
May 2020
Direct Primary Care: Evaluating a New
Model of Delivery and Financing
Health Care Cost Trends
2
Copyright © 2020 Society of Actuaries
Direct Primary Care: Evaluating a New
Model of Delivery and Financing
Caveat and Disclaimer
The opinions expressed and conclusions reached by the authors are their own and do not represent any official position or opinion of the Society of
Actuaries or its members. The Society of Actuaries makes no representation or warranty to the accuracy of the information.
This report was prepared by Milliman exclusively for the use or benefit of the Society of Actuaries for a specific and limited purpose. The report used data
from various sources, which Milliman has not audited. Any third party recipient of this report who desires professional guidance should not rely upon
Milliman’s report, but should engage qualified professionals for advice appropriate to its own specific needs.
Copyright © 2020 by the Society of Actuaries. All rights reserved.
AUTHORS
Fritz Busch, FSA, MAAA
Consulting Actuary
Milliman, Inc.
Dustin Grzeskowiak, FSA, MAAA
Consulting Actuary
Milliman, Inc.
SPONSORS
Society of Actuaries
Research Expanding Boundaries (REX)
Pool
Erik Huth, FSA, MAAA
Principal and Consulting Actuary
Milliman, Inc.

3
Copyright © 2020 Society of Actuaries
CONTENTS
1. Executive Summary ............................................................................................................................................... 5
Literature Review ........................................................................................................................................................... 6
Market Survey ................................................................................................................................................................ 7
Case Study ...................................................................................................................................................................... 7
2. Background ........................................................................................................................................................... 9
Current State of Primary Care ....................................................................................................................................... 9
Milliman DPC Research ................................................................................................................................................ 10
3. Overview of DPC ................................................................................................................................................. 12
Definition and Common Features ............................................................................................................................... 12
Key Findings from Market Survey ............................................................................................................................... 14
4. Summary of DPC Literature Review ..................................................................................................................... 17
Overview ....................................................................................................................................................................... 17
Selection Criteria .......................................................................................................................................................... 17
Summary of Existing Literature ................................................................................................................................... 17
Overview of DPC.............................................................................................................................................. 18
Cost Outcomes ................................................................................................................................................ 19
Gaps in Existing DPC Research .................................................................................................................................... 22
5. Overview of Case Study....................................................................................................................................... 23
Study Structure ............................................................................................................................................................ 23
Study Goals ................................................................................................................................................................... 23
Data Description .......................................................................................................................................................... 24
Exposure Measures ......................................................................................................................................... 24
Cost Measures ................................................................................................................................................. 25
Benefit Coverages............................................................................................................................................ 25
6. Case Study Findings ............................................................................................................................................. 27
Population Differences ................................................................................................................................................ 27
Demographics .................................................................................................................................................. 27
Risk Selection and Morbidity ....................................................................................................................................... 28
Overall Demand for Health Care Services .................................................................................................................. 28
Emergency Department Visits ..................................................................................................................................... 31
Inpatient Hospital Admissions ..................................................................................................................................... 32
Total Employer Costs (DPC ROI) .................................................................................................................................. 32
7. Case Study Generalized Actuarial Framework for Funding Employer DPC Options .............................................. 36
Development of Estimated DPC FFS Claim Cost Savings ........................................................................................... 36
Overall DPC FFS Claim Cost Savings ............................................................................................................................ 41
Development of DPC Membership Fee Schedule ...................................................................................................... 41
Other Considerations for Employers Considering a DPC Option............................................................................... 43
8. Case Study Discussion and Limitations ................................................................................................................ 46
Discussion ..................................................................................................................................................................... 46
Limitations .................................................................................................................................................................... 47
Sample Size ...................................................................................................................................................... 47
Lack of Quality Measures ................................................................................................................................ 47
Variability in DPC ............................................................................................................................................. 48
Data Quality ..................................................................................................................................................... 48
DPC Practice Structure .................................................................................................................................... 49
Reliance 49

4
Copyright © 2020 Society of Actuaries
9. Case Study Data Sources ..................................................................................................................................... 50
Administrative Medical Claims .................................................................................................................................... 50
Administrative Prescription Drug Claims .................................................................................................................... 50
Health Plan Enrollment ................................................................................................................................................ 50
Benefit Plan Design ...................................................................................................................................................... 50
10. Case Study Methodology ................................................................................................................................... 52
Analytic Data Processing.............................................................................................................................................. 52
Milliman Health Cost Guidelines Grouper (HCG Grouper)............................................................................ 52
Milliman GlobalRVUs (GlobalRVUs) ................................................................................................................ 52
Milliman Advanced Risk Adjusters (MARA) .................................................................................................... 52
Actuarial Methodology ................................................................................................................................................ 52
Cohort Selection........................................................................................................................................................... 53
Metric Selection ........................................................................................................................................................... 54
Risk Adjuster ................................................................................................................................................................. 55
Statistical Analysis ........................................................................................................................................................ 56
11. Lessons Learned/Future Research ..................................................................................................................... 56
Acknowledgments .................................................................................................................................................. 57
Appendix A: Articles Included in Literature Review ................................................................................................. 58
Definitions of DPC ........................................................................................................................................................ 58
Overview of DPC .......................................................................................................................................................... 61
Cost Outcomes ............................................................................................................................................................. 68
Regulatory Considerations .......................................................................................................................................... 77
Provider Experience ..................................................................................................................................................... 81
Patient Access .............................................................................................................................................................. 83
Appendix B: Full Market Survey Results .................................................................................................................. 86
Appendix C: Additional Development Detail for Milliman Advanced Risk Adjusters (MARA) ................................... 97
About the Society of Actuaries ................................................................................................................................ 98

5
Copyright © 2020 Society of Actuaries
Direct Primary Care: Evaluating a New Model
of Delivery and Financing
1. Executive Summary
Primary care is a vital and even foundational component of any health care system. Primary care physicians (PCPs)
are the front line of health care and are often the entry point for patients needing care. How often a patient accesses
primary care, and the quality of that care, can have significant impacts on downstream costs and patient health
outcomes. However, while PCPs are almost universally acknowledged as essential to achieving the health care Triple
Aim of providing high-quality care, at lower cost, with improved patient experience, many health care experts describe
the current state of primary care as being in crisis. This crisis is characterized by physician burnout, large PCP patient
panels, low pay for PCPs relative to other physician specialties, increased administrative burden, longer work hours
without increased reimbursement, an increased risk of mental health conditions and suicide, and ultimately a PCP
shortage relative to market demand.
Direct Primary Care (DPC) is an approach to delivering and financing primary care that attempts to respond to many
of these challenges. The DPC practice model is relatively new and still evolving, and there is no single accepted
definition of what constitutes a DPC practice. However, the most commonly used definition is as follows:
DPC physician practices are those that:
1. Charge patients a recurring—typically monthly—membership fee to cover most or all primary care-related
services.
2. Do not charge patients per-visit out-of-pocket amounts greater than the monthly equivalent of the retainer
fee.
3. Do not bill third parties on a fee-for-service (FFS) basis for services provided.
Other key features characterizing much of the DPC delivery model include:
• Contracting. DPC practices typically do not contract with insurers, government payers, or third-party
administrators (TPAs). DPC practices typically only contract directly with patients or with self-insured
employers.
• Recurring fee. The majority of DPC practice revenues typically come from monthly or annual DPC
membership fees, generally ranging from $40 to $85 per person per month.
• Smaller patient panels. DPC practices usually have fewer patients than traditional primary care practices,
typically fewer than 1,000 and most often around 200 to 600.
• Expanded patient access. Due primarily to smaller patient panels, members of a DPC practice have better
access to their PCP. This improved access manifests itself in longer-duration office visits, same-day or next-
day appointments, text or phone-based provider contact, and occasionally PCP home visits.
• Longer office visits. The typical length of an office visit for a traditional primary care practice is around 13 to
16 minutes. A significant portion of this time is typically not face time, because coding and documenting
electronic health records (EHRs) pressures keep physicians behind the computer screen. By contrast, for DPC
practices, office visits average around 40 minutes but can vary based on the patient’s need.

6
Copyright © 2020 Society of Actuaries
• Reduced patient cost sharing. Most DPC practices do not charge any cost sharing for services covered under
the DPC membership fee. Proponents of the model contend this improves care, because financial barriers
are often the cause of patients missing important follow-up visits.
The DPC financing and delivery model provides an alternative to traditional FFS-based primary care models, and
proponents of the DPC model claim that it greatly improves the patient-doctor relationship, reduces the
fragmentation of patient care, and improves both personal and professional satisfaction for physicians. Moreover,
DPC proponents also argue that this alternative primary care arrangement generates systemwide reductions in health
care utilization including hospitalization rates, emergency department usage, unnecessary radiology and diagnostic
tests, and specialist care, leading to broad-based health care cost savings.
Not surprisingly, DPC has its critics, who contend that any observed reductions in utilization or health care costs along
with membership in a DPC practice are either aberrant, based on small study sizes, or are driven by patient selection
(i.e., healthier patients choose DPCs and thus have lower costs than traditional patients). Critics also charge that the
model is not scalable to the public at large and exacerbates the physician shortages issue.
The Society of Actuaries (SOA) commissioned Milliman to develop this report to provide health care stakeholders—
patients, payers, policymakers and actuaries—with a comprehensive description of DPC as well as an objective
actuarial evaluation of certain claims made about the DPC model of care. We utilized three primary research
methodologies to develop this report: 1) a literature review, 2) a market survey of DPC practices, and 3) an
employer case study where we applied an actuarial methodology to evaluate certain cost and utilization outcomes
for patients enrolled in a DPC option. In addition to the formal methodologies presented in this paper, we also
conducted one-on-one interviews with 10 PCPs practicing under the DPC model to provide us with firsthand
background information and context for the key findings from our primary research methodologies.
Literature Review
Our literature review identified 36 relevant articles for our report and an additional seven sources providing definitions
of DPC. While the identified articles provided useful qualitative information relating to the DPC model of care, we
identified several quantitative gaps in the existing literature. Specifically, existing literature on DPC does not include
the following:
• A comprehensive survey of DPC practices to provide a landscape of the current DPC market
• A comparison of DPC patients versus non-DPC patients to determine characteristic differences between
patients choosing to enroll in DPC
• An actuarially adjusted comparison of cost, quality and utilization rates between patients enrolled in DPC and
patients who are not
• An actuarially adjusted return-on-investment (ROI) determination for an employer-based DPC program to
determine whether total FFS claim cost savings for enrolled patients offsets the cost of recurring DPC
membership fees
• A breakout of DPC results for chronically ill versus nonchronically ill patients
• A qualitative review of nondata-driven aspects of DPC such as provider engagement, patient engagement
and increased patient-provider face time
• A longitudinal study that measures whether DPC “bends the cost curve” in health care costs per patient over
time

7
Copyright © 2020 Society of Actuaries
Market Survey
Our DPC market survey was completed by about 200 DPC physicians, with most responding to all questions; we believe
that this sample size represents approximately 10% to 20% of all physicians currently practicing in a DPC setting.
Key findings from this survey included:
• The primary motivators for physicians choosing to operate a DPC practice were the “potential to provide
better primary care under a DPC model” (96%), “too little time for FFS visits” (85%), and “too much FFS
paperwork to complete” (78%). Just 10% of physicians indicated that the “potential to earn more under DPC”
was a primary motivator.
• The average per-person monthly DPC membership fees reported in the survey were $40 for children and
ranged from $65 to $85 for adults, depending on age. Most DPC practices do not charge a per-visit fee for
services covered under their DPC memberships (89%).
• The average reported current DPC patient panel size was 445, while the average target panel was 628. The
average ratio of the current to target DPC patient panel sizes was 70% (i.e., on average, the current DPC
patient panel was 30% below the target). For those DPC practices with a full DPC patient panel, the average
length of time to fill the panel was 21 months.
• Nearly all DPC physicians reported having better or much better “overall (personal and professional)
satisfaction” (99%), “ability to practice medicine” (98%), “quality of primary care” (98%), and “relationships
with their primary care patients” (97%) under a DPC model. Just 34% of DPC physicians reported having
better or much better “earnings as a PCP under a DPC model.”
• About 70% of respondents’ DPC practices were established in the last four years, indicating that the model
is growing in recognition and popularity but is still in its infancy.
Case Study
For our case study, we procured a longitudinal claims data set from an employer with a DPC option in its employee
health benefits plan. Members in the employer’s plan can elect to enroll in a traditional preferred provider
organization (PPO) style plan option, or they can choose to enroll in an option that includes a DPC membership, with
the employer covering the DPC membership fee. We applied various actuarial techniques in our evaluation of the
impact of the DPC option on cost and utilization.
We observed positive cost-related and utilization-related effects from the introduction of a DPC option in the
employer’s self-insured health benefits plan. About half of the members included in our analysis enrolled in the DPC
option, and the DPC option was associated with a statistically significant reduction in overall demand for health care
services (−12.64%) and emergency department usage (−40.51%) after controlling for differences in age, gender and
health status between the DPC and traditional cohorts. The DPC option was also associated with a lower inpatient
hospital admission rate (−19.90%), but the difference was not statistically significant due to the small number of
admissions during the two years analyzed. However, we also estimated that the introduction of a DPC option
increased total nonadministrative plan costs for the employer by 1.3% after consideration of the DPC membership
fee and other plan design changes for members enrolled in the DPC option.
We provided a generalized actuarial framework for funding employer DPC options. Our case study coupled with a
generalized actuarial framework show that implementing a DPC option may be financially viable for employers self-
insuring their health benefit plans but is heavily dependent on various employer-specific factors. Depending on three
factors—1) baseline level of claims costs in an employer’s plan; 2) how the DPC option is structured, including the
level of membership fees; and 3) the cost savings expected to be generated by the DPC delivery model—the
introduction of a DPC arrangement could be done on a cost-neutral basis or may potentially lead to overall cost savings
for the employer. The potential benefits to employers from the introduction of a DPC option may go beyond cost

8
Copyright © 2020 Society of Actuaries
considerations, however. A DPC option may give employees and dependents increased access to primary and urgent
care services, from the same provider at no cost, and may provide access to no-cost or low-cost basic labs and
prescription drugs as well. Employees may also have lower absenteeism rates, because DPC appointments can
generally be scheduled at almost any time and wait times at the office are usually shorter. Key challenges for
employers interested in offering a DPC option include the relatively limited number of DPC practices and the
geographic dispersion of employees and dependents.

9
Copyright © 2020 Society of Actuaries
2. Background
Current State of Primary Care
PCPs are often the entry point for patients needing care. How often a patient accesses primary care, and the quality
of that care, can have a significant impact on downstream costs and patient health outcomes.
1, 2
As clinicians, PCPs
are often treating illnesses, referring to specialists, prescribing medications or recommending diagnostic tests, just to
name a few responsibilities. Unlike specialists, who typically focus on specific body systems and related disease states,
PCPs routinely triage a variety of cases involving multiple body systems and overlapping symptoms. Moreover, PCPs
also often serve their patients in other more interpersonal roles, such as educator and trusted advisor, care
coordinator and health care system advocate. Optimally, a longitudinal and direct patient-physician relationship
should characterize primary care.
While almost universally acknowledged that PCPs are essential to achieving the health care Triple Aim of high-quality
care, lower cost and improved patient experience,
3
many PCPs and other health care experts describe the current
state of primary care as being in crisis.
4
This crisis is characterized by:
• Burnout. In their 2018 Journal of Internal Medicine article, C.P. West et al. define physician burnout as “a
work-related syndrome involving emotional exhaustion, depersonalization, and a sense of reduced personal
accomplishment.”
5
We note in particular that West et al. define depersonalization as “feelings of treating
patients as objects rather than human beings and becoming more callous towards patients.”
6
A recent survey
from Medscape showed that nearly 50% of family medicine physicians report burnout.
7
This feature of
burnout is thought to be related to several factors further described below.
• Large patient panels. Most PCPs have in excess of 2,500 patients under their care; some argue that to provide
high-quality primary care, PCPs should care for fewer than 1,000 patients.
8
The large number of patients
cared for by most PCPs can lead to other downstream issues for patients related to access—including shorter
office visits, longer wait times, lower-quality primary care and, as noted above, physician burnout.
• Lower pay. A 2019 report by Medscape states that PCPs make about $100,000 less in salary per year than
the average specialist does.
9
1
Macinko, James, Barbara, Starfield, and Leiyu, Shi. 2007. Quantifying the Health Benefits of Primary Care Physician Supply in the
United States. International Journal of Health Services 37, no. 1:111–126.
2
Reschovsky, James D., Arkadipta, Ghosh, Kate, Stewart, and Deborah, Chollet. Paying More for Primary Care: Can It Help Bend
the Medicare Cost Curve? The Commonwealth Fund, March 2012,
https://www.commonwealthfund.org/sites/default/files/documents/___media_files_publications_issue_brief_2012_mar_1585_r
eschovsky_paying_more_for_primary_care_finalv2.pdf (accessed February 6, 2020).
3
The Triple Aim does not have one single accepted definition, but it most often is defined by including some combination of
lowering costs, improving health quality and outcomes, and improving patient experience as well as health.
4
Schimpff, Stephen C. Why Primary Care Is in Crisis—and How to Fix It. Medical Economics, September 10, 2019,
https://www.medicaleconomics.com/news/why-primary-care-crisisand-how-fix-it (accessed February 6, 2020).
5
West, Colin, Liselotte, Dyrbye, and Tait, Shanafelt. 2018. Physician Burnout: Contributors, Consequences, and Solutions. Journal
of Internal Medicine 283, no. 1:516–529.
6
Ibid.
7
Kane, Leslie. Medscape National Physician Burnout, Depression, and Suicide Report 2019. Medscape, January 16, 2019,
https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056?faf=1#3 (accessed February 6, 2020).
8
Schimpff, Stephen. How Many Patients Should a Primary Care Physician Care for? MedCity News, February 24, 2014,
https://medcitynews.com/2014/02/many-patients-primary-care-physician-care/ (accessed February 6, 2020).
9
Kane, Leslie. Medscape 2019 Physician Compensation Overview. Medscape, April 10, 2019,
https://www.medscape.com/slideshow/2019-compensation-overview-6011286#2 (accessed February 6, 2020).

10
Copyright © 2020 Society of Actuaries
• Increased administrative burden. EHRs were supposed to increase efficiency of health care delivery, but some
believe EHRs have not delivered on that promise.
10
Kaiser Health News reports, “Physicians complain about
clumsy, unintuitive systems and the number of hours spent clicking, typing, and trying to navigate them—
which is more than the hours they spend with patients.” Furthermore, the use of EHRs is associated with
greater rates of physician burnout.
11
Moreover, value-based care, which is intended in part to transition the financing of health care away from
FFS and toward compensating health care providers for delivery of high-quality and evidence-based care,
has thus far also brought with it additional and complex administrative burdens for physicians related to
documenting quality measures and other information needed to receive bonus payments or avoid penalties.
West et al. correlate physician payment models with higher burnout, “with physicians reporting purely
incentive- or performance-based incomes experience far higher burnout rates than salaried physicians.”
12
• Long work hours. Larger patient panels combined with increased administrative burden cause many
physicians, including PCPs, to work longer hours. Most of this additional work time is not reimbursable under
either Medicare or from private payers.
13
• Risk of suicide. Tragically, the combination of these conditions has put many physicians, including PCPs, at
risk of higher rates of mental health-related conditions and at higher risks of suicide.
14
• PCP shortages. Combined, it is not surprising that these trends are leading to fewer medical students entering
primary care and greater numbers of current PCPs ceasing to practice medicine.
15
At a time when there is a
greater need for more PCPs to meet rising demands caused by population growth, aging and increased
insurance coverage (which drives higher utilization of medical services), lower entry rates and higher attrition
rates will only further exacerbate the PCP shortage.
16, 17
It is in this context that a new movement among PCPs has emerged: DPC. While not necessarily formulated as a direct
response to the challenges listed above, DPC is nonetheless an approach to primary care delivery that appears to
address many of them. Its overall feasibility as a delivery model capitalizes on the core idea that primary care, due to
both its comparatively low cost (relative to other health care services) and predictability, may not need to be included
in major medical insurance nor administered by a third party. Rather, primary care can be packaged and distributed
directly to employers and consumers by PCPs themselves. This feature, along with what DPC advocates claim are the
advantages inherent within the DPC model, has motivated many physicians to switch from traditional care delivery
models to DPC, including new physicians straight out of medical school.
18
Milliman DPC Research
10
Schulte, Fred, and Erika, Fry. Death by 1,000 Clicks: Where Electronic Health Records Went Wrong. Fortune, March 18, 2019,
https://khn.org/news/death-by-a-thousand-clicks/ (accessed February 6, 2020).
11
Gardner, Rebekah, Emily, Cooper, Jacqueline, Haskell, Daniel A., Harris, Sara, Poplau, et al. 2019. Physician Stress and Burnout:
The Impact of Health Information Technology. Journal of the American Medical Informatics Association 26, no. 2:106–114.
12
West, Colin, Journal of Internal Medicine (see footnote 5).
13
Wright, Alexi, and Ingrid, Katz. 2018. Beyond Burnout – Redesigning Care to Restore Meaning and Sanity for Physicians. The New
England Journal of Medicine 378, no. 1:309–311.
14
Hampton, Tracy. 2005. Experts Address Risk of Physician Suicide. Journal of the American Medical Association 294, no. 10:
1189–1191.
15
AAMC. Physician Supply and Demand: A 15-Year Outlook: Key Findings. July 2019, https://www.aamc.org/system/files/2019-
07/workforce_projections-15-year_outlook_-key_findings.pdf (accessed on February 6, 2020).
16
Petterson, Stephen, Winston R., Liaw, Robert L., Phillips Jr, David L., Rabin, David S., Meyers, et al. 2012. Projecting US Primary
Care Physician Workforce Needs: 2010-2025. Annals of Family Medicine 10, no. 6:503–509.
17
AAFP. Significant Primary Care, Overall Physician Shortage Predicted by 2025. March 3, 2015,
https://www.aafp.org/news/practice-professional-issues/20150303aamcwkforce.html (accessed on February 6, 2020).
18
Author interviews with DPC physicians.

11
Copyright © 2020 Society of Actuaries
The SOA commissioned Milliman to develop this report to provide health care stakeholders—patients, payers,
policymakers and actuaries—with a comprehensive description of DPC as well as an objective actuarial evaluation of
certain claims made about the DPC model of care.
Our report utilized three primary research methodologies:
1. Literature Review. We conducted a literature review to identify and summarize any existing literature relating
to the DPC model of care or its efficacy. The purpose of this research method was to provide the reader with
a comprehensive overview of existing literature on this relatively new model. We also provide the reader
with a specific definition as to what constitutes a DPC practice. Ultimately, we identified 36 relevant articles
for our literature review and an additional seven sources providing definitions of DPC.
2. Market Survey. We conducted a market survey of DPC physicians to provide an overview of the current DPC
landscape. We conducted this survey in partnership with the American Academy of Family Physicians (AAFP).
The survey was completed by about 200 DPC physicians, with most responding to all questions; we believe
that this sample size represents approximately 10–20% of all physicians currently practicing in a DPC setting.
The survey will provide the reader with an understanding of the current DPC landscape.
3. Employer Case Study. We conducted an actuarial-based evaluation of certain cost and utilization outcome
measures for patients enrolled in a DPC option. For this research, we procured a longitudinal claims data set
from an employer with a DPC option included in its health benefits plan for employees and dependents.
Members in the employer’s plan can elect to enroll in a traditional PPO-style plan option, or they can choose
to enroll in an option that includes a DPC membership, with the employer covering the membership fee.
About half of the members covered by the employer’s plan elected to enroll in the DPC option, and we
applied various actuarial techniques to evaluate the impact of the DPC option on their cost and utilization
measures.
Additionally, we conducted 10 one-on-one interviews with individual DPC physicians, each lasting at least one hour.
We guided these interviews with a short list of broad questions about each physician’s background, including their
experience with traditional primary care, their experience with DPC (and if applicable their transition from a traditional
primary care practice to a DPC practice), their motivations for operating a DPC practice, the impact of DPC on their
personal and professional satisfaction, the impact of DPC on their patients, and their views on the DPC model of care
broadly and where they see the movement trending. There is not a specific section of our report that summarizes
these interviews; rather, they helped to inform us as we conducted our research. Additionally, there are certain
instances in this report where we include information from these interviews as appropriate.

12
Copyright © 2020 Society of Actuaries
3. Overview of DPC
Definition and Common Features
The DPC practice model is relatively new and still evolving, and there appears to be no single accepted definition of
what constitutes a DPC practice. However, the most commonly used definition—based on our literature review—is
as follows:
DPC physician practices are those which:
1. Charge patients a recurring—typically monthly—membership fee to cover most or all primary care related
services.
2. Do not charge patients per-visit out-of-pocket amounts greater than the monthly equivalent of the retainer
fee.
3. Do not bill third parties on a FFS basis for services provided.
Even within this simple definition, there is a wide variety of DPC practice structures. However, based on our
experience, data collection from DPC physician surveys, and interviews with DPC physicians, the following features
are prominent among DPC practices:
• Contracting. DPC practices typically are not a part of insurer or TPA provider networks. Rather, DPC practices
typically only contract directly with patients or self-insured employers.
19
• Recurring fee. The majority of DPC practice revenues typically come from either a monthly or annual
membership fee that covers all services provided under the DPC arrangement. Reported monthly DPC
membership fees for adults generally range from $65 to $85.
20,21
Because DPC practices have lower
administrative overhead due to not contracting with TPAs (i.e., contracting, submitting claims), a larger
portion of the fee can go directly toward providing member care.
• Smaller patient panels. DPC practices usually have fewer patients than traditional primary care practices,
typically fewer than 1,000 and most often around 200 to 600.
22
• No third-party payments. DPC practices do not typically accept third-party payments from insurers or TPAs,
including Medicare and Medicaid, for services provided to their DPC patients.
• Expanded patient access. Because of smaller patient panels and reduced administrative tasks related to not
contracting with nor submitting claims to TPAs, DPC practices increase the amount of time PCPs can spend
providing patient care. In practice, this manifests itself in value-added aspects for DPC patients, such as
longer-duration office visits (discussed in more detail below), being able to schedule same-day or next-day
appointments, receive text or phone-based care, and occasionally have PCP home visits.
• Longer office visits. Smaller patient panels and reduced administrative overhead enable PCPs to spend more
time with each patient. The typical length of an office visit of a traditional primary care practice is around 13
19
Employers with self-insured health benefit plans are financially responsible for paying claims incurred by employees and
dependents enrolled in the plan. These employers typically retain traditional insurance carriers, such as Blue Cross Blue Shield, to
administer their health benefit plans, but the carriers in this instance only provide administrative services; the employer is liable
for all claim amounts. Fully insured employers on the other hand purchase group insurance products for their health benefit
plans where the employer pays fixed premium rates to a carrier and the carrier is financially responsible for paying claims
incurred by enrolled employees and dependents.
20
Huff, Charlotte. 2015. Direct Primary Care: Concierge Care for the Masses. Health Affairs 34, no. 12:2016–2019.
21
Rowe, Kyle, Whitney, Rowe, Josh, Umbehr, and Frank, Dong. 2017. Direct Primary Care in 2015: A Survey With Selected
Comparisons to 2005 Survey Data. Kansas Journal of Medicine 10, no. 1:3–6.
22
According to our DPC market survey.

13
Copyright © 2020 Society of Actuaries
to 16 minutes.
23
A significant portion of this time is typically not face time, because coding and EHR pressures
keep physicians behind the computer screen. By contrast, for DPC practices, it averages around 40 minutes
but can vary based on the patient’s need. For example, as noted above, PCPs are often dealing with disease
states related to multiple body systems, and providing high-quality patient care can be complex. Having
sufficient time with each patient to gather all relevant information, to thoroughly assess patient needs and
preferences, and to devise an appropriate care plan is of paramount importance.
• Reduced patient cost sharing. Most DPC practices do not charge any cost sharing for services covered under
the DPC membership fee. Proponents of the model contend this improves care, as financial barriers are often
the cause of patients missing important follow-up visits.
Covered services under a typical DPC arrangement include preventive care, basic illness treatment for both acute and
chronic conditions, and care coordination.
24
Many DPC physicians also arrange access for their DPC patients to other
discounted services such as prescription drugs, lab tests and imaging services. Patients from all segments of the health
insurance market—commercially insured, Medicare, Medicare Advantage, Medicaid and uninsured—can be and are
members of DPC practices.
25
Additionally, a number of employers have contracted with DPC practices to offer a DPC
option to employees and dependents through their self-insured group health benefit plans, where DPC membership
fees are covered by the employer for employees and dependents that choose to enroll.
Based on physician feedback gathered during our interviews, this financing and delivery model provides an alternative
to traditional FFS-based primary care models, which can be plagued by the challenges described above. The DPC
practice structure in many ways represents a patient-centered medical home (PCMH),
26
and proponents of the DPC
model claim that it greatly improves relationships with patients, reduces the fragmentation of patient care, reduces
costs and improves both personal and professional satisfaction of physicians. Moreover, the proponents argue that
this alternative primary care arrangement generates systemwide reductions in health care utilization, including
hospitalization rates, emergency department usage, unnecessary radiology and diagnostic tests, and specialist care.
Not surprisingly, DPC has its critics, who contend that these reductions are either aberrant, based on small study sizes,
or are driven by patient selection (i.e., healthier patients choose DPC and thus have lower costs than traditional
patients have). Critics also charge that the model is not scalable to the public at large and exacerbates the physician
shortage issue. It is beyond the scope of this paper to examine these criticisms and rebuttals in detail.
23
Wood, Debra. Average Time Doctors Spend With Patients: What’s the Number for Your Physician Specialty? Staff Care,
December 27, 2017, https://www.staffcare.com/physician-resources/which-physicians-spend-most-time-with-patients/ (accessed
February 6, 2020).
24
The Agency for Health care Research and Quality (AHRQ) notes that “Care Coordination in the primary care practice involves
deliberately organizing patient care activities and sharing information among all of the participants concerned with a patient’s
care to achieve safer and more effective care. The main goal of care coordination is to meet patients’ needs and preferences in
the delivery of high-quality, high-value health care.” See AHRQ. Care Coordination. August 2018,
https://www.ahrq.gov/ncepcr/care/coordination.html (accessed February 6, 2020).
25
One notable exception to this is those enrolled in qualified HDHPs paired with HSAs. Due to current IRS rules, a DPC
membership is not allowed with a HDHP/HSA coverage combination. According to the Bipartisan Joint Committee on Taxation,
“Under present law, a direct primary care service arrangement is other coverage or insurance, and therefore the HDHP covered
person is not an eligible individual to contribute to an HSA.” See Joint Committee on Taxation. Description of H.R. 3708, The
“Primary Care Enhancement Act of 2019. October 23, 2019,
https://www.jct.gov/publications.html?func=download&id=5228&chk=5228&no_html=1 (accessed February 6, 2020).
26
The term “patient centered medical home,” at its core, is a concept. However, it is typically associated most closely with the
National Committee for Quality Assurance (NCQA)-accredited practice model. DPC practices are generally not NCQA-accredited
PCMHs.

14
Copyright © 2020 Society of Actuaries
Key Findings from Market Survey
We conducted a survey of DPC physicians, in partnership with the AAFP, to provide an overview of the current DPC
landscape. The survey was completed by more than 200 DPC physicians, which we believe represents approximately
10% to 20% of all physicians currently practicing in a DPC setting, based on our interviews with DPC stakeholders. The
survey will provide the reader with an understanding of the current DPC landscape.
We summarize the key findings from the survey below, and we provide the full survey results in Appendix B.
Overview of Survey Respondents
• Most reported practicing in a “pure DPC” practice (85%) and either having already opted out of Medicare
(75%) or being in the process of opting out of Medicare (5%).
o A “pure DPC” practice was defined as one that meets the three-pronged DPC practice definition
provided previously.
• The average respondent completed medical residency in 2002, with the first and third quartiles being 1997
and 2009, respectively. Most are MDs (83%) who specialize in family medicine (74%).
• Most worked independently to open their DPC practices (74%), are the sole owners of their DPC practices
(76%), and opened their practices after 2015 (71%).
• The primary motivators for choosing to operate a DPC practice were the “potential to provide better primary
care under a DPC model” (96%), “too little time for FFS visits” (85%), and “too much FFS paperwork to
complete” (78%). Just 10% indicated that the “potential to earn more under DPC” was a primary motivator.
• Most reported a willingness to participate in employer-based contracts for DPC services (67%); however,
those respondents contracting with employers reported that on average just 25% of their patient panels
were attributable to employer contracts.
• Most DPC practices are small, with 78% reporting DPC offices with either one or two physicians plus zero or
one nonmedical staff members.
DPC Membership Fees and Covered Services
• The average monthly DPC membership fees reported in the survey were as follows:
o Children: $40
o Adults ages 19–24: $65
o Adults ages 25–50: $75
o Adults ages 51–64: $80
o Adults ages 65 and over: $85
o Families: $150
• Most do not charge a per-visit fee for services covered under the membership by their DPC practices (89%),
and about half charge a one-time enrollment fee for new DPC memberships (54%).
• About two-thirds of respondents reported that their membership fees have not increased in the past three
years (62%), and the average increase during that period was reported to be about 1.5% per year. DPC
physicians responded that just 5% of members terminated their DPC memberships after one year.
• The majority of respondents reported covering the following procedures or services for no additional fees
with a DPC membership at their practices:
o Phone/text consults (99%)
o Same-day appointments (99%)
o EKG (88%)
o Telemedicine (88%)
o Urgent care/walk-in appointments (84%)

15
Copyright © 2020 Society of Actuaries
o Nutritional counseling (83%)
o Weight management (82%)
o Wellness coaching (79%)
o Biopsy and excisions (70%)
o Cryosurgery (65%)
o House calls/home visits (58%)
o Joint injections (58%)
o Spirometry (56%)
• The majority of respondents reported covering the following procedures or services for DPC members at
their practices with an additional fee (i.e., patient cost sharing):
o Basic laboratory testing such as HgbA1C, lipids, CMP, TSH, PSA, PAP, CBC, U/A (69%)
27
o Sending off pathology specimens (66%)
o Prescriptions drugs (57%)
o Adult immunizations (53%)
• The majority of respondents reported not covering the following procedures or services at their practices
(i.e., not included as part of a DPC membership nor offered for an additional patient fee):
o Flexible sigmoidoscopy exam (97%)
o Obstetrical services (91%)
o Vasectomy (88%)
o Colonoscopy (82%)
o Tympanometry (82%)
o Ultrasound imaging (74%)
o X-ray (74%)
o Addiction medicine (73%)
o Functional/integrative medicine (61%)
o Department of Transportation (DOT) physicals (57%)
o Endometrial sampling (57%)
o Children and adolescent immunizations (51%)
DPC Effects on Physician Experience
• The respondents reported an average current DPC patient panel of 445 and a target DPC patient panel of
628. The average ratio of the current to target DPC patient panel size was 70% (i.e., on average the current
DPC patient panel was 30% below the target size).
• For those respondents with full DPC patient panels, the average length of time to fill the panel was 21
months, with first and third quartiles of 10 and 24 months, respectively.
• Most respondents reported that each of the following has been better or much better under a DPC model
of care:
o Overall (personal and professional) satisfaction (99%)
o Ability to practice medicine (98%)
o Quality of primary care (98%)
o Relationships with primary care patients (97%)
o The amount of time spent on paperwork (88%)
o The amount of time spent at the office (73%)
• Just 34% of respondents reported having better or much better earnings as a PCP under a DPC model of care.
27
The tests listed are relatively common tests. HbA1C is for diabetes, lipids is for cholesterol, CMP measures metabolism, TSH is
for thyroid, PSA is for prostate, PAP is for cervical cancer, CBC is a complete blood count, and U/A is a urine analysis.

