
psychological safety and well-being with infection prevention and control.
• Principal Recommendation 3B: Update cohorting guidance and reimbursement policy to
address differences in nursing home resources (e.g., facility, infrastructure, staff).
Summary: Addresses the public input noting the importance of social and emotional health
and need for evidence-based policies regarding cohorting, nursing home design, and
visitation. The public noted that there is significant work to be done as to the costs and
benefits of restrictive policies to prevent outbreaks versus the consequences of minimal care
and decreased socialization.
Count of Aligned Open Comments: 71
Specific Recommendation(s) from Open Comments:
• Require hospitals to test residents 48 hours prior to discharge to a nursing home
• Never require facilities to accept residents with highly infectious disease
• Study effects of isolation and lack of visitation on residents with mental health conditions
Count of Aligned Attachments: 31
Specific Recommendation(s) from Attachments:
• Relocate residents to a one person per room setting with community care and appropriate
staffing
• Implement peer mentorship programs in facilities to combat loneliness and depression
• Allow residents to determine visitation practices for their personal requirements
• Establish an expedited Transition Taskforce that would bring together key stakeholders,
policy and decision makers, providers, experts, and advocates to identify systemic
barriers and create innovative solutions for cohorting
5.2. Quality of Life – Visitation and Communications
Five principal recommendations were developed by the Commission in the quality of life
category grouping. The Commission noted how important addressing the quality of life,
especially emotional and mental well-being, of nursing home residents is to the public.
Moreover, the Commission noted the call for essential care partners to be able to return to
supporting their loved ones. The Commission also recognized the importance of planning and
timely communication as a central to quality of life concerns outlined in the public input.
Visitation Principal Recommendations:
•
Principal Recommendation 4A: Emphasize that visitation is a vital resident right. Update and
release consolidated, evidence-based guidance on safely increasing controlled, in-person
visitation prior to federal Phase 3 reopening.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-23
• Principal Recommendation 4B: Update and release consolidated, evidence-based guidance
on effectively planning for and implementing virtual visitation tools and techniques.
•
Principal Recommendation 4C: Provide resources to help nursing home staff assess and
improve the mental health and psychosocial well-being of residents during and after the
pandemic.
•
Principal Recommendation 4D: Assess, streamline, and increase the accessibility of COVID-
19-related directives, guidance, and resources on visitation into a single source.
Summary: Addresses the public input noting the importance of social and emotional health
and better coordination with essential care partners. Also addresses the need for additional,
timely communication with residents as to the purpose of various policies and built
infrastructure adjustments due to emergencies, especially related to cohorting and other
restrictive measures. Communications about provision of additional resources and/or
modified programming and polices are also addressed here.
Count of Aligned Open Comments: 195
Specific Recommendation(s) from Open Comments:
• Rescind the benchmark of no newly acquired cases inside facilities for 28 days to allow
for family/caregivers to visit residents
• Allow residents to identify 1-2 visitors (not limited to family) who undergo screening,
testing, and safety precautions (PPE) for scheduled weekly visits
• Require nursing homes to have resources to enable some level of family visitation now
• Add mental health boosting activities including social interaction to residents’ care plans
during times of emergency
• Ensure individual care plans address total well-being needs of residents regardless of
context
Count of Aligned Attachments:
31
Specific Recommendation(s) from Attachments:
• Require facilities to establish policies and procedures for how to designate and utilize an
essential care partner
• Allow residents to designate one “compassionate caregiver” who can visit the resident
daily and follow the same screening, testing, and PPE protocols.
• Continue preventative isolation of members who prefer and allow visitation in separate
area for residents who prefer that
• Lift the restrictions on visitations
• Allow for the managed admission of both primary and behavioral health clinicians to
sites for direct, in-person care and support of these residents
• Implement peer mentorship programs in facilities to combat loneliness and depression

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-24
Communication Principal Recommendation:
• Principal Recommendation 5A: Increase specificity and expand breadth of guidance on
communications between nursing home staff, residents, and families.
Summary: Addresses the public input noting the importance of unified, accessible, and
streamlined communication, including about nursing home policies and protocols.
Count of Aligned Open Comments: 54
Specific Recommendation(s) from Open Comments:
• Make family councils mandatory, not optional
• Increase essential caregiver contact via Skype/video tech with family members
• Set up regular times for provider and family member communication, and encourage
providers to contact families on a regular basis to provide updates on residents
Count of Aligned Attachments: 21
Specific Recommendation(s) from Attachments:
• Require transparency around COVID-19 data (cases and deaths) in nursing homes,
transfer and discharge rights, and provider relief funds utilization
• Facilitate ongoing meaningful engagement of residents, families, and their advocates
• Ensure any family member who had visitation rights to see their family member prior to a
pandemic declaration is provided with the right to obtain regular updates on resident’s
status as well as afforded assistance by the Ombudsman and the facility staff in arranging
video calls
5.3. Workforce—Ecosystem and Technical Assistance
Ten principal recommendations were identified by the Commission in the workforce category
grouping. The Commission noted the public’s views that a stable workforce with appropriate
staffing to resident ratios in emergencies saw better outcomes. Additionally, the Commission
noted the public’s perspectives that increased infection prevention and control training for and
availability of staff would allow for heightened facility preparedness and functionality.
Workforce Ecosystem Principal Recommendation(s):
•
Principal Recommendation 6A: Mobilize resources to support a fatigued nursing home
workforce and assess minimum care standards.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-25
• Principal Recommendation 6B: Provide equity-oriented guidance that allows nursing home
workforce members to safely continue to work in multiple nursing homes while adhering to
infection prevention and control practices.
•
Principal Recommendation 6C: Support 24/7 RN staffing resources at nursing homes in the
event of a positive SARS-CoV-2 test within that facility.
•
Principal Recommendation 6D: Identify and immediately leverage certified infection
preventionists to support nursing homes’ infection prevention needs.
•
Principal Recommendation 6E: Require nursing homes to employ infection preventionist(s)
with educator capabilities.
•
Principal Recommendation 7A: Catalyze interest in the CNA profession through diverse
recruitment vehicles; issue guidance for on-the-job CNA training, testing, and certification;
and create a national CNA registry.
•
Principal Recommendation 7B: Professionalize infection prevention positions in nursing
homes by updating regulations at 42 CFR § 483.80 so more fully qualified infection
preventionists are available to serve in nursing homes.
•
Principal Recommendation 7C: Catalyze the overhaul of the workforce ecosystem in
partnership with federal, SLTT, other public, private, and academic partners.
•
Principal Recommendation 7D: Convene a Long-Term Care Workforce Commission to
assess, advise on, and provide independent oversight for modernization of workforce
ecosystem.
Summary:
Addresses public input noting importance of protecting the workforce to ensure
essential care continues to be provided; enhancing training to ensure a constant state of
readiness for outbreaks; supporting critical staffing ratios proven to drive more positive
outcomes; and providing funding through enhanced reimbursement rates or incentives to
maintain care standards. Input included scholarly articles reviewing studies from multiple
geographic areas that tied resident outcomes and infection rates to the staffing levels of
various facilities.
Count of Aligned Open Comments:
136
Specific Recommendation(s) from Open Comments:
• Ensure facilities are prepared with an emergency preparedness plan; include workforce
readiness
• Ensure that minimum staff to resident ratios are consistent with HR5216/S2943. 4.1
hours per resident per day to promote infection control & quality of care
• Mandate at least 4.1 hours of direct care per 24-hour period for all residents of nursing
homes and at least 5.1 hours for residents of memory care wings and residents needing
total care

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-26
• Require all nursing home to have an infection control manager whose job is to monitor
staff to ensure compliance and prevent the spread of infection
• Hire staff trained in infection control policies to train and monitor staff, help them isolate
individuals, ensure a clean environment, and monitor residents
• Ensure staff is specially trained in infection control, provide increased compensation for
infection control champion(s), and offer recognition as professionals in their field
• Establish training contact hour minimums for staff
• Create registry of backup and flexible staff to backfill staff that must be out of work due
to illness or positive test for nursing homes similar to hospital systems
• Increase available funding and pay for Certified Nursing Aids (CNAs)
• Mandate unified training for nursing home staff on national level
Count of Aligned Attachments: 38
Specific Recommendation(s) from Attachments:
• Require nursing facilities to pay staff hazard pay during the pandemic
• Pay staff who test positive at least their full-time salaries while they are absent from work
• Increase the minimum staffing requirements based on the well-established standards of
care
• Require each facility to employ a full-time, trained infection preventionist
• Mandate new, COVID-specific, effective cleaning and disinfecting processes and
procedures
• Monitor staff personal hygiene practices
• Require and provide training in proper use of PPE for staff and residents
• Require states to establish plans and contracts with appropriate facilities to provide
additional capacity to provide care to residents
• Implement annual increase of $10,000 per resident (about 12% of 2016 expenditures)
would amount to $14 billion in new funding. Half of this new funding would support
improvements in staffing: increasing the number of direct care workers and staff nurses;
increasing the payment rates of front-line staff to a living wage; bringing a dedicated
infection preventionist on staff for each building, and increasing the engagement of the
medical director. The rest would go to improvements in services, technology,
infrastructure, training, testing, and supplies.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-27
Technical Assistance and Quality Improvement Principal Recommendation:
• Principal Recommendation 8A: Identify and work to achieve funding mechanisms for—or
reprioritize activities of—technical assistance providers and other contractors to increase the
availability of collaborative, on-site, data-driven, and outcomes-oriented support prior to,
during, and after a public health emergency.
Summary: Addresses the public input about lack of data reporting in some areas because of
disincentives to report. Input included a call for additional federal and state guidance as to
ratings and survey processes for nursing homes to achieve increased consistency and
comparability.
Count of Aligned Open Comments:
25
Specific Recommendation(s) from Open Comments:
• Use survey data to support identification of resources needed by nursing homes
(including enhanced funding, PPE, testing, workforce) rather than as a source of
punishment and blame
• Institute mandatory reporting and disclosure of critical nursing home operational
information to the public
Count of Aligned Attachments: 10
Specific Recommendation(s) from Attachments:
• Provide appropriate lawsuit protection for facilities
• Ensure funds are used for testing, PPE, staffing, virtual visitation, and other items that
directly relate to resident care, well-being, prevention, and treatment
• Develop standard guidelines for nursing homes to build into their disaster response
efforts
• Require inspection results to be posted on facility websites and nursing home compare
profiles
5.4. Facility Design
Three principal recommendations were identified by the Commission in the facility design
category grouping. The Commission noted public encouragement about facility design
modifications that would help support person-centered infection prevention and control
practices.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-28
Facility Design Principal Recommendations:
• Principal Recommendation 9A: Identify and share with nursing homes short-term facility
design enhancements to address immediate pandemic-related risks that can be implemented
at minimal cost.
• Principal Recommendation 9B: Establish a collaborative national forum to identify and share
best practices and recommendations; facilitate real-time learning on how to best use existing
physical spaces.
• Principal Recommendation 9C: Collaboratively establish long-term priorities and seek
appropriate funding streams for nursing homes to redesign and/or strengthen facilities against
infectious diseases.
Summary: Addresses public input noting how design can support cohorting practices while
maintaining modified programming to maintain social and emotional health of residents.
Count of Aligned Open Comments:
17
Specific Recommendation(s) from Open Comments:
• Create private rooms in a circle or spiral around a nursing station and pathways to
encourage movement in spaces reducing congregation
• Create cafes or small dining rooms with reservations for meals or ordering for delivery
looking like restaurants
• Build visitation centers
Count of Aligned Attachments: 9
Specific Recommendation(s) from Attachments:
• Cohort residents by COVID-19 status, with complete separation of residents and with
staff dedicated to different units
• Relocate residents to a one person per room setting
5.5. Data
Three principal recommendations were developed by the Commission in the data category
grouping. The Commission recognized the need for improved data reporting and synchronized
analysis and interoperability as central to addressing many of the public inputs. The ability to
quickly implement and improve data collection and provision methods drove the focus of the
Commission on the following recommendations.
Data Principal Recommendations:
• Principal Recommendation 10A: Standardize COVID-19 data elements, improve data
collection, and identify supportive actions that CMS and federal partners will take in
response to key COVID-19 indicators based on nursing home-reported data.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-29
• Principal Recommendation 10B: Create an easy-to-use, intuitive, and interactive technical
infrastructure for nursing homes that streamlines the process of data reporting and
consolidates dissemination of essential policy guidance, information about updated
regulations, and other communications.
• Principal Recommendation 10C: Enhance HIT interoperability to facilitate better
communication, improve quality measurement standards, and coordinate integration of
nursing home data with data from other health organizations.
Summary: Addresses the public input noting the importance of providing a centralized
collection and reporting hub for easy access by stakeholders to enable informed and
coordinated decision making. Addresses the public input noting the importance of
providing additional data context to enhance predictive ability of nursing homes for
planning and coordination with other health facilities.
Count of Aligned Open Comments: 32
Specific Recommendation(s) from Open Comments:
• Create a standardized reporting tool that includes demographic information to report
infection spread accurately and transparently to residents, family members, community
members, etc.
• Require facilities to conduct and track staff education using computerized training
software and electronic databases to improve the process and reduce costs
• Authorize a National Academy of Medicine study of the disproportionate impact on
nursing homes that serve significant numbers of residents of color
Count of Aligned Attachments: 14
Specific Recommendation(s) from Attachments:
• Streamline reporting to local, state, and federal agencies to ensure facility staff are not
pulled away from resident care to meet fragmented reporting mandates
• Gather data from every skilled nursing facility (SNF) and construct a post-acute COVID-
19 plan
• Ensure NH information be made available daily on facility websites/and or on state
websites with accommodations to assist limited English-speaking populations
• Create a database for tracking 2 CFR §483.70(h) and include additional data capture on
associate medical directors and other physicians being paid as administration personnel
• Require transparency around COVID-19 data (cases and deaths) in nursing homes and
other long-term care facilities, transfer and discharge rights, and provider relief funds
utilization

