
’
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’s
’sGuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
sGuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
P
LANNER’S GUID
E
Programs Work
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
Making
Health
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
Communication
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
U.S. DEPARTMENT OF HEALTH & HUMAN SERVICES
G
APuide
National Institutes of Health
G
uideAPlanner’sGuideAPlan
’sGuideAPlanner’sGuide
National Cancer Institute
G
uideAPlanner’sGuideAPlanner
G
uideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
Making
Health
Communication
Programs Work
U.S. DEPARTMENT OF HEALTH & HUMAN SERVICES
Public Health Service • National Institutes of Health
National Cancer Institute

Guide PlannersGuide PlannersGuide PlannersGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
Preface
T
his book is a revision of the original Making Health
Communication Programs Work, first printed in 1989, which
the Office of Cancer Communications (OCC, now the Office
of Communications) of the National Cancer Institute (NCI)
developed to guide communication program planning. During the 25
years that NCI has been involved in health communication, ongoing
evaluation of our communication programs has affirmed the value of
using specific communication strategies to promote health and prevent
disease. Research and practice continue to expand our understanding
of the principles, theories, and techniques that provide a sound
foundation for successful health communication programs. The purpose
of this revision is to update communication planning guidelines to
account for the advances in knowledge and technology that have
occurred during the past decade.
To prepare this update, NCI solicited ideas and information from
various health communication program planners and experts (see
Acknowledgments). Their contributions ranged from reviewing and
commenting on existing text to providing real-life examples to illustrate
key concepts. In addition, the Centers for Disease Control and
Prevention (CDC) provided extensive input as part of the agency’s
partnership with NCI.
Although communicating effectively about health is an exacting task,
those who have the earlier version of this publication know that it is
possible. We hope the ideas and information in this revision will help
new health communication programs start soundly and mature
programs work even better.

Acknowledgments
Many health communication experts contributed to the revision of this book.
For their invaluable input, we would like to thank:
Elaine Bratic Arkin
Health Communications Consultant
Cynthia Bauer, Ph.D.
U.S. Department of Health and
Human Services
John Burklow
Office of Communication and Public Liaison
National Institutes of Health
Lynne Doner
Health Communications Consultant
Timothy Edgar, Ph.D.
Westat
Brian R. Flay
University of Illinois at Chicago
Vicki S. Freimuth, Ph.D.
Office of Communication
Centers for Disease Control and Prevention
Joanne Gallivan, M.S., R.D.
National Institute of Diabetes and Digestive
and Kidney Diseases
Karen Glanz, Ph.D., M.P.H.
Cancer Research Center of Hawaii
Bernard Glassman, M.A.T.
Special Expert in Informatics
National Cancer Institute
Susan Hager
Hager Sharp
Jane Lewis, Dr.P.H.
UMDNJ, School of Public Health
Terry Long
National Heart, Lung, and Blood Institute

Kathleen Loughrey, M.S., R.D. Health Communications Consultant
Susan K. Maloney, M.H.S. Health Communications Consultant
Joy R. Mara, M.A.
Joy R. Mara Communications
John McGrath
National Institute of Child Health and
Human Development
Diane Miller, M.P.A.
National Institute on Alcohol Abuse and
Alcoholism
Ken Rabin, Ph.D.
Ruder Finn Healthcare, Inc.
Scott C. Ratzan, M.D., M.P.A.
Journal of Health Communication
U.S. Agency for International Development
Barbara K. Rimer, Dr.P.H.
Division of Cancer Control and
Population Sciences
National Cancer Institute
Victor J. Strecher, Ph.D., M.P.H.
University of Michigan
Tim L. Tinker, Dr.P.H., M.P.H.
Widmeyer Communications
We would especially like to thank Elaine Bratic Arkin, author of the original book, whose knowledge of
health communication program planning made this revision possible, as well as Lynne Doner, whose
broad-based consumer research and evaluation expertise has enhanced the book’s content and quality.
Both have provided hours of review and consultation, and we are grateful to them for their contributions.
Thanks to the staff of the Office of Communications, particularly Nelvis Castro, Ellen Eisner, and Anne
Lubenow. And thanks to Christine Theisen, who coordinated the revisions to the original text.
This document was revised in coordination with the Centers for Disease Control and Prevention during
development of CDCynergy—a program-planning tool on CD-ROM.

Table of Contents
Why Should You Use This Book?
i
Introduction
1
The Role of Health Communication in Disease Prevention and Control
2
What Health Communication Can and Cannot Do
3
Planning Frameworks, Theories, and Models of Change
7
How Market Research and Evaluation Fit Into Communication Programs
8
Selected Readings
9
Overview: The Health Communication Process
11
The Stages of the Health Communication Process
11
Stage 1: Planning and Strategy Development
15
Why Planning Is Important
16
Planning Steps
16
Common Myths and Misconceptions About Planning
48
Selected Readings
50
Stage 2: Developing and Pretesting Concepts,
53
Messages, and Materials
Why Developing and Pretesting Messages and Materials Are Important
54
Steps in Developing and Pretesting Messages and Materials
54
Planning for Production, Distribution, Promotion, and Process Evaluation
86
Common Myths and Misconceptions About Materials Pretesting
86
Selected Readings
87
Stage 3: Implementing the Program
91
Preparing to Implement Your Program
92
Maintaining Media Relations After Launch
95
Working With the Media During a Crisis Situation
98
Managing Implementation: Monitoring and Problem Solving
98
Maintaining Partnerships
102
Common Myths and Misconceptions About Program Implementation
103
Selected Readings
104

Stage 4: Assessing Effectiveness and
107
Making Refinements
Why Outcome Evaluation Is Important
108
Revising the Outcome Evaluation Plan
108
Conducting Outcome Evaluation
110
Refining Your Health Communication Program
121
Common Myths and Misconceptions About Evaluation
121
Selected Readings
123
Communication Research Methods
125
Types of Communication Research
126
Differences Between Qualitative and Quantitative Research Methods
126
Qualitative Research Methods
127
Quasi-Quantitative Research Methods: Pretesting Messages and Materials
141
Quantitative Research Methods
157
Additional Research Methods
161
Appendix A: Communication Planning
169
Forms and Samples
Appendix B: Selected Planning Frameworks, Social
217
Science Theories, and Models of Change
Appendix C: Information Sources
229
Appendix D: Selected Readings and Resources
235
Appendix E: Glossary
245

Guide PlannersGuide PlannersGuide PlannersGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Why Should You Use This Book?
T
he planning steps in this book can help make any
communication program work, regardless of size, topic,
geographic span, intended audience, or budget. (intended
audience is the term this book uses to convey what other
publications may refer to as a target audience.) The key is reading all
the steps and adapting those relevant to your program at a level of
effort appropriate to the program’s scope. The tips and sidebars
throughout the book suggest ways to tailor the process to your
various communication needs.
If you have limited funding, you might
• Work with partners who can add their resources to your own
• Conduct activities on a smaller scale
• Use volunteer assistance
• Seek out existing information and approaches developed by
programs that have addressed similar issues to reduce
developmental costs
Don’t let budget constraints keep you from setting objectives, learning
about your intended audience, or pretesting. Neglecting any of these
steps could limit your program’s effectiveness before it starts.
This book describes a practical approach for planning and
implementing health communication efforts; it offers guidelines, not
hard and fast rules.Your situation may not permit or require each step
outlined in the following chapters, but we hope you will consider each
guideline and decide carefully whether it applies to your situation.
To request additional copies of this book, please visit NCI’s Web site
at
www.cancer.gov or call NCI’s Cancer Information Service at
1-800-4-CANCER (1-800-422-6237).

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
INTRODUCTION
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

INTRO
Introduction
In This Section:
• The role of health communication in disease prevention and control
• What health communication can and cannot do
• Planning frameworks, theories, and models of change
• How research and evaluation fit into communication programs
Questions to Ask and Answer:
• Can communication help us achieve all or some of our aims?
• How can health communication fit into our program?
• What theories, models, and practices should we use to plan
our communication program?
• What types of evaluation should we include?

The Role of Health Communication in
Disease Prevention and Control
There are numerous definitions of health
communication. The National Cancer
Institute and the Centers for Disease Control
and Prevention use the following:
The study and use of communication
strategies to inform and influence
individual and community decisions
that enhance health.
Use the principles of effective health
communication to plan and create initiatives
at all levels, from one brochure or Web site
to a complete communication campaign.
Successful health communication programs
involve more than the production of
messages and materials. They use
research-based strategies to shape the
products and determine the channels that
deliver them to the right intended audiences.
Since this book first appeared in 1989,
the discipline of health communication has
grown and matured. As research has
continued to validate and define the
effectiveness of health communication, this
book has become a widely accepted tool
for promoting public health. Healthy People
2010, the U.S. Department of Health and
Human Services’ stated health objectives for
the nation, contains separate objectives for
health communication for the first time.
Meanwhile, the availability of new
technologies is expanding access to
health information and raising questions
about equality of access, accuracy of
information, and how to use the new tools
most effectively.
2

INTRO
What Health Communication Can
and Cannot Do
Understanding what health communication
can and cannot do is critical to
communicating successfully. Health
communication is one tool for promoting or
improving health. Changes in health care
services, technology, regulations, and policy
are often also necessary to completely
address a health problem.
Communication alone can:
• Increase the intended audience’s
knowledge and awareness of a health
issue, problem, or solution
• Influence perceptions, beliefs, and
attitudes that may change social norms
• Prompt action
• Demonstrate or illustrate healthy skills
• Reinforce knowledge, attitudes,
or behavior
• Show the benefit of behavior change
• Advocate a position on a health issue
or policy
• Increase demand or support for
health services
• Refute myths and misconceptions
• Strengthen organizational relationships
Communication combined with other
strategies can:
• Cause sustained change in which an
individual adopts and maintains a new
health behavior or an organization adopts
and maintains a new policy direction
• Overcome barriers/systemic problems,
such as insufficient access to care
Communication cannot:
• Compensate for inadequate health care or
access to health care services
• Produce sustained change in complex
health behaviors without the support of a
larger program for change, including
components addressing health care
services, technology, and changes in
regulations and policy
• Be equally effective in addressing all
issues or relaying all messages because
the topic or suggested behavior change
may be complex, because the intended
audience may have preconceptions about
the topic or message sender, or because
the topic may be controversial
Communication Can Affect Multiple
Types of Change
Health communication programs can
affect change among individuals and also
in organizations, communities, and society
as a whole:
• Individuals—The interpersonal level is the
most fundamental level of health-related
communication because individual
behavior affects health status.
Communication can affect individuals’
awareness, knowledge, attitudes, self-
efficacy, skills, and commitment to
behavior change. Activities directed at
other intended audiences for change may
also affect individual change, such as
involving patients in their own care.
• Groups—The informal groups to which
people belong and the community settings
they frequent can have a significant
impact on their health. Examples include
relationships between customers and
employees at a salon or restaurant,
exercisers who go to the same gym,
students and parents in a school setting,
employees at a worksite, and patients and
health professionals at a clinic. Activities
aimed at this level can take advantage of
these informal settings.
Making Health Communication Programs Work
3

• Organizations—Organizations are groups
with defined structures, such as
associations, clubs, or civic groups. This
category can also include businesses,
government agencies, and health insurers.
Organizations can carry health messages
to their constituents, provide support for
health communication programs, and
make policy changes that encourage
individual change.
• Communities—Community opinion
leaders and policymakers can be effective
allies in influencing change in policies,
products, and services that can hinder or
support people’s actions. By influencing
communities, health communication
programs can promote increased
awareness of an issue, changes in
attitudes and beliefs, and group or
institutional support for desirable
behaviors. In addition, communication
can advocate policy or structural changes
in the community (e.g., sidewalks) that
encourage healthy behavior.
• Society—Society as a whole influences
individual behavior by affecting norms and
values, attitudes and opinions, laws and
policies, and by creating physical,
economic, cultural, and information
environments. Health communication
programs aimed at the societal level can
change individual attitudes or behavior
and thus change social norms. Efforts
to reduce drunk driving, for example,
have changed individual and societal
attitudes, behaviors, and policies through
multiple forms of intervention,
including communication.
Multistrategy health communication
programs can address one or all of
the above.
Communication Programs Can Include
Multiple Methods of Influence
Health communicators can use a wide range
of methods to design programs to
fit specific circumstances. These
methods include:
• Media literacy—teaches intended
audiences (often youth) to deconstruct
media messages so they can identify the
sponsor’s motives; also teaches
communicators how to compose
messages attuned to the intended
audience’s point of view
• Media advocacy—seeks to change the
social and political environment in which
decisions that affect health and health
resources are made by influencing the
mass media’s selection of topics and by
shaping the debate about those topics
• Public relations—promotes the inclusion
of messages about a health issue or
behavior in the mass media
• Advertising—places paid or public service
messages in the media or in public spaces
to increase awareness of and support for
a product, service, or behavior
• Education entertainment—seeks to
embed health-promoting messages and
storylines into entertainment and news
programs or to eliminate messages that
counter health messages; can also include
seeking entertainment industry support for
a health issue
• Individual and group instruction—
influences, counsels, and provides skills to
support desirable behaviors
• Partnership development—increases
support for a program or issue by
harnessing the influence, credibility, and
resources of profit, nonprofit, or
governmental organizations
4
Introduction
INTRO
CHARACTERISTICS OF EFFECTIVE HEALTH COMMUNICATION CAMPAIGNS
Certain attributes can make health communication campaigns more effective.
Use the guidelines in this section to plan your campaign.
Define the communication campaign goal effectively:
• Identify the larger goal
• Determine which part of the larger goal could be met by a communication campaign
• Describe the specific objectives of the campaign; integrate these into a campaign plan
Define the intended audience effectively:
• Identify the group to whom you want to communicate your message
• Consider identifying subgroups to whom you could tailor your message
• Learn as much as possible about the intended audience; add information about beliefs,
current actions, and social and physical environment to demographic information
Create messages effectively:
• Brainstorm messages that fit with the communication campaign goal and the
intended audience(s)
• Identify channels and sources that are considered credible and influential by the
intended audience(s)
• Consider the best times to reach the audience(s) and prepare messages accordingly
• Select a few messages and plan to pretest them
Pretest and revise messages and materials effectively:
• Select pretesting methods that fit the campaign’s budget and timeline
• Pretest messages and materials with people who share the attributes of the
intended audience(s)
• Take the time to revise messages and materials based upon pretesting findings
Implement the campaign effectively:
• Follow the plans you developed at the beginning of the campaign
• Communicate with partners and the media as necessary to ensure the campaign
runs smoothly
• Begin evaluating the campaign plan and processes as soon as the campaign
is implemented
Note. Adapted from the University of Kansas Community Toolbox, Community
Workstation, available at
http://ctb.lsi.ukans.edu/tools/CWS/socialmarketing/outline.htm.
Accessed March 7, 2002.
Making Health Communication Programs Work
5

THEORIES GUIDE ACTION TO INCREASE MAMMOGRAPHY USE
Fox Chase Cancer Center, in cooperation with area managed care organizations, designed
a program that was based on key elements of the health belief model to encourage women
to have regular mammograms. Selected women received educational materials explaining
that virtually all women are at risk for breast cancer, regardless of the absence of
symptoms, and that risk increases with age (susceptibility). The materials stressed that
early detection brings not only the best chance of cure but also the widest range of
treatment choices (benefit). Women received a letter stating their physician’s support (cue
to action) and a coupon for a free mammogram (to overcome the cost barrier). Those who
did not have a mammogram within 90 days received different forms of reminders (cues to
action). In the most intensive reminder, a telephone counselor called selected women to
review their perceptions about susceptibility, benefits, and barriers. Program evaluation
showed that mammography use increased substantially.
The Fox Chase program also applied social learning theory in developing interventions to
encourage physician support of mammography and to improve clinical breast
examinations (CBEs). The planners examined the environmental and situational factors
that might affect physician behavior and tried to change the low expectations of
physicians about the benefits of breast screening. The interventions included
observational learning by watching an expert perform a CBE, an opportunity to increase
self-efficacy by practicing CBE with the instructor, and the use of a feedback report and
CME credits to reinforce physician skills.
In taking a community approach to change, a UCLA mammography program used a
diffusion of innovations model. Community analysis showed that women who were early
adopters (leaders) already had a heightened awareness of the value of mammography. To
reach middle adopters, the program mobilized the social influence of the early adopters by
using volunteers who had breast cancer to provide mammography information. The
program also provided highly individualized educational strategies linked to social
interaction approaches to reach late adopters. A social marketing framework influenced
the program’s planning approach, and media materials incorporated the health belief
model to promote individual behavior change.
Note. From “Audiences and Messages for Breast and Cervical Cancer Screenings,” by B. K. Rimer,
1995, Wellness Perspectives: Research, Theory, and Practice, 11(2), pp. 13–39. Copyright by University
of Alabama. Adapted with permission.
6
Introduction

INTRO
Communication programs can take
advantage of the strengths of each of the
above by using multiple methods. A program
to decrease tobacco use among youth, for
example, could include:
• Paid advertising to ensure that youth are
exposed to on-target, unfiltered
motivational messages
• Media advocacy to support regulatory or
policy changes to limit access to tobacco
• Public relations to support
anti-tobacco attitudes
• Media literacy instruction in schools
to reduce the influence of the
tobacco industry
• Entertainment education and advocacy
to decrease the depiction of tobacco use
in movies
• Partnerships with commercial enterprises
(such as retail chains popular
among youth) to spread the
anti-smoking message
Using multiple methods increases the need
for careful planning and program
management to ensure that all efforts are
integrated and consistently support program
goals and objectives.
Planning Frameworks, Theories,
and Models of Change
Sound health communication development
should draw upon theories and models that
offer different perspectives on the intended
audiences and on the steps that can
influence their change. No single theory
dominates health communication because
health problems, populations, cultures, and
contexts vary. Many programs achieve the
greatest impact by combining theories to
address a problem. The approach to health
communication we use in this book is based
on the social marketing framework.
(See Appendix B for an overview of some
other relevant theoretical models.) Social
marketing concentrates on tailoring
programs to serve a defined group and is
most successful when it is implemented as
NATIONAL OBJECTIVES FOR RESEARCH
AND
EVALUATION
The Health Communication chapter of
Healthy People 2010, the nationwide
health promotion and disease
prevention agenda, identifies increasing
the proportion of health
communication activities that include
research and evaluation as one of six
objectives for the field for the next
decade (objective 11-3). This objective
focuses attention on the need to make
research and evaluation integral parts of
initial program design. Research and
evaluation are used to systematically
obtain the information needed to
refine the design, development,
implementation, adoption, redesign,
and overall quality of a
communication intervention.
Making Health Communication Programs Work
7

a systematic, continuous process that is
driven at every step by decision-based
research, which is used as feedback to
adjust the program.*
Why Use Theories and Models?
Although theories cannot substitute for
effective planning and research, they offer
many benefits for the design of health
communication programs. At each stage of
the process outlined in this book, theories
and models can help answer key questions,
such as:
• Why a problem exists
• Whom to select
• What you need to know about the
population/intended audience before
taking action
• How to reach people and make an impact
• Which strategies are most likely to
cause change
Reviewing theories and models can suggest
factors to consider as you formulate your
objectives and approach, and can help you
determine whether specific ideas are likely
to work. Theories and models can guide
message and materials development, and
are also useful when you decide what to
evaluate and how to design evaluation tools.
How Market Research and Evaluation
Fit Into Communication Programs
Conducting market research is vital to
identifying and understanding intended
audiences and developing messages and
strategies that will motivate action.
Evaluations conducted before, throughout,
and after implementation provide data on
which to base conclusions about success or
failure and help to improve current and
future communication programs.
Evaluation should be built in from the start,
not tacked on to the end of a program.
Integrating evaluation throughout planning
and implementation ensures that you:
• Tailor messages, materials, and activities
to your intended audience
• Include evaluation mechanisms (e.g.,
include feedback forms with a
community guide)
• Define appropriate, meaningful,
achievable, and time-specific
program objectives
Evaluating your program’s communication
efforts enables you to:
• Understand what is and is not working,
and why
• Improve the effort while it is under way
and improve future efforts
• Demonstrate the value of the program to
interested parties such as partners,
funding agencies, and the public
• Help program staff see how its work
affects the intended audiences
In this book, we address appropriate
evaluation activities for each stage; see the
Communication Research Methods section
for a description of the different types of
research and evaluation that support each
stage of the health communication
process. See Appendix A for sample
forms and instruments.
* From Theory at a Glance: A Guide for Health Promotion
Practice (NIH Publication No. 97-3896), by the National
Cancer Institute, 1995. Bethesda, MD. In the
public domain.
8
Introduction

INTRO
Selected Readings
Andreasen, A. (1995). Marketing social
change: Changing behavior to promote
health, social development, and the
environment. San Francisco: Jossey-Bass.
Backer, T. E., Rogers, E. M., & Sopory, P.
(1992). Designing health communication
campaigns: What works. Thousand Oaks,
CA: Sage.
Bandura, A. (1986). Social foundations of
thought and action: A social cognitive theory.
Englewood Cliffs, NJ: Prentice-Hall.
Centers for Disease Control and Prevention.
(2001). CDCynergy 2001 [CD-ROM]. Atlanta.
Glanz, K., Lewis, F. M., & Rimer, B. K.
(Eds.). (1997). Health behavior and health
education: Theory, research, and practice
(2nd ed.). San Francisco: Jossey-Bass.
Glanz, K., & Rimer, B. K. (1995). Theory at a
glance: A guide for health promotion
practice (NIH Publication No. 97-3896).
Bethesda, MD: National Cancer Institute.
Goldberg, M. E., Fishbein, M. F., &
Middlestadt, S. E. (Eds.). (1997). Social
marketing: Theoretical and practical
perspectives. Mahwah, NJ: Erlbaum.
Green, L. W., & Kreuter, M. W. (1999). Health
promotion planning: An educational and
ecological approach (3rd ed.). Mountain
View, CA: Mayfield.
Maibach, E., & Parrott, R. L. (Eds.). (1995).
Designing health messages: Approaches
from communication theory and public
health practice. Thousand Oaks, CA: Sage.
National Cancer Institute. (1993). A picture
of health (NIH Publication No. 94-3604).
Rockville, MD: U.S. Department of Health
and Human Services.
Rimer, B. K. (1995). Audiences and
messages for breast and cervical cancer
screenings. Wellness Perspectives:
Research, Theory, and Practice, 11(2),
13–39.
Siegel, M., & Doner, L. (1998). Marketing
public health: Strategies to promote social
change. Gaithersburg, MD: Aspen.
U.S. Department of Health and Human
Services. (2000). Healthy people 2010 (2nd
Ed.; in two volumes: Understanding and
improving health and Objectives for
improving health.). Washington, DC: U.S.
Government Printing Office.
Making Health Communication Programs Work
9

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
OVERVIEW
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

OVERVIEW
Overview: The Health
Communication Process
In This Section:
• How the approach used in this book will help your organization produce
and implement a health communication program
• Each stage in the health communication process
The Stages of the Health Communication Process
For a communication program to be successful, it must be based on an
understanding of the needs and perceptions of the intended audience. In
this book, we incorporate tips on how to learn about the intended audience’s
needs and perceptions in each of the program stages. Remember, these
needs and perceptions may change as the project progresses, so be
prepared to make changes to the communication program as you proceed.
To help with planning and developing a health communication program, we
have divided the process into four stages: Planning and Strategy
Development; Developing and Pretesting Concepts, Messages, and
Materials; Implementing the Program; and Assessing Effectiveness and
Making Refinements. The stages constitute a circular process in which the
last stage feeds back into the first as you work through a continuous loop of
planning, implementation, and improvement.
1
2
3
4
Health
Communication
Program
Cycle
Planning and
Strategy
Development
Developing
and Pretesting
Concepts,
Messages,
and Materials
Implementing
the Program
Assessing
Effectiveness
and Making
Refinements

Use this book to produce and implement a
plan for a communication program. The final
plan will include the following components:
• General description of the program,
including intended audiences, goals,
and objectives
• Market research plans
• Message and materials development and
pretesting plans
• Materials production, distribution, and
promotion plans
• Partnership plans
• Process evaluation plan
• Outcome evaluation plan
• Task and time table
• Budget
Because this process is not linear, do not
expect to complete a stage and then move
to the next, never to go back.You will be
exploring opportunities, researching issues,
and refining plans and approaches as your
organization implements the program. This
ongoing, iterative process characterizes a
successful communication program.
To help work through program planning and
development, we suggest many steps within
each stage.You may not find all of the steps
suggested in each stage feasible for your
program, or even necessary. As you plan,
carefully examine available resources and
what you want to accomplish with the
program and then apply the steps that are
appropriate for you. However, if you carefully
follow the steps described in each stage of
the process, your work in the next phase
may be more productive.
Each of the four stages is described here;
they are described in more detail in the
subsequent sections of this book.
Stage 1: Planning and Strategy
Development
In this book, all planning is discussed within
the Planning and Strategy Development
section, but the concepts you learn there
apply across the life cycle of a
communication program. During Stage 1
you create the plan that will provide the
foundation for your program. By the end of
Stage 1, you will have:
• Identified how your organization can use
communication effectively to address a
health problem
• Identified intended audiences
• Used consumer research to craft a
communication strategy and objectives
• Drafted communication plans, including
activities, partnerships, and baseline
surveys for outcome evaluation
Planning is crucial for the success of any
health communication program, and doing
careful work now will help you avoid having
to make expensive alterations when the
program is under way.
Stage 2: Developing and Pretesting
Concepts, Messages, and Materials
In Stage 2, you will develop message
concepts and explore them with the
intended audience using qualitative
research methods. By the end of Stage 2,
you will have:
• Developed relevant, meaningful messages
• Planned activities and drafted materials
• Pretested the messages and materials
with intended-audience members
12
Overview

OVERVIEW
Getting feedback from intended audiences
when developing messages and materials is
crucial for the success of every
communication program. Learning now what
messages are effective with the intended
audiences will help you avoid producing
ineffective materials.
Stage 3: Implementing the Program
In Stage 3, you will introduce the fully
developed program to the intended
audience. By the end of Stage 3, you
will have:
• Begun program implementation,
maintaining promotion, distribution, and
other activities through all channels
• Tracked intended-audience exposure and
reaction to the program and determined
whether adjustments were needed
(process evaluation)
• Periodically reviewed all program
components and made revisions
when necessary
Completing process evaluations and making
adjustments are integral to implementing the
program and will ensure that program
resources are always being used effectively.
Stage 4: Assessing Effectiveness and
Making Refinements
In Stage 4, you will assess the program
using the outcome evaluation methods you
planned in Stage 1. By the end of Stage 4,
you will have:
• Assessed your health
communication program
• Identified refinements that would
increase the effectiveness of future
program iterations
Because program planning is a recurring
process, you will likely conduct planning,
management, and evaluation activities
described in Stages 1–4 throughout the
life of the program.
Making Health Communication Programs Work
13

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
STAGE 1
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Planning and
Strategy Development
In This Section:
• Why planning is important
• Six steps of the planning process
• Assessing health issues and identifying solutions
• Defining communication objectives
• Defining intended audiences
• Exploring communication settings, channels, and activities
• Identifying potential partners and collaborating
• Developing a communication strategy and drafting communication
and evaluation plans
• Common myths about planning
Questions to Ask and Answer:
• What health problem are we addressing?
• What is occurring versus what should be occurring?
• Whom does the problem affect, and how?
• What role can communication play in addressing the problem?
• How and by whom is the problem being addressed? Are other
communication programs being planned or implemented?
(Look outside of your own organization.)
• What approach or combination of approaches can best influence the
problem? (Communication? Changes in policies, products, or services?
All of these?)
• What other organizations have similar goals and might be willing to
work on this problem?
• What measurable, reasonable objectives will we use to define success?
• What types of partnerships would help achieve the objectives?
• Who are our intended audiences? How will we learn about them?
• What actions should we encourage our intended audiences to take?
• What settings, channels, and activities are most appropriate for reaching
our intended audiences and the goals of our communication objectives?
(Interpersonal, organizational, mass, or computer-related media?
Community? A combination?)
• How can the channels be used most effectively?
• How will we measure progress? What baseline information will we use to
conduct our outcome evaluation?
STAGE 1

Why Planning Is Important
The planning you do now will provide the
foundation for your entire health
communication program. It will enable your
program to produce meaningful results
instead of just boxes of materials. Effective
planning will help you:
• Understand the health issue you
are addressing
• Determine appropriate roles for
health communication
• Identify the approaches necessary to bring
about or support the desired changes
• Establish a logical program
development process
• Create a communication program that
supports clearly defined objectives
• Set priorities
• Assign responsibilities
• Assess progress
• Avert disasters
Under the pressure of deadlines and
demands, it is normal to think, “I don’t have
time to plan; I have to get started NOW.”
However, following a strategic planning
process will save you time. Because you will
define program objectives and then tailor
your program’s activities to meet those
objectives, planning will ensure that you
don’t spend time doing unnecessary work.
Program objectives are generally broader
than communication objectives, described
in step 2 on page 20, and specify the
outcomes that you expect your entire
program to achieve. Many of the planning
activities suggested in this chapter can be
completed simultaneously. Even if your
program is part of a broader health
promotion effort that has an overall plan, a
plan specific to the communication
component is necessary.
Planning Steps
This chapter is intended to help you design
a program plan. The health communication
planning process includes the following six
steps explained in this chapter:
1. Assess the health issue or problem and
identify all the components of a possible
solution (e.g., communication as well as
changes in policy, products, or services).
2. Define communication objectives.
3. Define and learn about
intended audiences.
4. Explore settings, channels, and activities
best suited to reach intended audiences.
5. Identify potential partners and develop
partnering plans.
6. Develop a communication strategy for
each intended audience; draft a
communication plan.
To complete this process, use the
Communication Program Plan template in
Appendix A to help ensure that you don’t
miss any key points.
1. Assess the Health Issue/Problem and
Identify All Components of a Solution
The more you understand about an issue or
health problem, the better you can plan a
communication program that will address it
successfully. The purpose of this initial data
collection is to describe the health problem
or issue, who is affected, and what is
occurring versus what should be occurring.
Doing this will allow you to consider how
communication might help address the
issue or problem. In this step, review and
gather data both on the problem and on
what is being done about it.
16
Planning and Strategy Development

Review Available Data
• Community service agencies (for related
To collect available data, first check for
sources of information in your agency or
organization. Identify gaps and then seek
outside sources of information. Sources and
availability of information will vary by issue.
The types of information you should (ideally)
have at this stage include descriptions of:
• The problem or issue
• The incidence or prevalence of the
health problem
• Who is affected (the potential intended
audience), including age, sex, ethnicity,
economic situation, educational or reading
level, place of work and residence, and
causative or preventive behaviors. Be sure
to include more information than just
basic demographics
• The effects of the health problem on
individuals and communities (state,
workplace, region, etc.)
• Possible causes and preventive measures
• Possible solutions, treatments,
or remedies
To find this information, search these
common data sources:
• Libraries (for journal articles and texts)
• Health-related resources on the Internet
• Sources of health statistics (a local
hospital, a state health department, the
National Center for Health Statistics on the
CDC Web site)
• Administrative databases covering
relevant populations
• Government agencies, universities,
and voluntary and health
professional organizations
• Clearinghouses
service-use data)
• Corporations, trade associations,
and foundations
• Polling companies (for intended audience
knowledge and attitudes)
• Depositories of polling information (e.g.,
the Roper Center)
• Chambers of commerce
• Advertising agencies, newspapers,
and radio and television stations
(for media-use data, buying and
consumption patterns)
Both published and unpublished reports
may be available from these sources. A
number of federal health information
clearinghouses and Web sites also provide
information, products, materials, and
sources of further assistance for specific
health subjects. A helpful first step in
planning may be to contact the appropriate
Web sites and the health department to
obtain information on the health issue your
program is addressing. See Appendix C,
Information Sources, for listings of
additional sources of information, including
Internet resources.
Identify Existing Activities and Gaps
Find out what other organizations are doing
to address the problem, through
communication and other approaches,
such as advocating for policy or
technological changes. Contact these
organizations to discuss:
• What they have learned
• What information or advice they may have
to help you plan
• What else is needed (what gaps exist in
types of change needed, media or
activities available, intended audiences
STAGE 1
Making Health Communication Programs Work
17

served to date, messages and materials
directed at different stages of intended
audience behavior change)
• Opportunities for cooperative ventures
Gather New Data as Needed
You may find that the data you have
gathered does not give enough insight into
the health problem, its resolution, or
knowledge about those who are affected in
order to proceed. In other instances, you
may have enough information to define the
problem, know who is affected, and identify
the steps that can resolve it, but other
important information about the affected
populations may be unavailable or outdated.
To conduct primary research to gather more
information, see the Communication
Research Methods section.
Sometimes it is impossible to find sufficient
information about the problem. This may be
because the health problem has not yet
been well defined. In this case, you might
decide that a communication program is an
inappropriate response to that particular
problem until more becomes known.
Identify All Components of a Solution
Adequately addressing a health problem
often requires a combination of the
following approaches:
• Communication (to the general public,
patients, health care providers,
policymakers—whoever needs to make or
facilitate a change)
• Policy change (e.g., new laws, regulations,
or operating procedures)
• Technological change (e.g., a new or
redesigned product, drug, service, or
treatment; or changing delivery of existing
products, drugs, services, or treatments)
Yet all too often we rely on health
communication alone and set unrealistic
expectations for what it can accomplish. It is
vitally important to identify all of the
components necessary to bring about the
desired change and then to carefully
consider which of these components is
being—or can be—addressed. For example,
consider a woman who needs a
mammogram. The mammogram graphic
shows some of the problems that may
Communication Strategy
A Case Study: Mammogram
Solution: Requires
Communication
Strategy
Communication
to Doctors
Persuade doctors to
give mammogram
referrals to all women
in the appropriate
age group
Communication
to Women
Present the benefits
(that women think are
important) of getting a
mammogram that will
outweigh her fears
My doctor
doesn’t
recommend a
mammogram.
I don’t think
I need it. I’m
afraid of getting a
mammogram.
Solution: Requires
Change in Policy
and Resources
My health
insurance
doesn’t cover
mammograms.
I can’t travel
40 miles to get a
mammogram and
I can’t miss
work.
Policy
Mandate coverage of
mammograms in
accordance with
screening guidelines
Technology
Outfit a van with
mammography
equipment and send
to her neighborhood
during nonworking
hours
18
Planning and Strategy Development

USING COMMUNICATION TO SUPPORT POLICY CHANGE
The goal of a communication campaign is not always to teach or to influence behavior; it
can also begin the process of changing a policy to increase health and wellness. This
might mean getting community leaders excited about a new “rails to trails” project or
working to bring up the issue of a lack of low-income housing. In each case, the final goal
(i.e., helping people exercise by increasing the number of walking/biking trails, making
sure that everyone in the community has a safe place to live by assigning more
apartments in newly built housing to low-income residents) is more than a
communication campaign can accomplish. However, the initial goal (gaining the support
of decision-makers who can change current policy) can be met.
One of the most popular and effective ways to build support for policy change is to work
with the media. Use the following questions to help plan your message:
• What is the problem you are highlighting?
• Is there a solution to it? If so, what is it?
• Whose support do you need to gain to make the solution possible?
• What do you need to do or say to get the attention of those who can make the
solution happen?
Once you have developed your message, create a media list that includes organizations,
such as newspapers and television stations; individuals, such as reporters, editors, and
producers; and other contacts. Keep this list updated as you communicate your message
and work to change policy. The following are a few methods to use:
• News releases
• Interviews
• Letters to the editor
• Media conferences
Media strategies are not the only way to build support for policy change. Also consider
attending and speaking at local meetings, approaching issue decision-makers either in
person or by letter, or working with and educating community members who are affected.
STAGE 1
Note. From American Public Health Association. APHA Media Advocacy Manual 2000.
Washington, DC. Adapted with permission.
Making Health Communication Programs Work
19

occur and potential solutions for each.
Solutions that communication programs
can help develop are highlighted.
Determine Whether Health Communication
Is Appropriate for the Problem and
Your Organization
Create a map that diagrams the
components of a problem and the steps
necessary to solve it (as in the mammogram
graphic) to help you determine a possible
role for health communication. In some
cases, health communication alone may
accomplish little or nothing without policy,
technological, or infrastructure changes
(e.g., successfully increasing physical
activity of employees in the workplace might
require employer policy changes to allow for
longer breaks or infrastructure changes
such as new walking paths). In some
instances, effective solutions may not yet
exist for a communication program to
support. For example, no treatment may
exist for an illness, or a solution may require
services that are not yet available. In these
cases, decide either to wait until other
program elements are in place or to
develop communication strategies directed
to policymakers instead of consumers
or patients.
If you determine that health communication
is appropriate, ask the following questions to
consider whether your organization is best
suited to carry it out:
• Does the organization have (or can it
acquire) the necessary expertise
and resources?
• Does the organization have the necessary
authority or mandate?
• Will the organization be duplicating efforts
of others?
• How much time does the organization
have to address this issue?
• What, if anything, can be accomplished
in that time?
2. Define Communication Objectives
Defining communication objectives will help
you set priorities among possible
communication activities and determine the
message and content you will use for each.
Once you have defined and circulated the
communication objectives, they serve as
a kind of contract or agreement about the
purpose of your communication, and
they establish what outcomes should
be measured.
It is important to create achievable
objectives. Many communication efforts are
said to fail only because the original
objectives were wildly unreasonable. For
example, it is generally impossible to
achieve a change of 100 percent. If you plan
to specify a numerical goal for a particular
objective, an epidemiologist or statistician
can help you determine recent rates of
change related to the issue so that you have
some guidance for deciding how much
change you think your program can achieve.
(Remember that commercial marketers
often consider a 2 to 3 percent increase in
sales to be a great success.) Fear of failure
should not keep you from setting
measurable objectives. Without them, there
is no way to show your program has
succeeded or is even making progress
along the way, which could reduce support
for the program among your supervisors,
funding agencies, and partners.
Because objectives articulate what the
communication effort is intended to do,
they should be:
• Supportive of the health program’s goals
• Reasonable and realistic (achievable)
• Specific to the change desired, the
population to be affected, and the time
20
Planning and Strategy Development

HOW COMMUNICATION CONTRIBUTES TO COMPLEX BEHAVIOR CHANGE
One can imagine how the process of change occurs: A woman sees some public service
announcements (PSAs) and a local TV health reporter’s feature telling her about the
“symptomless disease”—hypertension. She checks her blood pressure in a newly accessible
shopping mall machine, and the results suggest a problem. She tells her spouse, who has
also seen the ads, and he encourages her to have it checked. She goes to a physician who
confirms the presence of hypertension and encourages her to change her diet and return
for monitoring.
The physician has become more sensitive to the issue because of a recent article in the
Journal of the American Medical Association, some recommendations from a specialist
society, and a conversation with a drug retailer as well as informal conversations with
colleagues and exposure to television discussion of the issue.
Meanwhile, the patient talks with friends at work or family members about her
experience. They also become concerned and go to have their own pressure checked. She
returns for another checkup and her pressure is still elevated although she has reduced her
salt intake. The physician decides to treat her with medication. The patient is ready to
comply because all the sources around her—personal, professional, and media—are telling
her that she should.
This program is effective not because of a PSA or a specific program of physician
education. It is successful because the National High Blood Pressure Education Program
has changed the professional and public environment as a whole around the issue
of hypertension.
Note. From “Public Health Education and Communication as Policy Instruments for Bringing About
Changes in Behavior,” by R. Hornik. In Social Marketing: Theoretical and Practical Perspectives (pp.
49–50), by M. E. Goldberg, M. Fishbein, and S. E. Middlestadt (Eds.), 1997, Mahwah, NJ: Lawrence
Erlbaum Associates. Adapted with permission.
period during which change should
(you’ll design strategies and tactics for
take place
getting there later). Develop reasonable
• Measurable, to allow you to track progress
communication objectives by looking at the
toward desired results
health program’s goal and asking, “What
can communication feasibly contribute to
• Prioritized, to direct the allocation
attaining this goal, given what we know
of resources
about the type of changes the intended
audiences can and will make?”
Be Reasonable
Communication efforts alone cannot achieve
Objectives describe the intermediate steps
all objectives. Appropriate purposes for
that must be taken to accomplish broader
communication include:
goals; they describe the desired outcome,
but not the steps involved in attaining it
STAGE 1
Making Health Communication Programs Work
21

• Creating a supportive environment for a
change (societal or organizational) by
influencing attitudes, beliefs, or policies
• Contributing to a broader behavior
change initiative by offering messages
that motivate, persuade, or enable
behavior change within a specific
intended audience
Raising awareness or increasing knowledge
among individuals or the organizations that
reach them is also feasible; however, do not
assume that accomplishing such an
objective will lead to behavior change. For
example, it is unreasonable to expect
communication to cause a sustained
change of complex behaviors or
compensate for a lack of health care
services, products, or resources.
The ability and willingness of the intended
audience to make certain changes also
affect the reasonableness of various
communication objectives. Keep this in mind
as you define the intended audiences in
planning step 2.Your objectives will be
reasonable for a particular intended
audience only if audience members both
can make a particular behavior change and
are willing to do so.
Be Realistic
Once your program has developed
reasonable communication objectives,
determine which of them are realistic, given
your available resources, by answering
these questions:
• Which objectives cover the areas that
most need to reach the program goal?
• What communication activities will
contribute the most to addressing
these needs?
PLANNING TERMS
Goal
The overall health improvement that an
organization or agency strives to create
(e.g., more eligible cancer patients will
take part in cancer clinical trials, or
more Americans will avoid fatal heart
attacks). A communication program
should be designed to support and
contribute to achieving this specific
desired improvement.
Communication Objectives
The specific communication outcomes
you aim to produce in support of the
overall goal (e.g., by 2005, 75 percent of
Americans will know that participating
in cancer research studies may be an
option for them; or by 2005, 50 percent
of rural adults over age 40 will know the
warning signs for a heart attack and
what to do if they occur). Objectives
should be attainable, measurable, and
time specific.
Strategy
The overall approaches the program
takes. Strategies derive from and
contribute to achieving defined goals
and objectives. They should be based on
knowledge about effective
communication, the intended
audience’s needs and characteristics,
and your program’s capabilities,
timelines, and resources. (See planning
step 6 for more information on
developing a communication strategy
and evaluation plan.)
22
Planning and Strategy Development