16
Copyright © 2020 Society of Actuaries
DPC Effects on Patient Experience
• On average, DPC members are able to schedule an appointment with their DPC provider within one day, wait
just four minutes in the DPC office for scheduled appointments to begin, and spend 38 minutes with the DPC
clinician during visits.
• Most DPC members are able to access their EHRs from their DPC practices through a patient portal (58%)
and are also able to sign up and manage their DPC enrollment using their DPC practice’s website (58%).
28
• Ninety-eight percent of respondents indicated that they expect the DPC model of care to:
o Improve patient satisfaction with primary care experience. (98%)
o Increase the extent to which patients rely on their PCPs to navigate the health system for
nonprimary care services (81%)
o Lower patient out-of-pocket costs for primary care services, including the DPC membership fee
(81%)
o Increase patient compliance with preventive care guidelines (68%)
28
It is important to note that DPC doctors generally do not use standard industry EHRs that are designed for purposes of
payment. DPC providers most often use EHRs that are designed solely for purposes of facilitating diagnosis, patient care and
efficiency, not payment.

17
Copyright © 2020 Society of Actuaries
4. Summary of DPC Literature Review
Overview
This section of our research report summarizes the key findings from our literature review relating to DPC. The
purpose of our literature review was twofold:
1. To gather descriptive information relating to the DPC model including definitions of DPC, distinctive
characteristics of DPC, common variations between DPC and traditional primary care practices, and
variations among DPC practices.
2. To summarize academic literature regarding the efficacy or expected efficacy (including cost, quality and
outcomes) of DPC and similarly structured primary care arrangements.
Selection Criteria
To identify DPC-related research articles to include in our report, we utilized the following resources:
• U.S. National Library of Medicine’s PubMed search engine
• Google Scholar search engine
• Google search engine
• Health Affairs
• Society of Actuaries Health Watch
• DPC Frontier’s summary of DPC-related academic and nonacademic articles
First, we gathered relevant articles from the above resources by conducting separate searches for “Direct Primary
Care,” “DPC,” “Concierge Medicine,” “Retainer Medicine” and “Subscription Medicine.” We also gathered additional
relevant articles by reviewing the citations for the gathered articles and identifying articles not found during our initial
searches. Next, we narrowed the initial broad list of articles to the more targeted list included in this report by
reviewing the article abstracts or introductions and retaining for our report only those articles that provide material
descriptive information on DPC or report on observed or theorized effects from the DPC model.
Ultimately, we identified 36 relevant articles for our literature review and an additional seven sources providing
definitions of DPC. It is possible—and in fact, it is even likely—that our search did not identify all relevant research
articles related to the DPC model; however, we believe that our search was adequate and that our report provides a
comprehensive overview of existing literature on the DPC model and its effects. We provide key excerpts from and
full reference information for each of the articles included in our literature review in Appendix A.
Summary of Existing Literature
For clarity, we have grouped the articles included in our literature review into the following categories:
1. Overview of DPC
2. Cost outcomes
3. Regulatory considerations
4. Provider experience
5. Patient access

18
Copyright © 2020 Society of Actuaries
In this section, we summarize some of the key results, common observations and expectations, and arguments in
favor of and against the DPC model of care from the articles included in our literature review. While this summary
provides readers with a valuable high-level overview of the articles we reviewed, it is not a substitute for reading the
articles themselves. Readers can find a listing of all of the articles included in our literature review in Appendix A, as
well as reference information for each article. Both this section and Appendix A group the articles into the five
categories listed above.
The summary points listed here are not necessarily attributable to any single article included in our literature review.
Rather, these summary points represent our best attempt to distill the information provided in all of the various
articles into a series of distinct and informative statements. In instances where many of the included articles provide
similar information, our summary points represent our best effort to combine these various similar pieces of
information. In instances where a single article provides a piece of unique and useful information, our summary points
may quote directly from an article.
Overview of DPC
• Physician dissatisfaction has increased during the past two decades, and some recent surveys show a
majority of physicians reporting some level of burnout. Physician burnout may be most acute for PCPs, who
are challenged by what some describe as low per-visit reimbursement, high malpractice insurance premiums,
overwhelming insurance paperwork, and the need to continue adding patients to their panels to support
their practices.
• DPC can provide an alternate practice structure for PCPs, with the potential to reduce their patient panel
sizes by two-thirds, increase time spent with each patient, and avoid burdensome insurance paperwork.
• DPC can provide an alternate primary care relationship for patients, with increased clinician access and the
potential to receive less fragmented care via establishing a long-term relationship with a PCP.
• DPC has similarities to another alternate model of primary care—concierge care—but a key differentiator is
that DPC practices have lower membership fees than concierge practices and do not also bill third parties on
a FFS basis for provided services as concierge practices typically do.
• Reported monthly DPC membership fees for adults range from $25 to $125 and generally cover preventive
care, vaccinations, basic illness treatment, care coordination, basic labs and access to discounted
prescriptions. DPC patients generally have 24/7 access to their clinicians via email or other electronic
communication mediums and can schedule same-day appointments during clinic hours. Patients from all
segments of the health insurance market—commercial insured, Medicare FFS, Medicare Advantage,
Medicaid and uninsured—are enrolled in DPC practices. Those enrolled in a DPC practice are generally
encouraged by their DPC clinicians to carry catastrophic health insurance in addition to their DPC
memberships.
• Proponents of the DPC model of care argue that this alternative primary care arrangement generates
systemwide reductions in health care utilization, including hospitalization rates, emergency department
usage, unnecessary radiology procedures and diagnostic tests, and specialist care.
• Critics of the DPC model of care contend that DPC is not a scalable primary care arrangement and that it
exacerbates the existing shortage of primary care clinicians in the U.S. by reducing patient panel sizes for
DPC practitioners.
• Proponents argue that reported outcomes show reduced overall health care costs for patients enrolled in
DPC clinics, while critics argue that these reported savings are due to patient selection (i.e., healthier patients
enroll in DPC practices and are then compared to less healthy patients to measure outcomes).

19
Copyright © 2020 Society of Actuaries
Cost Outcomes
Due to the relative newness of the DPC model of care, there is not an abundance of literature assessing cost outcomes
for DPC arrangements. However, from a clinical standpoint, DPC shares key characteristics with other models of
primary care, such as PCMHs, which are somewhat more established and for which additional literature exists.
According to the American College of Physicians, the PCMH is a care delivery model whereby patient treatment is
coordinated through a patient’s PCP with the goal of ensuring the patient receives the necessary care when and where
it is needed and in a manner the patient understands. The purported improved outcomes from the DPC model are
said to largely result from its patient-centered and high-touch delivery of primary care—a key differentiator for
PCMHs. Thus, in our literature review, we have included articles measuring outcomes for DPC, as well as key articles
measuring outcomes for the PCMH model of care. We believe this literature pertaining to PCMHs provides valuable
insights and considerations for evaluating the DPC model of care. The included articles relating to PCMHs are not
meant to represent a comprehensive literature review pertaining to PCMH cost outcomes. Rather, the included
articles are meant to provide useful data points for our review of the DPC model of care.
We also differentiate between outcomes-related articles that explicitly account for differences in population
demographics and health status and make use of appropriate methodologies in their analyses and those that do not.
We herein refer to articles accounting for patient differences in their methodologies as providing adjusted results,
that is, the results presented in these articles are adjusted for any differences in patient acuity when comparing cost
outcomes. The articles included in our literature review that present adjusted results applied various statistical
methodologies. In our summary points below, we do not distinguish between, nor evaluate, the various
methodologies used.
DPC Outcomes Articles
Adjusted Results
• We did not identify any articles that evaluated adjusted cost outcomes for models of care that meet our
specific definition of DPC.
• However, we did identify two articles presenting adjusted results for a model of care with at least one
important aspect similar to DPC, namely smaller patient panels. The company MDVIP uses the model. We
consider MDVIP’s model to represent concierge care rather than DPC. In addition to charging MDVIP
members an annual membership fee ranging from $1,650 to $2,200
29
($137 to $183 per month), which is
much higher than typical DPC membership fees, MDVIP also bills third-party payers for all services provided
to members. Even though the MDVIP model does not meet our definition of DPC, we believe these two
articles are relevant to our review of DPC because of the similarity of concierge care and DPC, as well as the
robust data sets and methodologies applied in these articles.
o Both articles showed lower inpatient hospital and emergency department utilization rates for
patients enrolled in concierge care compared to patients not enrolled in concierge care.
o One article showed lower overall health care claim costs for patients enrolled in concierge care
compared to patients not enrolled in concierge care. The other article did not show lower overall
health care claim costs for all patients analyzed but did show lower costs for older patients with
higher baseline claim costs.
o Neither article considered the annual membership fee for enrolling in concierge care in their
evaluations of whether enrollment in concierge care was associated with lower overall health care
claim costs.
29
MDVIP. The MDVIP Difference: More Than Just a Doctor, A Partner in Health. https://www.mdvip.com/patients/benefits
(accessed February 6, 2020).

20
Copyright © 2020 Society of Actuaries
Unadjusted Results
• We identified three articles that evaluated unadjusted cost outcomes for models of care meeting our specific
definition of DPC. Each article compared various cost and utilization measures for patients enrolled in DPC
to cost and utilization measures for patients not enrolled in DPC, without consideration for differences in
patient acuity or health status. These articles, therefore, do not discern between differences directly related
to DPC versus differences caused by other factors unrelated to DPC, such as age, gender, health status,
geography, etc. We also identified additional articles reporting unadjusted results for DPC that we did not
include in our literature review because they were not source articles; rather, these additional articles were
reporting various figures from the three source articles already included.
o All three articles showed lower overall health care claim costs for patients enrolled in DPC compared
to patients not enrolled in DPC, without consideration for the DPC membership fees.
o One of the articles showed lower overall health care claim costs for patients enrolled in DPC
compared to patients not enrolled in DPC after consideration of the DPC membership fee; the other
two articles did not evaluate the level of the DPC membership fees relative to the lower claim costs.
o One of the articles showed lower inpatient hospital and emergency department utilization rates for
patients enrolled in DPC compared to patients not enrolled in DPC. The other two articles did not
evaluate these measures.
Articles on PCMH Outcomes
Adjusted Results
• Ghany et al. (2018) showed that Medicare Advantage patients enrolled in PCMHs had lower inpatient
hospital utilization rates and overall health care claim costs compared to patients not enrolled in PCMHs.
• David et al. (2015) showed that Medicaid patients enrolled in PCMHs did not show lower overall total health
care claim costs compared to patients not enrolled in PCMHs.
• Rosenthal et al. (2015) showed that commercially insured patients enrolled in PCMHs had lower emergency
department utilization rates and higher quality of care scores compared to patients not enrolled in PCMHs.
They also showed that certain results, such as the lower relative overall health care claim costs, were more
pronounced among PCMH patients with multiple comorbidities.
• Neal et al. (2015) showed that chronically ill commercial patients enrolled in PCMHs showed lower overall
health care claim costs, as well as lower utilization rates for inpatient hospital and physician specialist
services, compared to patients not enrolled in PCMHs.
• Friedberg et al. (2014) showed that chronically ill commercial patients enrolled in PCMHs showed lower
emergency department utilization rates compared to patients not enrolled in PCMHs. They also showed that
nonchronically ill commercial patients enrolled in PCMHs did not show lower emergency department
utilization rates compared to patients not enrolled in PCMHs.
• Meyers et al. (2019) showed that chronically ill patients enrolled in high-touch team-based models of primary
care showed lower inpatient hospital, outpatient hospital, emergency department and ambulatory care-
sensitive encounter utilization rates compared to patients not enrolled in high-touch team-based models of
primary care. They also showed that, under this model of care, nonchronically ill patients actually showed
higher utilization rates.

21
Copyright © 2020 Society of Actuaries
Regulatory Considerations
At the federal level
• The Patient Protection and Affordable Care Act (ACA) permits qualified health plans (QHPs) sold through the
ACA insurance exchanges to provide coverage through DPCs paired with wraparound insurance. No QHPs
have offered such a product to our knowledge.
• The Internal Revenue Service (IRS) prohibits individuals with health savings accounts (HSAs) paired with high-
deductible health plans (HDHPs) from having an agreement with a DPC provider.
• Various federal bills have been proposed that would permit patients with HSAs paired with HDHPs to not
only have agreements with a DPC provider but to use their HSAs to pay for DPC membership fees.
At the state level
• Certain consumer advocates and insurance commissioners have raised concerns as to whether DPC practices
are involved in “the business of insurance.”
• Some states have passed laws clarifying that DPC is outside of the business of insurance and constitutes a
medical service.
• Some states, such as Maryland, have recommended that DPC practices include certain contractual provisions
in member agreements to avoid being considered as involved in "the business of insurance.” These
recommended contractual provisions included:
o Limiting provided services under the DPC agreement to an annual physical, follow-up care relating
to the physical, and a specific number of other visits.
o Establishing the DPC membership fee by determining the market value of the expected services
provided under the agreement.
o Specifying the covered services under the DPC agreement with as much clarity as possible.
o Allowing patients to terminate their DPC agreements for any reason, at any time, and to receive
prorated reimbursements of any DPC membership fees already paid.
o Placing a cap on the number of patients with whom a DPC practice may enter into agreements.
Provider Experience
• Many DPC physicians claim that by not billing third parties on a FFS basis for provided services and by limiting
the size of their patient panels, they have more time to provide patient care.
• Some DPC practices have proved viable and sustainable from a financial standpoint, with patient panels
about one-third the size of traditional primary care patient panels and significantly reduced practice
overhead costs.
• Legal and ethical concerns have been raised about patient continuity of care when an existing nonretainer-
based primary care practice transitions to a retainer-based practice.
Patient Access
• DPC presents a theoretically sound model for improving the attributes of primary care for enrolled patients,
such as first contact care and long-term improved treatment.
• At a health system level, DPC theoretically improves access to health care for enrolled patients while reducing
access to health care for nonenrolled patients by reducing the number of nonretainer-based PCPs who would
otherwise have larger patient panels.
• Patients often do not have the analytic framework or information necessary to evaluate whether to remain
with their primary care clinicians during a transition to DPC.

22
Copyright © 2020 Society of Actuaries
• There is increased demand by health care patients for patient-centric solutions, and DPC may provide one
way of fulfilling this demand.
• DPC may run counter to the primary mission and goal of most health care payment and delivery reforms,
which are focused on expanding overall access to health care rather than increasing access for some patients
while decreasing access for other patients via reduced primary care panel sizes.
• Surveys of retainer-based primary care practices, including DPC and concierge style, have shown lower
prevalence of African American, Hispanic and Medicaid patients enrolled in retainer-based practices than
nonretainer counterparts.
Gaps in Existing DPC Research
The DPC model of care is relatively new and still evolving, and as such, the body of existing literature relating to this
model of care is somewhat limited. Stakeholders evaluating the efficacy and sustainability of this primary care
arrangement would benefit from the following research initiatives:
• A comprehensive survey of DPC practices including geographic information, services provided, membership
fee amounts and structures, motivation and resources for practicing under a DPC model, and information
related to provider and patient satisfaction. We believe that our market survey provided in Section 3
addresses this research gap.
• A comprehensive comparison of DPC patients versus non-DPC patients, particularly in a patient-choice
setting, to determine characteristic differences between patients choosing to enroll in DPC versus those who
are not choosing to enroll in DPC (e.g., DPC patients are younger, healthier and have more children). We
believe that our case study introduced in Section 5 addresses this research gap.
• An actuarially adjusted comparison of cost, quality and utilization rates between patients who are enrolled
in DPC and patients who are not. We believe that our case study introduced in Section 5 addresses this
research gap with respect to certain cost and utilization measures.
• An actuarially adjusted ROI determination for employers contracting with DPC practices on behalf of
employees to determine whether overall total health care claim cost savings for enrolled patients offset the
cost of recurring DPC membership fees. We believe that our case study introduced in Section 5 addresses
this research gap.
• A breakout of DPC results for chronically ill versus nonchronically ill patients. Similarly, structured primary
care arrangements have shown the most positive benefits for chronically ill patients, and preliminary
evidence indicates that DPC tends to attract healthier patients under an employer-arranged DPC offering. It
would be prudent for DPC practitioners to learn whether chronically ill patients are most likely to benefit
from the DPC model of care but also least likely to enroll. Our research does not address this gap due to data
limitations.
• A qualitative review of nondata-driven aspects of DPC, such as provider engagement, patient engagement,
increased patient-provider face time. Our research does not address this gap due to data limitations.
• A longitudinal study that measure whether DPC “bends the cost curve” in health care claim costs per patient
and whether any potential reduction in claim costs due to DPC only represents a one-time level shift in cost.
Our research does not address this gap due to data limitations.

23
Copyright © 2020 Society of Actuaries
5. Overview of Case Study
Because the DPC model is new, evolving and lacks consensus as to its efficacy, it will be necessary going forward to
accurately assess the impacts of the model on key features of the health care system, especially those related to the
Triple Aim goals of cost, quality and patient experience. If credible, quantitative data support the model’s net
advantages over the dominant conventional primary care model, all constituents stand to benefit, including
employers, policymakers, health plans and the general public. More quantitative information related to any favorable
impacts of DPC is, therefore, critical. Likewise, studies could also show weaknesses in the model that need to be
addressed, which may help the DPC movement evolve in a way that leads to the greatest overall public good.
Study Structure
Our study uses actual data of meaningful sample size,
30
combined with actuarial adjustments and analysis, to begin
quantifying the potential impacts of the DPC model relative to a traditional primary care model. As would be expected
for most studies of this nature, there are a number of potentially confounding variables that may obscure or distort
the true effect of the DPC model. Thus, our study design seeks to minimize any potential impacts of these confounding
variables through two key structural features:
• A quasi-control group: As we detail later in this paper, our data is derived from a single employer that offers
a DPC benefit option and a traditional benefit option. This arrangement will, as much as practically possible,
increase the likelihood that the cohorts of individuals in each option (DPC and traditional) are similar
demographically, particularly with regard to features other than age, gender and health status (which are
accounted for with other adjustments). For example, differences in expected claim costs due to working in
different industries do not influence study outcomes, because the data come from a single employer. Many
enrollees also share similar geographic regions and also likely utilize many of the same health care facility-
based providers such as hospitals, thus health care cost variations due to geography are also minimized.
Note that this is not a control group in the strictest sense, because that would entail various aspects of
random selection and matching that are beyond the feasibility of this data set. Moreover, for convenience,
we use the term “control” throughout in a broad sense to denote that various confounding variables that
may otherwise skew study results have been addressed either through the use of risk adjustment or through
study design.
We used a participant versus nonparticipant approach to assess outcomes associated with enrollment in the
DPC model. We compared outcomes during the same two-year period between members enrolled in DPC
and members enrolled in the traditional option.
• Normalization for patient selection: One aspect that is not directly controlled for under the single employer
structure of the study is patient self-selection. In fact, employees’ ability to choose which option they want
to enroll in is an important aspect of the study, because it points to one of the key criticisms of DPC—that
favorable results reported in other DPC studies are driven by patient populations with fewer health care
needs selecting DPC. Our analysis utilized risk adjustment techniques to estimate the differences in health
status between members enrolling in the DPC and traditional options and then to adjust for population
selection when analyzing differences in utilization rates and claim costs.
Study Goals
30
Our literature review identified other studies of DPC outcomes using sample sizes as low as 205.

24
Copyright © 2020 Society of Actuaries
We outline the study’s goals below:
1. Evaluate the impact of DPC on utilization and cost using adjusted results. Using the quasi-control group
framework and an appropriate actuarial methodology to adjust for demographic and patient selection
differences, we assessed the impact of the DPC option on various measures of health care cost and
utilization. Results from members enrolled in the DPC option are compared to results from members enrolled
in the traditional option on an adjusted basis (i.e., controlling for morbidity and demographic differences
between the two cohorts). We focused our analysis on metrics that relate to the major arguments made by
proponents and critics of the DPC model of care, which are determinable through the data sets that the
employer provided for our analysis.
In particular, we assessed the impact of the DPC option on overall health care claim costs, as well as on
utilization rates for emergency department and inpatient services specifically. We also assessed morbidity
differences between members enrolled in the DPC and traditional options and evaluated the expected
impact of any observed differences on cost and utilization rates.
2. Evaluate the impact of DPC option on total employer benefit costs. We assessed the impact of the DPC option
on total employer benefit costs for the self-insured employee health benefits plan (i.e., all non-administrative
plan expenses). Our evaluation took into account not only the effects of the DPC option on overall health
care claim costs and utilization rates but also the plan design changes for members enrolled in the DPC option
and the employer funding of the DPC membership fee.
3. Establish actuarial framework for funding employer DPC programs. Employers considering whether to offer a
DPC program through their self-insured employee health benefit plans may require a DPC program to be
cost-neutral or to generate savings for the employer. We provide an actuarial framework for employers to
use when considering the addition of a DPC option for their self-insured employee health benefit plans. Using
illustrative baseline claim costs from Milliman’s Health Cost Guidelines™ (HCGs) and DPC-related
assumptions informed by the results from the case study analysis herein, we illustrate a sample DPC
membership fee structure supported by expected claim cost savings resulting from the DPC model.
Data Description
Exposure Measures
The data set for this study was derived from the experience of a midsized employer that offered a DPC option
alongside a traditional option to the employees and dependents enrolled in its self-insured health benefit plan. The
health benefit plan covered approximately 1,000 employees and 1,000 dependents, and roughly half of the population
was enrolled in the DPC option. The experience data consisted of four years of medical and prescription drug claims
and enrollment data from the employer, as well as plan design summaries. These data sets covered the four-year
period from June 2014 through May 2018. The DPC option was introduced in July 2015.
We limited our selected DPC option and traditional option cohorts to members with at least 12 months of continuous
enrollment in their respective options during the two-year period immediately after DPC was introduced, and we also
excluded members with catastrophic levels of health care claims (above $75,000 per person annually) during either
the first or the last 12 months of the two-year period.
This resulted in final selected cohorts of 912 members for the DPC option and 1,074 members for the traditional
option. The average exposure period for these selected members during the two-year period of interest was 22.0 and
21.9 months for the DPC option and traditional option, respectively.

25
Copyright © 2020 Society of Actuaries
Cost Measures
Allowed costs represent the total payments made to health care providers for care (i.e., it includes both the patient
and plan paid amounts).
31
Using allowed costs provides the most accurate representation of the DPC option’s impact
on the total cost of health care.
The employer requires the contracted DPC providers to submit claim information to the self-funded plan’s TPA for
covered services furnished to members enrolled in the DPC option. These claims include service-level information
such as Current Procedural Terminology (CPT) and Health care Common Procedure Coding System (HCPCS) procedure
codes required for payment. However, the DPC providers are not reimbursed on an FFS basis for these claims. Rather,
the DPC providers are paid through the monthly DPC membership fees paid by the employer on behalf of members
enrolled in the DPC option. The TPA adjudicates the claims submitted by the DPC providers for reporting purposes
under the same fee schedule used to adjudicate claims from non-DPC providers for the same services. Therefore, the
medical claim data provided by the TPA for our analysis includes imputed allowed amounts for services provided by
the DPC providers based on the TPA’s network fee schedule. We verified that the reimbursement levels for
professional claims is consistent between the DPC and traditional cohorts.
Benefit Coverages
Pre-2016
Before the DPC option was offered through the health benefit plan, all enrolled members (employees and
dependents) were covered by a single plan design. This traditional offering covered 100% of preventive care claims
and covered prescription drug claims via coinsurance, with an annual limit on the total prescription drug-specific
coinsurance paid by members. Nonpreventive medical claims were covered via a major medical benefit structure with
five corridors, as illustrated in Figure 1.
Figure 1
TRADITIONAL OPTION MAJOR MEDICAL COVERAGE
Medical Coverage Corridor
Description
Single Employee Amounts
Routine medical deductible
Employee pays out-of-pocket for all covered medical
claims.
$150
Health reimbursement
arrangement (HRA)
All covered medical claims are covered by employer via
HRA contributions.
$750
Major medical deductible
Employee pays out-of-pocket for all covered medical
claims.
$600
Major medical coinsurance
Employee pays for percentage of all covered medical
claims.
20% employee
Coinsurance limit
Employer pays for all covered medical claims.
After $1,500 in member
coinsurance
Figure 2 illustrates how the claim liability for a single employee with annual routine and major medical claims totaling
$15,000 would be distributed between the employee and the employer by corridor.
31
Allowed costs are the contracted total payment rates between network providers and the health benefit plan for covered
services. Payment to providers for the entire contracted rate (i.e., allowed cost) is typically shared between patients in the form
of cost sharing and the plan in terms of plan pay amounts. To contrast, billed costs are essentially the “sticker price” for services,
and most payers do not pay that amount, which tends to be significantly higher than the allowed costs.

26
Copyright © 2020 Society of Actuaries
Figure 2
EXAMPLE: TRADITIONAL OPTION CLAIM LIABILITY DISTRIBUTION
Medical Coverage Corridor
Claim Amount
Employee Pays
Employer Pays
Routine Medical Deductible
$150
$150
$0
HRA
$750
$0
$750
Major Medical Deductible
$600
$600
$0
Major Medical Coinsurance
$7,500
$1,500
$6,000
Coinsurance Limit
$6,000
$0
$6,000
Total Paid
$15,000
$2,250
$12,750
2016 Forward
Beginning with the 2016 plan year, which started on July 1, 2015, the employer offered enrolled employees and their
dependents the option to enroll in an alternative plan design that included the DPC option. Members could choose to
enroll in the DPC option at any time throughout the plan year, or they could choose to remain in the traditional option.
The DPC option included the same coverage for preventive care and prescription drug claims as the traditional option.
Members enrolled in the DPC option were given no-cost access to two DPC practices for primary care services, and
the employer covered the DPC membership fee. Last, members enrolled in the DPC option had an alternate benefit
structure versus the traditional option for coverage of non-preventive, traditional medical claims, as illustrated in
Figure 3.
Figure 3
DPC OPTION MAJOR MEDICAL COVERAGE
Medical Coverage Corridor
Description
Single Employee Amounts
Routine Medical Deductible
The DPC option does not include a routine medical deductible.
$0
HRA
The DPC option does not include an HRA.
$0
Major Medical Deductible
The DPC option does not include a major medical deductible.
$0
Major Medical Coinsurance
Employee pays for percentage of all covered medical claims.
20% employee
Coinsurance Limit
Employer pays for all covered medical claims.
After $1,500 in coinsurance
Figure 4 illustrates how the claim liability for a single employee with annual medical claims totaling $15,000 would be
distributed between the employee and the employer by corridor under the DPC option.
Figure 4
EXAMPLE: DPC OPTION CLAIM LIABILITY DISTRIBUTION
Medical Coverage Corridor
Claims
Employee Pays
Employer Pays
Routine Medical Deductible
$0
$0
$0
HRA
$0
$0
$0
Major Medical Deductible
$0
$0
$0
Major Medical Coinsurance
$7,500
$1,500
$6,000
Coinsurance Limit
$7,500
$0
$7,500
Total Amount Paid
$15,000
$1,500
$13,500
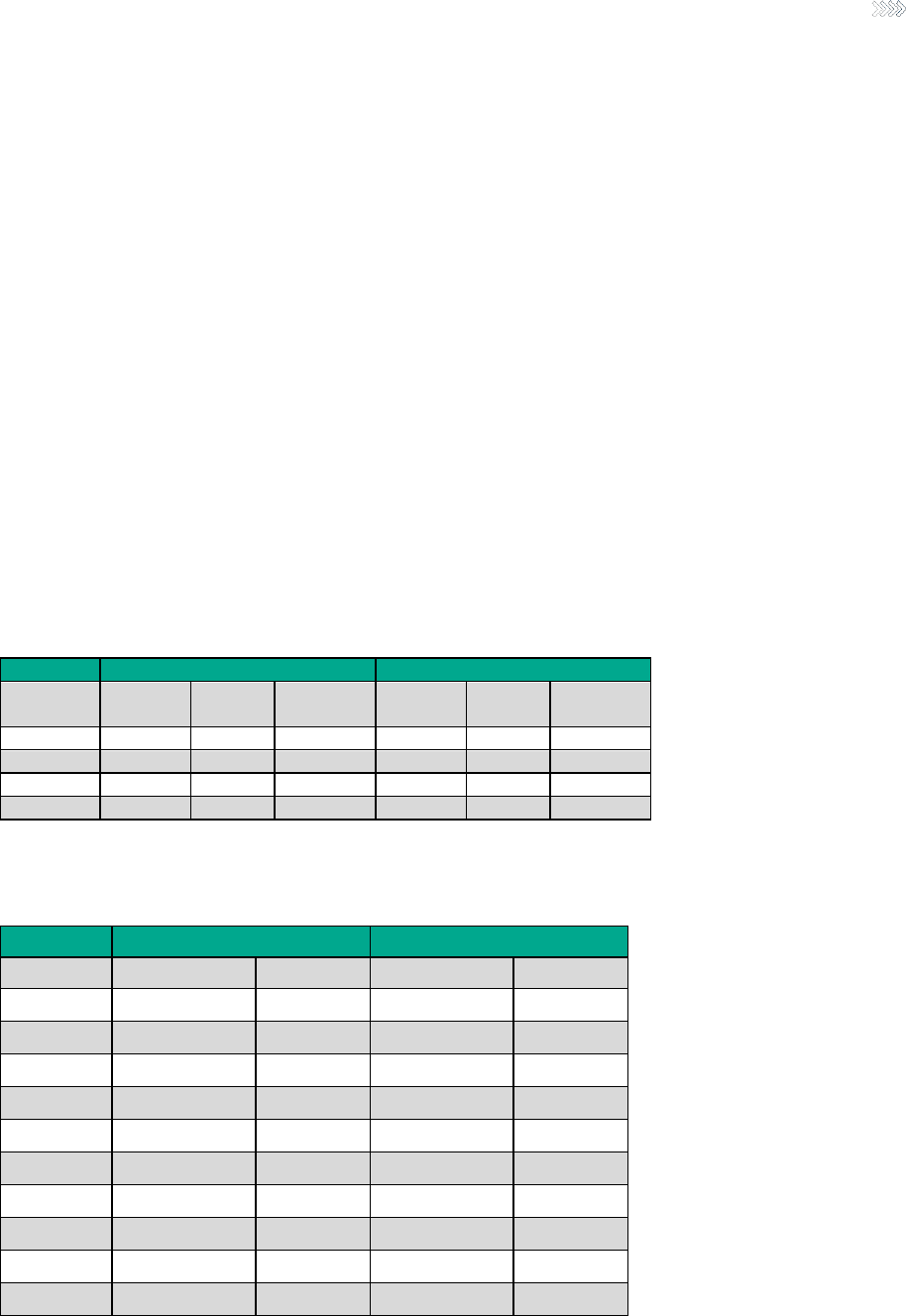
27
Copyright © 2020 Society of Actuaries
6. Case Study Findings
Population Differences
Demographics
Figures 5 and 6 provide a summary of the DPC option and traditional option cohort demographics. Results are
provided in total and broken out across various population groups: employees, spouses and children (Figure 5) and
age (Figure 6). Metrics include the unique members selected, the total member months analyzed for the selected
cohort during the two-year period of interest, and the distribution (i.e., mix) of member months for each cohort.
In general, the member mix did not vary materially between the DPC option and traditional option, although there
were minor differences. For example, Figure 5 illustrates that, while more than half of the DPC option and traditional
option members were employees, the DPC cohort had about 1% less employees and 2% less spouses than the
traditional cohort and thus about 3% more children. This mix difference drove a lower average age in the DPC cohort,
as illustrated further in Figure 6. Because children, on average, have lower health care costs than adults do, the
absence of any adjustment in morbidity differences between the DPC and traditional cohorts would likely cause the
average cost for the DPC cohort to be lower, all else equal. As detailed further below, our risk adjustment methodology
properly accounted for this difference.
Figure 5
DPC OPTION VS. TRADITIONAL OPTION DEMOGRAPHIC SUMMARY, MEMBER TYPE
DPC Option Cohort
Traditional Option Cohort
Member
Type
Unique
Members
Member
Months
Member
Month Mix
Unique
Members
Member
Months
Member
Month Mix
Employees
467
10,417
51.9%
557
12,408
52.7%
Spouses
85
1,845
9.2%
121
2,609
11.1%
Children
360
7,821
38.9%
396
8,534
36.2%
Total
912
20,083
100.0%
1,074
23,551
100.0%
Figure 6
DPC OPTION VS. TRADITIONAL OPTION DEMOGRAPHIC SUMMARY, AGE BRACKET
DPC Option Cohort
Traditional Option Cohort
Age Bracket
Member Months
Member Mix
Member Months
Member Mix
0–9
2,458
12.2%
2,437
10.3%
10–19
3,823
19.0%
3,502
14.9%
20–29
3,097
15.4%
3,863
16.4%
30–39
3,068
15.3%
2,572
10.9%
40–49
3,434
17.1%
3,576
15.2%
50–59
3,221
16.0%
4,334
18.4%
60–64
874
4.4%
2,286
9.7%
65+
108
0.5%
981
4.2%
Total
20,083
100.0%
23,551
100.0%
Average Age
31.8
36.1

