Page 1 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2019 MISSISSIPPI WORKERS’ COMPENSATION CLAIMS GUIDE
This Guide, now in its fifth edition, represents a collaborative effort by
representatives of the Mississippi Workers’ Compensation community who serve
on the Board of Directors of the Mississippi Workers’ Compensation Educational
Association, Inc.
The MWCEA Board members responsible for the 2019 revisions of this
Guide were:
James M. Anderson, Anderson Crawley & Burke, pllc
TG Bolen, Markow Walker, P.A.
Andre Ducote, Morgan and Morgan
Steve Funderburg, Funderburg Sessums & Peterson, PLLC
Gary Jones, Daniel Coker Horton and Bell, P.A.
Michael Traylor, Schwartz & Associates, P.A.
The Guide was designed to provide those responsible for claims decisions
with information that will facilitate appropriate claims handling. It is intended to
only be a summary that includes the basic provisions of the Mississippi Workers’
Compensation Law, and it does not attempt to cover every issue that might be
encountered in the handling of claims or to be a substitute for competent legal
advice. This guide is not an official publication of the Mississippi Workers’
Compensation Commission and since cases are usually fact intensive and the law
is continually evolving, it should not be construed as the Commission’s official
pronouncement of the law on any issue.

Page 2 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Mississippi Workers’ Compensation Educational Association, Inc.
Board of Directors, July 2019
Andre F. Ducote*
President
(601) 949-3388
aducote@forthepeople.com
T. G. Bolen, Jr.*
Vice President
(601) 853-1911
tgbolen@markowwalker.com
Tina O’Keefe*
Immediate Past President
(662) 357-1185
TOkeefe@goldstrike.com
Barbara Oltremari
Board Member
(601) 720-8091
barbaraoltremari@gmail.com
Steven H. Funderburg
Past President
(601) 355-5200
sfunderburg@jfsplawfirm.com
Molly Staley
Board Member
(601) 987-8200
mstaley@capitalortho.com
*Executive Committee

Page 3 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
MISSISSIPPI WORKERS’ COMPENSATION CLAIMS GUIDE
Guide Overview 1
1. MWCEA Board of Directors 2
2. Table of Contents 3
Chapter 1—The Basics 7
1. What is Workers’ Compensation? 7
2. Administration of Mississippi Workers’ Compensation 7
3. Who pays Workers’ Compensation Claims? 8
4. What are an Adjuster’s Responsibilities? 9
5. Adjuster Licensing 9
6. Adjuster Canons of Ethics 10
Chapter 2—Coverage 11
1. Employers Covered by the Act 11
2. What Happens if an Employer Refuses to Get Coverage? 11
3. Insurance Coverage 12
a. Standard Workers’ Compensation Insurance Policy 12
b. Employers’ Liability Insurance Coverage 13
c. Cancelling and Non-Renewing Coverage 13
4. Self-Insurance and Group Self-Insurance 14
5. Assigned Risk Coverage 14
6. Notice of Coverage 14
Chapter 3—Jurisdiction 16
1. Mississippi Jurisdiction 16
2. Injuries Outside of Mississippi 16
3. Non-Residents of Mississippi Injured in Mississippi 16
4. Concurrent Jurisdiction 17
Chapter 4—Exclusive Remedy 18
1. What is Exclusive Remedy? 18
2. Exceptions to the Exclusive Remedy Doctrine 18
Chapter 5—Compensability 20
1. Burden of Proof 20
2. Injury Defined 21
a. Arising Out of and In Course of Employment 22
b. Untoward Event 24
c. Contributed to, Aggravated, or Accelerated by Employment 24
d. Presumption in Death Cases 25
e. Willful Act of Third Person/Assaults 25

Page 4 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
f. Occupational Diseases 27
3. Hernia Claims 27
4. Going to and Coming from Work 28
5. Mental Injuries 29
6. Cumulative and Repetitive Injuries 30
7. Last Injurious Exposure 31
8. Multiple Carriers in Compensability Dispute 31
9. Idiopathic Falls 32
Chapter 6—Defenses to Claims 33
1. Employee Status 33
a. Undocumented Workers/Aliens 34
2. Pre-existing Conditions 35
a. Second Injury Fund 35
b. Apportionment 36
37
3. Statute of Limitations 37
a. Where No Indemnity Benefits are Paid 37
b. Where Indemnity Benefits are Paid 38
4. Intervening Cause of Disability 39
5. Intoxication 40
40
6. Willful Intention to Injure Self or Another 41
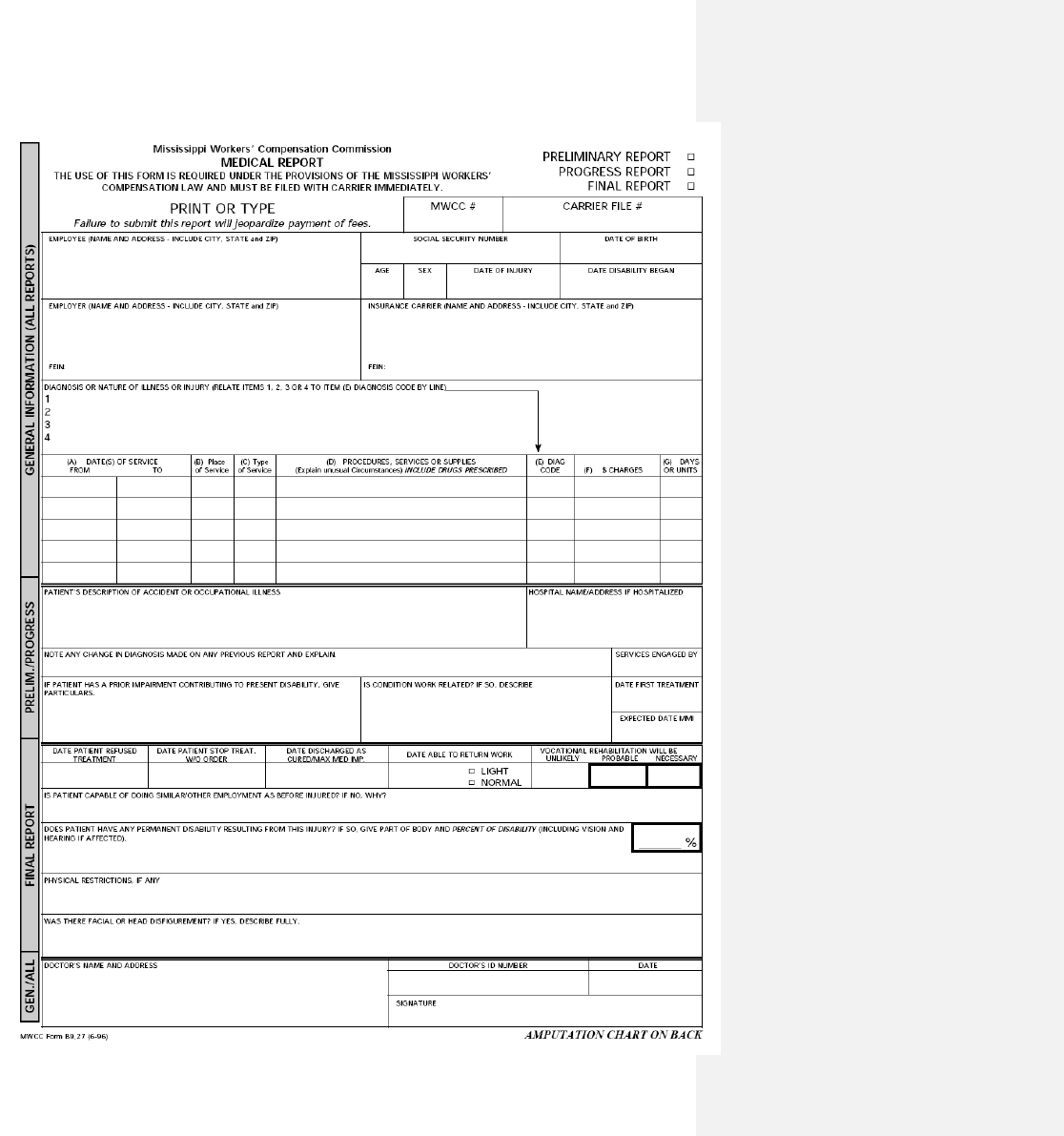
Chapter 7—Commission Forms 43
1. Address for Form Filing 43
2. A Forms 43
a. A-16, Notice of Coverage 43
b. A-24, Proof of Coverage 44
3. B Forms 44
a. IAIABC IA-1, (replaces the B-3), First Report of Injury 44
b. B-18, Notice of Payment 45
Practice Point: Possible admission of liability 45 c. B-19, Application for Lump Sum Payment
c. B-19, Application for Lump Sum Payment 45
d. B-9, 27, Medical Report 46
e. B-31, Notice of Final Payment 46
Practice Point: Completing B-31 for 5, 6, 7 days lost time 47
Practice Point: C-1 Issue 47
f. B-52, Employer’s Notice of Controversion 48
g. B-5, 11 and B-5, 22, Petition to Controvert and Answer 49
4. R Forms 49
a. R-1, Early Notification of Severe Injury 49
b. R-2, Referral for Rehabilitation and Initial Report 49

Page 5 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 8—Average Weekly Wage 50
1. Three Formulas 50
2. Partial Weeks Worked 51
3. Employed for Short Time Before Injury 51
4. Gratuities/Tips 52
5. Sick Pay and Vacation Pay 52
6. Part Time Employees 53
7. Claimant with More Than One Job at Time of Injury 53
Chapter 9—Disability Benefits 54
1. Maximum and Minimum Weekly Amounts 54
2. Waiting Period 54
3. Non-Consecutive Lost Time Days 55
4. Daily Compensation Rate 55
5. Maximum Recovery 55
6. Penalties for Late Payments 56
7. Overpayments 56
8. Child Support Liens 57
a. Obligations in the event of a settlement 58
Chapter 10—Categories of Disability 59
1. Temporary Total Disability 59
Practice Point: Salary in Lieu of Compensation 61
2. Temporary Partial Disability 61
3. Permanent Partial Disability 62
a. Scheduled Member Injuries 63
1) Use of AMA Guidelines 63
b. Body as a Whole Injuries 66
c. Serious Head or Facial Disfigurement 68
4. Permanent Total Disability 68
Chapter 11—Death Benefits 70
1. Immediate Lump Sum Payment 70
2. Funeral Allowance 70
3. Weekly Benefits to Dependents 70
a. Death Claims Involving Undocumented Workers (Aliens) 72
4. Payment to Second Injury Fund 73
Chapter 12—Medical Benefits 74
1. Choice of Physician 74
a. Selection of DME Vendor, Pharmacy Vendor 75
b. Selection of Diagnostic Testing Facilities 75
2. Travel Expense 76
3. Employer’s Medical Exam (EME) 76
4. Independent Medical Exam (IME) 77

Page 6 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
5. Ex parte Communications with Medical Providers 78
6. HIPAA Compliant Medical Authorization 79
7. Treatment by VA Hospital or Paid for by Government 79
8. Medical Payments by Health Insurance Providers 80
9. Mississippi Workers’ Compensation Fee Schedule 80
a. Where to Obtain Fee Schedule 80
b. Issues Addressed in Fee Schedule 81
c. Pre-Certification 81
d. Appeals for Denials of Pre-Certification 83
e. Retrospective Review 84
f. Provider’s Responsibilities 84
g. Fees for Copy Expenses 85
h. Payer’s Responsibilities 86
i. Facility Fee Issues 86
j. Explanation of Review 86
k. Request for Reconsideration 87
l. Dispute Resolution 87
Chapter 13—Vocational Rehabilitation 89
1. Use of Vocational Rehabilitation Professionals 89
Chapter 14—General Issues 90
1. Settlements 90
2. Lump Sum Payments 92
3. Subrogation/Claims Against Third Parties 92
4. Medicare’s Interests 94
5. Medicaid’s Interests 95
6. Social Security Offsets 96
7. Fraud 96
8. Claimant’s Attorney Fees 97
2012 Amendment Regarding Attorney Fees 97
Chapter 15—Litigation Procedures 98
Chapter 16—Mediation 101
Chapter 17—Bad Faith Claims 102
1. What is Bad Faith? 102
2. Suggestions for Avoiding Bad Faith 104
Chapter 18 – 2012 Legislative Changes 105
Epilogue 108
MWCEA Board of Directors 109

Page 7 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2019 MISSISSIPPI WORKERS’ COMPENSATION CLAIMS GUIDE
Chapter 1
THE BASICS
1.1. WHAT IS WORKERS’ COMPENSATION?
Workers’ compensation is a social program that is designed to provide
wage replacement and medical benefits to workers who are injured on the job.
Although the roots of workers’ compensation can be found in Germany in the
1800’s, it was not until 1911 that the first workers’ compensation law that
sustained constitutional challenges was enacted in this country. Now virtually
every state in the United States has a workers’ compensation law and there are
also federal workers’ compensation laws applicable to certain employees.
Mississippi adopted its workers’ compensation law in 1948 with the law becoming
effective January 1, 1949. The Mississippi Workers’ Compensation Law is
codified at Miss. Code Ann. §71-3-1, et. seq. (1972, as amended). Numerous
Commission Rules have also been adopted that explain and assist in the
implementation of the law. Those are available on the Commission Web site at
http://www.mwcc.state.ms.us/pdf/gen&proRules.pdf.
1.2. ADMINISTRATION OF MISSISSIPPI WORKERS’
COMPENSATION
In Mississippi, the Mississippi Workers’ Compensation Commission
administers the workers’ compensation law. See Miss. Code Ann. §71-3-85
(1972, as amended). The Commission is comprised of three individuals
appointed by the Mississippi Governor with approval of the Mississippi Senate.
Each appointment is for a six-year term and the appointments are staggered so
that an appointment comes up every two years. One Commissioner is designated
as Chairman who is the administrative head of the agency. One of the members
of the Commission must be a licensed Mississippi attorney, another is appointed

Page 8 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
to represent business interests and the other is chosen to represent employee
interests.
In Mississippi, litigated cases are tried before an Administrative Judge
(often referred to as an AJ or ALJ) who is an employee of the Commission. All of
the Administrative Judges are licensed Mississippi attorneys. See Miss. Code
Ann. §71-3-93 (1972, as amended). There are up to 8 Administrative Judges
who are hired by the Commission with the approval of the Governor, and their
appointments are not for any specific amount of time. The Commission employs
a staff to carry out the Commission’s statutory responsibilities. When an
Administrative Judge’s decision is appealed to the full Commission, the
Commission considers the appeal based on the record made before the
Administrative Judge. The Commission appellate review is not a new trial.
The Mississippi Workers’ Compensation Commission is located at 1428
Lakeland Drive, Jackson, Mississippi 39216. The Mailing address is P. O. Box
5300, Jackson, Mississippi 39296-5300. The telephone number is 601 987 4200
or toll free, 866 473 6922.
1.3. WHO PAYS WORKERS’ COMPENSATION CLAIMS?
Although some employers are exempt from the application of the law (as
discussed more fully in subsequent sections), all other employers are required to
protect their liability for the payment of workers’ compensation benefits by either
purchasing a workers’ compensation insurance policy, qualifying as a self-insurer
before the Mississippi Workers’ Compensation Commission, or participating in a
group self-insurance fund which is regulated by the Mississippi Workers’
Compensation Commission. The Commission does not pay claims. Some
employers might self-administer their workers’ compensation programs and pay
the claims themselves, but most employers utilize an insurance company or
third-party administrator to pay their claims. Miss. Code Ann. §71-3-75 (1972,
as amended).
Page 9 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
1.4. WHAT ARE AN ADJUSTER’S RESPONSIBILITIES?
The primary duties of a workers’ compensation adjuster, whether that
person is working for an employer, an insurance company or a third-party
administrator, are very similar. Those responsibilities begin with completing a
prompt and thorough investigation of every claim so that an informed and
timely decision may be made regarding the payment of benefits as is appropriate
under the facts of each claim. Talking with employers, claimants, and co-
employees to determine facts; obtaining and evaluating medical documentation
concerning the medical problems which are a part of each claim; evaluating
disability information from the medical providers; and timely paying
compensation, medical and rehabilitation benefits, as appropriate under the law
and the circumstances of each claim, are all a part of the claims professional’s
job. Those responsibilities require effective written and oral communication skills
and the ability to interact with employers, claimants, witnesses, the medical
community, attorneys, and the Commission staff regarding decisions made and
the reasons for those decisions and actions.
1.5. ADJUSTER LICENSING
Adjusters must obtain a Property and Casualty license from the Mississippi
Department of Insurance unless that adjuster only handles claims for the
insurance company by whom he or she is employed. (To explain, adjusters
employed by an insurance company and only handling claims for that insurance
company do not have to have a Mississippi adjuster license, while adjusters for a
third-party administrator do have to obtain a license.) Effective July 1, 2016
there is a separate insurance adjuster license applicable only to workers’
compensation claims, although a general adjuster’s license such as is required to
handle all other kinds of claims may be utilized instead of the specific workers’
compensation adjuster’s license. The applicant is required to attend training as

Page 10 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
dictated by the Mississippi Department of Insurance and pass a test. However, a
test is not required for one who is licensed as an adjuster in another state with
which the Mississippi Department of Insurance has entered into a Reciprocity
Agreement. For licensing requirements, see Miss. Code Ann. §83-17-417 (1972,
as amended) or details on the Mississippi Department of Insurance’s website,
http://www.mid.ms.gov/licensing/adjuster-licensing.aspx.
1.6. ADJUSTER CANONS OF ETHICS
Although there are no officially adopted canons of ethics applicable to
Mississippi workers’ compensation adjusters, the law indicates that an adjuster is
in a position of fiduciary responsibility and is responsible for making sure that
legitimate claims are paid timely. Many see the adjuster’s job as one that
includes responsibility for the maintenance of the integrity of the workers’
compensation system consistent with the social purposes of the legislation so as
to promote public confidence and trust in the system. Others urge that care
should be taken not to violate laws or regulations applicable to a situation and
argue that a sense of urgency to do the job promptly should be paramount.
Nearly everyone would agree that being courteous and sensitive to the issues is
a part of maintaining professionalism expected by the workers’ compensation
system. Just as the adjuster should strive to avoid unnecessary litigation and
delays, it is argued that the adjuster should also support efforts to prevent fraud
within the system. Common sense suggests that care must be taken by the
adjuster to avoid a conflict of interest and to make decisions free from personal
prejudices or other form of illegal discrimination.
The current adjuster continuing education hour requirements are 24 CEU
credits every two years and 3 ethics hours.
Page 11 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 2
COVERAGE
2.1. EMPLOYERS COVERED BY THE ACT
The Mississippi Workers’ Compensation Act requires coverage if an
employer “has in service five or more workmen or operatives regularly in the
same business or establishment under any contract of hire, express or implied.”
See Miss. Code Ann. §71-3-5 (1972, as amended). Often, the number of workers
employed may fluctuate above and below five and the employer and/or carrier
may be left wondering whether coverage is necessary. The test is generally one
of the size of the operation and whether five or more employees are “regularly”
used to carry it on (even if all 5 employees are not employed at the same time).
If the answer is “yes,” then coverage is necessary, and if in doubt, the employer
is encouraged to obtain coverage. There are certain categories of employers who
are not subject to the coverage requirements of the Act, regardless of the
number of workers employed. The list of exempted employers includes nonprofit
charitable organizations, fraternal, cultural, religious corporations or associations.
2.2. WHAT HAPPENS IF AN EMPLOYER REFUSES TO GET COVERAGE?
An employer who fails to secure workers’ compensation payments under
the Act, when required to do so, faces statutory criminal and civil penalties. See
Miss. Code Ann. §71-3-83 (1972, as amended). In addition, an employee injured
in the course and scope of his employment has the choice of either suing the
employer in tort or proceeding against the employer under the Act. See Miss.
Code Ann. §71-3-9 (1972, as amended). If suit is filed against the uninsured
employer, the employer may not plead as a defense that the injury was caused
by the negligence of a fellow servant, nor that the employee assumed the risk of
his employment, nor that the injury was due to the contributory negligence of
the employee.