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-30
6. Public Input Alignment with Long-Term Reform
An additional recommendation under consideration by the Commission that falls beyond the
scope of the short-term time frame for the requested recommendations relates to finance reform.
The Commission likewise recognized in the public inputs an interest in this theme. The long-
term reform recommendation and associated public input is outlined in this section.
Long-Term Recommendation: Review Medicare and Medicaid rates to account for future
sustained infection control, emergency management, and communication activities necessitated
by the prolonged public health emergency.
Summary: Addresses public input that noted necessary interventions and modifications to
nursing home policies and practices caused by the prolonged public health emergency, and
potential future emergencies, were difficult for many facilities to implement and maintain
due to constrained funding. Additionally, several respondents noted increased funding would
(1) allow for adaptations that would lessen the negative impacts of cohorting; (2) allow for
enhanced communication with healthcare providers such as hospice providers, geriatricians,
dental providers, pain management providers, mental health providers, and others through
technology and telehealth; and (3) create opportunity for sustained and more regular
communication with essential care partners.
Count of Aligned Open Comments:
9
Specific Recommendation(s) from Open Comments:
• Increase reimbursement to compensate for additional measures required to protect
residents and staff from COVID-19
• Do not allow nursing homes to charge residents or family members emergency fees,
“COVID-fees,” to pay for PPE, testing, etc.
• Increase reimbursements that are based on optimal level of care, not the bare minimum
• Ensure funding and reimbursements are adjusted to allow nursing homes to implement
new regulatory requirements
Count of Aligned Attachments: 3
Specific Recommendation(s) from Attachments:
• Implement annual increase of $10,000 per resident (about 12% of 2016 expenditures)
would amount to $14 billion in new funding. Half of this new funding would support
improvements in staffing: increasing the number of direct care workers and staff nurses;
increasing the payment rates of front-line staff to a living wage; bringing a dedicated
infection preventionist on staff for each building, and increasing the engagement of the
medical director. The rest would go to improvements in services, technology,
infrastructure, training, testing, and supplies.
• Increase funding from government programs, like Medicaid and Medicare
• Institute a Medical Loss Ratio for facilities
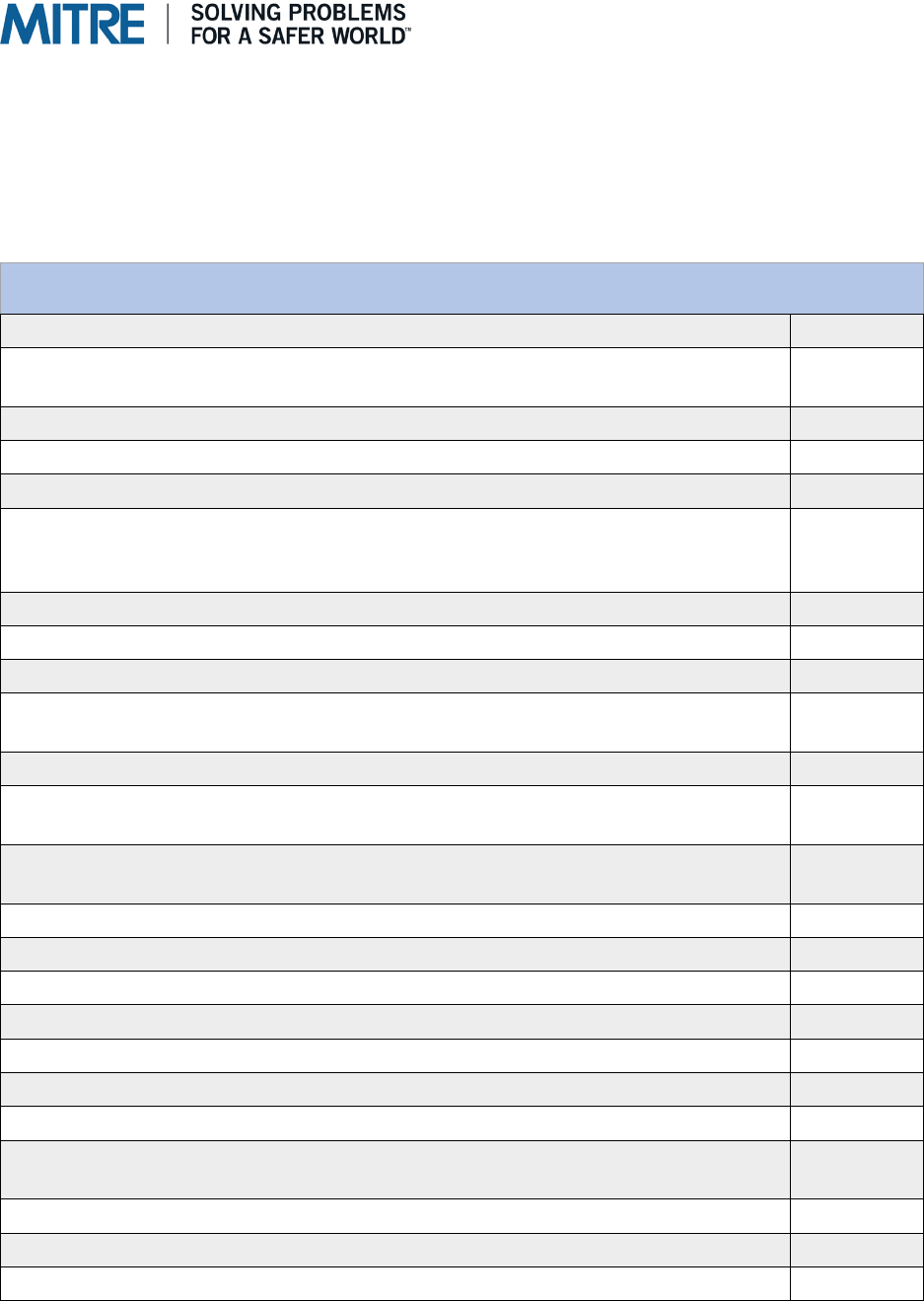
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-31
7. Additional Public Input Themes
Some public open-ended comments and attachments provided unique recommendation(s). These
inputs were synthesized into themes or groupings where possible, counted, and are listed here.
Some represent unique areas for additional interventions.
Table 9: Grouping Unique Recommendations
Unique Recommendations Provided by the Public
(Open-Ended Comments)
Count
Provide additional nursing home oversight 12
Consider nursing home alternatives for older adults and/or people with
disabilities
10
Provide additional care for residents with disabilities (e.g., deaf, dementia) 9
Allow residents to go home 9
Consider hospice workers as essential 7
Provide testing recommendations for transitions of resident care
(admitting/discharging patients from hospitals and/or residents from nursing
homes)
5
Ensure adequate environmental cleanliness
4
Consider ombudsman as essential 4
Promote the use of telehealth services in nursing homes 4
Provide family members with increased monitoring of rooms in facilities through
camera use
3
Ensure adequate oral care 3
Consider nursing home alternatives for older adults and/or people with
disabilities (Home and Community Based Services)
3
Implement contact tracing, social distancing protocols, and safety training for
staff
3
Provide residents with communication devices
2
Provide additional financial nursing home oversight 2
Add specificity to vague rules and regulations 2
Ensure equal quality of care and outcomes for nursing home residents of color 2
Enforce "pay for performance" regulations 1
Engage the National Guard to support COVID relief efforts
1
Ensure assisted living facilities held to same standards as nursing homes
1
Hire a clinical social worker with a master’s degree at every nursing home to
assist with resident care
1
Improve the diet of residents
1
Incorporate diversity in all levels of staff
1
Mandate a geriatrician or geriatrics trained staff in nursing homes 1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-32
Unique Recommendations Provided by the Public
(Open-Ended Comments)
Count
Mandate the transition to a single unified electronic staff training platform and
record keeping system
1
Do not permit Medicaid waivers to have enrollment caps 1
Observe young staff members and ensure proper infection control practices 1
Provide COVID-19 standardized treatments for nursing home populations 1
Reestablish staffing ratio guidelines based on level of resident care needed 1
Require all staff, including informal providers and administrators, to take
Hippocratic oath "first do no harm"
1
Require family councils at all nursing homes 1
Require ombudsmen to be out in facilities much more frequently to talk with
residents and facility staff
1
Require stricter provisions for pets 1
Review of residents' rights impact by liability protections 1
Study the Irish model for nursing homes
1
Update the system of reimbursement is sufficiently funded to assure high
quality care and a meaningful life for each resident or short stay patient
1
Consider the unintended consequences of the 3-day qualifying stay waiver for
residents on hospice who are required to revoke to get their skilled nursing
benefit
1
Table 10: Grouping Attachments
Unique Recommendations Provided by the Public (Attachments)
Count
Continue full standard and complaint surveys through the pandemic
5
Require supervision on the night shifts, weekends, and holidays
3
Institute zero tolerance for repeated abuse and neglect
2
Designate specific nursing facilities as specialized “COVID-19 Positive Centers”
using a data-driven approach
1
Encourage additional coordination between hospitals, nursing homes, and local
health authorities focusing on safe transfers
1
Ensure proper tailoring of guidelines for local conditions and specific facilities
1
Institute a medical loss ratio for facilities
1
Institute cost-based reimbursement
1
Limit visitors so that there is little opportunity for exposure to SARS-CoV-2
1
Mandate decisions for testing, visitation, isolation procedures, admittance
policies etc. by the State or federal DOH’s so that they are not left to the
discretion of the facilities
1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
E-33
Unique Recommendations Provided by the Public (Attachments)
Count
Prevent designating facilities as COVID facilities that are Special Focus
Facilities or SFF candidates, have fewer than 3 stars on the health inspection
domain on Nursing Home Compare, have fewer than 4 stars in the staffing
domain on Nursing Home Compare, or have civil money penalties (CMPs) of
$5000 or more imposed in the prior three years (including CMPs on appeal)
1
Provide FEMA reimbursement through Public Assistance Category B funds to
provide non-congregate temporary sheltering for people evacuating from skilled
nursing facilities and other institutional settings and reimbursement for providing
the support and wrap around services to people that have relocated to a cohort
setting
1
Provide nursing homes with medication management tools in a crisis
1
Provide telemedicine and make telehealth treatment guidelines permanent
1
Require cameras in resident rooms
1
Require staff to make daily notes and medical records on the residents
available to family members especially the POA’s during the pandemic
1
Streamline sources of guidelines/recommendations and ensure properly synced
with additional levels of government as well as other healthcare organizations
1
Test communities through wastewater testing for COVID-19 to detect problem
areas
1
Urge federal, state and local governments and health authorities to stipulate
that, in the chain of events leading to reopening businesses and buildings, that
PALTC facilities, where older adults most at risk of serious illness or death from
COVID-19 reside, be the last to open to visitors and outside contractors and
vendor
1
Require a Health Equity Impact Assessment into the Certificate of Need (CON)
process used by states focusing on closures and effect on low-income, rural
and urban, Black and Latinx, low-income communities, women, LGBTQ people
and people with disabilities
1
Mandate facilities have trained staff position designated to pandemic response
and implementation planning
1
Require advance planning to identify additional surge capacity space for
nursing home resident beds in emergencies
1
Enact protections against retribution and for nursing home workers who report
problems and abuse
1
Ensure survey agencies and organizations have adequate staffing to ensure
robust coverage and ability to follow-up directly with families on complaints
1

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
F-1
Appendix F: Commission Charter
[this page intentionally left blank]