28
Copyright © 2020 Society of Actuaries
Risk Selection and Morbidity
Figure 7 provides a summary of the relative health statuses of the DPC and traditional cohorts based on risk scores.
To calculate risk scores, we used the Milliman Advanced Risk Adjusters™ (MARA™) to quantify expected differences
in claim costs and utilization levels between the DPC and traditional cohorts, based on the mix of acute and chronic
clinical conditions attributable to the individuals within each cohort. MARA calculates risk scores in total and broken
out across six medical service types (inpatient, outpatient, emergency, physician, prescription drug and other), taking
into account each individual’s age, gender, comorbidities and prescription drug usage. An individual with a higher risk
score is generally less healthy and is associated with higher claim costs than an individual with a lower risk score.
Please see Section 10 below and Appendix C for additional information on MARA.
The relative risk scores provided in Figure 7 are the ratio of the DPC and traditional cohort risk scores determined by
MARA and express the relative estimated health status of the DPC cohort compared to the traditional cohort.
Subtracting 1.0 from these relative risk scores provides the expected percentage difference in per capita claim costs
between the cohorts based on the observed difference in health status. Overall, the DPC cohort has an 8.3% lower
risk score than the traditional cohort. This includes any differences between the two cohorts in demographics such as
age and gender. The estimated claim cost difference is greatest for prescription drug claims, where the DPC cohort
has 15.8% lower estimated claim costs than the traditional cohort, and the difference is lowest for inpatient facility,
where the DPC cohort has 5.0% lower claim costs than the traditional cohort. The DPC cohort’s estimated claim costs
are lower for each of the six types of services other than emergency department, where the DPC cohort has 5.6%
higher claim costs than the traditional cohort.
These observed differences in health status between the DPC and traditional cohorts further support the need for
proper adjustments to be made when analyzing differences in actual utilization rates and claim costs between these
cohorts.
Figure 7
DPC OPTION VS. TRADITIONAL OPTION OBSERVED RISK SCORES
Type of Service
DPC/Traditional
Relative Risk Score
Expected (based on risk score)
DPC vs. Traditional Claims Cost
Variance
Inpatient Facility
0.950
−5.0%
Outpatient Facility
0.937
−6.3%
Emergency Department
1.056
+5.6%
Physician
0.932
−6.8%
Other Medical
0.874
−12.6%
Prescription Drugs
0.842
−15.8%
Total
0.917
−8.3%
Overall Demand for Health Care Services
We compared per member per month (PMPM) total allowed claim costs between the DPC and traditional cohorts to
assess the impact of the DPC option on the overall demand for health care services among members enrolled in the
DPC option. Figure 8 shows the unadjusted and risk-adjusted relative differences in PMPM health care claim costs
between the DPC and traditional cohorts. The differences in health care costs are measured using allowed costs and
are inclusive of all types of services, including those furnished by DPC providers. Services provided by the DPC provider
were assigned allowed costs in the provided data using the same fee schedule as was applied to claims for traditional
option members. Here we are using total allowed claim costs, as determined by the applicable fee schedule and
utilization of both DPC-covered and non-DPC-covered services, as a proxy for member demand for overall health care
services. Thus, this cost comparison attempts to isolate the impact of the DPC delivery model on the overall level of
demand for health care services.
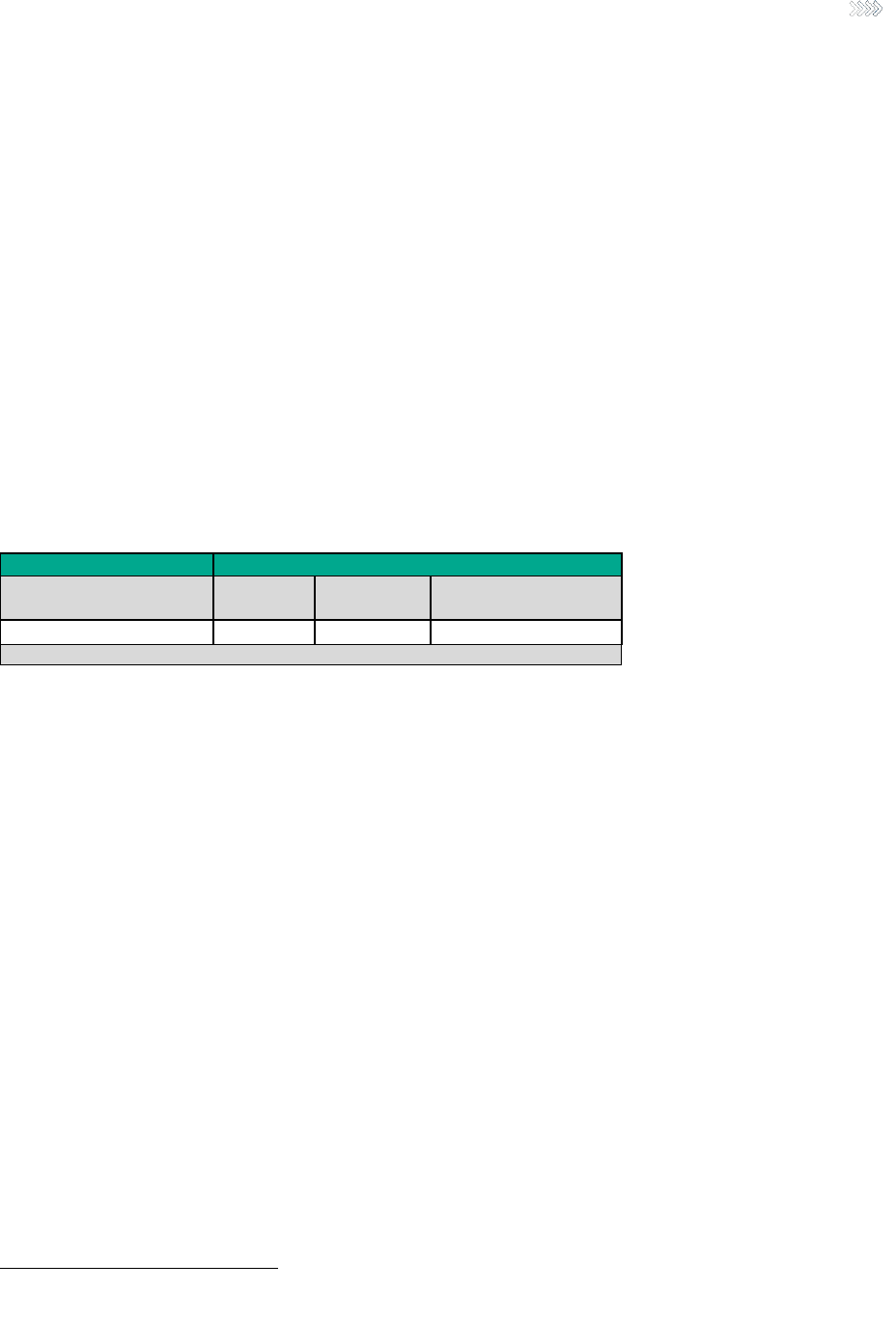
29
Copyright © 2020 Society of Actuaries
This is not the same thing as an analysis of the employer’s ROI from the introduction of the DPC option, which would
necessarily consider the DPC membership fees and the fact that the employer no longer pays for DPC-covered services
via FFS claims. We address the employer’s ROI from the DPC option later in this section. The assessment of the impact
of the DPC option on member overall demand for health care services provided in this section directly addresses the
question of whether the DPC option resulted in a reduction in systemwide health care utilization.
The risk-adjusted results normalize the unadjusted results for the estimated differences in health statuses between
the two cohorts. DPC members had 19.90% lower claim costs on an unadjusted basis and 12.64% lower claim costs
on a risk-adjusted basis during the two-year period of interest. Both differences were statistically significant (p-values
< .01). The 90% confidence interval
32
for the risk-adjusted difference in claim costs ranged from −6.41% to −18.87%
(DPC claim costs lower than traditional).
These results suggest that approximately one-third of the observed differences in claim costs between the DPC and
traditional cohorts is caused by differences in health status between the cohorts (−12.64%/−19.90% − 1). However,
even after adjusting for differences in health status, the DPC cohort experienced a statistically significant reduction in
total claim costs relative to the traditional cohort during the same time period, meaning that enrollment in the DPC
option was associated with a reduction in overall member demand for health care services.
Figure 8
DPC OPTION VS. TRADITIONAL OPTION: RELATIVE CLAIM COST DIFFERENCES
DPC vs. Traditional Health Care Cost Differences
Metric
Unadjusted
Actual
Risk-Adjusted
Actual
Risk-Adjusted Actual
90% Confidence Interval
Allowed Claims Cost PMPM
−19.90%*
−12.64%*
−6.41% to −18.87%
* The p-value < .01 (statistically significant result with 99% confidence).
Figure 9 shows the unadjusted and risk-adjusted relative differences in PMPM claim costs between the DPC and
traditional cohorts by type of service. The risk-adjusted results normalize the unadjusted results for the observed
differences in health status between the two cohorts. We also provide the baseline distribution of allowed claim costs
by type of service. The baseline distribution is based on claim costs from the traditional cohort.
Types of service with at least 5.0% of baseline claim costs are highlighted in turquoise. Readers are cautioned against
relying on results for types of service with limited claim volumes, because the observed differences for these services
are likely to be highly volatile. We have only conducted statistical testing for the turquiose-highlighted types of
services (i.e., those with at least 5.0% of baseline claim costs).
32
A 90% confidence interval means that we would expect the true value of the difference in claim costs to be in the stated range
90% of the time.

30
Copyright © 2020 Society of Actuaries
Figure 9
DPC OPTION VS. TRADITIONAL OPTION RELATIVE CLAIM COST DIFFERENCES
DPC vs. Traditional Health care Cost Differences
Type of Service
% of
Allowed
Costs
Unadjusted
DPC vs.
Traditional
Risk-Adjusted
DPC vs.
Traditional
Inpatient Total
9.1%
−12.78%
−8.19%
Outpatient: Emergency Department
10.9%
−49.81%***
−52.50%***
Outpatient: Surgery
15.6%
−11.37%
−5.36%
Outpatient: Other
6.4%
−28.05%
−23.18%*
Physician: Inpatient (non-Maternity)
1.4%
−29.50%
−24.33%
Physician: Maternity
0.5%
+0.62%
+8.00%
Physician: Emergency Department
1.1%
−32.23%
−35.86%
Physician: Outpatient Surgery
6.4%
−12.55%
-6.13%
Physician: Preventive Services
5.3%
−39.92%***
−35.51%***
Physician: Primary Care Visits†
2.3%
−20.65%
−14.83%
Physician: Specialist Office Visits†
Physician: Urgent Care Visits
0.5%
−24.41%
−18.86%
Physician: Other
8.0%
−5.72%
+1.20%
Other: Ambulance
0.4%
−33.16%
−23.57%
Other: DME/Medical Supplies
1.6%
−11.64%
+1.05%
Other: Home Health
0.0%
−81.7%
−79.07%
Prescription Drugs
28.1%
−14.95%
+1.02%
Total
100.0%
-19.90%**
-12.64%**
† The administrative medical claim data were not well populated with CMS provider specialty
codes, so we were unable to consistently distinguish between primary care and specialist physician
office visits. The results provided here are for all physician office visits (primary care and specialist
combined).
* The p-value < .05 (statistically significant result with 95% confidence).
** The p-value < .01 (statistically significant result with 99% confidence).
*** The p-value < .001 (statistically significant result with 99.9% confidence).
The DPC cohort experienced statistically significant reductions (p-values < .05) in risk-adjusted costs relative to the
traditional cohort for three of the eight detailed types of service, with at least 5.0% of baseline claim costs (Outpatient:
Emergency Department, Outpatient: Other, and Physician: Preventive Services).
Outpatient: Emergency Department
This category includes facility costs from claims corresponding to an emergency department visit. The DPC cohort
experienced a 53.6% reduction in Outpatient: Emergency Department claim costs on a risk-adjusted basis relative to
the traditional cohort, and this difference was statistically significant (p-value < .001). We further analyze differences
in emergency department usage later in this section.
This finding is consistent with a narrative coming from the proponents of DPC. The explanation would be that the DPC
model leads to reductions in emergency department usage due to the enhanced PCP access provided to DPC
members. Members of DPC practices can typically schedule same-day appointments during office hours and
essentially have 24/7 access to their PCPs via online or phone consultations.

31
Copyright © 2020 Society of Actuaries
Outpatient: Other
Included in this category are all outpatient facility claim costs (i.e., those not corresponding to an inpatient admission)
for services other than emergency department or surgery. This includes radiology, pathology, hospital pharmacy and
preventive services such as the facility charges for colonoscopies. The DPC cohort experienced a 22.2% reduction in
Outpatient: Other claim costs on a risk-adjusted basis relative to the traditional cohort, and this difference was
statistically significant (p-value < .01). The largest reduction in risk-adjusted Outpatient: Other claim costs for the DPC
cohort came from hospital pharmacy, preventive, pathology/lab services and residual noncategorized hospital charges
not relating to an admission.
Proponents of the DPC model state that this model of care leads to reductions in unnecessary diagnostic and other
facility services through increased visit times and less administrative burden on DPC physicians. Many DPC physicians
state that traditional primary care visits, which average just 13 to 16 minutes, provide physicians with inadequate time
to comprehensively diagnose and provide care to their patients, and this lack of time leads to higher-than-necessary
diagnostic referrals. The results here are mixed relating to these claims; while Outpatient: Other costs were lower due
to reduced hospital pharmacy, preventive and pathology/lab services, the DPC cohort had higher radiology costs than
the traditional cohort.
Physician: Preventive Services
This category includes physician claims for immunizations, annual physical exams, well-baby exams and other
professional services, such as colonoscopies. The DPC cohort experienced a 35.6% reduction in Physician: Preventive
claim costs on a risk-adjusted basis relative to the traditional cohort, and this difference was statistically significant (p-
value < .001). There was almost no difference in the risk-adjusted claim costs for well-baby exams and other
professional services; the decrease for the DPC cohort was the result of lower risk-adjusted claim costs for
immunizations and annual physicals. We hypothesize that the difference in annual physical exams may be due to the
increased and no-cost access to primary care provided to the DPC cohort. If DPC providers are able to establish
relationships that are more continuous with their patients through longer visits and increased access, then patients
may be less likely to schedule specific visits each year for a physical exam. This does not necessarily mean that the
DPC cohort is receiving less preventive care than the traditional cohort is, if the DPC providers during other visits are
monitoring clinical factors typically reviewed in annual physical exams.
Emergency Department Visits
We compared the number of annual emergency department visits per 1,000 members per year between the cohorts,
which is calculated for each cohort as the number of unique encounters at the emergency department, divided by
the number of total member months for the two-year period, multiplied by 12,000.
Figure 10 shows the unadjusted and risk-adjusted relative differences in emergency department utilization rates
between the DPC and traditional cohorts. The risk-adjusted results normalize the results for the estimated differences
in health status between the two cohorts. For this comparison, we used MARA risk scores specific to emergency
department usage. The DPC members had 36.39% lower usage on an unadjusted basis and 40.51% lower usage on a
risk-adjusted basis during the two-year period of interest. Both differences were statistically significant, with p-values
less than .001. The 90% confidence interval for the risk-adjusted difference in the utilization rate ranged from −28.42%
to −52.60% (DPC usage lower than traditional).

32
Copyright © 2020 Society of Actuaries
Figure 10
DPC OPTION VS. TRADITIONAL OPTION: RELATIVE EMERGENCY DEPARTMENT
USAGE DIFFERENCES
DPC vs. Traditional Utilization Rate Differences
Metric
Unadjusted
Actual
Risk-Adjusted
Actual
Risk-Adjusted Actual
90% Confidence Interval
Emergency Department
Utilization Rate (visits/1,000)
−36.39%***
−40.51%***
−28.42% to −52.60%
*** The p-value < .001 (statistically significant result with 99.9% confidence).
Inpatient Hospital Admissions
We compared the number of annual inpatient hospital admissions per 1,000 members per year between the cohorts,
which is calculated for each cohort as the number of unique hospital admissions, divided by the number of total
member months for the two-year period, multiplied by 12,000.
Figure 11 shows the unadjusted and risk-adjusted relative differences in inpatient hospital utilization rates between
the DPC and traditional cohorts. The risk-adjusted results normalize the results for the estimated differences in health
status between the two cohorts. For this comparison, we used risk scores corresponding to inpatient hospital allowed
claim costs for the normalization. The DPC members had 25.54% lower hospital admissions on an unadjusted basis
and 19.90% lower hospital admissions on a risk-adjusted basis during the two-year period of interest. However,
neither difference was statistically significant. The 90% confidence interval for the risk-adjusted difference in the
utilization rate ranged from −53.83% to 14.03% (DPC usage lower than traditional).
The 90% confidence interval range for the inpatient hospital admission rate was about 68%, which compares to 90%
confidence interval ranges of about 12% for total allowed claim costs and about 24% for emergency department
usage. The low frequency of inpatient hospital admissions during the two-year period causes the comparatively large
range for the confidence interval. There were 40 admissions for the DPC cohort of 912 members and 63 admissions
for the traditional cohort of 1,074 members during the two-year period of interest. Thus, our conclusion is that there
was insufficient data to determine whether the DPC option affected the inpatient hospital admission rate with
statistical significance.
Figure 11
DPC OPTION VS. TRADITIONAL OPTION: RELATIVE INPATIENT HOSPITAL
ADMISSION RATE DIFFERENCES
DPC vs. Traditional Utilization Rate Differences
Metric
Unadjusted
Actual
Risk-Adjusted
Actual
Risk-Adjusted Actual
90% Confidence Interval
Inpatient Hospital Utilization
Rate (admits/1,000)
−25.54%
−19.90%
−53.83% to 14.03%
* The inpatient results did not represent statistically significant reductions in utilization rates.
Total Employer Costs (DPC ROI)
Whether a particular DPC option generates a positive ROI for a particular employer is dependent upon many factors
specific to that employer and the way in which its DPC option was implemented. These factors include (but are not
limited to) the portion of the DPC membership fee covered by the employer, other plan design changes or contribution
changes made by the employer as part of the DPC option, and the effects of the DPC option on member utilization of
nonprimary care services. In the immediately preceding subsections, we have assessed the impact of the DPC option
on overall member demand for health care services. We now turn our attention to the employer’s ROI, which, in
addition to the impacts on overall member demand for health care services, includes other aspects of implementing
the DPC option, such as employer contributions and DPC fees paid by the employer.
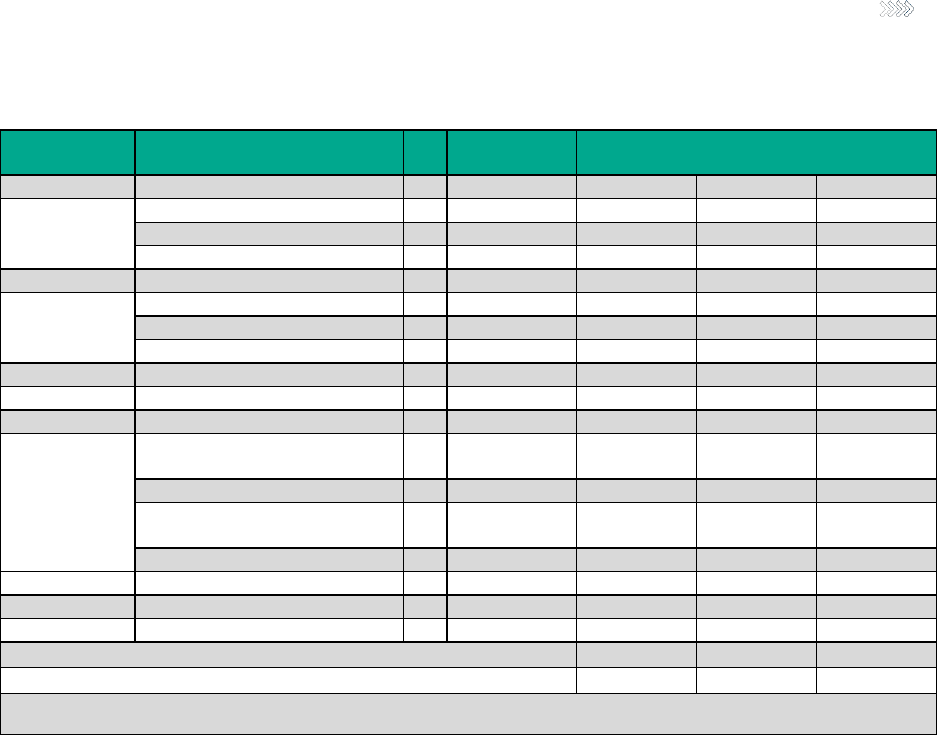
33
Copyright © 2020 Society of Actuaries
Figure 12
IMPACT OF THE DPC OPTION ON TOTAL EMPLOYER NONADMINISTRATIVE PLAN COSTS*
Actual Results
(DPC option)
Imputed Results Under Traditional Option
Low
Mid
High
Non-DPC-
Covered
Services
Allowed Claim Cost PMPM
(A)
$336
$359
$385
$415
% Paid by Plan
(B)
85%
85%
85%
85%
Plan Paid Claim Cost PMPM
(C)
$286
$306
$327
$352
DPC-Covered
Services
Allowed Claim Cost PMPM
(D)
$8
$9
$9
$10
% Paid by Plan
(E)
0%
85%
85%
85%
Plan Paid Claim Cost PMPM
(F)
$0
$7
$8
$9
All FFS Services
Plan Paid Claim Cost PMPM
(G)
$286
$313
$335
$360
Non-FFS
Services
Plan Cost of Medical Deductibles
PMPM
(H)
$31
$0
$0
$0
Plan Cost of $750 HRA PMPM
(I)
$0
$38
$38
$38
Plan Cost of DPC Membership
PMPM
(J)
$61
$0
$0
$0
Total Plan Non-FFS Cost PMPM
(K)
$92
$38
$38
$38
All Services
Total Plan Cost PMPM
(L)
$378
$350
$373
$398
Imputed Plan Savings from DPC Option PMPM
−$27
-$5
$20
Imputed Plan Savings from DPC Option (% of nonadministrative costs) †
−7.8%
−1.3%
5.2%
* The values in Figure 12 are rounded to the nearest dollar.
† A positive value here implies savings to the plan whereas a negative value here implies increased costs to the plan.
Figure 12 Key
(A) Allowed claim costs for non-DPC-covered services. Includes all medical and prescription drug claims other
than primary care services. The Actual Results column indicates the actual PMPM allowed claim costs for the DPC
cohort. The Imputed Results Under Traditional Option column estimates what the claim costs would have been
for the DPC cohort not enrolled in the traditional option. The imputed claim costs are equal to the actual claim
costs divided by one minus the risk-adjusted relative difference in claim costs between the DPC and traditional
cohorts. The mid-estimate uses the mean difference, while the low and high estimates use the 90% confidence
interval endpoints from Figure 8.
• Low DPC Savings Amount: $336 / (1 − 6.41%) = $359
• Mid DPC Savings Amount: $336 / (1 − 12.64%) = $385
• High DPC Savings Amount: $336 / (1 − 18.87%) = $415
(B) Percentage of allowed claim costs for traditional covered services expected to be paid by the employer. Based
on an analysis of historical claim costs for the employer, we estimate that the plan is expected to cover
approximately 85% of allowed claim costs under the traditional option. Differences between cost sharing under
the traditional and DPC options for major medical coverage are accounted for in rows H and I.
(C) Paid claim costs calculated as the allowed claim costs multiplied the percent paid by plan (actuarial value). (C)
= (A) x (B).

34
Copyright © 2020 Society of Actuaries
(D) Allowed claim costs for DPC-covered services (primary care office visits). We estimated the actual claim cost
for primary care office visits as actual claim cost for all office visits multiplied by expected percentage of all office
visits for primary care, because we were unable to consistently distinguish between primary care and specialist
physician office visits in the claim data. The expected percentage of all office visits for primary care was based on
the Milliman HCGs. See (A) for a description of the actual versus expected costs.
(E) Estimated percentage of allowed costs for DPC-covered services (primary care office visits) covered by the
plan. Under the DPC option, the plan does not reimburse the DPC providers via FFS claims for these services, so
the actuarial value in the Actual Results column is 0%. The DPC providers are reimbursed for these services
through the DPC membership fee (row J). Under the traditional option, the same actuarial value for non-DPC-
covered services applies (85%).
(F) Paid claim costs for DPC-covered services calculated as the allowed claim costs multiplied by the actuarial
value. (F) = (D) x (E).
(G) Total plan paid claim costs on a FFS basis for medical and prescription drugs. This is before the consideration
of the modified cost sharing for major medical coverage for the DPC option, as well as the HRA contribution for
the traditional option. (G) = (C) + (F).
(H) Estimated value of the plan covering the routine medical and major medical deductibles for members enrolled
in the DPC option. For single employees, these deductibles are $150 and $600, respectively. Based on the
Milliman HCGs, we estimate the value of the plan waiving these two deductibles for members enrolled in the DPC
option to be worth $31 PMPM on average. Because we used an actuarial value of 85% based on the traditional
option in row B for members enrolled in the DPC option and the plan waives these deductibles for members
enrolled in the DPC option, we add in the value of these deductibles to plan costs in row H.
(I) Estimated value of the plan HRA contributions for members enrolled in the traditional option. For single
employees, this amount is set to $750 per year. Members use the HRA to cover 100% of major medical claim
costs after the routine medical deductible. After a member has exhausted all HRA funds, the major medical
deductible applies. Based on the Milliman HCGs, we estimate the value of the HRA contribution to members to
total approximately $38 PMPM. Because the estimated actuarial value of 85% for the traditional option is before
consideration of the HRA contributions, we add in the value of these contributions in row I.
(J) The plan covers the DPC membership fee for members enrolled in the DPC option. Based on assumed monthly
DPC membership fees of $75 for adults and $40 for children and the enrolled mix of adults and children in the
DPC option, we estimate the cost of this coverage to the employer to total approximately $61 PMPM. The
employer did not provide us with its actual DPC membership fees; these assumptions are based on our DPC
market survey results.
(K) The total cost to the plan from non-FFS costs. (K) = (H) + (I) + (J).
(L) The total cost to the plan from the FFS claim and non-FFS cost items. This amount does not include any plan
administrative costs, which we assume would be equal between members enrolled in the DPC option and
traditional option. (L) = (G) + (K).

35
Copyright © 2020 Society of Actuaries
Figure 12 provides our estimated impact of the DPC option on total nonadministrative plan costs for the employer
during the two-year period of interest. We used the overall adjusted DPC savings of 12.64% from Figure 8 to estimate
what the costs for the DPC cohort would have been during this time period if those members had been enrolled in
the traditional option. Thus, we backed out the estimated DPC savings from the DPC cohort’s actual costs during this
time period to impute what the corresponding costs for this cohort would have been under the traditional option,
i.e., $366 / (1 − 0.1264) for the midpoint result. The low and high estimates provided in Figure 9 use the 90%
confidence interval estimates of the impact of the DPC option on claim costs from Figure 7 (−6.41% to −18.87%). The
lowest savings translate to the lowest DPC ROI for the employer. We broke out claim costs in Figure 9 between services
covered or not by the DPC providers under the DPC option. Under the DPC option, the employer pays for these
services via the monthly DPC membership fee instead of paying claims on a FFS basis.
The resulting overall actual plan costs for the DPC cohort, including the cost of covering the DPC membership fee, is
$378 PMPM (row L) during this period. If the DPC cohort had instead been enrolled in the traditional option during
this time period, we estimated that the total plan costs for the cohort would have totaled between $350 PMPM and
$398 PMPM, with a mid-estimate of $373 PMPM. Therefore, under the high DPC-savings scenarios, we estimated that
the DPC option saved the employer approximately $21 PMPM or 5.2% of total nonadministrative plan costs. Under
the low and mid DPC-savings scenarios, we estimated that the DPC option increased costs for the employer by
approximately $27 PMPM and $5 PMPM, respectively, or 7.8% and 1.3% of total nonadministrative plan costs.
The employer did not provide us with its actual DPC membership fees, so we based our ROI analysis on assumed DPC
membership fees from our DPC market survey. If the employer’s actual DPC membership fees varied from our
assumed level, then the actual ROI would have also varied from our estimated level.
Our analysis did not consider any administrative costs, such as TPA fees or stop-loss reinsurance premiums. We
assume that total per-member administrative costs for the employer’s self-insured health benefits plan are equal
between members enrolled in the DPC and traditional options, and thus these amounts have no impact on our
evaluation of the DPC option on an absolute basis.