Page 12 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2.3. INSURANCE COVERAGE
Employers may discharge their duty to provide workers’ compensation
coverage for their employees in several different ways. See Miss. Code Ann. §71-
3-75 (1972, as amended). The first method is by securing coverage with a third-
party insurer. According to the Act, once coverage is secured, the insurer’s
liability is coextensive with the employer’s, meaning that the insurer is obligated
to pay all workers’ compensation liability of the insured employer, despite any
limitations which the contract for insurance may contain which purports to limit
the insurer’s liability. See Miss. Code Ann. §71-3-77 (1972, as amended).
Nearly every insurance company utilizes the same basic workers’
compensation insurance policy form, and it is a policy form that has been in use
since the 1950’s with some revisions over the years. The National Council of
Compensation Insurance (NCCI) owns the copyright to the policy form. There
are endorsements to the policy form that can be used to modify or explain some
of the coverage details.
Details as to how to search for who has coverage for an employer on a
specific date of injury can be found at https://www.ewccv.com/cvs/.
2.3.a. STANDARD WORKERS’ COMPENSATION INSURANCE POLICY
The standard workers’ compensation policy form includes two coverage
parts. The first part of the policy requires the insurance company to pay on
behalf of its insured employer the workers’ compensation benefits owed by the
employer to its employees. Each policy has an “Information Page” that defines
the extent of the coverage by listing the States covered by the policy. The
workers’ compensation part of the policy does not have policy limits and requires
the carrier to pay the insured employer’s liability under the specified workers’
compensation law.

Page 13 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2.3.b. EMPLOYER’S LIABILITY INSURANCE COVERAGE
The second part of the policy form is an Employers’ Liability Insurance
Policy which was originally included in the policy form at a time when some kinds
of injuries, such as occupational diseases, were not covered by workers’
compensation systems. Because the law evolved over the years to include all
kinds of injuries and occupational diseases, this part of the policy form was
basically dormant and inactive in most jurisdictions for many years. With
increasing efforts to avoid the exclusive remedy doctrine (the thrust of which is
that workers’ compensation is intended to be the only remedy a claimant has
against his employer for a workplace injury—See Chapter 4 herein), the policy
has started being considered more frequently in recent years. It is written as a
more traditional kind of insurance policy with policy limits, exclusions, and other
specific provisions. In its simplest form, the policy imposes a contractual
obligation on an insurance carrier to indemnify and defend the insured employer
for those claims by employees against the employer for injuries arising out of
and occurring in the course of employment that are not covered by the workers’
compensation law. A careful coverage analysis will be required in the event a
claim is made which might fall under the terms of that policy.
2.3.c. CANCELLING AND NON-RENEWING COVERAGE
Cancellation and non-renewal of a workers’ compensation insurance policy
must be done in specific conformity with the law or the coverage could be
extended beyond the intent of the carrier. In an effort to provide a claimant with
a source to get his claim paid, coverage is going to be found to remain in effect
unless the carrier has precisely complied with the law regarding notice to the
insured and the Commission when cancelling or non-renewing the coverage. For
specific details, see Miss. Code Ann. §71-3-77 (1972, as amended) and MWCC
Rule 1.5.

Page 14 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2.4. SELF-INSURANCE AND GROUP SELF-INSURANCE
A company which wishes to be exempt from insuring its liability under the
Act may make application with the Mississippi Workers’ Compensation
Commission to be considered a “self-insurer.” The application must, among
other things, demonstrate the company’s financial ability to pay all compensation
required by the Act. The Act also provides for the pooling of liabilities by two or
more employers for the purpose of establishing a self-insured group. All
employers who wish to establish such a group must be comprised of members of
the same bona fide trade association or trade group, and all must be domiciled in
the State of Mississippi. See Miss. Code Ann. §71-3-75 (1972, as amended) and
Commission Rule 1.7.
2.5. ASSIGNED RISK COVERAGE
Finally, the Act provides for a “Mississippi Workers’ Compensation
Assigned Risk Plan” to be administered by the Mississippi Commissioner of
Insurance. See Miss. Code Ann. §71-3-111 (1972, as amended). These policies
are “for the assignment of risks which in good faith are entitled to insurance
under this chapter but which, because of unusual conditions and circumstances,
are unable to obtain such insurance.” In order to effectuate this provision, the
Commissioner of Insurance is authorized to advertise and contract with carriers
doing business in Mississippi to be servicing carriers for the Plan.
2.6. NOTICE OF COVERAGE
An employer is required to post a Notice of Coverage form on its premises
revealing details as to its coverage under Miss. Code Ann. §71-3-81 (1972, as
amended) and Commission Rule 1.8. Also, under Rule 1.3, each employer must
provide proof of its coverage to the Commission, but this reporting is handled
electronically. See additional provisions regarding these requirements on the
Page 16 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 3
JURISDICTION
3.1. MISSISSIPPI JURISDICTION
Most work-related accidents that fall within the Act are easy to identify as
such. The typical scenario involves a Mississippi resident working for a
Mississippi employer who has a work accident in Mississippi. Generally, coverage
exists if 1) the injury occurred in Mississippi, 2) the claimant was regularly
employed in Mississippi, or 3) the claimant was hired in Mississippi. The
Commission has exclusive jurisdiction over those cases covered by the Act. See
Miss. Code Ann. §71-3-47 (1972, as amended).
3.2. INJURIES OUTSIDE OF MISSISSIPPI
Questions arise, however, in situations where Mississippi workers are
injured outside of this State. For coverage to exist where an employee is injured
outside of Mississippi, the employee must have been hired or regularly employed
in Mississippi, and his work outside of the state must be temporary (generally
less than six months absent an election to extend coverage). In determining
coverage, the place of the claimant’s residence or domicile is not relevant.
Instead, the question is one of whether the work assignment outside the State is
temporary or permanent and not necessarily whether the worker’s departure
from the State was temporary or permanent. The Act does not apply if the work
assignment outside of the State is permanent (which includes work in a foreign
country.) See Miss. Code Ann. §71-3-109 (1972, as amended).
3.3. NON-RESIDENTS OF MISSISSIPPI INJURED IN MISSISSIPPI
When employees who were hired and/or regularly employed in another
state are injured in Mississippi while on a temporary job assignment, Mississippi

Page 17 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
law might not apply. However, in these situations, generally Mississippi law
applies unless all three of the following requirements are met: 1) the employer
has provided coverage under the laws of another state which cover the employee
for his work in Mississippi; 2) the other state recognizes the extraterritorial
provisions of the Act; and 3) the workers’ compensation law of the other state
must exempt Mississippi claimants and employers from its application. See Miss.
Code Ann. §71-3-109 (1972, as amended). The practical effect is that either
Mississippi law or the applicable law of the other State will cover a foreign worker
injured in Mississippi.
3.4. CONCURRENT JURISDICTION
One additional point to be made regarding jurisdictional issues relates to
successive awards: the Mississippi Workers’ Compensation Act does not bar a
claimant from filing a claim in Mississippi if benefits were awarded under the laws
of another State. The problem typically arises where an employee who was hired
and/or regularly employed in Mississippi is injured while on a temporary work
assignment in another state. It is possible that the employee would be covered
for that injury by the laws of the State in which he was injured. At the same
time, the claimant could also be entitled to coverage by the Mississippi Act. If
the employee is awarded benefits in the State where he was injured, he would
not be barred from filing a claim in Mississippi; however, the employer would be
entitled to credit for any award made in the foreign State against any liability
under the Mississippi Workers’ Compensation Law. (However, a denial of a claim
in the foreign jurisdiction will in some instances be construed to be res judicata
of the same issues if it is subsequently filed in Mississippi). Whether or not the
other involved State would have jurisdiction of the claim in addition to Mississippi
will depend entirely on the applicable provisions of the other State. The claims
professional should seek advice of counsel in the State where the other claim is
filed to fully evaluate those issues.

Page 18 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 4
EXCLUSIVE REMEDY
4.1. WHAT IS EXCLUSIVE REMEDY?
The Mississippi Workers’ Compensation Law is the exclusive or only remedy
available to a claimant for an injury arising out of and occurring in the course and
scope of employment. See Miss. Code Ann. §71-3-9 (1972, as amended). Stated
differently, the employer cannot be sued by an employee for a compensable
injury pursuant to common law for work related injuries based on a negligence
theory.
4.2. EXCEPTIONS TO THE EXCLUSIVE REMEDY DOCTRINE
There are exceptions to the rule that workers’ compensation is the only
remedy a claimant has against his employer. The first exception is where the
employer has not “secured payment of compensation”, which means that the
employer has failed to have a workers’ compensation insurance policy in effect or
failed to qualify as a self-insurer pursuant to procedures set forth in the Act. If
the employer does not have workers’ compensation coverage in effect, or is not a
qualified self-insurer, the employee is free to sue the employer outside the
confines of the workers’ compensation system and pursue remedies he has at
common law, and in that contingency, the employer loses certain defenses it
would otherwise have available. See Miss. Code Ann. §71-3-9 (1972, as
amended).
Another exception to the exclusive remedy rule involves claims for which
the Mississippi Workers’ Compensation Law does not provide a remedy. This is
best illustrated by the case of Miller v. McRae’s, 444 So.2d 368 (1984), in which
an employee was “falsely imprisoned” by a co-worker while in the course and
scope of employment. The co-employee detained the employee to question her
regarding a missing sum of money. The claimant filed a tort suit against the

Page 19 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
employer claiming that as a result of the false imprisonment, she suffered great
humiliation, loss of reputation, and physical illness. The Supreme Court held that
the exclusive remedy provisions in the Mississippi Workers’ Compensation Act did
not bar the employee’s false imprisonment claim since there was no “injury” as
defined by the Act for which a remedy would be available to the employee.
Still another area where the exclusive remedy provision does not apply is
where the employer intentionally injures the employee. In Franklin Furniture v.
Tedford, 18 So.3d 215 (Miss. 2009), the Mississippi Supreme Court held that
where acts committed by the employer are “substantially certain” to cause injury
to an employee, if there is actual intent to injure the employee, such actions fall
outside the exclusivity of the Act and the employee will be allowed to pursue
damages at common law.
As examined more fully in Chapter 17 herein, another type of claim that is
often discussed as an exception to the exclusive remedy doctrine is a claim in
tort by the employee against his employer, carrier, and others based on
allegations of “bad faith” claims handling. The details of issues involving those
claims are very important, and the claims professional is encouraged to read that
chapter closely.

Page 20 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 5
COMPENSABILITY
The premise of the Mississippi workers' compensation system is to provide
an injured employee a recovery for injuries that arise out of (referring to a causal
connection to the employment) and occur in the course of his employment
(involving an analysis of the time, place, and situation of the injury).
Compensability is established even if the employee caused or contributed to his
own injuries. Miss. Code Ann. §71-3-7. In exchange for imposing that liability on
an employer without determining who is at fault in causing the injury, the law
imposes a limit on the amount of money and type of benefits that can be
recovered by the injured employee. The system has survived constitutional
challenges over the years, but the fact that a claimant gives up an unlimited
recovery historically resulted in the workers' compensation system being liberally
interpreted in favor of the claimant. This means that disputed or doubtful cases
were resolved in favor of awarding compensation and the claimant was given the
benefit of the doubt in resolving issues or disputes. Legislative amendment in
2012 has potentially altered this historic interpretation as discussed below but
the trend toward resolving doubtful cases in favor of awarding benefits
continues.
Miss. Code Ann. §71-3-7 (1972, as amended) provides that a claim must
arise out of and occur in the course of employment and that medical causation
be established in order to receive compensation for an injury. Although both
tests must be met to establish compensability, practically the two are often
considered collectively so that compensability is found if “arising out of” is high
and “course of employment” is low, or vice versa. Some call such analysis the
“unitary test of work connection” or the “quantum theory of compensability.”
5.1. BURDEN OF PROOF
The claimant bears the burden of proving every element in his claim

Page 21 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
essential to a recovery, and that includes the fact of an injury that arose out of
and in the course of employment, that the medical problem in question is
causally related to the injury in question, and that claimant’s disability is
supported by medical findings. In meeting that burden, however, claimant has
traditionally been given the benefit of the doubt, and there is much case law
providing that “doubtful cases are to be resolved in favor of compensation” or
“the beneficent purposes of the Act” require a liberal interpretation of the
evidence in favor of claimant. The prior requirement that doubtful cases were to
be resolved in favor of compensability made it easier for a claimant to meet his
burden of proof with the burden then shifting to the employer/carrier to establish
that claimant’s story was inherently improbable of that the greater weight of the
evidence did not support claimant’s claim.
For injuries on or after July 1, 2012, the law is to be impartially construed
so as to favor neither the claimant nor employer/carrier, and the workers’
compensation laws are not to be liberally construed in order to fulfill any
beneficent purposes. That said, most workers’ compensation professionals
believe that close cases will probably result in awarding compensation even if
“liberal construction” is no longer mandated or mentioned in the MWCC Order.
5.2. INJURY DEFINED
The Act includes a definition of the term “injury” at Miss. Code Ann. §71-3-
3 (b) (1972, as amended). The complete definition is pasted below, and the
claims professional is encouraged to review the details when analyzing a
compensability issue. Some of the key phrases within the definition have been
bolded for emphasis and are further discussed in the following sections.
“Injury" means accidental injury or accidental death arising out of
and in the course of employment without regard to fault which
results from an untoward event or events, if contributed to or
aggravated or accelerated by the employment in a
significant manner. Untoward event includes events causing

Page 22 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
unexpected results. An untoward event or events shall not be
presumed to have arisen out of and in the course of
employment, except in the case of an employee found dead
in the course of employment. This definition includes injuries to
artificial members, and also includes an injury caused by the
willful act of a third person directed against an employee
because of his employment while so employed and working on
the job, and disability or death due to exposure to ionizing
radiation from any process in employment involving the use of or
direct contact with radium or radioactive substances with the use of
or direct exposure to roentgen (X-rays) or ionizing radiation. In
radiation cases only, the date of disablement shall be treated as
the date of the accident. Occupational diseases, or the
aggravation thereof, are excluded from the term "injury,"
provided that, except as otherwise specified, all provisions
of this chapter apply equally to occupational diseases as
well as injury.
PRACTICE NOTE: The determination of compensability requires a thorough
analysis of facts and the application of law to those facts. Although this guide
attempts to address many of the concepts encountered in this analysis, it does
not attempt to address every conceivable situation. The claims professional is
encouraged to not rely solely on this representative summary of decisions in
making decisions regarding compensability. These examples are intended to be
instructive in the analysis of whether a claim is compensable, but cases are
uniquely fact intensive, and every case must be considered on its own merits.
The claims professional is encouraged to seek advice of counsel to analyze
compensability before issuing a denial. As emphasized in this Guide, the reliance
upon the advice of counsel can shield the decision of the claims professional from
a punitive damage claim even if the claim decision is later claimed to have been
made in “bad faith.”
5.2.a. ARISING OUT OF AND IN THE COURSE OF EMPLOYMENT
Compensability analysis begins with a look at the issues of “arising out of
and in the course of employment”. In its simplest form, the “arising out of”

Page 23 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
requirement refers to the causal origin of the injury. The question focuses on
whether it is connected to the employment. Mississippi has adopted the
“positional risk test” in analyzing the issue which means that the injury would not
have occurred but for the fact that the employment placed a claimant in a
position where he was injured. As an example, in Wiggins v. Knox Glass, Inc.,
219 So. 2d 154 (Miss. 1969), the Court ruled that an injury from an act of nature
arises out of and in the course of employment so long as the worker is injured at
a place where he was required to be by the conditions of the employment.
The “course of employment” component of compensability generally refers
to the time, place and circumstances of the accident in relation to the
employment. If the claimant is generally doing his job at a time and place he is
supposed to be doing his job, the requirement is met.
Compensability is broadly construed and can still be found if there is a
sufficient work contribution present. As an example, there is no requirement that
the injury actually occur during work hours or on the employer’s premises. In
Mississippi Research and Development Center v. Dependents of Shults, 287 So.
2d 273 (Miss. 1973), the employee died in his kitchen at home, but
compensability was found on the premise that workplace stress had contributed
to a heart attack. Another illustration of the rule is one where the employee
manifested symptoms of a brain hemorrhage one evening at work and the acute
event actually did not occur until the next morning at home. Walker Mfg. Co. v.
Pickens, 206 So. 2d 639 (Miss. 1968).
Just because something occurs at work, however, does not make it
compensable. When the workplace is merely the place where the injury occurs,
it might not be compensable even though it occurs during the time of and at the
place of employment. It still has to arise from a risk incidental to the
employment. In Mathis v. Nelson’s Foodland, Inc., 606 So. 2d 101 (Miss. 1992),
the claimant was injured when he lit a firecracker at work but the injury was not
compensable because the lighting of the firecracker has no relationship to the
employment.
Page 24 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
PRACTICE NOTE: The “arising out of” and “in the course of” requirements
for compensability are captured in all workers’ compensation systems, but the
concepts have evolved uniquely in the different workers’ compensation systems,
and the conclusions reached on similar fact scenarios vary widely across the
United States. For that reason, a claims professional should not assume that a
fact scenario found compensable in one jurisdiction automatically translates to
the same conclusion in any other jurisdiction.
5.2.b. UNTOWARD EVENT
Note that the definition of “Injury” in section 5.2 above includes a
requirement for an “untoward event” as a part of the analysis of compensability.
Except in the case of a “Mental/Mental” injury discussed in section 5.5 of this
Guide, the significance of that phrase is hard to find in existing case law. An
incident can apparently meet the requirement of “untoward event” quite easily as
illustrated by the case of Beverly Healthcare v. Hare, 50 So.3
rd
1003 (Miss.
2011). That case involved an elderly employee with a significant history of pre-
existing problems with her leg (4 different identified injuries). She “pivoted” and
a bone in her leg snapped. Those facts were interpreted as representing a
compensable injury in spite of the significant pre-existing problems and
apparently minor work incident giving rise to the claim.
5.2.c. CONTRIBUTED TO, AGGRAVATED, OR ACCELERATED BY EMPLOYMENT
Compensability is found when the employment, or some component of
the employment, combines with pre-existing medical problems or congenital
defects to create disability. The employment need not be the sole cause of
problem, and it is sufficient to meet the definition of injury by showing that
the employment “contributes” to the disability, “aggravates” dormant or
active medical problems so as to create disability, or “accelerates”,
“exacerbates” or “lights up” an underlying medical problem so as to make it

Page 25 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
symptomatic. Cases abound finding an employment connection, and therefore
a compensable injury, when medical problems such as heart attacks, strokes,
hypertension, dermatological problems, cancer, arthritis, hemorrhoids,
pulmonary problems, and other conditions have been aggravated or
accelerated by the employment or injury.
In Quitman Knitting Mill v Smith, 540, So. 2d 623 (Miss. 1989) a
claimant purchased a cold tablet from her employer’s first aid station, and
that tablet was found to have contributed to the onset of the claimant’s
essential tremors. The Court reasoned that the employer benefited from
selling such items by lessening absenteeism as a part of the basis for finding
the claim compensable.
5.2.d. PRESUMPTION IN DEATH CASES
There is a presumption of compensability if a worker is found dead at a
time and place he was reasonably supposed to be during the performance of his
job. See e.g., Road Maintenance Supply, Inc. v. Dependents of Maxwell, 493 So.
2d 318 (Miss 1986).
The “found dead” presumption is contained within the definition of “injury”
in Chapter 5.2 above. It should be noted that the presumption is rebuttable and
after it has made its appearance, the employer/carrier have the burden of
proving that the claim is not compensable.
Also, where an employee falls dead in front of witnesses as opposed to
being “found dead” where no one witnessed the death, there is no presumption
of compensability. See In Re Dependents of Harbin, 958 So. 2d 1620 (Miss.
App., 2007).
5.2.e. WILLFUL ACT OF A THIRD PERSON/ASSAULTS
When a claimant is assaulted while on the job, compensability analysis
focuses on the one who committed the assault to the extent necessary to

Page 26 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
determine whether the assailant is connected to the employment, such as a co-
employee, or whether the assailant is a “third party” to the employment
relationship, such as a criminal.
If an assault causes injury between co-employees, it should be determined
whether the dispute between the co-employees that results in the injury is
rooted in personal, non-employment activity. If the assault is due to a personal
issue between the parties and not over an employment related issue, the injury
may not be compensable even if it happens on the job site. Sanderson Farms,
Inc. v. Jackson, 911 So. 2d 958 (Miss. Ct. App. 2005).
Conversely, if a claimant is injured from the intentional act of another
person who is a stranger to the employment relationship, compensability analysis
shifts to a determination as to whether there is a connection between the
employment and the assault. Stated differently, those injuries are compensable
only if the assault was committed “because of” the employment. Miss. Code
Ann. §71-3-3(b) (1972, as amended). For example, where an assault was
committed by a stranded motorist the claimant had stopped to help, the
“because of the employment” test was met because the employer benefitted by
having its employees attempt to provide “Good Samaritan” assistance to the
public. Big “2” Engine Rebuilders, v Freeman, 379 So. 2d 888 (Miss. 1980)
If the intentional assault has no connection to the employment, the claim
may not be found compensable. In Ellis v. Rose Oil Co. of Dixie, 190 So. 2d 450
(Miss. 1966), a claim involving a worker who was killed by his paramour’s
vengeful husband, the claim was not compensable since it was the worker’s
personal activity that created the risk of harm.
PRACTICE NOTE: If there is a work injury to an employee flowing from an
assault, the employer might be confronted with a suit under tort law such as
those causes of action discussed in Section 4.2 of this Guide. Such a claim might
require a focus on whether or not the loss is covered by the Employer’s Liability
Insurance Policy as mentioned in Section 2.3.b. of this Guide.