• What resources are available? Include:
— Staff and other human resources—
committee members, associates from
other programs, volunteers, and others
who have the requisite skills and time
— Overhead resources such as computer
time, mailing costs, and printing
— Services available from another source,
such as educational materials available
free or at cost and the effort by other
organizations willing to help
— Information about the issue, the
intended audience, the community, and
media structures, or about available
educational materials
— Budget available to fund the program
— Time (weeks, months, or years
available to complete the program)
• What supportive factors exist (e.g.,
community activities, other organizations’
interests, positive community attitudes)?
• What barriers exist (e.g., obstacles to
approval, absence of funding, sensitivity of
an issue, intended audience constraints)?
• Which objectives would best use the
resources your program has identified and
best fit within the identified constraints?
Your answers to the last question should
become your priority objectives. Sometimes
you may feel so constrained by a lack of
funds that proceeding appears impossible.
An honest assessment may lead you to
conclude that a productive communication
effort is not possible. However, creative
use of the resources already identified
may enable you to develop a communication
program that can make valuable
contributions.
3. Define and Learn About
Intended Audiences
In this step, determine whom you want to
reach based on decisions made in the
previous two steps.
Begin by identifying intended populations for
a program based on the epidemiology of the
problem (who is most affected? at risk?) and
other factors contributing to the problem.
Intended populations are often defined very
broadly, using just a few descriptors (e.g.,
women over age 50). Intended audiences
are carved from these broad population
groups and defined more narrowly based on
characteristics such as attitudes,
demographics, geographic region, or
patterns of behavior. Examples might
include physically inactive adolescents,
heavy smokers with low education and
income levels who are fatalistic about health
issues, or urban African-American men with
hypertension who live in the South. Because
the intended audience’s ability and
willingness to make a behavior change
affects the extent to which communication
objectives are reasonable and realistic, it is
most efficient to select intended audiences
and develop communication objectives
(planning steps 2 and 3) in tandem.
STAGE 1
SAMPLE COMMUNICATION OBJECTIVES
By 2005, the number of women (over age 50; Washington, DC, residents; income under
$45,000) who say they get annual screening mammograms will have increased by 25 percent.
By the end of our campaign, more than 50 percent of students at South Salem High School
will report having increased the number of servings of fruits and vegetables they eat (on
most days) by one.
Making Health Communication Programs Work
23

GOALS AND OBJECTIVES:
H
EALTHY PEOPLE 2010
Healthy People 2010, the Nation’s
prevention agenda for the next decade,
is designed to achieve two overarching
goals: 1) increase the quality and years
of healthy life, and 2) eliminate health
disparities. For the first time, the Health
Communication chapter of Healthy
People 2010 includes objectives to
improve the quality of health
communication interventions, the skills
of health professionals, the reach and
quality of interactive communication
media, and the health literacy of people
with inadequate or marginal literacy
skills. Meeting these communication
objectives will contribute to the
achievement of the overarching goals.
Some communication efforts that could
contribute to the achievement of these
goals include the following:
• Interventions to improve the
communication skills of health care
providers and patients
• Assistance for people searching for and
using health information
• Education for consumers and patients
about important health topics and
relevant risks, preventive measures,
and ways to access the health
care system
See www.health.gov/healthypeople
to learn more.
Note. U.S. Department of Health and Human
Services. (2000). Healthy People 2010 (2nd
ed.; in two volumes: Understanding and
Improving Health and Objectives for Improving
Health). Washington, DC: U.S. Government
Printing Office. In the public domain.
Move From Intended Population to Specific
Intended Audiences
Defining subgroups of a population
according to common characteristics is
called segmentation. Segmentation can help
you develop messages, materials, and
activities that are relevant to the intended
audience’s current behavior and specific
needs, preferences, beliefs, cultural
attitudes, knowledge, and reading habits. It
also helps you identify the best channels for
reaching each group, because populations
also differ in factors such as access to
information, the information sources they
find reliable, and how they prefer to learn.
Increase your program’s effectiveness by
developing strategies that are attuned to the
needs and wants of different intended
audience segments. In fact, given the
diversity of the general public, trying to
reach everyone with one message or
strategy may result in an approach that does
not effectively reach those most able or
ready to change. Be aware, though, that
moving from a mass-market strategy to a
differentiated strategy will add economic and
staff resource costs for each additional
segment. Segment a population into specific
intended audiences using the following
characteristics to define them:
• Behavioral—health-related activities or
choices, degree of readiness to change a
behavior, information-seeking behavior,
media use, and lifestyle characteristics
• Cultural—language proficiency and
language preferences, religion, ethnicity,
generational status, family structure,
degree of acculturation, and lifestyle
factors (e.g., special foods, activities)
• Demographic—occupation, income,
educational attainment, family situation,
and places of residence and work
24
Planning and Strategy Development

• Physical—sex, age, type and degree of
exposure to health risks, medical
condition, disorders and illnesses, and
family health history
• Psychographic—attitudes, outlook on life
and health, self-image, opinions, beliefs,
values, self-efficacy, life stage, and
personality traits
The key to success is to segment the
intended population on characteristics
relevant to the health behavior to be
changed. A logical starting point is the
behavior itself: When possible, compare
those who engage in the desired behavior
with those who do not and identify the
determinants of their behavior. Many
planners simply rely on demographic,
physical, or cultural segmentations.
However, people who share these
characteristics can be very different in terms
of health behavior. For example, consider
two 55-year-old African-American women.
They work together in the same department.
They have the same amount of schooling
and comparable household incomes. They
live next door to each other, attend the same
church, and often invite each other’s family
over for meals. They enjoy the same
television shows, listen to the same radio
stations, and often discuss articles that they
both read in the paper. Neither has a family
history of breast cancer, and both had
children before age 30.Yet one woman goes
for annual mammograms and the other has
never had one. A demographic, physical, or
cultural segmentation would group these
women together, yet one is a member of the
intended audience for health
communications about mammography and
the other is not.
Select Intended Audiences
Once you have identified intended audience
segments, begin to set priorities and select
DATABASES HELP NCI IDENTIFY
AND
COMMUNICATE WITH INTENDED-
A
UDIENCE SEGMENTS
To help identify and understand its
intended audiences, NCI’s Office of
Communications (OC) uses a unique
database that combines health behavior
information with geographic,
demographic, and lifestyle data. OC
uses this information to create
Consumer Health Profiles that give a
portrait of the intended audience
segments most in need of cancer
prevention and detection messages.
Consumer Health Profiles describe:
• Which populations within a region
most need cancer education and
outreach and where these populations
live, including maps (e.g., which areas
of a state have the lowest cancer
screening rates)
• How to reach these populations, based
on factors such as media habits and
knowledge, attitudes, and beliefs
about cancer
Consumer Health Profiles are useful not
only in locating an intended audience
but also in understanding people better.
NCI’s Cancer Information Service and
its partners have used the profiles to
plan media buys and direct mailings to
increase the number of women
participating in low-cost mammography
screening programs. For more
information, contact CIS’s Partnership
Program at 1-800-4-CANCER or the
Office of Communications at
301-496-6667.
STAGE 1
Making Health Communication Programs Work
25

the intended audiences (e.g., those
segments with whom you will communicate).
As you select your intended audiences,
distinguish among the audiences your
program will address. Primary intended
audiences are those you want to affect in
some way; you may have one or several
primary intended audiences. If you have
more than one, set priorities among them
to help order your planning and allocate
resources. Secondary intended audiences,
or gateway audiences, are those with
influence on the primary intended audiences
or those who must do something to help
cause the change in the primary intended
audiences. These intended audiences might
need different kinds of messages and tools
to make the desired change.
Select intended audiences by answering the
following questions for each segment:
• What is a reasonable and realistic
communication objective for this intended
audience? In other words, what behavior
change can the intended audience make,
and how willing is this group to make that
change? Sometimes an intended
audience can’t make a behavior change—
or can’t make it easily—until a policy
change is instituted or a new or improved
product is developed. If your program
cannot provide the necessary policy or
technological changes, perhaps another
intended audience would be a better
choice. (See Appendix B for a description
of relevant theories and models of
behavior change that may help you
answer this question.)
• Will achieving that communication
objective with this intended audience
adequately contribute to attaining the
health program goal? (See planning step 2.)
intended audience size factors
prominently in the answer to this question.
It is important to choose a segment or
segments large enough that changes in
their behavior will make a worthwhile
contribution to your program’s goal. If your
program’s goal is population-wide
improvement, asking a larger intended
audience to make a small change may get
you closer to the goal and require fewer
resources than helping a small group
make a very large change.
• To what extent would members of this
segment benefit from the communication?
Some segments may already engage in
the desired behavior or may be close to it
(e.g., eating four servings of fruits and
vegetables each day, but not five).
• How well can available resources and
channels reach this segment? If you must
rely on mass communication (e.g., mass
media, public events), yet one-on-one skill
modeling is needed to help this segment
make a behavior change, your program’s
resources will be wasted.
• For secondary intended audiences, to
what extent does this audience influence
the primary intended audiences?
• To what extent will we be able to measure
progress? See the Communication
Research Methods section for a
discussion of measurement
considerations.
Answering these questions will also help
you determine who will not be members of
an intended audience. Ruling out intended-
audience segments will allow you to make
decisions regarding message development
and dissemination more easily and will help
ensure that all program resources are spent
productively. Two examples of intended
26
Planning and Strategy Development

audiences are 1) teens who smoke, and
2) women over age 50 who are not having
regular mammograms.
Learn More About the Intended Audiences
You probably need to know more about the
intended audiences than you learned from
the initial research. Sometimes planners
conduct consumer research on all potential
intended audiences to help them set
objectives, complete intended audience
segmentation, and set priorities. At other
times, they define and set priorities among
intended audiences based on initial
research and then conduct more intensive
research with selected intended audiences.
The approach often depends upon the
amount of existing secondary research
and the resources available to conduct
primary research.
To learn about an intended audience, find
answers to the following questions:
• What does the intended audience
already know about the topic? Do
intended audience members have
any misconceptions?
• What are the intended audience
members’ relevant attitudes, beliefs, and
perceptions of barriers to change?
• How “ready” is the intended audience to
change? (Based upon the stages of
change model—see Appendix B for
a description.)
• What benefit do intended audience
members already associate with making
the behavior change?
• What social, cultural, and economic
factors will affect program development
and delivery?
• When and where (times, places, states of
mind) can the intended audience best
be reached?
• What communication channels (e.g.,
mass media, organization meetings,
Internet sites) reach this intended
audience? Which do its members prefer?
Find credible? (Look to the census for
this information.)
• Do certain individuals (or gatekeepers)
either have particular influence with this
intended audience or control access to it?
What is their degree of influence?
• What are the intended audience’s
preferences in terms of learning styles,
appeals, language, and tone?
See the Communication Research Methods
section to learn ways to gather information
about intended audiences.
4. Explore Settings, Channels, and
Activities to Reach Intended Audiences
In this step, begin to think about the best
ways to reach the intended audiences.
To reach intended audiences effectively and
efficiently, first identify the settings (times,
places, and states of mind) in which they are
most receptive to and able to act upon the
message. Next, identify the channels
through which your program’s message can
be delivered and the activities that can be
used to deliver it. In making these decisions,
weigh what will best:
• Reach the intended audience
• Deliver the message
Explore Settings
To identify possible settings for reaching the
intended audience, think of the following:
• Places where your program can reach the
intended audience (e.g., at home, at
school or work, in the car, on the bus or
STAGE 1
Making Health Communication Programs Work
27

train, at a community event, in the local
Interpersonal Channels
health care provider’s office or clinic)
• Times when intended audience members
may be most attentive and open to your
program’s communication effort
• Places where they can act upon
the message
• Places or situations in which they will find
the message most credible
Sometimes a given setting may be a good
place to reach the intended audience but not
a good place to deliver the message. For
example, a movie theater slide might be a
great way to reach the intended audience,
but if the message is “call this number to
sign up for this health program,” people may
not be receptive to (or able to act upon) the
message—and they are unlikely to recall the
message or the number later, when they can
act on it. In contrast, if you reach people
while they are preparing dinner—or in the
grocery store—with a message to increase
fruit and vegetable consumption, they are
likely to be receptive to and able to act upon
the message.
Explore Channels and Activities
Message delivery channels have changed
significantly in the decade since this book
first appeared. Today, channels are more
numerous, are often more narrowly focused
on an intended audience, and represent
changes that have occurred in health care
delivery, the mass media, and society.
Consider the following channels:
• Interpersonal
• Group
• Organizational and community
• Mass media
• Interactive digital media
Interpersonal channels (e.g., physicians,
friends, family members, counselors,
parents, clergy, and coaches of the intended
audiences) put health messages in a
familiar context. These channels are more
likely to be trusted and influential than
media sources. Developing messages,
materials, and links into interpersonal
channels may require time; however, these
channels are among the most effective,
especially for affecting attitudes, skills, and
behavior/behavioral intent. Influence through
interpersonal contacts may work best when
the individual is already familiar with the
message, for example, from hearing it
through mass media exposure. (Similarly,
mass media are most effective at changing
behavior when they are supplemented with
interpersonal channels.)
Group Channels
Group channels (e.g., brown bag lunches at
work, classroom activities, Sunday school
discussions, neighborhood gatherings, and
club meetings) can help your program more
easily reach more of the intended audience,
retaining some of the influence of
interpersonal channels. Health messages
can be designed for groups with specific
things in common, such as workplace,
school, church, club affiliations, or favorite
activities, and these channels add the
benefits of group discussion and affirmation
of the messages. As with interpersonal
channels, working through group channels
can require significant levels of effort.
Influence through group channels is more
effective when groups are already familiar
with the message through interpersonal
channels or the others described here.
28
Planning and Strategy Development

DOCTOR TO PATIENT: THE INTERPERSONAL CHANNEL
Interpersonal channels have shown great success in delivering credible messages that
produce desired results. When the one-to-one message comes from the doctor, people are
especially likely to listen. Good communication between health care providers and
individuals is so important to achieving positive health outcomes that the Health
Communication chapter of Healthy People 2010 includes an objective to “increase the
proportion of persons who report that their health care providers have satisfactory
communication skills” (objective 11-6). In addition, the chapter on cancer includes an
objective to “increase the proportion of physicians and dentists who counsel their at-risk
patients about tobacco-use cessation, physical activity, and cancer screening”
(objective 3-10).
Examples of the results of physician-patient communication include:
• Doctor-patient communication has been associated with improved recovery from
surgery, shortened hospital stays, lower blood pressure and blood sugar, and better
health status.
• People who quit smoking in response to physician advice are more likely to make
repeated attempts to quit and are more likely to remain off cigarettes.
• Women in a national survey said a major reason they never had a mammogram was,
“My doctor never recommended one.” When a Massachusetts program increased the
number of physicians who recommended mammography, screening rates also rose.
• Most people in a national survey said their preferred source of information about
prescription medicines is their physician. When patients and physicians communicate,
compliance improves.
STAGE 1
Making Health Communication Programs Work
29

Organizational and Community Channels
Organizations and community groups, such
as advocacy groups, can disseminate
materials, include your program’s messages
in their newsletters and other materials,
hold events, and offer instruction related to
the message. Their involvement also can
lend their credibility to your program’s
efforts. Organizational/community channels
can offer support for action and are two-way,
allowing discussion and clarification,
enhancing motivation, and
reinforcing action.
Mass Media Channels
Mass media channels (e.g., radio, network
and cable television, magazines, direct mail,
billboards, transit cards, newspapers) offer
many opportunities for message
dissemination, including mentions in news
programs, entertainment programming
(“entertainment education”), public affairs
programs, “magazine” and talk shows
(including radio audience call-ins), live
remote broadcasts, editorials (television,
radio, newspapers, magazines), health and
political columns in newspapers and
magazines, posters, brochures, advertising,
and public service campaigns.You may
decide to use a variety of formats and
media channels, always choosing from
among those most likely to reach the
intended audiences.
Mass media campaigns are a tried-and-true
communication approach. They have been
conducted on topics ranging from general
health to specific diseases, from prevention
to treatment. Overall, research has
demonstrated the effectiveness of mass
media approaches in:
• Raising awareness
• Stimulating the intended audience to seek
information and services
• Increasing knowledge
• Changing attitudes and even achieving
some change (usually) in self-reported
behavioral intentions and behaviors
However, behavior change is usually
associated with long-term, multiple-
intervention campaigns rather than with
one-time communication-only programs.
Interactive Digital Media Channels
Interactive digital media channels (e.g.,
Internet Web sites, bulletin boards,
newsgroups, chat rooms, CD-ROMs, kiosks)
are an evolving phenomenon and are useful
channels that should have even greater
reach in the future. These media allow
communicators to deliver highly tailored
messages to and receive feedback from the
intended audience. These channels are
capable of producing both mass
communication and interpersonal
interaction. Use these media to:
• Send individual messages via
electronic mail
• Post program messages (such as
information about health-related
campaigns) on Internet sites that large
numbers of computer users access
30
Planning and Strategy Development

INTERNET AND MULTIMEDIA CHANNELS
CD-ROMs—Computer disks that can contain an enormous amount of information,
including sound and video clips and interactive devices.
Chat rooms—Places on the Internet where users hold live typed conversations. The
“chats” typically involve a general topic. To begin chatting, users need chat software, most
of which can be downloaded from the Internet for free.
Electronic mail (e-mail)—A technology that allows users to send and receive messages to
one or more individuals on a computer via the Internet.
Interactive television—Technologies that allow television viewers to access new
dimensions of information (e.g., link to Web sites, order materials, view additional
background information, play interactive games) through their television during related
TV programming.
Intranets—Electronic information sources with limited access (e.g., Web sites available
only to members of an organization or employees of a company). Intranets can be used to
send an online newsletter with instant distribution or provide instant messages or links to
sources of information within an organization.
Kiosks—Displays containing a computer programmed with related information. Users
can follow simple instructions to access personally tailored information of interest and, in
some cases, print out what they find. A relatively common health application is placing
kiosks in pharmacies to provide information about medicines.
Mailing lists (listservs)—E-mail–based discussions on a specific topic. All the subscribers
to a list can elect to receive a copy of every message sent to the list, or they may receive a
regular “digest” disseminated via e-mail.
Newsgroups—Collections of e-mail messages on related topics. The major difference
between newsgroups and listservs is that the newsgroup host does not disseminate all the
messages the host sends or receives to all subscribers. In addition, subscribers need special
software to read the messages. Many Web browsers, such as Internet Explorer, contain this
software. Some newsgroups are regulated (the messages are screened for appropriateness to
the topic before they are posted).
Web sites—Documents on the World Wide Web that provide information from an
organization (or individual) and provide links to other sources of Internet information.
Web sites give users access to text, graphics, sound, video, and databases. A Web site can
consist of one Web page or thousands of Web pages. Many health-related organizations
have their own Web sites.
STAGE 1
Making Health Communication Programs Work
31

COMMUNICATION CHANNELS AND ACTIVITIES: PROS AND CONS
Type of Channel
Interpersonal
Channels
Organizational
and Community
Channels
Mass Media
Channels
Newspapers
Radio
Activities Pros Cons
• Hotline counseling • Can be credible • Can be expensive
• Patient counseling
• Permit two-way • Can be time-consuming
• Instruction
discussion • Can have limited
• Informal discussion
• Can be motivational, intended audience
influential, supportive reach
• Most effective for teaching • Can be difficult to link
and helping/caring into interpersonal
channels; sources need
to be convinced and
taught about the
message themselves
• Town hall meetings and • May be familiar, trusted,
• Can be costly, time-
other events and influential
consuming to establish
• Organizational meetings • May provide more
• May not provide
and conferences motivation/support than
personalized attention
• Workplace campaigns media alone
• Organizational
• Can sometimes be
constraints may require
inexpensive
message approval
• Can offer shared
• May lose control of
experiences
message if adapted to
• Can reach larger intended
fit organizational needs
audience in one place
• Ads
• Can reach broad intended • Coverage demands a
• Inserted sections on a
audiences rapidly newsworthy item
health topic (paid)
• Can convey health • Larger circulation
• News
news/breakthroughs more papers may take only
• Feature stories
thoroughly than TV or
paid ads and inserts
• Letters to the editor
radio and faster than • Exposure usually limited
• Op/ed pieces
magazines to one day
• Intended audience has • Article placement
chance to clip, reread, requires contacts and
contemplate, and pass may be time-consuming
along material
• Small circulation papers
may take PSAs
• Ads (paid or public
• Range of formats
• Reaches smaller
service placement)
available to intended
intended audiences
• News
audiences with known
than TV
• Public affairs/talk shows
listening preferences
• Public service ads run
• Dramatic programming
• Opportunity for direct
infrequently and at low
(entertainment
intended audience
listening times
education)
involvement (through call-
• Many stations have
in shows)
limited formats that may
• Can distribute ad scripts
not be conducive to
(termed “live-copy ads”),
health messages
which are flexible
• Difficult for intended
and inexpensive
audiences to retain or
pass on material
Continued on next page...
32
Planning and Strategy Development

COMMUNICATION CHANNELS AND ACTIVITIES: PROS AND CONS CONTINUED...
Type of Channel Activities Pros
Cons
Radio continued...
Television
Internet
• Ads (paid or public
service placement)
• News
• Public affairs/talk shows
• Dramatic programming
(entertainment
education)
• Web sites
• E-mail mailing lists
• Chat rooms
• Newsgroups
• Ads (paid or public
service placement)
• Paid ads or specific
programming can reach
intended audience when
they are most receptive
• Paid ads can be
relatively inexpensive
• Ad production costs are low
relative to TV
• Ads allow message and its
execution to be controlled
• Reaches potentially the
largest and widest range of
intended audiences
• Visual combined with audio
good for emotional appeals
and demonstrating behaviors
• Can reach low income
intended audiences
• Paid ads or specific
programming can reach
intended audience when
most receptive
• Ads allow message and its
execution to be controlled
• Opportunity for direct
intended audience
involvement (through
call-in shows)
• Can reach large numbers
of people rapidly
• Can instantaneously update
and disseminate information
• Can control information
provided
• Can tailor information
specifically for
intended audiences
• Can be interactive
• Can provide health
information in a graphically
appealing way
• Can combine the
audio/visual benefits of TV
or radio with the
self-paced benefits of
print media
• Can use banner ads to
direct intended audience to
your program’s Web site
• Ads are expensive
to produce
• Paid advertising is
expensive
• PSAs run infrequently
and at low viewing times
• Message may be
obscured by
commercial clutter
• Some stations reach
very small
intended audiences
• Promotion can result in
huge demand
• Can be difficult for
intended audiences
to retain or pass
on material
• Can be expensive
• Many intended
audiences do not have
access to Internet
• Intended audience must
be proactive—must
search or sign up
for information
• Newsgroups and chat
rooms may
require monitoring
• Can require
maintenance over time
STAGE 1
Making Health Communication Programs Work
33

• Create and display advertisements
• Survey and gather information from
computer users
• Engage intended audiences in
personalized, interactive activities
• Exchange ideas with peers and partners
Using interactive digital media is not without
challenges. If you choose to do so, consider
credibility and access issues.
Credibility. Anyone can put information on
the Internet, and it may or may not be
accurate. Thus it is important to demonstrate
the credibility of your organization when you
use this channel to disseminate health
information. This will help ensure that users
trust the information they receive.
To improve the quality of health information
on the Internet, Healthy People 2010
includes an objective to increase the
proportion of health-related Web sites that
disclose information that can be used to
assess the site’s quality (objective 11-4). To
improve quality, health Web sites should
disclose the following information:
• The identity of the developers and
sponsors of the site, how to contact them,
and information about any potential
conflicts of interest or biases
• The explicit purpose of the site, including
any commercial purposes and advertising
• The original sources of the content
on the site
• How the privacy and confidentiality of any
personal information collected from users
is protected
• How the site is evaluated
• How content is updated
Access. The average computer user is
affluent and well educated. Although access
to this medium is increasing, it is definitely
not universal; television and radio are better
choices to reach a larger intended audience.
The U.S. Department of Commerce issues
reports on the “digital divide,” the gap
between those with access to computers
and the Internet and those without. Healthy
People 2010 includes an objective to
increase from 26 to 80 the percentage of
households with access to the Internet so
that individuals will be able to get the
information and services they need to
address their health concerns
(objective 11-1).
Weigh Pros and Cons
As illustrated in the table Communication
Channels and Activities: Pros and Cons,
each type of channel—and activity used
within that channel—has benefits and
drawbacks. Weigh the pros and cons by
considering the following factors:
• Intended audiences you want to reach:
—
Will the channel and activity reach and
influence the intended audiences (e.g.,
individuals, informal social groups,
organizations, society)?
—
Are the channel and activity acceptable
to and trusted by the intended
audiences, and can they
influence attitudes?
• Your message:
—
Is the channel appropriate for
conveying information at the desired
level of simplicity or complexity?
—
If skills need to be modeled, can the
channel model and demonstrate
specific behaviors?
• Channel reach:
—
How many people will be exposed to
the message?
34
Planning and Strategy Development

BEST CHOICE: USING MULTIPLE CHANNELS TO REACH INTENDED AUDIENCES
Using several different channels increases the likelihood of reaching more of the intended
audiences. It also can increase repetition of the message, improving the chance that
intended audiences will be exposed to it often enough to absorb and act upon it. For these
reasons, a combination of channels has been found most effective in producing desired
results, including behavior change.
For example, Center for Substance Abuse Prevention (CSAP) communication grantees have
combined channels in unique ways that reflect their communities. One grantee used
posters in community facilities, placed radio spots, and distributed brochures through
community sites and requests by radio listeners. Another used a satellite network to show
videos, made small group presentations through organizations, and worked with schools
to promote at-home activities. Yet another promoted its message through a music and
visual arts training program that resulted in a live performance and television broadcast of
the program’s art and musical creations.
Note. Center for Substance Abuse Prevention Communications Cooperative Agreements. (1996).
Bridging the Gap for People with Disabilities. Rockville, MD: U.S. Department of Health and Human
Services. In the public domain.
STAGE 1
—
Can the channel meet intended
audience interaction needs?
—
Can the channel allow the intended
audience to control the pace of
information delivery?
• Cost and accessibility:
—
Does your program have the resources
to use the channel and the activity?
• Activities and materials:
—
Is the channel appropriate for the
activity or material you plan to
produce? (Decisions about activities
and channels are interrelated and
should be made in tandem. See Stage
2 for a list of possible materials for
health programs and a discussion of
decision factors.)
—
Will the channel and activity reinforce
messages and activities you plan
through other routes to increase
overall exposure among the
intended audiences?
5. Identify Potential Partners
Working with other organizations can be a
cost-effective way to enhance the credibility
and reach of your program’s messages. Many
public health institutions seek out partner
organizations to reach particular intended
audiences.
The benefits to your program of forming
partnerships can include:
• Access to an intended audience
• More credibility for your message or
program because the intended audiences
consider the potential partner to be a
trusted source
• An increase in the number of messages
your program will be able to share with
intended audiences
• Additional resources, either tangible or
intangible (e.g., volunteers)
• Added expertise (e.g., training capabilities)
Making Health Communication Programs Work
35

• Expanded support for your organization’s
priority activities
• Cosponsorship of events and activities
You may partner with one or a few
organizations to accomplish specific
projects. Some communication initiatives
may call for tapping into or assembling a
coalition of organizations with a shared goal.
In some cases, you may need to assemble
many organizations that support particular
recommendations or policies. At other times,
you may want the organizations to play an
active role in developing and implementing
communication activities.
To encourage selected groups to partner
with your organization, consider the benefits
you can offer, such as:
• Added credibility
• Access to your organization’s data
• Assurance of message accuracy
• Liaison with other partners
Decide Whether You Want Partners
Although working with partners can be
essential to achieving communication
objectives, there are also drawbacks that
you should recognize and prepare to
address. Working with other
organizations can:
• Be time consuming—Identifying potential
partners, persuading them to work with
your program, gaining internal approvals,
and coordinating planning and training all
take time.
• Require altering the program—Every
organization has different priorities and
perspectives, and partners may want to
make minor or major program changes
to accommodate their own structure
or needs.
• Result in loss of ownership and control of
the program—Other organizations may
change the time schedule, functions, or
even the messages, and take credit for
the program.
Decide how much flexibility you would be
willing to allow a partner in the program
without violating the integrity of your
program, its direction, and your own
agency’s procedures. If you decide to
partner with other organizations,
consider which:
• Would best reach the intended audiences
• Might have the greatest influence and
credibility with the intended audiences
• Will be easiest to persuade to work with
you (e.g., organizations in which you know
a contact person)
• Would require less support from you
(e.g., fewer resources)
Develop Partnering Plans
Think about the roles potential partners
might play in your program and use the
suggestions below to help identify specific
roles for partners:
• Supplemental printing, promotion, and
distribution of materials
• Sponsorship of publicity and promotion
• Purchase of advertising space/time
• Creation of advertising about your
organization’s priority themes
and messages
• Underwriting of communication materials
or program development with
your organization
See Appendix A for a partnership plan form.
36
Planning and Strategy Development

WORKING WITH FOR-PROFIT PARTNERS
The National Cancer Institute uses these guidelines when considering
commercial partners.
Policies
• The National Cancer Institute will not consider any collaboration that endorses a
specific commercial product, service, or enterprise.
• The National Cancer Institute name and logo may be used only in conjunction with
approved projects and only with the written permission of NCI. NCI retains the right to
review all copy (e.g., advertising, publicity, or for any other intended use) prior to
approval of the use of the NCI name and logo.
• The National Cancer Institute will formally review each proposal for partnership.
• No company will have an exclusive right to use the NCI name and logo, messages,
or materials.
• Confidentiality cannot be guaranteed for any collaboration with a federal program.
Criteria for Reviewing Corporations Prior to Partnership Negotiations
• Company is not directly owned by a tobacco company and is not involved in
producing, marketing, or promoting tobacco products.
• Company does not have any products, services, or promotional messages that conflict
with NCI policies or programs (e.g., the company does not market known carcinogens
or market some other product that NCI would not consider medically or
scientifically acceptable).
• Company is not currently in negotiation for a grant or contract with NCI.
• Company does not have any unresolved conflicts or disputes with NCI or NIH.
• Establishing a partnership with this company will not create tensions/conflicts with
another NCI partner or federal program.
• Company or institution satisfactorily conforms with standards of health or medical care.
• There is evidence that the company would be interested in becoming a partner
with NCI.
Working With Partners
Developing and Maintaining Coalitions
The staff person responsible for working
Community coalitions have become an
with partners should be:
important force in health promotion.
Coalitions have all of the advantages of
• A good manager who is able to balance
partnerships plus another benefit. Because
all program components
they harness the resources and
• A team player who is able to work with
commitment of multiple organizations, the
other organizations
attention those organizations pay to an
• Diplomatic and willing to negotiate
issue is institutionalized for long-term action.
The strongest potential partners may be
• Willing to share credit for success
interested in joining coalitions.
STAGE 1
Making Health Communication Programs Work
37

STEPS FOR INVOLVING PARTNERS IN THE PROGRAM
1. Choose organizations, agencies, or individuals (e.g., physicians) that can bring the
resources, expertise, or credibility your program needs.
2. Consider which roles partners might play to best support the program.
3. Involve representatives of the organizations you want to work with as early as
appropriate in program planning.
4. Give partners the program rationale, strategies, and messages (in ready-to-use form).
Remember that strategic planning, creative messages, and quality production are the
most difficult aspects of a communication program to develop and may be the most
valuable product you can offer to a community organization.
5. Give partners advance notice so that they can build their part of the program into
their schedule, and negotiate what will be expected of them.
6. Allow partners to personalize and adapt program materials to fit their circumstances
and give them a feeling of ownership, but don’t let them stray from the strategy.
7. Ask partners what they need to implement their part of the program. Beyond the
question of funding, consider other assistance, training, information, or tools that
would enable them to function successfully.
8. Provide partners with new local/regional/national contacts or linkages that they will
perceive as valuable for their ongoing activities.
9. Give partners an appropriate amount of work. Give them a series of small, tangible,
short-term responsibilities, as well as a feedback/tracking mechanism.
10. Gently remind partners that they are responsible for their activities; help them
complete tasks, but don’t complete tasks for them.
11. Assess progress through the feedback/tracking mechanism and help make adjustments
to respond to the organization’s needs and to keep the program on track.
12. Provide moral support by frequently saying “thank you” and by providing other
rewards (e.g., letters or certificates of appreciation).
13. Give partners a final report of what was accomplished and meet to discuss follow-up
activities and resources they might find useful. Make sure that they feel they are a part
of the program’s success.
14. Share one final, tremendous “Thank you for a job well done.”
38
Planning and Strategy Development

39

Coalitions often grow from informal
partnerships or advisory bodies created
around special projects. Experience in
working together lays the groundwork for
a long-term association.
Use the following guidelines to create a
successful coalition:
• Formalize the relationship to create
greater commitment. Formal
arrangements include written memoranda
of understanding, by-laws, mission
statements, or regular reminders of the
coalition’s purpose and progress.
• Make sure that the responsibilities of each
organization and its staff are clear. In
particular, staff members need to know
whether to take direction from the coalition
chairperson or from the agency that pays
their salary.
• Structure aspects of the coalition’s
operation. Elect officers. Form standing
committees. Have regularly scheduled
meetings with written agenda and
minutes. Expect and support action, not
just discussion, at these meetings.
Circulate action items resulting from
meetings among coalition members.
Establish communication channels and
use them frequently.
• Ensure the involvement of representatives
who show leadership characteristics, such
as the ability to obtain resources, problem-
solve, and promote collaboration and
equality among members. Members with
political knowledge, administrative or
communication skills, or access to the
media and decision-makers are
also valuable.
• Create and reinforce positive expectations
by providing information on the coalition’s
progress. Optimism and success sustain
member interest.
• Formalize accountability and develop
criteria for judging whether coalition
members are honoring their commitments.
• Be flexible. Losing prospective partners
can limit a program’s effectiveness.
• Provide training to help members
complete their tasks. For example,
coalition members may need training in
how to be effective advocates for your
program’s issues.
• Give members a stake in the coalition and
an active role in decision-making.
• Seek external resources to augment
member resources.
• Evaluate the effectiveness of the coalition
periodically and make necessary changes.
This should include process evaluation of
the coalition’s functioning and assessment
of the coalition’s impact on the health
problem being addressed.
6. Develop a Communication Strategy;
Draft Communication and
Evaluation Plans
At this point your program has:
• Defined intended audiences and the
actions you want their members to take
(communication objectives)
• Explored the settings, channels, and
activities that can be used to reach them
• Identified potential partners
• Developed partnering plans
In this step, you will use this information as
the basis for developing a communication
strategy and drafting communication and
evaluation plans.
40
Planning and Strategy Development

Develop a Communication Strategy
Statement (Creative Brief)
In this context, a strategy is a
communication approach your program
plans to take with a specific intended
audience; while you may develop many
different communication materials and use a
variety of activities, the strategies are
guiding principles for all program products
and activities. A communication strategy
includes everything you need to know to
communicate with the intended audience. It
defines the intended audience, describes
the action its members should take, tells
how they will benefit (from their perspective,
not necessarily from a public health
perspective), and how you can reach them.
A communication strategy is:
• Based on knowledge of the intended
audience’s wants, needs, values,
and accessibility
• Guided by general communication
research as well as theories and models
of behavior
• Tempered by the realities of available
resources and deadlines
Developing the strategy statement provides
a good test of whether your program has
enough information to begin developing
messages. It also gives you an opportunity
to obtain management and partner buy-in
for the approach.You may be tempted to
skip this step, but do not. Having an
approved strategy statement will save time
and effort later. The statement provides both
a foundation and boundaries for all the
materials you produce and all the activities
you conduct.
The communication strategy statement is
sometimes called a creative brief because it
is used to brief the creative team. In
addition, sharing the strategy statement with
management and partners allows you to
make sure there is support for your
program’s approach before resources are
expended and makes easier the approvals
and cooperation you may need later.
For each of the intended audiences, write a
creative brief (see Appendix A for a template
to use) that includes the following:
• A definition and description of the
intended audience (intended-audience
profile). Think of one person in the
intended audience and describe him or
her, rather than describing the group. The
information you gathered in planning step
3 should provide the basis for this section.
• A description of the action the intended
audience members should take as a result
of exposure to the communication. The
action is the change the communication
objective specifies (planning step 2). If you
haven’t already done so, now is the time to
find out if intended audience members are
willing and able to take the action—and to
identify the current behavior that you want
to change. Knowing what an intended
audience currently does—and why it does
it—will provide important insights into the
behavior change process and can be used
to develop communications that
demonstrate replacing the old behavior
with the new one.
• A list of any obstacles to taking action.
Common obstacles include intended
audience beliefs, social norms, time or
peer pressures, costs, ingrained habits,
misinformation, and product
inaccessibility. The “map” you created in
planning step 1 should identify many of
the obstacles, particularly those related to
product inaccessibility (e.g., a woman
can’t get to a mammography location, a
worker has no access to fruits or
vegetables at break times, a condom isn’t
available at the time of intercourse).
STAGE 1
Making Health Communication Programs Work
41
SAMPLE STRATEGY STATEMENT
Draft Creative Brief Used for NCI 5 A Day for Better Health Program Concept
Development and Testing (June 2001)
Intended Audiences—African-American and Latino adults (men and women) with
primary responsibility for shopping and food preparation who have children under the
age of 13 and have household incomes of $25,000 to $50,000 who believe they and their
families should eat more fruits and vegetables.
Objective(s)—1) to believe that increasing their fruit and vegetable (f/v) intake is possible
(provides a “can do” self-efficacy element), and 2) to increase their f/v intake (gets at the
behavioral element, which is the ultimate goal; provides the “do it” element).
Obstacles
• Low salience/competition with everyday concerns and priorities
• Storage
• Low self-efficacy
• Children’s reaction/sensory
• Cost, convenience, freshness (cost, both out of pocket and perishability, is a top barrier
among African Americans)
• Not filling and don’t taste good (Latino issues)
• Safety (safety/pesticide issues are top barriers for eating vegetables for Latinos)
• Lack of planning time
• Preparation time (preparation time is a “top” barrier for eating vegetables among
African Americans)
• Lack of familiarity with certain fruits and vegetables
• Competition with other food products; i.e., fast foods
• Nutritional concerns about frozen/canned; e.g., canned are high in sodium; and for
Latinos, “not as healthy” misconception
• Lack of confidence in ability to get fruits and vegetables outside the home (survey
data, Latinos)
Key Promise
• If we eat more fruits and vegetables every day, I’ll feel good knowing we’re setting a
good example for our children and investing in a healthy future.
• If my family members eat more fruits and vegetables, they will function at their best and
protect their health as well as feel more energetic, help control their weight, and cleanse
their system.
• If we eat more fruits and vegetables every day, my family will stay healthy while
reducing its risk of cancer or heart disease in the future.
• If we have plenty of fruits and vegetables available for our family, we will be setting a
good example and teaching our children good, lifelong eating habits.
Continued on next page...
42
Planning and Strategy Development

SAMPLE STRATEGY STATEMENT CONTINUED...
Support Statements
• Fruit and vegetable consumption helps people feel good, look good, and maintain
their weight.
• Fruit and vegetable consumption provides generous amounts of fiber and promotes
digestive health.
• Obesity and childhood diabetes are epidemic.
• Fruit and vegetable consumption reduces the risk of heart disease/cancer.
Tone—Urgency without fear; positive…
Media
• TV PSAs
• Radio PSAs/Live announcer scripts
• Posters
• Newspaper ads
• Billboard and Metro Transit ads
• Earned Media (“Do Yourself a Flavor”)—African-American/Latino women can send
Graham Kerr recipes that he can select and feature
• Web site
• Articles in women’s magazines
Other Channels/Intermediaries
• Produce for Better Health
• State coordinators
Openings
• Traveling home from work
• Mother’s Day
• Community outreach (health fairs, in-store events such as taste tests or demonstrations),
grassroots programs
Creative Considerations
• Adaptable to local needs (state health profiles)
• Focus on more than one fruit or vegetable (equal opportunity)
• Appetite appeal, culturally appropriate, cross-cultural concepts that can be tailored
in execution
• Focus groups that include men and women and low-income ($25,000 or less in San
Antonio) participants at each site, which may drive creative to accommodate low
literacy; this is a good thing if we have both English- and Spanish-speaking people in
the intended audience. (Note: Creative executions should be intended audience specific,
while the concepts will cross over and work for both ethnic groups.)
STAGE 1
Making Health Communication Programs Work
43