36
Copyright © 2020 Society of Actuaries
7. Case Study Generalized Actuarial Framework for Funding Employer
DPC Options
We expect that most employers considering the addition of a DPC option for their self-insured health benefits plans
will want to fund these options on at least a cost-neutral basis (i.e., with no increase in plan costs). In this section, we
provide a generalized actuarial framework that could be used to determine the feasibility of savings for employers as
they consider funding structures for a DPC option.
This framework is provided on a cost-neutral basis, with the hypothetical employer using estimated DPC claim savings
to fully (and exactly) cover DPC membership fees. Additional analysis could easily be incorporated if the employer
wished to retain a portion of the DPC claim savings to reduce plan costs or if it were acceptable to the employer for a
DPC option to increase overall plan costs due to other benefits of the DPC option (e.g., increased access to primary
care from members enrolled in the DPC option).
Development of Estimated DPC FFS Claim Cost Savings
Figure 13 illustrates the development of a generalized actuarial model. We discuss the key inputs and considerations
for each variable below the figure.
Figure 13
DEVELOPMENT OF ESTIMATED DPC FFS CLAIM COST SAVINGS
Type of Service
Base
Paid
PMPM
Selection
Factor
2-year
Trend
Factor
% FFS
Carved
Out
DPC %
Savings
Projected
FFS Paid PMPM
(no DPC)
Projected
FFS Paid PMPM
(w/ DPC)
(A)
(B)
(C)
(D)
(E)
(F)=(A)*(B)*(C)
(G)=(F)*[1-(D)*(1-
(E)]
Non-DPC-Covered Services
Inpatient Facility
Non-Maternity
$97.50
90.0%
113.4%
0.0%
5.0%
$99.53
$94.55
Maternity
$12.50
90.0%
113.4%
0.0%
0.0%
$12.76
$12.76
SNF
$2.50
90.0%
113.4%
0.0%
0.0%
$2.55
$2.55
Outpatient Facility
Emergency
Department
$27.50
90.0%
116.6%
0.0%
35.0%
$28.87
$18.76
Surgery
$45.00
90.0%
116.6%
0.0%
5.0%
$47.24
$44.88
Other
$62.50
90.0%
116.6%
0.0%
10.0%
$65.61
$59.05
Professional
Inpatient Non-
Maternity
$10.00
90.0%
111.3%
0.0%
5.0%
$10.02
$9.52
Maternity
$5.00
90.0%
111.3%
0.0%
0.0%
$5.01
$5.01
Outpatient Surgery
$20.00
90.0%
111.3%
0.0%
5.0%
$20.03
$19.03
Emergency
Department
$5.00
90.0%
111.3%
0.0%
35.0%
$5.01
$3.26
Urgent Care
$2.50
90.0%
111.3%
0.0%
0.0%
$2.50
$2.50
Specialist Physician
$10.00
90.0%
111.3%
0.0%
50.0%
$10.02
$5.01
Other Professional
$47.50
90.0%
111.3%
0.0%
10.0%
$47.58
$42.82
Other Medical
Ambulance
$2.50
90.0%
111.3%
0.0%
0.0%
$2.50
$2.50
Home Health
$2.50
90.0%
111.3%
0.0%
0.0%
$2.50
$2.50
DME/Supplies
$5.00
90.0%
111.3%
0.0%
0.0%
$5.01
$5.01
Prescription Drug
$102.50
90.0%
117.4%
0.0%
0.0%
$108.30
$108.30
DPC-Covered Services
Primary Care
$10.00
90.0%
111.3%
100.0%
0.0%
$10.02
$0.00

37
Copyright © 2020 Society of Actuaries
Preventive
$10.00
90.0%
111.3%
100.0%
0.0%
$10.02
$0.00
Total Cost
$482.50
$497.59
$438.02
Categorization of Claims
The baseline claim costs need to be organized with sufficient granularity by type of service so that appropriate
assumptions can be made in relation to the DPC arrangement being considered. For example, it may be reasonable
to anticipate somewhat lower emergency department usage under the DPC option, but it may not be appropriate to
assume lower maternity-related admissions under the DPC option. Therefore, the baseline claim costs need to be
broken out by categories for which corresponding cost savings assumptions relating to the DPC option can be made
appropriately.
For the model in Figure 13, we used a mid-level grouping with 19 different categories of services taken from Milliman’s
HCGs. Additional detail, even down to the service line level or CPT/HCPCS code level, is possible depending on the
structure of the current benefit plan and claim reporting capabilities and may be necessary to improve the accuracy
of the projections, depending on the design of the anticipated DPC arrangement. However, for smaller employers,
greater amounts of detail should be balanced with the credibility of smaller cuts. Larger employers may have enough
data that credibility at greater levels of detail may not be an issue.
Base Period Paid FFS Claim Costs (column A)
To determine the feasibility and likely range of savings from the introduction of a DPC arrangement for its employees,
an employer needs to understand its costs under the current program, as well as employees’ demographic and health
profile. This information is gathered from TPAs, summarized into relevant categories and used as a baseline in the
projection of potential savings related to the introduction of a DPC option in a future period.
The optimal inputs are actual paid claim costs and membership information arising under the employer’s current
health benefit plan offering from the most recent 12 to 36 months of claim experience. In the absence of actual
employer costs, or in the case of small employers whose experience is not statistically credible,
33
multiple years of
data or manual claim costs can be used, provided those costs are appropriately adjusted to represent the employer’s
geographic location, demographic and health status profile, provider reimbursement levels, time period and benefit
design.
The importance of using an employer’s actual costs (or using properly adjusted manual costs) can be understood by
considering the variations in cost by age, geographic area, industry and population. For example, using Milliman’s
HCGs, we estimate that aggregate health care costs for a typical employer can vary across the U.S. by a ratio of 3:1 at
the metropolitan statistical area (MSA) level. Similarly, health care costs by age and gender can vary by as much as
8:1. Even after accounting for these and other demographic considerations, the overall health status of a population
can vary widely as well.
33
Actuarial credibility is the degree to which observed claim patterns for a particular population are expected to be predictive of
future claim patterns for that same population. Credibility is represented as a percentage between 0% and 100% and is generally
calculated as the square root of the ratio between the number of life years of data included in the base period and an assumed
fully credible threshold. The fully credible threshold represents the number of life years for which actuarial credibility is assumed
to be 100%. For commercial populations, 4,000 to 5,000 life years are generally considered to be fully credible, based on
Milliman’s internal research. To increase the credibility of claim experience for groups with less than 4,000 to 5,000 enrolled
members, multiple years can be used to increase the number of life years for which base period claim data is included.

38
Copyright © 2020 Society of Actuaries
This cost variation is important in understanding potential available savings from a DPC model, because our data
suggests that DPC fees across the U.S. do not vary nearly to the same degree as underlying claim costs.
34
This
difference in variability leads to the following effects.
First, employer groups with higher costs (i.e., in higher-cost areas, with older populations, in higher-cost industries)
will be more likely to generate net savings from a DPC arrangement than employers that have lower costs.
We illustrate what is effectively a volume dynamic in Figure 14.
Figure 14
ILLUSTRATION OF HIGH EMPLOYER COSTS ON POTENTIAL DPC FFS CLAIM COST SAVINGS
Scenario 1
Scenario 2
Employer
A
B
Variation
C
D
Variation
High-Cost
Area
Low-Cost
Area
Older Age
Younger
Age
(a)
Base Health care Costs
$500
$500
$500
$500
(b)
Geographic Adjustment
1.20
0.80
1.00
1.00
(c)
Average Age
1.00
1.00
1.60
0.80
(d)
Health Status
1.00
1.00
1.00
1.00
(e) = Product(a, b, c,
d)
Adjusted Costs
$600
$400
−33%
$800
$400
−50%
(f)
Assumed DPC Savings
12%
12%
12%
12%
(g) = (1 − f) x (e)
Claim Costs After DPC
$528
$352
$704
$352
(h) = (e) − (g)
Claim Savings From DPC
$72
$48
−33%
$96
$48
−50%
(i)
DPC Fee
$65
$55
−15%
$75
$45
−40%
(j) = (h) − (i)
Net Savings/Cost of DPC
$7
-$7
$21
$3
Observations from Figure 14 include:
• The effectiveness of the DPC model (row f) under both scenarios is 12% of costs. Under Scenario 1, this
uniform percentage of DPC savings drives a larger PMPM savings in the high-cost area versus the low-cost
area. However, while the DPC fee varies by area as well, that variance is smaller and, therefore, drives a
different net savings by area after consideration of the relatively fixed DPC fee.
• Under Scenario 2, both health costs by age and the savings from DPC vary by 50%. Similar to Scenario 1, DPC
fees vary much less than this, leading to different financial outcomes depending on an employer group’s
demographic composition.
Second, if a health management protocol or delivery model is effective at managing costs, it will be most effective
on sicker populations that have a greater prevalence of manageable conditions. For example, a diabetes
management program will have a negative ROI if there are no diabetics in the population to manage. However, if a
population has a larger-than-average number of diabetics, that program will stand a much better chance of having a
positive ROI, because its effectiveness is multiplied across a greater opportunity set. Thus, in addition to varying
dollar savings due to the employer group demographics and costs noted above, varying percentage savings coming
from a DPC arrangement can be assumed in certain circumstances such as a higher age or morbidity. We extend our
examples above to Figure 15.
34
Source: DPC survey data used for Section 3 and Appendix B. Detail available on request.

39
Copyright © 2020 Society of Actuaries
Figure 15
ILLUSTRATION OF HIGH EMPLOYER MORBIDITY ON POTENTIAL DPC FFS CLAIM COST SAVINGS
Scenario 3
Scenario 4
Employer
C
D
Variation
E
F
Variation
Older
Age
Younger
Age
Less
Healthy
More
Healthy
(a)
Base Health Care Costs
$500
$500
$500
$500
(b)
Geographic Adjustment
1.00
1.00
1.00
1.00
(c)
Average Age
1.60
0.80
1.00
1.00
(d)
Health Status
1.00
1.00
1.20
0.80
(e) = Product(a, b, c,
d)
Adjusted Costs
$800
$400
−50%
$600
$400
−33%
(f)
Assumed DPC Savings
14%
10%
15%
5%
(g) = (1 − f) x (e)
Claim Costs After DPC
$688
$360
$510
$380
(h) = (e) − (g)
Claim Savings From DPC
$112
$40
$90
$20
100%
(i)
DPC Fee
$75
$45
-40%
$60
$60
0%
(j) = (h) − (i)
Net Savings/Cost of DPC
$37
−$5
$30
−$40
Observations from Figure 15 include:
• Under Scenario 3, the effectiveness of the DPC model is now estimated to be 14% of costs for Employer C
because the older average age implies more manageable chronic conditions and, therefore, more savings
opportunities. Conversely, Employer D only sees a 10% savings because it has a younger population with
fewer opportunities for cost savings given the lower incidence of manageable chronic conditions. As
previously shown, the variance in the DPC fee by age is less than the variance of the projected savings by
age, which drives different net savings and possibly different decisions on the employer’s part.
• Finally, under Scenario 4, the effectiveness of DPC again varies by employer, all of which are in the same
geographic region and have the same demographic profile but differ in their employees’ health status. As
with age, it is assumed that a population with greater health care needs will also yield greater savings
opportunities. However, in this case, DPC providers do not vary their fees by the risk profiles of their
populations; therefore, the net savings is magnified for the higher-cost group over Scenario 3 (where the fee
varied by age).
As the preceding figures and discussion illustrate, it is important to have an accurate view of an employer’s current
health care costs as well as the fee structure of the DPC arrangement for employees, as the net savings are dependent
upon both of these inputs.
Estimating DPC Selection (Figure 13 column B)
Baseline costs should be as representative as possible of the population expected to enroll in the DPC option.
However, if an employer is considering the introduction of a DPC option alongside its existing traditional health plan,
it is highly likely that the population that will ultimately select the DPC option will differ from the population selecting
the traditional option in age, gender and health status. If the baseline claim costs (column A) are based on the
historical claim costs for the combined population (those who will select the DPC option and those who will not), then
a DPC selection factor may be needed to estimate the relative difference in claim costs between the baseline
population and the population expected to enroll in the DPC option. In the case of an employer planning to enroll all
employees and dependents in the DPC option in the future period, this factor is unnecessary (because it would be
equal to 100%).

40
Copyright © 2020 Society of Actuaries
It may be difficult to estimate this factor until multiple studies are conducted on midsize to large employer groups
offering a dual choice between DPC and traditional options. In the absence of published research on historical DPC
selection patterns, historical experience from employer health plan choice offerings—e.g., health maintenance
organization (HMO), preferred provider organization (PPO), and HDHP—may be instructive. Further, it may be
prudent to select a conservative assumption for the DPC option feasibility analysis; that is, pick a reasonable selection
factor less than 100% to be conservative about the potential PMPM savings that may result from the DPC option.
It is possible that in an employer health benefit offering situation (as opposed to an individual seeking out a DPC
provider and individually contracting), employees may perceive the DPC option as an HMO-like offering because both
typically require a PCP selection. Because healthier individuals generally visit their PCPs less frequently than less
healthy individuals, the assignment to a single PCP under an HMO or DPC option may be less disruptive for healthy
individuals than for less healthy individuals. Thus, we surmise that, given a choice, healthier individuals may have less
aversion to enrolling in an HMO requiring a PCP or, in this case, a DPC arrangement.
This selection dynamic is important for the same reasons we noted above: Healthier individuals under a DPC may
drive less percentage and total dollar savings relative to an average population. In Figure 13, we assumed a 90%
selection factor (i.e., a 10% favorable selection), similar to the case study (in which the cohort expected to enroll in
the DPC option has 10% lower claim costs on average than the combined base period population).
Projecting Future Period Costs Using Underlying Trends (Figure 13 column C)
Baseline claim costs will likely come from the most recent plan year, and projections will likely apply to the next plan
year. Thus, an adjustment for the medical inflation of the two-year time period is typical. If other periods are used for
the analysis, then the assumed trend factor should be modified accordingly (i.e., if the projection is not for the next
plan year but for the following plan year instead, then a three-year factor would be appropriate).
Estimating the Impact of the DPC Arrangement (Figure 13 columns D and E)
The DPC arrangement may affect future health care claim costs paid under the employer’s benefit plan relative to the
base period in two ways:
1. Services carved out of FFS claims by the DPC arrangement (column D). Under a DPC plan, a certain set
of CPT/HCPCS codes and corresponding FFS claim costs for members enrolled in the DPC option will
disappear from an employer’s claim cost data because the DPC provider furnishes these services. DPC-
covered services are those benefits (or types of service) that the DPC practice provides and covers under the
DPC membership fee. The DPC providers will be reimbursed for these services through the DPC membership
fee rather than through FFS claims submission. While many DPC providers will cover a similar set of services,
some may not, and the specific services expected to be covered under each particular employer’s DPC option
should be taken into account.
Column D, the Percentage FFS Carved Out. This represents the percentage of historical FFS claim costs that
the DPC provider is expected to furnish under the DPC option. If members are required to receive only DPC-
covered services from the DPC provider, then the appropriate assumption would be 100% (i.e., 100% of these
baseline claims will be covered under the DPC membership fee and thus have no corresponding FFS claim
costs in the future period). If members enrolled in the DPC option are still permitted to receive DPC-covered
services from traditional providers, then an assumption close to but less than 100% may be appropriate.
2. Savings on categories of claim costs impacted by the DPC arrangement (column E). As noted earlier,
the DPC arrangement will affect different categories of claims differently. For example, specialist and
emergency department utilization rates both may decrease under a DPC option but at different rates, and
maternity utilization rates may be unaffected.

41
Copyright © 2020 Society of Actuaries
Column E, the DPC Percentage Savings. This represents the percentage reduction in utilization rates based on
improved care delivery from the DPC provider.
Projecting Future Period Final FFS Claim Costs (Figure 13 columns F and G)
Column F, Projected FFS Paid PMPM. This represents projected plan claim costs assuming the status quo (i.e., without
a DPC option). The projected PMPM is specific to the population expected to enroll in the DPC option (i.e., It is not for
the entire base period population). (F) = (A) x (B) x (C).
Column G, Projected FFS Paid PMPM. This represents projected plan claim costs assuming the introduction of a DPC
option. The projected PMPM is specific to the population expected to enroll in the DPC option (i.e., It is not for the
entire base period population). (G) = (F) x [1 − (D)] x [1 − (E)].
Figure 13 provides an illustration of estimated DPC claim savings for a sample population. Baseline paid claim costs
roughly approximate national average employer claim costs from the 2019 Milliman HCGs. The claim costs represent
a typical level of care management effectiveness for large self-insured employers, and an overall actuarial value of
90% is assumed. We also used secular trend factors from the 2019 Milliman HCGs. The various assumptions relating
to the DPC option are loosely based on the observed actual results for the employer whose DPC option we evaluated
herein.
The estimates provided in Figure 13 are meant to be illustrative only. Each employer’s estimate will vary from the
Figure 13 results to the extent that baseline claim costs and other employer-specific assumptions relating to a
potential DPC option vary from the Figure 13 assumed amounts.
Overall DPC FFS Claim Cost Savings
Figure 16 summarizes the overall estimate of DPC claim savings developed in Figure 13. The total estimated DPC claim
savings estimated from illustrative Figure 13 are $59.56 PMPM ($438.02 − $497.59), and the single largest driver of
DPC claim savings is carved-out DPC services. These are services furnished by the DPC provider, covered under the
monthly DPC membership fee rather than FFS claims to be paid by the plan. The second-largest driver of DPC claim
savings is reduced outpatient facility claims, mostly from a projected reduction in emergency department usage.
Carved-out DPC services and reduced emergency department usage account for nearly two-thirds of the total
estimated DPC claim savings. The estimated level and distribution of DPC claim savings will vary depending on an
employer’s baseline claim costs, the structure of the DPC option and the characteristics of the population expected
to enroll in the DPC option.
Figure 16
SUMMARY OF ESTIMATED DPC FFS CLAIM COST SAVINGS
Source of Savings
Savings
PMPM
% of Savings
Carved-Out DPC Services
$22.54
37.8%
Lower Outpatient Facility Claims
$19.03
31.9%
Lower Physician Claims
$13.02
21.9%
Lower Inpatient Facility Claims
$4.98
8.4%
Total DPC Claim Savings
$59.56
100%
Development of DPC Membership Fee Schedule
Most DPC practices vary their monthly membership fees by enrollee age. At a minimum, DPC practices tend to vary
their membership fees between adults and children, but many also vary adult membership fees by age-bands as well.
There is no standard structure for DPC monthly fees. Figure 17 provides an illustration of how the estimated DPC claim
savings from Figure 16 can be converted into a monthly DPC fee schedule. We varied the monthly fee paid to the DPC

42
Copyright © 2020 Society of Actuaries
provider between children and four adult age-bands (under age 30, between ages 31 and 44, between ages 45 and
64, and over age 65).
Assumptions are required for the distribution of members expected to enroll in the DPC option between each
assumed age category (e.g., child, adult under age 30, etc.), as well as the desired fee relativity between each age
category. DPC providers should agree to the relationship of the DPC fees between categories. If the DPC provider
already has an existing fee structure and corresponding fee relativities for individual members enrolling in its practice,
then it may be prudent for the employer to use a similar structure and relativities.
Figure 17
DEVELOPMENT OF DPC MEMBERSHIP FEE SCHEDULE
DPC Membership
Age Category
% DPC
Members
Relative
Fee
Monthly DPC Fee
Calculated
Rounded
(A)
(B)
(C)
(D)
Child
30%
1.00
$24.19
$25
Adult < Age 30
15%
1.50
$36.28
$35
Adult Ages 31-44
15%
2.50
$60.47
$60
Adult Ages 45-64
35%
3.75
$90.71
$90
Adult Over Age 65
5%
5.00
$120.94
$120
Average
100%
2.46
$59.56
$59.25
Average Child Fee:
$25.00
Average Adult Fee:
$73.92
The steps used in Figure 17 to develop the monthly DPC membership fee schedule are as follows:
1. Calculate the composite relative fee factor. This is the product of the assumed membership mix in column A
and relative fees by fee category (column B). For the illustrated example provided in Figure 14, the composite
relative fee factor is 2.46.
2. Calculate the monthly fee for each fee category. This is determined as the total DPC claim savings PMPM
multiplied by the relative fee for the fee category divided by the composite relative fee factor. For example,
the calculated monthly fee in Figure 17 for the child fee category is calculated as $59.56 x 1.00 / 2.46 =
$24.19.
3. Round the calculated monthly fees. Round to the level desired by the employer and DPC provider for
administrative simplicity. We rounded the monthly fees in Figure 17 to the nearest $5.
The resulting DPC fee schedule from this approach represents the tiered DPC membership fees based on the
estimated DPC claim savings.
If the resulting monthly fees from this modeling are insufficient to contract with a DPC provider, then other changes
such as increased member cost sharing for traditional covered services may be necessary to produce a cost-neutral
DPC funding structure. If the employer is able to either locate a DPC provider with a fee schedule more favorable than
the cost-neutral structure or negotiate such a schedule,
35
then the DPC option may be expected to reduce plan costs,
including the membership fee. It may be prudent for employers to evaluate a range of scenarios. A conservative
estimate of DPC claim savings may be to assume carve-out savings (column D in Figure 13) for the DPC option and
minimal impacts from the DPC option on other utilization rates (column E). If the resulting DPC fee schedule under
35
Based on author interviews with DPC physicians, fee negotiation is not a prevailing market practice on the part of DPC
providers.

43
Copyright © 2020 Society of Actuaries
these assumptions is sufficient to contract with a DPC provider, then it may be likely that the DPC option will generate
a net ROI for the employer.
Other Considerations for Employers Considering a DPC Option
Due to the newness of the DPC model of care, as well as the inclusion of DPC options in self-insured employer health
benefit plans, it is likely that the implementation of such DPC options will vary materially from one employer to the
next. While the actuarial framework that we outline provides a useful template for employers to evaluate the
feasibility, structure and funding of such options, it is not all-encompassing of every potential DPC option. Other items
for employers to consider when evaluating DPC options include:
DPC-Covered Services. In determining the feasibility of a positive financial return to the employer from a DPC
arrangement, it is important to understand the scope of covered services under the fee, as well as any access to
services that are not covered under the fee but are made available to the member at lower prices than they may
otherwise be able to get outside of the DPC arrangement. Many DPC providers negotiate reduced prices for
diagnostics, prescription drugs and even certain surgical services and provide access for their members to these
comparatively low-cost services. Our development of estimated claim savings from a DPC option provided in Figure 12
above assumes that the DPC provider limits its covered services to primary care office visits and office-based
preventive services. Most DPC providers also cover basic diagnostic tests and minor surgical procedures.
Membership fees often include access to other low-cost services, such as diagnostic radiology, laboratory tests and
common prescription drugs, at wholesale or near-wholesale costs. This access to lower-cost services can also
contribute to lower employer costs. The framework presented in Figure 13 allows for input of these savings in column
E but also requires the claim categories to be at the appropriate level of detail.
Other Plan Design Changes. Employers may wish to consider other plan design changes for the DPC option beyond the
coverage of the DPC membership fee. For example, the employer whose DPC option we evaluated also reduced the
routine medical and major medical deductibles to $0 for members enrolled in the DPC option. Additionally, members
enrolled in the DPC option were not provided with employer HRA contributions.
For employers estimating insufficient FFS savings from the DPC option to fully offset required DPC membership fees,
reducing the richness of the plan design for non-DPC-covered services may generate the additional savings required
to introduce the DPC option on a cost-neutral basis to the employer. To incorporate the impact of other plan design
changes in the actuarial framework provided in Figure 12, the estimated claim costs with the DPC option (row G)
would be additionally modified for the estimated impact of the plan design change. An assumption about the impact
of the plan design change on net claim costs would be required. For example, if the employer currently covers
approximately 90% of inpatient facility claim costs and it is considering plan design changes that would reduce this
coverage to approximately 85% of inpatient facility claim costs, then row G would be additionally multiplied by a factor
of 0.944 (85% / 90%). This assumed reduction in claim costs would result from an increase in employee cost sharing,
rather than a reduction in utilization resulting from improved care management under the DPC option.
Employee Contributions. Often, a key factor driving employee enrollment decisions in employer health benefit plan
designs and other programs is the employee contribution structure. Employee contributions for self-insured employer
health benefit plans refers to the portion of the monthly premium equivalent rates that employees provide to the
plan through payroll deductions. An employee contribution incentive for enrolling in a DPC option is likely to increase
enrollment in the option. If an employee contribution incentive is provided to employees, the employer should
consider the financial impact of any such incentives in its evaluation of the funding structure for the DPC option.
Reduced employee contributions would at least partially offset DPC claim savings and, depending on the extent of the
incentive, may fully offset DPC claim savings before consideration of the DPC membership fee.

44
Copyright © 2020 Society of Actuaries
Note, too, that employee contributions can have an impact on ultimate DPC savings (on both a percentage and PMPM
basis). Recall that the DPC savings are at least partially dependent on the overall health status of the population
selecting the DPC option. The potential for favorable selection (i.e., healthy people selecting) into the DPC, and hence
lower savings and ROI, can be reduced by offering a greater financial incentive for enrolling in the DPC option, thereby
enrolling a larger percentage of the employer group (and potentially the entire group).
DPC Enrollment and Adverse Selection. The employer whose DPC option we evaluated for our analysis allowed
individual members (employees or dependents) to enroll or disenroll from the DPC option at the beginning of any
month. Employers considering DPC options will need to determine the enrollment mechanism for their own DPC
options. For example, will enrollment in the DPC option be permitted at the member level, or will enrollment be
required at the employee level? Most likely, enrollment for any other plan designs offered through the employer
health benefits plan require enrollment at the employee level. Additionally, will enrollment and disenrollment be
permitted at any time or only during open enrollment? Permitting enrollment or disenrollment at any time may induce
adverse selection and result in higher overall costs on the plan, depending on the plan design variations between the
DPC option and the traditional plan options. It would also make it difficult to understand whether the DPC option has
any near- and long-term effects on member health care outcomes and the ROI for claim costs.
Compliance. There are instances of regulatory uncertainty around the DPC model, and employers considering the
implementation of a DPC option should consult with appropriate employee benefits compliance advisors as a part of
their evaluations. Currently, the IRS considers DPC to represent a health plan rather than a medical expense, which
means that individuals wishing to contribute to HSAs are ineligible from enrolling in a DPC option.
Use of DPC Provider. In the illustrated framework provided in Figure 12, the single largest driver of DPC claim savings
is carved-out DPC services (i.e., services provided by the DPC provider and covered under the membership fee). We
assume in the example that members are required to receive DPC-covered services exclusively from the DPC provider
(hence the assumed carve-out percentage in the example is 100%). If this is required, the employer and DPC
practices(s) will need to ensure there is enough physician capacity to handle all employees’ primary care needs.
If there is no requirement that those enrolled in the DPC option receive DPC-covered services from the DPC
provider(s), then the carve-out percentage in our framework would be less than 100%. If there is no cost sharing
associated with receiving DPC-covered services from the DPC provider, then it is still likely, even though not required,
that members enrolled in the DPC option will receive most of these services from the DPC provider.
Referrals. Employers, DPC providers and employees will need to have clear guidance on specialist referrals, because
the major medical plan will almost certainly be a network-based plan. Referrals to out-of-network specialists may cost
patients more out of pocket and possibly raise overall health plan costs as well. DPC providers should be aware of the
employer’s network configuration, and employees should ensure that any referrals to specialists are not out of the
network.
Employee Education. Many employees and covered dependents are likely unfamiliar with the DPC model of care and
potential benefits of enrolling in a DPC option, as well as any restrictions. As with any new program, service or plan
design introduced through an employer health benefits plan, it may be prudent for employers to provide employee
education when introducing a DPC option. Such educational information or sessions may help to maximize enrollment
in, and savings from, the DPC option, as well as minimize surprises to members after enrollment.
Outcomes Monitoring. Employers implementing DPC options should monitor the performance of these arrangements
after implementation. The assumptions used to develop the initial DPC option funding structure should be compared
to actual experience as it emerges (usually after at least a full year under the DPC arrangement) and the funding
structure should be adjusted if actual DPC claim savings vary materially from expected. Employers should also consider

45
Copyright © 2020 Society of Actuaries
the short- and long-term potential impacts of DPC. For example, reduced utilization of emergency department claims
is likely to be realized very soon after implementation of a DPC option, because greater access to the DPC provider is
an immediate benefit. However, other reductions in health care costs, such as reduced inpatient admissions, may
emerge over longer periods of time as the benefits of a longitudinal physician-patient relationship, improved patient
engagement and other results take hold. Further, sharing the detailed utilization data and health care outcomes
associated under the DPC option with the contracted DPC providers, based on an appropriate methodology, may help
them modify their care delivery to improve performance. If overall health care claim savings from introducing a DPC
are better than expected, sharing positive results with the DPC provider may help reinforce the relationship between
the employer and the provider. Employers experiencing better-than-anticipated results may wish to leverage the
increased DPC claim savings, adding additional incentives to induce more enrollment in the DPC option.

46
Copyright © 2020 Society of Actuaries
8. Case Study Discussion and Limitations
Discussion
We observed positive effects from the introduction of a DPC option in the employer’s self-insured health benefits
plan. About half of the members included in our analysis enrolled in the DPC option, and the DPC option was
associated with a statistically significant reduction in overall health care claim costs and emergency department usage
after controlling for differences in age, gender and health status between the DPC and traditional cohorts. The DPC
option was also associated with a lower inpatient facility admission rate, but the difference was not statistically
significant due to the small number of admissions during the two years analyzed. However, we also estimated that
the introduction of a DPC option increased total nonadministrative plan costs for the employer, after consideration
of the DPC membership fee and other plan design changes for members enrolled in the DPC option
The estimated health status of members choosing to enroll in the DPC option was more favorable than members
enrolling in the traditional option. This observation is consistent with arguments that some critics of the DPC model
of care made that healthier members enroll in DPC. We believe there are two key points with regard to this
observation:
1. The estimated selection pattern in our case study emphasizes the need for any analysis of cost and utilization
outcomes for DPC programs to account for the health status and demographics of the DPC population
relative to a control group or benchmark population. Without appropriate consideration for how differences
in underlying health status affect observed claim costs and utilization patterns, analyses could attribute
certain outcomes to DPC inappropriately. We urge readers to use caution when reviewing analyses of DPC
outcomes that do not explicitly account for differences in population demographics and health status and do
not make use of appropriate methodologies.
2. We believe the selection pattern of members enrolling in DPC is likely to differ between members enrolling
through an employer DPC option (as in our case study), with the employer covering the DPC membership fee
versus members enrolling on their own and thus paying for DPC membership fees out of pocket. We believe
this may be driven by the following factors:
• Members choosing to enroll in DPC and pay on their own may be less healthy simply because they
are better able to justify the recurring monthly DPC membership fee (which is likely in addition to
major medical insurance premiums) than members not choosing to enroll in DPC on their own. For
example, assuming copays of $35 and $50 for PCP and specialist, respectively, under traditional
coverage, an individual with a chronic condition would only have to see either a PCP or specialist
roughly twice a month on average (total cost of $85) to justify paying the DPC membership fee,
where there are typically no copays. Members without the need for this level of recurring primary
care may be less likely to see the financial value in enrolling in a DPC practice.
In addition to the financial considerations, members will value the greater access to the DPC
provider, in terms of appointment time waits and lengths of visit more so than a member with less
perceived need for regular primary care.

47
Copyright © 2020 Society of Actuaries
• Under an employer option, DPC—with its exclusive PCP relationship—may be perceived as a form
of HMO, with the PCP as the gatekeeper. Historically, the HMO gatekeeper restriction has tended
to cause favorable selection for HMOs relative to broader access plans, such as PPOs, because those
with fewer health care needs will be affected less by the restriction. Thus, given the option,
employees with fewer anticipated PCP encounters may be more likely to choose a DPC option for
the same reason.
That said, the enrollment pattern under an employer’s DPC option could vary based on many other factors, including
but not limited to socioeconomic factors attributable to employees including age, gender and health status profiles;
the net cost of the DPC option to the employee; covered services; provider location; and convenience.
Our data analysis and generalized actuarial framework show that implementing a DPC option may be financially viable
for employers self-insuring their health benefit plans. Depending on the baseline level of claim costs in an employer’s
plan, how the DPC option is structured and the cost savings generated by the DPC delivery model, the introduction of
a DPC arrangement could be done on a cost-neutral basis or may potentially lead to overall cost savings for the
employer. The potential benefits to employers from the introduction of a DPC option may go beyond cost
considerations, however. A DPC option may give employees and dependents increased access to primary and urgent
care services from the same provider at no cost and may provide access to no-cost or low-cost basic laboratory work
and prescription drugs as well. Key challenges for employers interested in offering a DPC option include the relatively
limited number of DPC practices and the geographic dispersion of employees and dependents.
Limitations
Sample Size
Our analysis is based on the statistical evaluation of differences in risk-adjusted health care claim costs and utilization
measures between approximately 900 members enrolled in DPC and approximately 1,100 members not enrolled in
DPC during the same two-year period. While this sample size is sufficient for meaningful analysis of certain measures
(e.g., total health care costs, emergency department visits), it is insufficient for the analysis of other measures (e.g.,
inpatient admission rates). Observed outcomes would likely fluctuate materially over time or across other employer
groups and populations. Further analysis into the effects of the DPC model of care on overall health care claim costs
and utilization rates that incorporates additional members and longer time periods is necessary.
Lack of Quality Measures
In addition to arguments about the effect of DPC on overall health care cost and utilization rates, proponents of DPC
also often purport that the DPC model of primary care improves the quality of care provided to patients, improves
patient outcomes related to health status, and increases patient satisfaction. We were unable to assess the validity of
these claims in our analysis due to the nature of the data sets provided to Milliman by the employer for our analysis.
Further analysis into the effect of the DPC model of primary care on the quality of care, patient health status and
patient satisfaction is necessary. Any such analysis of these factors should utilize a rigorous and appropriate actuarial
methodology. Ideally, such a study should employ a quasi-control-group-based approach similar to this study but also
incorporate longitudinal views over extended periods of time.

48
Copyright © 2020 Society of Actuaries
Variability in DPC
Given the largely grassroots nature of the growing prevalence of DPC practices, there is no standard DPC model of
care or DPC template for physicians to follow. While many common features and characteristics are shared among
DPC practices, the very nature of DPC—which emphasizes direct and enhanced physician-patient engagement—lends
itself to variability in care delivery between DPC practices.
Specifically, and perhaps more than any other primary care model, we believe the effectiveness of the DPC model of
care in achieving any of its practitioners’ stated goals depends heavily on the unique training, skills, experience,
motivations and care that each DPC physician provides.
Outcomes are unlikely to be uniformly distributed across DPC practices; each practice likely has strengths and
weaknesses relative to its peers; therefore, performance levels for various outcomes-related metrics will vary. For our
analysis, we were only able to assess performance during a two-year period for two DPC practices jointly contracted
to provide primary care services to a single employer population. It is possible, and perhaps even likely, that the
performance of those two practices vary from the average performance level of DPC practices, and their own
performance levels may change over time. Additionally, at the employer’s request for data reporting purposes, the
two contracted DPC practices submitted FFS claims to the TPA. Although those DPC practices are not reimbursed on
a FFS basis, the requirement for them to submit FFS claims increases their administrative burden. This additional
burden may also affect the applicability of the results from our study to other DPC practices where no FFS claims are
submitted. Further analysis into the effects of the DPC model of care on overall health care costs and utilization rates
that incorporates data sets from additional and diverse DPC practices is necessary.
In addition to variability in the care delivered by different DPC practices, there is also variability in the types of
members enrolled in this model of care. Generally, the member types are based on whether the member or employer
pays the DPC membership fee. There are potential variances in health status and the related utilization of medical
services between these different types of members. Members paying out of pocket for their DPC membership fees
may be more highly engaged with the DPC practice and their own care. Further, how these different types of members
compare to similarly situated members not enrolled in DPC may vary, which has important implications for
generalizing observations about DPC outcomes.
Data Quality
Although the data sets provided by the employer for our analysis were generally of high quality, there were two
specific drawbacks:
• The medical claim data was not well populated with provider specialty codes. Without this data, we were
unable to consistently distinguish between primary care and specialist physician office visits and thus were
unable to assess the impact of DPC on physician specialist utilization rates. Proponents of the DPC model of
primary care often claim that DPC reduces utilization of specialist physicians. Unfortunately, without
consistent population of provider specialty codes in the medical claims, we were unable to assess the validity
of this argument as it relates to this employer data set.
• The TPA and employer were not involved in our analysis after they provided us with the data set and
addressed our initial questions and requests for data updates. In particular, we requested feedback from the
TPA and the employer related to reconciling the total amount of allowed and paid claims included in the data
sets and did not receive any response. We were able to closely reconcile paid claims in the data sets to
publicly available reports for the employer covering two different time periods. Based on these
reconciliations, the general consistency of the data throughout the entire time period provided, and our
evaluation of the data for overall quality and reasonableness, we believe the data set provided was complete
and accurate. However, we were unable to secure an attestation from either the TPA or employer to this
due to their unresponsiveness.