Page 27 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
5.2.f. OCCUPATIONAL DISEASES
Occupational diseases can be compensable and the analysis is usually
focused on the medical proof as to whether or not the job caused the alleged
occupational disease or contributed to the development of the disease/injury in a
significant manner. Cases have supported a finding of compensability involving
allegations of increased blood pressure, cardiac problems, strokes, and many
other medical problems. Cases are all unique and require a clear understanding
of the allegations, the job in question, and the medical opinions addressing
causation.
5.3. HERNIA CLAIMS
Hernia claims are treated specially under the Mississippi Workers’
Compensation Act with specific tests to prove compensability and limitations on
the amounts payable. See Miss Code Ann. 71-3-23 (1972, as amended). The
statute lists 5 requirements for a compensable hernia paraphrased as follows:
1. The hernia immediately follows sudden effort.
2. There was severe pain in the area of the hernia.
3. There had not been a descent or protrusion in that area before this
hernia.
4. That the problem was noticed immediately and reported to the
employer within a reasonable time.
5. That the problem was such to have required medical treatment within
five days after the injury.
These “requirements” have not always been strictly enforced and many
cases have found compensability despite one or more of the statutory elements
being unfulfilled. In Lindsey v. Ingalls Shipbuilding Corp., 219 Miss 437, 442
(1954), the claimant clearly did not have treatment within five days, but the

Page 28 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
court said that the “statute does not require that the claimant prove that he was
actually attended by a physician or surgeon within five days after the injury. The
statute only requires that the claimant prove that the physical distress following
the descent of the hernia was such as to require the attendance of a physician or
surgeon within five days.” Id.
It is also noteworthy that the statute provides that a post-operative hernia
is considered an “original” hernia. That means that a hernia that occurs in the
same area, which was earlier repaired surgically, will still be compensable if the
five requirements are otherwise met.
PRACTICE NOTE: There is a statutory limitation on the number of weeks
an employer must pay compensation benefits related to a hernia. The benefits
for temporary total disability cannot exceed twenty-six (26) weeks when the
claimant has surgery to repair the hernia but only thirteen (13) weeks when he
or she undergoes conservative treatment instead of surgery.
5.4. GOING TO AND COMING FROM WORK
Generally, an injury that occurs while the employee is travelling to and
from work is not compensable. King v. Norrell Services, Inc., 820 So.2d 692
(Miss. Ct. App. 2000); Miller Transporters, Inc. v. Seay’s Dependents, 350 So.2d
689 (Miss. 1977). There are important exceptions to that generality, however,
many of which are tied to unique circumstances of the work in question.
Examples of such exceptions include: (1) where the employer furnishes the
means of transportation, or remunerates the employee for the travel; (2) where
the employee performs some duty in connection with his employment at home;
(3) where the employee is injured by some hazard or danger which is inherent in
the conditions along the route necessarily used by the employee; (4) where the
employer furnishes a hazardous route (5) where the injury results from a
hazardous parking lot furnished by the employer; (6) where the place of injury,
although owned by one other than the employer, is in such close proximity to the

Page 29 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
premises owned by the employer as to be, in effect, a part of such premises; or
(7) when the employee is on a special mission or errand for his employer, or
where the employee is accommodating his employer in an emergency situation.
PRACTICE NOTE: Claim denials based on the “going to and coming from”
work general rule against compensability should almost always be supported by
legal advice of counsel that none of the “exceptions” apply.
5.5. MENTAL INJURIES
When mental stress leads to mental injury without a physical injury, the
claim could be compensable, but the claimant has a heightened burden of proof.
For a “mental-mental” injury to be compensable, the claimant bears the burden
of proving, by clear and convincing evidence, that the mental injury resulted
from “more than the ordinary incidents of employment” and that there was an
“untoward event or unusual occurrence” that contributed to the mental or
emotional injury. The claimant’s burden of proof is greater than that
encountered in proving compensability in a physical injury situation, and all of
the cases are factually intensive.
Illustrations of cases found compensable for a mental-mental injury are
Brown & Root Construction v. Duckworth, 475 So. 2d 813 (Miss. 1985)
(psychological symptoms resembling a stroke after not getting a promised
promotion); Borden, Inc v. Eskridge, 604 So. 2d 1071 (Miss. 1991) (work
harassment and demotions caused depression); Mid-Delta Home Health, Inc v.
Robertson, 749 So. 2d 379 (Miss. App. 1999) (TTD awarded due to emotional
disorder stemming from being overworked and harassed); Kemper National
Insurance Co. v. Coleman, 812 So.2d 1119 (Miss. App. 2002) (a workers’
compensation adjuster was treated for depression as the result being passed
over for a promotion and being harassed by his supervisor).
Illustrations of cases found non-compensable for a mental-mental injury
are Smith and Sanders, Inc. v. Peery, 473 So. 2d 423 (Miss. 1985) (claimant

Page 30 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
experienced a psychological problem after being laid off due to a decline in
business); Smith v. City of Jackson, 792 So. 2d 335 (Miss. App. 2001) (claimant
had anxiety [a “nervous breakdown”] due to overwork; Radford v. CCA-Delta
Correctional Facility, 5 So. 3d 1158 (Miss. App. 2009) (claimant had depression
and post-traumatic stress disorder after being reassigned to another supervisor).
PRACTICE NOTE: All of the reported decisions illustrate a fact intensive
analysis, and no conclusions as to compensability or non-compensability should
be drawn from a scenario such as “overwork means it is compensable or not
compensable.” Most cases involving an individual who had been treated for pre-
existing psychological problems were ultimately denied, but that does not mean
that all of those cases are automatically denied. The claims professional should
thoroughly investigate every claim of this nature and would be well served to
seek advice of counsel in developing the correct position to take on each matter.
When an employee has emotional stress from work activity that leads to an
ailment with physical manifestations, the physical injury could be compensable.
Berry v. Universal Mfg. Co., 597 So. 2d 623 (Miss. 1992) was a compensable
claim where job stress contributed to hypertension.
Sometimes a mental injury causes another physical injury. In
Weyerhaeuser Co. v. Ratliff, 197 So. 2d 231 (Miss. 1967), a worker lacerated
three fingers in a work-connected injury and had stress and anxiety over the
finger injury which aggravated a chronic duodenal ulcer requiring surgery. An
award of benefits related to the surgery to repair the ulcer was approved.
Also, mental injury stemming from the physical injury (e.g. pain related
depression or Post Traumatic Stress Disorder from an accident) are not subject
to the heightened burden that applies to pure mental injuries. This is also true
for physical injuries that manifest from mental ailments.
5.6. CUMULATIVE AND REPETITIVE INJURIES
A compensable claim does not have to be tied to a single incident. A

Page 31 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
compensable disability can flow from a series of events or repetitive motion, the
cumulative effect of which can qualify as a compensable injury. Carpal tunnel
claims are illustrative of this rule of law. Compensable results have also been
found in other kinds of cumulative injury claims such as spine ailments caused or
aggravated by the work activity. See, e.g. Smith v. Masonite Corp., 48 So.3d
656 (Miss. Ct. App. 2010).
PRACTICE NOTE: Compensability of cumulative or repetitive injury claims
is heavily dependent upon medical opinions from the providers as to how the
work did or did not contribute to the injury.
5.7. LAST INJURIOUS EXPOSURE
Mississippi has adopted the “last injurious exposure” rule that is applicable
in cases where the exposure occurs over an extended period of time. In its
simplest form, that rule is that if a claimant has a series of employers (or
different carriers for the same employer) and the work activities ultimately cause
the claimant to be disabled, the last employer (or carrier) in that series of events
is responsible for the entire claim. See Thyer Mfg. Co. v. Mooney, 173 So. 2d
652 (Miss. 1965) (claimant worked for a manufacturer through three successive
carriers, and the last carrier was the one that bore the responsibility for the
claim).
Cases of this nature are always factually intensive, however, and the
claims professional is encouraged to thoroughly investigate the facts, analyze the
medical opinions, and seek advice of counsel if the correct response to the claim
is not apparent.
5.8. MULTIPLE CARRIERS IN COMPENSABILITY DISPUTE
Sometimes, in the cases involving a cumulative impact or repetitive motion
injury, progressive occupational disease, or multiple consecutive injuries, it is not
readily apparent which of the various employers and/or carriers might ultimately

Page 32 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
be responsible for a claimant’s injuries and medical treatment. Miss. Code Ann.
§71-3-37(13) (1972, as amended) provides a solution so that the claimant is not
left without treatment and benefits while the process for determining
responsibility evolves. The Commission can order the disputing parties to
provide the benefits equally until it is determined which party is solely liable, and
at that determination, the liable employer/carrier must reimburse the non-liable
employer/carrier for the benefits paid by the non-liable employer/carrier, with
interest.
PRACTICE NOTE: If confronted with this situation, the parties are
encouraged to get an Order from the Commission as contemplated by the
referenced code section. A volunteer who makes a payment that it doesn’t owe
might not have a remedy to recover payments which are ultimately not found to
be its responsibility unless the payments are done pursuant to the statute.
5.9. IDIOPATHIC FALLS
Sometimes the claimant is suffering from a medical condition that is not
caused by the job but the medical condition causes claimant to fall at work and
sustain other injuries. For example, if a claimant with epilepsy suffers a seizure
and is injured in a fall, the employer/carrier would not owe benefits for the
treatment of the epilepsy, but would owe benefits for the injuries caused by
striking the employer’s floor, or table or equipment. In Chapman, Dependents of
v. Hanson Scale Co., 495 So. 2d 1357 (Miss. 1986), the Mississippi Supreme
Court said:
We consider exposure to falls upon a concrete floor a sufficient risk
attendant upon employment so that an injury caused in part thereby
is compensable. Larry Ray Chapman, while at his usual place of
work, fell and struck his head upon just such a floor and as a result
died. His death arose out of and within the course and scope of his
employment.

Page 33 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 6
DEFENSES TO CLAIMS
6.1. EMPLOYEE STATUS
It is important to remember that only claims by employees of the employer
are payable. Often times questions center on whether or not someone is an
employee as opposed to a volunteer or an independent contractor.
In its simplest form, an employee is a person under a contract of hire,
expressed or implied. An independent contractor, on the other hand, is not an
employee who is entitled to benefits. The individual might be doing work for or
on behalf of the employer, but that alone is not enough to make that person an
employee. A variety of things are analyzed to determine whether a person is an
independent contractor as opposed to an employee, and among those things are
whether or not the employer has the right to control the work activities of the
person in question. Remember that the right to control is not the same thing as
actually exercising that control, however. Generally speaking, if an employer
specifies the time that an individual comes to work, when they leave, how the
work is supposed to be done, provides the tools necessary to do the job, etc., the
person will be considered an employee.
Sometimes the right of control question is not very clear and the Court
has, in those circumstances, then looked at whether or not the work being
performed is an integral part of the employer’s business enterprise. When
analyzing the nature of the work in question to address this issue, an
employee/employer relationship is found when the work performed is an integral
part of the employer’s business. As an example, trucking companies will
sometimes enter into a contract with a truck driver and that contract could
actually call the driver an “independent contractor”. However, in analyzing the
relative nature of the work test, the Court might find that trucking companies are
hired to deliver products in a truck from Point A to Point B and the only way they

Page 34 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
can do that is by having truck drivers. As a consequence, the truck driving
activity is an integral part of the trucking business’ operations, and the injured
worker driving the truck is therefore an employee. Conversely, however, if there
is a refrigerator in the office of a trucking company that breaks and someone is
called to the office to fix that refrigerator, that person is likely not doing
something that is an integral part of the employer’s business operation.
Accordingly, he will probably not be considered an employee for workers’
compensation purposes.
A “volunteer” is a person who is not hired to do the work of the employer
but just shows up and starts working. Under those circumstances he will
probably not be considered an employee, but the analysis is usually fact
intensive. That concept should not to be confused with a volunteer fireman, as an
example, because a volunteer fireman is actually doing the activities of the
employer entity as specifically agreed by the parties and he would therefore be
an employee.
A “statutory employee” is a concept generally tied to the issue involving an
employee of an uninsured subcontractor. As a simple illustration, if the employer
contracts to build a house and he then subcontracts to a roofing contractor to put
on the roof of that house, and one of the employees of that roofing subcontractor
is injured, the injured employee will have a claim against his subcontracting
employer, but if his employer does not have workers’ compensation insurance
coverage, he would also have a viable claim against the general contractor as the
general contractor’s “statutory employee”.
6.1.a UNDOCUMENTED WORKERS/ALIENS
Undocumented workers, or those who are not citizens of the United States
or who do not have legal documentation permitting them to be in the United
States, can be employees for workers’ compensation purposes. The Mississippi
Workers’ Compensation Law makes no special provisions regarding “aliens” other

Page 35 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
than to say that if they have an injury and return to their home country, any
permanent disability benefits due can be paid in a lump sum rather than bi-
weekly. Miss. Code Ann §71-3-27 (1972, as amended). (As stated in Chapter
10.3.a, herein, that code section also limits the death beneficiaries entitled to
benefits in claims involving undocumented workers.)
6.2. PRE-EXISITING CONDITIONS
It is important to remember that the aggravation of a pre-existing
condition is still a compensable injury. Cases have variously described the issue
as one involving the aggravation, exacerbation, acceleration, or lighting up of the
pre-existing condition. All of that together or singularly can constitute a
compensable injury if the pre-existing condition was aggravated in a significant
manner. Stated differently, the employment or work injury does not have to be
the sole cause of a medical problem in order for it to be compensable.
Where there is a pre-existing condition, however, two possibilities can be
considered in limiting the indemnity benefits payable, the second Injury Fund
and Apportionment, both of which are discussed below. Neither has any effect
on medical benefits.
6.2.a. SECOND INJURY FUND
Mississippi has a very limited Second Injury Fund that is rarely applicable.
One of the definitions of permanent total disability is dismemberment or loss of
use of both arms, legs, hands, feet, eyes or any combination of those five
scheduled members. To illustrate, the loss of a hand and an eye is permanent
and total disability.
If, at the time of the accident in question, the claimant had already lost
one of those scheduled members and in the accident in question loses another of
those scheduled members, the claimant is permanently and totally disabled. The
Mississippi Workers’ Compensation Commission’s Second Injury Fund is

Page 36 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
applicable in those very limited circumstances. In such a case, the
employer/carrier must pay claimant’s temporary total disability benefits related
to the injury in question and the permanent partial disability benefits for the loss
of the scheduled member lost in the compensable accident; the Commission’s
Second Injury Fund will pay the balance of indemnity benefits for permanent
total disability. To illustrate, if the injury involves the loss of use of an arm and
the injury in question involves twenty weeks of temporary total, the
employer/carrier would pay twenty weeks of temporary total, two hundred weeks
for loss of the arm, and the Commission Second Injury Fund would pay the
remaining two hundred thirty weeks so that the claimant recovers the full four
hundred fifty week benefit for permanent total disability.
The Second Injury Fund has no application in any other circumstances
such as a back injury or other “body as a whole” cases.
6.2.b. APPORTIONMENT
Where the claimant is suffering from a pre-existing condition that is a
material contributing factor to his permanent disability or death, then permanent
disability or death benefits may be reduced by the proportion to which the pre-
existing condition contributes to the disability or death. The burden of proof for
apportionment is on the employer/carrier and case law requires that the
employer/carrier prove that, from a medical standpoint, the pre-existing
condition is a material contributing factor to the disability. The pre-existing
condition does not have to be occupationally disabling for apportionment to
apply. To receive an apportionment of benefits, the injury must involve the
same part of the body.
The amount of apportionment or reduction of an award due to the pre-
existing condition is not limited to the medical estimate regarding the degree of
contribution. In other words, the Administrative Judge, after considering all the
testimony, could apportion (or reduce) the award by more or less than the fifty
Page 37 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
percent medical estimate.
6.3. STATUTE OF LIMITATIONS
There are two separate and distinct statutes of limitations with which to be
concerned. The first applies where compensation benefits have not been paid
and the second applies where compensation benefits have been paid.
6.3.a. WHERE NO INDEMNITY BENEFITS ARE PAID
In those cases where no indemnity or compensation benefits are paid to a
claimant, there is a two-year statute of limitations beginning on the date of
injury. Miss. Code Ann §71-3-35 (1972, as amended). Once the statute of
limitations has run, the claim for both indemnity and medical benefits is barred.
Speed Mechanical, Inc. v Taylor, 342 So. 2d 317 (Miss. 1977).
The claimant can toll or stop the running of the statute of limitations by
filing a Petition to Controvert. Also, if indemnity benefits are paid or if the
employer pays salary in lieu of compensation benefits, the statute of limitations
is no longer applicable.
There are some cases indicating that if the claim is a “lost time” claim but
the employer/carrier never filed the First Report of Injury with the Commission,
the statute of limitations does not begin to run.
There can be issues involving a latent injury or one in which the effects of
the injury do not show up until a later time. These cases are always factually
intensive, but in general terms, the statute of limitations begins to run on the
date that the claimant, as a reasonable person, recognizes the nature,
seriousness and probable compensable character of his injury or illness.
6.3.b. WHERE INDEMNITY BENEFITS ARE PAID

Page 38 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
If compensation benefits are paid, the two-year statute of limitations is not
applicable. In those cases where compensation or indemnity benefits are paid, a
claimant has one year from the date that Commission Form B-31, Notice of Final
Payment, is properly filed with the Mississippi Workers’ Compensation
Commission. The one-year statute of limitations is technically a jurisdictional
issue taken from the combined reading of Miss. Code Ann §§71-3-37(7), 71-3-53
(1972, as amended), and Commission Rule 2.17. A combined analysis of those
sections indicates that the Commission loses jurisdiction of the case one year
after the proper filing of a B-31, and if the Commission loses jurisdiction of a
case, no one has jurisdiction over the claim since workers’ compensation issues
are exclusively reserved for determination by the Commission. The net result is
still a one-year limitation after the filing of a B-31.
A change to MWCC Rule 2.17 effective January 18, 2018, is significant as it
relates to the B-31. Under the new rule, filing the B-31 starts the running of the
one-year limitation provided notice of the filing is given to Claimant or Claimant’s
attorney. Notice may be given by any means which acknowledges delivery of the
B-31. Claimant’s signature is no longer required on the form, but if Claimant
does sign it, that signature constitutes an acknowledged delivery of the B-31 to
Claimant.
If additional benefits are paid or treatment authorized after the filing of
form B-31, the running of the one-year statute of limitations is tolled (or
stopped), and an amended B-31 showing the new payment totals is required.
The same notice of the filing as outlined above must be followed when filing the
amended form B-31.
Sometimes, after the B-31 has been filed, additional medical bills will be
paid that concern treatment rendered before the date of the B-31 filing, and
arguably, payments for those items would not toll the statute requiring a new
form B-31 to be filed.
6.4. INTERVENING CAUSE OF DISABILITY