The additional information you gathered
about the intended audience in
planning step 3 should also help you
identify obstacles.
• The consumer-perceived benefit of taking
the action. Many theories and models of
behavior change include the idea that
people change their behavior because
they expect to receive some benefit (e.g.,
gain in time, money, enjoyment, potential
gain in stature among peers) that
outweighs the personal cost of the
behavior change. Short-term, high-
probability personal benefits generally are
more effective than long-term population
benefits (e.g., “stop smoking to smell
better and be more attractive” rather than
“stop smoking to reduce your risk of
developing lung cancer”).
• A description of the support that will make
the benefit, and its ability to attain it,
credible to the intended audience. Support
can be provided through hard data, peer
testimonials about success or satisfaction,
demonstrations of how to perform the
action, or statements from organizations
the intended audience finds credible. Tailor
the particular supports you use to the
concerns intended audience members
have about the action. For example, if they
are worried they can’t do it, a
demonstration may be warranted; if they
question why they should take the action
or whether it will have the promised health
benefit, hard data or statements from
credible organizations may be in order; if
they don’t believe they need to take the
action (e.g., they deny being in the
intended audience), a peer testimonial can
be compelling.
• The settings, channels, and activities that
will reach intended audience members—
particularly when they will be receptive to
or able to act upon the message. This
information should come from the work
you did in planning step 4.
• The image your program plans to convey
through the tone, look, and feel of
messages and materials. The goal should
be to convey an image that 1) convinces
intended audience members that the
communication is for them, and 2) is
culturally appropriate. Image is conveyed
largely through executional details. Printed
materials convey image through typeface,
layout, visuals, color, language, and paper
stock used. Web materials convey image
through design, typeface, color, layout,
and ease of use. Audio materials convey
image through voices, language, and
music; in addition to these details, video
materials convey image through visuals,
characteristics of the actors (including
their clothing and accessories), camera
angles, and editing. Work with the creative
team to develop the image you select.
The information in Appendix B and the
information you learned about your intended
audience in planning step 3 are the
foundation for strategy development. Use
this information to prepare a document
similar to the NCI sample strategy statement
provided here. At first, you may have
question marks next to some items, or lists
of possibilities for actions, benefits, support,
or image.You can fill in the answers, narrow
down the list, and get overall reactions to
the strategy by conducting research with the
intended audience. (See the Communication
Research Methods section for suggestions
on how to obtain this input.) Developing the
communication strategy is usually an
iterative process; as you learn more about
one element, other elements will likely need
to be adjusted.
The communication strategy provides all
program staff—including writers, creative
staff, and evaluators—with the same
direction for developing all messages and
materials. In a cooperative program with
partner organizations, the strategy
44
Planning and Strategy Development

statement can also help all players
• Message and materials development and
communicate consistent themes and take
similar action. Some organizations choose to
produce report-length strategy statements
that contain additional information, such as
background on the health problem being
addressed, extensive intended audience
profiles, and situation analyses.
Once your program has decided on a
communication strategy, all program elements
should be compatible with it. This means
every program task should contribute to
reaching the established objectives and be
designed to reach the identified intended
audiences; all messages and materials
should incorporate the benefits and other
information from the strategy statement.
As you learn more about the intended
audiences and their perceptions, you may
need to alter or refine the strategy statement.
However, it should be changed only to reflect
information that will strengthen your
program’s ability to reach the communication
objectives. Do not alter your strategy simply to
accommodate a great idea that doesn’t match
the objectives.
Draft Communication Plan
All of the elements of your planning should be
recorded in a communication plan that will
become your “blueprint.” It should be used to:
• Explain the plans within your agency and
with others
• Support and justify budget requests
• Provide a record of where your
program began
• Show the program’s planned evolution
over time
Include the following sections in the plan:
testing plans
• Implementation plans, including plans
for distribution, promotion, and
process evaluation
• Outcome evaluation plans
• Tasks and timeline
A template for a communication plan that
includes all of these sections is in Appendix
A. During Stage 1, prepare initial drafts of all
plan sections except distribution and
promotion. Realize that some of the
sections, such as implementation and
process evaluation (see Stage 3), may not
be as detailed as others at this point.
Draft Outcome Evaluation Plans
Outcome evaluation is used to assess the
degree to which the communication
objectives are achieved. Conducting useful
outcome evaluation can be challenging
because of the following constraints:
• Many standard evaluation approaches
assume a direct cause-and-effect
relationship between the stimulus (your
program’s communication) and the
intended audience’s response to it.
However, it can be impossible to isolate
the effects of a particular communication
activity, or even the effect of a
communication program on a specific
intended audience, because change does
not often occur as a result of just one
specific activity.
• Communication programs generally occur
in a real-world setting, where there are
many other influences on the intended
audiences. Other activities (and often
other organizations) may be addressing
the same problem. Attributing change to
program activities may be very difficult.
STAGE 1
• Communication strategy
• Partnering plans
Making Health Communication Programs Work
45

• Communication objectives can be
reasonable but not measurable because
of reasons such as:
— The change is too small for available
methodologies to detect (e.g., a
2 percent increase over the course of a
year in the number of women age 50 or
over who get a mammogram would
have important public health benefits,
but would not be detectable by a survey
with a typical 3.1 percent margin
of error).
— The change is difficult to measure
validly or reliably (e.g., self-reports of
behavior are often unreliable).
Plan Outcome Evaluation Activities
Before you begin to plan for outcome
evaluation, review Stage 4 for descriptions
of common methodologies. As you plan,
keep the following tips in mind:
• Ensure that the evaluation design is
appropriate for the particular
communication activity. Experimental
designs, in which a treatment group
(people exposed to the communication) is
compared to a control group (people not
exposed to the communication), are the
gold standard of outcome evaluation.
However, they often cannot be used to
assess communication activities, largely
because untreated control groups may not
exist, particularly for national-, state-, or
community-based efforts. Even if people
are not exposed to your program’s
communication, they are likely to be
exposed to some communication on the
same topic. In these situations,
appropriate designs include comparisons
between cross-sectional studies (such as
independent surveys taken at different
points in time), panel studies (the same
people are interviewed or observed
multiple times), and time series analyses
(comparisons between projections of what
would have happened without the
intervention versus what did happen).
However, each is appropriate in different
situations; seek the advice of an
evaluation expert before selecting
a design.
• Consider how the communication activity
is expected to work and the time period in
which it is expected to work. Then make
sure it is evaluated in accordance with
those expectations. For example, if you
expect people to need at least five to eight
exposures to the message before they will
take action, make sure that you allow
sufficient implementation time to achieve
the intended level of exposure. If you
expect people to take action immediately
after exposure, then the outcome
measurement should take place soon
after that. Conversely, if you don’t expect
to see effects for at least a year, outcomes
shouldn’t be measured until then.
Communication programs are often
deemed “failures” because they don’t
reach people with sufficient repetition to
work—either because they are
inadequately funded or because
everything runs late and they are not in
place long enough before outcomes are
measured. (Use process evaluation to
track the level of intensity and the duration
of message exposure to learn why
expected outcomes did or did not occur.)
• Consider what level of evidence is
acceptable for your outcome evaluation
purpose (e.g., to report back to
management or funding agencies).
• Consider what baseline measures you
have available or can collect and how to
track changes related to desired outcomes
(e.g., how, and how often, data will
be collected).
• Ensure that you measure change against
the communication objectives and not
46
Planning and Strategy Development

against your program’s goal. For example, 2. Take another look at these sections after
if the communication objective is to
increase the percentage of women age
50 or older who ask their doctor about a
mammogram, you would measure how
many women asked their doctor about a
mammogram, not how many women got
a mammogram.
• Ensure that progress toward outcomes is
captured. For example, if you expect
people to think about changing a behavior,
and perhaps try changing it a few times
before making and sustaining the change,
make sure the evaluation can capture
these intermediate outcomes. If the
objective is to increase the percent of
people engaging in moderate exercise on
most days of the week, it would be
important to determine 1) people’s current
behavior, and 2) whether they have
thought about increasing their amount of
activity, taken steps to increase it, or
increased it some weeks but
not consistently.
Appendix A contains an outcome evaluation
form. Although you may not be ready to
complete final evaluation planning now, it is
important to put together a general plan so
that your program can collect any necessary
baseline data before implementation begins,
build any needed evaluation mechanisms
into the program, and ensure that evaluation
resources are allocated. To get started, do
the following:
1. Read Stage 4 (Assessing Effectiveness
and Making Refinements) and look at the
table at the beginning of the
Communication Research Methods
chapter. What you learn about evaluation
may affect what you choose to do with
the program.
your initial communication plan is
complete to be sure the evaluation
activities will be appropriate and valuable.
3. Involve an evaluation expert familiar with
evaluating communication programs
during initial planning. His or her advice
can help prevent time-consuming fixes
later by ensuring you develop a program
that can be validly evaluated (e.g., making
sure data collection mechanisms are in
place, making sure baseline data are
collected for comparison later).
Create a Timetable
Finally, produce a time schedule for
development, implementation, and
evaluation. The schedule should include
every task you can think of from the time
you write the plan until the time you intend
to complete the program. The more tasks
you build into the timetable now, the more
likely you will remember to assign the work
and keep on schedule. Also, detailing the
tasks will make it easier to decide what
resources will be required. If you forget
important intermediate steps, your
program’s costs and schedule
might change.
The timetable should be considered a
flexible management tool. Review and
update it regularly (e.g., once a month) so
that it can function dually to manage and
track progress. Many managers believe
computer-based tools are especially useful
for this task. Project management computer
software contains schedule forms that you
can fill in and monitor on the computer and
print out for staff and others involved.
STAGE 1
Making Health Communication Programs Work
47

Common Myths and Misconceptions
About Planning
Myth: Our program can’t afford to conduct
intended audience research.
Fact:
Your program can’t afford not to
conduct intended audience research.
Without it, you do not know for sure whom to
select, where to reach them, what to ask
them to do, or how to ask it. The information
you need to develop effective communication
may be relatively inexpensive or free.
Resources include literature searches,
information available free from government
health agencies, and advisory groups and
representatives of the intended audience.
For example, the National Cancer Institute’s
5 A Day for Better Health Program media
campaign used primary research to identify
its intended audiences, actions they would
be willing to take, and benefits they would
find compelling, but used existing marketing
databases to obtain a great deal of
information about their lifestyles, interests,
outlook, and media habits. The cost for
analyzing the databases was substantially
less than it would have been to conduct and
analyze additional primary research.
Myth: Market research isn’t relevant for a
health program.
Fact:
Health program planners can use the
methodologies and types of information
normally associated with market research in
many ways, including:
• Understanding why individuals would
choose or not choose to undertake a new
behavior, other preferences regarding the
behavior, how communicators should talk
about the behavior (tone and language),
and where individuals seek out or
receive information
• Creating a multidimensional portrait of the
intended audience for communication
planning; knowing only health-related
factors limits understanding of the whole
person your program is trying to influence
and does not provide guidance on when
and where to reach the person or what to
say to persuade the intended audience
• Supporting strategy development for
policy initiatives by helping to describe
opinion leaders, policymakers, and
their constituents
Myth: We don’t have time for planning.
Our boss (or funding agency or partner
organization) wants us to get started
right away.
Fact:
Making health communication
programs work requires planning, but
planning need not be a long-term, time-
consuming activity. Nor should all the
activities suggested in this section be
conducted en masse, before any other
actions are taken. Planning is easiest and
best done bit by bit—related to and just in
time for the programmatic tasks it governs.
For example, you need certain kinds of
information about the intended audiences in
order to define them, select them, and set
objectives.You need different information to
guide message development; gather each
type as you need it.
One person should not be doing all planning
tasks. Divide responsibilities for individual
tasks such as managing market research or
drafting the strategic plan and have the
whole planning team (or manager) reconcile
and revise to create the final plan.
48
Planning and Strategy Development

Myth: If we work with partner
organizations that represent the intended
audience, we’ll have access to all the
channels we need.
Fact:
Channels you access through a
partner organization may be very useful, but
they may miss intended audience segments
the organization does not represent, and
they may not be the most credible or
effective way to influence the intended
audience. Using additional channels will
help reinforce your program’s messages
and enhance the likelihood that the intended
audience will recall them.
Myth: It’s best to use the channels we’re
comfortable with and have used before.
Fact:
Selecting the right channels is as
important to success as developing effective
materials or having a sound strategy. If the
intended audience never sees/hears the
message, doesn’t believe it because it
comes from an unrespected source, or
doesn’t attend to it because it comes from
a noninfluential source, the time and money
your program spends developing the
message will be wasted. While you may
well make good use of channels where you
have previous contacts, determine whether
these channels alone will reach and
influence intended audiences before relying
solely on them.
Myth: If we use only one channel, we
should use mass media.
Fact:
In the past, many programs may have
concentrated on mass media, particularly
public service announcements. Today,
however, many other effective channels
exist and relying on mass media alone may
not achieve some communication program
goals. Although it may take time, effort, and
possibly outside expertise to learn about
and use new channels, the potential rewards
make this a good investment in your
program’s future and in your organization’s
long-term skill/knowledge base.
Myth: Using interactive digital media
requires major technical capabilities we
don’t have, and we can’t keep up.
Fact:
Using interactive digital media
effectively does require professional
expertise in product design—just as
professional expertise is needed to create
other types of communication vehicles and
develop effective evaluations. Consultants
from other branches of your organization,
universities, a volunteer pool, or commercial
firms can help. Some advertising/creative
firms are beginning to develop expertise in
these media, or you can use experts to
advise you on the electronic end while you
take care of the communication aspects.
These media are changing rapidly, just as
the computer field as a whole. However, if
you determine that interactive digital
channels will be very effective in reaching
the intended audience, networking with
peers, and conducting program research,
the investment may pay off.
STAGE 1
Making Health Communication Programs Work
49

Myth: If you don’t have interactive digital
media in your program, you are missing out
on today’s hottest communication
opportunity and will look very out of date
and low tech to your peers.
Fact:
Remember, interactive digital media
are just other channels. The same steps
discussed in this guide still apply, and good
communication principles and skills are still
paramount. The key selection factor is how
well these media will reach the intended
audience and how suited they are to
carrying the message. The intended
audience may not have sufficient access to
computers or have the skills or
attitudes/interest to seek information
through them. And, despite their potential,
much remains to be learned about their best
uses and how intended audiences respond
to and interact with them.
Selected Readings
American Cancer Society. (2001). Cancer
facts and figures. Atlanta.
American Public Health Association. (2000).
APHA media advocacy manual 2000.
Washington, DC.
Andreasen, A. (1988). Cheap but good
marketing research. Homewood, IL: Dow
Jones-Irvin.
Andreasen, A. (1995). Marketing social
change: Changing behavior to promote
health, social development, and the
environment. San Francisco: Jossey-Bass.
Calvert, P. (Ed.). (1996). The
communicator’s handbook: Tools,
techniques, and technology (3rd ed.).
Gainesville, FL: Maupin House.
Center for Substance Abuse Prevention.
(1994). Following specific guidelines will
help you assess cultural competence in
program design, application, and
management [Technical Assistance
Bulletin]. Washington, DC: U.S. Government
Printing Office.
Center for Substance Abuse Prevention.
(1998). Evaluating the results of
communication programs [Technical
Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Center for Substance Abuse Prevention
Communications Cooperative Agreements.
(1996). Bridging the gap for people with
disabilities. Rockville, MD: U.S. Department
of Health and Human Services.
Centers for Disease Control and Prevention.
(1996). The prevention marketing initiative:
Applying prevention marketing (CDC
Publication No. D905). Atlanta.
Centers for Disease Control and Prevention.
(2000). Beyond the brochure (CDC
Publication No. PDF-821K). Atlanta.
Davis, J. (Ed.). (2001). Health and medicine
on the Internet: An annual guide to the
World Wide Web for health care
professionals. Los Angeles: Practice
Management Information Corporation.
The Dialog Corporation. (2001). Packaged
facts. Available: http://library.dialog.com/
sourcebook/researchline/pf.html.
Eng, T. R., & Gustafson, D. H. (Eds.). (1999).
Wired for health and well-being: The
emergence of interactive health
communication. Washington, DC: U.S.
Department of Health and Human Services,
U.S. Government Printing Office.
50
Planning and Strategy Development

Glanz, K., Lewis, F. M., & Rimer, B. K. (Eds.).
Schooler, C., Chaffee, S. H., Flora, J. A., &
(1997). Health behavior and health education:
Theory, research, and practice (2nd ed.). San
Francisco: Jossey-Bass.
Glanz, K., & Rimer, B. K. (1995). Theory at a
glance: A guide for health promotion practice
(NIH Publication No. 97-3896). Bethesda, MD:
National Cancer Institute.
Goldberg, M. E., Fishbein, M. F., &
Middlestadt, S. E. (Eds.). (1997). Social
marketing: Theoretical and practical
perspectives. Mahwah, NJ: Erlbaum.
Jernigan, D. H., & Wright, P. A. (1996). Media
advocacy: Lessons from community
experiences. Journal of Public Health Policy,
17, 306–330.
Maibach, E., Maxfield, A., Ladin, K., & Slater,
M. (1996). Translating health psychology into
effective health communication. Journal of
Health Psychology, 1, 261–277.
Matiella, A. C. (Ed.). (1990). Getting the word
out: A practical guide to AIDS materials
development. Santa Cruz, CA:
Network Publications.
Miller, J., & Pifer, L. K. (1993). Public
understanding of biomedical science in the
United States, 1993: A report to the National
Institutes of Health. Chicago: Chicago
Academy of Science.
National Cancer Institute. (1996). Cancer
rates and risks (4th ed.; NIH Publication
No. 96-691). Bethesda, MD: Surveillance,
Epidemiology, and End Results
(SEER) Program.
Roser, C. (1998). Health campaign channels:
Tradeoffs among reach, specificity, and
impact. Human Communication Research,
24, 410–432.
Slater, M. D. (1996). Theory and method in
health audience segmentation. Journal of
Health Communication, 1, 267–283.
U.S. Department of Health and Human
Services. (2000). Healthy people 2010 (2nd
ed.; in two volumes: Understanding and
improving health and Objectives for improving
health). Washington, DC: U.S. Government
Printing Office.
University of Toronto. (1999). Overview of
health communication campaigns. Toronto,
Canada: Health Communication Unit, Centre
for Health Promotion, University of Toronto.
Wallach, L., & Dorfman, L. (1996). Media
advocacy: A strategy for advancing policy and
promoting health. Health Education Quarterly,
23(3), 293–317.
Wallach, L., Dorfman, L., Jernigan, D., &
Themba, M. (1993). Media advocacy and
public health: Power of prevention. Thousand
Oaks, CA: Sage.
STAGE 1
Making Health Communication Programs Work
51

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
STAGE 2
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Developing and Pretesting
Concepts, Messages, and Materials
In This Section:
• Why developing and pretesting concepts, messages, and materials
are important
• General steps in developing and pretesting concepts, messages,
and materials
• Reviewing existing materials
• Deciding what materials to develop
• Developing effective materials
• Planning for production, distribution, promotion, and process evaluation
• Common myths and misconceptions about pretesting
Questions to Ask and Answer:
• What materials will fit our strategy, appeal to our intended audience,
and adequately convey our message? How can we make the materials
as effective as possible?
• Do we need to create new materials? What types?
• How do we develop culturally appropriate messages and materials?
• How do we develop effective materials for low-literacy
intended audiences?
• How can we make sure the materials will be used?
• When and how should we pretest our materials?
• How can we keep pretesting costs down?
• What should we do with pretest results?
• How can we get the best results from creative and research
professionals? From reviewers?
STAGE 2

Why Developing and Pretesting
Messages and Materials Are Important
Developing and pretesting messages and
materials are important because they allow
you to learn early in the program which
messages will be most effective with the
intended audiences. Knowing this will save
your program time and money by ensuring
that you do not go through the entire
development process with an ineffective
message. Positive results from pretesting
can also give you early buy-in from
your organization.
See Appendix B for descriptions of theories
and models that suggest important audience
factors to consider when creating messages
so they are both acceptable and persuasive
to the intended audience.
Steps in Developing and Pretesting
Messages and Materials
In Stage 1, you created a communication
strategy statement. In Stage 2, you will use
the strategy you developed as a guide to:
1. Review existing materials
2. Develop and test message concepts
3. Decide what materials to develop
4. Develop messages and materials
5. Pretest messages and materials
1. Review Existing Materials
Message and materials development and
production can be time-consuming and
costly. Because this process is creative and
has tangible results, it is frequently the key
developmental step for a health
communication program. Before you begin
developing and producing new materials,
however, determine whether creating them
is necessary.
You may have discovered existing
communication materials (booklets, leaflets,
posters, public service announcements,
videotapes) while gathering data to plan the
program. If not, look now.You may find
materials at the following sources:
• Health departments (in your state or
other states)
• University or public libraries
• Voluntary organizations
• Health professional associations
• Community-based coalitions
• Clearinghouses, Web sites, and telephone
information services relevant to the issue
• Materials produced by the National
Institutes of Health, the Centers for
Disease Control and Prevention, or other
agencies in the U.S. Department of Health
and Human Services
• Healthfinder
®
, the Federal gateway to
health information, to identify relevant
Federal clearinghouses and other Federal
information sources
(www.healthfinder.gov)
See Appendix C for additional contact
information for these suggested sources.
If you find materials related to the health
issue, decide whether they are appropriate
for your program, either as they are or with
modifications. Using the communication
strategy statement as a guide, consider the
following questions:
• Are the messages accurate, current,
complete, and relevant?
• Are the materials appropriate for the
intended audience in format, style,
cultural considerations, and readability
level? If not, could they be modified to
be appropriate?
54
Developing and Pretesting Concepts, Messages, and Materials

• Are the materials likely to meet the See Appendix A for a sample form that you
communication objectives? can modify to help you conduct a materials
review.You also may want to test promising
Pretesting, discussed later in Stage 2, can
materials with the intended audience (see
help you answer these questions. Check
step 2). If the materials prove to be
with the group that originally produced the
inappropriate, you will have gained valuable
materials to learn about:
information for modifying them or developing
• Results of any pretesting
new materials.
• Effectiveness of the materials to date
2. Develop and Test Message Concepts
• Whether the group has advice or
recommendations related to your
The communication strategy statement and
program’s needs
the other planning you did in Stage 1 form
If you are considering using existing the basis for developing message concepts.
materials, also ask the original producer Message concepts are messages in rough
these questions: form and represent ways of presenting the
information to the intended audiences.
• Are they available?
These may include statements only or
• Could your organization receive
statements and visuals. Do not develop the
permission to use the materials? Modify
actual messages at this point. (If you create
them? Note: Materials produced by the
two or more concepts for each message,
Federal Government are not copyrighted
you will be able to explore which alternative
and may be used freely.
works best.)
• Are they affordable?
In this step, you will learn about the
• How have they been used?
components that go into developing and
• How have they been received?
NCI ADAPTS PAIN BROCHURES FOR READERS WITH LOW LITERACY SKILLS
When a panel of experts set new guidelines for cancer pain control, NCI wanted to share
its practical recommendations with patients. A sophisticated handbook was already
available for well-educated readers, and NCI staff searched for existing materials that
might work for readers with lower literacy skills. They found several local clinic and
cancer center publications that could potentially fill this need, but each was at too high a
reading level, lacked appealing graphics, and needed to be updated to reflect panel
recommendations. NCI decided to adapt the existing pieces and worked with the original
producers and specialists to develop easy-to-read materials and graphics. The revised
brochure was reviewed in draft by partnering clinics and health professionals and
pretested using focus groups and nurse-administered patient questionnaires.
One of the objectives included in Healthy People 2010 is to “improve the health literacy of
persons with inadequate or marginal literacy skills” (objective 11-2). NCI’s initiative to
adapt a brochure from previous materials illustrates how increases in health literacy will
come not only with improvements in individuals’ skills, but also with improvements in
the materials used to communicate critical information to patients and consumers.
STAGE 2
Making Health Communication Programs Work
55

testing message concepts, including experts, and others. See the Communication
working with creative professionals, creating Research Methods section for tips on working
culturally appropriate communication with market research experts.
concepts, choosing a type of appeal, and
testing concepts.
Working With Creative Professionals
To develop, pretest, and eventually produce
Developing a communication campaign
messages and materials, assemble a team
usually involves working with creative
of creative professionals, market research
professionals, either within your organization
NCI’S CANCER RESEARCH AWARENESS INITIATIVE: FROM MESSAGE CONCEPTS TO
FINAL MESSAGE
In 1996, the NCI’s Office of Communications (OC), then the Office of Cancer
Communications, launched the Cancer Research Awareness Initiative to increase the
public’s understanding of the process of medical discoveries and the relevance of
discoveries to people’s lives. OC’s concept development and message testing for this
initiative included the following activities.
Three values of medical research were selected for concept development:
1. Progress (e.g., we are achieving breakthroughs)
2. Benefits (e.g., prevention, detection, and treatment research are benefiting all of us)
3. Hope (e.g., we are hopeful that today’s research will yield tomorrow’s breakthroughs)
Based on these values, the following message concepts were developed and explored in
focus groups with intended audience members:
• Research has led to real progress in the detection, diagnosis, treatment, and
prevention of cancer
• Everyone benefits from cancer research in some fashion
• Cancer research is conducted in universities and medical schools across the country
• Cancer research gives hope
• At the broadest level, research priorities are determined by societal problems and
concerns; at the project level, research priorities are driven primarily by past research
successes and current opportunities
The following messages were crafted after listening to intended audience members’
reactions and their language and ideas about the importance of medical research:
A: Cancer Research: Discovering Answers for All of Us
B: Cancer Research: Because Cancer Touches Us All
C: Cancer Research: Discovering More Answers Every Day
D: Cancer Research: Because Lives Depend on It
E: Cancer Research: Only Research Cures Cancer
Mall-intercept interviews were conducted to pretest them. Based on responses from the
intended audience in these interviews, message D was selected as the program theme.
56
Developing and Pretesting Concepts, Messages, and Materials

or on a contract basis. In either case,
managing the relationship effectively is
critical to getting the creative materials
you want:
• Get to know and feel comfortable with the
people who will be working on the project.
If you are considering a contract with an
advertising agency, public relations firm,
or consulting firm, interview the
professionals who will staff your effort (not
just the agency representatives who solicit
your business) and review samples of
their specific work (not just the agency’s).
Write into the contract who will work on
the project.
• Be a good client. Use the creative brief to
lay out the communication strategy
(developed in Stage 1) and make sure the
team understands the brief and that it
must be followed. Think about what you
want before you discuss the assignment
and show the creative team examples of
other materials that worked well or didn’t
and explain why. If you say, “I don’t know
what I want; you’re the creative one,” you
lose a valuable opportunity to give creative
professionals the fundamental direction
they want and need. This does not mean
asking for a blue brochure; it means
helping members of the creative staff
understand the objectives and concerns
and what you’ve learned about the
intended audience so that they can use
their expertise to suggest effective
approaches. Discuss sensitive issues, key
content points, and other aspects that you
want to see conveyed in the messages
and materials, based on your knowledge
and expertise.
• Agree at the outset to what pretesting and
approvals will be required, when they will
occur, and how long they will take.
• Discuss the theoretical grounding of the
communication effort and help creative
professionals understand and apply health
communication theory to messages and
materials development. Brainstorm with
them about how the theory might shape
the messages and materials and evaluate
works in progress with this perspective
in mind.
• Involve the creative team in concept
exploration and pretesting. Ask its
members what questions they would like
addressed and make sure they can
observe (not participate in) concept
exploration sessions. Listening to the
intended audience can help them craft
messages and materials that use
language and ideas that the audience will
identify with.
• Assess draft messages and materials
against the creative brief and what you
know about an intended audience
member’s point of view. If the intended
audience is urban teens at high risk of
pregnancy, and you are a middle-aged
suburbanite, recognize that the materials
most likely to be effective with the
intended audience may not appeal to
you at all.
• Trust the team’s professional expertise,
provided that the material is consistent
with your program’s strategy and the
intended audience’s culture. While you
have a key role to play in ensuring the
appropriateness and accuracy of
substantive content and in maintaining the
program’s strategic focus, developing the
team’s insights and commitment will keep
the team involved.
Developing Culturally
Appropriate Communications
Culture encompasses the values, norms,
symbols, ways of living, traditions, history,
and institutions shared by a group of people.
Culture affects how people perceive and
respond to health messages and materials,
and it is intertwined in health behaviors and
STAGE 2
Making Health Communication Programs Work
57

attitudes. Often, an individual is influenced
by more than one culture; for example,
teenagers are influenced by their individual
family cultures as well as the norms, values,
and symbols that comprise teen culture in
their locale.
To develop effective health communications,
you must understand key aspects of the
cultures influencing the intended audience
and build that understanding into the
communication strategy. Messages must
take into account cultural norms in terms of
what is asked (e.g., don’t ask people to
make a behavior change that would violate
cultural norms), what benefit is promised in
exchange (in some cultures, community is
most important; in others, individual benefit
is), and what image is portrayed. The
symbols, metaphors, visuals (including
clothing, jewelry, and hairstyles), types of
actors, language, and music used in
materials all convey culture.
While it is important to acknowledge and
understand the cultures within an intended
audience, developing separate messages
and materials for each cultural group is not
always necessary or even advisable. For
example, when print materials for a state
program for low-income people depicted
people of only one race, some intended
audience members who were of that race
felt singled out and said the materials
suggested that only members of their racial
group were poor. Careful intended audience
research can help your program identify
messages and images that resonate across
groups—or identify situations in which
different messages or images are likely to
work best.
According to a Center for Substance Abuse
Prevention Technical Assistance Bulletin,
culturally sensitive communications:
58
Developing and Pretesting Concepts, Messages, and Materials

• Acknowledge culture as a predominant educational level, occupation, income
force in shaping behaviors, values, level, and acculturation to mainstream
and institutions
• Reflect and respect the attitudes and
• Understand and reflect the diversity within values of the intended audience; some
cultures. In designing messages that are examples of attitudes and values that are
culturally appropriate, the following interrelated with culture include:
dimensions are important: — Whether the individual or the
— Primary cultural factors linked to race, community is of primary importance
ethnicity, language, nationality, — Accepted roles of men, women,
and religion and children
— Secondary cultural factors linked to — Preferred family structure (nuclear
age, gender, sexual orientation, or extended)
IDENTIFYING MESSAGES THAT RESONATE ACROSS CULTURES
As part of an effort to design messages that are meaningful and appealing to women in
different ethnic groups and to older women, NCI’s Office of Communications conducted
separate focus groups with African-American, American-Indian, Asian, Caucasian, and
Latina women.
The groups tested 10 motivational messages about mammography. Once participants had
individually selected the motivational messages they found most and least persuasive, the
moderator led them in a more detailed discussion of each message’s strengths and
weaknesses. Throughout the discussion, the moderator probed participants’ knowledge,
attitudes, and behaviors concerning breast cancer and mammography, sometimes
exploring underlying motivations and barriers.
Across focus groups, the following message elements were viewed most positively:
• Breast cancer can develop at any time
• All women are at risk—even those age 65 and older, or those without a family history
• Mammograms can detect breast cancer early
• Early detection can save lives
The least persuasive messages made explicit reference to issues that were considered
turnoffs, fear and age. Participants were uncomfortable with messages that specified age
and, in some cases, gender. Many said that cancer was a risk for all people (some pointed
out that men can get breast cancer), stating that older women (i.e., over 40) should not be
singled out. The notion of a mammogram being able to “save your life” was persuasive not
only because it was positive but also because it did not distinguish between age groups. In
general, messages that seemed to tell women what to think were deemed offensive, while
messages that were phrased as explanation or encouragement were more effective.
Note. From Multi-Ethnic Focus Groups to Test Motivational Messages on Mammography and Breast Cancer,
by National Cancer Institute, August 2000. Bethesda, MD. In the public domain.
STAGE 2
Making Health Communication Programs Work
59

— Relative importance of folk wisdom, life
experience, and value of common
sense compared with formal education
and advanced degrees
— Ways that wealth is measured (material
goods, personal relationships)
— Relative value put on different age
groups (youth versus elders)
— Whether people are more comfortable
with traditions or open to new ways
— Favorite and forbidden foods
— Manner of dress and adornment
— Body language, particularly whether
touching or proximity is permitted in
specific situations
• Are based on concepts and materials
developed for and with the involvement of
the intended audience. (Substituting
culturally specific images, spokespeople,
language, or other executional detail is not
sufficient unless the messages have been
tested and found to resonate with the
intended audience. Formative research
with audience members takes on added
CHOOSING MESSAGES FOR YOUNG SENSATION SEEKERS
Research has found that some youth have a preference for novel experiences and stimuli.
Called “sensation seekers,” members of this group have four subcategories that represent
degrees of the characteristic:
1. Thrill- and adventure-seeking (e.g., parachuting and scuba diving)
2. Experience-seeking (e.g., nonconforming lifestyle and musical tastes, drugs,
unconventional friends)
3. Disinhibition (sensation through social stimulation; e.g., parties, social drinking, a
variety of sex partners)
4. Boredom susceptibility (restlessness when things are the same for too long)
Some health communicators working on drug abuse prevention programs have found that
focusing on sensation seekers with messages that appeal to this aspect of their
personalities can be effective in promoting attention to and recall of the message and in
affecting factors such as behavioral intention and attitudes.
For example, a University of Kentucky program designed for adolescents a creative high-
sensation television PSA that focused on the importance of alternatives to substance use
for meeting sensation needs. The PSA, titled “Common,” featured heavy metal music and
quick-action cuts of high-sensation activities. “Wasted,” which had the highest sensation
value, also had heavy metal music and displayed the words “wasted,” “blasted,” “stoned,”
and “fried.” Voice-over and illustrative footage accompanied each word (e.g., “with drugs
you can get fried” had footage of a monk’s self-immolation). It closed with the words
“without drugs you can still get high” and offered examples of high-sensation alternatives.
Note. From “Reaching At-Risk Populations in a Mass Media Drug Abuse Prevention Campaign:
Sensation Seeking as a Targeting Variable,” by P. Palmgreen et al. In Drugs & Society 8(3), pp. 29–45.
1995, Binghamton, NY: Haworth Press. Adapted with permission.
60
Developing and Pretesting Concepts, Messages, and Materials

importance when planners and designers
have different cultural backgrounds than
the intended audience does.)
• Refer to cultural groups using terms that
members of the group prefer (e.g., many
people resent the term “minority” or
“nonwhite.” Preferred terms are often
based on nationality, such as Japanese
or Lakota.)
• Use the language of the intended
audience, carefully developed and tested
with the involvement of the audience
Choosing the Type of Appeal
To capture the intended audience’s
attention, you can scare people, tug at their
hearts, make them laugh, make them feel
good, or give them straight facts. What will
work best? The answer generally depends
on the intended audience’s preferences,
what your program is asking people to do,
and how you plan to use the appeal in
asking them to do it.
Positive emotional appeals show the
benefits intended audience members will
gain when they take the action portrayed in
the message. Research has shown that, in
general, messages that present a major
benefit but do not address any drawbacks
tend to be most appropriate when intended
audience members are already in favor of
an idea or practice. In contrast, messages
that present a major benefit and directly
address any major drawbacks work best
when people are not favorably predisposed.
Humorous appeals can work for simple
messages, especially if most competing
communication is not humorous. The humor
should be appropriate for the health issue
and convey the main message; otherwise,
people tend to remember the joke but not
the message. Also, humorous
messages can become irritating if repeated
too frequently.
Threat (or fear) appeals have been shown to
be effective with two groups. Research has
shown that such appeals tend to be more
effective with “copers” (people who are not
anxious by nature) and “sensation seekers”
(certain youth), and when exposure to the
message is voluntary (picking up a brochure
rather than mandatory attendance at a
substance abuse prevention program).
Research has also shown that, to be
effective, a threat appeal should include:
• A compelling threat of physical or
social harm
• Evidence that the intended audience is
personally vulnerable to the threat
• Solutions that are both easy to perform
(i.e., intended audience members believe
they have the ability to take the action)
and effective (i.e., taking the action will
eliminate the threat)
In general, however, the effectiveness of
threat appeals is widely debated.
The most appropriate type of appeal may
differ from this general guidance,
depending upon gender, age, ethnicity,
severity of the problem, and the intended
audience’s relationship to the problem.
For more information, please consult the
following sources under Selected Readings
at the end of this section: Backer, Rogers,
and Sopory (1992); Goldberg, Fishbein, and
Middlestadt (1997); Kotler and Roberto
(1989); Maibach and Parrott (1995);
Palmgreen et al. (1995); Siegel
and Doner (1998).
STAGE 2
Making Health Communication Programs Work
61

Concept Testing
Once you have defined intended audiences
and communication strategies and have
developed message concepts, testing the
concepts with intended audiences can help
you decide on message appeals (e.g., fear-
arousing versus factual), spokespersons
(e.g., a scientist, public official, or member
of the intended audience), and language
(determined by listening to research
participants’ language). Testing is especially
important if the program deals with a new
issue, because it will help you understand
where the issue fits within the larger
context of the intended audience’s life
and perceptions.
Concept testing will help save your program
time and money because it will identify
CANCER RISK MESSAGE CONCEPT DEVELOPMENT
To provide cancer risk information to the public in ways that it could be readily
understood and used, NCI conducted a series of focus groups to learn what the groups
thought of different methods for communicating about risks. The following insights from
the groups underscored the importance of considering both word usage and presentation
methods when developing message concepts and materials:
• Participants said that they want cancer risk messages to give them hope for preventing
cancer and that risk information is less threatening when written in optimistic terms.
• When faced with “bad news” about cancer risks, they said that they look for why it does
not apply to them.
• They wanted risk messages to address key questions such as “How serious is the risk?”
and “What can be done to reduce or avoid the risk?” as well as explain how and where
to get additional information.
• Word choice also influences how information is perceived; “risk” raises alarm, while
“chance” minimizes it.
• Use of vague or unfamiliar terms (including “fourfold,” “relative risk,” “lifetime risk”)
gives people reason to discount the information.
• Combining brief text and visuals (such as charts, graphs) can increase attention and
understanding.
• Statistical risk information was difficult for many participants to understand;
percentages were more understandable than ratios, but in either case accompanying
explanations of the seriousness of the risk were needed.
• Participants were interested in “the complete picture”—that is, what is known and what
is not yet known about a risk, and what it means for “human beings.”
• The source of risk information colors credibility, with participants saying that they are
less likely to trust the media or a source with a business interest and more likely to trust
risk information supplied by a physician or medical journal.
Note. From How the Public Perceives, Processes, and Interprets Risk Information: Findings from Focus Group
Research with the General Public, by the National Cancer Institute, June 1998. In the public domain.
62
Developing and Pretesting Concepts, Messages, and Materials

which messages work best with intended
audiences. Use concept testing to identify:
• Which concept has the strongest appeal
and potential for effect
• Confusing terms or concepts
• Language used by the intended audience
• Weaker concepts that should
be eliminated
• New concepts
Concepts can be presented in a number
of ways. The key is to convey the major
characteristics of the appeal along with the
action your program wants intended
audience members to take and the benefit
they will receive as a result. Focus groups
or in-depth interviews are most appropriate
for concept testing because they permit
discovery of:
• How an intended audience thinks about
an issue
• How its members react to different
appeals or aspects of a message concept
• Why they react that way
Message concept tests often ask
participants to rank a group of concepts
from most to least compelling and then to
explain their rankings. Participants then
discuss benefits and problems associated
with each concept. Health communicators
often use a sentence or brief paragraph to
describe a concept to participants. For
example, the following are two “don’t smoke”
concepts for teens:
1. Smoking harms your appearance.
2. Cigarette advertisers have created a myth
that smoking makes a person more
attractive. They’re lying.
While both concepts address attractiveness,
the first concept uses it as the focal point of
a negative appeal (to avoid becoming less
attractive, don’t smoke), whereas the
second concept uses a factual approach
and a different benefit—avoid being
manipulated by the tobacco industry—
designed to appeal to teens’ strong desire
not to be manipulated.
In each of the concepts above, both the
action the intended audience members
should take and the benefit are implied, not
stated. This approach works in situations
where the desired behavior is obvious. In
other situations, the behavior or the benefit
will need to be mentioned, as in the
following examples:
• Mammograms detect breast cancer long
before a lump can be felt. And finding it
early can save your life
• If you’re concerned about getting breast
cancer, getting a mammogram may give
you peace of mind
More detail on the structure of a concept
test is provided later in this section under
Conducting Concept Tests and Materials
Pretests and in the Communication
Research Methods section.
3. Decide What Materials to Develop
Once you have message concepts that are
effective with the intended audience,
determine the material formats (e.g.,
brochure, videotape) that will best suit your
program by evaluating:
• The nature of the message (e.g., its
complexity, sensitivity, style)
• The function of the message (e.g., to
call attention to an issue or to teach a
new skill)
STAGE 2
Making Health Communication Programs Work
63

HEALTH COMMUNICATION MATERIALS OPTIONS
Interpersonal Channels
• Fact sheet with a list of questions for patients to ask health care providers
• Physician pads for patient counseling (similar to prescription pads, but used to
provide information)
• Slides and a script to assist presenters
• How-to booklets and talking points for discussions in private homes or within
the family
• Videos to trigger discussion
• Telephone information service scripts and responses
• Tailored communications, such as letters or personalized newsletters (see page 71)
Organizational Channels
• Newsletters
• Educational programs (in-person, audiovisual, computerized, print)
• Speeches
• Tailored letters to members
• In-house radio or video broadcasts
• Kiosks/displays
• Buttons, refrigerator magnets, or other giveaways
• Add-ons to regular communication (e.g., messages handed out with paychecks or
organization notices)
• Event banners, flyers, stickers, buttons
• Conference exhibits, presentation slides
• Spokesperson training materials
Community Channels
• Displays for beauty and barber shops, pharmacies, grocery stores, airports, libraries,
transit, and other public venues
• Posters
• Inserts with bills, in or on shopping bags
• Community newsletters
• Health fair exhibits and handouts
• Letters, e-mail to organize community response
• Kiosks in shopping malls, post offices
• Handouts for meetings with community leaders, lawmakers
• Spokesperson training materials
Mass Media Channels
• Audio or video news releases or B-roll
• Cartoons/comics
• Direct-mail letters, brochures
• Photonovellas
• Magazine and newspaper articles
Continued on next page...
64
Developing and Pretesting Concepts, Messages, and Materials