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 1
Coronavirus Commission for Safety and Quality in
Nursing Homes
Charter and Operating Principles
Background
In response to the 2019 global coronavirus pandemic, which has disproportionately
impacted older adults and nursing homes residents in the U.S., the Centers for
Medicare & Medicaid Services (“CMS”) announced an independent commission
(hereinafter, “The Coronavirus Commission for Safety and Quality in Nursing
Homes” or the “Commission”) to address safety and quality in nursing homes. CMS
tasked the Health FFRDC, operated by The MITRE Corporation (hereinafter,
“MITRE”) to convene and facilitate the Commission. MITRE will independently
author a report of the Commission’s findings and recommendations, to be delivered
to CMS along with a report summary, by September 1, 2020.
Commission Objectives
The main purpose of the Commission is to solicit lessons learned and
recommendations for future actions to improve infection control and safety procedures
at nursing homes
.
Specifically,
the Commission is charged with
1. Identifying best practices for facilities to enable rapid and effective identification
and mitigation of transmission of COVID-19 and other infectious diseases in
nursing homes, and specifically to identify 3 to 5 recommendations that can be
implemented both immediately and long-term, taking into consideration the wide
array of individuals including residents, staff, visitors, essential and non-
essential personnel, that interact with nursing homes.
2. Recommending best practices as exemplars of rigorous infection control
practices and facility resiliency that can serve as a framework for enhanced
oversight and quality monitoring activities, and specifically to aim to provide 3 to
5 recommendations on best practices that can be incorporated into a larger
guidance/policy framework for oversight and quality monitoring.
(Recommendations should include prevention and mitigation methods for
inclusion in guidance, reporting requirements, survey tools, enforcement
considerations, and improvement activities.)
3. Endeavoring to i
dentify best practices for improved care delivery and
responsiveness to the needs of all nursing home residents in preparation for,
during, and following an emergency, and specifically to provide 3 to 5
recommendations on care delivery and management that can be immediately

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 2
implemented within nursing homes to address the Coronavirus pandemic as well
as 3 to 5 recommendations for long-term improvements.
4. Leveraging new sources of data to improve existing infection control policies
and enable coordination across federal surveyors, contractors and state and
local entities to mitigate Coronavirus and future emergencies, and specifically to
provide best practices for an analytic plan to monitor infection control and
recommendations to create a methodological framework for using data to
enhance coordination across all the above entities.
The Commission’s findings and recommendations will inform and guide the
development of an independent report and report summary prepared by MITRE, which
will be submitted to CMS by September 1. MITRE will be solely responsible for
ensuring the report and report summary are objective and accurately represent the
Commission findings and recommendations.
Commission Structure
The Commission members are a diverse group of leaders, including industry experts,
clinicians, resident/patient advocates, medical ethicists, nursing home administrators,
academics, infection control and prevention professionals, state and local authorities,
and other stakeholders whose expertise will benefit the areas on which the
Commission will focus. All Commission members will have an opportunity to voice
their views and opinions. MITRE is the convener of the Commission.
Commission Members
Commission members are appointed by MITRE based on their relevant
background, subject matter expertise, and leadership.
Commission members may not assign delegates to attend or listen to convenings
on their behalf, nor should Commission members invite others to listen in to
convenings. The kickoff meeting is a convening.
Members will:
•
Provide input and feedback to achieve the above Objectives during
convenings and as requested by MITRE.
•
Commit best efforts to attend all Commission convenings, and at least 4 of the
5 planned convenings, and participate in debriefing discussions as requested.
When unable to attend a convening, the member will notify MITRE.
•
Work collaboratively and respectfully with other members to achieve the
above Objectives.
•
Serve, as requested, on subcommittees or working groups that may be formed
to explore specific issues between the full Commission convenings.
•
Commit best efforts to complete any pre-work assigned in preparation for

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 3
convenings.
•
Commit best efforts to adhere to the Virtual Behaviors described later in this
document.
MITRE as Convener, Moderator, and Report Author
MITRE serves as the convenor of the Commission, providing logistics support for
Commission events, including the development and dissemination of convening
materials and briefings. MITRE will consult with CMS and Commission members as
it develops and finalizes agenda and materials in support of the Commission’s
convenings.
MITRE is responsible for documenting Commission member attendance, input and
feedback at each convening. MITRE is also responsible for determining how to
handle issues that may arise with respect to a member’s participation, such as if a
member fails to attend multiple convenings. MITRE is responsible for briefing CMS
leadership on progress on a regular basis.
MITRE’s Chief Medical Officer serves as the Commission moderator and provides
guidance on planning, facilitating, and executing Commission convenings. The
moderator is not a member of the Commission and maintains neutrality in all
convenings and discussions.
The moderator:
•
Provides guidance to the Commission and establishes a collaborative and
action-oriented culture to achieve the Objectives described above.
•
Provides strategic guidance on Commission agenda and convening
materials.
•
Moderates Commission convenings, ensuring that all members have an
opportunity to contribute, and that members adhere to their responsibilities
and the Rules of Conduct.
•
Determines the best approach to consensus-building and decision-making.
•
Provides guidance on the first draft and final versions of the report and report
summary.
•
Represents the findings and recommendations of the Commission in
discussions with CMS and the public as requested.
•
Maintains objectivity and independence in all communications on behalf of
the Commission.
As the preparer of the report and report summary, MITRE will create a framework for
prioritizing the Commission’s findings and recommendations.
MITRE will
independently prepare draft and final versions of the report and report summary for
submission to CMS. Commission members’ ability to review and comment on the

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 4
draft and final reports is denoted below under “Commission Scope and Authority.”
CMS may also review and comment on draft reports.
MITRE is not responsible for the publication of the report and report summary
delivered to CMS.
CMS owns the report and report summary and makes all decisions
regarding its eventual distribution.
CMS may choose to publish all or any parts of the
report and report summary and in doing so must indicate if any content has been
altered or removed from the final versions delivered to CMS by MITRE.
Invited Guests
CMS Leadership—It is anticipated that CMS leadership will participate as invited
guests in a listen-only mode during Commission convenings, unless present as
invited speakers. It is not anticipated that CMS invitees will necessarily listen in on
breakout sessions during the convenings where members work in small groups; this
will be determined by the moderator in discussion with the members.
Federal Partners or Other Experts—Other Federal partners or other subject matter
experts may attend portions of one or more Commission convenings as guests at
the recommendation of Commission members or CMS, and concurrence by the
MITRE moderator. Invitations would be extended by MITRE. They may participate
as interested constituents or serve to inform the Commission’s discussions.
Commission members will be informed when guests are present and when they
leave a convening.
Recording of Convenings
MITRE may elect to record Commission convenings to verify content and accurately
capture discussions. The video and audio recordings will be maintained by MITRE
and will not be released to the public; the documentation will be marked sensitive,
proprietary, and confidential. Further, MITRE will take measures to protect the video
and/or audio recordings from disclosure. The Commission members signal their
consent to these recordings through their participation in the convening, and MITRE
will remind participants at the outset of a meeting that it is being recorded.
Transcription of recordings will be made and shared with the Facilitator and
Moderator.
Separate recording of the convenings by any meeting attendees but MITRE is
prohibited.
Commission Scope and Authority
The Commission can, through MITRE, request information, data or presentations from
CMS that may help it in its work. CMS will share that information or data if available and
releasable and MITRE will coordinate with CMS on the provision of information or data

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 5
to the Commission and/or arranging for presentations to the Commission.
Commission members will develop findings and recommendations on topics relevant to
the Objectives based on their individual experiences, expertise, and background.
Commission members will have opportunity to comment on draft and final versions of
the report and report summary prepared by MITRE and may choose to endorse the final
report and report summary before submission to CMS.
The Commission does not have the authority to direct the writing of the independent
report and report summary, nor may it override recommendations of other Commission
members.
Neither the Commission nor MITRE has the authority to direct the actions of CMS or
any other governmental authorities
.
If needed, the Commission may request an Executive Session and may ask invited
guests and non-Commission members to leave the convening. A member may approach
the meeting moderator or facilitator about desire to go into executive session and MITRE
will keep the confidentiality of the requesting member’s identity. MITRE will provide
guidance on how to do this.
Commission Rules of Conduct
To ensure that the Commission works collaboratively to achieve the Objectives,
members will:
•
Communicate with respect, candor, objectivity, and intellectual honesty during
convenings and deliberations.
•
Give and accept feedback in a constructive, non-defensive manner.
•
Approach all interactions with the Commission as an opportunity to learn as
well as to inform.
•
Contribute to achieving convening objectives by thoroughly reviewing briefing
materials.
•
Provide qualitative and quantitative data to inform the Commission, as
requested.
• Provide follow-up input or materials after each convening, as requested.
• Refrain from publicizing the findings or recommendations of the convenings
without the written consent of MITRE as per the terms of the Non-Disclosure
Agreement that each member has signed.

Commission Confidential and Proprietary
June 23, 2020
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
Page 6
Virtual Behaviors
Because the Commission convenings will be held virtually, each member will:
•
Test their technology and video conferencing/webcam capability to ensure
they are functional prior to the first convening.
•
Make every effort to participate where privacy of the discussion can be
preserved (e.g., join from a private room and/or use headsets so that non-
member cannot listen in on the meeting).
•
Remain actively engaged and on-camera while others are speaking.
•
Indicate that they are ready to speak as instructed by the moderator.
•
Mute when not speaking unless/until called upon.
•
In all other ways, conduct themselves as if in an in-person convening.
Consensus Procedures
The findings and recommendations of the Commission will inform the report and
report summary written by MITRE. MITRE will independently evaluate the
Commission’s findings and recommendations and will work to achieve consensus
among Commission members on the final recommendations. If the members do not
reach consensus on a given issue, then the MITRE moderator will determine how to
reflect minority and/or dissenting opinions in the final report and report summary.
Confidentiality and Chatham House Rule
To maintain the confidentiality of the Commission’s work and promote candor
during its convenings, members will
refrain from publicizing the discussions, findings
or outcomes of the convenings without the written consent of the MITRE. For more
information about this topic, please refer to the non-disclosure agreement that members
signed upon their acceptance of their Commission appointments.
MITRE will operate Commission convenings and discussions under the Chatham
House Rule, whereby convening insights are extracted but not attributed to any
Commission member or guest in any convening summaries or in the report and
report summary prepared by MITRE. Commission members and all guests will
adhere to this rule in any communications that follow the convenings.
Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
G-1
Appendix G:
Commission Memorandum of Short-Term
Recommendations – July 17, 2020
[this page intentionally left blank]

FFRDC Deliverable to CMS on Behalf of the Commission
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
CMS Alliance to Modernize Healthcare
7515 Colshire Drive McLean, VA 22101-7539 (703) 983-6000
Coronavirus Commission for Safety and Quality in Nursing Homes
Short-term Recommendations for CMS
July 17, 2020
Purpose and Context of These Recommendations
During its July 14 convening, the Coronavirus Commission for Safety and Quality in Nursing Homes
(Commission) prioritized the Centers for Medicare & Medicaid Services’ (CMS) July 7 request for
recommendations the agency can implement in two to four weeks.
i
This memo summarizes that output.
Some of the following recommendations may require actions outside the authority of CMS. However,
the Commission recognizes CMS as the lead federal agency for nursing homes and their regulation, and
urges CMS to continue to advocate for nursing homes and their residents with other federal agencies and
states in the national response to the Coronavirus Disease 2019 (COVID-19) pandemic.
The Commission members considered established or emerging evidence in its discussions. Members
noted that some issues they considered most important may require more time for CMS to address but
need to be started now. The Commission will continue to discuss the themes covered in these
recommendations in its remaining convenings. MITRE expects the Commission will provide more
specific and additional recommendations in the final report, along with findings that reflect the emerging
evidence that inform the recommendations. MITRE anticipates incorporating this memorandum as an
appendix to the final report to be delivered to CMS on September 1, 2020.
The Commission recognized that CMS has taken initial steps to support access to testing and personal
protective equipment (PPE) as part of the national strategy to address COVID-19 and understands these
issues are not within the sole control of CMS. Members stressed that additional federal action is
necessary to ensure sufficient availability of high-quality testing and PPE. Without this, and related
training, the virus will continue to spread. The Commission considers its recommendations on testing
and PPE to be the highest priority for infection control. Beyond testing and PPE, many Commission
members consider hazard pay for nursing home staff to be the next most important short-term
recommendation. Other recommendations focus on hotspot anticipation and resource mobilization,
streamlined communication and reporting, resident- and staff-centered infection control, and an update
in the Resident Assessment Instrument/ Minimum Data Set (RAI/MDS) manual.
Recommendations of Highest Priority for Infection Control
• SCREENING AND TESTING: Release a recommended baseline COVID-19 screening and testing
strategy for nursing home residents, staff, and visitors that incorporates best/promising/emerging
practices with tailored options for local adaptations based on community spread of COVID-19.
Include in the strategy the type(s) of tests that should be used, for whom, and at what frequency.
Deploy – via appropriate federal or state mechanisms – additional funding to provide and sustain the
equipment, training, and supplies essential to implement a nationwide screening and testing strategy.
• PPE: Ensure all nursing homes have adequate and high-quality supplies of PPE. Provide up-to-date
guidance on the use and reuse of various types of PPE. Ensure nursing homes are prioritized at local,