49
Copyright © 2020 Society of Actuaries
DPC Practice Structure
The structure of DPC medical practices is not uniform. In particular, at least two important types of practices have
emerged thus far. First are DPC practices whose contracts are exclusively with individual patients who have sought
out the physician. The second are those practices that accept, and often actively seek out, contracts with employers.
In this case, the employer typically pays the DPC fee and the employees then have access to the DPC provider for their
primary care. It is also likely that practices have a mix of both types of contracted members. Further research is needed
into the differences that these (and possibly other) practice structures have on cost and quality. For example, from
our interviews with DPC physicians, several providers noted the possible impacts to patient engagement under the
employer model due to patients not paying the fee themselves. This is just one potential area of impact, but there
could be others.
Reliance
This analysis was prepared on behalf of the SOA to provide information on DPC, as well as to develop a framework for
analyzing DPC as an option for inclusion in an employer’s self-funded health care benefit arrangement. The analysis is
not intended for other purposes.
This report is based on information and data from various sources, which Milliman has not audited. In preparation for
writing this paper, we reviewed various published reports and studies on DPC. The case study presented is from
organizations with which we were familiar through our direct work with them, from information provided directly to
us, and through review of publicly available data sources. There could be other actual case studies that would indicate
results different from those presented in this report. To the extent that any of the information in these interviews and
reports was incorrect, incomplete or misunderstood by us, the information presented in this paper could be affected.
We have also not reviewed every IRS rule, regulation or care model related to DPC. A legal review of these DPC
programs may provide other insights.
Milliman does not intend to legally benefit any third-party recipient of its work product. Even though Milliman has
consented to the release of its work product to a third party, any third-party recipient of this report should not rely
upon Milliman’s report but should engage qualified professionals for advice appropriate to its own specific needs. The
statements contained in the report are those of the authors and do not necessarily represent the views of Milliman
or its other consultants.

50
Copyright © 2020 Society of Actuaries
9. Case Study Data Sources
The employer provided Milliman with the following data sets to complete the analysis.
Administrative Medical Claims
Included claim-level detail for all claims adjudicated by the TPA of the self-insured medical coverage. Medical claim
data was provided for all enrolled plan members, including employees and dependents, and spanned from June 2014
through May 2018. Most standard claim data fields were included in the data and well populated, including member
demographic information; dates of service and claim payments; revenue; CPT, HCPCS and International Statistical
Classification of Diseases and Related Health Problems (ICD) procedure codes; allowed and paid dollar amounts; units
of service; ICD diagnoses; and provider identifiers.
A unique arrangement with the contracted DPC providers allowed for claims to be submitted to the TPA for DPC-
covered services furnished to members enrolled in the DPC option. The DPC providers are not reimbursed for these
services on a FFS basis; the DPC providers are only reimbursed through monthly membership fees paid by the
employer on behalf of members enrolled in the DPC option. The claims that the DPC providers submitted include
service-level information such as CPT and HCPCS procedure codes, but do not include ICD diagnosis codes. Even
though the DPC providers are not reimbursed for these claims on a FFS basis, the TPA adjudicates claims for reporting
purposes. Therefore, the medical claim data provided by the TPA for our analysis not only includes claims for provided
DPC services, but these claims include imputed allowed amounts based on the network fee schedule.
Administrative Prescription Drug Claims
Included claim-level detail for all claims adjudicated by the pharmacy benefit manager and TPA of the self-insured
prescription drug coverage. Prescription drug claim data were provided for all enrolled plan members, including
employees and dependents, and spanned from June 2014 through May 2018. Most standard claim data fields were
included in the data and well populated, including member demographic information, dates of service and claim
payments, National Drug Code, allowed and paid dollar amounts, units of service and pharmacy identifiers.
Health Plan Enrollment
Included monthly member-level demographic and enrollment information for the self-insured health plan (i.e.,
medical and prescription drug coverage). Data were provided for all enrolled plan members, including employees and
dependents and spanned from June 2014 through May 2018. Provided data fields included gender, date of birth,
unique member and subscriber identifiers, and enrolled plan option (i.e., DPC option, traditional option).
Benefit Plan Design
Included a description of all medical and prescription drug plan design features for each plan option. A summary of
HRA and cost sharing amounts is provided in Figure 18 and Figure 19.
Figure 18
TRADITIONAL OPTION HRA
Coverage Tier
Traditional Option
DPC Option
Annual Contribution
Accumulation Limit
Annual Contribution
Employee Only
$750
$2,000
$0
Employee + Spouse
$1,250
$3,300
$0
Employee + Child(ren)
$1,500
$4,000
$0
Employee + Family
$1,875
$5,000
$0

51
Copyright © 2020 Society of Actuaries
Figure 19
PLAN DESIGN SUMMARIES (SINGLE EMPLOYEE AMOUNTS ILLUSTRATED)
Plan Design Element
Traditional Option
DPC Option
Preventive Care
100% Coverage
100% Coverage
Routine Medical Deductible†
$150
$0
Major Medical Deductible††
$600
$0
Medical Coinsurance†††
80%
80%
Generic Drug Coinsurance
0%
0%
Preferred Brand Drug Coinsurance
20%
20%
Non-Preferred Brand Drug Coinsurance
40%
40%
Specialty Drug Coinsurance
40%
40%
Specialty Drug Coinsurance Limit
$150/30-day script
$150/30-day script
Medical Coinsurance Maximum
$1,500
$1,500
Prescription Drug Coinsurance Maximum
$1,875
$1,875
† Applies to all nonpreventive medical services before benefits under the HRA are payable by the plan.
†† Applies to all nonpreventive medical services after annual and any accumulated HRA funds are exhausted by the member.
††† Applies to all nonpreventive medical services other than DPC services for members enrolled in the DPC option. All DPC services are
covered at no cost to the member.

52
Copyright © 2020 Society of Actuaries
10. Case Study Methodology
Analytic Data Processing
We used the following Milliman actuarial tools to process the data sets provided and apply various analytic data fields
to support our analysis:
Milliman Health Cost Guidelines Grouper (HCG Grouper)
The HCG Grouper categorizes medical and prescription drug claims into health care benefit service categories (e.g.,
hospital, surgical, medical, emergency), and applies a standard methodology for counting utilization (e.g., admissions,
days, visits, procedures, scripts). The HCG Grouper assigns detailed information at the claim line level and also applies
an algorithm to identify continuous stay inpatient claims.
Milliman GlobalRVUs (GlobalRVUs)
The GlobalRVUs are a relative value unit system covering the entire spectrum of health care claims and assign to
individual claims a measure of the level of health care resources consumed. This allows for conversion factors (total
claim dollars/relative value units) to be calculated and compared across types of service, points in time or populations
without bias as to differences in the level of utilization, patient morbidity, type of care provided or other factors.
GlobalRVU conversion factors reveal the true level of cost per unit of health care delivered.
Milliman Advanced Risk Adjusters (MARA)
36
MARA is a risk adjustment model that measures patient-level risk across six benefit service categories (inpatient,
outpatient, emergency, physician, prescription drug and other), taking into account each individual’s age, gender,
comorbidities and prescription drug usage. MARA quantifies expected differences in resource utilization levels
based on patient morbidity levels.
Actuarial Methodology
To assess the impact of enrollment in the DPC option on claim costs and utilization rates, we considered the actuarial
methodologies described in Figure 20.
36
For detailed information related to MARA’s performance relative to other available models, please see Health Section Research
Committee. Accuracy of Claims-Based Risk Scoring Models. Society of Actuaries, 2016,
https://www.soa.org/globalassets/assets/Files/Research/research-2016-accuracy-claims-based-risk-scoring-models.pdf (accessed April 28, 2020).

53
Copyright © 2020 Society of Actuaries
Figure 20
ACTUARIAL METHODOLOGIES CONSIDERED FOR CASE STUDY
Methodology
Pre-Post Cohort
Participant vs. Nonparticipant
Summary
Identify members of interest enrolled in the DPC
option and compare their claim costs and utilization
rates before and after enrolling in the DPC option.
Compare claim costs and utilization rates
between members enrolled in the DPC option
and members not enrolled in the DPC option.
Intervention
Group
Selected DPC option enrollees.
Selected DPC option enrollees.
Control Group
Selected traditional option enrollees.
Time Period
Intervention time period = after enrolling in the DPC
option
Control time period = before enrolling in the DPC
option
Same time period for both intervention and
control groups
Special
Adjustments
Claim costs and utilization rates from the control time
period need to be adjusted for health care inflation
and morbidity differences between the control and
intervention time periods.
Claim costs and utilization rates from control
group need to be adjusted for differences in
morbidity between the control and intervention
groups.
Key Drawbacks
Can be subject to “mean reversion” phenomenon
Only 13 months of data provided by employer before
DPC option was offered (control time period).
May require a larger morbidity adjustment than
the pre-post cohort methodology because
different members are in each cohort
Difficult to fully control for selection differences
between intervention and control groups (e.g.,
differences in level of patient self-engagement in
their health care)
Key Benefits
May control for member selection differences better
than participant versus nonparticipant methodology
by comparing the same members to themselves over
time
The employer provided 35 months of data for the
time period while the DPC option was offered.
No need to make adjustment for assumed level of
health care inflation between control and
intervention time periods
Given the limited control time period available for the pre-post cohort methodology (13 months), we decided to use
the participant versus nonparticipant methodology for our analysis. Further, we decided to focus our analysis on the
two-year period from January 2016 through December 2017. By focusing on the time period beginning in January
2016, our analysis will not be affected by any operational challenges that may have occurred during the first six months
of the program (the DPC option was first offered in July 2015). Additionally, by focusing on the time period ending
December 2017, we allow for five months of claim runout such that an actuarial adjustment to complete the claim
data provided was assumed unnecessary.
Cohort Selection
During the two-year period of interest (calendar years 2016 and 2017), there were 2,646 unique members enrolled
in the health plan for at least one month. There were 1,290 members enrolled in the DPC option for at least one
month, 1,537 members were enrolled in the traditional option for at least one month, and 181 members were
enrolled in each option for at least one month.
To allow sufficient time for the DPC model to affect claim costs and utilization rates, we decided to focus our analysis
on members with minimum continuous enrollment intervals of at least 12 months in the DPC or traditional option.
Using this definition, we identified 931 DPC option enrollees and 1,105 traditional option enrollees. Two of the

54
Copyright © 2020 Society of Actuaries
identified members were enrolled in the traditional option for calendar year 2016 and in the DPC option for calendar
year 2017, so they are included in both identified cohorts.
When assessing the impact of health care intervention programs on claim costs and utilization rates, it is important
to consider how high-cost members may affect the analysis. Certain intervention programs may be targeted to high-
cost members, and those members are thus crucial to any analysis of program outcomes. Other programs may be
targeted to only low- or moderate-cost members, and high-cost members may skew the results if they are not
properly accounted for. Proponents of DPC claim that this model of primary care benefits both low- and moderate-
cost members and may even benefit some high-cost members if their high costs are driven by manageable chronic
conditions. We believe the DPC model is unlikely to affect outcomes for the highest-cost members during a relatively
short time period such as two years, and we, therefore, removed those members from our analysis.
We decided to remove members with total allowed claim costs in excess of $75,000 in either calendar year 2016 or
2017 from the identified cohorts. According to Milliman’s 2019 HCGs, approximately 1% to 2% of commercial
members are expected to have claims in excess of this amount for a standard population. For the identified DPC option
members, we removed 19 out of 931 (2.0%), and for the identified traditional option members, we removed 31 out
of 1,105 (2.8%). This resulted in final selected cohorts of 912 members for the DPC option and 1,074 members for the
traditional option. The average exposure period for these selected members during the two-year period of interest
was 22.0 and 21.9 months for the DPC option and traditional option, respectively.
Metric Selection
We focused our analysis for each member on the months they were enrolled in the option for their selected cohorts.
For example, if a member was selected for the DPC option cohort and enrolled in that option from July 2016 through
December 2017, then we focused our analysis on that person’s claim costs and utilization rates during the July 2016
to December 2017 time period. The claim costs and utilization rates during January 2016 to June 2016 would not be
included in our analysis.
Based on our literature review and discussions with DPC practitioners, proponents of the DPC model of primary care
generally claim the following with regard to the main effects of DPC on overall health care spending:
1. DPC reduces the overall level of health care spending by improving care management, increasing patient
engagement and providing more care in the primary care setting.
2. DPC reduces the overall level of health care spending and improves the quality of care through the following
main mechanisms:
a. Reduced inpatient admission rates.
b. Reduced emergency department utilization rates.
c. Reduced physician specialist utilization rates.
We focused our analysis on the following metrics:
1. PMPM allowed claim costs:
a. Calculated as total allowed claim costs/total member months for the selected time interval.
b. Includes claims for services furnished by DPC providers, which were adjudicated by the TPA using
the same allowed fee schedule as similar claims from traditional providers, reimbursed via FFS
arrangement.
2. Annual inpatient admission rate per 1,000 members per year:
a. Calculated as total inpatient admissions/total member months x 12,000 for the selected time
interval.

55
Copyright © 2020 Society of Actuaries
b. Inpatient claims were identified by the presence of one or more room-and-board revenue codes,
and we applied an algorithm to identify continuous stay claims in the data to avoid double-counting
of admissions.
3. Annual emergency department utilization rate per 1,000 members per year:
a. Calculated as total emergency department visits/total member months x 12,000 for the selected
time interval.
b. Emergency department claims were identified by the presence of revenue codes 0450, 0451, 0452
or 0459.
Unfortunately, the medical claim data that the employer provided was not well populated with provider specialty
codes. Without these data, we were unable to consistently distinguish between primary care and specialist physician
office visits and thus were unable to assess the impact of DPC on specialist physician utilization rates.
To adjust for potential morbidity differences between the selected DPC and traditional option cohorts, we decided to
use a risk-adjusted approach. Using this approach, we normalized the unadjusted metrics from both the traditional
and DPC option groups to a standard risk level. That is, for each selected member, we determined a normative PMPM
claim cost amount, normative inpatient admission rate and normative emergency department utilization rate as the
ratio of that person'’s unadjusted metrics to the risk score. The normative metrics used risk scores specific to each
metric; total claim costs were normalized using a total medical and prescription drug risk score; inpatient admissions
were normalized using an inpatient risk score; and emergency department visits were normalized using an emergency
department risk score.
Ultimately, our analysis focused on the following six metrics:
1. Unadjusted overall PMPM allowed claim costs
2. Risk-adjusted overall PMPM allowed claim costs
3. Unadjusted inpatient hospital admission rate
4. Risk-adjusted inpatient hospital admission rate
5. Unadjusted emergency department utilization rate
6. Risk-adjusted emergency department utilization rate
Risk Adjuster
To normalize observed metrics for the selected cohorts for differences in morbidity between the DPC and traditional
option members, we considered the MARA commercial risk adjustment models shown in Figure 21.
Figure 21
MARA RISK ADJUSTERS CONSIDERED FOR CASE STUDY
Concurrent Model
Age/Sex
Cx (diagnoses)
Rx (therapeutic classes)
Summary
Estimates risk levels based on
age and sex only
Estimates risk levels based on
ICD-10 diagnoses coded on face-
to-face medical claims only (e.g.,
office visits)
Estimates risk levels based on
age, sex and usage of different
therapeutic classes of
prescription drugs
Key Drawbacks
Limited ability to predict
variability in claims on a
member-by-member basis
Likely understates risk scores for
DPC option members because
the majority of care was
furnished by DPC providers, and
DPC claims do not include ICD
diagnoses
Not as good at predicting claim
variability on a member-by-
member basis as a Cx model

56
Copyright © 2020 Society of Actuaries
Key Benefits
Required data consistently
populated for DPC and
traditional option members
Most accurate at predicting
variability in claims on a
member-by-member basis
Required data consistently
populated for DPC and
traditional option members
DPC Relative Risk
0.846
0.694
0.917
Raw Risk Range
0.4 − 2.2
0.1 − 27.2
0.1 − 15.4
For either the Cx or Rx risk adjusters, MARA can calculate risk scores on either a prospective or concurrent basis.
Prospective risk scores use base period claim experience to estimate utilization and cost levels in some future period.
Prospective risk scores generally de-emphasize nonchronic (acute) conditions, because claims associated with these
conditions tend to be nonrecurring over multiple years. By contrast, concurrent risk scores use base period claim
experience to assess the risk and health status of a population in that base period. Concurrent risk scores evaluate
the impact of both chronic and acute conditions on claims. For our case study, we used concurrent risk scores because
the goal of the study was not to predict future costs, utilization or health status but rather to do comparisons between
two populations during a specified historical period.
All three of the models (age/gender, Cx, Rx) estimated that the DPC option cohort had lower overall health care risk
than the traditional option cohort did. Given the limited variability in age/sex risk scores (i.e., the range of risk scores
across members provided in the “Raw Risk Range” row) and the inconsistent inclusion of ICD diagnoses on medical
claims between DPC option and traditional option members (claims for DPC members are frequently lacking diagnosis
codes), we chose the Rx model for our analysis. This model is reasonably able to predict claim variability on a
member-by-member basis (unlike the age/sex model), and both the DPC and traditional option cohorts have the
required data for the risk adjuster consistently populated in the provided data (unlike the Cx model).
For additional development information for MARA, please see Appendix C.
Statistical Analysis
To determine whether differences in observed and normative metrics of interest between the DPC and traditional
option cohorts were statistically significant, we used unmatched two-sample t-tests. We assumed equal variance
between the samples.
11. Lessons Learned/Future Research
Because the DPC movement is small but growing, our research represents one of the first robust, data-driven studies
on the model. However, our research into DPC outcomes was limited to analyzing just a single employer and a single
variation of the model over a two-year period. There are other variations of DPC, any of which may produce different
results than what we observed in our study. More research is required to validate model savings over a broader
population, with greater statistical credibility, in other geographical settings and under different DPC model variations.
The “Gaps in Research” and “Study Limitations” sections of this paper identify many areas for future research. The
greatest need, however, may simply be more data. As in any new area of research, the lack of quality data due to the
small number of DPC practitioners is a significant limitation on actuarial evaluations of the model. However, this may
be changing as the DPC movement grows and its core principles gain traction with health care leaders and policy
decision-makers. While DPC providers are generally opposed to medical administrative claims coding for purposes of
payment, they are not, as a rule, opposed to quantitative, data-driven studies that validate the cost savings, quality
improvement and customer satisfaction that they believe outperform traditional primary care models. To do this,
capturing high-quality, robust data sets that cover the whole spectrum of health care without interfering with patient
care or diminishing the effectiveness of DPC would be a significant step forward in future research.

57
Copyright © 2020 Society of Actuaries
As with any quantitative study, some of the most important information and understanding did not come from the
numbers but from the people and the process. Our research and personal understanding were greatly enhanced
because of the qualitative aspects of the study, which in turn made the quantitative aspects more meaningful.
Specifically, the survey and physician interviews greatly aided in our understanding of what DPC providers considered
the “secret sauce” of the model. It is from those discussions and survey responses that we were able to present what
we believe to be an accurate and comprehensive essence of DPC.
Acknowledgments
The authors wish to thank the Society of Actuaries for sponsoring this paper. In particular, the authors thank the
members of the Project Oversight Group for their assistance in preparing this paper and gratefully acknowledge the
assistance of Achilles Natsis, health research actuary for the SOA, throughout the course of the writing of this paper.
Additionally, the authors would like to thank James Grana for his expertise and insights related to the survey as well
as Deana Bell and Doug Norris of Milliman for additional review of the material. Mitch Johnson, Hanna Holzer and
Ryan LeRoy of Milliman contributed significant analytical content to this paper. Furthermore, the authors wish to
thank the American Academy of Family Physicians (AAFP), the Direct Primary Care Coalition and the DPC Alliance—
and in particular Bethany Burk from the AAFP, Jay Keese from the Direct Primary Care Coalition, and Joe Grundy
from the DPC Alliance—for their assistance gathering information for this paper. Last, the authors wish to thank the
many Direct Primary Care physicians who graciously volunteered their time to take our survey and speak to the
authors throughout the course of developing this paper.
Project Oversight Group Members
Joshua Axene, FSA, MAAA
Gayle Brekke, FSA, MAAA
Heather Clemens, FSA, MAAA
Sarah Osborne, FSA, MAAA
Heather Ozhogin, FSA
Mary Vollkommer, FSA, MAAA
Craig Winkler, ASA, MAAA
Woodrow Wong, ASA
SOA Project Coordinators
Achilles Natsis, FSA, MAAA, FLMI
Erika Schulty

58
Copyright © 2020 Society of Actuaries
Appendix A: Articles Included in Literature Review
Definitions of DPC
This section includes articles that explicitly provide definitions of the DPC model of care. Reference information for
each article, along with corresponding definitions of DPC, are provided below. Note that comments are directly from
sources and do not represent authors’ statements or opinions.
AAFP. Direct Primary Care. https://www.aafp.org/about/policies/all/direct-primary.html (accessed January
9, 2020).
A practice and payment model where patients/consumers pay their physician or practice directly in
the form of periodic payments for a defined set of primary care services. DPC practices typically
charge patients a flat monthly or annual fee, under terms of a contract, in exchange for access to a
broad range of primary care and medical administrative services.
American College of Physicians. Direct Patient Contracting. https://www.acponline.org/practice-
resources/business-resources/payment/delivery-and-payment-models/direct-patient-contracting (accessed
January 9, 2020).
Any practice that directly contracts with patients to pay out-of-pocket for some or all of the services
provided by the practice, in lieu of or in addition to traditional insurance arrangements, and/or
charges an administrative fee to patients, sometimes called a retainer or concierge fee, often in
return for a promise of more personalized and accessible care.
Rhoads, Jared, and Robert, Graboyes. Direct Primary Care. The Mercator Center at George Mason
University, June 13, 2018, https://www.mercatus.org/hoap/direct-primary-care (accessed January 9, 2020).
A model of health care provision in which a primary care doctor charges patients a retainer fee
covering all or most primary care services, including clinical, laboratory, and consulting services. This
model enables physicians to move away from fee-for-service insurance billing. Given the variety of
retainer practice models and the resulting legislative confusion, it is important to define direct
primary care accurately. A DPC practice charges a periodic fee for services, generally $25 to $85 per
month. It does not bill any third parties on a fee-for-service basis, and any per-visit charges are less
than the monthly equivalent of the periodic fee. Through this mechanism, DPC practices claim to
reduce administrative overhead by approximately 40 percent.
Direct Primary Care Coalition. What is Direct Primary Care? https://www.dpcare.org/ (accessed January 9,
2020).
An innovative alternative payment model improving access to high functioning health care with a
simple, flat, affordable membership fee. No fee-for-service payments. No third party billing. The
defining element of DPC is an enduring and trusting relationship between a patient and his or her
primary care provider. Patients have extraordinary access to a physician of their choice, often for as
little as $70 per month, and physicians are accountable first and foremost their patients.
Direct Primary Care Frontier. Defining Direct Primary Care. Retrieved January 9, 2020, from
https://www.dpcfrontier.com/defined/ (accessed January 9, 2020).
For the practice to qualify as a direct primary care practice the practice must:
1) Charge a periodic fee

59
Copyright © 2020 Society of Actuaries
2) Not bill any third parties on a fee for service basis, and
3) Any per visit charge must be less than the monthly equivalent of the periodic fee
New England Direct Primary Care Alliance. What Is Direct Primary Care? https://www.nedpca.org/
(accessed January 9, 2020).
By definition, a Direct Primary Care practice charges a periodic fee, does not bill third party payers
on a fee for service basis and any per-visit charge must be less than the monthly equivalent of the
periodic fee.
Holdsworth, Zak. Understanding Direct Care. Hint Health, February 16, 2015,
https://blog.hint.com/understanding-direct-care (accessed January 9, 2020).
There are two main criteria that define Direct Care practices.
The first, is that Direct Care providers charge their patients a recurring membership fee to be part
of their practice. In exchange for that fee, patients receive access to a pre-defined set of primary
care services, which typically includes better access to the provider through same or next day
appointments, remote access including text and cell phone access, longer and more in-depth visits,
and home visits. In many Direct Care practices, basic labs and procedures are also offered.
The second criteria for qualifying as Direct Care is based on the provider’s relationship to insurance.
Direct Care providers operate completely outside of the traditional fee-for-service based insurance
or third-party payer system, meaning that they do not accept insurance nor attempt to get
reimbursed for the services they provide.
Ghany, Reyan, Leonardo, Tamariz, Gordon, Chen, Elissa, Dawkins, Alina, Ghany, et al. 2018. High-Touch
Care Leads to Better Outcomes and Lower Costs in a Senior Population. American Journal of Managed Care
24, no. 9:e300–e304.
The National Institute for Health Care Reform defines high-intensity care as “care provided by a
multidisciplinary team for patients with complex conditions to improve care and lower health care
costs.” An emerging subtype of high-intensity care is high-touch care where frequent direct person-
to-person interaction between patients and their health care providers is encouraged to optimize
the value of care.
Huff, Charolette. 2015. Direct Primary Care: Concierge Care for the Masses. Health Affairs 34, no. 12:2016–
2019.
Sometimes dubbed “concierge care for the masses” by proponents, direct primary care refers to an
emerging style of physician practice where for a monthly fee, patients can get all of their primary
care covered by the practice, with little or nothing more out of pocket, and where neither the doctor
nor the patient bills an insurer.
Porter, Sheri. 2015. DPC Summit Draws Hundreds of Enthusiastic Family Physicians. Annals of Family
Medicine 13, no. 5:489–499.
A new practice model in which physicians charge patients a flat monthly or annual fee in exchange
for a wide array of health care services.

60
Copyright © 2020 Society of Actuaries
Health Policy Programs Group. Direct Primary Care (DPC): Potential Impact on Cost, Quality, Health
Outcomes, and Provider Workforce Capacity. University of Wisconsin Population Health Institute, 2018,
https://docs.legis.wisconsin.gov/misc/lc/study/2018/1790/010_july_24_2018_meeting_10_00_a_m_room
_412_east_state_capitol/uw_dpc_brief (accessed December 11, 2018).
A health care delivery model where a provider offers unlimited specified routine health care services
for a monthly fee.
Restrepo, Katherine, and Julie, Tisdale. Direct Primary Care for Local Governments. John Locke Foundation,
December 2, 2016, https://www.johnlocke.org/research/direct-primary-care-for-local-governments/
(accessed January 9, 2020).
A simplified health care business model that removes insurance companies from basic primary care.
In exchange for a monthly, out-of-pocket fee, patients have unrestricted access to their physician
and unlimited access to a defined package of services.
Twiddy, David. 2014. Practice Transformation: Taking the Direct Primary Care Route. Family Practice
Management 21, no. 3:10–15.
Most retainer-based practices act as a miniature insurance company, charging patients an annual
fee that covers a portion or all of their regular medical care, including check-ups, primary care,
preventive care, and coordinating care with specialists. Not all retainer-based practices are
completely severed from insurers; some work with insurers to pay for portions of a patient’s care.
Direct-pay practices that do not use a retainer or where the retainer covers only a portion of the
costs may also charge patients fees at the time of service. Concierge plans also use retainers, but
are frequently characterized by higher fees designed to significantly limit the size of the patient
panel. That gives patients greater access to the physician through longer appointments and
expanded office hours or even house calls. In all cases, not having to bill or negotiate with payers
can simplify and add predictability to the financial relationship between patient and physician. It
also can reduce staffing needs, bringing down overhead and improving practice profitability.
Adashi, Eli, Ryan, Clodfelter, and Paul, George. 2018. Direct Primary Care: One Step Forward, Two Steps
Back. Journal of the American Medical Association 320, no. 7:637–638.
Patients contract directly with a primary care physician to pay a recurring out-of-pocket fee in
exchange for a defined set of primary care benefits.
Cole, Evan S. 2018. Direct Primary Care: Applying Theory to Potential Changes in Delivery and Outcomes.
Journal of the American Board of Family Medicine 31, no. 4:605–611.
A model of primary care delivery that has been dubbed “membership medicine,” where patients
pay a periodic membership fee to a primary care provider (PCP) to obtain access to services.
Eskew, Philip, and Kathleen, Klink. 2015. Direct Primary Care: Practice Distribution and Cost across the
Nation. Journal of the American Board of Family Medicine 28, no. 6:793–801.
A primary care practice that 1) charges a periodic fee for services, 2) does not bill any third parties
on a fee-for-service basis, and 3) any per-visit charges are less than the monthly equivalent of the
periodic fee. A differentiating characteristic versus concierge practices is that many concierge
practices also bill third-parties, a practice many describe as “double dipping”.
Rowe, Kyle, Whitney, Rowe, Josh, Umbehr, and Frank, Dong. 2017. Direct Primary Care in 2015: A Survey
with Selected Comparisons to 2005 Survey Data. Kansas Journal of Medicine 10, no. 1:3–6.

61
Copyright © 2020 Society of Actuaries
A practice discipline based on the premise that the development of a high quality patient-physician
relationship is enhanced in an environment that provides unrestricted access, innovative and open
communication, and increased face-to-face time. Patients pay a practice determined membership
fee in exchange for a variety of included amenities and services, which are intended to support this
premise.
Eskew, Philip. 2017. Direct Primary Care Business of Insurance and State Law Considerations. Journal of
Legal Medicine 37, no. 1–2:145–154.
Involves a contract between the physician and patient whereby ongoing primary care services are
provided in exchange for a periodic fee. For the practice to qualify as a DPC practice (a subset of the
retainer category) the practice must 1) charge a periodic fee, 2) not bill any third parties on a fee
for service basis, and 3) any per visit charge must be less than the monthly equivalent of the periodic
fee.
Restrepo, Katherine. Direct Primary Care: A Simple Health Care Model Designed to Help Patients with
Chronic Diseases and Disabilities. John Locke Foundation, March 2017,
https://www.johnlocke.org/app/uploads/2017/03/DirectPrimaryCare.pdf (accessed January 9, 2020).
A simplified health care business model that removes insurance companies from basic primary care.
In exchange for an average monthly fee of around $75, patients have unrestricted access to their
physician and unlimited access to a defined package of services. In most cases, primary care
physicians are available around the clock, in person, by phone, text, or by e-mail.
McCorry, Daniel. Direct Primary Care: An Innovative Alternative to Conventional Health Insurance. Heritage
Foundation, August 6, 2014, https://www.heritage.org/health-care-reform/report/direct-primary-care-
innovative-alternative-conventional-health-insurance (accessed January 9, 2020).
Financed by direct payment, outside of insurance, usually in the form of a monthly fee. In return,
patients have ready access to physicians who deliver continuous, comprehensive, and personalized
primary care.
Carlasare, Lindsey. 2018. Defining the Place of Direct Primary Care in a Value-Based Care System. Wisconsin
Medical Society 117, no. 3:106–110.
The primary feature of this practice model is a recurring fee, paid by the patient directly to the
physician, in exchange for virtually unlimited access to the physician.
Overview of DPC
This section includes articles that provide an overview of the DPC model of care. Reference information for each article
along with key excerpts are provided below. Note that comments are directly from sources and do not represent
authors’ statements or opinions.
Huff, Charlotte. 2015. Direct Primary Care: Concierge Care for the Masses. Health Affairs, 34, no. 12:2016–
2019.
Sometimes dubbed “concierge care for the masses” by proponents, direct primary care refers to an
emerging style of physician practice that is driven in part by the frustration of patients and doctors
alike about treatment time constraints. But the approach has met with skepticism in some quarters,
with concerns that it could aggravate the shortage of primary care doctors and lead to a two-tier
health system.

62
Copyright © 2020 Society of Actuaries
For a monthly fee, generally $25 to $85, patients can get all of their primary care covered—from an
annual physical to treatment for various maladies and screening tests—with little or nothing more
out of pocket. Neither the doctor nor the patient bills an insurer. However, direct primary care
practices encourage patients to carry some kind of coverage for big-ticket items, such as surgeries
and cancer treatment.
Scarcely a decade old, the model appears to be gaining traction, particularly in the past few years.
Data about the number of direct primary care practices and their overall cost-effectiveness remain
limited. Nonetheless, the approach has attracted some prominent backers, including the American
Academy of Family Physicians (AAFP). By mid-2015 laws had been changed in at least thirteen states
to enable the approach—which looks a lot like insurance to patients, but is not—to be used outside
the oversight of state insurance regulators. Federal legislation called the Primary Care Enhancement
Act has been introduced that would further reduce some of the obstacles that enthusiasts say limits
the expansion of these practices, such as allowing patients with health savings accounts to use those
funds to pay the monthly fees.
Porter, Sheri. 2015. DPC Summit Draws Hundreds of Enthusiastic Family Physicians. Annals of Family
Medicine 13, no. 5:489–499.
This new practice model—in which physicians charge patients a flat monthly or annual fee in
exchange for a wide array of health care services—has piqued the interest of work-weary physicians
who like the idea of taking back control of their practices and eliminating insurance hassles.
According to the AAFP’s 2014 Practice Profile, 2% of family physicians are already practicing in a
DPC setting. Although the survey indicated very few family physicians were transitioning to a DPC
setting as of December 2014, 28% of family physicians are aware of DPC and are exploring the model
in more depth before making a decision. Only 21% have explored and decided against the DPC
model, and 49% are unaware of DPC.
Adashi, Eli, Ryan, Clodfelter, and Paul, George. 2018. Direct Primary Care: One Step Forward, Two Steps
Back. Journal of the American Medical Association 320, no. 7:637–638.
DPC models vary in their structure, yet they generally provide coverage for acute care and long-
term care, basic disease treatment, discounted prescriptions, vaccinations, screening tests, and
basic care coordination. Physicians can choose to include services that might not traditionally be
reimbursed in fee-for-service models, including electronic correspondence with patients, home
visits, and 24/7 service lines. Although DPC is similar in structure to “retainer” or “concierge”
medicine, the major differences are that the DPC model traditionally does not “double dip” by billing
insurers and historically has been less costly, with typical monthly fees between $70 and $100 per
patient. Patients with direct-pay primary care contracts must also purchase wraparound insurance
(i.e., typically high deductible plans) for services not covered by the retainer, such as hospitalization
and subspecialist care. To date, uptake has been limited, with only an estimated 13% of primary
care physicians adopting some form of direct payment models.