HEALTH COMMUNICATION MATERIALS OPTIONS CONTINUED...
• Newspaper inserts
• Media kits
• Music news releases/music videos
• Op-eds or letters to the editor
• Posters
• Radio, TV, print advertisements (paid or public service)
• Radio or TV programming
Interactive Digital Media Channels
• Ads on Web sites
• E-mail messages
• CD-ROMs
• Interactive quiz or game on Web site
STAGE 2
• The activities and channels selected
during Stage 1 (e.g., whether you will be
most likely to reach the intended audience
through a school, library, physician, the
media, or a combination of these)
• The budget and other available resources
Most important: Make sure that your
program’s decisions about materials fit
with the activities and channels you selected
and will contribute to reaching the
communication objectives developed
in Stage 1.
If your program has to develop new
materials, doing so will probably represent
a major expenditure. Make sure to choose
formats that your program can afford; don’t
allot so much of your budget to materials
production that you can’t afford sufficient
quantities, distribution promotion support,
or process evaluation. The list of materials
options below will give you ideas of
possible approaches. Don’t stop there; use
your knowledge of the intended audience
to combine, adapt, and devise new ways
to get the message across. Explore your
program’s preliminary decisions about
materials with the intended audience
or partners, perhaps in conjunction with
getting reactions to message concepts.
4. Develop Messages and Materials
The following guidelines will help your
program develop materials that intended
audiences understand, accept, and use:
• Ensure the message is accurate:
— Scientific accuracy is vital to producing
desired outcomes and to your
program’s credibility. This is particularly
important because of rapid changes in
advice and information for many health
topics; often, what is accurate one year
is no longer current the next. For this
reason, experts on the health topic
should always review your program’s
messages. However, you may have to
work with them to get them to accept
language that is simple enough for a
nonscientific intended audience to
understand. At times it may be helpful
to share pretest results with them or
Making Health Communication Programs Work
65
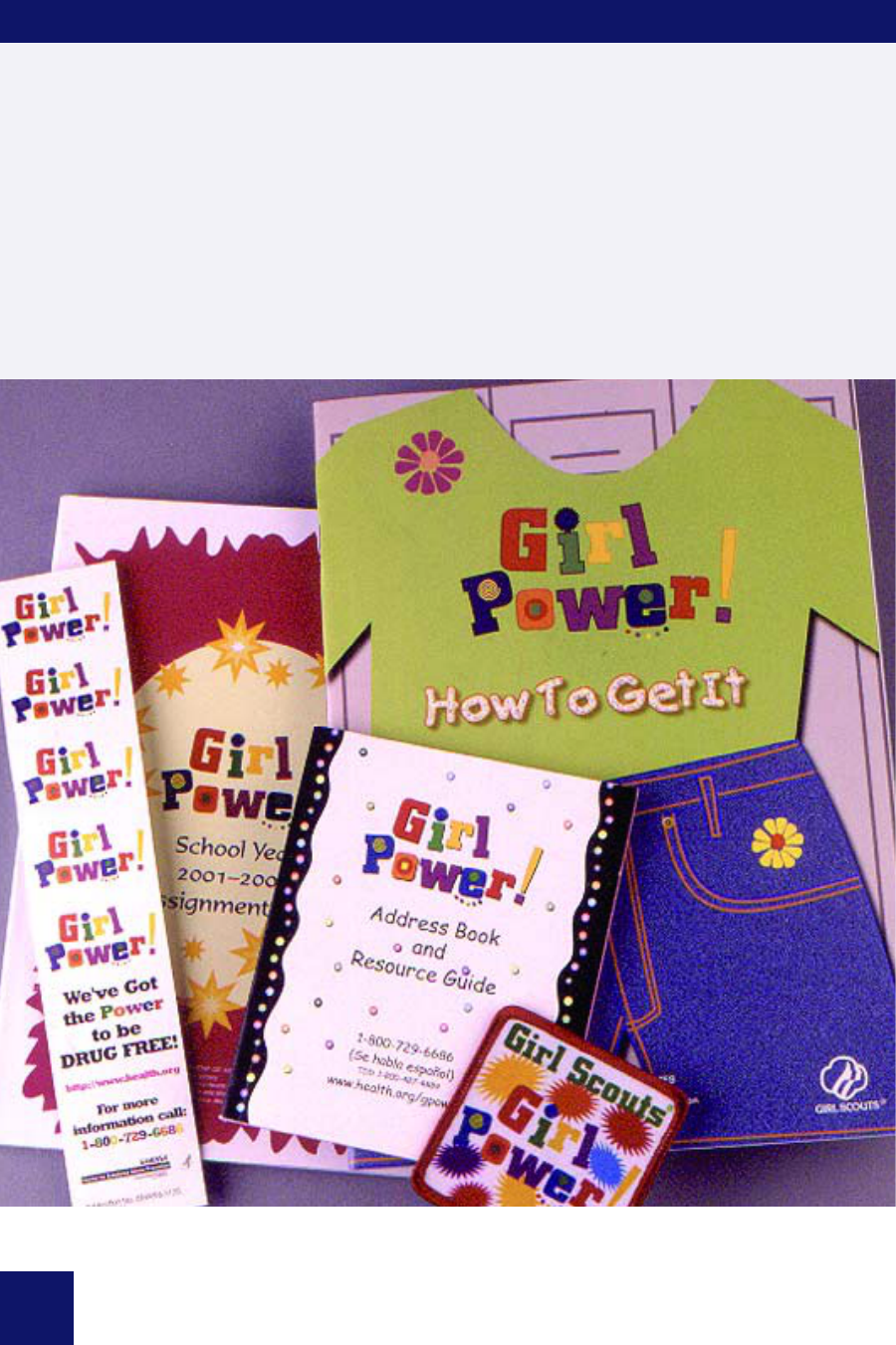
PATCHES: AN INNOVATIVE FORMAT TO REACH GIRLS
The Department of Health and Human Services, Substance Abuse and Mental Health
Services Administration’s Center for Substance Abuse Prevention’s Girl Power! campaign
partnered with the Girl Scouts of the USA to develop a Girl Power! Girl Scout patch
program. Girl Power!, a national public health education program, addresses a wide range
of issues affecting adolescent girls. The overall goal of Girl Power! is to delay and reduce
the use of alcohol, tobacco, and illicit drugs among girls ages 9–14. This program also
addresses related issues such as physical activity, nutrition, and mental health. Girl Power!
and the Girl Scouts cooperate in an ongoing relationship. Through the Girl Scouts, the
Center for Substance Abuse Prevention’s Girl Power! campaign materials are distributed to
over 2.8 million girls around the country. To see other formats both groups use to reach
girls, visit www.girlpower.gov or jfg.girlscouts.org.
66
Developing and Pretesting Concepts, Messages, and Materials

PRESENTATION OPTIONS FOR ADVERTISING AND AUDIOVISUAL MATERIALS
Animation—Use for young children and as an eye-catching approach for adults (older
children may consider some animation silly or “babyish”). Use animation to demonstrate
desired actions or to address abstract subjects (e.g., respite care), sensitive subjects (like
AIDS), or several disparate intended audiences (e.g., different ethnic groups) at once.
Demonstrations—Use an audiovisual format to demonstrate the desired health behavior,
especially if your program must teach skills.
Slice of life—Use a dramatization within an “everyday” or familiar setting to help the
intended audience relate to the message. A simple story is easy to remember; you might
choose to present the health problem and show the solution. This style can be both
credible and memorable, but it may not work with all intended audiences.
Testimonials—Use a credible presenter to lend credibility to the message. A recognizable
spokesperson may be attention grabbing. The most credible and relevant presenter may
vary for different intended audiences and may be an intended audience representative,
an authority (e.g., a physician), or a celebrity connected with the health issue.
STAGE 2
get them to sit in on research with the
intended audience so that they are
exposed to the intended audience’s
level of knowledge and
scientific sophistication.
• Be consistent:
— All messages in all materials and
activities should reinforce one another
and follow the communication strategy.
No matter how creative, compelling, or
wonderful a message is, if it does not fit
the strategy statement, objectives, and
identified intended audiences, throw it
out. Don’t compete with your own
campaign for attention.
— Recognize inconsistencies between the
message and what the intended
audience may have heard from other
sources due to controversies among
scientists, government agencies, and
advocacy groups. The best way to
determine whether and how to address
such inconsistencies is to ask the
intended audience what impact the
disparities have on them and what they
need from your program to make
decisions and take the desired action.
— Use the same graphic identity in all
campaign elements. In print materials,
use the same or compatible colors,
types of illustrations, and typefaces
throughout the campaign. If there is a
logo or theme, use it in all materials.
Graphics and messages should
reinforce each other, not send
different signals.
• Be clear:
— Keep it simple. Clear messages for lay
intended audiences contain as few
technical/scientific/bureaucratic terms
as possible and eliminate information
that the audience does not need in
order to make necessary decisions or
take desired actions (such as overly
detailed background about disease
physiology, research uncertainties, or
Making Health Communication Programs Work
67

68
background about your organization).
Readability tests (see the
Communication Research Methods
section for instructions and limitations)
can help determine the reading level
required to understand material and
can help writers be conscientious
about the careful selection of words
and phrases.
— Prominently feature the action you want
the intended audience to take. Give
people an explicit recommendation of
what you want them to do as a result of
the message. Don’t assume they will
figure it out for themselves. For
example, pretesting showed that a
brochure about taking part in AIDS
research studies was very well received
by a grateful and emotional intended
audience. However, no one recognized
that the purpose of the booklet was to
encourage people to consider
participating in research studies and to
talk about it with their health care
providers. Instead, almost everyone
thought the purpose was to give them
hope and comfort. The booklet was
revised to be more straightforward
without compromising the hopeful tone
intended audiences liked.
— Demonstrate the health behavior or
skills (if appropriate).
• Be relevant to the intended audience:
— Include incentives for the intended
audience to take the recommended
steps, beyond the health benefits they
will receive. Audience research will
help you understand what the intended
audience might value. Incentives may
be psychological (you’ll feel more in
control); altruistic (you’ll help others by
participating in a research study);
economic (not smoking saves
money); social (exercise is a fun
group activity, where you can make
friends, see friends); family-driven

(do it for them); or ego-driven (sun
exposure causes wrinkles).
— Choose a presentation style
appropriate to the intended audience’s
norms and expectations; people must
be able to see themselves in what your
program presents. For example,
intended audience preferences can
help determine whether to take a
rational or emotional approach, a
serious or light tone. Use a light,
humorous approach if appropriate, but
pretest to be sure that it works and
doesn’t offend the intended audience.
Responses to humor vary greatly.
— Keep regional differences in mind. A
lush, green park will not look like the
Southwest and an urban clinic will not
be familiar to people who live in a rural
area. The organization of the health
care system and the way medical and
social services agencies work together
also differ from region to region.
— Use intended audience experience
when creating materials. The intended
audience will learn new information
more easily when you build from the
familiar to the unfamiliar (e.g., “When
you have a headache that won’t go
away, you take an aspirin to relieve it.
But that is not the best way to control
cancer pain. Cancer pain medicines
work best if you take them before
your pain becomes severe and keep
taking them on the schedule your
doctors advise.”)
— Create the message to match the
readiness of the intended audience to
make a change. The Stages of Change
model (see Appendix B) describes five
stages that people pass through in
making behavior changes:
precontemplation, contemplation,
preparation, action, and maintenance.
Messages created to match readiness
to change start where the intended
audience starts. For example, it is
unrealistic to expect an intended
audience that has never heard of the
problem to immediately make changes.
A realistic outcome is beginning to
raise awareness of the issue
(precontemplation) and helping move
the intended audience to a consideration
of the change (contemplation).
• Be credible:
— Use celebrity spokespeople selectively.
Choose celebrity spokespeople who
are directly associated with the
message (e.g., using an athlete to
promote exercise or cancer survivor to
promote early detection) and who
practice the desired health habit. Check
with the intended audience about the
suitability of the celebrity. (For example,
while a famous television personality
was well liked by members of the
intended audience for a physical
activity promotion program, they said
she was not relevant to them because
she could afford a personal trainer to
make exercise easier.) Realize that
while celebrities can help gain attention
for the message, they may also
compete with the message for attention
or be unappealing to some intended
audiences. In addition, your program
will probably need to build its schedule
around theirs, and celebrity
involvement can cause production
delays and extra costs. Caution: A
network may not use TV PSAs
featuring a rival network’s star.
— Be sure that the person who presents
the message is seen as a credible
source of information, whether as an
authority, celebrity, or intended
audience representative.You may also
want to partner with organizations that
are credible with the intended audience
and emphasize their involvement. If the
message involves health services and
STAGE 2
Making Health Communication Programs Work
69

TIPS FOR DEVELOPING TV ADS
General
• Keep messages short and simple—just one or two key points.
• Use language and style appropriate for the intended audience.
• Repeat the main message as many times as possible.
• Recommend a specific action.
• Demonstrate the health problem, behavior, or skill (if relevant).
• Provide new, accurate, straightforward information.
• Be sure the message, language, and style are considered relevant by the
intended audience.
• Be sure that the message presenter is seen as a credible source of information, whether
an authority, celebrity, or intended audience representative.
Development
• Select an appropriate approach (e.g., testimonial, demonstration, or slice-of-life format).
• Be sure every word works.
• Use a memorable slogan, theme, music, or sound effects to aid recall.
• Check for consistency with campaign messages in other media formats.
Appeal
• Use positive rather than negative appeals.
• Emphasize the solution as well as the problem.
• Use a light, humorous approach, if appropriate, but pretest to be sure that it works and
doesn’t offend the intended audience.
• Avoid high degrees of fear arousal, unless the fear is easily resolved and the message is
carefully tested.
Visuals
• Use only a few characters.
• Make the message understandable from the visual portrayal alone.
• Superimpose text on the screen to reinforce the oral message’s main point.
Timing
• Identify the main issue in the first 10 seconds in an attention-getting way.
• Use 30-second spots to present and repeat the complete message; use 10-second spots
only for reminders.
• If the action is to call, show the phone number on the screen for at least 5 seconds, and
reinforce orally.
• Summarize or repeat the main point/message at the close.
70
Developing and Pretesting Concepts, Messages, and Materials

health care coverage, it is particularly
pitching a news story or producing an
important to have a source that the
intended audience believes is
unbiased, i.e., does not have a vested
(profit-driven) interest in people taking
the recommended action. For example,
consumers may dismiss health
practices an employer or government
agency suggests they take if they
perceive the motivation is just to save
the organization money.
• Be appealing:
— Produce variations of materials to
appeal to specific intended audience
segments. For example, NCI used
several different covers on a
mammography booklet to appeal to
different cultures. Similarly, audio
materials can be produced using
culturally specific voices or music.
Of course, changing executional detail
to appeal to specific intended audience
segments is appropriate only if the
underlying communication strategy
and messages have been tested with
those audiences.
— Get the intended audience’s attention.
Given the number of health and other
messages intended audiences receive,
yours must stand out to be noticed.
The best way to command attention will
differ among intended audiences. It
can be useful to know what has
interested them before, but concept
testing and message testing will help
ensure that your program’s approach
will grab their interest.
— Produce high quality materials. If you
feel you have to skimp on production,
choose a simpler way of presenting the
message. Producing poor quality
materials wastes funds and can damage
your program’s credibility and your own.
— Entertain while you educate when
using mass media. Whether you are
ad, remember that the mass media are
viewed as a source of information and
entertainment, not education.
Therefore, if the complete message is
too complicated, or simply not
considered interesting enough for use
by the media, redesign the message
so that it is more appealing to media
professionals and their perceptions
about what their intended audience
wants. Working with media professionals
will help ensure that your program’s
messages are interesting as well as
accurate and may help you obtain
greater exposure for the program.
Tailored Communications
Tailored communications are much more
refined than communications created for a
particular intended audience or segment of
the population. If you can tailor each
message for each individual, it is likely to be
even more effective. Tailored
communications are produced for each
person based upon what is known about the
individual. Obtain this information from
health plan data, surveys, medical records,
and other sources. This information permits
matching people with messages appropriate
for them. The following are two examples of
tailored communication:
• A series of letters (e.g., to give smokers
information about and support for quitting)
from which paragraphs are selected to
send to each individual based on past
behavior—on barriers to, for example,
quitting, or on other unique combinations
of characteristics
• A cover letter, referring readers to the
pages of an enclosed booklet that most
relate to their interests and concerns
STAGE 2
Making Health Communication Programs Work
71

With the help of a computer and ordinary
word processing software, individual letters
can be tailored within a mass mailing,
brochures can be printed on demand for
a specific patient, or telephone counselors
can appropriately focus their assistance
and follow up with messages tied to the
advice they gave.
When personal data are not available,
interactive computer programs can prompt
individuals to input key personal
characteristics that direct the software to
prepare individually tailored messages
immediately (e.g., on a Web site or at a
kiosk in a public location). NCI’s 5 A Day
Web site (
www.5aday.gov/ ) allows users to
chart their fruit and vegetable consumption
and exercise and offers positive reinforcement
in response to the behaviors they report.
Evaluation has shown that tailored
communications can, in some
circumstances, increase message effects,
although much research remains to be done
on how and why.
To use tailored communications, review
the planning information from Stage 1
and determine:
• The important individual characteristics
that affect a particular health behavior
(i.e., differences in readiness to change
behavior, or perceived benefits of or
barriers to changing the behavior)
• Appropriate messages tailored to address
individual characteristics (these messages
may be identified or confirmed through
primary research with each group, or
through collaboration with a behavior
change specialist or a subject matter
expert, such as a genetic counselor
or physician)
Then:
• Create a “library” of messages tied to each
relevant characteristic, such as gender or
risk factors (“as a woman who began
smoking in the last five years…”)
• Use word processing software with a mail
merge feature that will match variations in
personal characteristics with appropriate
messages and produce the materials in
the desired format
Tailoring is not always possible or
necessary. However, think about using some
of the principles of personalizing messages
when appropriate and when funding is
available. Find more information about
tailored communications in the Selected
Readings at the end of this section or use
NCI’s quick-start tutorial on the Internet at
http://dino.nci.nih.gov/public/glassman/
TailoringGuide.
Developing Effective Print Materials for
Low-Literacy Intended Audiences
Many intended audiences have a hard time
understanding health materials written in
technical language. This is especially true of
intended audiences with low literacy skills.
Present the message in a more easily
understood way to these intended
audiences by making specific choices about
writing style, vocabulary, typography, layout,
graphics, and color. These choices affect
whether the message is read and how well
intended audiences with low literacy skills
understand it. A great deal of health
information and promotion is organized
around the use of print materials, often
written far beyond the literacy skills of
intended audiences. Differences in the
ability to read and understand materials
related to personal health appear to
contribute to health disparities. The link
72
Developing and Pretesting Concepts, Messages, and Materials

TAILORED COMMUNICATIONS: HEALTHY BIRTHDAYS
In two 1999 projects, researchers designed tailored birthday cards and newsletters to
increase breast and cervical cancer screening and smoking cessation, primarily among
low-income African Americans.
In one study, the cards and newsletters were individually tailored based upon ethnicity,
gender, and the individual’s readiness to change according to the Stages of Change model.
Smokers received either:
• Provider prompting
• Tailored cards and newsletters
• Tailored cards and newsletters and telephone counseling
The tailored cards and newsletters showed a highly significant quitting effect. Thirty-three
percent of smokers who received only the tailored cards and letters quit smoking
compared to thirteen percent of smokers who received provider prompting and
nineteen percent of smokers who received the tailored cards and newsletters and
telephone counseling.
In the other study, people who received the tailored birthday cards and newsletters
showed higher rates of Pap tests and general cancer screening.
Image created by
Bernard Glassman and
Barbara K. Rimer.
All rights reserved.
STAGE 2
Note. From Glassman, B., Rimer, B. K. (1999). “Is There a Use for Tailored Print Communications in
Cancer Risk Communications?” (Monograph of the Journal of the National Cancer Institute, No. 25)
In the public domain.
Making Health Communication Programs Work
73

between literacy and health disparities
underlies the Healthy People 2010 objective
to “improve the health literacy of persons
with inadequate or marginal literacy skills”
(objective 11-2).
A common misconception is that low-literacy
materials are synonymous with low-reading-
level materials. That is, if you avoid
polysyllabic words and long sentences,
you’ve met the need. In fact, low literacy
encompasses more than reading level, and
meeting this need requires that you
complete the same planning and research
steps and adhere to the same fundamental
communication principles that you would
use for any other health communication
material. The difference is that certain
aspects of the process must be done with
particular rigor. The following list includes
pointers for designing materials for low-
literacy intended audiences:
• Include only the information needed to
convey the behavioral objective and
support the intended audience in attaining
it. Strictly limit content because poor
readers struggle with every word, often
reading letter by letter. Keep the piece
short and focused, and let the
communication strategy statement guide
you in answering the question, “From the
many possible information points, which
ones will predispose and enable the
reader to take the desired action?” The
biggest challenge will be excluding
concepts and content points that fall
outside of the category of “information the
reader must know.” Do not include
information just because it may interest
the reader or because you are trying to
promote your organization’s work.
• Organize topics in the order the reader
will use them. Less skilled readers have
particular difficulty connecting topics and
processing the flow of an argument.
• Present the most important points first
and last. Studies show that intended
audiences with limited literacy skills
remember these best.
• Group information into chunks, with a
clear, ordered format. Use steps (1, 2, 3),
chronology (by time of day), or topical
arrangement (main heading,
subheadings), depending on how the
person will use the information.
• Respect the intended audience. This is
especially critical when designing low-
literacy materials. Examples abound of
well-intentioned materials that talk down to
readers or have childlike or simple cartoon
illustrations. The low-literacy population
encompasses people of different ages,
genders, cultures, and socioeconomic
status, including highly intelligent adults
with significant life experience who just
cannot read very skillfully.
• Follow these guidelines.
— Use short sentences and paragraphs.
— Write in the active voice.
— Clarify concepts with examples.
— Avoid jargon, technical terms,
abbreviations, and acronyms.
— Include a glossary if necessary (but
define key words within the sentence).
— Give the reader an action step he or
she can take right away (e.g., call
your clinic, send in a request); this
tends to improve retention of
information and encourages the reader
to begin practicing the desired
behaviors immediately.
— Use graphics and design to make the
reader’s job easier and to increase
comprehension and recall; make sure
they support, rather than compete
with, the text.
— Don’t assume that pictorial signs,
symbols, and charts are more effective
than words for low-literacy intended
audiences. Some experts suggest that
74
Developing and Pretesting Concepts, Messages, and Materials

“universal” symbols, such as a stop
sign, an arrow, or a big black “X,”
usually test well. Don’t confuse this
intended audience with large, busy
matrices—for example, functionally
illiterate individuals have trouble using
a bus schedule.
— Avoid using all capital letters; they are
more difficult for everyone to read,
particularly so for less skilled readers.
— Use captioned illustrations that are
relevant to the subject matter and
model the desired behavior.
— Use headings and subheadings to
convey a message and help reinforce
the flow and content.
— Use bullets and other graphic devices
to highlight key messages and to avoid
large blocks of print.
— Avoid right-justified margins.
• Pretest all materials with the intended
audience. This is absolutely crucial with
low-literacy intended audiences. Writers
and communication specialists are highly
literate by definition. It is impossible for a
person who reads well and has a good
vocabulary to guess what people without
those skills will understand. For example,
an FDA brochure on food safety used the
key message, “Keep hot foods hot, keep
cold foods cold.” Pretesting showed that
low-literacy readers had no idea what they
were supposed to do based on this
message, nor did they understand what
foods fell into the hot and cold categories.
A final note: You will find that most intended
audiences of any reading level prefer
well-produced materials that follow
these guidelines.
Developing Effective Web Sites
A Web site should be graphically appealing
and provide information about health issues
in an informative manner. Some organizations
begin by creating sites that primarily provide
information to their stakeholders, employees,
or members. To extend outreach, create an
additional section in the site to appeal to the
intended audience. For consumers, you
might call this section the Help Center and
provide a place for users to receive
information about a particular health topic,
participate in online surveys, or download
your organization’s consumer information.
Many sites contain useful public health
information and resources, but too often this
information is buried within the site. Keep
visitors interested in the site by making it
easy to navigate.
To ensure that users will find the site well
designed and easy to use, pretest the site
as you would any other materials. Usability
testing, which tests the site to see how well
it helps users meet their goals, is crucial to
creating an effective site. The best time to
do this testing is as you are developing the
site, not after it’s completed. If the site is not
yet running on a computer, test using paper
or poster board mock-ups of pages. Conduct
usability testing by having people who
represent the intended audience actually sit
down and use the site to complete tasks,
either by themselves or in pairs. Observe
how they interact with the site and ask
specific questions once they have
completed the tasks.
Their experiences and responses will allow
you to improve the site before it is used. If
you make major modifications to the site
after usability testing, test again before the
site goes live. For more information on
usability testing, see
www.usability.gov.
Remember, your well-designed and
attractive site is useless unless people know
it exists. Therefore, consider launching a
Web site by conducting both traditional and
online media outreach. Online outreach can
include alerting search engines such as
STAGE 2
Making Health Communication Programs Work
75

CHARACTERISTICS OF WELL-DESIGNED WEB SITES
• Compliant with W3C accessibility guidelines (www.w3.org/wai), which ensure access to
the Web by everyone regardless of disability, and, for government publications, Section
508 guidelines (www.usability.gov/accessibility)
• Clean and consistent design (e.g., a simple background, legible type, a few carefully
selected colors)
• A search engine (program that helps users find information) and a link to the search
engine on all Web pages
• Fast display of graphics and text
• Clear and consistent navigation elements (to make it easy for users to move to and from
different information sources)
• Interactivity and fun elements
• Short/concise pages (e.g., a Web page should not exceed 250 words on average)
• Compatibility with major browsers and earlier versions of major browsers (e.g.,
Netscape, Microsoft Internet Explorer)
• Mechanisms to track site usage and invite user response
76
Developing and Pretesting Concepts, Messages, and Materials

Google or Yahoo about the site as well as
selecting publications that specialize in
online issues or exist only online.
5. Pretest Messages and Materials
Although working with advisory groups and
gatekeepers can add useful input for
developing intended audience-appropriate
materials, only testing with members of the
intended audience will tell you what their
reactions might be. It is always better to
conduct research with intended audience
members than to do without it, especially
with audiences that you do not know well
(e.g., cultural groups other than your own) or
whose education or skill levels are different
from yours (e.g., audiences with limited
literacy skills). When resources are an issue,
use lower cost methods and money-saving
strategies to keep costs down (see sidebar,
Keeping Pretest Costs Down, page 85).
Pretest preproduction draft materials.
Testing at this stage permits you to identify
flaws before spending money on final
production. To test materials in draft form,
use a facsimile version of a poster or
pamphlet, a video version of a television
PSA, or a prototype of text materials like a
booklet. Test these materials with members
of the intended audience to accomplish
the following:
• Assess comprehensibility—Does the
intended audience understand
the message?
• Identify strong and weak points—What
parts of the materials are doing their job
best—for example, attract attention,
inform, or motivate to act? What parts are
not doing their jobs?
• Determine personal relevance—Does
the intended audience identify with
the materials?
• Gauge confusing, sensitive, or
controversial elements—Does the
treatment of particular topics make the
intended audience uncomfortable?
A Review Process Adds Value
As you test materials in rough form with the
intended audience, it is also valuable to
obtain gatekeeper or other reviewer
comments. Health communicators often ask
gatekeepers (e.g., public service directors,
physicians, teachers, partner organization
leaders) to review materials both to get input
from people close to the intended audience
and to increase the likelihood that the
gatekeepers will use the materials with the
audience. If the graphics style or illustrations
depart from what gatekeepers or other
reviewers expect, focus on these issues
when testing draft products with the
intended audience. Use favorable responses
from the intended audience to persuade
gatekeepers to accept your program’s
approach. Gatekeeper review should not be
used as a substitute for pretesting materials
with members of the intended audience.
Many organizations have established review
procedures that can seem like hurdles to
timely production of materials. However,
reviewers can potentially add value, and
review by some experts can be imperative
for producing accurate, accepted
communication materials. Reviewers will
help create accurate documents for
pretesting. After pretesting, reviewers can
help synthesize the results and help with
revising the document. The following tips
will help you structure a value-added
review process:
• Choose reviewers carefully. Reviewers
should have relevant knowledge to
contribute and be conscientious enough
not to delay the process. Make sure there
STAGE 2
Making Health Communication Programs Work
77

PREFINISHED MATERIALS: FORMATS FOR PRETESTING
Print (e.g., paper-based)—It is best to test a complete prototype of the final material—for
example, the text, layout, typeface, and visuals—that is planned for the final piece. If the
test is conducted prior to commissioning original photography or artwork, stock
photography or drawings can be used. For longer pieces (e.g., booklets), try to avoid
testing text in manuscript form. Word-processing software makes it very easy to put the
text into the intended layout, and testing a prototype instead of a manuscript will allow
you to more accurately assess comprehensibility rather than assuming it will improve
once the text is laid out.
Audio (e.g., radio)—Even if you will have a script rather than a final recording, it is best
to produce and test a “scratch tape” so that every pretest respondent hears and reacts to
the same thing.
Video (e.g., PSAs)—Storyboards (line drawings showing key scenes, like a comic strip),
even if they are videotaped with a voice-over or soundtrack, are too rudimentary for
testing to be able to predict reactions to the final product. More useful formats are:
• Animatics (a series of detailed drawings, filmed in rapid succession and using camera
zooms and pans to give the illusion of motion)
• Photomatics (similar to animatics, but using a series of photos)
• Rough live action (filmed footage, with costs controlled by using nonunion talent and
simplified sets)
• “Ripomatics” (adaptations or alterations of existing footage to create a new
video product)
Interactive (e.g., Web, CD-ROM)—The site or program should be complete enough to
allow basic functionality and design to be assessed (e.g., does the site or program include
the information intended audience members want? Is it organized in such a way that they
can easily find it?).
is a range of expertise represented among when a top administrator was given
the reviewers, including subject experts, camera-ready layouts for his final
communication specialists, intended approval, and he wrote comments on
audience experts/representatives, and them. Reviewers are commonly handed
those who understand your organization materials without guidance; they may not
and your partners’ policies and priorities. understand the purpose or the context of
In some cases, reviewers with other skills the material and have no way of knowing
or viewpoints may be important, such as what you want from them. Often this
legal professionals, law enforcement results in reviewers’ simply tinkering with
officials, social workers, school personnel, words or proofreading the copy, delaying
or clergy. the process without adding value. Instead,
• Explain exactly what you want reviewers
give them a list of questions to answer or
to do and not to do. One organization’s
other guidance.
national campaign materials were delayed
78
Developing and Pretesting Concepts, Messages, and Materials

• Never skip technical review by an expert,
who may catch concerns or inaccuracies
others miss. For example, the facts you
present may be accurate but not reflect
new information that only an expert
would know.
• Incorporate as many comments as
possible.You may need to get clarification
on some comments or to talk with reviewers
whose comments seem off base.You may
find that you can compromise, but
remember you are not required to act on
all the comments you receive.
• Allow sufficient time in the development
process to deal with reviewers’ comments.
This includes giving reviewers enough time
to do a thorough job and giving creative
professionals enough time to make
revisions thoughtfully and carefully.
Conducting Concept Tests and
Materials Pretests
To plan and conduct concept tests and
materials pretesting, complete the
following steps:
1. Determine test objectives.
2. Choose methods.
3. Secure vendors, facilities, and moderators
or interviewers (if required).
4. Identify, screen, and recruit respondents.
5. Draft test instruments (discussion guides,
questionnaires).
6. Conduct pretesting.
7. Analyze results.
8. Make the best use of results.
Key aspects of each step are presented
below; see the Communication Research
Methods section for more detail.
Determine Test Objectives
The first step in planning pretesting is to
formulate research objectives. Write specific
objectives to provide a clear understanding of
what you want to learn from whom. Pretesting
can also help to answer questions about
alternate ways to present information,
questionable inclusions or depictions, and
reviewer conflicts regarding content, format,
and appearance.
Develop a description of which segments of
the intended audience you want to include
and exclude in testing. Do you want to include
individuals who have attempted a particular
health behavior and succeeded? Failed? Ever
thought of trying? Consider excluding
individuals whose professions may make
them too experienced with the topic or the
method (e.g., health professionals, market
researchers, employees of advertising
agencies, or public relations firms). In some
instances, exclude consumers whose past
experience makes them too knowledgeable.
For example, sometimes people with a
PROVIDING GUIDANCE TO REVIEWERS
NCI sends memos to reviewers with
each set of materials. The memo
outlines:
• Questions to answer, specific points to
check, or issues for reviewer to address
• The purpose, objectives, and intended
audience for the materials
• A history of how and why the product
was developed and who has already
contributed to or reviewed it
For example, the reviewers for this
book received instructions and
worksheets to help focus their input,
and not all reviewers were asked to
comment on all topics; they were
expected instead to focus on sections
related to their expertise.
STAGE 2
Making Health Communication Programs Work
79

BENEFITS AND LIMITATIONS OF PRETESTING
Benefits
Examples of benefits derived from pretests include:
• Assess attention. Central location intercept interviews conducted by the National Heart,
Lung, and Blood Institute showed that using symbols/analogies was a promising way to
gain attention and to convey a message. However, the message itself must be fairly
simple, or the use of an analogy becomes a complicating liability. For example, using a
freeze frame and reverse action to “reverse” the risk of high blood pressure was attention
getting, but no analogies for multiple risk factor messages proved straightforward
enough to work successfully.
• Assess comprehensibility. When developing the USDA food pyramid, extensive pretesting
revealed that the pyramid shape conveyed key concepts more clearly than a bowl or
other shapes. In addition, planners learned that representing fats, oils, and sugars as a
bottle of salad dressing, a can of soda, and a bowl of sugar created widespread
misunderstanding. Substituting a stick of butter, a droplet of oil, and a spoonful of sugar
improved comprehension.
• Assess motivation. Research conducted for the National Bone Health Campaign, Powerful
Bones, Powerful Girls™, explored campaign concepts designed to increase calcium
consumption and weight-bearing physical activity among 9- to 12-year-old girls. Girls
identified strength—in the form of self-confidence and physical strength—as a key
benefit of bone-healthy behaviors. The campaign theme, “Powerful Bones, Powerful
Girls,” was perceived as motivating, as were examples set in real-world settings and
during social activities.
• Assess recall. In a test of a booklet on lung cancer, patients could recall on average 2 out
of 12 ideas presented; half the patients could recall none. Too many technical terms, the
density of concepts, and too little differentiation between diagnostic and treatment
procedures inhibited intended audience recall. Another problem was the inclusion of
concepts unimportant to readers. Although they wanted more information on outcomes
and treatment, they had no interest in a description of the disease.
• Determine personal relevance. When the National Bone Health Campaign research team
explored the credibility of a spokesperson among girls 9–12 years old, the intended
audience wanted to hear from “a girl like me.” Girls said they wanted to hear the
message from a female who was strong, bold, confident, active, healthy, and popular.
This guided the development of Carla, a cartoon spokes-character whose name means
strong. Carla speaks to girls as a peer working to build powerful bones. In the pretesting
of a Web site featuring Carla, girls from varied backgrounds described her as “powerful,”
“fun,” “busy like girls I know,” and “someone who feels good about herself”—someone
they'd like to know and be like.
Continued on next page...
80
Developing and Pretesting Concepts, Messages, and Materials

BENEFITS AND LIMITATIONS OF PRETESTING CONTINUED...
• Gauge cultural appropriateness. Pretesting and revising were critical to developing the
“¡Mírame! Look at Me!” curriculum to help South Texas Hispanic youth ages 9–13 avoid
alcohol, tobacco, and drug use. The research found that this intended audience learned
best with active learning strategies and interpersonal interaction, which influenced
curriculum format revision. Testing also found that the language used (typical of South
Texas conversations, 85 percent English, 15 percent Spanish) was appropriate and easily
understood and that using intended audience representatives telling their own stories
ensured credibility and close audience attention.
• Identify strong and weak points. Pretests of an NCI booklet, “Cancer Research Studies with
Patients: What You Need to Know,” found that patients and family members were
enthusiastic about the format, comprehensibility, approach (enabling patients to take an
active role in decisions about their cancer care), and relevance of the book to patients’
needs and situations. Participants’ comments led to suggestions for strengthening
sections on treatment costs and insurance and adding specific questions to the list
patients should ask before agreeing to take part in a research study. In addition, pretests
provided useful feedback that allowed NCI to improve graphics portraying complex
concepts such as randomization and control groups.
• Identify sensitive or controversial elements. Would using vernacular language to discuss
diarrhea in a booklet on chemotherapy for a low-literacy intended audience be
preferable to a more technical approach? Pretest results showed that the intended
audience found the vernacular offensive and preferred the technical discussion, even
though it had a higher reading level.
Limitations
• A pretest is only as objective as the person designing and interpreting the study.
• Pretesting cannot absolutely predict or guarantee learning, persuasion, behavior change,
or other measures of communication effectiveness.
• Pretesting is not statistically precise. It will not reveal that booklet A is 2.5 percent better
than booklet B. (Presumably, pretests of such precision could be applied, but the cost of
obtaining such data would be high, and the findings may be no more useful than those
from more affordable approaches.)
• Pretesting is not a substitute for experienced judgment. Rather, it can provide additional
information to help guide sound decisions.
• Pretesting does not guarantee success. Good planning, thorough concept exploration,
and sound pretesting can be negated by mistakes in final production or in program
implementation. The message in a television PSA on cancer treatment, for instance,
may pretest well, but then be flawed by an execution that uses an actress who seems
too happy to be awaiting the results of a biopsy report. Similarly, leaflet copy that
pretests well may be rendered ineffective by a poor layout, hard-to-read type, or
inappropriate illustrations.
STAGE 2
Making Health Communication Programs Work
81

82

chronic disease know too much about the
condition to objectively assess materials
designed for patients recently diagnosed.
Don’t rely on these participants for creative
guidance. They are expert consumers, and it
is important to learn their preferences. They
are not, however, communication or creative
professionals, and their ideas for substantive
message or materials changes are likely to
be off the mark.
Choose Methods
A variety of research methods can and
should be used to explore message
concepts and test messages and materials.
Which you choose depends on the research
questions you want to have answered, the
nature of the materials, the intended
audience, and the amount of time and
resources available for pretesting.
The following is a list of methods to use to
test materials:
• Concept testing with intended-
audience members
— Focus groups (face-to-face
or telephone)
— In-depth interviews
• Pretesting with intended-
audience members
— Self-administered
surveys/questionnaires (by mail,
handout, or computer)
— Interviewer-administered
surveys/questionnaires (by telephone,
through central-location intercepts, or
other face-to-face scenarios)
— Theater testing (large groups respond
to messages via questionnaire
or electronic)
— Observational studies (e.g., observing
behaviors of shoppers in a store or
patients waiting in a clinic)
• Other assessment methods
— Readability assessments
— Expert/gatekeeper review
Sometimes, using several methods in
combination will help overcome the
limitations of individual methods. For
example, readability testing should be used
as a first step in assessing draft
manuscripts, followed by self-administered
questionnaires or interviews or, for some
long documents, a combination of the two
with intended audience respondents.
Central-location intercept interviews for
short audio, video, or print materials permit
contact with larger numbers of intended
audience respondents, which is especially
useful prior to final production of materials.
See the Communication Research Methods
section for definitions of commonly used
pretesting methods and descriptions of the
pros and cons and common uses of each.
Secure Vendors, Facilities, and
Moderators or Interviewers
Some research methods require securing
appropriate facilities. If you are using
commercial facilities (e.g., for focus groups,
central-location intercept interviews, or
theater tests), the American Marketing
Association’s New York Chapter’s Green
Book provides an extensive directory of
vendors, indexed by geographic locations
and services offered. The Communication
Research Methods section provides tips for
working with vendors and for securing
alternative facilities if location or budget
precludes using a vendor. The following are
vendor services your program may need:
• Teleconference services to set up
telephone focus groups. Most allow
observers to listen without being heard,
and some provide remote viewing programs
to allow the moderator to see a list of
participants (with a symbol next to the
STAGE 2
Making Health Communication Programs Work
83

name of the one currently speaking) or Draft Test Instruments (Discussion
notes sent by a technician from observers
Guides, Questionnaires)
listening to the call. Some teleconference
services can recruit participants; with others,
recruit or contract with a recruiter separately.
• Focus group facilities to recruit participants
that also offer audio and video recording
equipment as well as one-way mirrors with
observation rooms for viewing both focus
groups and in-depth interviews. These are
usually available only in larger
metropolitan areas.
• Commercial facilities to conduct central-
location intercepts at shopping malls.You
can also use other facilities or public
locations that attract a large number of
pedestrians (e.g., other stores, train
stations, university campuses, large
medical centers); usually permission is
required to interview people in these
types of locations.
If you are conducting focus groups or in-
depth interviews, identify trained,
experienced moderators or interviewers. If
your organization has no experience in such
studies, consider hiring a good, experienced
moderator or interviewer to conduct the
project or to train internal staff to develop in-
house skills. Local advertising agencies, the
American Marketing Association’s Focus
Group Directory, the Qualitative Research
Consultants Association, or other health
communication program managers may
be of assistance in identifying a good
moderator. Before choosing a moderator or
interviewer, ask for and check references.
Identify, Screen, and Recruit Respondents
Use the intended audience description
developed in Stage 1 to draft questions for
recruiters to use to identify participants. See
Appendix A for a sample form to use to
screen potential participants.
Involve the creative team in developing the
discussion guides or questionnaires. The
team will often have specific issues or
questions. Assess how much the intended
audience likes each set of material, because
research has found this to be a leading
indicator of success. Other specific
questions should be used to identify
strengths and weaknesses in rough
messages and materials. See Appendix A
for a sample focus group moderator’s guide
and an intercept questionnaire.
Conduct Testing
If possible, have other team members, such
as creative professionals, content experts,
partners, and gatekeepers (including
decision-makers who control your program),
observe at least some of the focus groups or
interviews. Creative professionals’
observations are particularly important
during concept exploration, because they
often spot comments or trends important for
creative development. Hearing the
responses improves team members’
understanding of intended audience
reactions and can illustrate, more vividly
than any report, the need for simple
language or the power of a particular
creative approach.
Analyze Results
To analyze and communicate the results of
materials testing, write a report outlining the
process and the findings. The report should
include the following sections:
• Background—Who was tested? Why?
How? What did you hope to learn?
(Describe each in detail.)
• Highlights—Summarize the main points
that emerged from testing that answer the
research questions.
84
Developing and Pretesting Concepts, Messages, and Materials