Nursing Home Commission Short-term Recommendations for CMS
Page 2
FFRDC Deliverable to CMS on Behalf of the Commission
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
CMS Alliance to Modernize Healthcare
7515 Colshire Drive McLean, VA 22101-7539 (703) 983-6000
state, and national levels for PPE acquisition and that a federal strategy exists to address PPE
shortages.
Further Recommendations for Short-Term Actions
• HAZARD PAY: Immediately implement hazard pay for direct services staff of nursing homes
through appropriate federal or state funding mechanisms.
• HOTSPOT ANTICIPATION AND RESOURCE MOBILIZATION: Use predictive analytics to
anticipate the need for nursing home workforce support across the nation. Deploy emergency
management, infection control, and capacity-building support to nursing homes in collaboration with
state-based strike teams.
• COMMUNICATION AND REPORTING: Initiate a single, bidirectional user interface to release
national guidance and data to nursing homes, and to simplify COVID-19 data collection from
nursing homes.
• RESIDENT- AND STAFF-CENTERED INFECTION CONTROL: Incorporate resident and
staff psychological safety and wellbeing into the nursing home infection prevention and control
program (IPCP), including specific, evidence-based guidance on:
o Cohorting of residents and staff to minimize disruption of daily routines while promoting
rigorous infection control practices.
o Maintaining resident contact with external support systems through facilitation of physically
distanced and/or virtual visits.
Facilitate collaboration among organizations to share emerging best practices that balance resident
and staff needs with infection control.
• CODING: Modify RAI/MDS manual coding instructions for isolation because of active infectious
disease (Chapter 3 of the MDS 3.0 RAI Manual (O0100M)) to allow capture of care and services
provided to persons with or suspected to have COVID-19 who are isolated per CDC and/or CMS
guidelines.
Commission Member Review of This Memo
All members had the opportunity to review this memo in its final draft form (just prior to this version).
Many members endorsed the memo without editorial comment. A handful of members offered edits to
give the recommendations more specificity; because there was not time to recirculate fully-revised
recommendations to the entire Commission, MITRE will share those inputs for the group to discuss in
future convenings. One member agreed the memo reflects the discussion of the majority; however, they
did not endorse the priorities reflected. For this member, cohorting is second only to the use of PPE.
i
Note: This memo is delivered in rapid-turn following the Commission’s July 14, 2020 convening. During that
meeting, the Commission members were unaware of the development, announced later on July 14, of a federal
initiative to distribute rapid point of care testing to nursing homes designated for prioritization by CMS. Thus, the
Commission members did not discuss this development. Some members have noted that they wish to discuss the
need for a specific recommendation regarding this new initiative, which MITRE anticipates will be forthcoming.

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
H-1
Appendix H:
Nursing Home COVID-19 Data Limitations
Given the broad impact of the COVID-19 pandemic on nursing homes and the desire to make
informed decisions, policymakers at all levels have been interested in obtaining high-quality,
timely, and actionable COVID-19 data. However, a variety of limitations exist with these data.
Surveillance data on COVID-19 are often incomplete and can lead to an undercount of cases and
deaths.
286
There are multiple specific limitations and cautions to consider with common COVID-
19 data types, including issues of representativeness; bias; measurement and sampling error; time
periods of reporting; and scale or location factors.
287
Approaches to collecting and reporting COVID-19 data in nursing homes can vary at the federal,
state, and local level. Although CMS instituted new reporting requirements for all federally-
certified nursing homes with the aim of gathering more complete and standardized COVID-19
data, discrepancies between federal and state data are still apparent in some instances – such as
when certain states report cumulative cases and deaths across multiple types of long-term
facilities or over a different timeframe compared to the federal government.
288
Some data
elements may be publicly available only from certain states but not others (or at the federal
level). Data definitions can also differ, such as criteria for determining resolved or suspected
cases.
289
CMS has highlighted that ongoing COVID-19 data reported to CDC’s NHSN system is
preliminary and subject to fluctuations, including changes made by nursing homes given the
opportunity to correct their submitted data when needed.
290
In addition, CMS has acknowledged
several limitations of the nursing home COVID-19 data, including variability in retrospective
reporting, inaccuracies due to the challenge faced by facilities adapting to new reporting
requirements, and the impact of variable access to COVID-19 testing on case identification.
291
286
United States Government Accountability Office. (2020, July 30). COVID-19: Data Quality and Considerations for
Modeling and Analysis. https://www.gao.gov/products/GAO-20-635SP
287
National Academies of Sciences, Engineering, and Medicine. (2020, June 11). Evaluating Data Types: A Guide for
Decision Makers using Data to Understand the Extent and Spread of COVID-19.
https://www.nap.edu/catalog/25826/evaluating-data-types-a-guide-for-decision-makers-using-data
288
Chidambaram P and Garfield R. (2020, June 15). Limits and Opportunities of Federal Reporting on COVID-19 in
Nursing Facilities. Kaiser Family Foundation.
https://www.kff.org/coronavirus-covid-19/issue-brief/limits-and-
opportunities-of-federal-reporting-on-covid-19-in-nursing-facilities/
289
Chidambaram P and Garfield R. (2020, June 15). Limits and Opportunities of Federal Reporting on COVID-19 in
Nursing Facilities. Kaiser Family Foundation.
https://www.kff.org/coronavirus-covid-19/issue-brief/limits-and-
opportunities-of-federal-reporting-on-covid-19-in-nursing-facilities/
290
Centers for Medicare & Medicaid Services. (2020, August 9). COVID-19 Nursing Home Data.
291
Centers for Medicare & Medicaid Services. (2020, June 4). Nursing Home COVID-19 Data Release External
FAQs. https://www.cms.gov/files/document/covid-nursing-home-data-release-external-faqs.pdf

Commission Final Report
For Limited External Release Only. PRS Release Number (20-2382).
© 2020 The MITRE Corporation. All Rights Reserved. Commission Confidential and Proprietary.
I-1
Appendix I:
Commission Recommendations Overview Presentation –
August 14, 2020
[this page intentionally left blank]

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Coronavirus Commission
on Safety & Quality in
Nursing Homes
Recommendations Overview
Preliminary Deliverable in Advance of Final Report. Content Subject to Change.
August 14, 2020

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Commission Process & Endorsement
Commission Formation & Focus. The 25-member commission kicked off on June 23; it then convened six times
throughout July to discuss and formulate recommendations in four focus areas. CMS staff and other federal guests joined
these sessions in listening mode. CMS advised commission members to limit the scope of their discussions and
recommendations to nursing homes that are solely regulated by CMS, which excludes nursing homes that operate solely
under the purview of the VA. CMS's ability to tailor, implement, and monitor the impact of the Commission's
recommendations will be subject to the varied authority granted to federal and state regulators in this space.
Public Input. MITRE sought comments from organizations and individuals interested in informing the Commission’s work via
two mechanisms: (1) a public-facing email inbox, and (2) a website-based structured engagement form. More than 600
submissions were received. Many themes emerged; visitation and workforce themes were of an order of magnitude higher
than all others. The final report will provide greater detail about this activity.
Purpose of This Slide Deck. MITRE prepared this preliminary slide deck in advance of a detailed report to be delivered to
CMS on September 1. The content is informed by Commission member input, public input via the Commission website, and
CMS actions through August 11.
Commission Member Endorsement of Contents. Commission members had the opportunity to review this slide deck from
Aug. 11 – 13. Twenty-one members generally approve; discussion continues in areas where opinions diverge. MITRE has
included notations on slides where there is lack of Commission member consensus or a dissenting opinion on a
recommendation or action step. MITRE has also denoted where certain text is derived solely from public input (P) or MITRE
(M); this content may not reflect Commission member discussion or opinion but was included to address a key gap in
actionable specificity.
2

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Commission Objectives
The main purpose of the Commission is to solicit lessons learned and recommendations for future
actions to improve infection control and safety procedures at nursing homes.
Objective Related Themes
1. Identify best practices for facilities to enable rapid and effective
identification and mitigation of transmission of COVID-19 and other
infectious diseases in nursing homes
Testing and Screening, Equipment and PPE, Cohorting, Visitation,
Workforce Ecosystem, Technical Assistance and Quality Improvement,
Facilities
2. Recommend best practices as exemplars of rigorous infection
control practices and facility resiliency that can serve as a
framework for enhanced oversight and quality monitoring activities
Testing and Screening, Equipment and PPE, Cohorting, Visitation,
Communication, Workforce Ecosystem, Technical Assistance and
Quality Improvement, Facilities
3. Endeavor to identify best practices for improved care delivery and
responsiveness to the needs of all nursing home residents in
preparation for, during, and following an emergency
Cohorting, Visitation, Communication, Workforce Ecosystem,
Technical Assistance and Quality Improvement, Facilities
4. Leverage new sources of data to improve existing infection
control policies and enable coordination across federal surveyors,
contractors and state and local entities to mitigate Coronavirus and
future emergencies
Nursing Home Data
3

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Commission Members
Roya Agahi, RN, MS HCM, WCC; Chief Nursing
Officer, CareRite, New York
Lisa M. Brown, PhD, ABPP; Professor of
Psychology, Palo Alto University, California
Mark Burket, CEO, Platte Health Center Avera,
South Dakota
Eric M. Carlson, JD; Directing Attorney, Justice in
Aging, California
Michelle Dionne-Vahalik, DNP, RN; Associate
Commissioner, State Health and Human Services
Commission, Texas
Debra Fournier, MSB, BSN, RN-BC, LNHA, CHC,
CPHQ, Chief Operations Officer, Veterans’ Homes,
Maine
Terry T. Fulmer, PhD, RN, FAAN; President,
The John A. Hartford Foundation, New York
Candace S. Goehring, MN, RN; Director,
State Department of Social and Health Services,
Aging and Long-Term Support Administration,
Washington
David C. Grabowski, PhD; Professor of
Healthcare Policy, Harvard University,
Massachusetts
Camille Rochelle Jordan, RN, BSN, MSN, APRN,
FNP-C, CDP; Senior Vice President of Clinical
Operations & Innovations, Signature
Healthcare, Kentucky
Jessica Kalender-Rich, MD, CMD, AGSF,
FAAHPM, FACP; Medical Director, Post-Acute Care,
University of Kansas Health System, Kansas
Marshall Barry Kapp, JD, MPH; Professor
Emeritus of Law, Florida State University, Florida
Morgan Jane Katz, MD, MHS; Assistant Professor
of Medicine, Johns Hopkins University, Maryland
Beverley L. Laubert, MA; State Long-Term Care
Ombudsman, State Department of Aging, Ohio
Rosie D. Lyles, MD, MHA, MSc, FACA; Director of
Clinical Affairs, Medline Industries, Illinois
Jeannee Parker Martin, MPH, BSN; President and
CEO, LeadingAge California
G. Adam Mayle, CHFM, CHC, CHE;
Administrative Director of Facilities, Memorial
Healthcare System, Florida
David A. Nace, MD, MPH, CMD; President,
AMDA – The Society for Post-Acute and Long-Term
Care Medicine, Pennsylvania
Lori Porter, LNHA, CNA; CEO, National
Association of Health Care Assistants, Missouri
Neil Pruitt, Jr., MBA, MHA, LNHA; Chairman and
CEO, PruittHealth, Inc., Georgia
Penelope Ann Shaw, PhD; Nursing Home
Resident and Advocate, Braintree Manor
Healthcare, Massachusetts
Lori O. Smetanka, JD; Executive Director,
National Consumer Voice for Quality Long-Term
Care, Maryland
Janet Snipes, LNHA; Executive Director, Holly
Heights Nursing Home, Colorado
Patricia W. Stone, PhD, MPH, FAAN, RN, CIC;
Professor of Health Policy in Nursing, Columbia
University, New York
Dallas Taylor, BSN, RN; Director of Nursing, Eliza
Bryant Village, Ohio
4

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Key Takeaways
The Commission put forward 9 themes and 27 principal recommendations.
Immediate and near-term actions by CMS (through policy or regulations, alone and with others) are necessary.
The Commission and the public alike call on CMS to continue advocating on behalf of beneficiaries based on the
following principles.
Residents and families must be able to connect in meaningful ways to ensure the physical and mental well-being of the resident
and to protect against neglect and abuse. To achieve positive outcomes, CMS must ensure nursing homes address this need and
residents’ other conditions while prioritizing rigorous infection control.
Nursing home staff must be kept safe and treated with respect in the workplace, which requires access to the right training and
equipment, along with compensation that recognizes the risks they take, their dedication to resident safety, and the quality of the
care they deliver.
Nursing home management and staff can be more effective if provided with streamlined communications, reporting
capabilities, and access to funds that will support myriad additional costs, and can reduce the trauma of some emergency
measures by communicating policies in advance and providing advance notice when activated.
CMS should work with its partners to identify funding sufficient to fully pay for each implemented recommendation.
CMS must begin now to take steps to solve longer-stan
ding, systemic issues illuminated by the pandemic.
A systems focus on long-term care financing and accountability, facility design, workforce, governance/management,
technology, and data will help ensure future nursing home safety and quality. The final report will present this discussion.
5