Page 39 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
The employer/carrier are responsible for compensation and medical
benefits that are related to the claim in question. Sometimes an issue will arise
which challenges whether or not the current medical problem, treatment and/or
disability is related to the accident in question as opposed to an intervening
cause. As with all affirmative defenses, the employer/carrier bear the burden of
proving that the continuing disability and medical treatment should not be their
responsibility.
There is a presumption under the law that disability, once it is shown to
exist, continues to be causally related to the accident. The presumption is not
that the disability in fact continues, but if it does continue, the presumption is in
favor of a continued causal connection.
The burden is on the employer/carrier to prove that the effects of the
original injury have subsided and that disability is now only the result of the new
or intervening accident. Medart Division of Jackes-Evans Manufacturing
Company, Inc. v. Adams, 344 So.2d 141 (Miss. 1977). It is not enough that the
new incident or medical problem simply combines with the original injury to
create disability. Rathborne, Hair & Ridgeway Box Company v. Green, 115
So.2d 674 (Miss. 1959).
6.5. INTOXICATION
Miss. Code Ann. §71-3-7 (1972, as amended) provides as follows: “No
compensation shall be payable if the intoxication of the employee was the
proximate cause of the injury….” That simple statement has struggled for
viability as a defense under Mississippi law over the years. In 2012, Mississippi
law was amended in such a way that the intoxication defense has a new life,
although it has yet to be thoroughly vetted. For injuries on or after July 1, 2012,
the intoxication defense was revised with changes to Miss. Code Ann §71-3-7,
Miss. Code Ann. §71-3-121, and Miss. Code Ann. §71-7-5 (1972, as amended).
The changes are intended to make the defense work in such a way that the

Page 40 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
burden of proof is passed to the claimant when alcohol, improperly used
prescription drugs, or illegal drugs are involved in a claim. The basic provisions
include the following:
• No compensation will be payable if the use of alcohol, illegal drugs, or a
prescription drug taken inconsistent with the prescribing physician’s
instructions is the proximate cause of the injury.
• The Employer has the right to request that a claimant undergo a drug or
alcohol test following an on-the-job injury.
• A rebuttable presumption is created that the use of alcohol/drugs was the
proximate cause of the injury in the event of a positive test for:
o A blood alcohol content of .08% or greater;
o An illegally used drug; or
o A prescription drug taken contrary to the prescribing physician’s
orders.
• If the Claimant refuses the drug test, it is presumed that one of the above
three reasons was the proximate cause of the injury.
• Once the presumption arises, it is the claimant’s burden to prove that the
alcohol or illegal/improperly taken drug was not a contributing cause of the
accident.
• Other provisions permit the results of the alcohol/drug tests to be
admissible into evidence; provide the employer with protection against a
cause of action for defamation, libel, slander when relying on the defense;
and confirm the right of the employer to administer a drug/alcohol test
whenever an on-the-job injury is claimed.
PRACTICE POINT: Although an employer might have a policy stating that an
employee who either tests positive for a controlled substance or refuses to take
the test can be terminated, those policies have no impact on the applicability of
the intoxication defense in the workers’ compensation setting. In other words,
although an employee can be fired for a positive drug test, that fact alone does
not provide grounds for denial of the workers’ compensation claim. Proof as

Page 41 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
outlined above must be provided.
PRACTICE POINT: Much is being said and written arguing that these provisions
might not sustain a constitutional challenge, and it will take some time for cases
to make it through the litigation process to see how the defense is interpreted by
the judiciary. The claims professional will be well served to seek advice of
counsel in dealing with cases involving the defense. Remember that the
presumption in favor of the defense is rebuttable, and in those cases where the
facts of the accident clearly indicate that the intoxication was not the cause of
the accident, the intoxication presumption can be rebutted. Some practitioners
believe that denying a claim based only on that positive test without proper
analysis of the facts of the accident will possibly lead to a suit alleging a “bad
faith” denial of a claim as more fully discussed in Chapter 17.
6.6. WILLFUL INTENT TO INJURE SELF OR OTHERS
Another statutory defense to claims concerns injuries intentionally caused
by the claimant where he is trying to injure himself or someone else. Miss. Code
Ann. §71-3-7 (1972, as amended). The cases involving the potential defense are
always factually intensive and there is no presumption in favor of the defense in
any circumstances. As an example, cases involving horseplay have generally
been held compensable on the reasoning that employees working together will
sometimes engage in frivolity and sometimes someone gets hurt; when that
happens, it is just a risk assumed by the employer. Mutual Implement and
Hardware Ins. Co. v. Pittman, 59 So. 2d 547 (Miss. 1952). Clearly, however, the
horseplay could involve such an abandonment of the job to challenge
compensability on the argument that claimant deviated from the employment.
Mathis v. Nelson’s Foodland, Inc., 606 So. 2d 101 (Miss. 1992).
Cases involving co-employee altercations have become increasingly difficult
to analyze in recent years. A long line of older cases can be cited that found
compensability on the “risk assumed by the employer” argument similar to that
found in the horseplay cases. However, the more recent approach has been to

Page 42 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
challenge a finding of compensability where the reason for the co-employee
altercation is personal to the employees rather than something related to the
employment. In other words, if they are fighting over a personal loan one made
to the other, the injury might not be compensable. Sanderson Farms, Inc. v.
Jackson, 911 So. 2d 958 (Miss. App. 2005).
The defense is tied to the concept that one who intentionally tries to hurt
himself just to collect workers’ compensation benefits should not be entitled to
recover. That premise has its limits, however, as illustrated by a case where a
claimant had a compensable back injury, developed significant pain issues, and
ultimately committed suicide from an inability to deal with the pain. Even though
the suicide was an “intentional” event, the claim was still held compensable due
to the unique circumstances presented. Printer’s Truck and Tractor Co. v.
Spencer, 87 So. 2d 272 (Miss. 1956).

Page 43 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 7
COMMISSION FORMS
There are three groups of forms utilized by the Commission broken down
into the “A” forms, “B” forms and “R” forms.
All MWCC forms are available at http://www.mwcc.state.ms.us/#/forms.
7.1. ADDRESS FOR FORM FILING
The mailing address for filing forms is:
The Mississippi Workers’ Compensation Commission
PO Box 5300
Jackson, MS 39296-5300
For information regarding electronic filing, go to
http://www.mwcc.state.ms.us/#/electronicDataInterchange.
It should be noted that Miss. Code Ann. §71-3-67 (1972, as amended),
gives the Commission authority to assess a fine of $100 for the failure to timely
file any form required by the Commission. A $100 penalty can also be added to
an award to the claimant for failure to file a required report. The Commission has
issued a Memorandum regarding the filing of forms and penalties. See the form
at http://www.mwcc.state.ms.us/pdf/monitoringofreports.pdf.
7.2. “A” FORMS
7.2.a. A-16 Notice of Coverage
The first official form of the Commission was originally called the A-16,
"Notice of Coverage." The notice was to be posted in a conspicuous place by the
employer so employees would know who to contact in the event of an on-the-job
injury. The amended version of the rule regarding the form permits employers
to design their own form for these purposes so long as the form includes all of
the information originally included in the A-16 form. See MWCC Rule 1.8.

Page 44 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2012 Amendment Regarding Notice—One of the provisions in the 2012
legislation requires Employer to post near their Notice of Coverage form a Notice
prepared by the Commission detailing the 2012 Amendments. A copy of that
notice to be posted is available at http://www.mwcc.state.ms.us/pdf/sb2576.pdf.
7.2.b. A-24 Proof of Coverage
Every employer subject to the Mississippi Workers’ Compensation Law
must file proof of compliance with the insurance provisions of the law consistent
with MWCC Rule 1.3. The A-24 form is therefore used only by self-insured
employers and self-insured groups that do not report to NCCI.
7.3 "B" FORMS
7.3.a. B-3 (IAIABC IA-1), First Report of Injury (FROI)
A standardized form designed by the International Association of Industrial
Accident Boards and Commissions is the First Report of Injury form, the B-3. It
is entitled "WORKERS COMPENSATION - FIRST REPORT OF INJURY OR ILLNESS."
Note that the back of the form has some specific instructions on the completion
of the form. See also MWCC Rule 2.1.
Employers should complete and file a first report of injury (FROI) with their
carrier or third-party administrator immediately upon receiving notice of an
injury, if the injury requires a loss of more than the shift on which the injury
occurs. If the injury causes lost time in excess of five days, or if the injury
results in permanent impairment, the carrier or third-party administrator must
file the form with the Mississippi Workers' Compensation Commission. The
Commission will return a file number to be used for any future filings related to
the claim. The statute contemplates such filing within ten days of the employer's
notice of the injury or notice that the injury has resulted in lost time in excess of
the waiting period or permanent impairment. See Miss. Code Ann. §71-3-67
(1972, as amended) and MWCC Rule 2.1.

Page 45 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
As of this printing, the Commission is accepting the FROI’s electronically
with the intent that eventually all FROI’s, and eventually other forms, will be filed
electronically. Details relating to the Electronic Data Interface (EDI)
requirements, deadlines, and procedures are available on the Commission web
site at http://www.mwcc.state.ms.us/#/electronicDataInterchange.
PRACTICE POINT: The failure to file a First Report of Injury has resulted in
court decisions refusing to apply the two-year statute of limitation on a claim and
has served as the basis for an employer to become a defendant in bad faith
litigation.
7.3.b. B-18, Notice of Payment
Once payments are initiated, the Commission is notified of that
development by the use of form B-18. Likewise, when benefits are stopped,
restarted, converted to permanent disability benefits, or otherwise changed, the
B-18 is the notice form used. Note that it does not have to be signed by the
claimant, but the claimant should be given a copy of any such filing.
PRACTICE POINT: The filing of a B-18 by the employer/carrier indicates to
the Commission that the employer/carrier are willing to pay the benefits specified
on the form. It is in effect an “admission of liability” for the specified benefits. If
the agreement to pay stated on the B-18 relates to the payment of permanent
disability or death benefits, the claimant can apply to the Commission to allow
those benefits to be paid in a lump sum. See B-19 below and Chapter 14
relating to Lump Sum Payments.
7.3.c. B-19, Application for Lump Sum Payment
Recall that benefits are to be paid bi-weekly unless otherwise ordered by
the Commission, and this is the form filed by a claimant to obtain authority to
get paid for permanent disability or death benefits in a full or partial lump sum.
See Chapter 14 for further discussion as to Lump Sum Payments.

Page 46 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
7.3.d. B-9, 27, Medical Report
The Commission has replaced all previous medical report forms (B-9, B-27,
and B-27-D) with a new form numbered B-9, 27. Commission Rule 1.9 allows
medical providers to provide copies of their office notes along with the CMS-1500
medical report forms used for health insurance purposes in lieu of these
Commission forms. All medical information relating to a claim is to be filed with
the Commission on all cases where the First Report of Injury is filed with the
Commission. Medical records filed with MWCC must contain the MWCC file # on
them or they will be returned by the Commission. A medical provider is required
to submit reports regarding treatment to the employer/carrier (and not directly
to the Commission) before being entitled to payment and should do so within
twenty days of the first treatment and periodically thereafter.
7.3.e. B-31, Notice of Final Payment
One of the most important forms to use and understand is the B-31,
"Notice of Final Payment." It is often a source of frustration for the Claims
Professional, but is one of the most important forms that the Claims Professional
uses in properly handling Mississippi Workers’ Compensation claims. This form,
when filed properly, starts the one-year statute of limitations on cases where
indemnity benefits are paid. If the form is not filed properly, the case in question
may never have a statute of limitations defense and will remain open indefinitely.
Stated differently, the function of this form is to provide the notice required by
Miss. Code Ann §71-3-37(7) before the claimant’s rights to benefits can be
terminated.
Since the proper filing of a B-31 terminates a claimant’s rights to benefits,
Court interpretations relating to its use have mandated that the procedures be
followed precisely. Hale v. General Box Mfg. Co., 228 Miss. 394 (1956).
Commission Rule 2.17 has been amended effective January 18, 2018, and

Page 47 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
arguably the process to now be followed is significantly streamlined. Under the
revised rule, the form no longer has to be signed by the Claimant, but Claimant
or Claimant’s attorney must be given notice of the filing by any means which
acknowledges delivery of the B-31. The Rule also provides that if the B-31 is
signed by the Claimant, that signature will constitute acknowledged delivery of
the B-31.
If additional benefits are paid or treatment is authorized after the filing of a
B-31, the running of the one-year statute of limitations is tolled (or stopped),
and a corrected B-31 showing the new amounts of payments is required. Notice
of the filing requirements should also be followed for the revised B-31.
Sometimes additional bills will be presented for payment for treatment that
was rendered before the date of the B-31 filing, and arguably, payments for
those items would not toll the statute requiring a new B-31 to be filed.
PRACTICE POINT: In completing the B-31, care should be taken to clearly
explain payments made. Although a full week of disability (5, 6, or 7 consecutive
days) results in the payment of the weekly maximum amount, scattered or non-
consecutive days of disability where 6 or 7 days in total are paid at the daily rate
will yield a higher total amount due. That should be reflected and explained on
the B-31. See Section 8.3 for further information regarding the calculation of
those benefits.
PRACTICE POINT: When the B-31 is filed, the Commission usually sends to
the claimant a notice in a form letter designated the C-1. That letter contains
information regarding the legal effect of the B-31 filing similar to what is
discussed in this Guide.
PRACTICE POINT: The new Rule contemplates that is it acceptable to notify
a Claimant of the filing of a B-31 by e-mail if the e-mail system generates a
“notice of delivery”. The pragmatic approach suggests that e-mail for these
purposes only be used if e-mail has been a successful method of communication
with the Claimant up to that point. The intent is to be able to prove that
Claimant was notified of the filing of the B-31. If e-mail is not a viable option,

Page 48 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
sending notice of the filing of the B-31 by any other means that generates a
receipt permits the use of resources such as FedEx or UPS or any other resource
that might be less expensive than the previously mandated use of “certified mail,
return receipt requested”.
7.3.f. B-52, Employers’ Notice of Controversion
Commission form B-52, Employer’s Notice of Controversion, is filed to give
notice to the Commission of a controversy on a particular case, and a copy
should also be sent to the claimant when it is filed. See MWCC Rule 2.2. It does
not initiate litigation but is simply notice to the Commission and the claimant that
there is an issue which is either under review or that the claim has been denied.
Filing a B-52 within fourteen days of the employer’s notice of an injury will avoid
the imposition of the 10% penalty for the untimely payment of compensation
benefits that may later be awarded.
PRACTICE POINT: Care should be used in completing this form to
accurately state the issue and explain the basis for the Controversion. The
claims professional should not state that the claim is denied unless a full
investigation has been completed and the decision to deny the claim has been
through appropriate internal protocols. Consider instead a statement such as:
“The employer/carrier controverts the right to benefits at this time as the
investigation is continuing and not yet complete; this is not a denial of the
claim.” Another possibility is to precisely state the reason benefits are not being
paid such as: “The employer/carrier have not received any medical information in
support of disability” or “The employer/carrier have not received any medical
information confirming that the claimant’s alleged disability is causally related to
the job”.

Page 49 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
7.3.g. B-5, 11 and B-5, 22, Petition to Controvert and Answer
These two forms are used in connection with litigated cases. The
claimant's "Petition to Controvert," form B-5, 11, is used by a claimant to
formally make a claim for benefits and seek a hearing on his claim. See MWCC
Rule 2.2. The employer's "Answer" to that Petition to Controvert is the B-5, 22.
See MWCC Rule 2.4. Once the Commission receives a claimant's Petition to
Controvert, the Commission will send a letter to the employer/carrier informing
them of that filing; the employer/carrier's Answer to the Petition is due twenty-
three days from the date of the Commission's letter. Except in a situation where
an employer is representing himself, a licensed Mississippi attorney must file the
Answer. See Miss Code Ann. § 71-3-63 (1972, as amended). Failure to timely
file an Answer could result in a default, loss of affirmative defenses, and impair
the ability to successfully defend the claim.
7.4. R FORMS
7.4.a. R-1, Early Notification of Severe Injury
The Commission wants to be notified immediately of a severe injury such as
a head injury, paralysis injury, or severe burn injury, and they have designated
the R-1 as the form to be filed along with a FROI to complete that notice.
7.4.b. R-2, Referral for Rehabilitation and Initial Report
The R-2 is a form used by the Commission to refer a claimant to the
Vocational Rehabilitation Division of the Mississippi Department of Education and
to other rehabilitation suppliers. It is not a form filed by the employer/carrier.
Page 50 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 8
AVERAGE WEEKLY WAGE
All workers’ compensation benefits are based on the claimant’s average
weekly wage. Consequently, it is important to understand how average weekly
wage should be calculated. Essentially Mississippi uses the wages earned during
the 52 weeks before the injury date in making this determination. To be precise,
there are three mutually exclusive methods for calculating the Average Weekly
Wage under Miss. Code Ann. §71-3-31 (1972, as amended):
8.1. THREE FORMULAS
a. If a claimant has worked for the employer for 52 weeks and has
missed less than seven unpaid days during that time, divide the total earnings by
52 to determine the average weekly wage. For example, if the claimant has
earned $20,000.00 (gross wages) in the 52-week period prior to the date of
injury, the claimant’s average weekly wage would be $384.62 ($20,000 divided
by 52 = $384.62).
b. If a claimant has worked for the employer for 52 weeks and has
missed more than seven unpaid days during that time, convert the lost time into
workweeks and subtract the number of lost time weeks from 52 and use the
remainder to divide into the total earnings. For example, if the claimant missed
ten days of work during the year in question and had a 5-day workweek, he
would have missed two workweeks. Subtracting 2 from 52 means that the
divisor into the total earnings would be 50. Consequently, if the claimant earned
$20,000.00 during the 52-week period prior to the injury in question and missed
two workweeks, the AWW would be $400.00. ($20,000 divided by 50 =
$400.00). For the purposes of this illustration, the 10 days missed from work
are not days for which the employee was paid sick leave or vacation leave, but
unpaid missed days from work that were available for other similarly situated

Page 51 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
employees to work.
c. If a claimant has not worked for the employer for 52 weeks prior to
the injury, divide the total earnings of the employee by the number of weeks (or
parts of weeks) during which wages were earned. For instance, if the claimant
worked for 40 weeks prior to the date of injury and earned $20,000.00, the AWW
would be $500.00 ($20,000 divided by 40 = $500.00)
8.2. PARTIAL WEEKS WORKED
It is typically argued that for partial weeks worked, one day will count as
.20 weeks, two days will count as .40 weeks, three days will count as .60 weeks,
and four days will count as .80 weeks for purposes of determining the
appropriate divisor. As an example, assume the claimant worked for parts of
four weeks before the injury date and earned a total of $1000. During those four
weeks, he worked one day one week, two days one week, three days one week
and 4 days one week. Adding up those partial weeks worked of .2, .4. .6, and .8
would total 2.0, so the $1000 earnings would be divided by 2 instead of 4 to give
an average weekly wage of $500.
Case law has held that as few as four weeks is an adequate period of time
to calculate the average weekly wage if those weeks are illustrative of the typical
workweek expected by similarly situated employees.
8.3. EMPLOYED FOR SHORT TIME BEFORE INJURY
If none of these methods work due to the shortness of time during which a
claimant was employed before the injury in question, the average weekly wage
to be used will be that of a similarly situated employee calculated according
whichever of these three methods is applicable.