KEEPING PRETEST COSTS DOWN
Use the following tips to keep pretest
costs down:
• Borrow questions from other pretests
when possible.
• Work with partner organizations to
recruit participants and conduct tests
(e.g., an African-American church,
patient educators, a clinic).
• Pay for and use transcripts when you
conduct focus groups so that you can
review the results and make your own
decisions rather than paying an
analyst to do so.
• When testing with a large number
of respondents:
—Keep the questions short and to the
point.
—Use as many close-ended or
multiple choice questions
as possible (for easier
tabulation analysis).
—Develop codes in advance for
quantifying responses to open-
ended questions.
• Avoid overtesting (test to answer
questions, not to gather the view of
a large number of respondents).
• Findings—Present a complete report of
findings. Where appropriate, describe
participants’ reactions, quote participants,
and use examples from the test
documents to support the findings.
• Conclusions—Describe patterns that
emerged or significant differences
observed between groups. (If no patterns
are apparent, more research may
be needed.)
• Recommendations—Suggest revisions for
materials or planned approaches based
on findings and conclusions.
• Appendixes—Include copies of test
instruments used, such as discussion
guides, screening questions,
and questionnaires.
Decide who should prepare the report.
Ideally, choose a team member with a
background in market research and health
communication, and have that person
include input from the creative team on
recommendations. If such a person is not
available, whoever conducted the test may
be able to prepare a basic report on the
findings but, depending on his or her
background, this person may not be able to
draft useful recommendations. Before
relying on vendors to write reports, ask to
see samples of reports they’ve written for
other clients.
One problem that can arise in pretesting
concerns interpretation of respondent
reactions to a sensitive or emotional subject
such as breast cancer or AIDS.
Respondents may become unusually
rational when reacting to such pretest
materials and cover up their true concerns,
feelings, and behavior. Therefore, the
pretester must examine and interpret
responses carefully.
The following are some tips for using
pretest results:
• Involve the creative professionals who
designed the materials in recommending
creative solutions or revisions, rather than
expecting researchers to make
recommendations that creative
professionals may later legitimately reject.
• Consider pretesting again if your program
has made major changes to a message or
product based on the original pretest
conclusions.You may have addressed the
right problems, but you can’t be sure the
STAGE 2
Making Health Communication Programs Work
85

new solutions will be effective without
intended audience testing. The key is
allowing time for this possibility in the
initial schedule.
Make the Best Use of Results
Pretesting findings can be used to solve
problems, plan programs, develop
materials, or refine materials or messages.
It is important to avoid misuse of market
research results. Perhaps the most
common error is to overgeneralize.
Qualitative, diagnostic pretest methods
should not be used to estimate broad-scale
results. If 50 of the 100 respondents in an
intercept test do not understand portions
of a pamphlet, it does not necessarily
mean that 50 percent of the total intended
audience will be confused. The lack of
understanding among those pretest
respondents suggests, however, that
the pamphlet may need to be revised to
improve its comprehensibility. Remember
that pretesting is indicative, not predictive.
Planning for Production, Distribution,
Promotion, and Process Evaluation
Once you have decided which materials to
produce, determine how many copies of
each will be needed and develop a
production schedule. To write a realistic
production schedule, review or revise the
following three components of the
communication plan:
1. Distribution channels you plan to use
(including specific organizations,
companies, sites, etc.), how many
materials you plan to disseminate
through each, and how many intended
audience members you propose to reach.
2. Promotion plans, which describe
how you intend to promote use of
the materials.
3. Process evaluation plans, which describe
the way the use of materials will be
monitored (e.g., using bounceback cards
to identify how respondents are using the
materials). Go to the process evaluation
section of Stage 3 for more details.
Distribution and promotion sections of the
program plan will define both production
costs and the quantity of materials to
produce. It is a good idea to get input on
the distribution, promotion, and evaluation
sections of the program plan from partners
and others involved with implementation.
Common Myths and Misconceptions
About Materials Pretesting
Myth: I don’t have the time or money.
Fact:
Pretesting needs to be planned as an
integral step in the materials development
process from the beginning. Include time
and resources for pretesting and for any
changes you might need to make as a result
in the project budget and timeline.
Otherwise, your program may not have the
funds, and your boss may see the time for
pretesting and alterations in materials as a
delay in production rather than evidence of
careful planning and development.
Myth: My boss won’t support pretesting.
Fact:
Use the information in this guide
and in the Selected Readings to convince
your boss that you need to pretest. Beautiful
materials and an elegant design can’t
guarantee that the intended audience will
pay attention to, understand, or relate to
the messages. It’s cheaper to find out
whether the materials might work before
they are produced than to have to start
86
Developing and Pretesting Concepts, Messages, and Materials

over later or, worse, to have an unsuccessful
program. Once you have pretested, be sure
to explain to your superiors (in a report) how
it worked and what resulted. Build a case for
their acceptance of future pretesting. Using
quotes from the intended audience or
anecdotes to illustrate the findings can make
the report more interesting and memorable.
Myth: I can tell the difference between good
and bad materials, so I don’t need to pretest.
Fact:
Many people have said this, only to
find out they can be wrong.Your training
and experience are essential credentials,
but are you sure you can react objectively
to materials you have created or are
responsible for? Can you really assume
the role of someone who is different from
you (if you are not representative of the
intended audience) and see your materials
through his or her eyes? Can you defend
your decision, without objective evidence,
to those who may disagree?
Myth: Our artist/producer says that
pretesting can’t be used to judge creativity.
Fact:
Graphics staff, artists, and creative
writers may be sensitive to criticism from
“nonprofessionals,” including the intended
audience. Explaining the purpose of
pretesting and involving them in the
pretesting may help them understand and
appreciate the process. Explain that you are
testing all elements of the communication
and not just their work. By testing alternative
concepts or executions, you can provide the
creative staff with direction without telling
them their work “failed.”
Selected Readings
American Marketing Association, New York
Chapter. (2001/2002). Green Book:
International directory of marketing research
companies and services. New York.
Backer, T. E., Rogers, E. M., & Sopory, P.
(1992). Designing health communication
campaigns: What works. Thousand Oaks,
CA: Sage.
Campbell, M. K., DeVellis, B. M., Strecher, V.
J., Ammerman, A. S., DeVellis, R. F., &
Sandler, R. S. (1994). The impact of
message tailoring on dietary behavior
change for disease prevention in primary
care settings. American Journal of Public
Health, 84, 783–787.
Center for Substance Abuse Prevention.
(1994). Careful concept development paves
the way to effective prevention materials
[Technical Assistance Bulletin]. Washington,
DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention.
(1994). Conducting focus groups with young
children requires special considerations and
techniques [Technical Assistance Bulletin].
Washington, DC: U.S. Government
Printing Office.
Center for Substance Abuse Prevention.
(1994). Following specific guidelines will
help you assess cultural competence in
program design, application, and
management [Technical Assistance
Bulletin]. Washington, DC: U.S. Government
Printing Office.
Center for Substance Abuse Prevention.
(1994). A key step in developing prevention
materials is to obtain expert and gatekeeper
reviews [Technical Assistance Bulletin].
Washington, DC: U.S. Government
Printing Office.
STAGE 2
Making Health Communication Programs Work
87

Center for Substance Abuse Prevention.
(1994). Pretesting is essential:You can
choose from various methods [Technical
Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Center for Substance Abuse Prevention.
(1994). You can manage focus groups
effectively for maximum impact [Technical
Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Center for Substance Abuse Prevention.
(1994). You can prepare easy-to-read
materials [Technical Assistance Bulletin].
Washington, DC: U.S. Government
Printing Office.
Center for Substance Abuse Prevention.
(1994). You can use communications
principles to create culturally sensitive and
effective prevention materials [Technical
Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Centers for Disease Control and Prevention.
(1994). Listening to your audience: Using
focus groups to plan breast and cervical
cancer public education programs (CDC
Publication No. PDF-245K). Denver: AMC
Cancer Research Center.
Centers for Disease Control and Prevention.
(2000). Beyond the brochure (CDC
Publication No. PDF-821K). Atlanta.
Debus, M. (1988). Methodological review: A
handbook for excellence in focus group
research. Washington, DC: Academy for
Educational Development.
Goldberg, M. E., Fishbein, M. F., &
Middlestadt, S. E. (Eds.). (1997). Social
marketing: Theoretical and practical
perspectives. Mahwah, NJ: Erlbaum.
Jones, J. P. (Ed.). (1998). How advertising
works: The role of research. Thousand
Oaks, CA: Sage.
Kotler, P., & Roberto, E. L. (1989). Social
marketing: Strategies for changing public
behavior. New York: Free Press.
Lipkus, I. M., Lyna, P. R., & Rimer, B. K.
(1999). Using tailored interventions to
enhance smoking cessation among African
Americans at the community health center.
Nicotine and Tobacco Research, 1(1),
77–85.
Maibach, E., & Parrott, R. L. (Eds.). (1995).
Designing health messages: Approaches
from communication theory and public
health practice. Thousand Oaks, CA: Sage.
Merton, R. K. (1987). Focused interviews
and focus groups: Continuities and
discontinuities. Public Opinion Quarterly, 51,
550–556.
Merton, R. K., Riske, M., & Kendall, P. L.
(1996). The focused interview (2nd ed.).
New York: Free Press.
Morgan, D. L., & Krueger, R. A. (1998). The
focus group kit. Thousand Oaks, CA: Sage.
National Cancer Institute. (1994). Clear and
simple: Developing effective print materials
for low-literate readers (NIH Publication No.
95-3594). Bethesda, MD.
National Cancer Institute. (1998). How
the public perceives, processes, and
interprets risk information: Findings from
focus group research with the general
public. Bethesda, MD: U.S. Department of
Health and Human Services.
National Cancer Institute. (2000). Multi-
ethnic focus groups to test motivational
messages on mammography and breast
cancer. Bethesda, MD.
88
Developing and Pretesting Concepts, Messages, and Materials

Palmgreen, P., et al. (1995). Reaching at-risk
populations in a mass media drug abuse
prevention campaign: Sensation seeking as
a targeting variable. Drugs and Society, 8(3),
29–45.
Rice, M., & Valdivia, L. (1991). A simple
guide for design, use, and evaluation for
education materials. Health Education
Quarterly, 18(1), 79–85.
Rimer, B. K., & Glassman, B. (1998).
Tailoring communications for primary care
settings. Methods of Information in
Medicine, 37(3), 171–177.
Selden, C. R., Zorn, M., Ratzan, S., &
Parker, R. M. (2000). Health literacy, January
1990 through October 1999. Bethesda, MD:
National Library of Medicine.
Siegel, M., & Doner, L. (1998). Marketing
public health: Strategies to promote social
change. Gaithersburg, MD: Aspen.
Strecher, V. J., Kreuter, M. W., DenBoer,
C. H., Kobrin, S. C., Hospers, H. J., &
Skinner, C. S. (1994). The effects of
computer-tailored smoking cessation
messages in family practice settings.
Journal of Family Practice, 39, 262–270.
U.S. Department of Health and Human
Services. (2000). Healthy people 2010 (2nd
ed.; in two volumes: Understanding and
improving health and Objectives for
improving health). Washington, DC: U.S.
Government Printing Office.
Wells, W. D. (Ed.). (1997). Measuring
advertising effectiveness. Mahwah,
NJ: Erlbaum.
STAGE 2
Making Health Communication Programs Work
89

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
STAGE 3
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Implementing the Program
In This Section:
• Preparing to launch and implement your program
• Holding a press conference
• Maintaining media relations after launch
• Working with the media during a crisis
• Managing implementation: monitoring and problem solving
• Maintaining partnerships
• Common myths and misconceptions about implementation
Questions to Ask and Answer:
• How should we launch the program?
• Should we use a kickoff event?
• How should we develop and sustain media coverage?
Partner involvement? Audience interest?
• How should we manage a press conference?
• How should we work with the media during a crisis?
• How can we ensure that our program operates according to plan?
• How can we use process evaluation?
• How can we find out whether we are reaching the intended
audience with our information?
• How can we find out whether they are responding favorably to
our message and materials?
• Are we maintaining good relationships with our partners?
STAGE 3

Preparing to Implement Your Program
Before you launch the program, plan for
distribution, promotion, and process
evaluation. Make sure you also develop a
launch plan, produce sufficient quantities of
materials, and prepare your staff for the
work ahead.
Program Launch
You may choose to launch your program
quietly, starting activities on a limited basis
in one geographic area or with just one
partner to test the program. Using a limited
approach will permit you to make
adjustments before you fully commit your
resources. This can be particularly useful for
a large-scale program or for programs using
a new technique or involving a new intended
audience. Or, you may choose to launch
with a kickoff event.
Kickoff Event
A kickoff event can create broader
awareness of the program and promote
community involvement. Kickoff events are
an excellent way to develop relationships
with people who may be willing to get
involved in the program. Scheduling an
event also creates a deadline, which will
help your program avoid unnecessary lag
time or protracted preparations.
To begin with a kickoff event, you might:
• Plan an event to celebrate the start of
the program.
• Tie the kickoff to newsworthy happenings,
such as the Great American Smokeout,
Talk About Prescriptions Month, or the
announcement of the results of a
major study.
• Tie into community events, such as
sporting events, church activities,
shopping mall promotions, or
holiday happenings.
• Work with partner organizations to fund
events that the intended audience already
participates in and that have broad
media interest.
To enhance media coverage of your
kickoff event:
• Create a news “hook” or angle that makes
the event newsworthy
• Use a checklist to track preevent, event,
and postevent activities. These may
include room arrangements, speakers,
expenditures, media kits, refreshments,
transportation, equipment, and
follow-up actions.
• Inform the media of your event in a timely
way. Ask about their schedules, if possible,
to avoid holding an event that conflicts
with other media activities. Conflicts might
prevent you from getting media coverage.
• Don’t forget to include specialized media,
such as community newspapers, cable TV
stations, radio, health-related publications
(the trade press), foreign-language
publications or broadcast media, Internet
“zines” and Web sites, and organization
publications. These media may have a
greater incentive to use your story than
general newspapers or regular TV
stations, and they can ensure an audience
at a press conference if the mainstream
media don’t show up.
• Launch activities in multiple locales on
the same date to make them
more newsworthy.
• Create media kits to facilitate accurate
reporting of the issue.
• Invite spokespeople who support your
program and who may attract
media interest.
92
Implementing the Program

• Hold the event in a location that is
connected to your message and involves
members of the intended audience. This
might be a youth center for a program
aimed at teenagers, a grocery store for
a program about nutrition, or a
neighborhood where screening will
be offered. Make sure the location has
sufficient space for the media and
their equipment.
Holding a Press Conference
One effective kickoff event is holding a press
conference.Your health communication
program launch is unlikely to get much
LAUNCH CHECKLIST
• Are our partners prepared for
the launch?
• Have we invited reviewers,
gatekeepers, and others who
have been involved in
program development?
• Have we prepared (or trained, if
necessary) our staff and spokespeople?
• Are program-related services (e.g., a
hotline, screening facilities) in place?
• Do we have a list of the media outlets
we need to contact?
• Are all of our promotional
materials ready?
• Do we have enough materials to start
the program (e.g., PSAs and media
kits) and respond to inquiries (e.g.,
leaflets for the public)?
• Are reordering mechanisms in place?
• Do we have mechanisms in place to
track our program’s progress and to
identify potential problems?
• Are health professionals and other
service providers in the community
aware of our program and prepared to
respond if their clients ask about it?
media attention if you just set up a press
conference. News media have many
opportunities to attend events and at the
same time are finding it easier to get
information electronically. This means that
you must stand out to attract media to your
event. Tying the program’s launch to
important health news can help. Such news
could include announcing the results of a
recent health study, releasing new statistics
on your topic, or announcing the start of a
comprehensive or multiorganization health
program of which your program is a part.
Even more attractive is announcing such
news plus having representatives of the
intended audience or other individuals tell
compelling personal stories.
The following are tips for planning and
conducting a successful press conference.
Invitations
Be realistic about the media you invite. Local
press people and those with whom you
already have a relationship are more likely
to attend than representatives from national
newspapers or TV stations. Don’t forget the
health-related trade press, which often
needs news and will help bolster
attendance. Give reporters three to four
days’ notice. If yours is a major story, call
wire services to have the event put on their
daybooks. Remind the staff person
responsible for contacting the media to call
reporters the day before the event to pitch
its importance.
Speakers
Decide who will announce which aspects of
your news. In general, select people for their
recognizable names. If they are not familiar
with your program, you can brief them,
provide materials, and have knowledgeable
people on hand to answer questions your
main speakers cannot. Don’t overlook the
opportunity for personal testimony by
STAGE 3
Making Health Communication Programs Work
93

patients, physicians, and family members.
You may want to pretape their statements at
their homes or in the hospital (you will
usually need a written release from
patients). Remember that all speakers,
including patients, will need to be available
during the day of the press conference to
answer press inquiries and be interviewed.
Timing
The conventional wisdom is to hold press
conferences between Tuesday mid-morning
and Thursday afternoon. However, it is
important to know the schedule of the media
you’ve invited. Reporters from afternoon
newspapers have morning deadlines and
may not be able to attend a late morning or
early afternoon conference. Try to limit your
press conference to 15 minutes or less,
including plenty of time for questions.
Emphasize to speakers the need to keep
their remarks short and simple, to avoid
scientific jargon, and to focus on the action
you want your intended audience to take.
Logistics
Assign a staff person to arrange a suitable
room and any equipment you may need,
including a “mult box” that allows the media
to connect their equipment to the public
address system for better sound quality. The
staff person should also arrange for parking,
tell people where to park, and put up signs
to help reporters find your room.You should
also plan to have another person who has
media experience on hand to distribute
media kits, show media representatives
where they can set up their equipment,
answer questions, and point out who is
available for follow-up interviews.
94

Media Kits
At a minimum, include:
• A press conference agenda
• A press release
• Local, state, and national statistics about
your issue
• Background information
• Biographies of your speakers
• Reproducible copies of charts or graphs
used in your speakers’ presentations
• Copies of other program materials
or reports
• Name and telephone number of someone
who can be called to answer questions or
verify information
To increase the usefulness of your kit to
television reporters, include broadcast-
quality stock video (B-roll). If you have
invited non-English-language media
representatives to attend, provide materials
in their language (have the materials
prepared and reviewed by people fluent in
the language).
Follow Up
Deliver your new release or press kit in
person to key reporters who didn’t attend
the press conference. Explain why your
news is important.
Maximizing Media Coverage of
Your Program
To maximize media coverage, be sure to:
• Know what different publications, stations,
and shows typically cover, and which staff,
editors, and reporters are responsible for
what. Giving your story to the right outlets
and the right people shows your
understanding of their work and can
improve the likelihood of coverage.
• Understand your media market. Some
media, such as those in the Washington,
DC, area, see themselves as providers of
regional or national rather than local
coverage, which makes it more difficult for
local stories and issues to receive
attention. In similar situations, pitch your
story with a regional or national slant to
increase the possibility of coverage.
• Respond quickly to requests for
information. If you are able to give
answers or statements within an hour of a
request, media outlets will continue to call.
• Provide information the media can use.
• Be honest about your issue, your
organization, what you know, what you
can do for the media, and what you want
from them. If you don’t know the answer to
a question they ask, tell them so and offer
to get the answer quickly.
• Work personally with the media to help
them understand your issue; just sending
them news releases or PSAs is much less
effective. Provide background information
so that when a story breaks they have
accurate facts on hand.
• Ask for something the media can give
besides coverage. For instance, they
may be able to provide data about their
audience to help you decide which
media to use, or help produce broadcast
segments or PSAs, or cosponsor
an event.
Maintaining Media Relations
After Launch
Support your program’s messages by
encouraging media to cover your program
after launch. To get continuing coverage of
your program, you must develop an ongoing
relationship with the media. These steps can
help ensure continuing media coverage.
STAGE 3
Making Health Communication Programs Work
95

1. Make a list of key media contacts,
establish relationships with them early,
and nurture the relationships throughout
the life of your program. Many people can
help you identify media contacts. Begin
within your own organization. Ask whether
staff or volunteers have media contacts or
know media figures such as owners of
newspapers or broadcast stations.
Outside your organization, talk with
partners; people you know at media
outlets, public relations/advertising firms,
and on the public relations staff of
business firms; members of professional
associations (such as chapters of the
Public Relations Society of America); and
people in public relations or marketing
programs at local universities. Other
sources include reference books in your
local library that list local and national
media contact information. Update your
media lists regularly; using an incorrect
name or title can mean the media won’t
cover your message.
2. Develop a plan for periodic media
coverage of your program and make your
program newsworthy. Your plan should
include your program’s objectives, the
messages you want to communicate to
the media (including why your program or
message deserves coverage), any
promotional activities you plan to sponsor,
and a schedule for media contact (when it
will occur and who will initiate it).
3. Identify and train media spokespeople.
It is a good idea to select no more than
three spokespeople. Be sure that all of
them are providing the same information
about your program by giving them
written briefing points. The media usually
prefer spokespersons with authority in
your organization. The person who
regularly handles media relations may
not have that status. Some spokespersons
will be savvy about working with the
media and need only a briefing on your
program. Others may need training on
how to give interviews, respond to media
queries during crisis or “bad news”
situations, or how to be effective on TV
or radio.
4. Track media coverage. This includes
coverage of issues generated by your
media relations efforts as well as
coverage that occurs independently.
Monitoring all types of coverage can
provide important process evaluation
data. It will enable you to identify and take
steps to correct misstatements and
errors, determine the impact of your
media activities and whether changes are
needed, identify other media
representatives interested in your issue,
and find out whether your organization is
being overlooked. Media coverage can be
measured in terms of quantity (how much
space did a story get and how often are
stories published?); prominence (does it
appear on the front page or not?); slant
(is coverage positive or negative?);
accuracy of content; and type of story (is
the story an editorial or hard news?).
5. Capitalize on breaking news. When
something happens that is related to your
program, call news outlets and offer them
an expert opinion. If a negative event
occurs, take the opportunity to explain
how the changes advocated by your
organization could help prevent similar
problems in the future. For example, when
the story about traces of poisonous
substances in Chilean grapes received
widespread coverage, tobacco control
activists used the event to point out that
larger amounts of those same substances
are found in a single cigarette.
96
Implementing the Program

PROCESS EVALUATION TRACKS EFFECTIVENESS OF MEDIA LAUNCH FOR CLINICAL TRIAL
START-UP
In 2001, the National Cancer Institute kicked off a large national clinical trial on prostate
cancer using an extensive media launch, including national, local, and Spanish-language
press releases as well as a professionally produced video news release (VNR). The launch
employed extensive outreach to news outlets designed to make the media aware of the
clinical trial. The hope was that these outlets would then report on the trial and that
eligible participants would be encouraged to volunteer. The following process evaluation
activities were used to measure the effectiveness of the media push in distributing the
launch messages:
• Monitoring use of the VNR through Nielsen’s SIGMA
®
encoding
• Tracking calls about the trial to the Cancer Information Service’s toll-free information
line (1-800-4-CANCER), which was promoted in the media materials
• Observing print coverage of the trial through LexisNexis
• Monitoring traffic to NCI Web sites describing the trial
• Surveying each study site about its specific media efforts
• Monitoring the total accrual rate to the trial
Findings showed that the full-fledged media push produced nearly 1,000 print and
broadcast hits in the month following the launch and that the messages were successful
in reaching the intended audiences. Men in the correct age range, for example, called the
1-800 information line in numbers far exceeding their usual number. The data also
indicated that the media were effective in both reaching and motivating potential
minority participants. Calls from minority men to the toll-free number were
substantially higher than for previous trials and roughly equivalent to their proportion
in the population.
UNDERSTANDING THE MEDIA
What Do the Media Like?
• Stories with audience appeal
• Issues that stimulate debate, controversy, or conflict
• Stories that create higher ratings and larger audiences
• Fresh angles or twists on issues that will attract public interest
• Accurate background information
What Do the Media Dislike?
• Covering old topics
• Duplicating stories reported by competitors
• Reporting inaccuracies or an incomplete picture
• Receiving numerous calls when on a deadline
• People who persist when a story idea is rejected
• Organizations that believe their story is interesting simply because it is theirs or that
convey the attitude that the importance of the story is obvious
STAGE 3
Making Health Communication Programs Work
97

Working With the Media During
a Crisis Situation
If a crisis develops related to your health
topic, your organization, or your program,
the media will likely contact you. The
following suggestions will help you work
effectively with the media in these situations:
Be Prepared
• Identify a spokesperson to handle
media inquiries.
• Train the spokesperson to handle routine
inquiries, interviews, media appearances,
and crises. A professional media
consultant can help with this training.
Take Control
• Stay calm. Show your staff and the public
that you are on top of the problem and are
taking steps to resolve it.
• Respond quickly. Help reporters who call
you meet their deadlines and call them if
no one calls you.
• Tell the truth. Admitting mistakes and
taking responsibility for them is important
for your credibility. Crisis situations can
work to your advantage by showing
your ability to take charge under
difficult circumstances.
• Be well informed. Get the facts you need
to understand the situation and develop a
response. When talking to reporters, focus
on the main message you want to send.
• Track incoming calls. Keeping a record of
who called, from where, why, and how the
information you gave them will be used
will give you a list of names to call if new
information becomes available (and
provide a good resource for the future).
• Say, “I don’t know” when you cannot
answer a reporter’s question. Promise to
get the answer quickly and follow through.
• Consider preparing a short statement
with comments from your
organization’s leadership.
Managing Implementation:
Monitoring and Problem Solving
Managing a health communication program
is much like managing any other project.
Key activities include monitoring activities,
staff, and budget; problem solving; process
evaluation; measuring intended audience
satisfaction; and revising plans
and operations.
Your communication plan should indicate
how and when resources will be needed,
when specific events will occur, and at what
points you will assess your efforts. Once
implementation is under way, however,
contingencies may arise. Periodically,
assess whether:
• Activities are being completed at
scheduled times
• Your intended audiences are
being reached
• Certain activities or materials are more
successful than others
• Certain aspects of the program need to be
altered or eliminated
• Your expenditures are within budget
You can often correct problems quickly if you
can identify them. For example, if you ask
the public to call you for more information,
you should provide a simple form (electronic
or manual) for telephone operators to use to
record the questions asked and the answers
given. Frequently review responses to
identify inquiry patterns, to be sure that
correct or adequate information is being
given, and to find out whether more or
different information may be needed.
98
Implementing the Program

99

Process Evaluation
Process evaluation takes place during
implementation and monitors the functioning
of program components. It includes
assessment of whether messages are being
delivered appropriately, effectively, and
efficiently; whether materials are being
distributed to the right people and in the
right quantities; whether the intended
program activities are occurring; and other
measures of how well the program is
working. Use process evaluation to
track the following:
• The functioning and quality of
your program
• Partner/coalition involvement
• The effectiveness of publicity, promotion,
and other outreach efforts
• Media response
• intended audience participation, inquiries,
and other responses
• Adherence to schedule
• Expenditures and adherence to budget
• Contractor activities:
— Are seasoned professionals doing the
creative and managerial work?
— Is the contractor devoting enough time
and money to your project?
— Are deadlines being met?
— Are performance and deliverables in
keeping with the contract?
— Are the hours billed reasonable for the
work performed?
— Are there problems in the relationship?
The following are examples of ways to
gather the information needed for
process evaluation:
• Use activity tracking forms.
• Monitor the volume of public inquiries and
requests for information.
EXAMPLES OF PROCESS
EVALUATION MEASURES
Dissemination
• Amount of time given to your
message by radio and television
stations and what the estimated
size/demographics of the
audiences are
• Print coverage and
estimated readership
• Quantities of educational
materials distributed
• Number of speeches and
presentations given
• Number of special events
• Size of audiences at presentations
and events
Response
• Number of telephone, mail, and
e-mail inquiries (how people heard of
the program, what they asked)
• Number of people visiting Web sites
or Internet services
• Number of organizations, businesses,
or media outlets participating in
the program
• Response to presentations (measured
by completed participant
feedback forms)
• Number of publications requested
and distributed
Audience
• Demographic or other characteristics
of the responding audience (to find
out whether the intended
audience responded)
100
Implementing the Program

• Ask callers what prompted their call.
• Use clipping services to gauge
media coverage.
• Gather feedback cards from or make
follow-up phone calls to television and
radio stations.
• Review telephone responses for accuracy.
• Follow up with teachers, physicians, or
other gatekeepers to check their
preparedness and interest.
• Gather regular status reports from staff,
contractors, and partners.
• Meet in person or by telephone with
partners to review your
program’s progress.
• Track traffic to project Web sites.
• Review publication requests
and distribution.
Measuring Audience Satisfaction
Audience satisfaction surveys are an
important tool for both process and outcome
evaluations of health communication
programs. Use surveys to help you identify
the following:
• The characteristics of those you
reached—how well do they match
the characteristics of your
intended audiences?
• How the intended audience reacted to
your materials and services—were
materials easy to understand? Useful?
• How the intended audience used your
materials—were materials read?
Passed on to others? Saved? Were
events attended?
Making Health Communication Programs Work
101

This information will help you determine
whether you are reaching your intended
audiences, whether your materials or
activities need to be revised, and whether
your materials are being used as you
intended. Some managers also use these
surveys to learn what information intended
audiences would like to receive in the future.
See Appendix A for an example of a user
survey. The survey example, the Breast
Cancer Risk Assessment Tool Evaluation
from NCI, includes a summary of the
responses as an example of the range
of information you can glean from surveys
like these.
USING PROCESS EVALUATION TO MAKE
MIDCOURSE CORRECTIONS
By tracking call frequency, one regional
Cancer Information Service (CIS) office
found that calls increased when certain
PSAs were run, thus showing the CIS
office how to maximize its promotional
efforts. Tracking showed that men of all
ethnicities and African-American
women were not well represented
among the callers. The CIS office also
found that special promotions increased
the call rate among African-American
women, but did not prompt more men
to call. As a result, the office stopped
trying to reach this intended audience
through PSAs and explored other ways
to reach it.
Note. From “Effect of the mass media in
promoting calls to the Cancer Information
Service,” by Arkin, E. B., Romano, R. M., Van
Nevel, J. P., & McKenna, W. (1993). In The
Cancer Information Service: A 15-year history
of service and research (Monograph of the
Journal of the National Cancer Institute,
No. 14).
Making Adjustments
The implementation stage will not always
proceed as you expect. Materials may be
delayed at the printer, a major news story
may preempt your publicity (or focus
additional attention on your issue), or a new
priority may delay community participation.
A periodic review of your planned tasks and
time schedules will help you revise any
plans that might be affected by unexpected
events or delays. There is nothing wrong
with altering your plans to fit a changed
situation. In fact, you may risk damaging
your chances of success if you are not
willing to be flexible.
Maintaining Partnerships
If your organization has partnered with
others, you will need to work to maintain a
good relationship between your organization
and your partners. Frequent two-way
communication is essential to productive
partnerships. If partners hear from you only
when you need something or you hear from
partners only if problems arise, the
relationship will suffer.
To keep partners involved:
• Periodically call to find out how your
partners’ work is progressing. Offer to
help when appropriate, congratulate
them on their accomplishments, and
show an interest in them that mirrors
the interest you hope they take in
your program.
• Involve them whenever it is reasonable
(and they are interested) in your
activities, such as special events or
process evaluation.
• Give them regular updates on the
program. Some organizations formalize
this task by sending out newsletters or
reports. Others handle it informally
102
Implementing the Program

through calls, meetings, or letters.
Tell partners about any changes in
program activities that may impact
their organization.
• Give them credit in your news releases
and other publicity. If you generate
a story that mentions them, send
them a copy.
• Share new materials and information
(e.g., about breaking stories relevant to
their organization).
• Notify them of program results, whether
positive or negative.
• Share feedback from your
process evaluation.
• Explore opportunities for
further collaboration.
Continue to Consider New Opportunities
For Partnering
You may have planned to use one or several
media, interpersonal, organizational, and
community channels for your program.
Before you implemented your program,
you likely partnered with appropriate
organizations. Once your program is under
way, however, other organizations may
want to get involved, or you may find that
you need a new partner to reach a certain
segment of your intended audience.
Partners that have fulfilled objectives
may step aside.
Common Myths and Misconceptions
About Program Implementation
Myth: People need the information we are
providing, so we will have a large number
of requests for our materials.
Fact:
“If we print it they will come” holds true
only if you are printing money. For most
programs, effective promotion is critical to
getting materials into the hands of those
who need them. Disseminating printed
products is as challenging, and as
important, as developing them.
Myth: Working with the media is more
trouble than it is worth. They take
statements out of context, don’t bother to
check facts, and care only about
sensationalism.
Fact:
Although is possible to have bad
experiences with the media, if you pay
attention to your work with them, you can
help foster positive outcomes. Learn which
reporters are responsible journalists and
develop relationships with them. Then
provide accurate background materials and
offer to check their stories for technical
correctness. Respect their need for stories
of interest to the public and try to help them
by thinking of positive, attention-getting
angles for your program. If your topic is
controversial, you may want to provide
media training for your spokespeople to
help avoid giving statements that could be
misinterpreted or taken out of context. Work
with the media to correct inaccuracies.
STAGE 3
Making Health Communication Programs Work
103

Myth: When the press conference is over,
we can relax.
Fact:
The longevity of news can be
measured in days—if not minutes. Single
channels or even the entire mass media are
unlikely to reach all intended audiences, and
one event or activity is not enough. Just as
health messages need repetition and
reinforcement, so do promotions.Your job
isn’t over until the warehouse is empty
(unless you create enough demand for a
second printing) or until you have met all of
your objectives.
Myth: We have partners, so we don’t have
to worry as much about implementation.
They’ll do a lot of the work for us.
Fact:
Partners can help with
implementation, but they are unlikely to
reduce your workload. Developing and
maintaining partnerships is itself very labor
intensive, and your role in leading,
coordinating, and monitoring program
operations is essential.
Myth: If a program is not an immediate
success, it is a failure.
Fact:
All change takes time. Even the best-
planned health communication programs
have to make midcourse corrections. The
information you get from process evaluation
can help you recognize where
improvements are needed and get back on
track. Each time you learn more about your
intended audience, your own processes,
and the barriers you face, you increase your
likelihood of success.
Myth: It is unseemly for a
government/nonprofit health program to
spend money to promote itself.
Fact:
By promoting your program, you are
promoting your issue and your message.
The more people who know about what you
have to offer, the more the community will
benefit. Having your organization recognized
lends credibility to your program and will
help you recruit supporters, partners,
volunteers, and funding sources when you
need them. As long as you keep the focus
on your communication objectives and not
on your office (or yourself!), program
promotion is a legitimate, integral aspect of
health communication.
Selected Readings
Agency for International Development,
Academy for Educational Development.
(1992). Results and realities: A decade of
experience in communication for child
survival. Washington, DC.
Arkin, E. B., Romano, R. M., Van Nevel,
J. P., & McKenna, W. (1993). Effect of the
mass media in promoting calls to the
Cancer Information Service. In The Cancer
Information Service: A 15-year history of
service and research (Monograph of the
Journal of the National Cancer Institute,
No. 14).
Center for Substance Abuse Prevention.
(1994). Following specific guidelines will
help you assess cultural competence in
program design, application, and
management. [Technical Assistance
Bulletin]. Washington, DC: U.S. Government
Printing Office.
104
Implementing the Program

Center for Substance Abuse Prevention.
(1994). You can increase your media
coverage [Technical Assistance Bulletin].
Washington, DC: U.S. Government
Printing Office.
Dignan, M. B., & Carr, P. A. (1992). Program
planning for health education and health
promotion (2nd ed.). Philadelphia: Lea
& Febiger.
Jernigan, D. H., & Wright, P. A. (1996).
Media advocacy: Lessons from community
experiences. Journal of Public Health Policy,
17, 306–330.
Wallach, L., Dorfman, L., Jernigan, D., &
Themba, M. (1993). Media advocacy and
public health: Power of prevention.
Thousand Oaks, CA: Sage.
Wallach, L., Woodruff, K., Dorfman, L., &
Diaz, I. (1999). News for a change: An
advocate’s guide to working with the media.
Thousand Oaks, CA: Sage.
Making Health Communication Programs Work
105
STAGE 3

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
STAGE 4
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Assessing Effectiveness
and Making Refinements
In This Section:
• Why outcome evaluation is important
• Revising the outcome evaluation plan you wrote during Stage 1
• Conducting the assessment
• Refining the health communication program
• Common myths and misperceptions about evaluation
Questions to Ask and Answer:
• How can we use outcome evaluation to assess the effectiveness
of our program?
• How do we decide what outcome evaluation methods to use?
• How should we use our evaluation results?
• How can we determine to what degree we have achieved our
communication objectives?
• How can we make our communication program more effective?
I
n Stage 3, you decided how to use process evaluation to monitor
and adjust your communication activities to meet objectives. In
Stage 4, you will use the outcome evaluation plan developed in
Stage 1 to identify what changes (e.g., in knowledge, attitudes, or
behavior) did or did not occur as a result of the program. Together, the
progress and outcome evaluations will tell you how the program is
functioning and why. (If you combine information from the two types of
evaluation, be sure that you focus on the same aspects of the program,
even though you look at them from different perspectives.) This section
will help you revise your plans and conduct outcome evaluation.You
should begin planning assessment activities either before or soon after
you launch the program.
STAGE 4

Why Outcome Evaluation
Is Important
Outcome evaluation is important because
it shows how well the program has met its
communication objectives and what you
might change or improve to make it more
effective. Learning how well the program
has met its communication objectives is
vital for:
• Justifying the program to management
• Providing evidence of success or the need
for additional resources
• Increasing organizational understanding
of and support for health communication
• Encouraging ongoing cooperative
ventures with other organizations
Revising the Outcome
Evaluation Plan
During Stage 1, you identified evaluation
methods and drafted an outcome evaluation
plan. At that time, you should have collected
any necessary baseline data. The first step
in Stage 4 is to review that plan to ensure it
still fits your program. A number of factors
will influence how your communication
program’s outcomes should be evaluated,
including the type of communication
program, the communication objectives,
budget, and timing. The outcome evaluation
needs to capture intermediate outcomes
and to measure the outcomes specified in
the communication objectives. Doing so can
allow you to show progress toward the
objectives even if the objectives are not met.
Consider the following questions to assess
the Stage 1 outcome evaluation plan and to
be sure the evaluation will give you the
information you need:
EXAMPLES OF EFFECTIVENESS MEASURES
FOR
HEALTH COMMUNICATION PROGRAMS
Knowledge
A public survey conducted before and
after NCI’s 5 A Day campaign found
that knowledge of the message (a
person should eat 5 or more servings
of fruits and vegetables each day for
good health) increased by 27
percentage points.
Attitude
In 1988, the U.S. Surgeon General sent
a pamphlet designed to influence
attitudes on AIDS to every U.S.
household. An evaluation conducted
in Connecticut showed no change in
attitude between residents who read
the pamphlet and those who did not.
Behavior
The Pawtucket Heart Health Program
evaluated a weight-loss awareness
program conducted at worksites.
More than 600 people enrolled, and
they lost an average of 3.5 pounds
each compared with their
preprogram weight.
• What are the communication objectives?
What should the members of the intended
audience think, feel, or do as
a result of the health communication plan
in contrast to what they thought, felt,
or did before? How can these changes
be measured?
• How do you expect change to occur?
Will it be slow or rapid? What measurable
intermediate outcomes (steps toward the
desired behavior) are likely to take place
before the behavior change can occur?
The behavior change map you created in
Stage 1 should provide the answers to
these questions.
108
Assessing Effectiveness and Making Refinements

• How long will the program last? What
kinds of changes can we expect in that
time period (e.g., attitudinal, awareness,
behavior, policy changes)? Sometimes,
programs will not be in place long enough
for objectives to be met when outcomes
are measured (e.g., outcomes measured
yearly over a 5-year program). To help
ensure that you identify important
indicators of change, decide which
changes could reasonably occur from
year to year.
• Which outcome evaluation methods can
capture the scope of the change that is
likely to occur? Many outcome evaluation
measures are relatively crude, which
means that a large percentage of the
intended audience (sometimes an
unrealistically large percentage) must
make a change before it can be
measured. If this is the case, the
evaluation is said to “lack statistical
power.” For example, a public survey of
1,000 people has a margin of error of
about 3 percent. In other words, if 50
percent of the survey respondents said
they engage in a particular behavior, in all
likelihood somewhere between 47 percent
and 53 percent of the population
represented by the respondents actually
engages in the behavior. Therefore, you
can conclude that a statistically significant
change has occurred only if there is a
change of 5 or more percentage points. It
may be unreasonable to expect such a
large change, and budgetary constraints
may force you to measure outcomes by
surveying the general population when
your intended audience is only a small
proportion of the population.
QUANTITATIVE VERSUS QUALITATIVE EVALUATION
Quantitative research is used to gather objective information by asking a large number
of people a set of identical questions. Results are expressed in numerical terms (e.g., 35
percent are aware of X and 65 percent are not). If the respondents are a representative
random sample, quantitative data can be used to draw conclusions about an intended
audience as a whole. Quantitative research is useful for measuring the extent to which a
knowledge set, attitude, or behavior is prevalent in an intended audience.
Qualitative research is used to gather reactions and impressions from small numbers of
intended audience members, usually by engaging them in discussion. Results are
subjective and are not described numerically or used to make generalizations about the
intended audience. Qualitative research is useful for understanding why people react the
way they do and for understanding additional ideas, issues, and concerns.
Quantitative research methods are usually used for outcome evaluation because they
provide the numerical data necessary to assess progress toward objectives. When
evaluating outcomes, qualitative research methods are used to help interpret quantitative
data and shed light on why particular outcomes were (or were not) achieved. See the
Communication Research Methods section for detailed explanations of quantitative and
qualitative research methods and the circumstances under which you should use each.
STAGE 4
Making Health Communication Programs Work
109