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Principal Recommendations (1/3)
Theme 1: Securing Testing & Screening Capabilities (slides 10 – 11)
With federal, state, local, territorial, and tribal (SLTT) partners, immediately develop and execute a national strategy for testing and delivering rapid
turnaround of results (i.e., results in less than 24 hours) in nursing homes, in combination with CDC recommended screening protocols. Allow nursing
homes to tailor the strategy in partnership with federal and SLTT authorities.
Theme 2: Increasing PPE Supply and Use (slides 12 – 13)
Take responsibility for a collaborative process with federal and SLTT partners to ensure nursing homes can procure and sustain a three-month supply of
high-quality supplies of Personal Protective Equipment (PPE) and essential equipment.
Work with federal partners, including CDC and FDA, to creat
e specific guidance on the use, decontamination, and reuse of PPE and essential
equipment.
Collaborate with federal and SLTT partners to pr
ovide guidance on training to all staff on proper use of PPE and equipment.
Theme 3: Rethinking Cohorting Practices (slides 14 – 15)
Update cohorting guidance to balance resident and staff psychological safety and well-being with infection prevention and control.
Update cohorting guidance to ad
dress differences in nursing home resources for cohorting.
Theme 4: Prioritizing Visitation Activities (slides 16 – 19)
Emphasize that visitation is a vital resident right. Update and release consolidated, evidence-based guidance on safely increasing controlled, in-
person visitation prior to Phase 3 reopening.
Update and rel
ease consolidated, evidence-based guidance on effectively planning for and implementing virtual visitation tools and techniques.
Provide resources to help nursing homes assess and improve the mental health and psychosocial well-bei
ng of residents during and after the
pandemic.
Assess, streamline, and in
crease the accessibility of COVID-19-related directives, guidance, and resources on visitation into a single source.
6

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Principal Recommendations (2/3)
Theme 5: Supporting Nursing Home Communications with Residents and Families (slide 20)
Increase specificity and expand breadth of guidance on communications between nursing homes, residents, and families.
Theme 6: Strengthening the Workforce Ecosystem (slides 21 – 27)
Address nursing home workforce hazard pay; assess and leverage emergency nursing home surge support options; and emphasize minimum care
standards.
Issue guidance for on
-the-job certified nursing assistant (CNA) training, testing, and licensure; track all CNAs via a central registry; and catalyze
interest in the CNA profession through diverse recruitment vehicles.
Provide guidance grounded in maximizing equity and preventing employee burnout that allows nursing home workforce members to continue to
wo
rk in multiple nursing homes while adhering to infection prevention and control practices.
Require a Reg
istered Nurse (RN) to be present around-the-clock in a nursing home when 10% or more of residents test positive for COVID-19.
Identify and immediately leverage cert
ified infection preventionists who can support nursing homes’ infection prevention needs.
Professionalize in
fection prevention positions in nursing homes by updating regulations at 42 CFR § 483.80 so more fully qualified infection
preventionists are available to serve in nursing homes.
Require nursing homes to emp
loy infection preventionist(s) with specific educator duties (1.0FTE < 30 resident beds; 2.0FTE > 30 resident beds).
Convene a Lo
ng-Term Care (LTC) Workforce Commission and/or Advisory Board to assess, advise on, and provide independent oversight for
modernization of workforce ecosystem. (M)
Work with feder
al, state, local, public, private, and academic partners to catalyze overhaul of workforce ecosystem.
7

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Principal Recommendations (3/3)
Theme 7: Catalyzing Technical Assistance and Quality Improvement (slide 28)
Identify and work to achieve funding mechanisms for – or reprioritize activities of – technical assistance and other contractors to increase the
availability of collaborative, on-site, data-driven support prior to, during, and after a COVID-19 outbreak.
Theme 8: Enhancing Facility Design (slides 29 – 30)
Identify and share with nursing homes short-term facility design enhancements to address immediate pandemic-related risks that can be implemented
at minimal cost.
Establish a collaborative national forum to i
dentify and share best practices and recommendations; facilitate real-time learning on how to best use
existing physical spaces.
Collaboratively establish long-term
priorities and seek appropriate funding streams for nursing homes to redesign and/or strengthen facilities against
infectious diseases.
Theme 9: Making Data More Actionable (slides 31 – 33)
Improve COVID-19 data element standardization and data collection while identifying specific actions that CMS and federal partners will take in
response to changes in key COVID-19 data indicators based on data reported by nursing homes.
Develop a sing
le, bidirectional application to serve as a central interface for nursing home data collection and information dissemination that
includes essential COVID-19 guidance, statistics, and outcomes.
Enhance health information technology (HIT) interoperability to f
acilitate better communication, improve quality measurement standards, and coordinate
integration of nursing home data with data from other health organizations.
8

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Themes, Recommendations,
and Actions
Refer to slide 35 for additional guidance on how to read the Themes, Recommendations, and Actions slides
9

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 1: Testing and Screening (1/2)
Problem:
Nursing homes face four challenges to successful implementation of testing and screening protocols: (1) there are testing and screening supply shortages
and nursing homes may not be prioritized, (2) wait times for testing results prevent meaningful infection control; (3) there are funding gaps that prevent
nursing homes from implementing staff screening and testing per existing CMS and CDC guidance; and (4) staff may lack adequate training (to administer
tests properly) and sufficient resources and time (to conduct screening of visitors and staff per CDC recommendations).
Principal Recommendation:
With federal, state, local, territorial, and tribal (SLTT) partners, immediately develop and execute a national strategy
for testing and delivering rapid turnaround of results (i.e., results in less than 24 hours) in nursing homes, in combination
with CDC recommended screening protocols. Allow nursing homes to tailor the strategy in partnership with federal and SLTT
authorities.
Recommended Action Steps:
Work with federal and SLTT partners to ensure that nursing homes are prioritized to receive testing and screening supplies, and
reporting of results, based on the prevalence of COVID-19 in facilities and in the surrounding community. Accompanying
instructions should note limitations to rapid tests in terms of reliability and accuracy.
With federal partners, develop a central point for coordinating distribution of testing kits, including molecular point-of-care
t
esting and adequate supplies. Ensure that testing with sufficient supplies is available in one quarter, one half, three quarters, and
all of the nation’s nursing homes by Oct. 1, Nov. 1, Dec. 1, 2020, and Jan. 1, 2021, respectively.
Identify and work to achieve funding mechanisms for nursing home staff to ensure nursing home capability to conduct baseline
and itera
tive testing. In the interim, seek access to additional funding from the HHS Public Health and Social Services Emergency
Fund to ensure that nursing homes have access to funding to support the scale of screening and testing required for effective
operations.
It is assumed that visitors to the facility pay for their own COVID test or have coverage for such testing; this may be a barrier
for some populations and this potential access barrier should be assessed and solution devised, at least to enable entry of
essential care partners.
CMS actions to date:
With CDC, released
iterative guidance
outlining details for
screening and testing of
residents, staff, and
visitors. (2), (8)
With HHS, began
providi
ng rapid point-of-
care diagnostic devices
and tests for nursing
homes located in 62
hotspot geographic areas
and allocated $5B for
testing through the
Provider Relief Fund.
(23), (27)
10

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 1: Testing and Screening (2/2)
Recommended Action Steps:
Partner with CDC, FDA, NIH, AHRQ, and other federal agencies to ensure approved rapid tests, such as tests approved under the NIH Radx initiative, are
providing accurate results.
Provide a list of recommended tests for nursing home use.
Provide training for all rapid testing machines and waive current Clinical Laboratory Improvement Amendments (CLIA) limitations to
permit onsite testing.
Recommend, with support of CDC and FDA, technology-base
d solutions that can improve daily screening processes and reduce staff burden. Include
recommendations for web and phone-based applications that can quickly capture and assess screening questions without the use of staff input or
assistance; and recommendations for physical screening technologies, like touchless temperature devices.
Develop a decision tree that incorporates recommendations from Nursing Home Reopening Recommendations for State and Local Officials,
QSO-20-30-
NH (May 18, 2020) and that communicates the most appropriate testing strategy for residents, staff, and visitors, for baseline and iterative testing,
tailored for community prevalence and other risk factor (i.e., staff travelling between nursing homes and residents receiving offsite care, including
dialysis) to encourage effective intervention. The decision tree should explain what to do when a resident or staff member (1) is exposed to COVID-19; (2)
is presumptively positive; (3) confirmed positive, or (4) refuses testing. (M) If a resident refuses testing under 42 CFR § 483.10(c)(6), require that the
resident is isolated for the 10-14 day period pursuant to the waiver of 42 CFR §483.10 (e)(6) & (7) and that the reasoning and action are documented in
the resident’s record.
11

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 2: Equipment and PPE (1/2)
Problem:
Nursing homes do not have consistent access to an adequate quantity and quality of PPE and nursing homes may have gaps in understanding of best
practices for PPE training, use, and reuse.
Principal Recommendation:
Take responsibility for a collaborative process with federal and SLTT partners to ensure nursing homes can procure and
sustain a three-month supply of high-quality supplies of PPE and essential equipment. This process must provide
accountability and oversight.
Recommended Action Steps:
Work with federal partners, including ASPR and FEMA, to develop a process for procurement of PPE that includes:
Coordinated joint purchasing procurement and distribution of PPE with federal and SLTT agencies to ensure adequate
availability and quality
Ability to identify status of PPE inventory, procurement pipeline, and projected demand at facility, state, and national levels
Established quality standards and requirements for commercial use of PPE
Ability for CMS to exercise its enforcement powers to ensure compliance and accountability
Integrated tools to monitor inventory, rotate stockpiles, manage burn rates, and maintain the federal recommendation of
supplies.
Add a requirement in the Emergency Preparedness Rule, 42 C.F.R
. § 483.73, (M) to include PPE utilization in emergency
preparedness and infection control protocols.
Work with federal partners including the CDC to enhance established federal reporting sites (e.g., NHSN, PBJ) to capture detailed
COVID-19 cas
e reporting and status of PPE availability. (See related Data recommendations.)
Develop guidelines for equipment and PPE shortages (i.e., procurement options when normal supply chains are unavailable or
proto
cols for reallocation of supplies currently stored by states, facilities, and other entities).
CMS actions to date:
Issued guidance for:
Use of PPE (3)
State S
urvey Agencies:
Refra
in from citing
facilities for lack of PPE
and supplies that are
beyond their control (5)
State Survey Agencies:
Use o
f PPE (with state
and local leaders) (5)
With FEMA: issued 14-day
supplies of PPE to nearly
15,000 nursing homes
With CDC: released national
COVID-19 training modules
12

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 2: Equipment and PPE (2/2)
Principal Recommendation: Use, Decontamination, and Reuse: Work with federal partners, including CDC and FDA, to provide specific guidance on
the use, decontamination, and reuse of PPE and essential equipment.
Recommended Action Steps:
Develop and provide guidance for when to utilize different PPE such as face shields, surgical or cloth facemasks, gloves, gowns and NIOSH certified N95 respirators.
This guidance must be specific to nursing home administrators, residents, staff, contractors, essential care partners, and visitors and it must identify expectations
during COVID-19 outbreaks as well expectations for ramping down when appropriate. The use should be guided by the level of infection severity within the facility
and geographic location.
Release guidance for FDA-ap
proved reuse of PPE and other essential equipment with prioritizing the use of N95 masks for high risk staff. Guidance should provide a
framework for facility medical directors to implement practices most appropriate on a case by case basis.
Release guidance on fit testing for PPE and NIOSH-app
roved N95 respirators.
Establish requirements and guidance on decontamination of N95 respirators.
Provide guidelines for equipment and PPE shortages (i.e., refresh/reuse protocols, strategies for extending limited supplies, alt
ernative products where applicable).
Identify and recommend acceptable methods for refresh and reuse of PPE by nursing homes.
Principal Recommendation: Training: As needed, collaborate with other federal and state agencies to provide guidance on training to all clinical
and nonclinical facility staff on proper use of PPE and equipment. (See also recommendation on Infection Preventionist under Workforce Ecosystem)
Recommended Action Steps:
Establish national training requirements for infection control and use of PPE for all nursing home staff and other individuals with direct and indirect contact with
residents.
Tailor training modules for PPE utilization for administrators, residents, staff, contractors, ess
ential care partners, and visitors.
Incorporate PPE training modules into Nursing Home Preventionist Tr
aining course and the Infection Prevention and Control Program (IPCP).
Establish national training standards for nursing home staff based on extant core competency standards or other model standards/c
ertifications developed by states.
13