63
Copyright © 2020 Society of Actuaries
At its core, DPC emphasizes to patients that their health care dollars are best spent on cultivating a
longitudinal, therapeutic relationship with an accessible primary care physician. Proponents of DPC
argue that the model generates system-level cost savings, improved patient outcomes, broader
access to care, and clinician and patient satisfaction. Because DPC models do not rely on fee-for-
service reimbursement, physicians are able to devote resources to previously non-billable care
coordination efforts. With a smaller patient panel and because DPC physicians do not bill third-party
payers, physicians can focus on building therapeutic, longitudinal relationships with patients. DPC
advocates suggest that these changes yield significant improvements in both patient and
population-level health outcomes, reducing the rates of hospital readmissions, specialist visits,
radiologic and laboratory testing, and emergency care. Individual DPC practices have indicated that
practice-level data on outcomes support these claims; however, no study, to our knowledge, has
produced data to support anecdotal claims by individual practices.
Changes to the current fee-for-service reimbursement model are needed, but DPC is not the
promised panacea of payment reform. Though flawed in design and execution, the fundamental
argument of DPC is tenable: comprehensive care must be compensated with comprehensive
payment. DPC shifts payment from encounter-based reimbursement to comprehensive global
payments, giving physicians flexibility in determining the most appropriate mix of patient services
and care coordination. DPC therefore represents a simplified model of risk-adjusted,
comprehensive payment that lacks the necessary oversight needed to hold physicians accountable
for data reporting, as well as individual and population health outcomes. DPC directs attention to
the many shortcomings of the current fee-for-service reimbursement model. However, DPC is not
a scalable model built on fundamental incentive drivers that shape physician and patient behavior
to achieve systemic cost savings, promote equity in access, and yield improvement in population
health outcomes. Lessons learned from DPC—mainly the potential utility of global capitated
payments—should be applied when developing new payment reform models and envisioning a new
future for primary care delivery. However, DPC is not the answer to the problem.
Rowe, Kyle, Whitney, Rowe, Josh, Umbehr, and Frank, Dong. 2017. Direct Primary Care in 2015: A Survey
with Selected Comparisons to 2005 Survey Data. Kansas Journal of Medicine 10, no. 1:3–6.
Introduction: Direct primary care (DPC), a fee for membership type of practice, is an evolving
innovative primary care delivery model. Little is known about current membership fees, insurance
billing status, physician training, and patient panel size in DPC practices. This study aimed to obtain
current data for these variables, as well as additional demographic and financial indicators, and
relate the findings to the Healthy People 2020 goals. It was predicted that DPC practices would (1)
submit fewer claims to insurance, (2) have decreased membership fees, (3) be primarily family
medicine trained, and (4) have increased the projected patient panel size since 2005.
Methods: An electronic survey was sent to DPC practices (n = 65) requesting location, membership
fees, projected patient panel size, insurance billing status, training, and other demographic and
financial indicators. Data were aggregated, reported anonymously, and compared to two prior
characterizations of DPC practices done in 2005.
Results: Thirty-eight of 65 (59%) practices responded to the 2015 survey. The majority of
respondents (84%) reported using an electronic medical record (EMR), offering physician email
access (82%), 24-hour access (76%), same day appointments (92%), and wholesale labs (74%). Few
respondents offered inpatient care (16%), obstetrics (3%), or financial/insurance consultant
services. Eighty-eight percent (88%) of practices reported annual individual adult membership rates
between $500 and $1,499, decreased from 2005 where 81% reported greater than a $1,500 annual
fee. The proportion of practices who submit bills to insurance decreased from 75% in 2005 to 11%

64
Copyright © 2020 Society of Actuaries
in 2015. Fifty-six percent (56%) of practices reported projected patient panel size to be greater than
600, increased from 40% in 2005. Family medicine physicians represented 87% of respondents,
markedly different from 2005 when 62 - 77% of DPC respondents were general internal medicine
physicians.
Conclusions: Most DPC practices no longer submit to insurance and are family medicine trained.
Compared with the previous sampling, DPC practices report decreased membership fees and
increased projected panel size. These trends may signify the DPC movement’s growth in application
and scope.
Brekke, Gayle. Direct Primary Care: Good for What Ails Us. Health Watch, May 2016,
https://www.soa.org/Library/Newsletters/Health-Watch-Newsletter/2016/may/hsn-2016-iss-80.pdf
(accessed January 9, 2020).
Direct Primary Care – What it is and how it works: DPC is a newer incarnation of concierge medicine
or retainer medicine in which patients pay a modest monthly membership fee in exchange for
unlimited primary care. There are many practice models emerging; I will use the term “direct
primary care” to refer to those practices that do not take insurance. Hybrid models are also
common; these are practices that use a traditional insurance-based model for some patients and a
DPC model for others. Sometimes a hybrid model is used to transition from an existing traditional
practice to a DPC practice over time.
The median monthly DPC fee for an adult is about $70 and the DPC Journal reports that 68 percent
of fees are between $25 and $85 per month. Monthly per child fees are modest, often $10 to $20
per child with a cap on the total monthly fee for a family. Rates are independent of pre-existing
conditions and health status. There are typically no copays, deductibles or coinsurance for most or
all services provided by the physician. Care management and care coordination are included.
Patients receive 24/7 access to the physician for office visits, emails and phone calls, and many DPC
providers include technology visits such, as texts, as well as visits at other locations as needed. DPC
practices typically promise same-day or next-day appointments of 30 to 60 minutes. As an example
of enhanced access, consider the following story. DPC physician Dr. Josh Umbehr of AtlasMD in
Wichita, Kansas, tells of a patient who cut himself carving the family’s Thanksgiving turkey. The man
was not sure whether he needed stitches so he texted Dr. Josh a picture of his hand. Sure enough,
he needed stitches. The patient met Dr. Josh at the DPC clinic. Dr. Josh sewed him up for no charge
and got a piece of pumpkin pie for his trouble. One thing that is interesting about this story is that
it is typical of the sorts of interactions we see in other areas of our lives, but atypical of the
interactions we see in health care. For one thing, this is a customer-centered transaction. With no
third party in the middle, patient and doctor are free to interact in a way that works well for both
parties. And in the process, money and time were saved by avoiding a trip to the emergency
department.
DPC patients receive many preventive and primary care services at no additional charge beyond the
monthly membership fee; common low-cost ancillary services and supplies are provided at no
additional charge. This often includes routine office testing, such as electrocardiograms, some
medications, on-site lab testing and various procedures, as well as digital x-rays. Higher-cost items,
such as prescription medications and durable medical equipment are often provided at cost or for
a small mark-up above cost. In addition, many DPC providers partner with local imaging centers and
labs to provide high-quality services at a reduced price if the patient pays cash at the time of service.
For example, Dr. Brian Forrest of Access Health care has obtained prostate cancer tests for $5 from
the same lab that would charge a Medicare patient at least $175; $80 for mammograms instead of
$350 and colonoscopies for $400 when the going rate is $2,000.

65
Copyright © 2020 Society of Actuaries
Another cost-saving measure that many DPC providers offer (subject to state regulations) is to
dispense prescription medications to their patients at wholesale cost. About a dozen states allow
this without restriction. It is not unusual for DPC providers to shop around for lower-cost pharmacies
so that their patients get even more bang for their health care dollar. With insurance removed from
the relationship, the focus is on the service, convenience and value that the DPC provider can offer
his or her customer patients.
DPC is an effective way to deliver primary care for almost every segment of the population. Some
DPC providers are expanding beyond the individual market and are successfully delivering primary
care to employees of all-sized employers, resulting in savings of 15 to 30 percent on employee
health benefit costs. Employers pay the DPC membership fees as an employee benefit.
DPC providers are also embracing Medicare and Medicaid populations. For example, the large DPC
practice Qliance recently enrolled 15,000 patients via a Medicaid managed care contract, where
Medicaid simply pays the membership fee on behalf of the patients as part of a shared savings
program. Dr. Garrison Bliss of Qliance estimates that Washington state will save between 15 and 20
percent on these beneficiaries, compared to what traditional Medicaid would have spent. Another
5,000 patients recently signed up with Qliance via the Washington state health insurance exchange.
Iora Health, a DPC practice that contracts with unions and employers, a year ago launched clinics in
Washington and Arizona catering to Medicare Advantage patients, and they are setting up similar
clinics in Colorado and Massachusetts. Qliance and Iora Health are just two examples of innovative
DPC practices that are expanding and finding new ways to serve all sorts of patients, including those
with Medicare or Medicaid.
The Affordable Care Act (ACA) allows DPC to count as ACA-compliant insurance as long as it is
bundled with a “wraparound” catastrophic medical policy. Many patients use DPC in conjunction
with a high-deductible health plan, and insurance carriers are starting to develop catastrophic plans
specifically designed to complement DPC. At this time, membership fees paid to DPC practices are
not recognized by the IRS as health savings account (HSA) expenses, and thus, they are not counted
as tax deductions the way that other health expenses are. Legislative efforts are underway to
change this. In addition, efforts are underway to clarify at the state level that DPC practices are
engaged in the practice of care, rather than insurance. In states where such legislation has been
passed, the state’s department of insurance cannot treat DPC physicians as insurers subject to its
regulatory scheme. As of July 2015, 13 states have DPC laws on the books.
Restrepo, Katherine. Direct Primary Care: A Simple Health Care Model Designed to Help Patients with
Chronic Diseases and Disabilities. John Locke Foundation, March 2017,
https://www.johnlocke.org/app/uploads/2017/03/DirectPrimaryCare.pdf (accessed January 9, 2020).
Abstract: For the nation’s health care system to slow the growth of health care spending and better
manage the prevalence of chronic disease and its association with disabilities, patients need better
access to health care. In turn, providers need the flexibility to spend more time with their patients.
Direct Primary Care (DPC) is a health care delivery model that has proven to strengthen the
physician-patient relationship, provides health care in a transparent and cost-effective manner, and
benefits patients with complex conditions. Extending Direct Primary Care as a benefit option for the
most costly and complex Medicaid patients can help slow rising health care costs and improve
overall chronic care management. Better chronic care management can therefore reduce the
incidence or severity of disabilities.

66
Copyright © 2020 Society of Actuaries
McCorry, Daniel. Direct Primary Care: An Innovative Alternative to Conventional Health Insurance. Heritage
Foundation, August 6, 2014, https://www.heritage.org/health-care-reform/report/direct-primary-care-
innovative-alternative-conventional-health-insurance (accessed January 9, 2020).
Abstract: Insurance-based primary care has grown increasingly complex, inefficient, and restrictive,
driving frustrated physicians and patients to seek alternatives. Direct primary care is a rapidly
growing form of health care that not only alleviates such frustrations, but also goes above and
beyond to offer increased access and improved care at an affordable cost. State and federal
policymakers can improve access to direct primary care by removing prohibitive laws and enacting
laws that encourage this innovative model to flourish. As restrictions are lifted and awareness
expands, direct primary care will likely continue to proliferate as a valuable and viable component
of the health care system.
Carlasare, Lindsey. 2018. Defining the Place of Direct Primary Care in a Value-Based Care System. Wisconsin
Medical Society 117, no. 3:106–110.
Introduction: Direct primary care, one of several retainer-based practice models, is a niche practice
type that offers an alternative to the traditional fee-for-service and insurance-based practices most
prevalent in US health care. In Wisconsin, the prevalence of direct primary care practices is higher
than in most other states. The market for direct primary care practice may be growing along with
the industry shift to value-based care and an increase in physicians’ desire to reduce the increasing
administrative work and regulations that detract from patient care and increase burnout. Many
physicians are seeking ways to reduce these burdens so they have more time with patients. Some
are transitioning their practice to a retainer-based model, such as direct primary care, in which they
collect a retainer from patients in exchange for more time, freer communication, and less
paperwork.
Objective: The objective of this review is to provide information about the direct primary care
practice model, possible drivers to this model of care, and its advantages and drawbacks for
physicians and patients. This discussion also aims to evaluate the care model’s place in the shift to
value-based care, and key positions and policy from leading organizations.
Methods: A literature review was conducted to collect and analyze current evidence about the
prevalence of retainer-based practices, the average fees associated with such models, the
contributors to physician burnout that may lead to a transition to the direct primary care model,
and the relevant ethical and policy considerations associated with direct primary care.
Discussion: Eighty-two percent of Wisconsin physicians report some level of burnout. Estimates
demonstrate an increase in the number of direct primary care practices, and that Wisconsin is
among the top three states with the highest number of direct primary care practices. The literature
suggests that since the early stages of modern retainer-based models, patient fees have decreased
and the patient base for these practices has expanded. The practice model is relatively rare,
although there are indicators that its presence has increased in recent years.
Conclusions: Physicians seeking strategies to reduce administrative burden, spend more time with
patients, or simply streamline their practice may experience benefits in transitioning to a retainer
practice, such as direct primary care. There are foundational concepts about direct primary care,
including advantages, drawbacks, and ethical considerations, to heed when transitioning to this
model. There is a need for further research to quantify key data about direct primary care and its
effects on patient outcomes and physician burnout and satisfaction.

67
Copyright © 2020 Society of Actuaries
Chase, David. On Retainer: Direct Primary Care Practices Bypass Insurance. California Health care
Foundation, April 30, 2013, https://www.chcf.org/publication/on-retainer-direct-primary-care-practices-
bypass-insurance/ (accessed January 9, 2020).
Direct primary care (DPC) is an emerging model for delivering medical care that has gained some
attention in California and nationally in recent years. Sometimes referred to as “retainer practices,”
DPC practices generally do not accept health insurance, instead signing up patients in exchange for
a recurring monthly fee – usually $50 to $80 – for a defined set of services.
This issue brief describes the landscape of DPC practices, which collectively have more than a half
million people on their rolls. It explores the opportunities and challenges for the DPC model,
especially in light of the Affordable Care Act (ACA), and legislation in some states providing for the
retainer practice model.
Because the field is too young for a detailed national study of its effectiveness in delivering cost-
efficient quality care, this report relies on research on some of the early notable players. More than
a dozen DPC organizations were included in the research, which involved interviews with payers,
purchasers, and consumers. The DPC providers profiled were selected because they have significant
market presence and/or major corporate/venture capital backing and they represent a geographic
distribution nationally.
For the purposes of this report, DPC is defined as retainer practices that usually charge less than
$100 per month per patient. The research excludes what are known as “concierge” practices, which
charge higher fees and target more affluent patients.
Doherty, Robert. 2015. Assessing the Patient Care Implications of “Concierge” and Other Direct Patient
Contracting Practices. Annals of Internal Medicine 163, no. 12:949–952.
The growth of DPCPs [Direct Primary Care Practices] seems to be principally motivated by
physicians' frustration with paperwork, low reimbursement, and restrictions on time spent with
patients. It is essential that policymakers address these and other factors. Yet it must also be
recognized that DPCPs potentially exacerbate racial, ethnic, and socioeconomic disparities in health
care and impose too high a cost burden on some lower-income patients.
The [American] College [of Physicians] supports physician and patient choice of practices that are
accessible, viable, and ethical. It asserts that physicians in all types of practices must ensure that
they are meeting their obligations to serve patients of all types, especially the poor and other
vulnerable patients. ACP recommends that DPCPs consider ways to mitigate any adverse impact on
the poor and other underserved populations.
Finally, the College calls for independent research to study the factors contributing to the growth
of DPCPs and their impact on workforce, cost, and access to care especially for vulnerable
populations.
Clark, P., J., Friedman, D., Crosson, and M. Fadus. 2010. Concierge Medicine: Medical, Legal and Ethical
Perspectives. The Internet Journal of Law, Health care and Ethics 7, no. 1:1–16.
Abstract: Over the last 20 years, dissatisfied primary care physicians have turned to an alternative
medical practice known as “concierge medicine,” “boutique medicine” or “retainer medicine.”
Concierge medicine is a system in which the physician limits the amount of patients in the practice
and offers exclusive services for an annual fee. Primary care physicians today are challenged with
low reimbursements, malpractice premiums, overwhelming paperwork, and the responsibility of
taking on thousands of patients to offset the rising cost of health care. They also face an immense

68
Copyright © 2020 Society of Actuaries
pay discrepancy compared to medical specialists. To maintain their income levels, primary doctors
may take on more patients and more hours to compensate for the transaction costs of dealing with
insurance, which can take up nearly 40% of a physician’s income. The increasing volume of patients
and responsibility can compromise the overall quality of a physician’s attention. Today, the average
primary care physician sees dozens of patients a day, and can treat thousands of patients a year.
Primary care physicians may feel the need to comply with the overloaded standards of today’s
health care system rather than the best interest of the patient’s health to keep up with patient
demand in primary care. With this being said, it is no surprise that many primary-care physicians
report that they no longer enjoy practicing medicine. A 2004 survey of physicians age 50-65 found
that over three-quarters of them viewed medicine as increasingly unsatisfying. Although only a small
percentage of these disgruntled physicians have made the switch to concierge practices, the trend
is expanding rapidly across the country. There are an estimated 5,000 physicians practicing
concierge medicine in 2010 across the nation out of an estimated 240,000 internal medicine
physicians and related subspecialists. Of these 5,000 concierge medicine physicians, 1,000 of them
opened their practice in 2009 alone. The purpose of this article is fourfold: First, to examine the
history of concierge practices; Second, to compare medical benefits and disadvantages of concierge
practices; Third, to explore the legal implications for concierge physicians and their contractual
agreements with patients; and fourth to determine if a concierge model follows solid ethical
principles. The paper will be concluded with recommendations based on whether concierge
medicine as a whole is in the best interest of the patient or the physician providing the service, as
well as health care as a whole. It is the authors’ goal to provide unbiased information about
concierge medicine so that readers can make informed decisions.
Cost Outcomes
This section includes articles that summarize cost and other outcomes-related metrics for the DPC model of care or
similarly structured primary care arrangements. Reference information for each article along with key excerpts are
provided below. Note that comments are directly from sources and do not represent author’s statements or opinions.
DPC (Adjusted)
Musich, Shirley, Andrea Klemes, Michael Kubica, Sara Wang, and Kevin Hawkins. 2014. Personalized
Preventive Care Reduces Health Care Expenditures Among Medicare Advantage Beneficiaries. American
Journal of Managed Care 20, no. 8:613–620.
Objectives: To investigate the impact on health care expenditure and utilization trends of a
personalized preventive care program designed to deliver individualized care focused on disease
prevention among Medicare Advantage beneficiaries.
Study Design: MD-Value in Prevention (MDVIP) consists of a network of affiliated primary care
physicians who utilize a model of health care delivery based on an augmented physician-patient
relationship and focused on personalized preventive health care. The cost-effectiveness of the
program was estimated using medical and pharmacy claims data relative to nonmembers.
Methods: Multivariate modeling was used to control for demographic, socioeconomic, supply of
health care services, and health status differences between members and nonmembers. Health
care expenditure and utilization trends for members and nonmembers were tracked from the pre-
period prior to member enrollment for a period of two years post enrollment.
Results: MDVIP members experienced significantly reduced utilization rates for emergency
department visits and inpatient admissions. Reduced medical utilization resulted in program savings

69
Copyright © 2020 Society of Actuaries
of $86.68 per member per month (PMPM) in year 1 and $47.03 PMPM in year two compared with
nonmembers.
Conclusions: A primary care model based on an augmented physician-patient relationship and
focused on personalized preventive medicine can reduce Medicare Advantage health care
spending.
Musich, Shirley, Shaohung, Wang, Kevin, Hawkins, and Andrea, Klemes. 2016. The Impact of Personalized
Preventive Care on Health Care Quality, Utilization, and Expenditures. Population Health Management 19,
no. 6:389–397.
Abstract: The objective of this study was to evaluate the impact on health care utilization and
expenditure trends over time of a personalized preventive medicine program delivering
individualized care focused on lifestyle behavior modification, disease prevention, and compliance
with quality-related metrics. MD-Value in Prevention (MDVIP) is a network of affiliated primary care
physicians who utilize a model of health care delivery based on an augmented physician-patient
relationship and focused on personalized preventive health care. Multivariate modeling was used
to control for demographics, socioeconomics, supply of health care services, and health status
among 10,186 MDVIP members and randomly selected, matched nonmembers. Health care
utilization and expenditure trends were tracked from the pre period prior to member enrollment
for a period of up to three years post enrollment. MDVIP members experienced reduced utilization
of emergency room and urgent care services compared to nonmembers. Program savings ranges
indicated that, over time, increasing percentages of members achieved cost savings compared to
nonmembers. Older age groups were more likely to realize savings in the early years with preventive
activities indicating condition management, and younger age groups were most likely to achieve
savings by the third year after enrollment. These results indicate that a primary care model based
on an enhanced physician-patient relationship and focused on quality and personalized preventive
care within a time frame of three years can achieve positive health care expenditure outcomes and
improved health management.
DPC (Unadjusted)
Restrepo, Katherine, and Julie, Tisdale. Direct Primary Care for Local Governments. John Locke Foundation,
December 2, 2016, https://www.johnlocke.org/research/direct-primary-care-for-local-governments/
(accessed January 9, 2020).
Introduction: Local governments across North Carolina, like other employers, are wrestling with the
question of how to provide quality health care to their employees in a cost-effective manner. This
is particularly important for local governments because those plans are paid for by taxpayers.
One county, Union County, has piloted an innovative program in an attempt to both lower the cost
of providing health care to its employees and improve the quality of, and access to, that care. In
2015, Union County expanded its health benefits to include a Direct Primary Care (DPC) option for
employees. It is the first county in the state to offer such a plan, and its experience offers valuable
lessons to other counties.
DPC in Union County, NC: Local governments, like all employers, are concerned with fulfilling the
“quadruple aim,” goals generally agreed to by the health care industry:
1. Improve provider engagement
2. Improve overall population health
3. Enhance the patient experience
4. Lower cost of care

70
Copyright © 2020 Society of Actuaries
This is what motivated Union County Human Resources Executive Director Mark Watson to consider
whether DPC could be a beneficial addition to the health care options provided to the county’s
employees.
Granted, employers have been combating rising health care costs by transitioning their workers
from comprehensive plans to consumer-driven health plans (CDHPs). These plans come with lower
premiums and higher out-of-pocket cost sharing, and they are paired with either a tax-preferential
health savings account (HSA) or health reimbursement account (HRA). The idea behind CDHPs is
that when policyholders are responsible for a higher portion of out-of-pocket medical expenses,
they will be more cost-conscious and shop around for the best value for health care dollars spent.
Twenty-four percent of workers are enrolled in these types of plans.
Consumer-driven plans do not come without criticism, however. For the healthy and high-wage
earners, making the switch may not be so much of a problem. However, it can impose financial
burdens on low-wage workers and for those who frequent the health care system.
Union County was an early adopter in providing its employees with a CDHP starting in 2003. Watson
says that such benefit packages can yield high satisfaction rates if they are designed and managed
properly. Watson and other key players then took an additional step to optimize the consumer-
driven model by bringing in Paladina Health, a Direct Primary Care provider.
In April 2015, Union County added DPC to the mix, allowing employees to choose to receive their
primary care services from a DPC primary care physician at a clinic set up near government offices.
After the first year, results have been promising.
Results: According to 2015-2016 results, DPC saved Union County, and the taxpayers who foot the
bill, over $1.28 million in health care claims. This calculation is based on a comparison of the
average-per-employee per-month (PEPM) cost of both medical and prescription claims incurred by
employees who subscribe only to Union County’s consumer-driven health plan versus those who
use DPC. The previous table illustrates that the $1.28 million represents an average PEPM savings
of over $260 for the 44 percent of Union County’s employees who have chosen DPC.
DPC participants:
• incur 23 percent less in medical expenses than CDHP participants, yielding annual savings
of $1.28 million
• incur 36 percent less in prescription expenses compared to CDHP participants, yielding
annual savings of $239,000
• spend 46 percent less out-of-pocket for prescription and medical expenses than CDHP
patients, a $333,639 annual savings
• report significant improvement in their overall health since electing the DPC option by a
nearly 3 to 1 margin
Union County was able to implement DPC while also saving money. They did so by redirecting the
$750 they were previously putting into a health reimbursement account (HRA) and using it instead
to pay for a portion of the employees’ DPC memberships. This, along with claims savings, allows
Union County to extend an added benefit to its employees at lower cost.
Nextera Health Care. Nextera Health Care + DigitalGlobe: A Case Study. 2016, https://nexterahealth
care.com/wp-content/uploads/2016/08/NH-Digital-Globe-Study-2016.pdf (accessed January 9, 2020).

71
Copyright © 2020 Society of Actuaries
Evaluating the DPC Option: The DigitalGlobe HR Team reviewed the DPC model to see if it appeared
to meet all three criteria: an improved experience, better health outcomes, and cost savings. They
were encouraged since it seemed likely that:
• Employees would enjoy improved access to a personal physician and health care team.
• Employees’ health conditions would be detected earlier and treatment compliance would
be improved by breaking down barriers to care (e.g., inconvenience and doctor
inaccessibility).
• Costs would likely be reduced for DigitalGlobe, thanks to fewer spur-of-the-moment
Emergency Department/Urgent Care visits, better long-term management of chronic
conditions, and fewer claims to process.
• Costs would be reduced for employees, thanks to waived or significantly reduced fees for
office visits and lab/diagnostic tests.
Choosing a DPC Partner: DigitalGlobe approached several of the larger DPCs serving Colorado, but
none were willing to take on a short-term trial, and all required a minimum sign-up level beyond
what DigitalGlobe could guarantee.
At the same time, several DigitalGlobe employees suggested the company talk to Nextera Health
care—the first DPC practice in Colorado, founded in 2011. Many of these employees already were
seeing Nextera Health care’s doctors in Longmont, Frederick and Boulder through their fee-for-
service practice, North Vista Medical Center. After extensive discussions, DigitalGlobe agreed to
partner with Nextera Health care on the case study.
Hopkins recalls, “We felt good about the opportunity to work with Nextera Health care because
they were willing to give our employees the high-touch experience we wanted for them and they
clearly were in the growth mode, eager for our input, and willing to offer personalized solutions—
including ergonomic assessments, an on-site clinic, and targeted ‘lunch and learns.’”
Nextera Health care’s locations mirrored DigitalGlobe’s facilities, with offices in Boulder, Longmont,
and Frederick. DigitalGlobe was in the process of relocating many employees from Longmont to a
new facility 25 miles south in Westminster, and Nextera Health care agreed to offer coverage
through an affiliated office there as well.
Clint Flanagan, M.D., Founder and CEO of Nextera Health care, explains, “One of the great things
about the DPC model is that it is scalable. DigitalGlobe was the first client we took on that had more
than one campus, but thanks to affiliate relationships—we now have several extending as far south
as Colorado Springs—we can efficiently expand our footprint. We thoroughly vet these affiliate
practices and work with them to implement our DPC model, standards, and practices, so patient
service is seamless from location to location.”
The arrangement between Nextera Health care and DigitalGlobe was finalized in April 2015, with
coverage starting on June 1, 2015. In addition to setting out the per-member per-month rate, the
agreement stipulated specific preventive and primary care services Nextera Health care would
provide and the discounted rates for certain specialists, diagnostic services, and integrative
treatments, such as acupuncture and hypnosis. Nextera Health care physicians and nurses would
staff an on-site clinic at DigitalGlobe’s Westminster facility on two days each month (and expand
that presence if demand warranted), as well as arrange for ergonomic training for DigitalGlobe’s
employees.
Overall claim costs: The overall incurred claim costs for the DigitalGlobe employees participating in
the case study were less than the costs for their co-workers not in the study. While the claims data

72
Copyright © 2020 Society of Actuaries
suggest that relatively healthy employees were more inclined to participate in the study, during the
study, their claim costs declined much more on a percentage basis compared to their peers.
Nextera
Health Care
Members
Claims
PMPM
1/1/2015–
5/31/2015
$283.91
6/1/2015–
12/31/2015*
$211.93
*Period of
the case
study
(25.4%
reduction)
Qliance. New Primary Care Model Delivers 20 Percent Lower Overall Health care Costs, Increases Patient
Satisfaction and Delivers Better Care. Cision PR Newswire, January 25, 2015,
https://www.prnewswire.com/news-releases/new-primary-care-model-delivers-20-percent-lower-overall-
healthcare-costs-increases-patient-satisfaction-and-delivers-better-care-300021116.html (accessed
January 9, 2020).
Introduction: A review of two years’ worth of health care claims data on thousands of patients
reveals, contrary to the prevailing view, that unlimited primary care drives down overall costs while
improving patient outcomes and experience.
The analysis by Qliance Medical Management Inc. – hailed by Time magazine as “one of the most
intriguing experiments in the medical industry” – reveals that the increasingly popular “direct
primary care” model, with its emphasis on unrestricted access to primary care, makes health care
20 percent less expensive than traditional health insurance yet leaves patients feeling more satisfied
with their care.
The success of the monthly-fee primary care model challenges the notion that simply making
traditional health insurance available to all is the best way to heal the nation’s troubled health care
system, according to Qliance President and Chief Executive Officer Erika Bliss, MD.
Methods: Qliance examined insurance claims data from 2013 and 2014 for approximately 4,000
Qliance patients covered by employer benefit plans, and compared the cost of their care to that of
non-Qliance patients who worked for the same employers. The results (see table) revealed a savings
of $679,000 per 1,000 Qliance patients on total claims –19.6 percent less than the total claims for
non-Qliance patients during the same period. The savings were driven by a marked reduction in
expensive emergency room visits, inpatient care, specialist visits, and advanced radiology, which
more than made up for the higher investment in primary care for Qliance patients.
Rather than coming at the expense of patient satisfaction, the cost savings were accompanied by a
strong uptick in the overall patient experience. A 2014 assessment of Qliance’s patients’ experience,
conducted using the national CAHPS survey, placed Qliance above the 95th percentile in overall
patient satisfaction, well above the 90th percentile nationally.
Nextera Health Care Non-Members
Claims PMPM
1/1/2015–5/31/2015
$408.31
6/1/2015–12/31/2015*
$388.09
*Period of the case study
(4.1% reduction)

73
Copyright © 2020 Society of Actuaries
Qliance Savings Data – 2013–2014
PCMH (Adjusted)
Ghany, Reyan, Leonardo, Tamariz, Gordon, Chen, Elissa, Dawkins, Alina, Ghany, et al. 2018. High-Touch
Care Leads to Better Outcomes and Lower Costs in a Senior Population. American Journal of Managed Care
24, no. 9:e300–e304.
Objectives: There are several models of primary care. A form of high-intensity care is a high-touch
model that uses a high frequency of encounters to deliver preventive services. The aim of this study
is to compare the health care utilization of patients receiving two models of primary care, with high-
touch care and 1 without.
Study Design: Retrospective cohort study.
Methods: We conducted a retrospective cohort study of two models of care used among Medicare
Advantage populations. Model 1 is a high-touch care model, and model two is a standard care
model. Compared with model 2, model 1 has smaller panel sizes and a higher frequency of
encounters. We compared patients’ health care utilization and hospitalizations between both
models using a propensity score–matched analysis, matching by Charlson Comorbidity Index (CCI)
score, age, and gender.
Results: We included 17,711 unmatched Medicare Advantage primary care patients and matched
5,695 patients from both models of care. CCI scores, age, and gender were similar between both
matched groups (P >.05). The median total per member per month health care costs in model 1
were $87 (95% CI, $26-$278) compared with $121 (95% CI, $52-$284) in model 2 (P <.01). The mean
number of hospital admissions was lower in model 1 (0.10 ± 0.40) compared with model 2 (0.20 ±
0.58). The number of primary care physician visits and preventive medication use were higher in
model 1 (P <.05 for both).
Conclusions: In a propensity-matched sample of Medicare Advantage patients, those receiving high-
touch care had lower health care costs and fewer hospitalizations. Potential explanations are higher
preventive medication use and more frequent visits.
Neal, Jason, Ravo, Chawla, Christine M., Colombo, Richard L., Snyder, and Somesh, Nigam. 2015. Medical
Homes: Cost Effects of Utilization by Chronically Ill Patients. American Journal of Managed Care 21, no. 1:
e51–e61.
Incidents
Per 1,000
Qliance
Patients
Incidents Per
1,000 Non-
Qliance
Patients
Difference
(Qliance vs.
Other)
Savings per
patient per
year
ER Visits
81
94
−14%
($5)
Inpatient (days)
100
250
−60%
$417
Specialist Visits
7,497
8,674
−14%
$436
Advanced Radiology
310
434
−29%
$82
Primary Care Visits
3,109
1,965
+58%
($251)
Savings Per Patient
---
---
---
$679
Total Savings per 1000 (after Qliance fees)
$679,000
% Saved Per Patient
19.6%

74
Copyright © 2020 Society of Actuaries
Objectives: The impact of primary care practices adopting the patient-centered medical home
(PCMH) model is analyzed by comparing per member per month (PMPM) costs and utilization
among commercial HMO members with chronic illnesses in PCMH and non-PCHM practices in the
Philadelphia area. Transforming primary care practices to conform to the PCMH model has shown
early promise in reducing costs and improving outcomes, and chronically ill patients’ frequent
contact with the health care system and costly care make them ideal targets for such health system
reforms.
Study Design and Methods: The impact of the PCMH model on PMPM costs was analyzed using a
generalized linear regression model to adjust for age, gender, and baseline cost. The impact of the
PCMH model on utilization per 1000 rates was analyzed with the Poisson regression model,
adjusting for baseline differences in age, gender, and risk score.
Results: After accounting for differences at baseline, PCMH practices achieved lower total, inpatient,
and specialist PMPM costs, as well as lower relative utilization of hospital admissions and specialist
visits.
Conclusions: These findings suggest that policy makers should maintain or expand incentives to
adopt PCMH reforms and that targeting chronically ill patients may be the most effective way to
leverage the benefits of PCMH adoption.
Cole, Evan S., Claudia, Campbell, Mark L., Diana, Larry, Webber, and Richard, Culbertson. 2015. Patient-
Centered Medical Homes In Louisiana Had Minimal Impact On Medicaid Population’s Use Of Acute Care
And Costs. Health Affairs 34, no. 1: 87–94.
Abstract: The patient-centered medical home model of primary care has received considerable
attention for its potential to improve outcomes and reduce health care costs. Yet little information
exists about the model’s ability to achieve these goals for Medicaid patients. We sought to evaluate
the effect of patient-centered medical home certification of Louisiana primary care clinics on the
quality and cost of care over time for a Medicaid population. We used a quasi-experimental pre-
post design with a matched control group to assess the effect of medical home certification on
outcomes. We found no impact on acute care use and modest support for reduced costs and
primary care use among medical homes serving higher proportions of chronically ill patients. These
findings provide preliminary results related to the ability of the patient-centered medical home
model to improve outcomes for Medicaid beneficiaries. The findings support a case-mix-adjusted
payment policy for medical homes going forward.
David, Guy, Candace, Gunnarsson, Philip A., Saynisch, Ravi, Chawla, and Somesh, Nigam. 2015. Do Patient-
Centered Medical Homes Reduce Emergency Department Visits? Health Service Research 50, no. 2:418–
439.
Objective: To assess whether adoption of the patient-centered medical home (PCMH) reduces
emergency department (ED) utilization among patients with and without chronic illness.
Data Sources: Data from approximately 460,000 Independence Blue Cross patients enrolled in 280
primary care practices, all converting to PCMH status between 2008 and 2012.
Research Design: We estimate the effect of a practice becoming PCMH-certified on ED visits and
costs using a difference-in-differences approach, which exploits variation in the timing of PCMH
certification, employing either practice or patient fixed effects. We analyzed patients with and
without chronic illness across six chronic illness categories.