Page 52 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
8.4. GRATUITIES/TIPS
Gratuities or tips are a part of the average weekly wage as well and should
be included in the total wages earned as a part of the calculation. In fact,
allowances of any character that are paid the claimant, which are in lieu of wages
or specified as part of the wage contract, are a part of the earnings to be
considered. Miss. Code Ann. §71-3-31 (1972, as amended).
PRACTICE POINT: Proof of the dollar amount of tips to be considered as
part of the average weekly wage can be problematic, and decisions can be found
supporting the proposition that only reported taxable income from tips can be a
part of the average weekly wage, while other decisions have permitted the
claimant’s testimony on tips received to be the “best evidence” of the total
income. When confronting this issue, the claims professional will need to fully
investigate the allegations regarding tips received so that an informed decision
can be made as to the appropriate average weekly wage to use.
8.5. SICK PAY AND VACATION PAY
Sick pay and vacation pay are not “salary in lieu of compensation” meaning
that the employer/carrier do not take credit for those payments against
compensation benefits that are due. Whether an employer’s policies permit or
prohibit that is not addressed in the workers’ compensation law. However, in
dealing with an employee of the State of Mississippi, there is statutory authority
addressing the extent to which an employee can take both workers’
compensation benefits and accrued sick leave. See Miss. Code Ann. §25-3-95
(1972, as amended). In summary, a state employee who misses work due to a
work injury can receive both workers’ compensation benefits and
personal/medical leave but the amount of personal/medical leave can be limited
to prevent the employee from receiving benefits which exceed the total amount
of wages earned at the time of injury. The statute doesn’t allow for a reduction
in workers’ compensation benefits based on the receipt of sick leave benefits.

Page 53 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
8.6. PART TIME EMPLOYEES
Part time employees are not discriminated against and are entitled to
benefits based on their actual average weekly wage calculated as above. The
minimum compensation rate, however, is $25 per week.
8.7. CLAIMANT WITH MORE THAN ONE JOB AT TIME OF INJURY
If a claimant is working for more than one employer at time of injury, only
the wages paid to the claimant from the job in which the injury occurred are
included in the average weekly wage calculation; however, those additional
wages will be included in the average weekly wage calculation if both jobs are for
the same employer. As an example, if the claimant is working for a school as a
cafeteria worker and also drives a bus for the school, the wages earned in both
jobs will be included in the total earnings to calculate the average weekly wage.
PRACTICE NOTE: The Claims Professional is encouraged to obtain the
claimant’s wage record and analyze it appropriately to calculate the correct
average weekly wage and compensation rate so that payments are correctly
made.

Page 54 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 9
DISABILITY BENEFITS
9.1. MAXIMUM AND MINIMUM WEEKLY AMOUNTS
The weekly compensation rate for disability is calculated by taking 66 2/3%
of the claimant’s average weekly wage subject to the applicable maximum and
minimum weekly rates established under the law. The Act sets a maximum
weekly compensation rate as well as a weekly minimum in Miss. Code Ann. §71-
3-13 (1972, as amended). The maximum and minimum weekly rates in effect as
of the date of injury will remain with the claim throughout its life. A listing of
those applicable weekly minimums and maximums is available on the MWCC
Web site: http://www.mwcc.state.ms.us/#/maximumBenefitMileageRatesChart.
9.2. WAITING PERIOD
There is a five (5) day waiting period for disability benefits, but after
fourteen (14) days of disability, the waiting period is eliminated and benefits are
paid from the date of injury. See Miss. Code Ann. §71-3-11 (1972, as amended).
If the employee is paid in full for the date of injury, disability is calculated as
beginning on the day following the injury date. If the employee is not paid in full
for the injury date, disability is calculated as beginning on the injury date.
Neither the five-day waiting period nor the fourteen-day period of disability has
to be consecutive days. See MWCC Rule 1.11. It is important to note that a day
of disability, under the stated rule, is any day on which the injured employee is
unable, because of injury, to earn the same wages as before the injury. That
means that lost time, if supported by medical findings, includes weekend days or
other days on which the employee is not scheduled to work. For example, an
employee usually works Monday through Friday and is injured on Friday and is
paid wages in full for the injury date. His five-day waiting period would be
Saturday, Sunday, Monday, Tuesday & Wednesday. See Commission Rule 1.11.

Page 55 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
9.3. NON-CONSECUTIVE LOST TIME DAYS
Lost time does not have to be consecutive or even full days in order to
trigger an obligation to pay compensation benefits. When completing the B-31 in
a situation involving non-consecutive lost time days, care should be taken to
clearly explain payments made. Although a full week of disability (five, six or
seven consecutive days) results in the payment of the same weekly maximum,
scattered or non-consecutive days of disability, where six or seven days in total
are paid at the daily rate, will yield a total amount due that is higher than the
weekly maximum. That should be reflected and explained on the B-31.
9.4. DAILY COMPENSATION RATE
Under Commission Rule 1.10, the daily rate of compensation is the weekly
compensation rate divided by five. That means that a claimant gets the same
compensation amount if he or she is being paid five, six or seven days. To
illustrate, assume the claimant has an Average Weekly Wage of $500 and a
resulting compensation rate of $333.33. His daily compensation rate is therefore
$66.67 ($333.33 divided by 5) and if he has five days of disability, he gets
$333.33 (daily rate multiplied by 5). If he is being paid for six days of disability,
he also gets $333.33; and if he is being paid for a full seven days lost time, he
also gets $333.33. See Commission Rule 1.10.
9.5. MAXIMUM RECOVERY
There is a dollar maximum applicable to indemnity or compensation
benefits set forth in Miss. Code Ann. §71-3-13 (1972, as amended). It is
reached by the payment of a single period of 450 weeks at the applicable
maximum compensation rate for the year in which the injury occurred. As per
the chart on the MWCC website explaining the weekly indemnity maximum at
http://www.mwcc.state.ms.us/#/maximumBenefitMileageRatesChart, there is
Page 56 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
also a lifetime disability maximum which is reached by the payment of the
applicable weekly maximum for 450 weeks. It is an overall dollar maximum
applicable to the claim for indemnity benefits. This indemnity maximum is not
applicable to a claim for medical benefits.
9.6. PENALTIES FOR LATE PAYMENTS
Any installment of compensation not paid within fourteen days of the due
date is subject to a 10% penalty. See Miss. Code Ann. §71-3-37(5) (1972, as
amended). Each installment of compensation is to be paid beginning on the 14
th
day of disability with additional installments due each fourteen days thereafter.
Miss. Code Ann. §71-3-37(2). To illustrate, if the disability begins on January 1,
the first installment of compensation is due on January 14; if that payment is not
made by January 28, then the penalty is applicable.
The penalty can be avoided by (1) paying the amount due within fourteen
days of the due date; (2) controverting the right to compensation benefits within
fourteen days of the employer’s notice of the injury by filing a Form B-52,
Employer’s Notice of Controversion (See Section 6.3.f); or (3) proving that the
inability to make payments was due to circumstances beyond the control of the
employer.
If an installment of compensation payable under the terms of an award is
not paid within 14 days of the due date, the penalty is 20%. Miss. Code Ann.
§71-3-37(6).
In addition to penalties for late payments, the Commission can determine
that interest might also be payable on late installments of compensation.
9.7. OVERPAYMENTS
If the employer has made advance payments of compensation, it shall be
entitled to be reimbursed out of any unpaid installment or installments of
compensation due. Miss. Code Ann. §71-3-37(11) (1972, as amended).

Page 57 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
9.8. CHILD SUPPORT LIENS
Child and spousal support liens against workers’ compensation benefits are
enforceable. See Miss. Code Ann §71-3-129 (1972, as amended). A lien against
the wages of a claimant served on the employer is not the same thing as a valid
and enforceable lien against the claimant’s workers’ compensation benefits, but
that notice should serve as a requirement to further investigate the obligation to
honor the attempted lien. A lien formally attaches to workers’ compensation
benefits once the Mississippi Department of Human Services, Division of Child
Support Enforcement, obtains the lien in the court of appropriate jurisdiction.
Notice of that lien, once established, must then be filed (my mail or fax) with the
Executive Director of the Mississippi Workers’ Compensation Commission. The
Commission Executive Director then puts the employer/carrier on notice of the
lien, and, once that notice is received by the employer/carrier, the lien attaches
to the workers’ compensation benefits payable to that claimant. The parties are
deemed to have notice of the lien within five days of the mailing and the lien
shall attach to all workers’ compensation benefits that are thereafter payable.
If payments are ongoing, the appropriate child support department may
send an income withholding order. It will specify the monthly payments as well
as provide weekly and bi-weekly breakdowns. There are limits as to how much
can be withheld from the benefits, however. Child support payments are
excepted from the limits on normal garnishments in Miss. Code Ann. §85-3-21
(1972, as amended). For child support payments, limits are established as
follows:
If the employee is supporting a spouse or dependent other than the
dependent named in the Order, the maximum is 50% of disposable income;
If the employee is not supporting a spouse or dependent other than the
dependent named in the Order, the maximum is 60% of disposable income;
If the payment is in arrears for more than 12 weeks, those limits get a 5%
bump to 55% and 65%, respectively.

Page 58 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Child and spousal support liens are the only liens against workers’
compensation benefits that are enforceable pursuant to Miss. Code Ann §71-3-43
(1972, as amended).
a. Obligations in the event of a settlement: The Commission,
pursuant to an official notice dated June 26, 2012, has been working
with the Mississippi Department of Human Services (DHS) to
establish a uniform policy regarding the handling of support liens in
cases that are being settled. That policy notice is found on the
Mississippi Workers’ Compensation Commission website at
http://www.mwcc.state.ms.us/pdf/Child%20Support%20Web%20Pol
icy.pdf. In summary, the policy places on the employer/carrier the
responsibility for withholding the proceeds needed to satisfy a
support lien and to pay those proceeds directly to the Department of
Human Services, or to a support obligee who has his or her own
attorney and is not using the DHS to help with collection. If the DHS
has negotiated the amount of the lien with the parties, a written
confirmation from the DHS regarding that compromise of the lien is
required by the Commission before approval of the settlement.
Note, however, that the employer/carrier still has the obligation to
withhold the necessary proceeds to satisfy the lien in the situation
involving lien compromise.

Page 59 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 10
CATEGORIES OF DISABILITY
There are four categories of disability benefits and they will each be
discussed briefly in turn. Disability is defined under the Act as “the incapacity
because of injury to earn the wages which the employee was receiving at the
time of injury in the same or other employment, which incapacity and the extent
thereof must be supported by medical findings.” Miss. Code Ann. §71-3-3(i)
(1972, as amended). Disability benefits are therefore conditional on a medical
opinion to the effect that the injury prohibits or impairs the claimant from
working on either a temporary or permanent basis.
10.1. TEMPORARY TOTAL DISABILITY
Temporary Total Disability (TTD) benefits are discussed in Miss. Code Ann.
§71-3-17(b) (1972, as amended), and are generally payable when the employee
is completely unable to work because of injury but the disability is not expected
to be permanent. Installments of compensation are payable every fourteen
days (although weekly payments are permissible).
The weekly maximum changes annually but the weekly minimum is
$25.00. A complete listing of the applicable maximum and minimum
compensation rates is on the MWCC website at
http://www.mwcc.state.ms.us/#/maximumBenefitMileageRatesChart. Each
category of benefits (i.e. TTD, TPD, PPD, or PTD) is payable for a maximum of
450 weeks. However, the overall indemnity maximum discussed in Section 9.5
will be reached in a single 450-week period at the weekly maximum.
As previously noted, there is a five-day waiting period for benefits unless
the disability lasts longer than fourteen days. Temporary total disability is
essentially a medical issue in that if medical opinions support the inability to
return to work, then benefits would be payable. Conflicting medical opinions on
this issue are often a source of contention and the basis for controversion and

Page 60 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
litigation. The resolution of such disputes is often fact intensive.
The first installment is due on the fourteenth day after the employer has
notice of the disabling injury or death and is paid bi-weekly thereafter until the
claimant is released to return to work full duty, placed at maximum medical
improvement (MMI) or returns to work in any capacity.
An Order from the Commission is not usually required to suspend TTD
benefits, but suspending benefits without an appropriate reason could be
problematic from a bad faith standpoint. In two similar circumstances, an Order
authorizing the suspension of benefits must be obtained if the basis for the
suspension of benefits is an assertion that the claimant is (1) unreasonably
refusing to submit to medical treatment or (2) unreasonably refusing to submit
to an examination at the instance of the employer/carrier. In those instances, a
hearing is first required to determine whether claimant’s refusal to do either is
unreasonable. Miss. Code Ann. §71-3-15(1), Miss. Code Ann. §71-3-37(3) (1972,
as amended) and MWCC Rule 1.9.
PRACTICE POINT: The suspension of benefits issue usually comes up at
the point when a claimant is at maximum medical recovery or is released to
return to work. Suspending benefits without an Order when neither of those
contingencies has occurred can be particularly problematic from a bad faith
standpoint. In addition, automatically suspending benefits when those
contingencies occur can also be problematic in those cases, as examples, where
there is an issue of permanent disability, conflicting medical opinions on the
release, or multiple body parts involved and claimant is only at maximum
medical recovery from a part of his injury. To further illustrate, in scheduled
member disability cases, the employer/carrier owe at a minimum the medical
impairment rating. (As an example, if a claimant is released to return to work
with a 10% impairment rating to an arm, 10% of 200 weeks or 20 weeks is also
due at a minimum so those benefits should continue. See Chapter 9.3.a for a
discussion of those benefits).
Also, in body-as-a-whole cases such as back injuries, which are more fully

Page 61 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
discussed in Chapter 9.3.b, a “big picture” analysis must be made to see if
benefits should be suspended at maximum medical recovery or release to return
to work. As examples: Does the claimant have permanent work restrictions?
Can the employer accommodate the restrictions? Has the employer terminated
the claimant? A decision to terminate benefits is too important to adopt an
“always or never” approach to handling this issue. A decision to terminate
benefits that is designed to use the superior economic weight of the
employer/carrier to force the claimant to settle his case for less than it might be
worth can be fuel for a bad faith case, and a claims professional should carefully
evaluate facts and analyze a decision to terminate benefits. That analysis might
also include advice of counsel if uncertainty prevails on the appropriate decision
to take.
Form B-18 is the MWCC form used to inform the Commission and the
claimant that his benefits have started, stopped, restarted, or changed to a
different category.
It is possible that the employer will pay claimant’s regular salary in lieu of
compensation benefits, and that is permissible. However, those payments must
be reported to the Commission on a B-18 and B-31 as well.
PRACTICE NOTE: If an employer pays salary in lieu of compensation on a
case involving more than five days lost time, the claim becomes a lost time claim
that must be reported to the Commission. A B-31 will need to be filed in order
for the statute of limitations to beginning running. The case is not a “medical
only” just because the employer pays salary in lieu of compensation.
10.2. TEMPORARY PARTIAL DISABILITY
Temporary Partial Disability (TPD) benefits are payable when the employee
sustains a partial disability before maximum medical recovery. It is usually
found in those cases where claimant returns to work with temporary work
restrictions and, due to the injury, is unable to earn the same wages he was

Page 62 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
earning prior to the injury. Miss. Code Ann. §71-3-21 (1972, as amended). The
benefit is calculated by taking the pre-injury average weekly wage minus the
wage-earning capacity after the injury times 66 2/3%. The TPD benefit is
subject to the same maximum limitations as to TTD benefits, but there is no
applicable minimum weekly benefit. Examples: A claimant’s pre-injury weekly
wage was $500. After the injury (and before maximum medical recovery)
claimant had a wage earning capacity of $200. The TPD benefit would be
calculated as follows: $500 - $200 = $300 x 66 2/3rds % = $200.00 per week.
Assume instead the AWW of $500 but claimant returns to work at $490 per
week. The benefit is arguably $6.67 per week or 66 2/3rds% of the $10 per
week difference in his pre- and post-injury wages.
A common question dealing with TPD benefits is what to do if a claimant
has been released to return to light duty work, and the employer is willing and
able to accommodate the restrictions, but the claimant refuses to return to work.
Arguably TPD benefits are not owed because claimant is under a duty to make a
reasonable effort to return to work. At the same time, if the employer is
unwilling to or unable to accommodate the light duty work restrictions, claimant’s
benefits probably continue at the same rate paid for TTD.
MWCC Form B-18 is the form used to notify the MWCC and the claimant
about the payment of TPD benefits.
10.3. PERMANENT PARTIAL DISABILITY
Permanent Partial Disability (PPD) benefits are payable after the claimant
attains maximum medical improvement and is left with a disability that is less
than total but nonetheless permanent. See Miss. Code Ann. §71-3-17(c) (1972,
as amended). Permanent partial disability benefits fall into two categories: those
involving scheduled injuries and those involving non-scheduled injuries, or what
are generally referred to as "body as a whole" cases. There are similarities as
well as differences in the analysis and payment of these benefits. PPD for certain

Page 63 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
body parts likes arms, legs, hands, feet, eyes, etc. are “scheduled” members,
while injuries not included in the schedule, such as back or head injuries, are
“body as a whole” injuries.
10.3.a. SCHEDULED MEMBER INJURIES
Scheduled member PPD benefits are in addition to temporary disability
benefits and begin once a claimant is at maximum medical improvement. The
value of the impairment is a reflection of the claimant’s “industrial loss of use” of
the scheduled member. For a partial loss of use of a scheduled member, the
benefit is calculated by applying the percentage of industrial loss of use of the
scheduled member to the applicable number of weeks in the schedule, and those
benefits are then paid out at the same compensation rate paid for TTD (2/3rds of
the AWW subject to the weekly maximum). Unless ordered by the Commission,
they are not to be paid in a lump sum but should be paid out biweekly (although
weekly payments are also permissible).
1. USE OF AMA GUIDELINES: The permanent impairment rating
obtained from the claimant’s doctor should be calculated according to
the latest edition of the Guidelines to the Evaluation of Permanent
Impairment published by the American Medical Association, currently in
its Sixth edition.
The medical impairment rating stated by the treating physician is not,
however, the only factor to be considered in evaluating the industrial loss of use
of the scheduled member, and often times a claimant is entitled to more than
just the permanent impairment rating. The value of a scheduled member
permanent disability is based on a number of factors taken together including
claimant’s age, education, training, work experience, transferrable work skills,
and post-injury work history and earnings. The employer/carrier owe at least
the medical impairment rating to the scheduled member even if the industrial
loss of use is less than the rating. Stated differently, a claimant is entitled to the

Page 64 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
greater of (1) the functional or medical impairment or (2) the industrial loss of
use of the scheduled member. Ard v Marshall Durbin Companies, Inc., 818 So.
2d 1240 (Miss. 2002). In general terms, if the scheduled member injury
prohibits a claimant from performing the substantial acts of his usual
employment, the whole scheduled member can be awarded. There are even
instances where permanent total disability can be awarded where the scheduled
member impairment prohibits a claimant from returning to any work for which he
is capable when considered in light of those factors identified above.
To calculate the amount payable for a scheduled member PPD rating, the
doctor should first calculate the permanent impairment rating pursuant to the
latest edition of the AMA Guidelines to the Evaluation of Permanent Impairment.
Once that number is established, multiply the percentage loss of the scheduled
member times the number of weeks allowed for total loss of the scheduled
member and pay benefits for that number of weeks at the claimant’s applicable
compensation rate beginning with the date of maximum medical improvement.
To illustrate, the leg is worth 175 weeks under the Act. Assume a compensation
rate of $400 and a 10% PPD rating to the leg. Benefits would be calculated as
follows: 175 weeks x 10% = 17.5 weeks x compensation rate of $400 to be paid
out biweekly. Recall, however, that the real issue is not just the impairment
rating, and if this rating represents a 25% industrial loss of use of the scheduled
member, the number of weeks payable would be 175 weeks x 25% or 43.75
weeks at the claimant’s compensation rate.
PPD benefits are supposed to be paid biweekly. Weekly payments can by
made although monthly payments cannot be made unless ordered by the
Commission. The agreement to pay PPD benefits is reported to the Commission,
with notice to the claimant, on Form B-18. The clamant can request that the
Commission allow future benefits to be paid in a lump sum payment by filing
form B-19, Application for Lump Sum Payment. Upon receipt of the Order and
the lump sum calculation from the Commission, payment should be made within
fourteen days of the Order date.