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 3: Cohorting
i
(1/2)
Problem:
Cohorting of nursing home residents based on their COVID-19 status has negatively affected their social and emotional health, contributing to increased anxiety
and/or depression among residents.
Principal Recommendation:
Update cohorting guidance to balance resident and staff psychological safety and well-being with infection prevention and
control.
Recommended Action Steps:
Develop clear and concise guidance for cohorting using the TB Training Module 12B in the CDC Infection Preventionist training
course and the Recommended Nursing Home Phased Reopening for States (M). Ensure CMS cohorting guidance:
Prioritizes resident social and emotional health and minimizes disruption of resident daily routines.
Includes tiers for advanced resident notification and appeals options about cohorting transfers for Phases 1, 2, and 3.
Includes instructions for determining, monitoring, and adapting staffing assignments that maintain cohorts while
minimizing inequity of staff workload. (see Workforce Ecosystem, Slide 23)
Is adaptable based on community COVID-19 prevalence.
Reflects resident rights to return to original room after risk of COVID-19 transmission has been mitigated. (M)
Modify 42 C.F.R. § 483.
15 waiver to require proactive, advance communication about facility cohorting protocols with
residents and residents’ representatives. In the event of a positive COVID-19 test, require advance written notice to residents
and residents’ representatives for all transfers. Commission a study to establish an evidence-based standard for specific time
requirements of advance written notice (e.g., 24-, 48-, 72-hour advance written notice) in the event of a positive test.
Commission a study by the National Academy of Sciences, Engineering, and Medicine (NASEM) to identify effects of cohorting
for prolonged periods of indefinite duration, methods for nursing homes to address those effects, when to use isolation, and
how to adapt when a vaccine emerges. (P).
CMS actions to date:
With CDC, provided
guidance on cohorting.
(8), (14), (15)
Issued 1135 emergency
waiv
ers to provide states
with regulatory flexibilities
to permit and support
cohorting. (20)
Continuing to allow
Hospi
tal Without Walls
and Temporary Expansion
Sites, mitigating the
effects of workforce
shortages and
resident cohorting. (25)
i
- Cohorting is the process of
locating individuals with the same
condition in the same space with
the intent of reducing or eliminating
interaction between infected
persons with uninfected persons.
14
Note to CMS: Some members have not yet endorsed all recs & actions on Cohorting theme

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 3: Cohorting (2/2)
Problem:
Nursing homes may not be able to implement existing cohorting guidance because of staffing, equipment, and/or environmental limitations
(e.g., cleaning, tight space, lack of physical barriers, inadequate ventilation systems) and/or may be inappropriately incentivized to isolate residents.
Principal Recommendation:
Update cohorting guidance to address differences in nursing home resources for cohorting.
Recommended Action Steps:
Recommend nursing homes have an observation unit or separate area for new admission or transfer residents. For nursing homes without sufficient
facilities to create an observation unit or separate area for new residents, continue to allow a long- term care facility to cohort new admissions in another
LTC facility for the purpose of observation by waiving requirements in 42 CFR 483.10(c)(5); 483.15(c)(4)(ii), (c)(5)(i) and (iv), (c)(9), and (d); and
§483.21(a)(1)(i), (a)(2)(i), and (b) (2)(i). Ensure residents and residents’ representatives receive ongoing communications about observation plans and
actions.
Prevent perverse incentivization by addressing and updating the reimbursement differential between cohorted and isolated resident
s. Specifically, modify
RAI/MDS manual coding instructions for isolation because of active infectious disease (Chapter 3 of the MDS 3.0 RAI Manual (O0100M)) to allow capture
of care and services provided to persons with or suspected to have COVID-19 who are isolated per CDC and/or CMS guidelines. Note: Some Commission
members feel this action step is logical and important; others do not.
Redirect and prepare Quality Improvement Network-Quality Improvement Organizations (QIN-QIOs) to assist nursing home providers with development
of effective cohorting plans. (see Technical Assistance and Quality Improvement, Slide 28)
Note to CMS: Some members have not yet endorsed all recs & actions on Cohorting theme
15

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 4: Visitation (1/4)
Problem:
Visitation restrictions implemented to prevent COVID-19 transmission have protected the physical health of residents but also resulted in unintended harm.
Residents are experiencing loneliness, anxiety, and depression due to prolonged separation from families and loved ones. Such measures also compromised
the ability of families and guardians to validate resident wellbeing and safety and caused significant distress for families.
Principal Recommendation:
Emphasize that visitation is a vital resident right. Update and release consolidated, evidence-based guidance on safely
increasing controlled, in-person visitation prior to Phase 3 reopening.
Recommended Action Steps:
Provide guidance on in-person visitation that immediately enables nursing homes to use emerging and established
evidence to adjust protocols and safely increase in-person visitation by essential care partners, compassionate care
visitors, and ombudsman. This CMS in-person visitation guidance should:
Restate the existing right to visitation and clarify modifications to this right for each phase of the pandemic.
Describe o
r restate mini
mum standards for testing, facial coverings and other PPE, temperature checks, physical
distancing, visitor movement restrictions (e.g., separate visitor rooms, indoor/outdoor options, staggered visitation
schedules), post-visit disinfection, instructional signage, supervision and assistance from staff, and COVID-19+ visits.
Outline how to adapt visitation policies based on local prevalence of COVID-19 i
nternal and external to nursing homes.
Encourage nursing homes to have residents designate an Essential Care Partner (ECP); when resident cannot, the
durabl
e power of attorney (DPOA) holder could serve as an ECP or appoint a loved one as an ECP.
Include a revised, person-cent
ered definition of compassionate care and criteria for assessing when compassionate
care and extended end-of-life visitation is appropriate.
Stress that Ombudsmen may visit residents and relay information to families and guardians prior to Phase 3 reopening.
CMS actions to date:
Advised nursing homes to
adopt restrictive visitation
policies. (4)
Expanded visitation
guide
lines in
compassionate care and
other situations. (15)
Provided FAQ about
visitation. (19)
Provided ideas to help
resi
dents connect with
their families. (14)
Incorporated visitor entry
prot
ocols into the COVID-
19 survey tool for nursing
homes. (13)
Advised on Phase 2 and 3
visitation. (15)
16

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 4: Visitation (2/4)
Problem:
Virtual visitation is frequently an insufficient substitute to address resident needs as limitations related to equipment and internet availability; resident,
family, and/or staff unfamiliarity with proper equipment use and functionality; and differing physical abilities may prevent successful implementation.
Principal Recommendation:
Update and release consolidated, evidence-based guidance on effectively planning for and implementing virtual visitation
tools and techniques.
Recommended Action Steps:
Provide guidance on virtual visitation that specifies evidence-based protocols for acquiring, using, and sharing
technology and communicative devices (e.g., cell phones, tablets, web-cams, web applications/platforms) to safely
facilitate virtual visitation. This CMS virtual visitation guidance should:
Emphasize that when a resident has the capability to use such technology independently or with minimal
assistance, it should be permanently issued to them, just as residents used to have with landlines.
Link residents, families, and staff with learning resources about various technology tools.
Include information on accessing and utilizing low-cost, creative methods for maintaining two-way contact
between residents and their loved ones (e.g., messages through windows, Jitterbug flip phone, postcards). (M)
Continue to facilitate the sharing of ideas about virtual visitation options among nursing homes.
Encourage state agencies to approve applications to use civil money penalty (CMP) funds for the purpose of providing
com
municative devices for virtual visitation. (M)
CMS actions to date:
Provided FAQ about
visitation. (19)
Provided ideas to help
resi
dents connect with
their families. (14)
Notified state survey
age
ncies that Civil Money
Penalty (CMP)
reinvestment funds may
be used for programs
that provide residents
with adaptive
communicative
technologies for virtual
visits. (13)
17

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 4: Visitation (3/4)
Problem:
The extent of unintended harm to residents (e.g., loneliness, anxiety, and depression) due to prolonged separation from families and loved ones has not
been adequately assessed; additionally, nursing home staff have under-prioritized routine daily activities, exacerbating the unintended harm caused by
overly restrictive visitation policies.
Principal Recommendation:
Provide resources to help nursing homes assess and improve the mental health and psychosocial well-being of residents during and after the pandemic.
Recommended Action Steps:
Develop and distribute a mental health supplement for the comprehensive resident assessment instrument (RAI) required at 42 C.F.R. § 483.10 to help
nursing homes assess and improve the psychosocial well-being of residents exhibiting a mental health status change. The supplement should:
Include assessment items separate from the current RAI questions on mood and behavior that would specifically identify when a resident is
suffering emotionally due to isolation and lack of family contact due to restricted visitation
Include adaptation options so nursing homes can tailor to enhance their current resident assessments and meet unique needs of residents (M)
Include instruction for implementation by staff with training in behavioral health (P)
Inform resident care, recognizing that residents continue to have the right to shape their own care plans
Monitor a subset of data generated from mental health supplement use and resultant care changes to assess impact; then consider form
ally integrating
this mental health supplement into the RAI. Note: Some Commission members feel this action step is logical and important; others do not.
Issue guidance that promotes regular socialization within facilities and outside of resident rooms; prohibits unnecessary isolatio
n within resident rooms;
and emphasizes the importance of routine daily activities (e.g., showering and personal hygiene, communal meals, meditation, exercise).
Issue guidance for accessing and integrating telehealth mental health services for nursing home residents.
Provide training at no cost to direct care providers on trauma-inf
ormed care.
Amend 42 CFR § 483
.10 to include reference to compassionate care under the residents’ rights provision and define contingencies for emergencies.
18
© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 4: Visitation (4/4)
Problem:
CMS and its federal partners have issued directives and guidance pertaining to visitation during the COVID-19 pandemic that now exist in multiple
documents, making it harder to track federal expectations of nursing homes and any evolving flexibility that has been provided.
Principal Recommendation:
Assess, streamline, and increase the accessibility of COVID-19-related directives, guidance, and resources on visitation
into a single source.
Recommended Action Steps:
Categorize CMS’s COVID-19-related ideas, suggestions, guidance, FAQs, and directives to-date regarding visitation
(“visitation information”). (M)
Analyze visitation information released to date for accuracy and actionability. (M)
Synthesize visitation information into single, user-fri
endly source.
Add single, user-fri
endly visitation information source to dynamic multi-user interface (see Data, Slide 32) to enable
nursing home staff to exchange updated information with CMS and its federal partners and make evidence-based
decisions about visitation policies and procedures.
Establish an operating procedure to ensure timely updates on visitation as new evidence emerges. (M)
Regularly update single visitation source based on emerging evidence.
Work with state and local authorities to harmonize federal, state, and local visitation guidance, ideally through single,
us
er-f
riendly, dynamic multi-user interface (see Data, Slide 32).
CMS actions to date:
Advised nursing homes to
adopt restrictive visitation
policies. (4)
Expanded visitation
guide
lines in
compassionate care and
other situations. (15)
Provided FAQ about
visitation. (19)
Provided ideas to help
resi
dents connect with
their families. (14)
Incorporated visitor entry
prot
ocols into the COVID-
19 survey tool for nursing
homes. (13)
Advised on Phase 2 and 3
visitation. (15)
19

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 5: Communication
Problem:
Knowledge about COVID-19 (e.g., incidence, prevalence, virulence, symptoms, prevention, control, and treatment) is rapidly evolving. Keeping nursing home
residents and their loved ones informed about the most up-to-date information on COVID-19, related protocols, and polices is a significant challenge.
Principal Recommendation:
Increase specificity and expand breadth of guidance on communications between nursing homes, residents, and families.
Recommended Action Steps:
Provide standardized templates (e.g., for progress notes, email blasts, newsletters, bulletins, town hall discussion guides)
for issuing regular COVID-19 updates that nursing homes can tailor to the literacy and cultural needs of recipients,
including residents, essential care partners, resident representatives, family members, loved ones, and advocates.
Define the type of information that nursing homes are expected to communicate (e.g., cohorting plan if a resident or staff
membe
r tests COVID-19 positive; transfer and discharge rights during phases of an emergency; visitation and/or
connection options; screening/testing protocols and policies; COVID-19 cases and deaths).
Define time-se
nsitivity of key communication messages (e.g., messages about transfers, discharge, hospitalization). (M)
Require an individualized communication plan as part of each nursing home resident’s individual care plan that include
pr
eferred mode (e.g., recordings, letters, phone, video, in-person) and frequency (e.g., weekly) of communications;
between whom (e.g., residents, providers, loved ones; one-on-one, small groups, or large groups); and action steps for
missed communications.
Assess and advise nursing homes how federal COVID-19 relief funds can support nursing homes’ adoption of multi-media
communication systems (i.e., involving text SMS, phone, email, virtual townhalls, websites, applications, cameras).
Amend federal requirements for nursing homes to create adoption protocols of multi-medi
a communication systems. (M)
Consider long-te
rm regulations requiring nursing homes to integrate these updated communications methods.
CMS actions to date:
Released guidance to
nursing homes on
alternative means of
communication about
visitation restrictions
including signage at
entrances/exits, letters,
emails, phone calls, and
recorded messages for
receiving calls. (4)
Released the Toolkit for
Sta
te Actions to Mitigate
COVID-19 Prevalence in
Nursing Homes including
examples of
communications practices
across all states. (14)
20