• Which aspects of the outcome evaluation
plan best fit with your organization’s
priorities? Only rarely does a
communication program have adequate
resources to evaluate all activities.You
may have to illustrate your program’s
contribution to organizational priorities to
ensure continued funding. If this is the
case, it may be wise to evaluate those
aspects most likely to contribute to the
organization’s mission (assuming that
those are also the ones most likely to
result in measurable changes).
Conducting Outcome Evaluation
Conduct outcome evaluation by following
these steps:
1. Determine what information the
evaluation must provide.
2. Define the data to collect.
3. Decide on data collection methods.
4. Develop and pretest data
collection instruments.
5. Collect data.
6. Process data.
7. Analyze data to answer the
evaluation questions.
8. Write an evaluation report.
9. Disseminate the evaluation report.
See a description of each step below.
1. Determine What Information the
Evaluation Must Provide
An easy way to do this is to think about the
decisions you will make based on the
evaluation report. What questions do you
need to answer to make those decisions?
EVALUATION CONSTRAINTS
Every program planner faces limitations
when conducting an outcome
evaluation. You may need to adjust your
evaluation to accommodate constraints
such as the following:
• Limited funds
• Limited staff time or expertise
• Length of time allotted to the
program and its evaluation
• Organizational restrictions on hiring
consultants or contractors
• Policies that limit your ability to
collect information from the public
• Difficulty in defining the program’s
objectives or in establishing consensus
on them
• Difficulty in isolating program effects
from other influences on the intended
audience in “real world” situations
• Management perceptions of the
evaluation’s value
These constraints may make the ideal
evaluation impossible. If you must
compromise your evaluation’s design,
data collection, or analysis to fit
limitations, decide whether the
compromises will make the evaluation
results invalid. If your program faces
severe constraints, do a small-scale
evaluation well rather than a large-scale
evaluation poorly. Realize that it is not
sensible to conduct an evaluation if it is
not powerful enough to detect a
statistically significant change.
110
Assessing Effectiveness and Making Refinements

2. Define the Data You Need to Collect
Determine what you can and should
measure to assess progress on meeting
objectives. Use the following questions
as a guide:
• Did knowledge of the issue increase
among the intended audience (e.g.,
understanding how to choose foods low in
fat or high in fiber, knowing reasons not
to smoke)?
• Did behavioral intentions of the intended
audience change (e.g., intending to use a
peer pressure resistance skill, intending to
buy more vegetables)?
• Did intended audience members take
steps leading to the behavior change
(e.g., purchasing a sunscreen, calling for
health information, signing up for an
exercise class)?
• Did awareness of the campaign message,
name, or logo increase among intended
audience members?
• Were policies initiated or other institutional
actions taken (e.g., putting healthy snacks
in vending machines, improving school
nutrition curricula)?
3. Decide on Data Collection Methods
The sidebar Outcome Evaluation Designs
on the next page describes some common
outcome evaluation designs, the situations
in which they are appropriate, and their
major limitations. (See the Communication
Research Methods section for more
information.) Complex, multifaceted
programs often employ a range of methods
so that each activity is evaluated
appropriately. For example, a program that
includes a mass media component to reach
parents and a school-based component to
reach students might use independent
cross-sectional studies to evaluate the
111

OUTCOME EVALUATION DESIGNS APPROPRIATE FOR SPECIFIC COMMUNICATION PROGRAMS
Programs Not Delivered to the Entire Population of the Intended Audience
Evaluation Design
Randomized experiment. Members
of the intended audience are randomly
assigned to either be exposed to the
program (intervention group) or not
(control group). Usually, the same series
of questions is asked pre- and
postintervention (a pretest and posttest);
posttest differences between the two
groups show change the program
has caused.
Quasi-experiment. Members of the
intended audience are split into control
and intervention groups based simply
upon who is exposed to the program and
who is not.
Major Limitations
• Not appropriate for programs that will
evolve during the study period.
• Not likely to be generalizable or have
external validity because of tight controls
on program delivery and participant
selection. Delivery during the evaluation
may differ significantly from delivery
when the program is widely
implemented (e.g., more technical
assistance and training may be available
to ensure implementation is proceeding
as planned).
• For programs delivered over time, it is
difficult to maintain integrity of
intervention and control groups; group
members may leave the groups at
different rates of attrition.
• Often costly and time-consuming.
• May deprive the control group of positive
benefits of the program.
• Same as randomized experiments.
• Difficult to conclude that the program
caused the observed effects because
other differences between the two
groups may exist.
Continued on next page...
112
Assessing Effectiveness and Making Refinements

OUTCOME EVALUATION DESIGNS APPROPRIATE FOR SPECIFIC COMMUNICATION PROGRAMS CONTINUED...
Programs Delivered to the Entire Population of the Intended Audience
Evaluation Design
Before-and-after studies. Information is
collected before and after intervention
from the same members of the intended
audience to identify change from one
time to another.
Independent cross-sectional studies.
Information is collected before and after
intervention, but it is collected from
different intended audience members
each time.
Panel studies. Information is collected at
multiple times from the same members of
the intended audience. When intended
audience members are differentially
exposed to the program, this design helps
evaluators sort out the effects of different
aspects of the program or different levels
of exposure.
Time series analysis. Pre- and
postintervention measures are collected
multiple times from members of the
intended audience. Evaluators use the
preintervention data points to project what
would have happened without the
intervention and then compare the
projection to what did happen using the
postintervention data points.
Major Limitations
• Difficult to say with certainty that the
program (rather than some unmeasured
variable) caused the observed change.
• Cannot say with certainty that the
program caused any observed change.
• Generalizability may be compromised
over time. As participants age, leave, or
respond to repeated questions on the
same subject, they may no longer
closely represent the intended audience.
• Can be difficult to say with certainty
that the program caused the
observed change.
• Large number of pre- and
postintervention data points are
needed to model pre- and
postintervention trends.
• Normally restricted to situations in which
governmental or other groups routinely
collect and publish statistics that can
be used as the pre- and
postintervention observations.
STAGE 4
Making Health Communication Programs Work
113

EXAMPLES OF OUTCOME EVALUATION FOR COMMUNICATION PROGRAMS
NCI’s Cancer Information Service
Customer satisfaction surveys are one means of gathering data about a program’s effects.
Surveys of telephone callers to NCI’s Cancer Information Service (CIS) have shown that:
• Eight out of 10 callers say they take positive steps to improve their health after talking
with CIS staff.
• Seventy percent of those who call about symptoms say the CIS information was helpful
in their decision to see a doctor.
• Fifty-five percent of those who call about treatment say they use CIS information to
make a treatment decision.
• Two-thirds of callers who are considering participation in a research study talk with a
doctor after calling the CIS.
Note. From Morra, M. E. (Ed). (1998). The impact and value of the Cancer Information Service: A
model for health communication. In Journal of Health Communication, Vol. 3, Number 3,
Supplement 1, pp. 7–8. Copyright Taylor & Francis Co. Adapted with permission.
The Right Turns Only Program
Right Turns Only is a video-based drug education series produced by the Prince George’s
County, Maryland, school system. The effects of this series (including collateral print
material) on student knowledge, attitudes, and behavioral intentions were tested among
approximately 1,000 seventh grade students.
Twelve schools were assigned to one of four groups: three intervention groups and one
control group. One intervention group received only the video-based education, a second
received both the video-based and a traditional drug education curriculum, a third
received only the traditional curriculum, and the control group received no drug abuse
prevention education. All interventions were completed within a 3-week period.
The six outcomes measured included: 1) knowledge of substance abuse terminology, 2)
ability to assess advertisements critically, 3) perception of family, 4) conflict resolution,
5) self-efficacy in peer relationships, and 6) behavioral intentions related to substance
use/abuse prevention.
Changes were measured using data from questionnaires completed by students before and
after the interventions. The data were analyzed to identify differences based on gender,
race, grades (self-reported), and teacher. Groups that received drug education scored
higher than the control group on all posttest measures except self-efficacy. On two of the
six measures, the group receiving the combination of the video series and traditional
curriculum scored significantly higher than other groups.
Continued on next page...
114
Assessing Effectiveness and Making Refinements

EXAMPLES OF OUTCOME EVALUATION FOR COMMUNICATION PROGRAMS CONTINUED...
The evaluation demonstrated that instructional videos (particularly when used in
conjunction with print materials and teacher guidance) could be an effective tool for
delivering drug education in the classroom.
Note. Adapted from Evaluating the Results of Communication Programs (Technical Assistance Bulletin),
by Center for Substance Abuse Prevention, August 1998, Washington, DC: U.S. Government
Printing Office. In the public domain.
NIDDK’s “Feet Can Last a Lifetime” Program
In 1995 the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
developed a feedback mechanism for the promotion of its kit, “Feet Can Last a Lifetime,”
that was designed to reduce the number of lower extremity amputations in people with
diabetes. The first printing of the kit included a feedback form for health care providers to
comment on the materials. Based on the feedback, NIDDK revised the kit in 1997. The
new kit’s contents were then pretested extensively with practitioners for technical
accuracy, usefulness, and clarity. The original kit was developed primarily for providers;
based upon evaluation results, the revised kit also includes materials for patients. These
include an easy-to-read brochure; a fact sheet with “foot care tips” and a “to do” list that
contains steps for patients to follow to take care of their feet; and camera-ready, laminated
tip sheets for providers to reproduce and give to patients.
mass media component and a randomized
or quasi-experimental design to evaluate
the school-based component.
The following limitations can make
evaluation of your communication
program difficult:
• Lack of measurement precision (e.g.,
available data collection mechanisms
cannot adequately capture change or
cannot capture small changes). Population
surveys may not be able to identify the
small number of people making a change.
Self-reported measures of behavior
change may not be accurate.
• Inability to conclusively establish that the
communication activity caused the
observed effect. Experimental designs, in
which people are randomly assigned to
either receive an intervention or not, allow
you to assume that your program causes
the only differences observed between the
group exposed to the program and the
control group. Outcome evaluations with
experimental designs that run more than a
few weeks, however, often wind up with
contaminated control groups, either
because people in the group receiving the
intervention move to the control group, or
because people in the control group
receive messages from another source
that are the same as or similar to those
from your program.
The more complex your evaluation design
is, the more you will need expert assistance
to conduct your evaluation and interpret
your results. The expert can also help you
write questions that produce objective
results. (It’s easy to develop questions that
STAGE 4
Making Health Communication Programs Work
115

CONDUCTING CULTURALLY COMPETENT EVALUATION
When you evaluate communication programs, you form a set of assumptions about
what should happen, to whom, and with what results. Recognize that these assumptions
and expectations may vary, depending on the cultural norms and values of your
intended audiences.
You may need to vary your methods of gathering information and interpreting results.
Depending on the culture from which you are gathering information, people may react
in different ways:
• They may think it is inappropriate to speak out in a group, such as a focus group, or
to provide negative answers. (This does not mean that you should not use focus groups
within these cultures; observance of nonverbal cues may be more revealing than
oral communication.)
• They may be reluctant to provide information to a person from a different culture
or over the telephone.
• They may lack familiarity with printed questionnaires or have a limited ability to
read English.
Remember that the culture of the evaluator your program uses can inadvertently affect the
objectivity of your evaluation. When possible, try to use culturally competent evaluators
when you examine program activities. If your program cuts across cultures and you adapt
your evaluation methods to fit different groups, you may find it difficult to compare
results across groups. This type of evaluation is more complicated, and if you plan to
conduct one, enroll the help of an expert evaluator.
inadvertently produce overly positive
results.) If you do not have an evaluator on
staff, seek help to decide what type of
evaluation will best serve your program.
Sources include university faculty and
graduate students (for data collection and
analysis), local businesses (for staff and
computer time), state and local health
agencies, and consultants and organizations
with evaluation expertise.
4. Develop and Pretest Data
Collection Instruments
Most outcome evaluation methods involve
collecting data about participants through
observation, a questionnaire, or another
method. Instruments may include tally
sheets for counting public inquiries, survey
questionnaires, interview guides. Select a
method that allows you to best answer your
evaluation questions based upon your
access to your intended audience and your
resources. To develop your data collection
instruments—or to select and adapt existing
ones—ask yourself the following questions:
Which Data?
The data you collect should be directly
related to your evaluation questions.
Although this seems obvious, it is important
to check your data collection instruments
against the questions your evaluation must
answer. These checks will keep you focused
on the information you need to know and
116
Assessing Effectiveness and Making Refinements

ensure that you include the right measures.
For example, if members of your intended
audience must know more about a topic
before behavior change can take place,
make sure you ask knowledge-related
questions in your evaluation.
From Whom?
You will need to decide how many members
of each group you need data from in order
to have a sufficiently powerful evaluation to
assess change. Make sure you have
adequate resources to collect information
from that many people. Realize that you may
also need a variety of data collection
instruments and methods for the different
groups from whom you need information.
How?
Before you decide how to collect your data,
you must assess your resources. Do you
have access to, or can you train, skilled
interviewers? Must you rely on self-reports
from participants?
Also consider how comfortable the
participants will be with the methods you
choose to collect data. Will they be willing
and able to fill out forms? Will they be willing
to provide personal information to
interviewers? Will the interviews and
responses need to be translated?
5. Collect Data
Collect postprogram data.You should have
collected baseline data during planning in
Stage 1, before your program began, to use
for comparison with postprogram data.
6. Process Data
Put the data into usable form for analysis.
This may mean organizing the data to give
to professional evaluators or entering the
data into an evaluation software package.
7. Analyze the Data to Answer the
Evaluation Questions
Use statistical techniques as appropriate to
discover significant relationships.Your
program might consider involving university-
based evaluators, providing them with an
opportunity for publication and your program
with expertise.
8. Write an Evaluation Report
A report outlining what you did and why you
did it, as well as what worked and what
should be altered in the future, provides a
solid base from which to plan future
evaluations.Your program evaluation report
explains how your program was effective in
achieving its communication objectives and
serves as a record of what you learned from
both your program’s achievements and
shortcomings. Be sure to include any
questionnaires or other instruments in the
report so that you can find them later.
STAGE 4
Making Health Communication Programs Work
117

See Appendix A for a sample evaluation
report. As you prepare your report, you will
need someone with appropriate statistical
expertise to analyze the outcome evaluation
data. Also be sure to work closely with your
evaluators to interpret the data and develop
recommendations based on them.
Why?
Writing an evaluation report will bring
your organization the following
additional benefits:
• You will be able to apply what you’ve
learned to future projects. Frequently,
other programs are getting under way
when evaluation of an earlier effort
concludes, and program planners don’t
have time to digest what has been learned
and incorporate it into future projects.
A program evaluation report helps to
ensure that what has been learned will get
careful consideration.
• You will show your accountability to
employers, partners, and funding
agencies. Your program’s evaluation report
showcases the program’s accomplishments.
Even if some aspects of the program need
to be modified based on evaluation
results, identifying problems and
addressing them shows partners and
funding agencies that you are focused on
results and intend to get the most benefit
from their time and money.
118

• You will be able to give evidence of your
program and methods’ effectiveness. If
you want other organizations to use your
materials or program, you need to
demonstrate their value. An evaluation
report offers proof that the materials and
your program were carefully developed
and tested. This evidence will help you
explain why your materials or program may
be better than others, or what benefits an
organization could gain from using its time
and resources to implement your program.
• You will provide a formal record that will
help others. A comprehensive evaluation
report captures the institutional memory of
what was tried in the past and why, which
partners had strong skills or experience in
specific areas, and what problems were
encountered. Everything you learned
when evaluating your program will be
helpful to you or others planning
programs in the future.
How?
Consider the Users
Before you write your evaluation, consider
who will read or use it. Write your report for
that audience. As you did when planning
your program components in Stage 1,
analyze your audiences for your report
before you begin to compose. To analyze
your audience, ask yourself the
following questions:
• Who are the audiences for this
evaluation report?
— Public health program administrators
— Evaluators, epidemiologists,
researchers
— Funding agencies
— Policymakers
— Partner organizations
— Project staff
— The public
— The media
EVALUATION REPORT HELPS CIS
P
ROMOTE PROGRAM AREAS, STRENGTHS
NCI’s CIS used an evaluation report,
“Making a Difference,” to show its
partners, the research community,
NCI/CIS leadership, and the media that
its programs are effective. The
document both quantified CIS results
(e.g., making 100,000 referrals a year to
research studies, providing information
on breast cancer to 76,000 callers in
1996, providing information that
increased fruit and vegetable
consumption among callers) and put a
human face on the calling public.
Quotations from callers and leaders in
the cancer community illustrated the
personal impact of the service on
people’s lives and health.
The report was written in lay language
and used pullouts and simple charts to
explain statistics. Ideas for using the
report with regional partners, the
media, and community leaders were
included with the copies sent to each
CIS office. To maximize opportunities
for using the report, CIS has also made
it available on computer disk and as a
PowerPoint
®
slide presentation.
• How much information will your
audience want?
— The complete report
— An executive summary
— Selected sections of the report
• How will your audience use the
information in your report?
— To refine a program or policy
— To evaluate your program’s performance
— To inform others
— To support advocacy efforts
— To plan future programs
STAGE 4
Making Health Communication Programs Work
119

Consider the Format Letting others know about the program
Decide the most appropriate way to present
information in the report to your audience.
Consider the following formats:
• Concise, including hard-hitting findings
and recommendations
• General, including an overview written for
the public at the ninth-grade level
• Scientific, including a methodology
section, detailed discussion,
and references
• Visual, including more charts and graphics
than words
• Case studies, including other
storytelling methods
Selected Elements to Include
Depending on your chosen audience and
format, include the following sections:
• Program results/findings
• Evaluation methods
• Program chronology/history
• Theoretical basis for program
• Implications
• Recommendations
• Barriers, reasons for unmet objectives
9. Disseminate the Evaluation Report
Ask selected stakeholders and key
individuals to review the evaluation report
before it is released so that they can identify
concerns that might compromise its impact.
When the report is ready for release,
consider developing a dissemination
strategy for the report, just as you did for
your program products, so the intended
audiences you’ve chosen will read it. Don’t
go to the hard work of writing the report
only to file it away.
results and continuing needs may prompt
them to share similar experiences, lessons,
new ideas, or potential resources that you
could use to refine the program. In fact,
feedback from those who have read the
evaluation report or learned about your
findings through conference presentations
or journal coverage can be valuable for
refining the program and developing new
programs.You may want to develop a formal
mechanism for obtaining feedback from peer
or partner audiences. If you use university-
based evaluators, the mechanism may be
their publication of findings.
If appropriate, use the evaluation report to
get recognition of the program’s
accomplishments. Health communication
programs can enhance their credibility with
employers, funding agencies, partners, and
the community by receiving awards from
groups that recognize health programs,
such as the American Medical Writers
Association, the Society for Technical
Communication, the American Public Health
Association, and the National Association of
Government Communicators. A variety of
other opportunities exist, such as topic-
specific awards (e.g., awards for consumer
information on medications from the U.S.
Food and Drug Administration) and awards
for specific types of products (e.g., the
International Communication Association’s
awards for the top three papers of the year).
Another way to get recognition is to publish
articles about the program in professional
journals or give a presentation or workshop
at an organization meeting or conference.
120
Assessing Effectiveness and Making Refinements

Refining Your Health
Communication Program
The health communication planning process
is circular. The end of Stage 4 is not the end
of the process but the step that takes you
back to Stage 1. Review the evaluation
report and consider the following to help you
identify areas of the program that should be
changed, deleted, or augmented:
• Goals and objectives:
— Have your goals and objectives shifted
as you’ve conducted the program? If
so, revise the original goals and
objectives to meet the new situation.
— Are there objectives the program is not
meeting? Why? What are the barriers
you’re encountering?
— Has the program met all of your
objectives, or does it seem not to be
working at all? Consider ending
the program.
• Where additional effort may be needed:
— Is there new health information that
should be incorporated into the
program’s messages or design?
— Are there strategies or activities that did
not succeed? Review why they didn't
work and determine what can be done
to correct any problems.
• Implications of success:
— Which objectives have been met, and
by what successful activities?
— Should successful communication
activities be continued and
strengthened because they appear to
work well or should they be considered
successful and completed?
— Can successful communication
activities be expanded to apply to other
audiences or situations?
• Costs and results of different activities:
— What were the costs (including staff
time) and results of different aspects
of the program?
— Do some activities appear to work as
well as, but cost less than, others?
• Accountability:
— Is there evidence of program
effectiveness and of a continued need
to persuade your organization to
continue the program?
— Have you shared the results of your
activities with the leadership of
your organization?
— Have you shared results with partners?
— Do the assessment results show a
need for new activities that would
require partnerships with
additional organizations?
Once you have answered the questions
above and decided what needs to be done
to improve the program, use the planning
guidelines in Stage 1 to help determine new
strategies, define expanded or different
intended audiences, and rewrite/revise your
communication program plan to accommodate
new approaches, new tasks, and new
timelines. Review information from the other
stages as you plan the next phase of
program activities.
Common Myths and Misconceptions
About Evaluation
Myth: We can’t afford an evaluation.
Fact
: Rarely does anyone have access to
adequate resources for an ideal health
communication program, much less an ideal
evaluation. Nevertheless, including
evaluation as a part of your work yields the
practical benefit of telling you how well your
program is working and what needs to be
changed. With a little creative thinking, some
form of useful evaluation can be included in
almost any budget.
STAGE 4
Making Health Communication Programs Work
121

Myth: Evaluation is too complicated. No
one here knows how to do it.
Fact:
Many sources of help are available for
designing an evaluation. Several pertinent
texts are included in the selected readings
at the end of this section. If your
organization does not have employees with
the necessary skills, find help at a nearby
university or from someone related to your
program (e.g., a board member, a volunteer,
or someone from a partner organization).
Also, contact an appropriate clearinghouse
or Federal agency and ask for evaluation
reports on similar programs to use as
models. If the program has enough
resources, hire a consultant with experience
in health communication evaluation. Contact
other communication program managers
for recommendations.
Myth: Evaluation takes too long.
Fact:
Although large, complicated outcome
evaluation studies take time to design and
analyze (and may require a sufficient time
lapse for changes in attitudes or behavior to
become clear), other types of evaluation can
be conducted in a few weeks or months, or
even as little as a day. A well-planned
evaluation can proceed in tandem with
program development and implementation
activities. Often, evaluation seems
excessively time-consuming only because it
is left until the end of the program.
Myth: Program evaluation is too risky.
What if it shows our funding source (or
boss) that we haven’t succeeded?
Fact:
A greater problem is having no results
at all. A well-designed evaluation will help
you measure and understand the results
(e.g., if an attitude or a perception did not
change, why not?). This information can
direct future initiatives and help the public
health community learn more about how to
communicate effectively. The report should
focus on what you have learned from
completing the program evaluation.
Myth: We affected only 30 percent of
our intended audience. Our program
is a failure.
Fact:
Affecting 30 percent of the intended
audience is a major accomplishment; it
looks like a failure only if your program’s
objectives were set unrealistically high.
Remember to report your results in the
context of what health communication
programs can be expected to accomplish.
If you think the program has affected a
smaller proportion of the intended audience
than you wanted, consult with experts
(program planning, communication, or
behavioral) before setting objectives for
future programs.
122
Assessing Effectiveness and Making Refinements

Myth: If our program is working, we should
see results very soon.
Fact
: Results will vary depending on the
program, the issue, and the intended
audience. Don’t expect instant results;
creating and sustaining change in attitudes
and particularly in behavior or behavioral
intentions often takes time and commitment.
Your program may show shorter term,
activity-related results when you conduct
your process evaluation; these changes in
knowledge, information seeking, and skills
may occur sooner than more complex
behavioral changes.
Selected Readings
Academy for Educational Development.
(1995). A tool box for building health
communication capacity. Washington, DC.
Agency for Toxic Substances and Disease
Registry. (1994). Guidelines for planning and
evaluating environmental health education
programs. Atlanta.
Center for Substance Abuse Prevention.
(1998). Evaluating the results of
communication programs [Technical
Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Flay, B. R., & Cook, T. D. (1989). Three
models for evaluating prevention campaigns
with a mass media component. In R. E. Rice
& C. K. Atkin (Eds.), Public communication
campaigns (2nd ed.). Thousand Oaks,
CA: Sage.
Flay, B. R., Kessler, R. C., & Utts, J. M.
(1991). Evaluating media campaigns. In
S. L. Coyle, R. F. Boruch, & C. F. Turner
(Eds.), Evaluating AIDS prevention
programs. Washington, DC: National
Academy Press.
Morra, M. E. (Ed.). (1998). The impact and
value of the Cancer Information Service: A
model for health communication. Journal of
Health Communication, 3(3) Suppl.
Muraskin, L. D. (1993). Understanding
evaluation: The way to better prevention
programs. Washington, DC: U.S.
Department of Education.
Rice, R. E., & Atkin, C. K. (2000). Public
communication campaigns (3rd ed.).
Thousand Oaks, CA: Sage.
Rossi, P. H., Freeman, H. E., & Lipsey,
M. W. (1998). Evaluation: A systematic
approach (6th ed.). Thousand Oaks,
CA: Sage.
Siegel, M., & Doner, L. (1998). Marketing
public health: Strategies to promote social
change. Gaithersburg, MD: Aspen.
Windsor, R. W., Baranowski, T. B., Clark,
N. C., & Cutter, G. C. (1994). Evaluation of
health promotion, health education and
disease prevention programs (2nd ed.).
Mountain View, CA: Mayfield.
STAGE 4
Making Health Communication Programs Work
123

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
METHODS
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Communication
Research Methods
In This Section:
• Types of communication research
• Differences between qualitative and quantitative research methods
• Qualitative research methods
• Quasi-quantitative research methods
• Quantitative research methods
METHODS

QUALITATIVE VERSUS QUANTITATIVE METHODS
Types of Communication Research
Research into intended audiences’ culture,
lifestyle, behaviors and motivations, interests,
and needs is a key component to a health
communication program’s success. This
section describes communication research
methods commonly used throughout
program planning. See the chart Types
of Research and Evaluation for more detail
about research conducted in each of
the stages of health communication
program planning.
Most programs use more than one research
method. For example, conducting exploratory
focus groups with an intended audience at
the start of program planning can orient you
to the types of approaches, messages, and
channels that are most likely to be successful
with a particular group. In some cases, focus
groups might be augmented with in-depth
interviews to learn more about intended
audience members’ motivations. Later,
messages and materials might be pretested
Qualitative
Provides depth of understanding
Asks “Why?”
Studies motivations
Is subjective; probes individual reactions
to discover underlying motivations
Enables discovery
Is exploratory
Allows insights into behavior and trends
Interprets
with the intended audience, using central-
location intercept interviews to more closely
approximate how an individual would
encounter them in “real life.” Theater-style
testing also approximates reality, using a
simulated television-viewing environment.
Clearly, some methods are better suited to
specific purposes than others. Using
multiple methods can help ensure that you
get an accurate picture of your intended
audience members and their likely
responses to your program.
Differences Between Qualitative and
Quantitative Research Methods
There are two basic types of research you
might conduct with intended audiences:
qualitative and quantitative.You will use
methods from one of these two types
depending upon what you want to learn.
See the sidebar below, Qualitative Versus
Quantitative Methods, for common
distinctions between qualitative and
quantitative research.
Quantitative
Measures level of occurrence
Asks “How many?” and “How often?”
Studies actions
Is objective; asks questions without
revealing a point of view
Provides proof
Is definitive
Measures levels of actions and trends
Describes
Note. From Methodological Review: A Handbook for Excellence in Focus Group Research by M. Debus.
Copyright 1988 by The Academy for Educational Development, Washington, DC. Reprinted
with permission.
126
Communication Research Methods

In this section, you will learn when to use
each type of research, how to conduct
research with members of your intended
audience, and how you can use the data
you collect to inform your project.
Qualitative, quasi-quantitative, and
quantitative research methods are
discussed separately.
Qualitative Research
Use qualitative research methods when:
• You are planning a communication
program and developing materials for it
• When the goal of your research is to
explore a topic or idea
• When the goal of your research is to gain
insights into an intended audience’s
lifestyle, culture, motivations, behaviors,
and preferences
Conduct qualitative research by:
• Selecting a small group of people chosen
for particular characteristics
• Convening a discussion (i.e., a focus
group or in-depth interview) or observing
individuals’ behaviors in schools, malls,
supermarkets, etc.
• Keeping the discussion fairly unstructured,
so that participants are free to make any
response and are not required to choose
from a list of possible responses
• Choosing which question to ask next
based on your participants’
previous responses
Qualitative research results cannot be:
• Quantified or subjected to
statistical analysis
• Projected to the population from which the
respondents were drawn because
participants are not selected randomly (to
be representative of the population as a
whole) and because not all participants
are asked precisely the same questions
Quantitative Research
Use quantitative research methods when:
• You are planning a communication
program (e.g., to measure the prevalence
of a particular behavior) or assessing a
program already in place
• The goal of your research is measurement
of particular variables
Conduct quantitative research by:
• Selecting a large group or groups
of people
• Using a structured questionnaire
containing predominantly forced-choice
or closed-ended questions
Quantitative research results can be:
• Analyzed using statistical techniques
• Considered representative of the
population from which the respondents
were drawn if each person in the
population had an equal chance of
being included
Qualitative Research Methods
Use qualitative research methods during
the following parts of your program:
• Stage 1—to find out more about your
intended audiences and to learn what
the priorities and approach should be
for trying to influence their awareness,
knowledge, attitudes, intentions,
or behaviors
METHODS
Making Health Communication Programs Work
127

TYPES OF RESEARCH AND EVALUATION
Stage
Stage 1
Planning and
Strategy Development
Stage 2
Developing and
Pretesting Concepts,
Messages, and Materials
Type of
Research/Evaluation
Consumer Research,
Market Research
Provides information on
the problem, intended
audiences, and barriers
to and opportunities
for change
Pretesting
Assesses reactions to
proposed messages or
materials
Pilot or Field Testing
Assesses program
activities in limited areas
and/or time periods
Benefits
Answers questions
such as:
What dimensions of the
health problem do we need
to address?
How should the population
be segmented and which
intended audience should
be targeted?
What are the best ways
of reaching the
intended audience?
What benefits would be
credible and appealing to
the intended audience?
What images should
be conveyed?
What barriers need to
be overcome?
What actions can the
intended audience take?
Tests and refines
messages and materials
prior to production
Tests and refines activities
prior to full-scale
implementation
Continued on next page...
128
Communication Research Methods

TYPES OF RESEARCH AND EVALUATION CONTINUED...
Stage
Stage 3
Implementing
the Program
Stage 4
Assessing Effectiveness
and Making Refinements
Type of
Benefits
Research/Evaluation
Process Evaluation
Documents and assesses
Identifies areas for
implementation; quantifies
improvement as
what was done; when,
implementation proceeds
where, and how it
was done; and who
Documents progress of
was reached
implementation
Outcome Evaluation
Measures whether, and
Documents the extent of
to what extent, a program
the campaign’s success
or activity had the
or failure
planned effects
Documents success to
support replication
Determines any need to
improve the existing
program or future efforts
Impact Evaluation
Measures whether, and
Is not often used for health
to what extent, a
communication activities
program contributed to
(improving health status
long-term goals
usually requires
multifaceted approaches—
e.g., communication plus
changes in health care
service delivery and
relevant policies—and it is
generally not possible to
isolate a particular
communication program’s
contribution to achieving
longer-term goals)
METHODS
Making Health Communication Programs Work
129

• Stage 2—to determine whether your
materials communicate the intended
messages effectively and persuasively
• Stage 3—to understand why the program
is or isn’t working as expected
• Stage 4—to learn more about what
worked and what didn’t, and why certain
outcomes occurred
Focus groups and in-depth interviews are
the most common methods used in
qualitative communication research.
However, there are many innovative
methods, some described here, that can
help you learn about an audience. Because
the methodologies for each are very similar,
they are discussed together here, using
instructions for focus groups as a guide.
About Focus Groups
Working from a discussion guide, a skilled
moderator facilitates a 1- to 2-hour
discussion among 6 to 10 participants,
which can be conducted either in person or
by telephone (ideally in person). The
moderator keeps the session on track while
participants talk freely and spontaneously.
As new topics related to the material
emerge, the moderator asks additional
questions to learn more.
Common Uses
• Developing a communication strategy:
—Learning about feelings, motivators,
and past experiences related to a
health topic
—Exploring the feasibility of various
potential actions (from the intended
audience’s viewpoint)
—Identifying barriers to those actions
—Exploring what benefits the intended-
audience members find compelling and
what results they expect from taking a
particular action
—Learning about the intended-audience’s
use of settings, channels, and activities
—Capturing the language used by the
intended audience to discuss issues
• Exploring reactions to message concepts
(concept testing):
—Identifying concepts that do or do not
resonate and understanding why
—Triggering the creative thinking of
communication professionals
—Illustrating to others how the intended
audience thinks and talks about a
health issue
• Developing hypotheses (or broad issues)
for quantitative studies and identifying the
range of responses that should be
included in closed-ended questionnaires
WORKING WITH MARKET RESEARCH PROFESSIONALS
You may need to hire or contract with two kinds of market research professionals as you
design, conduct, and analyze your concept and materials testing:
1. Someone to design the research and data instruments (e.g., questionnaires, discussion
guides, screeners), to analyze the results, and to prepare a report
2. A vendor to handle the fieldwork (i.e., recruiting and hosting focus groups;
administering telephone, mail, or in-person surveys)
Continued on next page...
130
Communication Research Methods

WORKING WITH MARKET RESEARCH PROFESSIONALS CONTINUED...
Ideally, these professionals will have a background in health communication or, if not, a
background in marketing or advertising research. You can get the best service from these
professionals by:
• Providing clear research objectives and appropriate background information, including
the creative brief.
• Learning enough about common communication research methods to understand their
strengths and limitations, so that you don’t ask for more than a given method can
deliver (e.g., asking, “What percentage of the American public does that represent?”
when a focus group study was conducted).
• Letting market researchers’ expertise guide your selection of methods. Rather than
saying, “We want to focus test this,” explain your research objectives, timing, budgetary
constraints, and any additional factors (such as the need for a publication to be tested
with people from a wide range of cultures). Then let the experts propose methods to you
and explain their rationale.
• Being realistic about timelines, quantity of information, materials to be tested at one
time, and the level of “proof” you need. Pretesting is diagnostic; it can provide guidance
on what needs to be improved, but it can’t tell you how successful something will be.
Other factors, such as the final production of your message, the number of people who
see it, the frequency with which it is seen, and the presence of competing messages will
all influence your message’s success.
• Recognizing that there are inherent differences between testing advertising and other
commercial communication materials versus testing health communication materials,
even if the channel and activity (e.g., a television spot) are the same. Individuals trained
in commercial concept development and copy testing will be able to draw on their
commercial experience for selecting the appropriate methodology. However, they often
have little experience assessing reactions to complex health messages; they are more
familiar with assessing efforts to direct an existing behavior toward use of a particular
product brand than with assessing efforts to completely change a behavior.
Sometimes, one individual or organization can play both roles; at other times, you may
have internal staff, a consultant, or staff at a health communication firm to handle the
first role but contract externally for the second. The American Marketing Association’s
Green Book lists suppliers and services geographically throughout the United States. Other
sources include the Marketing Research Association, the Association of Public Opinion
Researchers, the Qualitative Research Consultants Association, and faculty at university
departments of marketing, communication, health education, psychology, and sociology.
METHODS
Making Health Communication Programs Work
131

132

• Providing insights into the results of
quantitative studies by obtaining in-depth
information from individuals typical of the
intended audience to help understand why
individuals responded in certain ways
Pros
• Group interaction can help elicit in-depth
thought and discussion.
• Group interaction can help with
brainstorming because respondents can
build off one another’s ideas.
• Moderators have considerable opportunity
to probe responses.
• Focus groups yield richer data than
surveys about the complexities of an
intended audience’s thinking and behavior.
Cons
• Findings are not generalizable to
the population.
• Focus groups can be labor intensive and
expensive, especially if sessions are
conducted in multiple locations.
• Group responses do not necessarily
reflect individuals’ opinions because some
individuals in the group may dominate
the discussion or may influence
others’ opinions.
• Each person is limited to about 10 minutes
of talking.
About In-Depth Interviews
The process, benefits, and drawbacks of
in-depth interviews are similar to those of
focus groups, except that the interviewer
speaks with one person at a time. In-depth
interviews can take place at a central facility
or at the participant’s home or place of
business. As with focus groups, when
individual interviews cannot be conducted
in person, they can be conducted by phone
or over the Internet. Although these
interviews are more time intensive, one of
their key benefits is that each respondent is
isolated from other respondents and
therefore not influenced by what others say.
How to Design and Conduct a Focus Group
or In-Depth Interview Study
To design and conduct a qualitative
research study, complete the
following steps.
Plan the Study
Determine the following:
• What you want to learn. Determine the
objectives of your study at the outset, and
then check to make sure that the
moderator’s/interviewer’s guide includes
lines of questioning that will provide the
answers.You may also use the objectives
to help analyze the results of the
discussions and to organize the focus
group or in-depth interview report.
• When you need to have that information.
• How you will apply what you learn. It is
important to decide how you will use your
focus group or in-depth interview results
before you conduct your study.
• Your budget.
• Your criteria for who should participate.
Select people who are:
—Typical of your intended audience (the
same behavioral, demographic, and
psychographic characteristics).You may
want to conduct separate groups with
“doers” (those who already engage in
the desired behavior) and “nondoers”
(those who do not) to help identify what
actions the doers take, and why, so that
those approaches can be explored with
the nondoers.
METHODS
Making Health Communication Programs Work
133

—Not experts. Exclude market
researchers and advertising
professionals (because of their
familiarity with the methodology) and
those who have, or might be perceived
by other group members as having,
expertise in the subject matter (e.g.,
exclude health professionals from focus
groups when the topic is a health issue).
—Relative newcomers to focus groups or
interviews, so that their reactions will be
spontaneous. This will help you avoid
“professional” respondents (i.e., those
who have participated in many previous
focus groups or individual interviews
before) who may lead or monopolize
the discussion.
• The number of groups you will convene.
—Divide participants into different focus
groups based on their gender, race,
age, level of formal education, or any
other variable likely to hinder their
freedom of expression (e.g., teenage
girls will be more comfortable
discussing sexual activity if teenage
boys or college-age women are not in
the group).
—Conduct a minimum of two focus groups
with each intended audience segment
(e.g., if you are conducting separate
groups with men and women, you will
need at least four groups—two with
men, two with women). If intended
audience perceptions vary or the
audience feedback is unclear, you may
want to conduct additional groups with
each segment, especially if you revise
the discussion guide to more fully
explore unresolved issues.
—If you are using in-depth interviews,
conduct approximately 10 interviews
per intended audience segment. If
common themes do not emerge or the
intended audience feedback is unclear,
you may want to conduct additional
interviews, especially if you revise the
interview guide in between interviews.
Choose the Location
You can convene focus group discussions or
in-depth interviews in a variety of ways:
• Commercial focus group facilities can
recruit participants for you (for both focus
groups and interviews) and offer audio
and video recording equipment as well as
observation rooms with one-way mirrors
for viewing. However, these facilities are
usually available only in larger
metropolitan areas.
• Teleconference services can set up
telephone focus groups for you. Most allow
observers to listen without being heard,
and some provide remote viewing
programs to allow the moderator to see a
list of participant names (with a symbol
next to the one currently speaking) or
notes sent in by a technician from
observers listening to the call. Some
teleconference services can recruit
participants; with others, you will have to
recruit participants or contract with a
recruiter separately.
• You can also conduct focus groups or
in-depth interviews in meeting rooms at
churches, office buildings, or other
locations. If an observation room with a
one-way mirror is not available, staff may
still listen in through speakers hooked up
in a nearby room or by audiotaping or
videotaping the session. In some cases,
one or two quiet observers may be
allowed in the room to take notes.
See the sidebar Pros and Cons of Different
Formats on the next page for the advantages
and disadvantages of different formats for
focus group and in-depth interview research.
134
Communication Research Methods

PROS AND CONS OF DIFFERENT FORMATS
Format Pros Cons
Face-to-Face
Moderator/interviewer and Can assess body language Responders lose some
participants are in one room, If videotaped, can share with anonymity
usually around a table; others who couldn’t attend
observers (members of the
Higher travel expenses due
research team) are behind a
Have participants’ to multiple locales
one-way mirror
undivided attention
Usually excludes people in
rural areas or small towns
Telephone
Moderator/interviewer and
More convenient for
Can’t assess nonverbal
participants are on a
participants and observers
reactions
conference call; observers
listen in
Can easily include people in
More difficult to get reactions to
rural areas, in small towns, and
visuals (although they can be
who are homebound
sent ahead of time)
For professional groups, may
Participants can be distracted
be easier to gain participation
by their surroundings
because it is less likely
participants will know
each other
Relative anonymity may result
in more frank discussion of
sensitive issues
Internet Chat Sessions
Moderator and participants
Complete record of session
Only useful for participants
“chat”; observers watch
instantly available
comfortable with this mode
of communication
Relative anonymity may result
in more frank discussion of
Relatively slow pace limits
sensitive issues
topics that can be covered
No way to assess if
participants meet
recruitment criteria
Can’t assess body language
or tone of voice
More difficult to get reaction
to visuals
METHODS
Making Health Communication Programs Work
135