Page 65 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Inasmuch as it is often difficult to determine the exact amount payable for
injuries to scheduled members without having a hearing and determination by an
Administrative Judge, these cases are often settled on a compromise basis
pursuant to Miss. Code Ann. §71-3-29 (1972, as amended), and MWCC Rule
2.15. These compromise settlements, which often also include a closure of
medical, are referred to as 9(i) settlements, a reference to the original code
section nomenclature when the law was first passed. Any settlement is subject
to approval by the Commission, and a licensed Mississippi attorney must be
retained by the employer/carrier to prepare the proper paperwork and present
the settlement to the Commission. The claimant does not have to be represented
in such a settlement, but if he is not, the Commission will interview him or her
(usually in person, but sometimes by telephone), to make sure that the
settlement is in his/her best interests. The MWCC has established a number of
specific rules regarding settlements and those rules may be obtained from the
MWCC website: http://www.mwcc.state.ms.us/pdf/memotoattorneys.pdf.
Changes effective January 18, 2018 related to settlements are also included in
Commission Rule 2.15. See Section 14.1 for further discussion of settlements.
A chart showing the number of weeks payable for scheduled members
follows. Other specific provisions are included in the Act relating to amputations
of fingers and toes, hearing loss, and loss of sight that should be consulted. See
Miss. Code Ann. §71-3-17(c) (1972, as amended). It is important to note that
the impairment rating for a partial loss of use of a schedule member must be
determined by a licensed medical doctor. A quick listing of the number of weeks
scheduled for most of the “scheduled members” is as follows:
Arm
200 weeks
Third finger
20 weeks
Leg
175 weeks
Toe other than great toe
10 weeks
Hand
150 weeks
Fourth finger
15 weeks
Foot
125 weeks
Testicle, one
50 weeks
Eye
100 weeks
Testicle, both
150 weeks
Thumb
60 weeks
Breast, female, one
50 weeks
First finger
35 weeks
Breast, female, both
150 weeks
Great toe
30 weeks
Loss of hearing, 1 ear
40 weeks
Second finger
30 weeks
Loss of hearing, both ears
150 weeks

Page 66 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
10.3.b. BODY AS A WHOLE INJURIES
The permanent partial disability benefits for non-scheduled injuries such as
those involving the back, head, or heart are calculated differently but have some
commonality with the scheduled member awards. The claimant is entitled, in
those cases, to two-thirds of his/her loss of wage earning capacity payable over
450 weeks. See Miss. Code Ann §71-3-17(c)(25) (1972, as amended). Please
note that such benefits are not calculated by multiplying 450 weeks by the
permanent impairment rating as might be done in scheduled member cases.
Also, the loss of wage earning capacity percentage may be more or less than the
medical impairment rating and, in some instances, a claimant might receive
permanent total disability benefits even though he/she had only a partial
disability rating.
A formula to follow as a starting point in calculating PPD benefits to the
body as a whole is the average weekly wage of the claimant, times the percent of
his/her loss of wage earning capacity, times 66 2/3rds percent, for 450 weeks.
Again, the concept of loss of wage earning capacity encompasses a review of
multiple factors such as the claimant’s age, education, training, work experience,
transferrable work skills, post-injury efforts to find a job, and actual work history
and earnings, all in an effort to evaluate claimant’s ability to earn wages on the
open labor market. The net result of that kind of analysis is that the outcome is
quite subjective. An award is not limited to an impairment rating.
To illustrate the calculation of benefits, assume the claimant has a back
injury and is left with a 15% anatomical impairment rating. His pre-injury
average weekly wage is $500. If he has a 15% loss of wage earning capacity
consistent with the rating, the amount payable is calculated as follows: $500
times 15% ($75.00) times 2/3rds ($50.00) for 450 weeks. The benefit would
total $22,500, but is supposed to be paid bi-weekly unless the Commission
orders a lump sum payment (or a 9(i) settlement is reached).
The calculation is easy to conceptualize and implement once the percent

Page 67 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
loss of wage earning capacity is known. The harder part is the analysis of how to
establish the percentage of loss of wage earning capacity. Since the award is
supposed to be a reflection of how the injury has affected claimant’s ability to
earn wages on the open labor market, the analysis is subjective. Whatever the
loss of wage earning capacity percent turns out to be, however, the formula is
the same. If it is 25% loss of wage earning capacity, the benefit is calculated as
follows: $AWW x 25% x 2/3rds payable for 450 weeks. If it is a 50% loss of
wage earning capacity, the benefit is calculated as follows: $AWW x 50% x
2/3rds payable for 450 weeks. The formula remains the same with the variable
being a change in the assumed percent loss of wage earning capacity. The
benefit is not calculated by taking a percent of 450 weeks.
Although Mississippi contemplates the payment of PPD benefits to the body
as a whole based on a loss of the capacity to earn wages due to the injury,
sometimes the result is a reflection of a comparison of the pre-injury and post-
injury earnings. Although those decisions do not appear to analyze the capacity
to earn wages issue, it is another way to look at a potential result. If the pre-
injury AWW is $500 and the post-injury AWW is $300, a potential result is 2/3rds
of the difference for 450 weeks. $500 - $300 = $200 x 2/3rds = $133.33 for
450 weeks.
The $25.00 per week minimum is not applicable for partial disability cases,
but the same weekly maximum for temporary total disability does apply. See
Commission Rule 1.13 for additional provisions applicable to paying PPD benefits
at the same rate as TTD being considered an acceptable acceleration of
payments.
There are some presumptions to consider in evaluating these cases, all of
which are considered rebuttable:
A. If claimant returns to work at the same wage he/she was earning
before the injury date, it is presumed that claimant has no loss of wage earning
capacity; claimant can rebut that presumption, however, by showing that his
post-injury earnings are not a reliable basis for evaluating the capacity to earn

Page 68 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
wages on the open labor market. Proof that claimant is only receiving sympathy
wages, or that the job is only temporary, or other similar factors, could still yield
an award for benefits.
B. If an employer refuses to allow a claimant to return to work after
maximum medical improvement and claimant presents himself for re-
employment at that time, there is a presumption that the claimant is totally
disabled. That presumption can be rebutted, however, by proof that there was
another legitimate reason the claimant was not rehired other than the refusal to
accommodate the injury. As an example, proof that the claimant violated an
established employment policy, such as failing to abide by the drug free work
place policy, or violating an established “no call, no show” policy, could be
adequate to rebut that presumption.
C. If the claimant fails or refuses to make a legitimate effort to return to
work, there is a presumption that the claimant has sustained no loss of wage
earning capacity.
10.3.c. SERIOUS HEAD OR FACIAL DISFIGUREMENT
A claimant who sustains serious head or facial disfigurement is entitled to a
payment not to exceed $5,000.00. No such award can be made, however, until
a lapse of one year from the injury date that caused the disfigurement. See Miss
Code Ann. §71-3-17(c) (24) (1972, as amended). The parties are permitted to
agree on the amount to be paid and report it on a B-18 or the claimant can go to
the Commission on a Tuesday or Wednesday and have the Commission make the
determination of the amount due.
10.4 PERMANENT TOTAL DISABILITY
Permanent Total Disability (PTD) benefits are not payable for life but are
subject to the same 450-week limitation, weekly minimums and maximums, and
overall dollar maximum referenced above. PTD is payable for loss, either by
amputation or total loss of use, of both arms, legs, hands, feet, eyes, or any

Page 69 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
combination, and in other cases as the facts may appear. Miss. Code Ann. §71-
3-17(a) (1972, as amended). The “other cases” provision is where PTD comes
up most frequently, and in its simplest form, PTD is payable when an employee is
unable, because of the injury, to return to any reasonable employment for which
he is trained by education, training or experience. PTD could be the result even if
the injury concerns only the loss of or loss of use of a single scheduled member.
The analysis is always focused on how the injury has affected a claimant’s ability
to earn wages on the open labor market, and a review of multiple factors such as
the claimant’s age, education, training, work experience, transferrable work
skills, post-injury efforts to find a job, and actual work history and earnings, is all
a part of the analysis on the extent of disability.
From a claims handling standpoint, the benefit is calculated by taking 66
2/3% of the claimant’s average weekly wage, subject to the maximum and
minimum compensation rates applicable for TTD. Installments of compensation
are payable every fourteen (14) days unless otherwise ordered by the
Commission. In some cases, the permanent and total nature of the disability is
apparent at the time of injury and benefits are therefore commenced
immediately. In most cases, however, benefits are paid for a period of
temporary total disability and at some later date, it is determined that PTD is
due. In these cases, the employer/carrier take credit for the number of weeks
previously paid for temporary disability and pay the balance of the remaining 450
weeks for PTD. As an example, if the claimant has been paid fifty weeks of TTD
when he is found to be at MMI and deemed PTD, the employer/carrier would get
credit for the previously paid 50 weeks and owe an additional 400 weeks to be
paid because the total disability has existed since the beginning of the claim.

Page 70 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 11
DEATH BENEFITS
Death benefits are payable only for a maximum of 450 weeks and are
subject to the same minimum and maximum weekly compensation rates as
disability cases. As with disability benefits, the statute contemplates the
payment of benefits on a bi-weekly basis unless otherwise ordered by the
Commission. Benefits payable are set forth in Miss. Code Ann. §71-3-25 (1972,
as amended) and include the following:
11.1. $1,000 IMMEDIATE PAYMENT
An immediate lump sum payment of one thousand dollars ($1,000.00) is
owed to the surviving spouse.
11.2. FUNERAL ALLOWANCE
Reasonable funeral expenses, not to exceed five thousand dollars
($5,000.00), are owed on behalf of the decedent. The benefit is payable even if
the funeral expenses were paid by any other insurance or collateral sources.
11.3. WEEKLY BENEFITS TO DEPENDENTS
A surviving spouse and minor children are conclusively presumed
dependent on the decedent. They are in a priority category for the death
benefits and will take to the exclusion of any other dependents. A surviving
spouse is entitled to 35% of the decedent’s average weekly wage and each child
is entitled to 10% of the decedent’s average weekly wage, so long as the total
payable to all dependents does not exceed 66 2/3% of the decedent’s average
weekly wage.
If there is no surviving spouse, each child gets 25% of the decedent’s
average weekly wage, subject to the overall 66 2/3% for all dependents
Page 71 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
combined. If the surviving spouse remarries, the surviving spouse’s death
benefit is suspended and each child’s rate is increased from 10% to 15%.
Children above age 18 may be entitled to benefits if they are incapable of
self-support by reason of mental or physical disability or if they are under age 23
and remain a full-time student. The Commission may, in its discretion, require
the appointment of a guardian for the purpose of receiving the compensation of a
minor dependent, but usually payments are made to the surviving parent who is
considered under Mississippi law to be the “natural guardian.”
If the surviving spouse and children do not take the full 66 2/3% of the
decedent’s AWW, then other dependents of the decedent such a parents,
grandparents, brothers, and sisters may qualify. Dependency is not presumed,
and each would have to prove at least a partial dependency on the decedent at
the time of the decedent’s death. Each such dependent would be entitled to 15%
of the decedent’s average weekly wage, but remember that they are in a
secondary category and are paid only if the amount payable to the surviving
spouse and minor children is less than 66 2/3rds% of the decedent’s AWW.
As an example, assume a decedent leaves as dependents a surviving
spouse, 3 children and his mother. The widow’s portion is 35% and each child is
10% for a total of 65%. In that scenario, the decedent’s mother would be paid 1
2/3rds% of the decedent’s AWW since it is the amount between the 65% for the
priority beneficiaries and 66 2/3rds percent of the AWW.
The $25 minimum payment has been held to be applicable to all
beneficiaries collectively and not to each individual death beneficiary.
If the total percentage of the decedent’s AWW for all beneficiaries
collectively exceeds 66 2/3rds, the benefits are distributed based on a
proportionate basis. Assume the decedent had a $600 AWW giving him a
maximum compensation rate of $400, and he leaves a widow and 5 children. In
that instance, the total percentage of the AWW would be 85% (35% + 10% +
10% + 10% + 10% + 10%), but the benefit is subject to a maximum of 66

Page 72 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
2/3rds %. In that scenario, the widow’s portion would be 35/85ths of $400 and
each child’s portion would be 10/85ths of the $400 compensation rate.
Since benefits for each child stop at age 18 (unless he/she remains a full-
time student or is incapable of self-support because of a mental or physical
disability), once the benefits for a child stop, it is necessary to recalculate each
benefit. In other words, in our assumed scenario above, once the first child’s
benefits stop, the widow’s portion is recalculated at 35/75ths of $400 and each
child’s portion is 10/75ths of $400. When the next child’s benefits stop, the
widow’s portion becomes to 35% of the $600 AWW and each remaining child
gets 10% of $600 since total percentages for the remaining widow and 3 children
are now only 65%.
Dependency status is determined as of the date of death. Definitions of
“surviving spouse” and “child” in Miss. Code Ann. §71-3-3 (1972, as amended)
must be consulted for careful analysis in most cases. With the modern American
family, it is not unusual to find multiple families with a connection to the
decedent claiming benefits. It is the Claims Professional’s responsibility to do a
thorough investigation into those allegations so the payments are made to the
appropriate parties. This is another instance when consultation with counsel
might be warranted to thoroughly evaluate those issues.
11.3.a DEATH CLAIMS INVOLVING UNDOCUMENTED WORKERS (ALIENS)
There are special provisions applicable to death claims involving
undocumented workers (still referred to in the statute as “aliens”) who are not
residents (or about to become residents) of the United States or Canada. As an
example of those differences, death beneficiaries living in a foreign country are
limited to the surviving wife and child or children of the decedent (with other
provisions also applicable as a contingency). When confronted with this situation,
consult the specific provisions applicable to cases of this nature in Miss. Code
Ann. §71-3-27 (1972, as amended) and seek advice of counsel.

Page 73 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
11.4. PAYMENT TO SECOND INJURY FUND
An additional payment due on a death claim, but not a benefit to death
claim beneficiaries, is a payment to the Mississippi Workers’ Compensation
Commission Second Injury Fund. If there are no dependents entitled to benefits,
a $500 payment should be paid to the MWCC. If there are dependents entitled
to benefits, the payment due to the MWCC is $300; however, that payment can
be suspended by the MWCC once the amount of money accumulated in the Fund
exceeds a statutorily established level. See Miss. Code Ann. §71-3-73 (1972, as
amended).

Page 74 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 12
MEDICAL BENEFITS
Restoring the claimant to good health (and thus gainful employment) is a
primary objective of the Mississippi Workers' Compensation Law. Miss. CODE ANN.
§71-3-1. To that end, the employer must furnish the claimant all necessary and
reasonable medical services, supplies and other attendance or treatment such as
the nature of the injury and the process of recovery requires. Medical Benefits
under the Mississippi Workers' Compensation Act are unlimited in amount and
have no time limitations unless a statute of limitations proves applicable. Miss.
Code Ann. §71-3-15 (1972, as amended).
12.1. CHOICE OF PHYSICAN
An employer's obligation in the event of an injury is to tender medical
treatment to the claimant. The claimant's option is to either accept that tender
or to choose his own. Acceptance of the employer's tender of a physician must
be made in writing in order to be enforceable. MWCC Rule 1.9. In addition, a
part of the 2012 amendments provides that a physician shall be deemed to be
claimant’s choice whether or not the claimant had previously “chosen” that
physician in writing, if (1) the claimant had treated with that physician for six
months or (2) had undergone surgery by that physician.
Once the choice is made, the claimant's choice is limited to the chosen
physician and referrals by that physician to one physician in other areas of
specialty. In other words, a general practitioner chosen by the claimant can
make a referral to one orthopedic surgeon, one neurosurgeon, one neurologist,
one psychiatrist, etc., but could not make a referral to two different orthopedic
surgeons.
A chiropractor may be chosen as a treating physician, but the Mississippi
Workers' Compensation Medical Fee Schedule limits chiropractic treatment to
Page 75 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
fifteen visits or treatment for thirty days, whichever occurs first, unless additional
treatment is authorized by the employer/carrier.
Claimant's choice of physician is limited to an area reasonably convenient
to the injury or the residence of the claimant.
PRACTICE POINT: An open discussion with claimant about physician choice issues
is encouraged to avoid misunderstanding and added expense. Remember that
the Commission can still permit a change of physician after the physician choice
has been established, so a pragmatic analysis of these issues is recommended.
12.1.a. SELECTION OF DME VENDOR, PHARMACY VENDOR
An interesting point involving choice issues is that the Mississippi Workers'
Compensation Medical Fee Schedule gives to the employer/carrier control over
the vendor to be used for durable medical equipment. However, the selection of
a pharmacy vendor is left to the claimant. See Mississippi Workers'
Compensation Medical Fee Schedule, General Rules XI and Pharmacy Rules III.
B.
12.1.b. SELECTION OF DIAGNOSTIC TESTING FACILITIES
The selection of appropriate providers for diagnostic testing or analysis,
including but not limited to CAT scans, MRI, x-ray, lab, physical and occupational
therapy, work hardening, FCE, back school, chronic pain programs, massage
therapy, EMG/NCV shall be at the direction of the treating or prescribing
physician. In the absence of specific direction from the treating or prescribing
physician, the employer/carrier, in consultation with the treating or prescribing
physician, shall make the selection.
12.2. TRAVEL EXPENSE
Travel expense to and from medical treatment is the responsibility of the
employer/carrier, and there is no minimum distance to travel before the
obligation to pay accrues. The rate changes regularly consistent with the rate

Page 76 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
approved for reimbursement to state employees. See MWCC Rule 1.14. For a
complete listing of the applicable mileage reimbursement rates, see
http://www.mwcc.state.ms.us/#/maximumBenefitMileageRatesChart. The Fee
Schedule requires the payer to notify claimant in writing of his or her right to
receive mileage reimbursement, and reimbursement must be paid within 30 days
of the receipt of the request. Failure to do so can result in an assessment of
attorney’s fees, expenses, and a penalty of up to $10,000!
PRACTICE POINT: Remember that the applicable mileage reimbursement rate is
the rate in effect at the time the travel occurs rather than the rate in effect at the
time payment is actually issued.
12.3. EMPLOYER’S MEDICAL EXAM (EME)
The employer/carrier have the right to have a claimant evaluated by a
physician of their choosing for the purposes of evaluating disability issues, the
necessity or reasonableness of treatment recommended by claimant's treating
physician, and other issues. Miss. Code Ann. §71-3-25 (1972, as amended) and
MWCC Rule 1.9. The procedure to be used is as follows:
(a) The appointment is scheduled with the treating physician and
notice, in writing, is given to the claimant and the Commission
of the appointment date, time, place, etc.
(b) The claimant's travel expense to and from the scheduled evaluation
at the applicable mileage rate must be prepaid.
(c) Once the evaluation has been completed, all of the expenses
in connection with same must be paid and a copy of the report
setting forth the physician's findings must be provided to both
the claimant and the Commission.
There may be instances where an employer is entitled to an evaluation by
more than one physician. As an example, if a claimant alleges both back and
psychiatric injuries, an evaluation by separate specialists for those different
problems might be obtainable. Also, there may be a situation where an EME for

Page 77 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
the purpose of evaluating whether or not a person needs surgery is obtained and
then, a year or so later after the surgery has been performed, another
examination to evaluate whether disability is ongoing may be permitted. The
Commission will obviously not permit an abuse of the procedure, however, and
the focus is on what is “reasonable” under the circumstances.
As referenced in Chapter 12.9 of this guide, there is a two-day time
limitation for notifying a provider of the intent to use an EME in lieu of pre-
certification.
12.4. INDEPENDENT MEDICAL EXAM (IME)
Miss. Code Ann. §71-3-15(2) (1972, as amended) provides that the
Commission may order the worker to submit to an independent medical
evaluation (“IME”) when it suspects a treating or examining physician may not
have correctly estimated the extent or duration of disability or for other issues
such as appropriate treatment protocols to be provided. The Commission
generally requests the evaluating physician to do an extensive review of all prior
medical records relating to the work injury, to order diagnostic procedures as
needed, and to submit a written report of the findings of the evaluation. The
Commission may use an IME as a “tie-breaker” to resolve a dispute between
physicians offering different opinions about a worker's disability or necessity of
certain medical treatment. The employer/carrier must pay for the evaluation.
12.5. EX PARTE COMMUNICATIONS WITH MEDICAL PROVIDERS
Miss. Code Ann. §71-3-15(6) (1972, as amended) specifically provides that
medical treatment obtained in connection with a workers’ compensation claim is
not privileged information. Case law has had a significant impact on that
provision, however, and once a case becomes controverted, case law indicates
that there can be no ex parte, or one sided, communications with the medical
providers. The fruit of such inappropriate contact with the medical providers