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (1/7)
Problem:
Nursing home workforce ecosystem (education, recruitment, training, and retention) challenges are some of the key systemic failures at the root of the
COVID-19 nursing home crisis. Specifically, low wages, high resident-to-staff ratios, pressure to deliver care for residents with complex needs under difficult
conditions, and a dearth of systemic support significantly contribute to gaps in care for nursing home residents during the COVID-19 pandemic.
Principal Recommendation:
Address nursing home workforce hazard pay; assess and leverage emergency nursing home surge support options; and
emphasize minimum care standards.
Recommended Action Steps:
Assess federal COVID-19 relief funds for hazard pay options; have nursing homes access and distribute hazard pay.
Continue Hospital Without Walls and Temporary Expansion Sites to flex hospital staff to nursing homes. (P)
Assess and adapt existing predictive analytics platforms to anticipate hotspots and nursing home workforce surge needs.
With FEMA and State Departments of Health, update existing emergency management plans to reflect emerging data.
Work with state governments to update interstate compact language for public health emergencies to specifically include
l
i
censed and certified individuals, such as CNAs, to encourage the development of a hotspot staffing pool that can be
used to ensure sufficient staff is available for surge support.
Consider long-te
rm guidance and regulations requiring nursing homes to integrate minimum care standards of hours of
care per resident per day. Commission a study to establish an evidence-based standard for specific minimum care
requirements during times of normal and emergency operations.
Recommend that nursing homes incorporate increased break/recuperation time as well as time for proper PPE donning
and
doffing for direct care providers in emergency management planning.
Assess engagement of medical directors in nursing home emergency management planning and execution.
CMS actions to date:
With HRSA, has provided
$4.9 billion in CARES Act
funding to support skilled
nursing facilities.
With CDC, developed
guidelines for healthcare
facilities to address
potential staffing
shortfalls.
With HHS, enabled
addi
tional $5B through
CARES Act to build skills
and enhance response,
including enhanced
infection control. Funding
can be used to hire
additional staff, implement
infection control
“mentorship” programs.
(23)
21

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (2/7)
Problem:
Certified Nursing Assistants (CNAs) spend more time with nursing home residents—including residents with additional COVID-19 care needs—as compared
to other members of the nursing home workforce, yet they earn the lowest wages among direct care providers and receive few to any benefits. Moreover,
the COVID-19 pandemic has disrupted CNA training critical for reinforcing the nursing home workforce, leading to serious CNA workforce deficits.
Principal Recommendations:
Issue guidance for on-the-job CNA training, testing, and certification; track all CNAs via a central registry; and catalyze
interest in the CNA profession through diverse recruitment vehicles.
Recommended Action Steps:
Permit nursing homes to hire less experienced personnel; provide them with on-the-job, developmentally-appropriate,
culturally mindful CNA training, testing, and certification using current state standards and testing for nursing assistance
certification; and require them to work under supervision upon completion of their on-the-job training and testing.
Assess federal COVID-19
relief funds for on-the-job CNA training options; have nursing homes access these funds.
With academia, monitor on-the-j
ob programs for CNAs and their subsequent performance to verify effectiveness (e.g.,
standard of care, retention rates, continued education) and to accurately track workforce growth. (M)
Include content and relevant links related to CNA careers and certification in the administration’s “Find Something New”
ca
mpaign website. (M)
In partnership with CNA professional associations (e.g., National Association of Health Care Assistants), develop and
impl
ement a National CNA Community of Excellence recruitment campaign.
Develop a public-pri
vate partnership with relevant industry partners and academia to promote and amplify the CNA
Community of Excellence campaign.
CMS actions to date
Waived the requirements
at 42 CFR 483.35(d) –
except for the
competency requirement
under 42 CFR 483.35
(d)(1)(i) – to assist
facilities in addressing
potential staffing
shortages with the
pandemic. (7, 23a)
22

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (3/7)
Problem:
Emerging evidence indicates an increased risk of COVID-19 infection of direct care providers who work across multiple nursing homes. A preliminary analysis
from CDC concluded that direct care providers working across multiple nursing homes — along with direct care providers continuing to work while sick —
helped to hasten the spread of COVID-19. However, systemic workforce ecosystem problems prevent wholesale prohibition of multi-facility employment.
Principal Recommendation:
Provide guidance grounded in maximizing equity and preventing employee burnout that allows nursing home workforce
members to continue to work in multiple nursing homes while adhering to infection prevention and control practices.
Recommended Action Steps:
Distribute guidance for direct care staffing assignment patterns that require multi-facility direct care providers to work only with
residents testing negative for COVID-19 or only with residents testing positive for COVID-19 across nursing homes within a given
week (M). This guidance should include:
A recommendation that multi-facility direct care providers must be tested (diagnostic and serological) before rotating from
serving residents with COVID-19 infection to serving residents without COVID-19 infection
A recommendation that nursing homes enable multi-facility direct care providers who test positive for COVID-19 to
adequately quarantine before rotating from serving residents with COVID-19 infection to serving residents without COVID-
19 infection
A recommendation that direct care providers work at no more than two nursing homes during the pandemic to allow for
accurate contact tracing and monitoring
Assess federal COVID-19
relief funds for paid leave options to support direct care providers during quarantine.
Work with professional associations and organizations representing nursing homes and/or their staff to catalyze adoption of
evid
ence-based, equitable assignment patterns by nursing home administrators and direct care providers. (M)
Develop long-t
erm regulations requiring integration of multi-facility direct care staffing assignment patterns into emergency
planning.
CMS actions to date:
With CDC, issued
guidance that
encourages direct care
providers to tell facilities
if they have had
exposure to COVID-19
cases in other facilities.
(8)
23

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (4/7)
Problem:
SARS-CoV-2 manifests itself in sudden clinical changes that require astute triage, assessment, intervention, and stabilization and/or transfer of the resident
to a higher level of care. These capabilities fall within the scope of practice of a registered nurse (RN); however, RNs are insufficiently present in nursing
homes, especially during overnight hours, leaving LPNs and CNAs to complete tasks that may fall beyond their scope of practice.
Principal Recommendation:
Leverage funding and encourage the use of regional health system resources in partnership with state and local authorities
to provide 24/7 RN staffing resources at nursing homes in the event of a positive COVID-19 test within that facility.
Recommended Action Steps:
Support 24/7 RN staff augmentation in nursing homes with COVID-19 incidence among residents.
Monitor and evaluate mortality and transfer rates of residents who have tested COVID-19
positive when an RN has
been consistently present during their care.
Commission a study to establish an evidence-bas
ed standard for specific, competency-based care requirements during
times of normal and emergency operations.
CMS actions to date:
Waived requirements in
42 CFR 483.30(e)(4)
related to the delegation
of certain tasks
physicians must provide
personally; allows
delegation of these tasks
to a physician assistant,
nurse practitioner, or
clinical nurse specialist.
(23a)
24

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (5/7)
Problem:
While the current regulation for an infection preventionist in a nursing home requires facilities to designate a minimally-qualified infection preventionist, the
requirement is insufficient to meet the infection control and prevention demands of the current COVID-19 pandemic. Specifically, there are few
recommendations included about training and licensure requirements. Moreover, this position is not financially supplemented, so the position is
traditionally assigned to a supervisor, nursing manager, or provider as an added rather than a core responsibility.
Principal Recommendations:
Identify and immediately leverage certified infection preventionists to support nursing homes’ infection prevention needs.
Pr
ofessionalize infection prevention positions in nursing homes by updating regulations at 42 CFR § 483.80
so more fully
qualified infection preventionists are available to serve in nursing homes.
Recommended Action Steps:
Create a national registry of certified infection preventionists to provide immediate assistance to nursing homes
without dedicated infection prevention support. Leverage infection preventionist resources from FEMA, the National
Guard, the Public Health Service Corps, infection prevention recruiting companies, and infection prevention
professional organizations (e.g., APIC and/or SHEA).
Utilize training programs to provide a standardized, required, regularly-updated training curriculum and certification for
infection preventionists in nursing homes at no cost to nursing homes. Established programs to consider:
Center for Disease Control and Epidemiology’s Nursing Home Infection Preventionist Training Course
Association for Professionals in Infection Control’s EPI in Long-Term Care Certificate Program, EPI Intensive
Certificate Program, CIC Certification Preparation, Basics of Infection Prevention and Control for Non-Clinicians
Society for Healthcare Epidemiology of America’s Podcast Series: Infection Control in Long-Term Care Facilities,
SHEA/CDC Outbreak Response Training Program
Certification Board of Infection Control and Epidemiology Certified in Infection Control process
American Healthcare Association Infection Preventionist Specialized Training
CMS actions to date:
• With CDC, developed and
released nursing home
infection preventionist
training courses (6)
• Mandated that all
nursing homes have at
least a part-time
infection preventionist
under 42 CFR § 483.80
(23)
25

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (6/7)
Problem:
Workforce members with expertise in infection prevention and control competency development are not sufficiently utilized in nursing homes. When
utilized, nursing homes may use external vendors/ staffing agencies with fewer insights into local nursing home context. This underutilization and insufficient
integration has yielded knowledge and skills deficits among the workforce, especially related to emerging evidence about COVID-19 infection mitigation.
Maintaining updated standards of care requires dedicated, onsite education and infection prevention professionals. This is a critical workforce problem that
has caused serious infection prevention and control challenges throughout the pandemic.
Principal Recommendations:
Require nursing homes to employ infection preventionist(s) with educator duties and assess clinical evidence to establish an
FTE: bed ratio, including considerations for Health Professional Shortage Areas (HPSAs).
Recommended Action Steps:
Require infection prevention educators (“IP Educators”) to provide and document competency-driven, experiential
training on core practice; crisis standards of care, including fit testing of N-95 masks and PPE donning and doffing; and
recovery; and regularly assess competency achievement of all direct and contract staff (e.g., administrators, nurses, CNAs,
environmental services, maintenance, food service, and ancillary staff).
Provide templates for IP Educators to track staff infection prevention onboarding, training, and competency achievement.
With CDC, develop for and distribute to IP Educators competency and self-eff
icacy measurements for proper PPE usage.
Endorse individual competency assessment and achievement at an 80% threshold or higher.
With state health departments, encourage collaborative site visits by infection control and prevention experts.
With state and local authorities, develop partnerships with acute care/academic facilities to share simulation resources.
Encourage state agencies to approve applications to use civil money penalty (CMP) funds for training costs (M).
Include in Quality Assurance and Performance Improvement (QAPI) programs audits of IP education provision and
pa
rt
icipation and related IP emergency management protocols (M).
CMS actions to date:
• With CDC, developed and
released nursing home
infection preventionist
training courses (6)
• Mandated that all
nursing homes have at
least a part-time
infection preventionist
under 42 CFR § 483.80
(23)
26

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 6: Workforce Ecosystem (7/7)
Problem:
Workforce ecosystem (education, recruitment, training, retention) challenges are notably longstanding, but have been exacerbated by the pandemic.
Efforts to address workforce ecosystem challenges have been delayed, further jeopardizing an already fragile nursing home system. In addition to low pay
and limited benefits, lack of educational support (e.g., limited assistance in progressing into LPN/RN training), insufficient competency standards, low-to-no
exposure to geriatrics in formal education programs, and limited opportunities for professional advancement (e.g., no clinical ladder or lattice) limit the
potential of the emerging workforce required to stabilize the nursing home system.
Principal Recommendations:
Convene a Long-Term Care (LTC) Workforce Commission and/or Advisory Board to assess, advise on, and provide independent oversight for
modernization of workforce ecosystem. (M)
Work with federal, state, local, public, private, and academic partners to catalyze overhaul of workforce ecosystem.
Recommended Action Steps:
Develop a charter and criteria to identify potential stakeholders to participate in the LTC Workforce Commission and/or Advisory Board. (M)
Identify and work to achieve funding mechanisms that defer/reimburse CNA and LPN education costs after 3+ years of service in nur
sing homes.
Establish a competitive grant program and/or national scholarship to fund entry into practice education for aspiring CNAs.
With CDC and OSHA, identify core competencies for long-t
e
rm care direct care providers; use to develop and/or update national training programs and
standards (e.g., Nurse Aid National Training and Competency Evaluation Program).
Work with the ANA, NAHCA, trade schools, universities, and state certification/licensure authorities to modify RN, LPN, and CNA
clinical training
standards for certification and licensure to include a clinical rotation in geriatrics in a long-term care setting to supplement staffing and provide
immersion into geriatric care.
With professional nursing associations and organizations, develop a meaningful national clinical ladder and lattice for long-term
direct care providers—
including CNAs, LPNs, and RNs—that includes access to career advancement opportunities and improved compensation.
27