Draft a Recruitment Screener Recruit Participants
A recruitment screener is a short
questionnaire that is administered to
potential participants, typically by telephone,
to ensure that they meet the criteria you
developed during step 1. Ideally, the
screener should help you exclude
participants who are already familiar with
the specific subject of the sessions, or who
know each other. If participants know the
subject in advance, they may formulate
ideas or may study to become more
knowledgeable about the subject than the
typical intended audience member. If
participants know each other, they may
speak less freely. See Appendix A for a
sample screener.
Recruit participants by telephone one to
three weeks in advance of the sessions.
You can identify potential participants in
different ways depending upon the type of
people you are seeking and the resources
you have available. Identify members of the
public through focus group facility
databases, by running an ad in a local
publication, by working with community
organizations, or by using the phone book
(although the latter will be extremely time
consuming if you have stringent recruitment
criteria). Identify professionals through a
relevant association or mailing list service or
through a focus group facility’s recruiting
databases. Depending on your budget and
CONTRACTING WITH COMMERCIAL FACILITIES
Before you contract with a commercial facility to conduct in-depth interviews or focus
groups, prepare a specification sheet detailing all of the services you need and, if you will
be asking the facility to recruit, a profile of your intended audience. Vendors will use this
information to estimate the cost of the project and to develop bids.
Decide whom to approach by using the following checklist to determine which vendors
will fit your needs. Each vendor should provide the following information:
• Descriptions of past projects
• Descriptions of, or a list of, clients
• Location of facility (Is the facility conveniently located? Is parking available? Is the
facility accessible by public transportation? If not, does vendor provide transportation
assistance, such as taxi money or van service? What does this add to cost?)
• Diagram of table/seating arrangement (What size and shape are tables? Rooms?)
• Description of the size and features of observation rooms
• Details about audio and video recording arrangements and costs
• Details about food arrangements for participants and clients
• Description of moderator services
• Description of recruitment methods and geographic coverage
• Recommendations for participant incentives
• Reasonable rates for the services they will provide (ask for nonprofit rates, if appropriate)
136
Communication Research Methods

internal resources, you may choose to
recruit in one of the following ways:
• Use your own organization’s staff to
recruit participants.
• Hire a focus group facility or independent
recruiter (to identify such facilities, consult
a directory such as the American
Marketing Association’s Green Book or
the Marketing Research Association’s
Blue Book). If you have many facilities
and recruiters to choose from, consider
getting recommendations from local
corporations or organizations that conduct
qualitative research.
• Get help from a university marketing
research or advertising class.
• Work through gatekeepers such as
teachers (for students), health care
providers (for patients, physicians, or
nurses), religious institutions or
community organizations (a small
donation may encourage them to
participate), and instructors of English as
a second language.
Regardless of how the recruiting is done,
ensure that the screener is followed
carefully so that only individuals who qualify
for participation will be included.
Getting People to Show Up
To ensure that enough people show up, offer
an incentive (usually money) and recruit two
or three more people than you actually
need. If all show up, select those who best
fit the screening criteria, thank the extra
participants, give them the agreed-upon
incentive, and dismiss them. Other ways to
increase participation include:
• Scheduling sessions at times that are
convenient for your potential participants
(e.g., at lunch or after work)
• Choosing a safe and convenient site with
easy parking
• Providing transportation (or
reimbursement for agreed-upon
transportation costs)
• Arranging for childcare, if necessary
• Letting them know you will be
serving refreshments
Recruiting Patients and Their Families
Recruiting patients and their families
requires special consideration. Contact
clinics, hospitals, or local HMOs for help
and make adequate plans to ensure that
the participants and their family members
are not inconvenienced or upset. Some
organizations may require institutional
review board (IRB) approval of your
research. Gaining IRB approval is often a
long process, so be sure you check with the
organization early in the planning stage of
your study to find out whether you will need
IRB approval.
Recruiting for Telephone Interviews
If you are recruiting for in-depth interviews to
be conducted on the telephone, create a
spreadsheet that includes spaces for the
following information about each potential
participant:
• Time zone in which the person is located
• Date, time, and telephone number at
which he or she should be called for
the interview
• Disposition of each call (e.g., scheduled
an interview, no answer, busy, refused)
Develop a Moderator’s Guide
The moderator’s guide tells the moderator
what information you want from the groups
and helps him or her keep the discussion on
track and on time. It is only a guide,
however. During the focus groups,
METHODS
Making Health Communication Programs Work
137

WORKING WITH COMMUNITY ORGANIZATIONS TO CONDUCT FOCUS GROUPS
Once you have identified potentially cooperative community groups (see the following
sidebar for a list of groups you might approach), contact an official within each group
(e.g., the president or program director) to request cooperation. You may make these
initial contacts by telephone and follow up with a formal written request that includes
the following:
• Description of your agency or organization
• Description of the material/topic to be discussed and its purpose
• Details regarding the participants to be recruited and how you will protect
their confidentiality
• Outline of the activities involved
• Incentives you are offering the organization and the participants
• Detailed explanation of why the organization official should not reveal details about
the nature of the discussion to participants in advance, unless the organization is to
recruit participants
• If and how you will share the information learned
Once you have an agreement with a community organization, decide how you will recruit
participants. One possibility is to conduct your research as part of the group’s regularly
scheduled meeting.
The advantages of this approach are:
• Little extra effort is required to recruit participants.
• You may need to provide only minimal or no incentives.
• The group’s regular and familiar meeting place can be used.
The disadvantages of this approach are:
• You have little control over the number of people who will come or the composition
of the group.
• It is difficult to place a 1- to 2-hour focus group on the agenda of a regularly
scheduled meeting.
• Many organizations set their calendars months ahead of time (it may be difficult to
schedule the focus group within a reasonable time frame).
An alternative is to recruit the group’s members to a special meeting. Schedule this
meeting immediately before or after the group’s regular meeting to make it most
convenient for the participants. If you use this alternative, contact members in advance
on behalf of the group and ask them to participate. A person from the community group
can also ask others to participate. To ensure that participants attend and stay through the
whole meeting, let them know in advance that you will be providing refreshments
(assuming that you are doing so).
Continued on next page...
138
Communication Research Methods

WORKING WITH COMMUNITY ORGANIZATIONS TO CONDUCT FOCUS GROUPS CONTINUED...
The advantages of recruiting participants to a special meeting are:
• It provides an opportunity to screen participants on relevant characteristics and to
eliminate market researchers or other experts who should not participate.
• It helps reduce participant fatigue because the entire meeting will be devoted to
your research.
If you recruit participants yourself, you will have more control over what the participants
are told about the focus group, and you will be able to screen potential participants to
make certain that they fit special intended audience characteristics. However, recruiting
participants takes a significant amount of time, and it is possible that people would be
more likely to participate if asked by someone whom they know.
If the member organization recruits participants, it is essential that you provide the
recruiter with detailed instructions for carrying out the task. These instructions must
include a written description of the focus group topic, which should be read to potential
participants verbatim, and a questionnaire to screen participants on relevant criteria.
experienced moderators flow with the
conversation, asking questions in the
prescribed language and sequence when
possible but sometimes deviating from the
guide to avoid awkward transitions or
unnecessary back-and-forth between topics.
Before you draft the moderator’s guide,
answer the following questions:
• What do we want to learn from the
focus group?
• How will we apply what we learn?
• What tools (e.g., descriptive information,
message concepts, or other draft creative
work) will we need to provide?
Then, write questions for the guide that
relate to the purposes you have identified.
Make most questions open-ended so that
participants can provide more in-depth
responses than just “yes” or “no,” but make
sure the questions are not leading. This will
help you get answers that reflect
participants’ true feelings and not what they
think you would like to hear. The amount of
time and depth of questions devoted to each
issue should reflect the value of the issue to
the research. See Appendix A for an
example of a moderator’s guide.
Do not include questions for group
discussion when you need individual
responses. However, you can have the
moderator give self-administered
questionnaires to each participant to be
completed prior to conducting a focus group,
or participants can be asked to individually
rank items on paper—such as potential
actions, benefits, or message concepts—
during a group to obtain both individual and
group reactions.
Conduct the Focus Groups
Focus groups typically begin with the
moderator welcoming participants and
briefing them on the process (e.g., all
opinions welcome—there are no right or
wrong answers; the presence of audio- and
METHODS
Making Health Communication Programs Work
139

videotaping and observers; the importance
of speaking one at a time; confidentiality).
Participants introduce themselves to the
group by first name, usually including some
information relevant to the topic of
discussion (e.g., number of years with
glaucoma, amount/type of insulin used each
day). Next, the moderator asks a few simple
“ice-breaker” questions to help participants
get used to the group process and to
reduce participant anxiety. This also helps
the moderator develop rapport with
the participants.
Continuing to follow the moderator’s guide,
the moderator manages the group and
ensures that all topics are covered without
overtly directing the discussion. Participants
are encouraged to express their views and
even disagree with each other about the
discussion topics. The moderator does not
simply accept what participants say but
probes to learn more about participants’
underlying thinking and attitudes. The
moderator also seeks out opinions from all
participants so that all are heard and a few
do not dominate the discussion.
Near the end of the discussion, the
moderator will often give participants an
activity or simply excuse him- or herself from
the room for a moment to check with the
observers and obtain any additional
questions. Alternatively or additionally, notes
can be sent in to the moderator while the
group is in process if the observers would
like different questions asked or other
changes made to the group.
One advantage of focus group methodology
is that the moderator’s guide, and any
materials presented, can be revised
between groups if necessary.
EXAMPLES OF COMMUNITY
ORGANIZATIONS TO CONTACT FOR HELP
RECRUITING PARTICIPANTS
American Legion
B’nai B’rith Women
Business groups
Jaycees
Junior League
Knights of Columbus
League of Women Voters
Lions Club
NAACP
National Council of Negro Women
National Urban League
Parent Teacher Associations
Religious organizations
Rotary Club
Schools
Senior citizen centers
Unions
Veterans of Foreign Wars
YWCA/YMCA
Analyze Results
The easiest and most thorough way to
analyze focus groups is by reviewing
transcripts, although groups can also be
analyzed (albeit less thoroughly) by
reviewing notes taken during the discussion.
In many analyses, the goal is to look for
general trends and agreement on issues. At
the same time, it is important to note
divergent opinions. Don’t ignore individual
comments that raise interesting ideas or
concerns such as lack of cultural sensitivity
or difficulty in comprehension. In some
instances, the goal is to capture the range of
opinions about an issue, rather than to look
for evidence of agreement or consensus.
140
Communication Research Methods

Avoid counting or quantifying types of
responses (e.g., “75 percent of participants
preferred concept A”). Attempting to quantify
the results—or suggesting in other ways that
they represent the opinions of the intended
audience as a whole—is inappropriate for
qualitative research.
Quasi-Quantitative Research Methods:
Pretesting Messages and Materials
Some commonly used communication
research methods, such as central-location
intercept interviews and theater tests, are
best termed quasi-quantitative. While these
methods are used in situations in which the
goal is measurement and typically involve a
questionnaire with mostly forced-choice
questions, the results cannot be projected to
the population as a whole (as with true
quantitative surveys) because of the way in
which participants are selected. For central-
location intercept interviews, the only people
who have a chance to participate are those
who go to the location where the interviews
are being held and who go there during the
times they are conducted; this is not a truly
representative sample of the intended
audience. For theater tests, the only people
who have a chance to participate are those
who are recruited for the test, and
recruitment does not follow a truly
representative sampling design.
Quasi-quantitative methods are most often
used during Stage 2 to pretest messages
and materials. If your intended audience is
geographically dispersed or it is difficult for
them to get to a central facility, you can use
telephone interviews and send participants
any materials in advance. This type of
pretest typically resembles an in-depth
interviewing project in price and number of
interviews, although there may be more
closed-ended questions and the question
sequence may be adhered to more closely.
THE MODERATOR’S ROLE
The moderator does not need to be an
expert in the subject of your research
but must have experience facilitating
group discussions. A good moderator
builds rapport and trust and probes,
without reacting to or influencing,
participants’ opinions. The moderator
must be able to lead the discussion and
not be led by the group. He or she must
emphasize that there are no right or
wrong answers to the questions that are
posed. A good moderator understands
the process of eliciting comments, keeps
the discussion on track, and figures out
other ways of approaching a topic if the
first way is unproductive. Good
moderators understand what you are
looking for and what you need to do
with the information, and they are able
to probe and guide the discussion
accordingly. Go over the guide with the
moderator to point out any topics or
concerns you want emphasized or
discussed in depth. By the end of the
focus group or interview, the moderator
should ensure that all agreed-upon
topics are covered sufficiently.
If your organization plans to conduct
focus groups regularly, consider hiring
a skilled, experienced moderator to
train your internal staff to moderate
focus groups. Use local advertising
agencies, the American Marketing
Association’s Focus Group Directory,
or the Qualitative Research
Consultants Association to identify
a good moderator.
METHODS
Making Health Communication Programs Work
141

USING SOFTWARE TO ANALYZE QUALITATIVE DATA
If you have conducted a large number of focus groups or interviews with many intended
audience subsets—and are interested in analyzing results by different cultural groups, age
groups, or economic groups within the overall respondent population—you may want to
use computer software to do a comparative analysis of your results. If your results are from
only a few groups, however, computer analysis will be too time consuming to benefit your
program. Be sure to supplement computer analysis with “human” analysis, since the
strength of qualitative research is that it can uncover unexpected human reactions that
software cannot properly capture or weigh.
Before you decide to use computer software to analyze your qualitative data, assess the
following advantages and drawbacks of this type of analysis.
Advantages
• The ability to highlight sections of the transcript that are important to the project and
to eliminate “noise” or sections of the transcript that are not important to answering
your research questions (of course, a wordprocessor’s cut-and-paste functions can also
accomplish this).
• The ability to quickly access and compare information on one topic or questions
across several transcripts.
Disadvantages
• You must tape all interviews.
• It costs time and money to transcribe focus group sessions and in-depth interviews.
• Coding the transcripts is both time intensive and expensive. If more than one person
will be coding, you will need to train the coders, periodically assess intercoder reliability,
and retrain as necessary.
• While all comments on a particular topic can be gathered, they are taken out of
context in the process. Sarcasm and other tonal characterizations may be lost.
• Analysis by software will help you organize information, but will also produce
overwhelming amounts of paper.
Steps
If you decide to use software to analyze your qualitative data, follow these steps:
1. Transcribe the focus group discussions or interviews into an electronic format that can
be read by the analysis software. If you decide to use qualitative data analysis software,
check the requirements of the package you choose.
2. Develop and apply the codes you will use to organize the information in the
transcripts. A code is a word or number that represents a research objective, research
question, theory, or idea you are testing. The codes you develop will be unique to your
research. For example, if your first research question is to find out how many vaccine
Continued on next page...
142
Communication Research Methods

USING SOFTWARE TO ANALYZE QUALITATIVE DATA CONTINUED...
shots a parent is willing to give his or her infant, you might code all lines of your
transcript that include comments on that question as “A,” signifying that they
correspond to your first research question. Applying the code requires that you review
the transcripts and use a mouse to indicate on the computer screen all the lines of the
transcript that pertain to that code word.
3. Generate reports using the codes you developed. To do this, you instruct the program
to search for a particular code or a combination of codes. The program then presents a
single report showing all the lines of the transcript bearing the requested codes.
For a complete review of qualitative data analysis software, refer to Computer Programs for
Qualitative Data Analysis: A Software Sourcebook, by Eben A. Weitzman and Matthew B.
Miles, 1995, Thousand Oaks, CA: Sage. A new edition of this book is due out in 2002.
Central-Location Intercept Interviews
Central-location intercept interviews consist
of stationing interviewers at a point
frequented by individuals from your intended
audience and asking the individuals to
participate in a study. If they agree, they are
asked specific screening questions to see
whether they fit the study criteria. If so, the
interviewer takes them to the interviewing
station (a quiet spot at a shopping mall or
other site), shows the pretest materials, and
then administers the pretest questionnaire.
For intercept interviews to be effective, you
must obtain results from a minimum of 60 to
100 respondents from each intended
audience segment you want to test.
Pros
• You can connect with harder-to-reach
respondents in locations convenient and
comfortable for them.
• The interviews can be conducted quickly.
(The interview should be no longer than
15 to 20 minutes.)
• The interviews are a cost-effective means
of gathering data in a relatively short time.
• If you choose an appropriate location,
you will increase your chance to interview
respondents who are among your
intended audience.
Cons
• You must train interviewers.
• Your results are not representative
or generalizable.
• Intercept interviews are not appropriate
for sensitive issues or potentially
threatening questions.
• Intercept interviews do not allow you to
probe easily for additional information.
Central-location intercept interviews should
not be used if respondents must be
interviewed in depth or on emotional or
sensitive subjects. The intercept approach
also may not be suitable if respondents are
likely to be resistant to being interviewed on
the spot. In cases in which central-location
intercepts will not work well, schedule
interviews with respondents instead.
METHODS
Making Health Communication Programs Work
143

ESTIMATED COSTS OF FOCUS GROUPS AND IN-DEPTH INTERVIEWS, 2002
These estimated costs are included to suggest how you should budget for focus groups and
in-depth interviews if you are using commercial research firms. Your actual costs will vary
depending upon your geographic location, the intended audience to be recruited, and the
amount of time donated by staff, companies, and participants. Be sure you do not
jeopardize the quality of your results with a budget that is too small.
The focus group cost estimate in the table assumes that you conduct two groups, each
composed of 10 members of the general public. A group size of 6 to 8 is sometimes
preferred, because it is easier to engage all participants in the conversation. This estimate
is also based on the assumption that each group session is 2 hours long, is conducted in
English, and includes audiotapes. Staff travel, food for participants, and videotaping
are not included.
The in-depth interview estim
English and audiotaped.
Develop screener
Develop discussion guide
Recruit
Rent facility
Provide respondent
incentives
Compensate moderator or
interviewer to conduct
Analyze and report results
ate assumes a total of ten 30-minute interviews conducted in
2 Focus Groups
$ 920 – 1,380
$ 920 – 1,840
$1,725 – 2,875
$ 705 – 1,380
$ 690 – 1,380
$1,000 – 2,200
$1,840 – 2,760
10 In-Depth Interviews
$ 920 – 1,380
$ 920 – 1,840
$ 860 – 1,725
$ 0 – 1,150
$ 0 – 575
$ 500 – 1,000
$1,840 – 2,760
Total
$7,800 – 13,815* $5,040 – 10,430**
*Add an additional $400–600 for transcribing focus group audiotapes (optional).
**Add an additional $300–400 for transcribing in-depth interview audiotapes (optional).
144
Communication Research Methods

145

ESTIMATED COSTS OF CENTRAL-LOCATION INTERCEPT INTERVIEWS, 2002
The central-location intercept interview cost estimate below assumes that you question
100 respondents from the general population for 15 to 20 minutes each.
Develop questionnaire
Produce questionnaire, schedule facility,
phones, and mail
Screen/conduct interviews
Provide respondent incentives
Code/enter data/tabulate
Analyze and report results
Total
Questionnaire Contents
Unlike focus groups or in-depth interviews,
the questionnaire used in central-location
intercept pretesting is highly structured and
contains primarily multiple choice or closed-
ended questions to permit quick response.
Open-ended questions, which allow free-
flowing answers, should be kept to a
minimum because they take too much time
for the respondent to answer and for the
interviewer to record. Questions that assess
the intended audience’s comprehension and
perceptions of the pretest materials form the
core of the questionnaire. A few additional
questions, tailored to the specific item or
items being tested (“Do you prefer this
picture—or this one?”), may also be
included to meet your program planners’
particular needs. The questionnaire should
be pretested before it is used in the field.
See Appendix A for a sample questionnaire.
$ 460 – 4,025
$ 400 – 600
$1,955 – 4,025
$ 345 – 575
$ 805 – 1,495
$1,495 – 4,025
$5,460 – 14,745
Interview Setup
A number of market research companies
throughout the country conduct central-
location intercept interviews in shopping
malls.You can also conduct these interviews
in clinic waiting rooms, religious institutions,
Social Security offices, schools, work sites,
train stations, and other locations frequented
by members of your intended audience. Be
sure to obtain permission well in advance of
the time you want to set up interviewing
stations in these locations.
If you are using a market research company
to conduct the interviews, you will need to
provide screening criteria, test materials,
and the questionnaire. In some cases,
market research companies have offices in
shopping malls, and you can watch the
testing through a one-way mirror.
146
Communication Research Methods

Participant Recruitment
If you or someone in your organization is
recruiting the participants, you will need to
develop a script and provide training in
approaching members of the intended
audience. For example, if you are recruiting
participants in a clinic waiting room, the
interviewer should be familiar with the
screening criteria (e.g., women under 60
years of age) and approach only those
people who appear to fit the criteria. When,
after screening, individuals do not qualify to
participate, the interviewer should thank
them for their time and indicate that this
study is not the right fit for them but that
their willingness to participate is
appreciated. If they do qualify, the
interviewer can bring them to a designated
location (e.g., another room or corner of the
waiting room) and proceed with the study.
University and college departments of
marketing, communication, or health
education may be able to provide
interviewer training or trained student
interviewers. Pretesting is an excellent real-
world project for a faculty member to adopt
as a class project or for a master’s student
to adopt as a thesis project. However, this
approach may mean that it takes longer to
accomplish the research, and you could
compromise the quality of the results if the
individuals are not experienced in this type
of research.
Theater-Style Tests
Theater testing is often used in the
commercial arena to test advertisements for
products and services. Theater testing can
also be used to test the effectiveness of
PSAs. In this methodology, participants are
invited to a central location to respond to a
pilot for a new television show; in the midst
of viewing the TV pilot, they are shown your
PSA or advertisement along with other ads.
Participants complete a questionnaire
following the presentation, first answering
questions about the show and then
answering questions about how effectively
your message was communicated to them
and what their overall reactions were.
Common Uses
Theater-style tests are most commonly used
to test TV advertisements and PSAs. For
theater-style tests to be effective, you must
obtain results from 50 to 100 respondents
from each segment you want to test.
Pros
• You can obtain responses from a large
number of respondents at the same time.
• Theater-style tests more closely replicate
what goes on in someone’s home when
they are watching TV, so you can
accurately judge people’s reactions to
your message.
• Theater-style tests can be cost-effective if
you use donated facilities and equipment.
Cons
• It is expensive to rent a facility and
equipment (if necessary).
• Your results are not representative of the
general population.
General Format
Individuals typical of your intended audience
are invited to a conveniently located meeting
room. The room should be set up for
screening a television program. Participants
should not be told the real purpose of the
session, only that their reactions to a
television program are being sought.
METHODS
Making Health Communication Programs Work
147

At the session, participants watch a
television program. The program can be any
entertaining, nonhealth video approximately
15 to 30 minutes in length. The videotape is
interrupted about halfway through by a
sequence of four commercials.Your
message should be inserted between the
second and third commercials. See
Appendix A for a description of how to
create a roughcut video for theater-testing
your message.
At the end of the program, participants
receive a questionnaire and answer
questions designed to gauge their reactions,
first to the program and then to the
advertisements. Finally, your ad is played
again and participants complete several
questions about your ad. The majority of
these questions should be closed-ended to
enable an easy and accurate summary of
participant responses.
In more sophisticated theater testing,
participants use automated intended
audience response systems to answer
questions. Participants are provided with a
small device that has response keys. Once a
question is asked, they push a key to
respond and the data are automatically
tabulated.You have instant access to the
numbers using this system. In addition,
questions can be instantly added or deleted
from the questionnaire based on the
previous responses. Using an automated
system is much more costly than using a
standard paper-and-pencil questionnaire.
Other Media You Can Test
This methodology can also be used to test
videos by asking participants to view a
series of videos in which yours has been
included. Examples of videos that might be
tested include a 15- to 30-minute breast
cancer awareness video that will be played
in a clinic or a “how-to” video on
administering epinephrine. These testing
sessions will, of course, last longer than
those testing ads. Participants evaluate the
videos as described above.
Print advertisements can also be tested
using a variation of this methodology.
Several ads, including yours, are inserted
into a magazine. Participants are given an
adequate amount of time to read through
the article, which includes your ad and
others. After reading the article, participants
receive a questionnaire and answer
questions designed to gauge their reactions,
first to the article and then to the
advertisements. Finally, your ad is displayed
alone and participants complete several
additional questions.
Designing and Conducting a
Theater-Style Pretest
The process for conducting a theater-style
test includes the following steps:
1. Planning the pretest
2. Developing the questionnaire
3. Recruiting respondents
4. Preparing for the pretest
5. Conducting the pretest
6. Analyzing the pretest
You may find step 2 also useful for central-
location intercept interviews.
Plan the Pretest
Determine:
• The purpose of the study (e.g., what do
you want to learn?)
• When you need to produce results
• What your budget is
• The type and number of people who
should participate in the pretest
148
Communication Research Methods

• The locations where the pretest will
be conducted
To conduct theater testing, you must have a
large enough space to accommodate all of
your participants at the same time.You must
also ensure that you have several video
monitors so that all participants can
adequately view the program. Space
constraints may be overcome by seeking out
low-cost facilities such as a school
auditorium or church hall.You may be able
to borrow the audiovisual equipment from
these facilities as well.You can also rent
space, such as a hotel ballroom, if you want
to test a large number of people. Hotels
often rent audiovisual equipment as well.
Reserve facilities and equipment well in
advance of your pretest.
Develop the Questionnaire
To gather useful information from the
pretest, you must carefully construct the
questionnaire. See the sidebar Components
Used in Most Questionnaires on the next
page for general guidelines. Once you have
written your questionnaire, be sure to test
and revise it before you use it with a large
number of respondents.
Recruit Respondents
Participants may be recruited through a
market research facility or through local
community organizations. In either case,
you will need to provide an incentive for
participants. If using a market research
facility, you will also incur recruiting
expenses. If you are working with a
community organization, you may choose
to make a donation.
ESTIMATED COSTS OF THEATER TESTING, 2002*
Develop questionnaire
Produce questionnaire
Recruit
Rent audiovisual equipment
Conduct theater test
Provide respondent incentives
Code/enter data/tabulate
Analyze and report results
$ 460 – 2,760
$ 400 – 600
$ 0 – 5,750
$ 0 – 2,300
$ 0 – 920
$ 285 – 2,875
$ 920 – 3,680
$1,840 – 3,680
Total
$3,905 – $22,565+
METHODS
* Estimates assume 50 participants. They exclude facility rental costs. The costs of large facilities
(e.g., hotel ballrooms) vary widely by geographic location. Check with local facilities for
approximate costs.
Making Health Communication Programs Work
149

COMPONENTS USED IN MOST QUESTIONNAIRES
Although the following components should be used in most questionnaires, these
descriptions are specific to a theater-style pretest.
Program Questions
Program questions elicit general intended audience reactions to the program viewed.
Use the questions in Part I of the sample Theater-Style Pretest Questionnaire in Appendix
A as the first page of your questionnaire.
Recall, Main Idea, and General Reaction Questions
These three standard questions that assess your message’s ability to attract attention,
convey its main point, and create a positive response should appear on the second
page of your questionnaire. Use the questions in Part II of the sample questionnaire
in Appendix A.
These standard questions should be incorporated into the pretest for several reasons.
The questions address the most important indicators of a message’s potential effectiveness:
1) whether it attracts intended audience attention (recall), 2) whether it communicates
your main point (main idea), and 3) what respondents thought and felt when they
viewed the ad (reaction).
If you test many ads and always use the same questions, you can develop a database of
results to allow you to assess the relative strength of various ads.
Specific intended audience Reaction Questions
These provide answers to specific questions you have about your message.
Develop questions that address specific concerns you have about your message. For
example, suppose your message asks viewers to call a toll-free number for more
information. You may want to include a question that asks, “What action, if any, does
the message ask you to take?” A related question may be, “Did the telephone number
appear on the screen long enough for you to write it down (or remember it)?”
It is best to develop one or more questions addressing each characteristic of your message.
The list below includes various characteristics commonly found in messages. Note the
characteristics that apply to your test message and then develop questions that focus on
those characteristics.
• Use of music (with or without lyrics)
• Use of famous spokesperson
• Use of telephone number/Web site address
• Request for a particular action
• Instructions for adopting a specific health behavior
Continued on next page...
150
Communication Research Methods

COMPONENTS USED IN MOST QUESTIONNAIRES CONTINUED...
• Presentation of technical or medical information
• Presentation of new information
• Promotion of a sponsoring organization or event
• People intended to be typical of the intended audience
• Use of a voice-over announcer
• Presentation of controversial or unpleasant information
See Part III of the sample in Appendix A for examples of questions you can use for each
message characteristic listed above. These questions are just examples and should be
adapted to your needs. Remember that the objective of pretesting is to uncover any
problems with your ad before final production.
Demographic Questions
These questions help to record the characteristics of the participants (e.g., their sex, age,
level of education, health status).
Once you have written your questionnaire, be sure to test it before you use it with a large
number of respondents. After any necessary revisions, you are ready to make copies for
the pretest participants. You will need a cover page that instructs participants not to open
their questionnaires until they are asked to do so by the meeting host. Place a cover sheet
between each part of the questionnaire and instruct participants not to continue until
they are asked to do so by the meeting host.
Prepare for the Pretest
Rehearse the testing session at your own
office to anticipate and avoid any problems
before actual pretesting. Review the
following questions to be sure that your
session will go as smoothly as possible:
• Is the pretesting videotape ready for use?
Are the video and audio portions clear?
• Is the videotape equipment—recorder and
television monitors—functioning properly?
• Is the facility set up? Is the room
reserved? Are there enough chairs? Are
extra chairs available in case more people
show up than you expect? Do you need
another monitor so that everyone will be
able to see the program? Is the heat or air
conditioning working properly? Do you
know where the light switches are?
If a microphone is needed, is it set up and
functioning properly?
• Have you made all the necessary staffing
arrangements? Are your assistants
coming to the session? Do they have
transportation and directions for
getting there?
• Have you made enough copies of your
pretest questionnaire (including some
extras)? Is each questionnaire complete
(with no pages missing)? Do you have
pencils for participants? Will they need
clipboards or pads?
• Has participant recruitment taken place as
scheduled? Did you call and remind
participants to attend? Do they have
transportation and directions?
• Has the moderator rehearsed?
METHODS
Making Health Communication Programs Work
151

Conduct the Pretest
The procedures to follow during the pretest
session are relatively simple. The keys to a
successful testing session are to:
• Be friendly and courteous to participants
from the moment they arrive until they
leave (remember to say “thank you”).
• Keep calm and cool-headed throughout
the session.
• Anticipate problems in advance
(conducting a rehearsal to make sure
that both equipment and timing work is a
good idea).
The test session should take no more than
1 hour and 15 minutes if you are organized
and well prepared. Follow the steps below to
conduct your test:
1. Encourage participants to take a seat
as they arrive. Close the doors no later
than 10 minutes after the scheduled
starting time.
2. When everyone is seated, introduce
yourself by your name only (assuming
you are the host). Do not tell participants
the name of your organization during the
session because it might bias their
responses to your test ad.
3. Thank participants for coming and assure
them that the evening should be
enjoyable and that they will have a
chance to give their views to the
producers of “new” television program
material. Discourage participants from
talking to one another during the session.
Tell them you are interested in their own
individual views and that there are no
right or wrong answers. Also, encourage
them to write their answers clearly in the
space provided on the questionnaire.
4. After your introductory remarks, have
your assistants hand out the
questionnaires (see Appendix A for a
sample), pencils, and clipboards (if
needed). Instruct the participants not to
open the questionnaire until you ask them
to do so. Turn on the video recorder and
monitor to begin the test session.
5. Be attentive and watch for any problems
with the sound or picture on the monitor.
Be sure that the equipment is functioning
properly throughout the program.
6. Be prepared to stop the recorder when
the television program has ended.
Introduce the questions, and thank the
participants for their help so far. Ask them
to open their questionnaires and
complete the questions on the first page.
7. When the participants have finished Part I
of the questionnaire, tell them that you
would like to gather their reactions to the
messages/PSAs that were shown during
the program. Have them turn to Part II
and instruct them to fill out the questions
about the messages. When they have
completed these questions, tell them that
you want to obtain their reactions to one
particular message in the series of
messages they viewed.
8. Start the video. (Note: To avoid an
awkward pause in the session’s pace, be
sure there is not too much lead tape
before the message starts.) After your
PSA/ad has been replayed, ask
participants to turn to the next page of the
questionnaire and complete the
remaining questions. Encourage them to
answer every question and to avoid giving
more than one answer, except when this
option is indicated on the questionnaire.
9. Circulate through the room to monitor
progress and to be sure participants are
not discussing their responses. Collect
the questionnaires as participants finish.
152
Communication Research Methods

10. Thank participants for their cooperation.
If you have incentives or token gifts,
distribute them to participants as they
leave. If you have provided a donation to
a group in lieu of payment to
participants, mention that you hope the
group will find the donation helpful.
Analyze the Pretest
Analyze the questionnaires in two steps.
First, tabulate or count how many
participants gave each possible response
to each question. Next, look for patterns in
the responses to both closed- and open-
ended questions. The patterns will help you
draw conclusions about the effectiveness of
your message. See Appendix A for detailed
instructions on tabulating closed- and
open-ended questions and for a table of
average ratings to help interpret standard
question responses.
At this point, look at the overall results:
• What did you learn from the pretest?
• Did your message receive a favorable and
appropriate intended audience reaction?
• Did your message fulfill its
communication objectives?
• What are your message’s strengths?
Weaknesses?
• Did answers to any particular question
stand out?
Use your answers to these questions to
decide whether your message is both
effective and appropriate and whether you
need to revise your message prior to
program implementation.
Diaries and Activity Logs
Other tools you can use to evaluate your
program are diaries and activity logs. If you
plan to use these tools to gauge the quality
of program planning or execution, be sure to
start keeping the diaries and activity logs as
soon as you begin program planning. For
each activity, request information in a
specific format from program managers or
participants. This information may cover
issues such as the quality of program
components or track how your intended
audience uses the components.
Common Uses
• Track program implementation
• Assess effectiveness of
program implementation
• Monitor whether planned activities
are being conducted on schedule and
within budget
• Learn what questions program
participants had
• Learn what technical assistance was
needed by program staff
• Track intended audience exposure to
program components
Pros
• Allow respondents flexibility in
their responses
• Enable researchers to observe behavior
over time, rather than only once
Cons
• Require considerable effort on
respondents’ parts (for this reason,
consider offering incentives for completion
of the diaries/logs)
• Require staff able to code voluminous and
challenging incoming data
• Are not appropriate for respondents who
have low literacy skills or who have poor
writing skills or penmanship
METHODS
Making Health Communication Programs Work
153

Instituting Diary/Activity Log Use
Steps in instituting the keeping of diaries
and activity logs are:
1. Planning the study
2. Identifying who will participate
3. Developing and pretesting the form
you will use
4. Collecting data
5. Analyzing results
Follow the steps below to institute the
keeping of diaries and activity logs.
Plan the Study
Determine the following:
• What you want to learn
• How much information you need to collect
• How you will apply what you learn
• When you need the information
• What your budget is
• Your criteria for who should participate
Identify Who Will Participate
The sample you select depends on the
goals of your study. If you are focusing on
program implementation, you will want the
diaries/logs to be completed by program
staff (e.g., nurses in a clinic). In this case,
you may have some control over the quality
of responses you receive.
When planning the study, you must obtain
permission from a manager or supervisor on
site for staff to complete the diaries/logs
during the study.You should provide an
estimate of the amount of time and effort
participation will entail (e.g., 15 minutes per
154
Communication Research Methods

day, 1 hour per day). Share drafts of the
Examples of the types of information you
diaries/logs and get input from the
supervisor prior to the study. This will help
to ensure cooperation during the study.
Before the study begins, you should train
staff to complete the diaries/logs. Even if it
seems obvious to you, it is essential that
you explain exactly what you want recorded
in the diary/log. (See the sample log in
Appendix A.) In addition, you should provide
detailed, written instructions for future
reference. These instructions can be used in
lieu of training if you cannot physically get to
the study site.
If you are focusing on participant experience
with a program, you will want the
diaries/logs to be completed by people who
were exposed to program components. In
this case, you will have much less control
over the quality and quantity of responses.
Obtaining cooperation from participants may
also be more difficult in this situation. For
example, people attending an educational
program on nutrition might be recruited to
complete a diary of what they eat for a week
and send it back to the researchers.You will
likely need to provide an incentive (e.g., a
gift certificate upon receipt of the completed
diary), and you may also need to remind
participants to send back the diaries at the
end of the study period.
Develop and Pretest the Form You Will Use
Once you have identified what you want to
learn and who will complete the diaries/logs,
you must create a user-friendly document to
collect the necessary information.
Create questions. Write questions that are
specific to your study objectives.
might collect include:
• For a toll-free hotline activity log:
—Date?
—What is the gender of the caller?
—Where did the caller get the number?
—Did the caller request any
educational materials?
—What questions did the caller ask?
• For a health education program diary:
—Date?
—Which module was used?
—Which of the suggested activities
were completed?
—How long did it take to complete the
suggested activities?
—Would you use these activities again?
—Why or why not?
• For a clinic observation activity log:
—Date?
—How many people passed by the
display containing the new breast
cancer information?
—How many stopped to look at
the information?
—How many took a brochure?
Pretest the diary/log. Once you have
created the draft diary/log, you must pretest
it with individuals who represent your
intended audience. Describe the scenario
for them before the pretest. For example, in
the case of a hotline, you might say, “You
are an operator on a hotline. People will be
calling in, and you will need to fill out this
activity log as you complete each call.” Sit
together with them and ask them to read
each question aloud and tell you what they
think they are supposed to do. Do not
correct them if they do not say what you
intended. This probably means that your
diary/log is unclear. Continue through the
METHODS
Making Health Communication Programs Work
155

entire diary/log and then ask them if there
was anything that they found confusing or
unclear. Pretest the diary/log with everyone
as planned before you make any changes.
Revise the diary/log. Revise questions that
people found confusing during the pretest.
If a question was confusing only to one
person, use your judgment to decide
whether to change the question. Ask
yourself whether there is something you can
easily fix that would have helped that one
person understand the question (e.g.,
providing an example). If so, you may be
able to make a simple change or addition to
clarify the question. Also consider whether
this respondent found many of the questions
confusing while other respondents had no
problem with them. If this is the case, you
may not want to make changes.You will
have to decide on a case-by-case basis.
If you make substantial changes to the
diary/log, you should conduct another
pretest before finalizing the form.
Collect Data
Produce diaries/logs in sufficient quantities
so that respondents have several extra
forms in case they make errors or need
more space. Deliver the diaries/logs to
respondents, along with detailed written
instructions, prior to training (if applicable)
or at least 1 week before the study begins.
If you are asking program participants rather
than program staff to complete diaries/logs
for you, you will have to distribute the
materials on site. Give respondents a fixed
time frame to complete the diaries/logs and
provide them with a means (envelope/postage)
to return the data to you. If your study is
longer than a week or two, you may want to
ask respondents to ship the first week of
data to you so that you can review the logs
for accuracy and completeness and even
begin to tally some of the information.
Analyze Results
In the planning phase, you determined what
you wanted to learn from the study. Now you
will have the chance to look through the
diaries/logs to answer these questions.
Diaries generally contain qualitative
information (e.g., how food choices were
made that day, evaluation of programs
completed). Activity logs may contain
several types of information—quantitative
information you can tabulate easily (e.g.,
how many people called a hotline each day,
whether people picked up a brochure) as
well as qualitative information (e.g., reasons
that students liked or participated in
an activity).
Analyzing qualitative responses. The best
way to analyze qualitative information is to
read through the information, searching for
similarities and differences between diaries.
You will need to consider all of the questions
that you determined were important in the
planning phase. Once you have reviewed
several diaries, you should be able to pull
out general themes or patterns from the
information. The best way to analyze these
themes is to develop categories for the
responses. For example, if you want to know
why teachers thought their students liked or
disliked a certain educational module in your
program, you might group responses into
categories such as “challenging,” “fun,” “too
much work,” “boring.” Continue reading
through the remaining diaries and see how
many responses fall into these categories.
As you go along, you may come up with
additional categories or decide to collapse
several categories together.You can
certainly make inferences (e.g., “Teachers
liked the module because…”) about diary
information, but resist the temptation to
quantify this information.
156
Communication Research Methods

Analyzing quantitative responses. The Two different quantitative research
easiest way to analyze these types of
responses is to create a coding sheet for
each quantitative question. Use a separate
sheet for each question, writing the question
at the top and creating columns for each
possible response. For example, for a
question about how many people picked up
particular brochures, you could create
columns for the following categories: 0, 1–5,
6–10, 11–15, 16–20, >20.
Use the following procedure to record
the responses:
1. Take the first activity log and record the
response by making a check mark in the
appropriate column.
2. Repeat this procedure for
every questionnaire.
3. Tally the total number of check marks in
each column and then calculate the
percentage of participants who gave each
type of response.
Quantitative Research Methods
Use quantitative research methods during
the following parts of your program:
• Stage 1—to obtain information on
prevalence of relevant knowledge,
attitudes, behaviors, and
behavioral intentions
• Stage 3—to monitor usage of materials
and intended audience awareness of
the communication program and its
various tactics
• Stage 4—to measure progress
toward objectives
methods, surveying and readability testing,
can be used.
Surveys
Surveys are characterized by large numbers
of respondents (100 or more) and
questionnaires that contain predominantly
forced-choice (closed-ended) questions.
Common Uses
Used in planning and assessment to obtain
baseline and tracking information on
knowledge, attitudes, behaviors, and
behavioral intentions
Pros
• Provides generalizable results (to
generalize to a broader population,
you must have a statistically valid
random sample)
• Can be anonymous (useful for
sensitive topics)
• Can incorporate visual material (e.g., can
pretest prototype materials)
Cons
• Limited ability to probe answers
• Potential bias from possible respondent
self-selection
Most surveys are custom studies that are
designed to answer a specific set of
research questions. Some surveys, however,
are omnibus studies, in which you add
questions about your topic to an already
existing survey. A number of national and
local public opinion polls offer this option.
METHODS
Making Health Communication Programs Work
157

PROS AND CONS OF VARIOUS SURVEY FORMATS
Survey Formats
Mail
Telephone
With interviewer using
paper-and-pencil
questionnaires
Using computer-assisted
telephone interviewing
(CATI)
In Person
Interviewer-administered
Pros
Can be used to cost-
effectively access difficult-to-
reach populations (e.g., the
homebound, rural populations)
Respondents can answer
questions when most
convenient for them
Appropriate for those with
limited literacy skills
Results in more complete
responses because
interviewer fills out
questionnaires
Can control
question sequence
Useful for complex
questionnaires because
“skip patterns” can be
programmed in
Data entry is eliminated
Face-to-face persuasion
tactics can be used to
increase response rates
Can be used with those with
limited literacy skills
Useful with difficult-to-reach
populations (e.g., homeless,
rural) or when intended
Cons
Not appropriate for
respondents with limited
literacy skills
Low response rate diminishes
value of results
May require extensive/
expensive followup by mail or
telephone to increase
response rate
Respondents may return
incomplete questionnaires
Can be difficult to
read responses
May take long time to
receive sufficient numbers
of responses
Postage may be expensive if
sample is large, questionnaire
is long, or multiple reminder
cards are needed
Potential respondents without
phones cannot participate
Respondents may hang up
if they believe the survey is
part of a solicitation call or
they don’t want to take time
to participate
Requires CATI software
and computers
Requires extensive
interviewer training
Requires time to program
questionnaire into CATI
More expensive than self-
administered or telephone
data collection
Not appropriate for sensitive,
threatening, or controversial
questions (respondents may
not answer as truthfully
in person)
Continued on next page...
158
Communication Research Methods