Page 78 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
could be that the information obtained is not admissible in a hearing. The rule of
law is tied to the idea that such is inappropriate discovery under established
rules. Arguably, other problems could also be flow from such inappropriate
contact.
PRACTICE NOTE: The prohibition against ex parte communications with
medical providers is not applicable to such things as obtaining medical records
and bills or, usually, dealing with pre-certification of testing and treatment
issues. Whether the activity is done by the claims professional or by a nurse case
manager, the professional is encouraged to not have one-sided communications
with medical providers to avoid these problems in controverted cases.
Conferencing with the medical providers when claimant is not present or writing
to the providers and not copying claimant’s attorney is not the way to handle
claims appropriately under the law as currently interpreted. Writing the medical
providers to ask the necessary questions and copying the claimant’s attorney
with that letter can still permit the claims professional to obtain information
regarding claimant’s injuries, however. The issue often comes up as well in
cases where the claimant is represented but the case is not yet controverted,
and claimant’s attorney requests that no ex parte communications take place
with the medical providers. Although technically the rule of law is not applicable
in non-controverted cases, ignoring the request will only result in a controversion
to invoke the rule, and that will only add legal expense to the claim and impair
the claims professional’s working relationship with the attorney.
12.6. HIPAA COMPLIANT MEDICAL AUTHORIZATION
Although the medical privilege is statutorily minimized in workers’
compensation cases as noted above, and the HIPAA regulations specifically
provide that they are not applicable to workers’ compensation cases, the Claims
Professional is encouraged to request that a claimant sign and return a HIPAA
compliant medical authorization. Many medical practitioners are reluctant to
release medical information, which is necessary to properly handle the claim,

Page 79 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
without the authorization. See provisions on the MWCC WEB site relating to the
HIPAA issues at http://www.mwcc.state.ms.us/pdf/HIPAAWebNotice.pdf. Also
see the provisions on the website of the U. S. Department of Health & Human
Services related to disclosures for workers’ compensation purposes:
http://www.hhs.gov/hipaa/for-professionals/privacy/guidance/disclosures-
workers-compensation/index.html
12.7. TREATMENT BY VA HOSPITAL OR PAID FOR BY GOVERNMENT
Sometimes a claimant’s medical treatment is obtained at a Veterans
Administration Hospital or at the expense of the State Division of Medicaid or the
Mississippi Department of Rehabilitation Services. Pursuant to Commission Rule
1.9, the employer/carrier are not liable for that treatment UNLESS the officials at
those facilities fully comply with Miss. Code Ann. §71-3-15 (1972, as amended)
and the Commission Rules. With recent changes required by the Centers for
Medicare and Medicaid Services relating to Medicaid, this rule as it relates to
Medicaid may no longer be the final word related to a claim by Medicaid for
reimbursement as discussed in Chapter 14.5 of this Guide.
12.8. MEDICAL PAYMENTS BY HEALTH INSURANCE PROVIDERS
If medical treatment for a work-related injury is paid for by a health
insurance carrier, that health carrier may put the employer/carrier on notice of
its lien, and the employer/carrier may reimburse the health carrier. Payment to
the health carrier shall be considered payment of the employer/carrier’s
obligation to pay for medical expenses under the workers’ compensation law.
See Miss. Code Ann. §71-3-15(7) (1972, as amended).
12.9. MISSISSIPPI WORKERS’ COMPENSATION FEE SCHEDULE
The Mississippi Workers’ Compensation Medical Fee Schedule was
established pursuant to statutory authority under Miss. Code Ann. §71-3-15(3)

Page 80 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
(Rev. 2000) and adopted pursuant to Commission Rule 1-12. It provides rules
and regulations for reimbursement of services provided to the workers’
compensation claimant. It includes maximum allowances for medical
procedures, as well as rules for appropriate services and determination of
medical necessity.
A significant provision included in the statute authorizing the establishment
of the Fee Schedule is that a medical provider is not permitted to “balance bill” a
claimant for the charges of the medical provider that exceed the reimbursable
amount specified in the Fee Schedule. See Miss. Code Ann. §71-3-15(3) (Rev.
2000).
12.9.a. WHERE TO OBTAIN FEE SCHEDULE
The Fee Schedule has been amended by the MWCC several times since its first
implementation, and the latest version was adopted effective June 15, 2019.
http://www.sos.ms.gov/adminsearch/ACProposed/00024122b.pdf. It can be purchased at
https://orders.fairhealth.org/.
12.9.b. ISSUES ADDRESSED IN THE FEE SCHEDULE
The Fee Schedule is a comprehensive document spanning more than 400
pages. A discussion of every point included in the Fee Schedule is not the intent
of this publication, but a few important points and time frames will be
mentioned. The Fee Schedule addresses numerous issues including important
things such as, but not limited to:
• Rules/guidelines to provide and pay for medical treatment;
• Maximum reimbursement levels;
• Utilization review;
• Peer Review to determine medical necessity;
• Pre-certification;
• Procedures considered to be investigational and not reimbursable;
• Deposition/witness fees;

Page 81 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
• Medical report fees;
• Billing Guidelines;
• Impairment ratings;
• Out-of-state services;
• Authorized providers;
• Medical records requirements;
• Provider rights for reconsideration and dispute resolution; and
• Reimbursement requirements.
12.9.c. PRE-CERTIFICATION
One early distinction is important: utilization review companies provide
certification for proposed treatment while claims professionals provide approval
for those services to be rendered. The claims professional sometimes will be
called upon to overrule a pre-certification opinion. Care must be taken in
overruling an approval as denying procedures without a compelling and
legitimate reason when the pre-certification opinion favors approval can be fuel
for a bad faith lawsuit. Many claims organizations recognize the need to override
the pre-certification only when it is in favor of approving the procedure.
Under Fee Schedule Authorization/Pre-certification Rule I, specific
procedures requiring utilization review are listed to include;
a. Inpatient admissions;
b. Surgical procedures;
c. Repeat MRI and other similar studies;
d. Pain Management;
When a medical provider requests authorization to proceed with treatment,
initial review determination must be made within two (2) business days of
receiving the review request. Fee Schedule Authorization/Pre-certification Rule
IV A. If the Provider chooses to obtain an Employer’s Medical Exam (EME) in lieu
of pre-certification, notice of such election must be given to the Provider within
Page 82 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
the same 2-day period applicable to a utilization review.
Failure to follow the required timelines with an ultimate determination of
the requested treatment in favor of the provider could result in the imposition of
penalties, attorneys and expenses.
When an initial determination is made to certify the service, notification
shall be provided within at least one (1) business day or before service is
scheduled, whichever occurs first. If initial determination to certify is provided
by phone, written confirmation shall be provided within two (2) business days
thereafter.
12.9.d. APPEALS FOR DENIALS OF PRE-CERTIFICATION
When a determination is made to not certify the procedure, the ordering
medical provider should be notified by phone within one (1) business day with
written notification within one (1) business day thereafter. Written notification
must include the principal reason for determination not to certify and instructions
regarding how to complete an appeal.
The Medical Services Provider has the right to either an expedited or
standard appeal:
An expedited appeal is appropriate when denial of services interrupts
current treatment (i.e. the patient is in the hospital and additional days to stay in
the hospital are denied). The provider has right to an appeal response within
one (1) business day.
A standard appeal is just that: “standard”. It requires notification of the
decision regarding the appeal to the provider within twenty (20) days.
After this appeals process, if the payer and medical provider cannot agree
on the appropriate resolution of the dispute, either party can appeal to the Cost
Containment Division of the Commission within twenty (20) days following the
conclusion of the underlying appeal process described above.
It is important to note that failure to timely notify the medical provider of
the decision regarding the requested service shall be deemed an approval by the

Page 83 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
payer, and shall obligate the payer to reimburse the provider in accordance with
the fee schedule. Notification can be by mail, fax, email or phone (followed by
written notification), as long as provided within the applicable time periods set
forth in the Fee Schedule. As earlier indicated, failure to follow the required rules
and denying certification of procedures consistent with the Fee Schedule rules
can result in the imposition of penalties, attorneys and expenses.
12.9.e. RETROSPECTIVE REVIEW
The failure to obtain pre-certification shall not, of itself, result in denial of
payment for the services. Instead, the payer, if requested to do so by the
provider within one (1) year of the date of service, shall conduct a retrospective
review of the services, and if the payer determines that the services would have
been pre-certified if it had been timely sought, the payer shall reimburse the
provider according to the Fee Schedule, less a 10% penalty (computed as 10%
of the total allowed reimbursement). Fee Schedule General Rules IX. I.
12.9.f. PROVIDER’S RESPONSIBILITIES
The medical provider must file appropriate billing forms and necessary
supporting documentation within twenty (20) days of rendering services. The
required documentation is mandatory and must support medical necessity. Late
billings are subject to discounts (a onetime 10% discount if over sixty days late)
and penalties (not to exceed 1 ½% per month). Billing & Reimbursement Rule
II(B).
Providers must include with their bills the medical records supporting the
charges. Medical records must include:
• Office notes;
• Progress notes
• Lab, x-ray and diagnostic test results;
• Physical medicine evaluation and treatments;

Page 84 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
• Operative reports;
• Consult reports;
• Impairment rating (projected and actual);
• Anticipated MMI date.
A plan of care should be included and should address:
• The disability;
• Degree of restoration anticipated;
• Measurable goals;
• Specific therapies to be used;
• Frequency and duration of treatments to be provided;
• Anticipated return to work date;
• Projected impairment.
Facilities must submit:
• Admission History and Physical;
• Discharge summary;
• Operative reports;
• Pathology/lab reports;
• Radiology reports;
• Consult reports;
• Other dictated reports; and
• Emergency room records.
See Fee Schedule Billing and Reimbursement Rules I.
12.9.g. FEES FOR COPY EXPENSES
The above listed records are to be provided at no cost to the payer. Any
additional records requested may warrant a copy fee as follows: $20.00 for the
first 20 pages; $1.00 per page for pages 21—100; $0.50 per page for everything
thereafter. Added to these charges are 10% of the total charge for postage and
handling and an additional $15.00 for retrieving records stored off premises.

Page 85 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
There may also be up to 10% of this amount added for postage and handling,
and/or $ 15.00 for obtaining records from an off-the-premise site. These
charges apply regardless of the media/storage system used. In-patient
admissions are reimbursable at the same levels subject to a maxim reimbursable
allowance of $100.00 per admission. Charges for copies of x-ray films are
$10.00 per film. Providers should provide these records within 14 working days
of the request.
12.9.h. PAYER’S RESPONSIBILITIES
Properly submitted bills (with the required supporting documentation) must
be paid within thirty (30) days of receipt. If not fully paid within thirty days, the
provider is also entitled to be paid interest (not to exceed 1 ½% per month) and
penalties (a one-time 10% if over sixty days late). Fee Schedule Billing &
Reimbursement Rule III(D).
When part of a bill is disputed, the undisputed portion must be paid within
thirty days of receipt of the properly submitted bill with supporting
documentation. The Payer must notify the Provider of the basis for the dispute
within thirty days from its receipt of the bill.
12.9.j. EXPLANATION OF REVIEW
When any payment is made, an Explanation of Review (EOR) must
accompany the payment. When the Payer’s reimbursement differs from the
amount billed, the EOR must be provided within thirty days of receipt of the bill.
12.9.k. REQUEST FOR RECONSIDERATION
If the medical provider challenges the conclusion regarding the
reimbursable amount under the Fee Schedule, the medical provider must make a
written request for reconsideration within thirty days from its receipt of the EOR
or other written documentation evidencing the basis for the dispute.
Commented [l1]: Omitted from 2019 Update

Page 86 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
The payer must provide notification of its decision on the requested
reconsideration to the requesting party within thirty days after receipt of the
request for reconsideration. Fee Schedule Billing & Reimbursement Rule VI(C).
If the Payer finds that the Provider’s request for reconsideration is well
taken, the additional payment should be made within the same thirty day period
as notification of outcome mentioned above. The additional payment shall
include interest from original due date of payment and the additional 10%
penalty, if applicable.
Failure of the Provider to seek reconsideration within the established time
shall bar any further reconsideration of the bill or other issue unless the
Commission, for good cause, extends that time period; however, the time shall
never be extended by more than thirty additional days.
12.9.l. DISPUTE RESOLUTION
The Fee Schedule includes significant Dispute Resolution Rules to which the
readers are referred as all of the details are too cumbersome to be incorporated
into this summary. In brief summary, a request for resolution of a dispute may
be filed with the Cost Containment Division of the Commission. Following
review, the Cost Containment Division of the Commission shall render an
administrative decision.
An appeal to the Commission is permissible thereafter within 20 days of
the decision of the Cost Containment decision. Failure to timely request
Commission review shall bar further review. No extension of this time shall be
allowed. If no request for review to the Commission is filed, the parties to the
dispute shall have fourteen days thereafter to comply with the final decision of
the Cost Containment Division.
Unless permitted by the Commission to proceed pro se, all parties
participating in a Commission review of the Cost Containment Division are
required to be represented by an attorney licensed in Mississippi.

Page 87 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 13
VOCATIONAL REHABILITATION
Although Mississippi Law does not have mandatory vocational rehabilitation
for claimants, considerable focus on those issues occurs inasmuch as one of the
stated purposes of the Act is to assist claimants in “their rehabilitation or
restoration to health and vocational opportunity….” See Miss. Code Ann. §71-3-
1, (1972, as amended). Therefore, the Commission also focuses on vocational
rehabilitation, and the claims professional is encouraged to review the
information on the Commission WEB site regarding vocational rehabilitation at
http://www.mwcc.state.ms.us/#/frequentlyAskedQuestions. In addition, the
Mississippi Department of Rehabilitation Services, http://www.mdrs.state.ms.us/,
can offer assistance in dealing with rehabilitation issues.
In the event a claimant is enrolled in a vocational rehabilitation program,
the employer/carrier have an obligation to pay $25.00 a week for a maximum of
fifty-two weeks during the period of time a claimant is undergoing an approved
vocational rehabilitation program. That payment is in addition to compensation
benefits that are otherwise payable. Miss. Code Ann §§71-3-19 and 71-3-105,
(1972, as amended) and MWCC Rule 2-19.
13.1. USE OF VOCATIONAL REHABILITATION PROFESSIONALS
Vocational rehabilitation counselors and case managers are often used by
claims professionals to assist in finding post-injury employment possibilities for a
claimant to consider. In addition, vocational rehabilitation counselors are often
called as expert witnesses in the hearings on cases to offer opinions as to post-
injury employability.

Page 88 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 14
GENERAL ISSUES
14.1. SETTLEMENTS
Mississippi workers’ compensation claims can be settled; typically
settlements include a closure of medical as well as indemnity benefits. Miss. Code
Ann §71-3-29 (1972, as amended) is the statutory basis for a compromise
settlement. These settlements are often referred to as 9(i) settlements, a
reference to the original code section nomenclature when the law was first
passed. All settlements are subject to the approval of the Commission, and a
licensed Mississippi attorney must be retained by the employer/carrier to prepare
the proper paperwork and present the settlement to the Commission. For a
complete summary of the Commission’s requirements related to settlements, see
http://www.mwcc.state.ms.us/pdf/memotoattorneys.pdf.
A claimant does not have to have an attorney to settle his case. If he or
she is not represented, he/she will have to be interviewed by a Commissioner (or
an Administrative Judge) to make sure that the settlement is in the claimant’s
best interests. (See below regarding a change in procedure effective January 18,
2018). The settlement will not be approved if the MWCC finds that the settlement
is not accurately reported; is not completely understood by the claimant; or that
the settlement is not in the best interest of the claimant. The MWCC will approve
the settlement if the facts and settlement terms are accurately reported; the
claimant understands the settlement; and that it is in claimant’s best interest.
If the claimant travels to the Commission to have the settlement
considered, the employer/carrier are to pay claimant’s mileage expense to and
from the interview just as is paid for travel to and from medical treatment. See
Commission Rule 2.15.
Pursuant to a change in Commission Rule 2.15 effective January 18, 2018,
in a settlement involving an unrepresented Claimant, the settlements documents
Page 89 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
and supporting medical or other records must be filed with the MWCC before the
settlement conference at the MWCC is scheduled; after a review of the
documents and records, the MWCC will notify the attorney representing the
employer/carrier by e-mail that the settlement conference can be scheduled.
If an attorney represents a claimant, the interview of the claimant by the
Commission is not required. The Commission processes those settlements based
on the representations of the parties, through their attorneys, although
settlements are not automatically approved as the Commission will still make
sure that the settlement is in the best interest of Claimant.
If the claimant is a minor or is incompetent, the settlement might also
have to be considered by the Chancery Court so that an appropriate person who
is competent can be appointed to represent claimant in a fiduciary capacity
before consideration of the settlement by the Commission.
The Commission usually considers these types of settlements on Tuesdays
and Wednesdays. See Commission Rule 2.15 for additional details and rules
regarding settlements.
A settlement approved by the Commission can be set aside if it is
determined that the settlement was induced by fraud. There is also case law
supporting the proposition that a settlement can be set aside and the case
reopened for other reasons, and fortunately those circumstances rarely occur.
As discussed in Section 9.8, if there is a spousal or child support lien
pending at the time of any settlement, the employer/carrier have the obligation
to withhold proceeds necessary to satisfy the support lien and to pay those
directly to the Mississippi Department of Human Services, or, in some
circumstances, directly to the obligee. See the notice regarding this issue that is
posted on the website of the Commission at
http://www.mwcc.state.ms.us/pdf/Child%20Support%20Web%20Policy.pdf.

Page 90 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
14.2. LUMP SUM PAYMENTS
A lump sum payment, as contemplated by Miss. Code Ann §71-3-37(10)
(1972, as amended), is often confused with a “settlement”. Some refer to it as a
"13(j) settlement, but the lump sum payment is neither a settlement nor an
adjudication of any liability. It is only a vehicle for paying, in a lump sum,
permanent disability or death benefits awarded following a hearing or agreed to
be paid on a form B-18. Recall that benefits are to be paid bi-weekly, unless
otherwise ordered by the Commission, and this is the vehicle used for getting
authority to pay benefits in a partial or full lump sum. To obtain an Order
Authorizing Lump Sum Payment, the claimant would file a B-19, Application for
Lump Sum payment, and the Commission would consider that application with
the only issue being whether or not the lump sum payment would be in the
claimant’s best interests.
The Commission on Tuesdays or Wednesdays of each week usually
considers lump sum payment applications. See Commission Rule 2.15 for other
provisions regarding lump sum payments.
PRACTICE NOTE: Remember that a 13(j) lump sum payment is not a
settlement of anything. It is only a way to pay in a lump sum weekly benefits
that were either awarded by an Administrative Judge or voluntarily set up to be
paid as shown on a B-18. A compromise 9(i) settlement discussed in section
14.1 above where medical is left open is possible, but that is not a 13(j) lump
sum settlement.
14.3. SUBROGATION/CLAIMS AGAINST THIRD PARTIES
Under Mississippi Law, a claimant (or his dependents in a death claim) has
a right to pursue a claim for workers’ compensation benefits and a claim against
a third party responsible for causing the injury. See Miss. Code Ann. §71-3-71
(1972, as amended). That third-party claim would be pursued in a court of
general jurisdiction and not before the Commission. When a third-party suit is

Page 91 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
filed, the employer/carrier is authorized by law to intervene in the suit, and a
claims professional should retain legal counsel to pursue the intervention. If
there is a recovery from the third party, it is distributed as follows: the costs of
collection (including claimant’s attorney’s fees) are paid first; the
employer/carrier are reimbursed for their compensation and medical expense
payments on the claim; and any balance thereafter belongs to the claimant. The
employer/carrier are also entitled to a credit against any additional liability they
might have to claimant in the workers’ compensation claim up to the amount of
the balance that was paid to the claimant over and above the costs of collection
and the amount used to reimburse the employer/carrier.
The employer/carrier has the right under the statute to pursue the claim
against the third party on its own behalf and in the name of the claimant, but
that rarely happens since the employer/carrier’s claim is heavily dependent on
claimant’s cooperation in the suit. There is a three-year statute of limitations on
most causes of action that could be brought against a third party in these
circumstances. For intentional torts such as an assault, however, the statute of
limitations is one year.
Any settlement of the third party claim is subject to the approval of the
Commission, unless suit has been filed against the third party. In the event the
claimant has filed suit against the third party, the settlement is subject to the
approval of the court in which the suit against the third party is pending. The
established Commission procedures relating to settlements must be followed
regarding the settlements of third party claims:
http://www.mwcc.state.ms.us/pdf/memotoattorneys.pdf. It is also important to
note that in a third party settlement, the third party must have a Mississippi
attorney sign the documents on its behalf; it would be deemed an unauthorized
practice of law for the claims professional to sign the documents.
Some claimant’s counsel will argue that the employer/carrier should not be
reimbursed in a third-party recovery until the claimant is “made whole”, but the
Mississippi Supreme Court specifically rejected that argument in Federated

Page 92 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Mutual Insurance Company v. McNeal, 943 So.2d, 658 (Miss. 2006).
PRACTICE NOTE: In some cases, the employer/carrier may be called upon
to compromise their lien in the third-party claim. Sometimes it is prudent to do
so, particularly where the liability of the third party is doubtful or when there are
inadequate assets with which to satisfy the entire claim. A pragmatic approach
in dealing with such issues is usually the better course to follow.
14.4. MEDICARE’S INTERESTS
The Mississippi Workers’ Compensation Commission has not adopted any
rules specifically dealing with the Medicare Secondary Payer Statute, 42 USC
1395(y), a statute designed to keep the nation’s Medicare system viable by
requiring that any other entity who is liable for medical expenses, such as a
workers’ compensation insurance carrier, pay for that medical expense before
Medicare is responsible for that payment. Approval of a settlement of a workers’
compensation claim by the Center for Medicare and Medicaid Services (CMS) is
required: (a) on all workers’ compensation settlements involving a Medicare
beneficiary where the settlement amount is more than $25,000; and, (b) where
the claimant has a reasonable expectation that he will become a Medicare
Beneficiary within thirty months from the date of the settlement AND the
settlement is for more than $250,000. These factors are referred to by CMS as
its “workload management thresholds” and, if the case meets these thresholds,
CMS will be asked to approve a Medicare Set-Aside Arrangement. A Medicare
Set-Aside Arrangement provides or “sets aside” a specified amount of the
settlement proceeds to cover claimant’s future medical expenses for which
Medicare would otherwise be responsible.
Therefore, the settlement of a workers’ compensation claim will often
involve approval by the Commission and by the CMS. There is no requirement as
to which entity must approve the settlement first; as such, that decision is left to
the agreement between the claims professional and claimant.