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 7: Technical Assistance and
Quality Improvement
Problem:
Technical assistance and quality improvement support have not been sufficiently available to nursing homes during the pandemic. While Quality
Improvement Organizations (QIOs) provide asynchronous toolkits, information guides, and online learning options, nursing homes need proactive, tailored,
timely, on-the-ground support in emergency management, infection prevention and control, and workforce capability development.
Principal Recommendation:
Identify and work to achieve funding mechanisms for–or reprioritize activities of–technical assistance and other contractors
to increase the availability of collaborative, on-site, data-driven support prior to, during, and after a COVID-19 outbreak.
Recommended Action Steps:
Redirect, prepare, and coordinate in partnership with regional strike teams Quality Improvement Network (QIN)-QIOs
and other technical assistance contractors to provide on-the-ground technical assistance with organizational
diagnosis, strategic direction, organizational resilience, resource prioritization, emergency management assistance,
data management assistance, and workforce capability development in infection prevention and control, trauma-
informed care, person-centered and person-directed care, visitation, and family communications and engagement.
Research and provide exemplars of federal and regional strike teams.
Support QIN-Q
IO
technical assistance work with nursing homes and reinforce a cultural of learning by grounding
information about citations and penalties in QAPI methodologies.
Create and distribute an organizational-le
vel Quality Assurance & Performance Improvement (QAPI) tool on how to
effectively respond to COVID-19.
Encourage nursing homes to use QAPI tools, data, and methodologies to improve their performance.
Provide instruction to state surveyors on the Focused Infection Control (FIC) rules and survey process, including
in
formation about when surveyors should provide nursing homes with immediate feedback.
CMS actions to date:
Announced the
deployment of QIN-QIO
resources to hotspots.
(21)
With CDC and OASH,
deployed Federal Task
Force Strike Teams for
onsite infection control
technical assistance and
education to nursing
homes experiencing
COVID-19 outbreaks. (23)
28

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 8: Facilities (1/2)
Problem:
The physical environment in many nursing homes is not optimally designed to limit spread of transmissible diseases. Fundamental design changes are costly
and may take longer to implement but may be necessary due to the prolonged risks to residents from COVID and to position facilities to manage future
epidemics.
Principal Recommendations:
Identify and share with nursing homes short-term facility design enhancements to address immediate pandemic-related
risks that can be implemented at minimal cost.
Establish a collaborative national forum to identify and share best practices and recommendations; facilitate real-tim
e
learning on how to best use existing physical spaces.
Collaboratively establish long-te
rm priorities and seek appropriate funding streams for nursing homes to redesign and/or
strengthen facilities against infectious diseases. (M)
Recommended Action Steps:
Close information gaps on how best to modify the physical plant by gathering best practices and issuing guidance.
Examples of design enhancements:
Resident rooms: The ability to physically separate residents is greatly enhanced when rooms are occupied by only a
single resident.
HVAC and air flow: modification and upgrades to HVAC systems further harden the infrastructure and potentially limit
transmission.
CMS actions to date:
With CDC:
Recommended identifying
space in nursing homes
that could be dedicated to
preventing and controlling
COVID-19 (Updated June
25)
29

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 8: Facilities (2/2)
Recommended Action Steps:
Work with CDC to supplement CDC guidance with guidelines for the manipulation of HVAC systems that can reduce risk of transmission by:
Adjusting existing systems to support infection control (e.g. creating negative pressure, replacing filters)
Supplementing systems with equipment that can further purify air (e.g. air ionization, air scrubbers)
Setting standards for HVAC system performance as part of the long-term plan to upgrade systems and redesign nursing homes
Encourage nursing homes to shift residents to single occupancy rooms for facilities that can accommodate this approach without de
trimental reduction in
census. Examine changes to the CMS reimbursement that would promote single occupancy (temporarily during pandemic and long-term).
Establish a task force jointly led by industry, safety and consumer organizations to identify long term priorities for elder care
in the United States with
emphasis on the redesign, retrofitting, and reconfiguration of nursing homes to be resilient to infectious disease threats. (M) Topics to be considered
include, but are not limited to:
The ability to separate wings for cohorting
Separate entrances and exits
Separate areas for staff and restrooms
Separate areas to put on and remove PPE
UV systems for decontamination
HVAC upgrades and retrofitting
Design considerations that take resident quality of life into consideration
Consider a public-pr
ivate partnership that issues a challenge for nursing home redesign. (M)
30

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 9: Nursing Home Data (1/3)
Problem:
Nursing homes’ burden to report COVID-19 data to the federal government is not being sufficiently offset by the resulting benefit provided to nursing home
residents, families, staff, and other stakeholders.
Principal Recommendation:
Improve COVID-19 data element standardization and data collection while identifying specific actions that CMS and federal
partners will take in response to changes in key COVID-19 data indicators based on data reported by nursing homes.
Recommended Action Steps:
Work with CDC to improve existing data elements and incorporate additional elements into the NHSN dataset that are
essential for improved clinical outcomes and quality care delivery such as data on diagnostic test turnaround time,
infection-control measures, staffing information, and housekeeping services.
Capture and identify actions responding to the experiences, perspectives, and other specific issues of nursing home
resi
dents, families and staff through data related to demographics, visitation, satisfaction, quality of life, depression, and
basic behavioral needs – such as ensuring residents have access to a phone.
Partner with state and local authorities to develop threshold criteria for key nursing home data indicators (positive
COVI
D-19 test results, deaths, low PPE supplies, staffing details) that will trigger responses by CMS along with state and
federal partners (M).
Leverage actionable nursing home equipment and supplies data reported to NHSN to assist with coordination of available
res
ources and support for screening, testing, cohorting, training, and equipment needs at a national level.
Provide clear guidance regarding the use of nursing home data to support facilities in a cap
ability-enhancement manner
while recognizing the need for enforcement of quality and safety standards.
Require nursing homes to retrospectively report data on COVID-19 c
ases and deaths that occurred prior to the reporting
requirements established in the May 2020 Interim Final Rule. Note: Some Commission members feel this action step is
logical and important; others do not. Note: CMS has stated publicly that it lacks legal authority to require this.
CMS actions to date:
With CDC, refining and
creating more specificity
for certain COVID-19
NHSN data elements.
With CDC and OASH,
prov
ided staff for Task
Force Strike Teams to
provide technical
assistance and training to
certain nursing homes, in
response to data that
they reported to CDC
indicating increases in
COVID-19 cases. (23)
Based on data reported,
shar
e list of nursing
homes with increased
cases each week to assist
states in targeting
support. (23)
Note to CMS: Some members have not yet endorsed all recs & actions on Data theme
31

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 9: Nursing Home Data (2/3)
Problem:
Information about the COVID-19 pandemic that is relevant to nursing homes has been inconsistent and scattered across multiple locations, making it difficult
to find relevant, trustworthy, up-to-date data and guidance. Although the situation continues to rapidly evolve and some initial efforts have been made to
consolidate information, a more cohesive approach to data collection and information dissemination is needed.
Principal Recommendation:
Develop a single, bidirectional application to serve as a central interface for nursing home data collection and information
dissemination that includes essential COVID-19 guidance, statistics, and outcomes.
Recommended Action Steps:
Collaborate with health IT resource and nursing home data providers to define and prioritize features and capabilities
of the single, bidirectional application (M).
Develop a secure method for nursing homes to enter new data and correct previously submitted data.
Provide dynamic, real-time
, mobile-friendly, HIPAA-compliant, and actionable feedback reports to nursing homes and
federal partners based on the data entered or queried. The reporting elements should include, but are not limited to,
clinical and performance metrics, resource utilization, survey responses, inspection data, and information related
to the well-being of residents.
Integrate a COVID-19 toolkit into the application to include an interactive map of states with the current
applicable metrics, mandates, and guidance.
CMS actions to date:
Established the COVID-19
Nursing Home Data website,
which provides access to the
COVID-19 Public File
containing data reported by
nursing homes to CDC’s NHSN
system, along with related
resources and statistics. (10),
(13), (26)
Published actions taken in
resp
onse to COVID-19 on the
CMS website. (26)
Indicated to the Commission
at it
s final convening that
work on a new user interface
has been initiated.
Note to CMS: Some members have not yet endorsed all recs & actions on Data theme
32

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Theme 9: Nursing Home Data (3/3)
Problem:
The lack of consistent nursing home data communication standards has hindered data management and data sharing between providers and payers, delayed
effective care delivery, and resulted in poor data integration across care settings.
Principal Recommendation:
Enhance health information technology (HIT) interoperability to facilitate better communication, improve quality
measurement standards, and coordinate integration of nursing home data with data from other health organizations.
CMS actions to date:
Recommended Action Steps:
Partner with ONC to develop interoperability and communication standards to integrate nursing home data with data
from other health organizations, as demonstrated by ONC’s Health IT Certification Program in the EHR market (M).
Incentivize nursing homes to adopt health information technology to standardize data collection, transmission, and
manage
ment to support health information exchange and access to comprehensive electronic health records by care
providers across settings.
Promote interoperability standards across nursing homes.
Partner with state and local authorities to assess data needs and leverage data assets.
Foster collaboration, data transparency, and information-s
haring
across health organizations and information technology
vendors. Note: Some Commission members feel strongly that if nursing homes are encouraged to contribute to data
transparency, CMS should ensure protection of the facilities and healthcare providers through federal protections.
Worked with states to survey
nursing homes for
compliance with 42 CFR
483.80 and CDC guidance,
requiring nursing homes to
notify state or local health
department about residents
or staff with suspected or
confirmed COVID-19. (11)
Used the NHSN to collect
standar
dized COVID-19 data
from nursing homes through
new reporting requirements.
(13)
Note to CMS: Some members have not yet endorsed all recs & actions on Data theme
33

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
CMS Actions to Date Reference List (still being validated; updated through 8/11)
(1) Initial Action to Prepare Healthcare Facilities (February 6, 2020)
(2)
Screening of entrants into nursing homes (March 4, 2020)
(3)
The use of PPE (March 10, 2020)
(4)
Restriction of staff and visitors (March 13, 2020)
(5)
Inspections and immediate jeopardy (March 23, 2020)
(6)
COVID-19 Survey for Nursing Homes Webinar Series (March 23, 2020)
(7)
Hospitals / laboratories can test for COVID-19 (March 30, 2020)
(8)
Infection control responsibilities (April 2, 2020)
(8a)
Emergency Declaration Blanket Waivers (April 9, 2020) (same as 23)
(9)
Payment for COVID-19 testing doubles (April 15, 2020)
(10)
Nursing homes must report cases to residents/families (April 19, 2020)
(11)
Notification of Confirmed COVID-19 ... Residents/Staff (April 19, 2020)
(12)
Independent COVID-19 Commission (April 30, 2020)
(13)
Details to State Survey Agency directors (May 6, 2020)
(14)
COVID-19 toolkit for Nursing Homes (May 13, 2020)
(15)
Guidance on the reopening of nursing homes and related FAQs (May
18, 2020)
(16)
COVID-19 survey activities (June 1, 2020)
(17)
COVID-19 nursing home results from inspections (June 4, 2020)
(18)
Coronavirus Commission membership (June 19, 2020)
(19)
FAQs on nursing home visitation (June 23, 2020)
(20)
The end of the emergency blanket waiver (June 25, 2020)
(21)
Assistance from QIOs to hotspot nursing homes (July 10, 2020)
(22)
Rapid point-of-care diagnostic devices and tests (July 14, 2020)
(23)
New resources to protect nursing home residents (July 22, 2020)
(23a)
Emergency Declaration Blanket Waivers (July 28, 2020)
(24)
Reimbursement for counseling isolated residents (July 30, 2020)
(25)
CMS Flexibilities to Fight COVID-19 (July 30, 2020)
(26)
COVID-19 Nursing Home Data (Aug. 2, 2020)
(27)
Nursing Home Data - Point of Care Device Allocation (Aug.6, 2020)
34

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
How to Read These Slides
Problem:
This area contains the problem(s) identified by the Commission for each of the topic areas/themes
Principal Recommendation(s):
This area outlines the Commission recommendation(s) to address the identified problem(s), at
times enhanced by MITRE based on subsequent research and/or by public input.
Recommended Action Steps:
This
area contains specific action steps for CMS to address the recommendation(s) above, with a
focus on chronological actionable steps, at times enhanced by MITRE based on subsequent
research and/or by public input.
CMS
actions to date:
This area outlines CMS’s
actions to date relevant to
the theme. In some cases,
the area may also mention
actions by other federal
partners.
Numbers in parentheses
refer to specific CMS action
source citations on Slide 34
35

© 2020 THE MITRE CORPORATION. WORK PRODUCT - PRE-DECISIONAL – FOR RELEASE TO SPONSOR - CMS –
NOT FOR DISTRIBUTION. COMMISSION CONFIDENTIAL & PROPRIETARY.
Data Rights Notice
NOTICE
This presentation was produced for the U. S. Government under Contract Number
75FCMC19F0012, and is subject to Federal Acquisition Regulation Clause 52.227-14,
Rights in Data-General.
No other use other than that granted to the U. S. Government, or to those acting on
behalf of the U. S. Government under that Clause is authorized without the express
written permission of The MITRE Corporation.
For further information, please contact The MITRE Corporation, Contracts Management
Office, 7515 Colshire Drive, McLean, VA 22102-7539, (703) 983-6000.
© 2020 The MITRE Corporation.
36