75
Copyright © 2020 Society of Actuaries
Principal Findings: Among chronically ill patients, transition to PCMH status was associated with 5–
8 percent reductions in ED utilization. This finding was robust to a number of specifications,
including analyzing avoidable and weekend ED visits alone. The largest reductions in ED visits are
concentrated among chronic patients with diabetes and hypertension.
Conclusions: Adoption of the PCMH model was associated with lower ED utilization for chronically
ill patients, but not for those without chronic illness. The effectiveness of the PCMH model varies
by chronic condition. Analysis of weekend and avoidable ED visits suggests that reductions in ED
utilization stem from better management of chronic illness rather than expanding access to primary
care clinics.
Friedberg, Mark W., Eric C., Schneider, Meredith B., Rosenthal, et al. 2014. Association Between
Participation in a Multipayer Medical Home Intervention and Changes in Quality, Utilization, and Costs of
Care. Journal of the American Medical Association 311, no. 18:815–825.
Importance: Interventions to transform primary care practices into medical homes are increasingly
common, but their effectiveness in improving quality and containing costs is unclear.
Objective: To measure associations between participation in the Southeastern Pennsylvania Chronic
Care Initiative, one of the earliest and largest multipayer medical home pilots conducted in the
United States, and changes in the quality, utilization, and costs of care.
Design, Setting, and Participants: Thirty-two volunteering primary care practices participated in the
pilot (conducted from June 1, 2008, to May 31, 2011). We surveyed pilot practices to compare their
structural capabilities at the pilot’s beginning and end. Using claims data from four participating
health plans, we compared changes (in each year, relative to before the intervention) in the quality,
utilization, and costs of care delivered to 64,243 patients who were attributed to pilot practices and
55,959 patients attributed to 29 comparison practices (selected for size, specialty, and location
similar to pilot practices using a difference-in-differences design.
Exposures: Pilot practices received disease registries and technical assistance and could earn bonus
payments for achieving patient-centered medical home recognition by the National Committee for
Quality Assurance (NCQA).
Main Outcomes and Measures: Practice structural capabilities; performance on 11 quality measures
for diabetes, asthma, and preventive care; utilization of hospital, emergency department, and
ambulatory care; standardized costs of care.
Results: Pilot practices successfully achieved NCQA recognition and adopted new structural
capabilities, such as registries to identify patients overdue for chronic disease services. Pilot
participation was associated with statistically significantly greater performance improvement,
relative to comparison practices, on 1 of 11 investigated quality measures: nephropathy screening
in diabetes (adjusted performance of 82.7% vs 71.7% by year 3, P < .001). Pilot participation was
not associated with statistically significant changes in utilization or costs of care. Pilot practices
accumulated average bonuses of $92,000 per primary care physician during the 3-year intervention.
Blumenthal, David, Sara, Collins, and David C., Radley. 2015. A Difference-in-Difference Analysis of Changes
in Quality, Utilization and Cost Following the Colorado Multi-Payer Patient-Centered Medical Home Pilot.
Journal of General Internal Medicine 31, no. 3:289–296.
Background: Research on the effects of patient centered medical homes on quality and cost of care
is mixed, so further study is needed to understand how and in what contexts they are effective.

76
Copyright © 2020 Society of Actuaries
Objective: We aimed to evaluate effects of a multi-payer pilot promoting patient-centered medical
home implementation in 15 small and medium-sized primary care groups in Colorado.
Design: We conducted difference-in-difference analyses, comparing changes in utilization, costs,
and quality between patients attributed to pilot and non-pilot practices.
Participants: Approximately 98,000 patients attributed to 15 pilot and 66 comparison practices two
years before and three years after the pilot launch.
Main measures: Health care Effectiveness Data and Information Set (HEDIS) derived measures of
diabetes care, cancer screening, utilization, and costs to payers.
Key Results: At the end of two years, we found a statistically significant reduction in emergency
department use by 1.4 visits per 1000 member months, or approximately 7.9 % (p=0.02). At the end
of three years, pilot practices sustained this difference with 1.6 fewer emergency department visits
per 1000 member months, or a 9.3 % reduction from baseline (p=0.01). Emergency department
costs were lower in the pilot practices after two (13.9 % reduction, p<0.001) and three years (11.8
% reduction, p=0.001). After three years, compared to control practices, primary care visits in the
pilot practices decreased significantly (1.5 % reduction, p=0.02). The pilot was associated with
increased cervical cancer screening after two (12.5 % increase, p<0.001) and three years (9.0 %
increase, p<0.001), but lower rates of HbA1c testing in patients with diabetes (0.7 % reduction at
three years, p=0.03) and colon cancer screening (21.1 % and 18.1% at two and three years,
respectively, p<0.001). For patients with two or more comorbidities, similar patterns of association
were found, except that there was also a reduction in ambulatory care sensitive inpatient
admissions (10.3%; p=0.05).
Conclusion: Our findings suggest that a multi-payer, patient-centered medical home initiative that
provides financial and technical support to participating practices can produce sustained reductions
in utilization with mixed results on process measures of quality.
Meyers, David J., Alyna, Chien, Kevin H., Nguyen, Zhonghe, Li, Sara J., Singer, et al. 2019. Association of
Team-Based Primary Care with Health Care Utilization and Costs Among Chronically Ill Patients. Journal of
the American Medical Association 179, no. 1:54–61.
Importance: Empirical study findings to date are mixed on the association between team-based
primary care initiatives and health care use and costs for Medicaid and commercially insured
patients, especially those with multiple chronic conditions.
Objective: To evaluate the association of establishing team-based primary care with patient health
care use and costs.
Design, Setting, and Participants: We used difference-in-differences to compare preutilization and
postutilization rates between intervention and comparison practices with inverse probability
weighting to balance observable differences. We fit a linear model using generalized estimating
equations to adjust for clustering at 18 academically affiliate primary care practices in the Boston,
Massachusetts, area between 2011 and 2015. The study included 83,953 patients accounting for
138,113 patient-years across 18 intervention practices and 238,455 patients accounting for 401,573
patient-years across 76 comparison practices. Data were analyzed between April and August 2018.
Exposures: Practices participated in a four-year learning collaborative that created and supported
team-based primary care.

77
Copyright © 2020 Society of Actuaries
Main Outcomes and Measures: Outpatient visits, hospitalizations, emergency department visits,
ambulatory care–sensitive hospitalizations, ambulatory care–sensitive emergency department
visits, and total costs of care.
Results: Of 322,408 participants, 176,259 (54.7%) were female; 64,030 (19.9%) were younger than
18 years and 258,378 (80.1%) were age 19 to 64 years. Intervention practices had fewer
participants, with two or more chronic conditions (n = 51,155 [37.0%] vs n = 186,954 [46.6%]), more
participants younger than 18 years (n = 337,931 [27.5%] vs n = 74,691 [18.6%]), higher Medicaid
enrollment (n = 39,541 [28.6%] vs n = 81,417 [20.3%]), and similar sex distributions (75,023 women
[54.4%] vs 220,097 women [54.8%]); however, after inverse probability weighting, observable
patient characteristics were well balanced. Intervention practices had higher utilization in the pre-
period. Patients in intervention practices experienced a 7.4% increase in annual outpatient visits
relative to baseline (95%CI, 3.5%-11.3%; P < .001) after adjusting for patient age, sex, comorbidity,
zip code level sociodemographic characteristics, clinician characteristics, and plan fixed effects. In a
subsample of patients with two or more chronic conditions, there was a statistically significant
18.6% reduction in hospitalizations (95%CI, 1.5%-33.0%; P = .03), 25.2% reduction in emergency
department visits (95%CI, 6.6%-44.0%; P = .007), and a 36.7% reduction in ambulatory care–
sensitive emergency department visits (95%CI, 9.2%-64.0%; P = .009). Among patients with less than
two comorbidities, there was an increase in outpatient visits (9.2%; 95%CI, 5.10%-13.10%; P < .001),
hospitalizations (36.2%; 95%CI, 12.2-566.6; P = .003), and ambulatory care–sensitive
hospitalizations (50.6%; 95%CI, 7.1%-329.2%; P = .02).
Conclusions and Relevance: While establishing team-based care was not associated with differences
in the full patient sample, there were substantial reductions in utilization among a subset of
chronically ill patients. Team-based care practice transformation in primary care settings may be a
valuable tool in improving the care of sicker patients, thereby reducing avoidable use; however, it
may lead to greater use among healthier patients.
Regulatory Considerations
This section includes articles that summarize regulatory issues and considerations relating to the DPC model of care.
Reference information for each article along with key excerpts are provided below. Note that comments are directly
from sources and do not represent authors’ statements or opinions.
Health Policy Programs Group. Direct Primary Care (DPC): Potential Impact on Cost, Quality, Health
Outcomes, and Provider Workforce Capacity. University of Wisconsin Population Health Institute, 2018,
https://docs.legis.wisconsin.gov/misc/lc/study/2018/1790/010_july_24_2018_meeting_10_00_a_m_room
_412_east_state_capitol/uw_dpc_brief (accessed December 11, 2018).
Introduction: Direct Primary Care (DPC) contracts, or “medical retainer agreements,” are a health
care delivery model where a provider offers unlimited specified routine health care services for a
monthly fee. Proponents of DPC suggest that the delivery method will improve access to care,
reduce administrative costs, foster stronger patient-provider relationships, and reduce reliance on
expensive emergency department services. Critics of DPC contend that it double-charges for
services already covered by insurance, and that DPC contracts lack accountability for quality and
access. This paper 1) describes proposed and existing DPC bills, 2) reviews existing DPC experience
and evaluations, and 3) considers what effect DPC could have on health care in Wisconsin.
Federal Law and DPCs: The Patient Protection and Affordable Care Act (ACA) allows a qualified health
plan (QHP) issuer to “provide coverage through a direct primary care medical home…so long as the
QHP meets all requirements that are otherwise applicable and the services covered by the direct

78
Copyright © 2020 Society of Actuaries
primary care medical home are coordinated with the QHP issuer.” That is, DPC may be included in
plans sold on the ACA insurance exchanges, but must be paired with a wraparound insurance policy
covering everything outside of primary care.
In April 2018, the federal Centers for Medicare and Medicaid Services (CMS) released a public
request for information regarding DPC models for primary care and other specialties, titled “Direct
Provider Contracting.” CMS solicited input on direct provider contracting between payers and
primary care or multi-specialty groups. This would inform potential testing of a DPC model within
the Medicare fee-for-service program (Medicare Parts A and B), Medicare Advantage program
(Medicare Part C), and Medicaid.
Current Internal Revenue Service (IRS) rules prohibit individuals with health savings accounts (HSAs)
paired with high deductible health plans (HDHPs) from having an agreement with a DPC provider.
The IRS interprets DPC arrangements as health plans under Section 223(c) of the Internal Revenue
Code, The law is unclear whether primary care services are qualified health expenses under Section
213(d) of the code if paid for as a capitated periodic fee rather than on a fee for service basis. IRS
regulations require HSAs be paired with an HDHP, and the HSA holder may not have a second health
plan. The IRS interpretation of DPC as a health plan bars an individual who has an agreement with
a DPC provider from funding an HSA.
A bipartisan bill in Congress, the Primary Care Enhancement Act (HR 365/S. 1358), clarifies the tax
code regarding the use of HSAs for DPC. The bill would clarify the tax code to allow patients with
HSAs paired with HDHPs to use those funds to pay for periodic fee-based DPC. As of June 2018, the
House Committee on Ways and Means has not yet considered this bill.
Federal Medicaid law specifies that that “The State Medicaid agency must require all ordering or
referring physicians or other professionals providing services under the State plan or under a waiver
of the plan in the fee-for-service program to be enrolled as participating Medicaid providers.” A DPC
provider would need to be a Medicaid participating provider to serve Medicaid members. However,
CMS has determined that, in Medicaid risk-based managed care arrangements, states hold
discretion over provider enrollment requirements for the ordering or referring physicians. An
advocacy website of a group that supports expansion of DPC contracts reviews questions that DPC
practices have about this CMS guidance.
State Law and DPCs: Twenty-five states have passed legislation generally defining DPC outside of
state insurance regulation. This state action defines DPC as a medical service, not a health plan.
Wisconsin, Georgia, Maryland, Pennsylvania and South Carolina have introduced DPC legislation,
but have not enacted those bills into law. Montana Governor Steve Bullock is the only governor to
have vetoed a DPC bill, doing so in 2017.
Eskew, Philip. 2017. Direct Primary Care Business of Insurance and State Law Considerations. Journal of
Legal Medicine 37, no. 1–2:145–154.
Introduction: Direct Primary Care (“DPC”) practices have been small and overlooked group for many
years. Recent growth may gain the attention of previously tacit insurance commissioners. Laws
enacted by seventeen state legislatures and the Affordable Care Act provide a background from
which a legal framework can be developed. This Article will articulate “business of insurance”
concerns encountered by DPC physicians, recommend contractual drafting techniques to minimize
this risk, and compare state legislation designed chiefly to address this concern. The Article will also
consider the DPC provisions of the Affordable Care Act, and attempt to anticipate future regulatory
debates about the scope of practice of physicians using the DPC model.

79
Copyright © 2020 Society of Actuaries
Summary: Physicians electing to operate a DPC practice should be aware that legal, policy, and
regulatory issues are continually evolving. The lack of legislation the majority of states should not
be a concern at this stage. Only three out of six states with legislation aimed at encouraging DPC
practices made any attempt to define DPC or similar terms, and the three that attempted a
definition largely missed the mark. Look to the three part definition above and model legislation
when speaking to your state legislators. Monitor the anticipated debates about the tax treatment
of DPC periodic fees, and anticipate the scope of practice discussions that are likely to follow.
Physicians are also advised to consult competent legal counsel who are familiar with DPC.
Eskew, Philip. 2014. Direct Primary Care Membership Medicine. West Virginia Medical Journal 110, no. 2:8–
11.
Introduction: Health policy experts often debate how to increase access to physicians via increased
third party funding. Often overlooked, third party free medical practices increase access via lower
costs. The direct primary care membership medicine (“DPCMM”) model, a type of third party free
practice referred to by some as concierge for the masses, is a wonderful option for West Virginians.
Under the DPCMM model patients send a flat monthly payment directly to their family physician
without any insurance company or government involvement. In exchange for this single payment
the patient may visit the physician without incurring a per visit charge. This monthly membership
fee is the only payment requested of the patient, and is often an excellent option for those without
insurance or those that wish to pair it with a high deductible health insurance (“HDHP”) plan.
Depending upon the office, the fee often covers basic radiologic and lab testing, and sometimes
standard prescriptions. Since no per visit fees are charged, state insurance commissioners have
threatened these physicians by arguing that this practice style amounts to the “unauthorized
practice of insurance.”
Unfortunately, the DPCMM model of care remains in its infancy more than ten years after its initial
development. This lack of progress is due to barriers within the insurance industry, state
government, and federal government, coupled with a lack of physician entrepreneurship. Only four
states (West Virginia, Washington, Oregon, and Utah) have enacted legislation encouraging
physicians to practice using the DPCMM model. This article will: 1) compare West Virginia and
Washington legislation permitting the formation of DPCMM pilot programs that are outside the
“business of insurance;” 2) briefly discuss other state and federal concerns, and 3) analyze the scope
of primary care services permitted within these DPCMM models.
Restrepo, Katherine. Direct Primary Care: Restoring the Doctor-Patient Relationship. John Locke
Foundation, 2016, https://www.johnlocke.org/app/uploads/2016/02/DPC-Spotlight.pdf (accessed January
9, 2020).
Recommendations: While DPC in North Carolina faces minimal regulatory hurdles at the state level,
it would be wise for policymakers to pass legislation that simply states that direct care providers do
not act as a risk-bearing entity, so that patients’ monthly DPC membership fees are not classified as
an insurance premium. Legislation that clearly defines DPC as not being an insurance product will
save this health care delivery method from being subject to regulations under the North Carolina
Department of Insurance (DOI). To date, 13 states have enacted legislation that specifically defines
DPC not acting as insurance. Passing clarifying legislation would likely lead to a stronger DPC
presence in North Carolina. It would also assist in rekindling the appeal of the primary care
profession, which in turn would help mitigate the projected primary care physician shortage.
Flood, Jarrett. Direct Primary Care in Louisiana: A White Paper for Louisiana Lawmakers and Health care
Stakeholders In Support of Senate Bill 516. Flood International Consulting Agency, April 2014,

80
Copyright © 2020 Society of Actuaries
http://www.floodconsulting.com/pdf/Direct%20Primary%20Care%20in%20La_Support%20for%20SB516.pd
f (accessed January 9, 2020).
Forward: The State of Washington is generally considered a “healthy” state. In a side-by-side
comparison to Louisiana in factors, such as obesity, smoking, diabetes and more, America’s Health
Rankings® ranks Washington State #14; Louisiana #48. Even Washington, however, has its state
health care challenges, including a primary care physician shortage. In Washington, a privatized
medical practice model, Direct Primary Care (DPC), has emerged to help meet individuals’ and
employees’ primary care needs. Direct Primary Care is a medical practice model of paying for
primary care outside of insurance. Individuals or businesses pay for unlimited access to care for a
flat monthly fee. Hallmarks of DPC are its patient-centered and preventive medicine approaches to
health care. Since passage of Washington’s DPC law, DPC practices have expanded into 11 counties.
As of 2012, there were 29 practices, and the number continues to rise. Seattle-based DPC provider
Qlinace has attracted several big-name investors including Amazon’s Jeff Bezos and Dell founder
Michael Dell. Venture capitalists elsewhere have also been attracted to DPC. Billionaire Tony Hsieh,
CEO of Zappos, recently invested in Iora Health to bring an innovative DPC practice to his urban
renewal project in downtown Las Vegas. Other large DPC providers, such as Medlion, Paladina and
others are expanding, some nationally. The “little guys” are getting involved too. Individual doctor-
entrepreneurs, eager to return to the concept of old-fashioned patient-centered health care, are
creating direct primary care practices across the U.S. Direct Primary Care is explicitly a medical
practice model and not insurance. Even so, a few lawmakers in other state have mislabeled the flat-
fee payment model as “risk” and its patient fee agreement as an “insurance premium.” This white
paper seeks to clarify the DPC concept, distinguish it from insurance products, increase awareness
of the model and describe DPC’s overall win-win. Passage of Senate Bill 516 recognizing DPC as a
medical practice model would facilitate unencumbered expansion of new DPC practices in the State.
SB516 will also provide a welcoming business environment that could bring new health care
investments and resources into Louisiana. We ask your support in passing the bill. Thank you for
taking time to review this information. I look forward to answering your questions and meeting with
lawmakers and health care stakeholders to discuss this topic.
Maryland Insurance Administration. Report on “Retainer” or “Boutique” or “Concierge” Medical Practices and
the Business of Insurance (MIA-2008-12-002). Maryland Insurance Administration, January 2009,
https://insurance.maryland.gov/consumer/documents/agencyhearings/2009retainermedicinereport-final.pdf
(accessed January 9, 2020).
Introduction: In late 2008, the Maryland Insurance Administration (“MIA”) received information
about so-called “boutique”, “concierge” or “retainer” medical practices (hereinafter “retainer
practice”) in which the patient pays an annual fee to a physician for certain services. To ascertain if
these arrangements constitute the business of insurance, the MIA held an informational hearing on
December 19, 2008. The MIA requested individuals and organizations provide information on
retainer medicine in the State of Maryland as noted in Attachment 1. This report summarizes the
information provided to the MIA at its hearing regarding the economic reasons for establishing a
retainer practice, the potential impact of the growth of retainer practices on physician supply, and
the types of retainer practices. It also provides information on the business of insurance and a
framework for ascertaining when a retainer practice is engaged in the business of insurance. It is
important to note what this report does not cover. Much of the literature on retainer practices
focuses on balance billing and medical ethics. These issues were not addressed at the hearing, and
the MIA did not explore these issues.

81
Copyright © 2020 Society of Actuaries
Conclusions: Given the current economic realities of primary care practice, retainer practice is likely
to remain an attractive alternative to some primary care physicians. Physicians interested in
establishing a retainer practice can take certain steps to avoid engaging in the business of insurance.
For the Annual Evaluation Model retainer practice, the annual fee should not exceed the market
value of the services included in the annual physical exam. An annual fee in excess of the market
value of the services included in the annual physical exam may approach a capitation payment,
triggering a finding that the retainer practice is engaged in the business of insurance.
For the Bundled FFS Model retainer practice, the MIA recommends:
• Limiting the services provided in the year for an annual fee to an annual physical exam, a follow-
up office visit and a limited number of other office visits;
• Establishing the annual fee by reviewing the market value of the annual physical exam and a
follow-up office visit, as well as each office visit, with the annual fee equal to sum of the market
value for each specified service;
• Defining the services to be provided in a written agreement;
• Allowing a consumer or the physician to terminate the retainer agreement for any reason and
provide for the pro rata reimbursement of the retainer fee if the written agreement is
terminated; and
• Placing a cap on the number of patients based on the physician’s ability to provide all the
services specified in the written agreement to each patient on the panel.
The MIA reiterates that the “devil is in the contract.” In the interest of resolving issues before they
become problems, the MIA urges physicians and medical practices considering the establishment
of retainer practices to approach the matter with care and to consult with the MIA in advance. And,
for those currently engaged in retainer medicine, the MIA encourages these practices to contact
the MIA to share their written agreements to be sure these retainer practices are not inadvertently
engaging in the business of insurance.
There are other ethical and legal issues physicians should keep in mind when establishing a retainer
practice. These include continuity of care for those patients electing not to participate in the
retainer practice and balance billing. Although not a subject of our review, the MIA strongly
encourages physicians who are interested in establishing a retainer practice and who currently
contract with insurers and/or participate with Medicare to carefully review the statutory, regulatory
and contractual prohibitions on balance billing. And, because of the ethical and legal issues
surrounding retainer practices, the MIA believes physicians should seek appropriate professional
and legal assistance when establishing a retainer practice.
It is not clear how many primary care physicians have established retainer practices. The growth of
retainer practices may decrease the number of primary care physicians available to those who
cannot afford to pay an annual fee. Because any significant growth in retainer practice raises
substantial policy issues regarding access to primary care services, the General Assembly may wish
to explore requiring retainer practices to register with a state agency. In addition, the General
Assembly may wish to consider the broader (non-insurance) public policy implications of the
establishment of retainer practices on health care delivery in Maryland.
Provider Experience
This section includes articles that summarize issues relating to the provider experience and the DPC model of care.
Reference information for each article along with key excerpts are provided below. Note that comments are directly
from sources and do not represent authors’ statements or opinions.

82
Copyright © 2020 Society of Actuaries
Rubin, Rita. 2018. Is Direct Primary Care a Game Changer? Journal of the American Medical Association
319, no. 20:2064–2066.
Direct primary care is related to, but not the same as concierge medicine. Both models charge a
membership or retainer fee, but DPC practices’ fees are typically lower, while their panels are larger.
The average DPC membership fee is $70 a month, according to Jay Keese, director of the Direct
Primary Care Coalition, a lobbying group in Washington, DC, that has 770 member practices in 48
states. The biggest difference, however, is that neither DPC physicians nor their patients file
insurance claims for primary care, unlike concierge physicians.
By not taking insurance and limiting their panels to only several hundred patients, DPC physicians
say they have more time to practice primary care medicine the way it should be practiced, not the
way payers dictate.
“The burnout in the world of doctors is largely fueled by the hectic, crazy overutilization mode that
we have created with our finance system,” said Seattle family practice physician and DPC pioneer
Garrison Bliss, MD, who adopted the no-insurance, retainer-fee model in 1997, before it even had
a name. “There’s this notion that playing along with a corrupt, hopelessly ineffective system is good,
that being forced to see 30 people a day is something you should just get over.” Bliss and other
proponents claim DPC can cut health care spending by keeping patients healthier, thus, reducing
their need for specialty care or hospitalization.
Wu, William N., Garrison, Bliss, Erika B., Bliss, and Larry A., Green. 2010. A Direct Primary Care Medical
Home: The Qliance Experience. Health Affairs 29, 5:959–962.
Practice: Qliance Medical Group.
Who and Where: A Seattle primary care practice accepting patients of all ages, staffed by internists,
family physicians, and nurse practitioners.
Core Innovations: In this direct care practice, in lieu of insurance, patients pay an age-adjusted
monthly fee for unrestricted, comprehensive primary care. Patients have no copayments for visits.
Low overhead allows providers to have small patient panels, giving patients better access and
allowing more time per visit. The objective is to shift care away from expensive specialists and
hospitals.
Key Results: Qliance has established a viable, sustainable business model with low overhead and
patient panels about a third the size of those of the average insurance-based family physician. This
has allowed patients to enjoy much greater access and clinicians to delve much more deeply into
patients’ health issues, do more research on health problems, work more closely with consultants
when necessary, and work more intensively with patients on health change, leading to greater
engagement of and satisfaction among clinicians.
Challenges: Patients still need to have health insurance to cover specialty services, high-cost
procedures, emergency treatments, and hospitalization. Current patient expenses are less than
prevailing insurance rates, but there are no quantified data yet on how this model affects overall
health care costs. A proliferation of similar small-panel practices might exacerbate the shortage of
primary care providers in the near term, although it might eventually attract more physicians to
primary care.
Alexander, George Caleb, Jacob E., Kurlander, and Matthew K., Wynia. 2005. Physicians in Retainer
(“Concierge”) Practice: A National Survey of Physician, Patient, and Practice Characteristics. Journal of
General Internal Medicine 20:1079–1083.

83
Copyright © 2020 Society of Actuaries
Background: Retainer practices represent a new model of care whereby physicians charge an up-
front fee for services that may not be covered by health insurance. The characteristics of these
practices are largely unknown.
Design, Setting, and Participants: We conducted a cross-sectional mail survey of 144 retainer
physicians (58% response rate) and a national random sample of 463 nonretainer physicians (50%
response rate) to compare retainer and nonretainer practices. Outcomes of interest included
physician demographics, size and case-mix of patient panel, services offered and, for retainer
practices, characteristics of practice development.
Results: Retainer physicians have much smaller patient panels (mean 898 vs 2,303 patients,
P<.0001) than their nonretainer counterparts, and care for fewer African-American (mean 7% vs
16%, Po.002), Hispanic (4% vs 14%, P<.001), or Medicaid (5% vs 15%, P<.001) patients. Physicians
in retainer practices are more likely to offer accompanied specialist visits (30% vs 1%), house calls
(63% vs 26%), 24-hour direct physician access (91% vs 40%), and several other services (all P values
<.05). Most retainer physicians (85%) converted from nonretainer practices, but kept few of their
former patients (mean 12%). Most retainer physicians (84%) provide charity care and many
continue to see some patients (mean 17%) who do not pay retainer fees.
Conclusions: Despite differences between retainer and nonretainer practices, there is also
substantial overlap in services provided. These findings, in conjunction with the scope of patient
discontinuity when physicians transition to retainer practice, suggest that ethical and legal debates
about the standing of these practices will endure.
Patient Access
This section includes articles that summarize issues relating to the DPC model of care and patient access. Reference
information for each article along with key excerpts are provided below. Note that comments are directly from sources
and do not represent authors’ statements or opinions.
Cole, Evan S. 2018. Direct Primary Care: Applying Theory to Potential Changes in Delivery and Outcomes.
Journal of the American Board of Family Medicine 31, no. 4:605–611.
Abstract: Direct Primary Care (DPC), where patients pay a fee to a primary care provider to obtain
access to services, is a delivery model that has received notable attention and enthusiasm from
some providers. Proponents of DPC believe that the model increases accessibility, reduces
overhead, and ultimately improves care for patients; however, there is little evidence in the peer-
reviewed literature to support these claims. The objective of this analysis was to apply Starfield’s
adaptation of Donabedian’s Structure-
Process: Outcome conceptual model to evaluate primary care to formally display the links between
potential changes in clinical structure and processes from DPC adoption. Based on existing literature
on the constructs in Starfield’s model, expectations of DPC’s impact at the patient, clinic, and system
levels were defined. DPC uses changes to financing and the population eligible to trigger potential
gains in continuity and accessibility to subsequently improve care processes. There is evidence to
support DPC as a theoretically sound approach to improve attributes of primary care, such as first
contact care and longitudinality at the clinic level for participating patients. At the health system
level, DPC has low-construct validity that would suggest a positive impact on the potentially eligible
population’s health due to membership fees that exclude patients who are more likely to be
vulnerable and complex than patients who are willing and able to stay in the practice. Descriptive
and comparative research of included and excluded patients is needed to inform providers,

84
Copyright © 2020 Society of Actuaries
patients, and policy makers of the DPC’s ability to attain the attributes of primary care and ultimately
achieve better outcomes over alternative primary care delivery and financing models. Meanwhile,
theoretic application informed by years of research on primary care provide insight as to what
changes to expect and to monitor as practices consider DPC adoption.
Eskew, Philip, and Kathleen, Klink. 2015. Direct Primary Care: Practice Distribution and Cost across the
Nation. Journal of the American Board of Family Medicine 28, no. 6:793–801.
Abstract: Direct primary care (DPC) is an emerging practice alternative that (1) eliminates traditional
third-party fee-for-service billing and (2) charges patients a periodic fee for primary care services.
We describe the DPC model by identifying DPC practices across the United States; distinguish it from
other practice arrangements, such as the “concierge” practice; and describe the model’s pricing
using data compiled from existing DPC practices across the United States. Lower price points and a
broad distribution of DPC practices were confirmed, but data about quality are lacking.
Gavirneni, Srinagesh, Andrew, Manikas, Vidyadhar, Kulkarni, and Alexis, Karageorge. Concierge Medicine:
Adoption, Design, and Management. Presented at the 2013 Winder Simulation Conference, 2013,
Washington, DC, 2340–2349.
Abstract: Concierge Medicine is a relatively new development in the U.S. Health care system and is
designed and implemented, mostly by primary care physicians, to provide comprehensive care in a
timely manner. Physicians often struggle with the decisions associated with adoption (implement
or not), design (pricing and membership), and management (day-to-day execution) of these
systems. The patients also struggle with decisions associated with signing up (or not) as it is
predicated on the performance measures of complex service systems. We develop a simulation
model that could be used by both the physicians and the patients to help them with these decisions.
We demonstrate the effectiveness of this tool using data from a primary care physician in the
Louisville, KY area.
Conclusion: Concierge medicine is an attractive prospect for a traditional practice physician because
having fewer patients allows them to spend more time with each patient. The annual retainer fee
supplements the office visit charges so the doctor does not have adverse financial outcomes from
moving to a smaller panel size. For patients, having the doctor spend an hour with them rather than
ten minutes, is very appealing. In addition, they also experience a reduction in waiting times they
experience. Patients that value their time highly will benefit from the concierge practice, and thus,
be willing to pay the retainer. In this study, we did not include different acuity rates. Patients with
less severe issues may more than likely not sign up for concierge medicine implying that the average
demand per patient may go up under concierge medicine. Future research should account for the
additional complexity. Concierge medicine is attractive to both patients and physicians and could
lead to better health outcomes for the entire society. However, for that to happen, these practices
should be implemented under the right circumstances, should be designed appropriately for the
customer base, and managed effectively. This can only be done with a strong analytical foundation
for answering these questions and we believe that this paper is a first step in that direction.
Shrank, William. 2017. Primary Care Practice Transformation and the Rise of Consumerism. Journal of
General Internal Medicine 32, no. 4:387–397.
Concierge and Direct Care: Some primary care physicians are meeting patient demand for
convenience and greater attention by contracting directly with patients, either via “concierge care,”
where the patient pays a retainer fee that provides for highly personalized, round-the-clock access,
but where the physician still bills the patient’s insurance for services, or “direct care,” where the
patient pays out-of-pocket for all services, bypassing insurance altogether. Concierge practices

85
Copyright © 2020 Society of Actuaries
typically charge $1,500 or more a year, with elite practices charging as much as $25,000 annually.
A 2013 survey found that approximately 6% of physicians were in concierge or cash-only practices,
with surprisingly low levels of attrition during the economic recession. Advocates of direct care
believe that such arrangements improve quality, as they remove insurers from the authorization
process and offer physicians ample time to meet the needs of willing patients.
However, this model seems to run counter to the overall mission of payment and delivery reform.
Such exclusive practices would be expected to further reduce the already limited supply of primary
care physicians that do take health insurance, potentially limiting access to primary care for those
without the means to contract directly. Moreover, this model may be expected to exacerbate
disparities in care, as the most vulnerable will be most likely to face access issues. The result could
be a tiered system of primary care, where those physicians who do not contract directly with
patients would care for a sicker and more vulnerable population, further challenging their mission
to manage the health of the populations they serve. Nevertheless, the popularity of concierge care
and direct primary care suggests that patients with the financial wherewithal are willing to pay for
access to high-quality primary care; these trends underscore patients’ interest in a more meaningful
relationship with their primary care physician. And from the perspective of the primary care
physician, there is a clear desire to get out from under the yoke of insurance paperwork,
documentation requirements, and time pressure. Absent issues of physician supply and equity,
these models are attractive to many patients and physicians alike, and have implications for the
future design (“reinvention”) of primary care.