Page 93 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Another important issue involving Medicare concerns payments already
made on claimant’s behalf by Medicare for the medical problems associated with
the claim. The CMS calls these “conditional payments” that were made pending
reimbursement by the responsible party such as a workers’ compensation
insurer, and those conditional payments will have to be considered and handled
independently of the Medicare Set-Aside Arrangement for claimant’s future
medical expenses.
14.5. MEDICAID’S INTERESTS
Medicaid is a “need based” system that sometimes pays medical expenses
for people who have been injured on the job. It is administered by the State of
Mississippi, and payments made by the Division of Medicaid for medical problems
which are related to an on-the-job injury are intended under the law to be the
responsibility of the employer/carrier. Medicaid is supposed to be notified when
a Medicaid recipient files a claim and Medicaid may intervene in the action. A
claimant who fails to cooperate with the Division of Medicaid in its claim against
someone else liable for payment of the medical expenses, such as an
employer/carrier in a workers’ compensation claim, or who fails to pay to the
Division proceeds received by claimant from a “third-party” as provided by the
Mississippi Medicaid Law, will become ineligible for Medicaid benefits. Miss. Code
Ann. §43-13-307 (1972, as amended).
Unlike the Medicare Secondary Payer Statute, discussed in the previous
section, the Mississippi Statutes which authorize and outline the Medicaid system
in Mississippi do not appear to impose any duties on parties to a workers’
compensation settlement relating to medical expenses for treatment to be
obtained in the future. However, Medicaid has the right to recover its payments
already made for a claimant’s medical services out of a recovery in a workers’
compensation and a third-party claim. Miss. Code Ann. §43-13-125 (1972, as
amended). Failure to honor Medicaid’s subrogation rights by an employer/carrier

Page 94 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
could permit Medicaid to recover double the benefits paid by Medicaid and costs
of collection. Miss. Code Ann. §43-13-315 (1972, as amended).
PRACTICE POINT: The claims professional would be well served to
ascertain whether a claimant is a Medicaid beneficiary prior to the settlement of
any claim in order to insure the finality of the settlement. If the claimant is a
Medicaid recipient at the time of settlement, no compromise is binding upon the
Medicaid Division unless ratified and/or approved by the Division. Miss. Code
Ann. §43-13-125(3) (1972, as amended).
14.6. SOCIAL SECURITY OFFSETS
The Mississippi Workers’ Compensation Law is silent regarding Social
Security benefits. As such, a claimant’s entitlement to Social Security benefits
does not affect the workers’ compensation benefits payable. However, according
to Section 224 of the Social Security Act, if a claimant receives workers’
compensation benefits and Social Security benefits, the Social Security benefits
will be reduced under rules adopted by the Social Security Administration.
14.7 FRAUD
The pursuit of, or defense of, a claim without reasonable grounds is
contrary to public policy and is discouraged in several ways. There are both civil
and criminal remedies and penalties that can be brought into play.
Under Miss. Code Ann. §71-3-59 (1972, as amended), costs of
proceedings, including attorney’s fees, can be assessed against the party who
institutes or continues a claim without reasonable grounds. Further, under
paragraph 2 of that code section, and in addition to the costs referenced above,
a civil penalty not to exceed $10,000 may be assessed against the party, the
attorney advising or assisting the party, or both. This administrative remedy is
vested with the Commission.

Page 95 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Miss. Code Ann. §71-3-69 (1972, as amended) provides that it is a felony
to make a false or misleading statement or representation to obtain or wrongfully
withhold workers’ compensation benefits, punishable by a fine not to exceed
$5000.00, or double the value of the fraud, whichever is greater, or by
imprisonment not to exceed three years, or both fine and imprisonment.
The Mississippi Attorney General operates a Fraud Unit that can be of
assistance in investigating and prosecuting suspected fraud. Additional
information regarding those efforts is available from the Office of the Attorney
General, http://www.ago.state.ms.us/.
14.8 CLAIMANT’S ATTORNEY FEES
Fees due an attorney representing a claimant are addressed in Miss.
Code Ann. §71-3-63 (1972, as amended) and Commission Rule 2.12. Under
that statute and rule, the attorney is obligated to inform the Commission of
his/her representation of a claimant and get the approval of the Commission
for any fee in excess of $200.00. The Commission cannot approve a fee in
excess of 25% of the recovery, but a court on appeal may approve a higher
fee. Those fees are paid by the claimant out of a recovery and are not in
addition to the benefits due the claimant.
For injuries on or after July 1, 2012, an attorney is not entitled to
recover a fee from benefits voluntarily paid for temporary or permanent
disability; however, any settlement negotiated by the attorney is not
considered a voluntary payment under this provision.
An amendment to MWCC Rule 2.12 effective January 18, 2018 provides
that the allowable 25% attorney’s fee in any proposed settlement must be
calculated only on the amount of the settlement that is not designated for a
Medicare Set Aside arrangement. If, however, in cases where there are no
indemnity benefits payable, the Commission may consider a claimant’s
attorney’s request for payment of attorney fees on a quantum meruit basis.

Page 96 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 15
LITIGATION PROCEDURES
The litigation of a claim for benefits is not a matter handled in the courts of
Mississippi, but instead takes place pursuant to Rules of the Mississippi Workers’
Compensation Commission. The trial is held before an Administrative Judge who
is an employee of the Commission. Even in subsequent appeals, there is not a
new trial where additional evidence is offered.
A claimant controverts a case by filing a Petition to Controvert, Form B-
5,11. The Commission provides written notice of that filing to the
employer/carrier. In cases in which no indemnity or medical benefits have been
paid, a claimant is required to file medical records supporting the claim along
with the Petition to Controvert; however, if a statute of limitations is about to
run, claimant shall file them within 60 days of the filing of the Petition.
The employer/carrier's Answer, B-5,22, is due within twenty-three days of
the date the Commission mails the Petition to Controvert to the employer/carrier,
and its cover letter will show the date that the Answer is due. The Answer
should be filed by a licensed Mississippi attorney, and should contain any
affirmative defenses that the employer/carrier intend to raise.
The rules of the Commission provide that discovery shall be completed
within one hundred twenty days from the date of notice from the Commission
that the case has been placed on the active docket. Discovery may include
interrogatories, depositions, requests for production of documents, and requests
for admissions.
Either party can file prehearing motions to be heard before the
Administrative Judge. Motions may be heard in person or by telephone
conference between the parties and the Judge on pre-established motion days or
at the discretion of the Administrative Judge. If a party desires oral argument,
the party should notice the motion for any motion day at least five calendar days
before the motion day. Emergency hearings can be scheduled in certain

Page 97 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
circumstances consistent with statutory notice requirements and Rules.
Within fifteen days of the expiration of the discovery period, claimant is
required to file a properly completed prehearing statement. The
employer/carrier have fifteen days after the filing of claimant’s properly
completed prehearing statement to file a properly completed prehearing
statement. These deadlines can be, and often are, extended. The claimant’s
failure to timely file a prehearing statement may result in the dismissal of the
case. Failure of the employer/carrier to file a timely and complete prehearing
statement can result in a unilateral setting of the case by the claimant. The rules
are designed to have a controverted case tried to a conclusion before the
Administrative Judge within about six months from the date of controversion,
although from a practical standpoint, that rarely occurs.
Generally a prehearing statement contains the following documentation:
(1) claimant’s education and employment history; (2) a description of the
accident and injuries which are alleged; (3) dates and amounts of indemnity
benefits paid; (4) the medical treatment and maximum medical improvement
date; (5) permanent partial impairment rating and restrictions, if any; (6) all
affirmative defenses; (7) the details of disputes regarding unpaid medical
expenses; (8) the claimant’s post-injury job search efforts; (9) the claimant’s
post-injury employment details; (10) any reports regarding vocational efforts
and labor market surveys; (11) stipulations; (12) hearing exhibits; and (13) a
proposed witness list.
After the Pre-Hearing Statements are filed, the case is set for hearing
before the Administrative Judge. The hearing is usually held at one or more
central locations with the territory of each Administrative Judge. The claims
professional handling the claim is required to be present or available to the
Commission by phone during the entirety of the hearing. The evidentiary record
is created at that hearing, and, although the Administrative Judge is not bound
by technical or formal rules of procedure or evidentiary rules, the hearing has the
appearance of a trial, except there is no jury present. The Administrative Judge

Page 98 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
does not usually announce a decision at the hearing but will usually issue a
written order that includes an itemization of the issues, analysis of evidence,
findings of fact, conclusions of law, and an award or denial of benefits.
Depending on the judge and the complexity of the case, the Judge’s decision
may be received anywhere between a week and six months after the hearing.
Once the Administration Judge’s order is written, it becomes final unless,
within twenty days of the date of the decision, either side may file an appeal to
the Full Commission. The three Commissioners do not generally hear new
evidence sitting in their appellate capacity. The full Commission reviews the
record, considers the briefs of the parties, hears oral arguments (if requested by
the parties and granted by the Commission), and then by written Order either
affirms, reverses, or amends the Administrative Judge's decision.
Within 30 days of the Commission's Order, either party has the right of
appeal that decision to the Mississippi Supreme Court. The Mississippi Supreme
Court, in its discretion, will either hear the appeal or assign it to the Court of
Appeals for final disposition. From a practical standpoint, most workers’
compensation appeals do get referred to the Court of Appeals. This is an
appellate review and not a trial de novo, and the appeals court is not permitted
to disturb the Commission's findings if its findings are supported by substantial
evidence. After the decision by the Court of Appeals, the Mississippi Supreme
Court can thereafter review the Court of Appeals’ decision by granting certiorari.
Page 99 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 16
MEDIATION
Mediation is not mandatory on any case but is permissible by agreement of
the parties. Members of the Workers’ Compensation Section of the Mississippi
Bar Association often serve as mediators, and many of them agree to donate a
part of the fees paid to them to the Kid’s Chance Scholarship Fund, a college
scholarship program designed to assist the children of workers who were
significantly injured or killed on the job. It is not mandatory that Kid’s Chance
Mediators be used for mediation and the parties are free to choose any qualified
mediator.
That said, the panel of mediators approved by the Kids’ Chance program
have received specific training in mediation and were selected based on their
extensive experience with Mississippi workers’ compensation law. Since its
inception the mediation program has successfully helped parties reach
compromise resolution of thousands of claims.
The decision to mediate and the decision to agree upon settlements is
always voluntary. Mediation of workers’ compensation claims – like most
litigation – is strongly encouraged and recommended by the judiciary and the
Mississippi Workers’ Compensation Commission.

Page 100 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Chapter 17
BAD FAITH CLAIMS
17.1. WHAT IS BAD FAITH?
In Mississippi, courts have recognized a separate cause of action against
employers, carriers, and third-party administrators for a “bad faith” denial of a
claim—a potentially dangerous issue that should not be taken lightly. “Bad faith”
breach of contract is often described as the willful or intentional denial of a claim,
or a part of a claim, without reasonable grounds, where the denial reflects an
intent to injure the claimant or was made in reckless disregard of the claimant’s
rights. Southern Farm Bureau Casualty Ins. Co. v. Holland, 469 So.2d 55, 59
(Miss. 1985). The cause of action can lie against the employer as well as the
carrier. Luckett v. Mississippi Wood Inc., 481 So. 2d 288 (Miss. 1985).
Damages recoverable in such a suit are not a part of the workers' compensation
system and the cases are not tried before the Commission but in state or federal
court. Mississippi Power & Light Co. v. Cook, 832 So. 2d 474 (Miss. 2002)
illustrates the exposure in such cases because the jury awarded $150,000 for
actual damages, $5,000,000 for punitive damages and a large attorney’s fee. On
appeal, the punitive award was somewhat reduced but bad faith cases can be
very expensive due to the exposure to a punitive damage award. Cook, 832
So.2d 474 (Miss. 2002).
AmFed Companies, LLC v Jordan, 34 So3d 1177 (Miss. App. 2009), cert
granted, 31 So.3d 1217 (Miss. 2010) is a recent example of a bad faith
determination and verdict where the thrust of the alleged wrongdoing was a
delay of about 11 weeks in making a payment.
Mississippi imposes an affirmative duty on employers, carrier and third-
party administrators to perform a reasonable and prompt claim investigation.
Bankers Life & Cas. Co. v. Crenshaw, 483 So. 2d 254 (Miss. 1985). What
constitutes a “reasonable” investigation will vary on a case-by-case basis but

Page 101 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
will typically require that all relevant witnesses be interviewed and all relevant
documents (especially relevant medical records) be obtained. Eichenseer v.
Reserve Life Ins. Co., 682 F. Supp. 1355 (N.D. Miss. 1988). See also,
Crenshaw at 271-73. The claim investigation should allow for a realistic
evaluation of the claim and decision. If the claim is owed, benefits should be
promptly paid. If the claim is to be denied, then there is an affirmative duty
to honestly advise the claimant why the claim has been denied. Even after a
claim is denied there is an ongoing duty to reevaluate and reconsider if new
evidence develops.
Unfortunately, mistakes can and will happen. Claims personnel are
human and it is important to remember that clerical errors and inadvertence
do NOT represent bad faith conduct. Universal Life Ins. Co. v. Veasley, 610
So. 2d 290 (Miss.1982). General negligence, unaccompanied by malice, does
not rise to the level of bad faith conduct. Consolidated Am. Life Ins. Co. v.
Touche, 410 So.2d 1303 (Miss. 1982). Moreover, as mentioned throughout
these materials, seeking and relying on the advice of counsel is not only good
claim investigation but can also provide protection from a subsequent punitive
damage claim if the claim decision is incorrect. Murphree v. Federal Ins. Co.,
707 So.2d 523 (Miss.1997). Reliance on objectively reasonable legal advice
in making a claim decision will almost always prevent a conclusion that the
denial was make in bad faith.
Punitive damages, when awarded, are designed to punish the wrongdoer
and to set an example to keep others from committing a similar wrong. Effective
in 2004, statutory limits were imposed on punitive damages based on the net
worth of the defendant. Miss. Code Ann §11-1-65 (1972, as amended).
Nevertheless, modest punitive damage awards can be staggering in comparison
to the relatively limited benefits involved in most compensation claims. Punitive
damages awards, and the potential for such in bad faith causes of action, cannot
be overemphasized.

Page 102 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
The potential for bad faith exposures can be reduced through a focus on
timely, informed, and reasonable claims handling practices. Unnecessary delays
in the processing of claims are the primary basis for such suits, and legitimate
disputes can become disastrous bad faith suits by the simple failure to follow
through on the completion of a prompt and thorough investigation so that an
informed and timely decision can be made.
17.2. SUGGESTIONS FOR AVOIDING BAD FAITH
To avoid “bad faith” suits, it is recommended that the claims professional
(1) encourage prompt reporting of injuries; (2) act with a sense of urgency in the
proper handling of the claim; (3) complete a prompt and thorough investigation
of the claim; (4) have a legitimate and arguable basis for any denial; (5) act with
a commitment to competent, rational, and objective professionalism; and (6)
seek advice of counsel before issuing a denial.
Some other common-sense points to consider include the following:
A. Do not write disparaging comments about the claimant or his claim
that could be considered as anything less than an unbiased professional analysis
of the facts and the application of law to those facts.
B. Be open minded and objective in analyzing the law and the facts on
every claim. Thinking the answer to a question is “always or never this or that”
is generally a path that can become problematic.
C. Consider having committee reviews that include the adjuster,
supervisor, manager, and defense attorney before issuing a denial. Again,
advice of counsel is a powerful defense to bad faith cases and should be part of
the claim decision process.
D. Avoid delays in the processing of each claim. Unexplained delays in
processing benefits and failing to communicate issues can lead to problems.
With a focus on quality claims handling practices rooted in rational and
objective professionalism, the claims professional will avoid the pitfalls of “bad
faith” allegations.

Page 103 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
EPILOGUE
This Mississippi Workers’ Compensation Claims Guide is designed to
provide claims and other professionals with an outline of the basic provisions in
the Mississippi Workers’ Compensation law, and every issue cannot be
thoroughly addressed. No guide of this nature should be treated as a substitute
for advice from competent legal counsel, so every professional is encouraged to
consider seeking such advice when confronted with an unusual situation or if
there is uncertainty as to the correct steps that should be taken on a claim.
To reiterate what was stated at the outset of this Guide, it is not to be
construed as an official publication of the Mississippi Workers’ Compensation
Commission. Cases are usually fact intensive and the law is continually evolving,
and it is not the intent for this guide to be construed as the Commission’s official
pronouncement of the law on any issue.
The Mississippi Workers’ Compensation Educational Association, Inc.
(MWCEA), the publisher of this Guide, is a non-profit entity whose purposes
include the dissemination of information related to Mississippi Workers’
Compensation Law and the education of those interested in that area of the law.
The MWCEA does not provide legal advice or services, nor is it involved in the
adjudication of any disputes. The MWCEA may be contacted by mail at Post
Office Box 13508, Jackson, Mississippi 39236; by email at info@mwcea.com; or
by phone at 601.987.4200 to speak to the Chairman of the Mississippi Workers’
Compensation Commission.

Page 104 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019
Mississippi Workers’ Compensation Educational Association, Inc.
Board of Directors, July 2019
Andre F. Ducote*
President
(601) 949-3388
aducote@forthepeople.com
T. G. Bolen, Jr.*
Vice President
(601) 853-1911
tgbolen@markowwalker.com
Tina O’Keefe*
Immediate Past President
(662) 357-1185
TOkeefe@goldstrike.com
Barbara Oltremari
Board Member
(601) 720-8091
barbaraoltremari@gmail.com
Steven H. Funderburg
Past President
(601) 355-5200
sfunderburg@jfsplawfirm.com
Molly Staley
Board Member
(601) 987-8200
mstaley@capitalortho.com
Becky Hillhouse
Past President
(769) 300 0334
beckyhillhouse@eains.com
*Executive Committee

Page 105 of 109
A publication of the Mississippi Workers’ Compensation Educational Association, Inc.
©2019