86
Copyright © 2020 Society of Actuaries
Appendix B: Full Market Survey Results
1. Which of the following best describes your current DPC practice?
Response
Count
Percentage*
Pure DPC: Charge a periodic fee and do not bill any third parties on a fee-for-service basis.
Any per visit charge must be less than the monthly equivalent of the periodic fee. All
membership fees are paid by patient or employer
164
85%
Hybrid: My practice still incorporates some portion of fee-for-service billing to a third-party
payer – typically a separate panel.
27
14%
Other: “Pure DPC except the per visit charge is more than the periodic fee.”
1
1%
Other: “Time based billing”
1
1%
Other: “Employer-sponsored DPC and cash only fee for service hybrid. No insurance
billing.”
1
1%
Total Respondents
194
100%
*Percentages may not add up to 100% due to rounding
2. What is your gender?
Response
Count
Percentage*
Male
46
58%
Female
33
42%
Total Respondents
79
100%
*Percentages may not add up to 100% due to rounding
3. What year did you finish your medical residency?
Statistical Measures
Results
Average response
2002
25th percentile of responses
1997
50th percentile of responses (median)
2002
75th percentile of responses
2009
Total Respondents
80
4. What is your medical designation?
Response
Count
Percentage*
MD
68
83%
DO
13
16%
MBBS
1
1%
Total Respondents
82
100%
*Percentages may not add up to 100% due to rounding
5. Are you opted out of Medicare?
Response
Count
Percentage*
Yes
105
75%
In process of opting out
7
5%
Do not plan to opt out
28
20%
Total Respondents
140
100%
*Percentages may not add up to 100% due to rounding
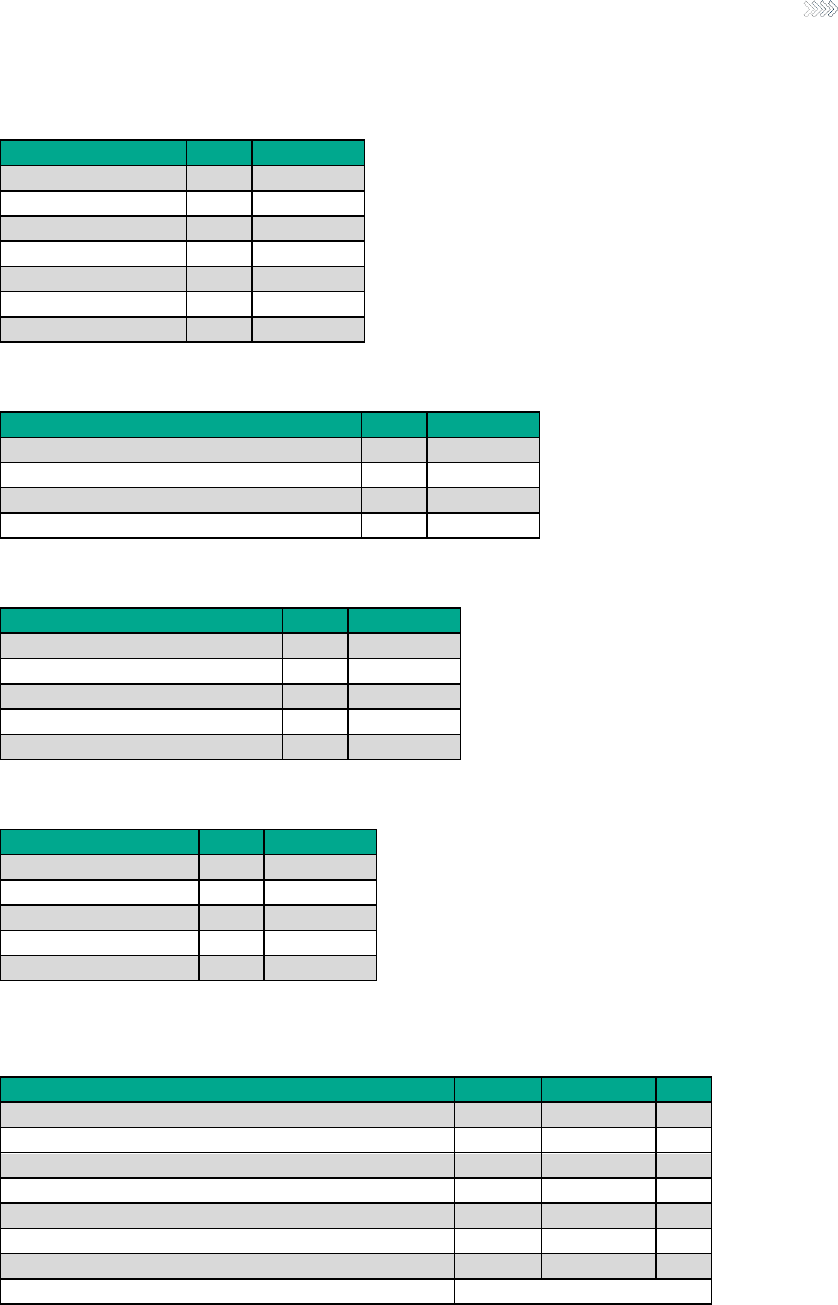
87
Copyright © 2020 Society of Actuaries
6. What is your primary medical specialty?
Response
Count
Percentage*
Family Medicine
135
74%
Internal Medicine
21
11%
Pediatrics
8
4%
Obstetrics/Gynecology
3
2%
Emergency Medicine
5
3%
Other
11
6%
Total Respondents
183
100%
*Percentages may not add up to 100% due to rounding
7. What was your role in the opening of your DPC practice?
Response
Count
Percentage*
Worked independently
144
74%
Worked with other physicians
41
21%
Had no role/employed by existing DPC practice
9
5%
Total Respondents
194
100%
*Percentages may not add up to 100% due to rounding
8. Which best describes your role in your DPC practice?
Response
Count
Percentage*
Sole owner
112
76%
Partial owner/shareholder
24
16%
Not an owner (i.e., 100% employed)
9
6%
Not in clinical practice
2
1%
Total Respondents
147
100%
*Percentages may not add up to 100% due to rounding
9. What year did your practice open?
Response
Count
Percentage*
Between 2000 and 2005
10
6%
Between 2006 and 2010
6
3%
Between 2011 and 2015
34
19%
Between 2016 and 2020
125
71%
Total Respondents
175
100%
*Percentages may not add up to 100% due to rounding
10. How did each of the following factors contribute to you choosing to operate a DPC practice?
RESPONDENT COUNTS
Response
Not at all
A little/some
A lot
Too much FFS paperwork to complete
8
31
138
Potential to earn more under DPC
98
61
18
Too large of a FFS panel size
29
59
88
Too little time for FFS visits
7
20
151
Contracting complexities with insurance companies
16
38
124
Potential to provide better primary care under a DPC model
1
5
171
DPC entrepreneurial spirit
16
68
93
Total Respondents
178
RESPONDENT PERCENTAGES

88
Copyright © 2020 Society of Actuaries
Response
Not at all
A little/some
A lot
Too much FFS paperwork to complete
4%
17%
78%
Potential to earn more under DPC
55%
34%
10%
Too large of a FFS panel size
16%
33%
49%
Too little time for FFS visits
4%
11%
85%
Contracting complexities with insurance companies
9%
21%
70%
Potential to provide better primary care under a DPC model
1%
3%
96%
DPC entrepreneurial spirit
9%
38%
52%
Total Respondents
100%
11. Which best describes your average monthly membership fees as of December 1, 2018?
RESPONDENT COUNTS
Member Category
Below
$20
$21–
$49
$50–
$75
$76–
$100
$101–
$150
$151–
$175
$176–
$200
Over
$200
Total
Respondents
Children
47
83
20
15
2
1
0
0
168
Adults ages 19–25
3
44
88
28
5
5
0
0
173
Adults ages 26–50
0
12
104
43
7
2
3
1
172
Adults ages 51–65
0
7
85
61
12
4
1
3
173
Adults ages 66+
0
9
51
78
22
3
2
3
168
Families
0
2
7
13
43
20
31
20
136
RESPONDENT PERCENTAGES
Member Category
Below
$20
$21–
$49
$50–
$75
$76–
$100
$101–
$150
$151–
$175
$176–
$200
Over
$200
Total
Respondents
Children
28%
49%
12%
9%
1%
1%
0%
0%
100%
Adults ages 19–24
2%
25%
51%
16%
3%
3%
0%
0%
100%
Adults ages 25–50
0%
7%
60%
25%
4%
1%
2%
1%
100%
Adults ages 51–64
0%
4%
49%
35%
7%
2%
1%
2%
100%
Adults ages 65+
0%
5%
30%
46%
13%
2%
1%
2%
100%
Families
0%
1%
5%
10%
32%
15%
23%
15%
100%
APPROXIMATE AVERAGES (ROUNDED TO NEAREST $5)
Member Category
Approximate
Average Fee
Children
$40
Adults ages 19–24
$65
Adults ages 25–50
$75
Adults ages 51–64
$80
Adults ages 65+
$85
Families
$150
12. Do you charge a per-visit fee (i.e., member cost sharing beyond membership fee)?
Response
Count
Percentage*
Yes
19
11%
No
155
89%
Total Respondents
174
100%
*Percentages may not add up to 100% due to rounding

89
Copyright © 2020 Society of Actuaries
13. Do you charge a member enrollment fee?
Response
Count
Percentage*
Yes
94
54%
No
81
46%
Total Respondents
175
100%
*Percentages may not add up to 100% due to rounding
14. Do you have an annual limit as to the number of visits covered by the DPC membership fee?
Response
Count
Percentage*
Yes
26
15%
No
149
85%
Total Respondents
175
100%
*Percentages may not add up to 100% due to rounding
15. Do you dispense prescription drugs in your DPC practice?
Response
Count
Percentage*
Yes
98
57%
No – My state does not allow me to do so
19
11%
No – I choose not to
54
32%
Total Respondents
171
100%
*Percentages may not add up to 100% due to rounding
16. Approximately what percent have your DPC membership fees increased per year over the last 3 years?
Response
Count
Percentage*
Fees have decreased
4
2%
No increases
106
62%
1% to 5% per year
28
16%
6% to 10% per year
13
8%
Over 10% per year
4
2%
Do not know
16
9%
Total Respondents
171
100%
*Percentages may not add up to 100% due to rounding
17. What percent do you expect your DPC membership fees to increase next year?
Response
Count
Percentage*
Fees have decreased
1
1%
No increases
111
65%
1% to 5% per year
32
19%
6% to 10% per year
6
4%
Over 10% per year
5
3%
Do not know
15
9%
Total Respondents
170
100%
*Percentages may not add up to 100% due to rounding

90
Copyright © 2020 Society of Actuaries
18. What percent of your DPC members terminate their membership after one year?
Response
Count
Percentage*
None
8
5%
1–5% per year
90
53%
6–10% per year
28
16%
Over 10% per year
15
9%
Do not know
30
18%
Total Respondents
171
100%
*Percentages may not add up to 100% due to rounding
19. How many patients are currently in your patient panel (i.e., current patients receiving or paying for a DPC
membership)?
Statistical Measures
Results
Average response
445
25th percentile of responses
200
50th percentile of responses (median)
359
75th percentile of responses
600
Total Respondents
164
20. What is your target patient panel (i.e., how many patients would you like to have that are receiving or
paying for a DPC membership)?
Statistical Measures
Results
Average response
628
25th percentile of responses
450
50th percentile of responses (median)
600
75th percentile of responses
700
Total Respondents
157
RATIO OF RESPONDENTS ACTUAL DPC PANEL SIZE TO TARGET DPC PANEL SIZE
Statistical Measures
Results
Average response
75%
25th percentile of responses
46%
50th percentile of responses (median)
75%
75th percentile of responses
100%
Total Respondents
156
21. If your DPC patient panel is full, how many months did it take to fill your panel?
Statistical Measures
Results
Average response
21
25th percentile of responses
10
50th percentile of responses (median)
18
75th percentile of responses
24
Total Respondents
53

91
Copyright © 2020 Society of Actuaries
22. What is the percent of the patients in your panel covered by each of the following as their primary
insurance?
Statistical Measures
Medicare
Medicaid
Private
coverage
No
coverage
Other
coverage
Do not
know
Average response
15%
5%
43%
27%
7%
3%
25th percentile of responses
5%
0%
33%
9%
0%
0
50th percentile of responses
(median)
10%
5%
5%
2%
0%
0
75th percentile of responses
25%
5%
60%
33%
9%
0
Total Respondents
136
23. How many full time equivalent staff members do you have in your practice?
Statistical Measures
Physicians
Non-Physician
Clinicians
Average response
1.5
.6
25
th
percentile of responses
1
0
50
th
percentile of responses (median)
1
0
75
th
percentile of responses
2
1
Total Respondents
162
131
*Excludes outlier responses
24. Which of the following procedures or services do you provide in your DPC practice?
RESPONDENT COUNTS
Procedure / Service
Yes
(part of DPC
membership
Yes
(additional
charge)
Not
available
Total
Respondents
Same day appointments
162
1
0
163
Phone/text consults
162
0
1
163
Telemedicine
144
0
19
163
EKG
143
9
11
163
Urgent care/walk-in appointments
137
3
23
163
Nutritional counseling
136
7
20
163
Weight management
134
10
19
163
Wellness coaching
128
8
27
163
Biopsy and excisions
114
42
7
163
Cryosurgery
106
20
36
162
Joint injections
94
42
27
163
House calls/home visits
94
37
31
162
Spirometry
90
7
64
161
Functional/integrative medicine
57
7
99
163
Endometrial sampling
49
21
92
162
Sending off pathology specimens
48
107
7
162
Department of Transportation (DOT) physicals
48
22
93
163
Basic laboratory testing (e g , HgbA1C, lipids,
CMP, TSH, PSA, PAP, CBC, U/A)
34
113
16
163
Tympanometry
25
4
133
162
Ultrasound imaging (non-OB)
25
17
120
162
Addiction medicine
25
19
119
163
Children and adolescent immunizations
23
56
81
160
Colposcopy
19
10
134
163
Adult immunizations
19
86
58
163
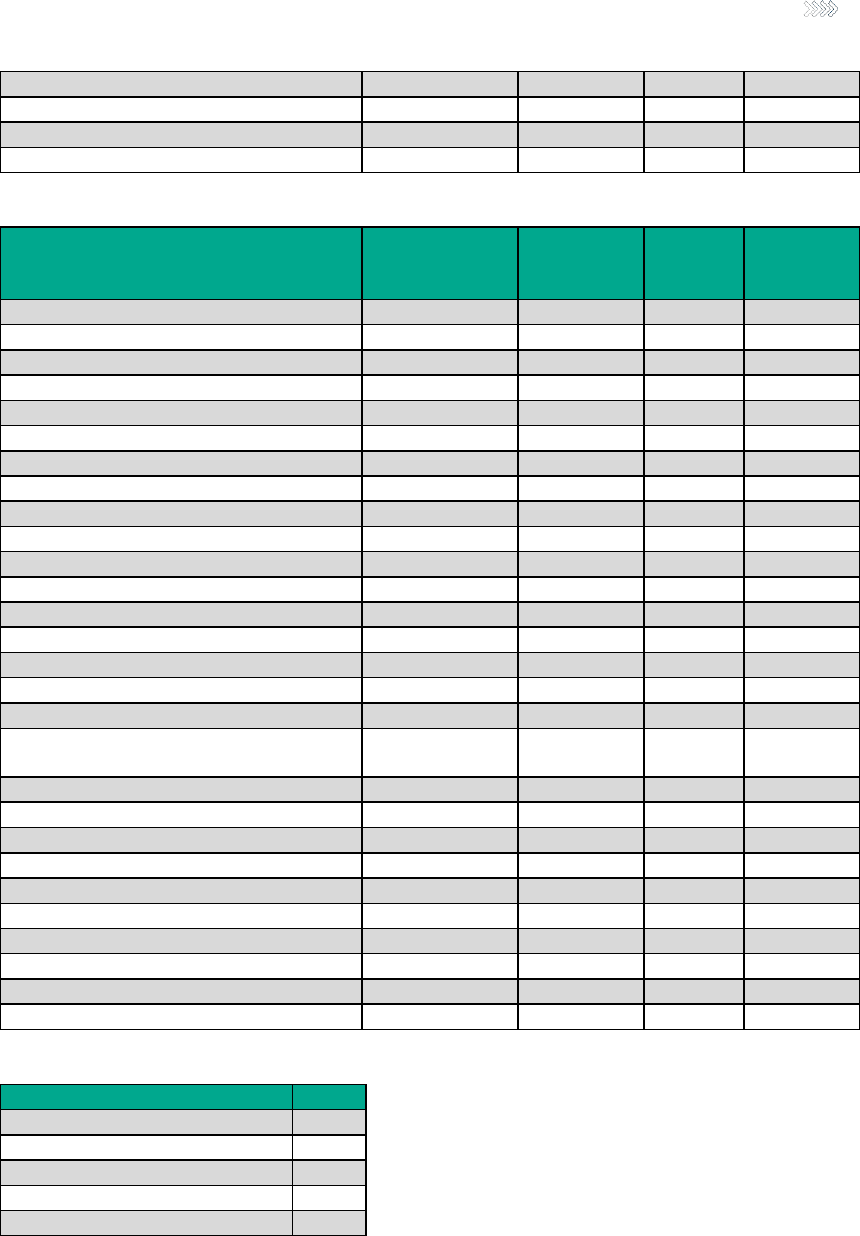
92
Copyright © 2020 Society of Actuaries
X-ray
9
33
120
162
Obstetrical services
9
5
149
163
Vasectomy
4
15
142
161
Flexible sigmoidoscopy exam
1
4
156
161
RESPONDENT PERCENTAGES
Procedure / Service
Yes
(part of DPC
membership
Yes
(additional
charge)
Not
available
Total
Respondents
Same day appointments
99%
1%
0%
100%
Phone/text consults
99%
0%
1%
100%
Telemedicine
88%
0%
12%
100%
EKG
88%
6%
7%
100%
Urgent care/walk-in appointments
84%
2%
14%
100%
Nutritional counseling
83%
4%
12%
100%
Weight management
82%
6%
12%
100%
Wellness coaching
79%
5%
17%
100%
Biopsy and excisions
70%
26%
4%
100%
Cryosurgery
65%
12%
22%
100%
Joint injections
58%
26%
17%
100%
House calls/home visits
58%
23%
19%
100%
Spirometry
56%
4%
40%
100%
Functional/integrative medicine
35%
4%
61%
100%
Endometrial sampling
30%
13%
57%
100%
Sending off pathology specimens
30%
66%
4%
100%
Department of Transportation (DOT) physicals
29%
13%
57%
100%
Basic laboratory testing (e g , HgbA1C, lipids,
CMP, TSH, PSA, PAP, CBC, U/A)
21%
69%
10%
100%
Tympanometry
15%
2%
82%
100%
Ultrasound imaging (non-OB)
15%
10%
74%
100%
Addiction medicine
15%
12%
73%
100%
Children and adolescent immunizations
14%
35%
51%
100%
Colposcopy
12%
6%
82%
100%
Adult immunizations
12%
53%
36%
100%
X-ray
6%
20%
74%
100%
Obstetrical services
6%
3%
91%
100%
Vasectomy
2%
9%
88%
100%
Flexible sigmoidoscopy exam
1%
2%
97%
100%
25. During a typical patient visit, what percentage of time is DPC care provided directly by you, the physician?
Statistical Measures
Results
Average response
90%
25
th
percentile of responses
90%
50
th
percentile of responses (median)
95%
75
th
percentile of responses
100%
Total Respondents
128

93
Copyright © 2020 Society of Actuaries
26. What is your average wait time (in days) for a DPC member to schedule an appointment?
Statistical Measures
Results
Average response
1
25th percentile of responses
0
50th percentile of responses (median)
1
75th percentile of responses
1
Total Respondents
152
27. What is your average wait time (in minutes) for a DPC member in the office for an appointment to begin?
Statistical Measures
Results
Average response
4
25th percentile of responses
0
50th percentile of responses (median)
3
75th percentile of responses
5
Total Respondents
148
*Outlier responses of 240, 120, 120 and 60 were excluded.
28. What is your average time (in minutes) spent with DPC members in the exam room?
Statistical Measures
Results
Average response
38
25th percentile of responses
30
50th percentile of responses (median)
30
75th percentile of responses
45
Total Respondents
145
29. Do DPC members have access to their electronic health records through a patient portal?
Response
Count
Percentage*
Yes
89
58%
No
64
42%
Total Respondents
153
100%
*Percentages may not add up to 100% due to rounding
30. Can DPC members/patients sign up and manage their enrollment (i.e., add family members, disenroll, pay
membership fees) using your practice’s website?
Response
Count
Percentage*
Yes
89
58%
No
64
42%
Total Respondents
153
100%
*Percentages may not add up to 100% due to rounding
31. Does your practice advertise DPC membership fees and other fee-related information on your practice’s
website?
Response
Count
Percentage*
Yes
138
90%
No
15
10%
Total Respondents
153
100%
*Percentages may not add up to 100% due to rounding

94
Copyright © 2020 Society of Actuaries
32. Does your practice you participate (signed, formal agreement) in any employer-based contracts for DPC
services provided by your practice to their employees?
Response
Count
Percentage*
Yes
102
67%
No
50
33%
Total Respondents
152
100%
*Percentages may not add up to 100% due to rounding
33. What percentage of your DPC panel are from employer-based contracts?
Statistical Measures
Results
Average response
25%
25th percentile of responses
5%
50th percentile of responses (median)
15%
75th percentile of responses
35%
Total Respondents
101
34. Which of the following best represents what is included in your employer-based contracts?
Response
Count
Percentage*
All of our DPC contracts include the same bundle of covered services
79
78%
We customize the services being covered based on the employer
22
22%
Total Respondents
101
100%
*Percentages may not add up to 100% due to rounding
35. Do your employer-based contracts require you to submit claims to their TPA for reporting purposes?
Response
Count
Percentage*
Yes – All contracts
12
12%
Yes – Some contracts
20
20%
No
70
69%
Total Respondents
102
100%
*Percentages may not add up to 100% due to rounding
36. How do you expect the DPC model of primary care to impact utilization rates compared to FFS primary care
for the following types of service?
RESPONDENT COUNTS
Types of Service
Reduce
Utilization
No Impact
On Utilization
Increase
Utilization
Total
Respondents
Primary Physician Care
32
16
100
148
Preventative Care
9
10
128
147
Specialty Physician Care
134
12
2
148
Hospitalization
138
8
2
148
Emergency Care
140
7
1
148
Urgent Care
140
6
2
148
Prescription Drug Usage
90
46
11
147
RESPONDENT PERCENTAGES
Types of Service
Reduce
Utilization
No Impact
On Utilization
Increase
Utilization
Total
Respondents
Primary Physician Care
22%
11%
68%
100%
Preventative Care
6%
7%
87%
100%
Specialty Physician Care
91%
8%
1%
100%

95
Copyright © 2020 Society of Actuaries
Hospitalization
93%
5%
1%
100%
Emergency Care
95%
5%
1%
100%
Urgent Care
95%
4%
1%
100%
Prescription Drug Usage
61%
31%
7%
100%
37. Compared to FFS patients, what is DPC patients’ level of satisfaction with their primary care experience?
Response
Count
Percentage*
Less satisfied
1
1%
Equally satisfied
2
1%
More satisfied
145
98%
Total Respondents
148
100%
*Percentages may not add up to 100% due to rounding
38. Compared to FFS patients, what is DPC patients’ level of reliance on their primary care provider to navigate
through the health system for nonprimary care services?
Response
Count
Percentage*
Rely less
0
0%
Rely the same amount
28
19%
Rely more
120
81%
Total Respondents
148
100%
*Percentages may not add up to 100% due to rounding
39. Compared to FFS patients, what is DPC patients’ level of out-of-pocket spending for primary care services
including DPC monthly fee?
Response
Count
Percentage*
Spend less
119
81%
Spend about the same amount
16
11%
Spend more
12
8%
Total Respondents
147
100%
*Percentages may not add up to 100% due to rounding
40. Compared to FFS patients, what is DPC patients’ level compliance with preventive care guidelines?
Response
Count
Percentage*
Comply less often
2
1%
Comply about the same
46
31%
Comply more often
100
68%
Total Respondents
148
100%
*Percentages may not add up to 100% due to rounding
41. Compared to FFS patients, what is DPC patients' level of chronic conditions?
Response
Count
Percentage*
About the same number of chronic conditions
90
61%
Less chronic conditions
17
12%
More chronic conditions
40
27%
Total Respondents
147
100%
*Percentages may not add up to 100% due to rounding

96
Copyright © 2020 Society of Actuaries
42. Compared to FFS patients, what is DPC patients’ level of referrals to specialists?
Response
Count
Percentage*
Referred less often
127
86%
Referred about the same
20
14%
Referred more often
1
1%
Total Respondents
148
100%
*Percentages may not add up to 100% due to rounding
43. How would you rate the impact of being a DPC physician on the following factors?
RESPONDENT COUNTS
Factors
Much
Worse
Worse
Neutral
Better
Much
Better
Total
Respondents
My overall (personal and professional) satisfaction
0
0
2
19
125
146
My ability to practice medicine
0
0
3
7
137
147
Quality of my primary care provided to patients
0
0
2
5
140
147
Length of time I expect to practice primary care
1
0
11
11
123
146
My earnings as a primary care physician
7
36
54
22
28
147
The number of hours that I spend in the office
0
2
38
35
72
147
The amount of time that I spend doing paperwork
1
5
11
24
106
147
My relationship with my primary care patients
0
0
4
8
135
147
RESPONDENT PERCENTAGES
Factors
Much
Worse
Worse
Neutral
Better
Much
Better
Total
Respondents
My overall (personal and professional) satisfaction
0%
0%
1%
13%
86%
100%
My ability to practice medicine
0%
0%
2%
5%
93%
100%
Quality of my primary care provided to patients
0%
0%
1%
3%
95%
100%
Length of time I expect to practice primary care
1%
0%
8%
8%
84%
100%
My earnings as a primary care physician
5%
24%
37%
15%
19%
100%
The number of hours that I spend in the office
0%
1%
26%
24%
49%
100%
The amount of time that I spend doing paperwork
1%
3%
7%
16%
72%
100%
My relationship with my primary care patients
0%
0%
3%
5%
92%
100%

97
Copyright © 2020 Society of Actuaries
Appendix C: Additional Development Detail for Milliman Advanced Risk Adjusters
(MARA)
MARA v3 was developed using a commercial population of 7 million members. Member records include person-
specific claim and enrollment data for inpatient, outpatient and prescription drug services. The data set is longitudinal,
meaning that enrollees can be linked across years. Each year of data is compiled from approximately 100 payers in
the private health sector and contains over 500 million unique claims.
The starting points for MARA’s risk assessment methodology are the Milliman Clinical Classifications (MCCs), which
offer a clinically transparent method to organize data. MCCs are a result of more than 20 years of research and
development. Created by an interdisciplinary team of physicians, actuaries and statisticians, the MCCs are the
foundation for a number of widely distributed Milliman products, including the Health Cost Guidelines, which were
also utilized in our case study. MCCs exhaustively map all diagnosis codes from the International Classification of
Diseases (ICD9 and ICD10) and certain procedure codes (Current Procedural Terminology/CPT) into a manageable
number of clinically meaningful categories to improve risk assessment and risk-based analytics. The MCCs number
greater than 1,200, offering transparency for describing the clinical risk drivers for each individual processed.
Additional proprietary logic in the model also considers several other inputs in the model design, including timing of
diagnosis codes, service types, and CPT/HCPCS procedure codes. Comprehensive models use both medical
information and drug data as prediction variables.
With regard to the concurrent model, which was used for our case study, a concurrent risk adjustment model
quantifies a member’s severity of illness and the expected cost during the 12-month assessment period based upon
member demographics and data from medical and pharmacy claims. This model recognizes the relative morbidity
associated with acute conditions or injuries. The observed costs during the assessment period can then be adjusted
by the member’s attributed risk for that period.
Following best practices, MARA model performance is measured on validation populations rather than the samples
on which the models were calibrated; this helps ensure that the results are real and are not overfit to random
occurrences in the calibration population. Several modeling approaches are utilized in the model development,
ranging from the multiple linear to nonlinear regressions. These advancements include the use of prevalence
refinement and severity refinement models. Both types of refinement models are combined to produce an overall
refined prediction of the contribution of a particular condition to the projection period costs.
Separate models, one for each of the six health service categories, enhance performance. The benefit of having risk
scores by health service category is that there is more insight into the intensity of resource use at the population level.
The dependent variable in each of the service category models represents only the claim costs associated with that
particular service category. The independent predictor variables are the same for all six models. The six category level
risk scores are normalized such that they add up to an average total cost risk score of 1.00 on the MARA development
data set.

98
Copyright © 2020 Society of Actuaries
About the Society of Actuaries
The Society of Actuaries (SOA), formed in 1949, is one of the largest actuarial professional organizations in the world
dedicated to serving more than 31,000 actuarial members and the public in the United States, Canada and
worldwide. In line with the SOA Vision Statement, actuaries act as business leaders who develop and use
mathematical models to measure and manage risk in support of financial security for individuals, organizations and
the public.
The SOA supports actuaries and advances knowledge through research and education. As part of its work, the SOA
seeks to inform public policy development and public understanding through research. The SOA aspires to be a
trusted source of objective, data-driven research and analysis with an actuarial perspective for its members,
industry, policymakers and the public. This distinct perspective comes from the SOA as an association of actuaries,
who have a rigorous formal education and direct experience as practitioners as they perform applied research. The
SOA also welcomes the opportunity to partner with other organizations in our work where appropriate.
The SOA has a history of working with public policymakers and regulators in developing historical experience studies
and projection techniques as well as individual reports on health care, retirement and other topics. The SOA’s
research is intended to aid the work of policymakers and regulators and follow certain core principles:
Objectivity: The SOA’s research informs and provides analysis that can be relied upon by other individuals or
organizations involved in public policy discussions. The SOA does not take advocacy positions or lobby specific policy
proposals.
Quality: The SOA aspires to the highest ethical and quality standards in all of its research and analysis. Our research
process is overseen by experienced actuaries and nonactuaries from a range of industry sectors and organizations. A
rigorous peer-review process ensures the quality and integrity of our work.
Relevance: The SOA provides timely research on public policy issues. Our research advances actuarial knowledge
while providing critical insights on key policy issues, and thereby provides value to stakeholders and decision
makers.
Quantification: The SOA leverages the diverse skill sets of actuaries to provide research and findings that are driven
by the best available data and methods. Actuaries use detailed modeling to analyze financial risk and provide
distinct insight and quantification. Further, actuarial standards require transparency and the disclosure of the
assumptions and analytic approach underlying the work.
Society of Actuaries
475 N. Martingale Road, Suite 600
Schaumburg, Illinois 60173
www.SOA.org