P
ROS AND CONS OF VARIOUS SURVEY FORMATS CONTINUED...
Survey Formats
In Person/Interviewer-
administered continued...
Written, self-administered
Respondents are asked to
complete survey at a location
frequented by the target
population (e.g., during a
conference, in a classroom,
after viewing an exhibit at a
health fair)
Computerized, self-
administered
Questionnaire is displayed
on computer screen and
respondents key in
their answers
Internet
Computerized, self-
administered
Questionnaire is displayed on
respondent’s computer screen
via a Web site
Pros
audience cannot be sampled
using other data
collection methods
Interviewer can clarify
questions for respondents
Results in more complete
responses because
interviewer fills out
questionnaires
Can connect with harder-to-
reach respondents in locations
convenient and comfortable
for them
Can be conducted quickly
Cost-effective means of
gathering data in relatively
short time
Can result in increased
number of respondents within
intended audience if
appropriate location chosen
Useful for complex
questionnaires because
computerized “skip patterns”
can be used
Can control
question sequence
Eliminates data entry and
provides quick summary or
analysis of results
Useful for complex
questionnaires because
computerized “skip patterns”
can be used
Can control
question sequence
Eliminates data entry and
provides a quick summary or
analysis of results
Cons
Must be able to reach
respondents in person at a
central location or a gathering
Respondents must have
adequate literacy skills and be
self-motivated to respond
Not appropriate for intended
audiences with limited literacy
skills or those unfamiliar or
uncomfortable with computers
Requires expensive technical
equipment that may not be
readily available or may be
cumbersome in many settings
Not appropriate for audiences
with limited literacy skills or
those unfamiliar with or
uncomfortable with computers
Respondents must have
access to the Internet and
be somewhat familiar with
using computers
No way to confirm the validity
of information provided
by respondents
METHODS
Making Health Communication Programs Work
159

160

Follow these steps to conduct a survey: be completed before pretesting is
1. Plan the study
2. Determine how the sample will be
obtained and contacted
3. Develop and pretest the questionnaire
4. Collect the data
5. Analyze results
Sampling size and composition,
questionnaire design, and analysis of
quantitative data are complex topics beyond
the scope of this book. If you are planning
a quantitative study, see the reference list
at the end of this book for
additional information.
Additional Research Methods
Gatekeeper Reviews
Public and patient education materials are
often routed to their intended audiences
through health professionals or other
individuals or organizations that can
communicate with these audiences for you.
These intermediaries act as gatekeepers,
controlling the distribution channels that
reach your intended audiences. Their
approval or disapproval of materials can be
a critical factor in your program’s success. If
they do not like a poster or a booklet or do
not believe it to be credible or scientifically
accurate, it may never reach your
intended audience.
Common Uses
Gatekeeper review of rough materials is
important and should be considered part of
the pretesting process, although it is not a
substitute for pretesting materials with
intended audience members. Neither is it a
substitute for obtaining clearances or expert
review for technical accuracy; these should
undertaken. Sometimes, telling gatekeepers
that technical experts have reviewed the
material for accuracy will reassure them and
may speed their approval of your material.
Methodology
The methodology you should use for
gatekeeper review depends upon your
available resources, time, and budget.
Common methods include:
• Self-administered questionnaires—
Participants are sent the materials and the
questionnaire at the same time.
• Interviewer-administered questionnaires—
Typically, an appointment for the interview
is scheduled with the gatekeeper, and the
materials are sent for review prior to
the interview.
Develop questionnaires that ask about
overall reactions to the materials and for
assessment of the information’s
appropriateness and usefulness.
In some cases, you might not use a formal
questionnaire (especially if you don’t think
the reviewer will take the time to fill it out)
but will instead schedule a telephone
conversation or a meeting about the
materials. If you are not using a
questionnaire, consider in advance what
kind of questions you want to ask in the
meeting or interview and determine whether
you need formal approval of the materials.
A discussion with gatekeepers (e.g., a
television public service director, the
executive director of a medical society) at
this point can also be used to solicit their
involvement in a variety of ways that extend
beyond materials development.
METHODS
Making Health Communication Programs Work
161

Readability Testing*
Readability formulas often are used to
assess the reading level of materials. Fry,
Flesch, FOG, and SMOG are among the
most commonly used. Applying these
formulas is a simple process that can be
done manually or by using a computer
software program. Each method takes only
a few minutes.
Typically, readability formulas measure the
difficulty of the vocabulary used and the
average sentence length. In addition,
computer software programs analyze a
document’s grammar, style, word usage,
and punctuation, and assign a reading level.
These formulas, however, do not measure
the reader’s level of comprehension.
Readability software programs are available
at computer stores. Some software
programs, such as Microsoft Word, include
a readability-testing function. (Note: Mention
of software products does not constitute
an endorsement by the National
Cancer Institute.)
Researchers James Pichert and Peggy
Elam suggest three principles for using
readability formulas effectively:
1. Use readability formulas only in concert
with other means of assessing the
effectiveness of the material.
2. Use a formula only when the text’s
intended readers are similar to those on
whom the formula was validated.
3. Do not write a text with readability
formulas in mind.
* Adapted from Clear and Simple: Developing Effective
Print Materials for Low-Literate Readers (NIH Publication
No. 95-3594), by the National Cancer Institute, 1994.
Bethesda, MD. In the public domain.
Before you choose a readability testing
method, decide on an appropriate reading
level for the materials you’ve written. Then
use readability testing to determine whether
your text corresponds to the reading
level you want.
The term reading level refers to the number
of years of education required for
a reader to understand a written passage.
Some experts suggest aiming for a level
that is two to five grades lower than the
highest average grade level of your intended
audience to account for a probable decline
in reading skills over time. Others note that a
third- to fifth-grade level is frequently
appropriate for low-literacy readers. Keep
publications as simple as possible to
increase reader comprehension
of the material.
Readability Testing Methods
You can test readability easily using a
formula such as Fry, Flesch, FOG, or
SMOG. These tests can be done quickly to
indicate any problems with the drafted text.
They do not involve the intended audience.
SMOG
To calculate the SMOG reading grade level
of a written sample, begin with the entire
written work that is being assessed, and
follow these four steps:
1. Count off 10 consecutive sentences each
near the beginning, in the middle, and
near the end of the text.
2. From this sample of 30 sentences, circle
all of the words containing three or more
syllables (polysyllabic), including
repetitions of the same word, and total
the number of words circled.
3. Estimate the square root of the total
number of polysyllabic words counted.
162
Communication Research Methods
Do this by finding the nearest perfect
square and taking its square root.
4. Finally, add a constant of three to the
square root. The resulting number is the
SMOG grade or the reading grade level
that a person must have reached to fully
understand the text being assessed.
A few additional guidelines will help to clarify
these instructions:
• A sentence is defined as a string of words
punctuated with a period, an exclamation
point, or a question mark.
• Hyphenated words are considered
one word.
• Numbers that are written out should also
be considered, and if in numeric form in
the text, they should be pronounced to
determine whether they are polysyllabic.
• Proper nouns, if polysyllabic, should be
counted, too.
• Abbreviations should be read as
unabbreviated to determine whether they
are polysyllabic.
Not all pamphlets, fact sheets, or other
printed materials contain 30 sentences. To
test a text that has fewer than 30 sentences:
1. Count all of the polysyllabic words in
the text.
2. Count the number of sentences.
3. Find the average number of polysyllabic
words per sentence as follows:
Average = T
otal # of polysyllabic words
Total # of sentences
4. Subtract the total number of sentences
from 30.
5. Multiply that number by the average.
6. Add that figure to the total number of
polysyllabic words.
7. Find the square root and add a
constant of 3.
Perhaps the quickest way to administer
the SMOG test is by using the SMOG
conversion table. Simply count the number
of polysyllabic words in 30 sentences
(chains of 10 each from the beginning,
middle, and end of the text) and look up
the approximate grade level on the chart.
See the sidebar Example Using the SMOG
Readability Formula on the next page for
an example of how to use the SMOG
Readability Formula and the SMOG
conversion table. In the sidebar, each of
the 3 sets of 10 sentences is marked
with brackets.
Readability Testing With the
Intended Audience
*
Other methods of evaluating reading levels
and comprehension include having your
intended audience pretest your materials.
The WRAT or the Cloze technique can be
used to do this. These types of testing are
useful when you suspect that the intended
audience may encounter difficulties with the
material. Including pretest participants who
have the same characteristics as the low-
literacy intended audience you are trying to
reach is critical to the validity of your pretest
results. Recruiting participants through
groups or settings that include people with
limited literacy skills is a logical starting
point. But the only way to be sure your
pretest volunteers read at the same level
as your intended audience is to test their
reading skills.
The Wide Range Achievement Test (WRAT)
is used to measure reading levels, and the
Cloze technique is used to measure
comprehension. To avoid offending or
* Adapted from Clear and Simple: Developing Effective
Print Materials for Low-Literate Readers (NIH Publication
No. 95-3594), by the National Cancer Institute, 1994.
Bethesda, MD. In the public domain.
METHODS
Making Health Communication Programs Work
163
EXAMPLE USING THE SMOG READABILITY FORMULA
Benign Prostate Hyperplasia (BPH)
[Benign prostatic hyperplasia (BPH) is an enlarged prostate. Benign means noncancerous
and hyperplasia means excessive growth of tissue. BPH is the result of small, noncancerous
growths inside the prostate. It is not known what causes these growths, but they may be
related to hormone changes that occur with aging. By age 60, more than half of all
American men have microscopic signs of BPH, and by age 70, more than 40 percent will
have enlargement that can be felt on physical examination.
The prostate normally starts out about the size of a walnut. By the time a man is age 40,
the prostate may already have grown to the size of an apricot; by the age of 60, it may be
as big as a lemon.
BPH, which usually does not affect sexual function, is a troublemaker because the
prostate, as it enlarges, presses against the bladder and the urethra, blocking the
flow of urine.
A man with BPH may find it difficult to initiate a urine stream or to maintain more than a
dribble. He also may need to urinate frequently, or he may have a sudden, powerful urge
to urinate.] Many men are forced to get up several times a night; others have an annoying
feeling that the bladder is never completely empty.
Straining to empty the bladder can make matters worse; the bladder stretches, the bladder
wall thickens and loses its elasticity, and the bladder muscles become less efficient. The
pool of urine that collects in the bladder can foster urinary tract infections, and trying to
force a urine stream can produce back pressure that eventually damages the kidneys. The
kidneys are where urine is formed as waste products are filtered from the blood.
BPH sometimes leads to problems. [For instance, a completely blocked urethra is a medical
emergency requiring immediate catheterization, a procedure in which a tube called a
catheter is inserted through the penis into the bladder to allow urine to escape. Other
serious potential complications of BPH include bladder stones and bleeding.
Diagnosing BPH
A detailed medical history focusing on the urinary tract—kidneys, ureters (the pair of
tubes that carry urine from the kidneys to the bladder), the bladder, and the urethra—
allows the doctor to identify symptoms and to evaluate the possibility of infection or
other urinary problems.
The initial medical workup typically includes a physical exam called a digital rectal
examination (DRE), a urinalysis to check for infection or bleeding, and a blood test to
measure kidney function. Some physicians may also check the amount of prostate-specific
antigen (PSA) using a PSA test to help rule out the likelihood of cancer. PSA is a protein
that is produced by the cells of the prostate gland.
Continued on next page...
164
Communication Research Methods

EXAMPLE USING THE SMOG READABILITY FORMULA CONTINUED...
In addition, other tests may help a urologist—a doctor who specializes in disorders of the
urinary tract and the male reproductive tract—to determine if BPH has affected the
bladder or kidneys. These include tests that measure the speed of urine flow, pressure in
the bladder during urination, and how much urine is left in the bladder after urinating.
Some other tests that are widely used, according to an expert panel sponsored by the
United States Public Health Service (USPHS) practice guidelines, are expensive, sometimes
risky, and, for most men, unnecessary. These include cystoscopy, in which the doctor
inserts a viewing tube up the urethra to get a direct look at the bladder; an x-ray called a
urogram, in which urine is made visible on an x-ray after dye is injected into a vein; and
ultrasound, which obtains images of the kidneys and bladder after a probe is placed on
the abdomen.]
Treating BPH
About half of men with BPH develop symptoms serious enough to warrant treatment. BPH
cannot be cured, but its symptoms can be relieved by surgery or by drugs in many cases.
BPH does not necessarily grow worse. According to one review, mild to moderate
symptoms worsened in only about 20 percent of the cases. They improved (without any
specific treatment) in another 20 percent and stayed about the same in the rest.
[Men whose symptoms are mild enough often opt for an approach called watchful
waiting. This means that they report for regular checkups and have further treatment only
if and when their symptoms become too bothersome.
The USPHS Clinical Practice Guidelines call watchful waiting “an appropriate treatment
strategy for the majority of patients.” Men who choose watchful waiting should have
regular, perhaps annual, checkups, including DREs and laboratory tests.
For those who choose watchful waiting, a number of simple steps may help to reduce
bothersome symptoms. These include limiting fluid intake in the evening, especially
beverages containing alcohol or caffeine, which can trigger the urge to urinate and can
interfere with sleep; taking time to empty the bladder completely; and not allowing long
intervals to pass without urinating.
Men monitoring prostate conditions should also be aware that certain medications they
are taking for other ailments may make their symptoms worse. These include some over-
the-counter cough and cold remedies, prescribed tranquilizers, antidepressants, and drugs
to control high blood pressure. Switching to a different prescription may help.
Watchful waiting, of course, is not always enough for BPH, and surgery or drug therapy
may be required.]
Continued on next page...
METHODS
Making Health Communication Programs Work
165

EXAMPLE USING THE SMOG READABILITY FORMULA CONTINUED...
Readability Test Calculations
Total Number of Polysyllabic Words
Nearest Perfect Square
Square Root
Constant
SMOG Reading Grade Level
= 104
= 100
= 10
= 3
= 13
We have calculated the reading grade level for this example. Compare your results to ours,
and then check both with the SMOG conversion table:
SMOG CONVERSION TABLE*
Total Polysyllabic Word Counts
0 – 2
3 – 6
7 – 12
13 – 20
21 – 30
31 – 42
43 – 56
57 – 72
73 – 90
91 – 110
111 – 132
133 – 156
157 – 182
183 – 210
211 – 240
Approximate Grade Level
(± 1.5 Grades)
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
* Developed by Harold C. McGraw, Office of Educational Research, Baltimore County Schools,
Towson, Maryland.
166
Communication Research Methods

causing discomfort to those whose reading
ability you are testing, you can integrate a
WRAT or a Cloze test into the pretest
interview. For example, in a recent pretest
conducted by the National Cancer Institute,
the interviewers introduced the WRAT test
as the last part of the pretest. They stated,
“Thank you for helping with the questions
on the chemotherapy booklet. We need your
help with one last part—a word list. This will
take only a few minutes. The word list will
help us understand how difficult the words
are in the chemotherapy booklet.” This
integrated approach spared participants
the pressure or potential embarrassment
of “failing a reading test.”
The WRAT is based on word recognition
and does not measure comprehension or
vocabulary. The WRAT is an efficient way
to determine reading levels and takes only
a short time to administer.
The WRAT involves listening to the
participant read from a prepared list of
words, arranged in increasing order of
difficulty. Pronouncing the word correctly
shows that the reader recognizes the
word. The WRAT focuses on recognition
because, at the most basic level, if a
person does not recognize a word,
comprehension is impossible.
The test is over after the reader
mispronounces 10 words. The test
administrator notes the level at which the
last mispronunciation occurred. The “stop”
level equates to a grade level of reading
skills.You can compare this level with the
reading level of your intended audience to
see if your pretest readers are a
representative match for that audience.
The Cloze technique measures the reader’s
ability to comprehend a written passage.
Because it requires readers to process
information, it may take up to 30 minutes
to administer.
In a Cloze test, text appears with every fifth
word omitted. The reader tries to fill in the
blanks. This task demonstrates how well
he or she understands the text. The reader’s
ability to supply the correct word also reflects
his or her familiarity with sentence structure.
While packaged Cloze tests are available,
Leonard and Cecilia Doak’s Teaching
Patients with Low Literacy Skills explains
how to make up and score a Cloze test
yourself, based on the materials you are
pretesting. The book also discusses use of
the WRAT to assess reading levels.
Making Health Communication Programs Work
167
METHODS

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
APPENDIX A
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Communication Planning
Forms and Samples
The following is a listing of forms and samples that appear in this appendix.
Stage 1: Planning and Strategy Development
• Communication Program Plan
— Sample Promotion Plan
— Partnership Plan
— Evaluation Plan
• Strategy Statement/Creative Brief Template
Stage 2: Developing and Pretesting Concepts, Messages,
and Materials
• Sample Focus Group Screener Form
• Sample Focus Group Moderator’s Guide
• Sample Intercept Questionnaire
Stage 3: Implementing the Program
• Breast Cancer Materials User Survey
• Breast Cancer Risk Assessment Tool Evaluation: Summary
of Responses
Communication Research Methods
Please also see Stage 2 forms listed above.
• Producing Rough-Cut Video for Pretesting/Theater Testing
• Sample Theater-Style Pretest Questionnaire
• Sample Script for Hosting a Theater-Style Test
• Tabulating Responses to Closed- and Open-Ended Questions
• Average Ratings for Commercial Ads to Help Interpret Standard
Pretesting Questions
APPENDIX A
Stage 1: Planning and
Strategy Development
Forms and Samples

Communication Program Plan
Overview
Name of Program:
Sponsoring Agency:
Contact Person:
Issue or Problem to Be Addressed:
Evidence of Need (why the program is being developed):
Program Objective(s):
Communication Objective(s):
Primary intended audiences (in priority order; include pertinent characteristics and rationale):
Secondary intended audiences (in priority order with rationale):
Market Research
Market Research Plans (include pretesting):
APPENDIX A
Activities (list for each intended audience):
Continued on next page...
171

Messages (list for each defined market):
Materials to Be Developed/Adapted:
Materials Distribution and Program Promotion
Promotion/Materials Distribution Plan (see sample provided):
Key Tasks, Timeline, and Resources Needed (list person responsible; address fixed deadlines
and required approvals):
Partnerships
Potential Partner Organizations (describe their roles):
Partnership Plan (see separate form provided):
Evaluation Plan (see separate form provided):
172

Sample Promotion Plan
Promotion Plan for New Mammography Materials
National Cancer Institute
Office of Communications
Audiences: Primary Women in their 40s and older
Women at increased risk for breast cancer
Secondary Partners and advocates in the effort to reduce breast cancer
State and local health agency leaders
Health professionals and cancer research organizations
policymakers and interested public
Medical media
Products: The National Cancer Institute has developed the following new mammography
educational materials.
• Understanding Breast Changes: A Health Guide for All Women
This booklet includes information about many breast changes that are
not cancer and explains the procedures used to discover the presence
of breast cancer.
• Mammograms . . . Not Just Once, But for a Lifetime!
A 2-page, easy-to-read pamphlet that defines mammography, describes who
needs this important examination, and explains the procedure step-by-step.
• The Facts About Breast Cancer and Mammography
An 8-page booklet explaining the risk factors for breast cancer and the benefits
and limitations of mammography.
• Over Age 40? Consider Mammograms
A set of 5 posters, each featuring a woman from a special population.
For display in health care settings.
• Mammograms . . . Not Just Once, But for a Lifetime!
An attractive bookmark with facts on breast cancer and mammography
(25 to a pack).
• Why Get Mammograms?
A physician’s pad with tear-off fact sheets on mammograms for patients.
Includes NCI’s new recommendations, risk factors for breast cancer, and the
benefits and limitations of mammography.
• Breast Cancer Risk Assessment Package
A computer tool that helps physicians determine an individual woman’s 5-year
and lifetime risk of developing invasive breast cancer. (The materials review
form and the evaluation report NCI completed after this tool was released are
included later in this appendix.)
APPENDIX A
Continued on next page...
173

Promotion/Materials Distribution Plan:
NCI’s Office of Communications will promote the availability of these new materials to
organizations, health professionals, patients and the public, and the media in the
following ways:
Organizations
• Develop and distribute a breast cancer materials promotional brochure and copies of the
materials to the Cancer Information Service, and ask CIS to make the new materials
available to callers and their outreach partners.
• Distribute the promotional brochure and copies of the new materials to recipients on the
in-house mailing list. The in-house list includes breast cancer advocacy and voluntary
organizations, NCI-designated cancer centers’ public affairs and patient education networks,
nurses, physicians, occupational health care professionals, high school science teachers,
medical writers, dieticians, librarians, patient educators, genetic counselors, social workers,
health program planners, and community educators.
Health Professionals
• Distribute letters announcing the availability, including ordering information and copies of the
new materials, to the American College of Physicians, American College of Family Physicians,
Oncology Nursing Society (ONS), the Breast Cancer Progress Review Group, and attendees
of CDC’s meeting “Integrating Public Health Programs for Cancer Control” mailing lists.
• Develop a print public service announcement promoting the availability of the materials and
publish it in the Journal of the National Cancer Institute, CIS outreach and cancer center
newsletters, and other medical and association journals.
• Announce the availability of the materials in NCI’s column in the American College of
Obstetrics and Gynecology newsletter.
• Distribute the promotional brochure and materials at NCI’s fall exhibits, including CDC’s
“Integrating Public Health Programs for Cancer Control” meeting, American Public Health
Association, American Academy of Family Physicians, and ONS. Display a sign announcing
the availability of NCI’s new mammography materials.
Patients and the Public
• Consumer Information Center Spring Catalog will include the Facts About Breast Cancer
and Mammograms and CIC will send out a “New for Consumers” news release regarding
the booklet.
• Include mammography materials with ordering information on OC’s home page for patients,
the public, and the media.
Media
• Promote availability through the media, particularly women’s magazines, minority
publications, and medical journals.
174
Continued on next page...

Evaluation:
OC will evaluate its promotion efforts in the following ways:
• Track requests for the materials.
• Analyze feedback from readers who return bounceback evaluation cards from Understanding
Breast Changes: A Health Guide for All Women.
• Analyze feedback from recipients of the materials that included fax-back feedback form.
175
APPENDIX A

Partnership Plan
Program Title:
Communication Objective(s):
Intended audiences:
Potential Partner Organizations (in priority order):
Potential Partner Roles/Tasks:
Benefits to Partners of Participation in Program:
Other Considerations (such as your organization’s constraints or policies):
Steps Planned to Approach and Engage Potential Partners:
176
Continued on next page...

Negotiated Partners/Roles of Each:
Mechanisms for Communicating/Working Together:
Plans for Measuring Accomplishments:
Plans for Completing (Ending) Partnerships:
APPENDIX A
177

Evaluation Plan
Program name:
Communication objectives:
Intended audiences:
Identify each type of evaluation to be conducted (formative, process, and outcome):
For each type of evaluation, include:
Evaluation questions to be answered:
Data collection methods (e.g., telephone surveys, participant evaluation forms in
the classroom):
Analysis plan (what you are going to do with the data gathered to answer the
questions posed):
Evaluation products and use of evaluation data (e.g., final report to recommend program
revisions, conference presentation to share lessons learned with others):
Also include how you are going to get the evaluation done (tasks, time schedule, resource
requirements, persons responsible):
178

Strategy Statement/Creative Brief Template
1. Intended audiences
Whom do you want to reach with your communication? Be specific.
2. Objectives
What do you want your intended audiences to do after they hear, watch, or experience
this communication?
3. Obstacles
What beliefs, cultural practices, peer pressure, misinformation, etc. stand between your
audience and the desired objective?
4. Key Promise
Select one single promise/benefit that the audience will experience upon hearing, seeing, or
reading the objectives you’ve set?
5. Support Statements/Reasons Why
Include the reasons the key promise/benefit outweighs the obstacles and the reasons what
you’re promising or promoting is beneficial. These often become the messages.
6.Tone
What feeling or personality should your communication have? Should it be authoritative, light,
emotional…? Choose a tone.
7. Media
What channels will the communication use, or what form will the communication take?
Television? Radio? Newspaper? Internet? Poster? Point-of-purchase? Flyer? All of the above?
8. Openings
What opportunities (times and places) exist for reaching your audience?
9. Creative Considerations
Anything else the creative people should know? Will it be in more than one language?
Should they make sure that all nationalities are represented?
APPENDIX A
NOTE: All creative briefs must be accompanied by a page summarizing the background situation.
179
Stage 2: Developing and Pretesting
Concepts, Messages, and Materials
Forms and Samples
Sample Focus Group Screener Form
NCI/NIEHS Environmental Focus Group Project
Screening Questionnaire for North Carolina, Iowa, and California
Group 1: The Public “Touched by Cancer”
Group 2: The Public “NOT Touched by Cancer”
Summary of recruiting specifications for each group
Equal mix of men and women
Spread of ages 35–60
High school degree or some college
50% white; 50% mix of African American, Hispanic, and Asian
50% with children < age 10; 50% with children age 10+ or no children
Experience with cancer:
Group 1 – “Touched by cancer” only
Group 2 – “Not touched by cancer” only
Interested but not well informed about environmental/health issues
Not an opinion leader or activist
Never worked in the health/medical or environmental field
Not been in a focus group in the past year
(RECRUIT FOR 9–10 TO SHOW PER GROUP)
1. Good morning/evening. My name is_______, and I’m a researcher calling from (INSERT
NAME OF FACILITY) in (INSERT LOCATION). We are talking to people to learn their
opinions on some health-related issues that concern many Americans. Is there an adult in
the household between the ages of 35 and 60? ONCE SPEAKING TO ADULT, REPEAT
FIRST TWO SENTENCES IF NECESSARY. THEN ASK: Would you be willing to answer a
few questions?
a.Yes (CONTINUE)
b. No (THANK AND END)
Note whether respondent is male or female and recruit an equal mix for each group.
2. First, I need to ask you some basic information. Which category best describes your age?
a. Under 35 (THANK AND END)
b. 35–43 (CONTINUE)
c. 44–52 (CONTINUE)
d. 53–60 (CONTINUE)
e. 61 or older (THANK AND END)
Recruit 4 from each age category, with good age spread.
3. What is the highest grade you have completed in school? READ LIST IF NECESSARY.
a. 8th grade or less (THANK AND END)
b. Some high school (grades 9, 10, or 11) (THANK AND END)
c. High school graduate (CONTINUE)
d. GED (High school equivalency) (CONTINUE)
Continued on next page...
181
APPENDIX A

e. Some college/2-year college/technical school/
associate degree (CONTINUE)
f. College graduate (THANK AND END)
g. Some graduate school/post-graduate degree (THANK AND END)
For each group, recruit half with high school diploma or GED and half with some college.
4. We want to make sure we represent different ethnic and racial groups in our study. Would
you describe yourself as… ? (READ AND RECORD)
a. Hispanic or Latino/Latina (SKIP TO Q.6)
b. Not Hispanic or Latino/Latina (CONTINUE)
5. Next, would you describe yourself as…? (READ AND RECORD)
a. White (SKIP TO Q.7)
b. Black or African American (SKIP TO Q.7)
c. American Indian or Alaskan Native (THANK AND END)
d. Asian (CONTINUE)
e. Native Hawaiian or Other Pacific Islander (THANK AND END)
Recruit 4 from each age category, with good age spread.
6. (FOR HISPANICS AND ASIANS ONLY) What language do you usually speak at home?
a. English only (CONTINUE)
b. Another language only (THANK AND END)
c. English and another language equally (CONTINUE)
For each group, recruit 2 Hispanics and 2 Asians having English as their primary language.
Make sure ALL participants speak clearly and are easy to understand (no heavy accents).
7. Do you have any children under the age of 10, either by birth or adoption?
a.Yes (CONTINUE)
b. No (CONTINUE)
For each group, recruit half with children UNDER age 10, and half with children age 10 and
older or no children.
8. How would you describe your overall health? Would you say it was…?
(READ AND RECORD)
a. Excellent(CONTINUE)
b. Good (CONTINUE)
c. Fair (CONTINUE)
d. Poor (CONTINUE)
9. Now I’d like to ask you about several health conditions. Please tell me if either you, a
member of your immediate family, or a close friend has been diagnosed with any of these
conditions in the past 5 years? (READ LIST. IF ASKED, “IMMEDIATE FAMILY” INCLUDES
SPOUSE, GRANDPARENT, PARENT, SIBLING, OR CHILD.)
182
Continued on next page...

Ye s N o
a. Heart disease? (CONTINUE) (CONTINUE)
b. Diabetes? (CONTINUE) (CONTINUE)
c. Cancer? (RECRUIT FOR GRP 1) (RECRUIT FOR GRP 2)
Recruit participants who say “YES” to cancer for group 1 (“Touched by Cancer Group”).
Recruit those who say “NO” to cancer for group 2 (“NOT Touched by Cancer Group”).
10. There are a number of issues in the news, and it’s hard to keep up with every area. I’m
going to read you a brief list of issues. Please tell me if you are “very interested,”
“interested,” “somewhat interested,” or “not at all interested” in each issue. (READ LIST) Are
you very interested, interested, somewhat interested, or not at all interested in…? (INSERT
ISSUE; CIRCLE ONE RESPONSE FOR EACH ISSUE)
ISSUE:
Very
interested
Interested
Somewhat
interested
Not at all
interested
a. School issues
b. Economy and
business issues
c. Environment and
health issues
(GO TO B)
(GO TO C)
(CONTINUE)
(GO TO B)
(GO TO C)
(CONTINUE)
(GO TO B)
(GO TO C)
(THANK & END)
(GO TO B)
(GO TO C)
(THANK & END)
11. Now I’d like to go through the list again; for each issue, please tell me whether you consider
yourself “well informed,” “moderately informed,” or “poorly informed.” (READ LIST) Are you
well informed, moderately informed, or poorly informed about…? (INSERT ISSUE; CIRCLE
ONE RESPONSE FOR EACH ISSUE)
ISSUE Well informed Moderately informed Poorly informed
a. School issues
b. Economy and business issues
c. Environment and health issues
(GO TO B)
(GO TO C)
(THANK & END)
(GO TO B)
(GO TO C)
(CONTINUE)
(GO TO B)
(GO TO C)
(CONTINUE)
12. In the past 12 months, have you done any of the following? (READ LIST AND CIRCLE ALL
THAT APPLY. IF RESPONDENT HAS DONE 3 OR MORE, THANK AND END. IF
RESPONDENT HAS DONE 2 OR LESS, CONTINUE.)
a. Written a letter to the newspaper?
b. Written an article?
c. Written to your Congressman or Senator?
d. Made a speech?
e. Worked for a political party?
f. Served on a committee for some local organization?
g. Held or ran for political office?
h. Served as an officer of some club or organization?
i. Been a member of some group for better government?
APPENDIX A
Continued on next page...
183

13. Have you ever had a job in the following areas?
Ye s N o
a. In the health or medical field? (THANK AND END) (CONTINUE)
b. In the environmental area? (THANK AND END) (CONTINUE)
14. Have you ever participated in a focus group or been paid to be part of a discussion group?
a.Yes (CONTINUE)
b. No (SKIP TO 16)
15. How recently did you participate in the focus group?
a. Within the past year (THANK AND END)
b. More than a year ago (CONTINUE)
16. We are conducting an informal group discussion on health issues, and your views would be
valuable in helping us better understand this area. The discussion will take place in
(INSERT NAME OF TOWN/CITY) on (INSERT DATE) at 5:30 p.m. (Group 1) or 8:00 p.m.
(Group 2) at (INSERT FACILITY ADDRESS). The discussion will last two hours, and there
will be no attempt to sell you anything. We are simply interested in your opinions. We will
pay you $____________ as a way of thanking you for participating.You will also be given a
light meal or snack. Would you be interested in attending?
a. No (THANK AND END)
b. Yes (RECORD NAME, ADDRESS, PHONE NUMBER BELOW)
NAME:
ADDRESS:
PHONE NO:
Will attend: (CHECK ONE)
______ Group 1 (“Touched by cancer”)
______ Group 2 (“NOT touched by cancer”)
Let me mention two additional things:
1) If you wear reading glasses, please be sure to bring them to the discussion, as there may
be some reading involved; and
2) Please be aware that we have a no-smoking policy. If you have any questions or find that
you can’t attend, please call us right away at ______________________ so that we can find
a replacement.
Thank you for your time and for agreeing to participate in this discussion.
184

Sample Focus Group Moderator’s Guide
Cancer and the Environment
Moderator’s Guide for NCI/NIEHS Focus Groups
A. Introduction (3 minutes)
Good evening, my name is ____________, and I’ll be your moderator this evening. Welcome to
our focus group discussion tonight.
A focus group is a small group discussion that focuses on a particular topic in depth. Tonight
we will be talking about various health issues. I’m not an expert in the topics we’ll be discussing
tonight, and I’m not here to give you information. I’m here to listen to your ideas and thoughts
on these issues. It’s also important for you to know that I’m an independent consultant and do
not work for the sponsors of this discussion.
In a focus group, there are no right or wrong answers, only opinions, and I’d like to hear from all
of you about equally. It’s important that I hear what each of you thinks, because your thoughts
may be similar to those of many other people who aren’t here at this table tonight.Your ideas
are extremely important to us, and I’m interested in your comments and opinions. Please feel
free to speak up even if you disagree with someone else here. It’s OK to disagree, because it’s
helpful to hear different points of view. I’m also interested in any questions you may have as we
go along.
We have a lot of ground to cover in the next two hours, so, for the sake of time, I may jump
ahead to the next topic from time to time, but please stop me if you want to add anything.
We’re audiotaping and videotaping our discussion. Everything you say is important to us, and
we want to make sure we don’t miss any comments. Later, we’ll go through all of your
comments and use them to prepare a report on our discussion. I want to assure you, however,
that all of your comments are confidential and will be used only for research purposes. Nothing
you say will be connected with your name. Also, if there are any questions you would prefer not
to answer, please feel free not to respond to them.
There are also some colleagues of mine behind the one-way mirror who are interested in what
you have to say.
B. Warm Up (10 minutes)
[While participants are in the waiting room, they will be given magazines and asked to tear out
a picture by which to introduce themselves to the group.]
1. I’d like to begin by having each of you tell us your first name and a little about yourself—and
show us the picture you chose to introduce yourself to us.
2. What are some of the health problems that you personally worry about (not necessarily
health problems you have, but are concerned about getting)?
APPENDIX A
Continued on next page...
185
C. Perceptions and Beliefs About Cancer (25 minutes)
1. Now I’d like to talk specifically about cancer. If I had never heard of “cancer” before, how
would you describe it to me? What is it?
2. [Draw stick figure on easel] This is Pat, and all we know about her/him is that she/he has
cancer. I’d like to talk about how she/he came to have cancer. What do you think are some
of the reasons why she/he might have gotten cancer? [List on easel]
3. Now that you’ve told me some possible causes of cancer, how do you think cancer actually
develops in a person? How would you describe what happens inside the body? How do the
things on our list actually cause cancer? (Probe: gene mutation/gene malfunctioning)
4. Do you have any idea how scientists know what causes cancer and what doesn’t? How do
they go about finding out?
5. How concerned are you about cancer on a scale of 1–10, where “1” is “Not at all concerned”
and “10” is “Very concerned”? How much do you think about it? When do you think about it?
[For older groups] Did you feel differently about cancer when you were younger? [If yes]
How so? [For younger participants] Do you think you’ll feel the same way about cancer
when you’re 50? How do you think you’ll feel then?
6. Is there one particular type of cancer you are most concerned about? Why?
D. Cancer and the Environment (25 minutes)
1. [Drawing exercise] Now we’re going to be discussing cancer and the environment. On the
sheet of paper in front of you, I’d like you to take a couple of minutes and draw or write
something on the theme of “Cancer and the Environment.” You can draw or list anything that
fits with this theme; then we’ll talk about it in a couple of minutes. [After 2–3 minutes] Now
let’s talk about what you drew or wrote on this theme. Who would like to start?
2. Are you familiar with the word “carcinogen”? If I didn’t know what that meant, how would you
describe it to me? How many cancer-causing agents or carcinogens do you think there are?
(A few? Many?)
3. I’ve heard some people say, “Everything is a carcinogen.” What do you think of that
statement? Do you think that any substance/chemical can cause cancer if the dose is
high enough?
4. Which is of greatest concern to you—carcinogens out-of-doors, in the workplace, or
at home? (Probe: concern for selves versus concern for children) In general, are you
more concerned about carcinogens in the food you eat, the water you drink, or the air
you breathe?
5. What specific environmental agents/chemicals are you most concerned about? [List on
easel] (Probe: fluoride, gasoline, electrical power lines, food additives such as aspartame or
other sweeteners, dry cleaning solvents, fat in the diet, meat, air pollution, radiation, glass
wool insulation, talc, pesticides, prescription drugs)
6. Are any of the items we listed (above) of particular concern to you here in your local area?
Which ones? How concerned are you about them?
186
Continued on next page...

7. What are your thoughts about people having a genetic predisposition to cancer? Are some
groups of people more prone to cancer from the environment than others? Which
ones/why? (Probe: children, elderly, women, specific races, smokers) What have you heard
about childhood cancer and the environment?
8. Can people do anything to decrease their chance of getting cancer from the environment?
How well do you think these things work in preventing cancer? Do you personally do
anything now to decrease your chances of getting cancer? (Probe: cancer screening for
early detection, diet changes, dietary supplements, organic food, exercise, immunity
boosters like antioxidants or vitamins C & E)
E. Information Needs (10 minutes)
1. Has there been any environmental cancer concern in the past few years that you’ve tried to
find information about? How did you go about it? Where did you find the most valuable
information? Did you get enough information (or enough good information)? Were there any
questions you couldn’t find enough information about?
2. In general, do you have enough information to protect yourself and/or your children from
cancer-causing agents? If no, what kind of information do you need?
3. If you wanted to find out more about something that is suspected of causing cancer in your
local area, or at home, or at work, where would you look for information? (Probe:
newspapers, magazines, Internet, TV news, books that list carcinogens, etc.)
4. Do you know of any organizations or government agencies that try to protect the public from
things in the environment that might cause cancer? Which ones? How would you get in
touch with them if you had questions? Do you think you would get in touch with them?
F. Developing a Brochure (45 minutes)
1. The sponsors of this focus group want to develop a brochure about cancer and the
environment. We want your help in telling us what you, the public, want to know. Imagine
that we are the committee charged with the task of developing this brochure about cancer
and the environment, and we want to give people information they would be interested in
having about this topic. Let’s brainstorm for a few minutes about what type of information
should be included in this brochure. [List suggested information on easel] Is there anything
else that should be covered in our brochure?
2. Now, let’s go a step further. If you could have any questions answered about cancer and the
environment in this brochure, what questions would you want answered? [List questions]
3. Now I’d like to show you a draft outline for a new brochure and get your reactions. [Pass out
NCI/NIEHS outline with introductory paragraph]
a. What’s your general reaction to this draft outline?
b. Is there anything you especially like about it?
c. Is there anything you especially dislike?
d. Is anything confusing?
e. Which parts would be most useful to you?
f. What would you do with a brochure with this information?
APPENDIX A
Continued on next page...
187
4. In the time remaining, I’d like to show you a booklet about cancer and the environment that
was produced a while back. Please take about 5 minutes to examine the booklet as a whole,
and then pick one question/answer to read thoroughly. Once you’ve looked over the booklet,
I’d like to talk with you about your overall reactions. [Give participants 5 minutes to
review booklet]
a. What are your general reactions to this booklet?
b. Was there anything you especially liked?
c. Was there anything you especially disliked?
d. Was anything confusing?
e. Was anything missing that you would have liked to see included?
f. What did you think about the Q&A format?
g. What did you think about the tone? Level of detail? Amount of information?
h. How useful would a booklet like this be to you?
i. What question/answer section did you pick to read thoroughly? [Take tally]
j. Why did you pick that section? What did you get out of it? Did you want to
know more?
5. A number of you told me that you hear conflicting information about what does and doesn’t
cause cancer, and that this information changes from week to week. How do you think we
can make sense of this for the public in our brochure?
G. Close (2 minutes)
1. We’ve come to the end of our discussion. The sponsors of this focus group are the National
Cancer Institute (NCI) and the National Institute of Environmental Health Sciences (NIEHS).
Both these organizations are part of the National Institutes of Health (NIH), which is part of
the Federal Government. [If time permits] Are you familiar with either the National Cancer
Institute or the National Institute for Environmental Health Sciences?
2. Do you have any additional comments you would like to make on tonight’s topics?
3. On behalf of NCI and NIEHS, I want to thank you for your participation.Your opinions tonight
will be very valuable as they create and develop materials about cancer and the
environment for the public. Please stop at the front desk on your way out.
188

Sample Intercept Questionnaire
Central-Location Intercept Questionnaire
National Eye Institute, National Institutes of Health
Introduction
Good morning/afternoon/evening.
My name is _____________________, and I work for _______________, a marketing
research company located here in _________________ mall. We are conducting a study of
different ideas for television public service announcements. I would like to show you a couple
and get your reaction to them. The interview will take approximately 15 minutes, and you will
receive $5.00 for your time. Would you be willing to spend a few minutes answering
some questions?
1. To make sure we are representing different groups in our study, would you describe
yourself as:
White..............................
African American ...........
Hispanic .........................
Some other race ............
2. Are you 40 years old or older? (African American only)
Yes............
No ............. (Thank & End)
3. Are you 60 years old or older? (Anyone, including African American)
Yes............
No ............. (Thank & End)
4. Gender
Male ..........
Female ......
Note to interviewer: Repeat questions 5–10 for both storyboards. Ask questions 11–16 after
questions have been answered for the last storyboard.
Now I am going to show you ideas for two advertisements and ask you a few questions about
each. I am going to show you storyboards that represent what the advertisement will be like.
I will read the information that goes with each storyboard aloud as you see it.
Continued on next page...
189
APPENDIX A

Storyboard Sequence: Black Out, POV
5. Which of the following would describe your general reaction to this ad?
a. Do you really like it?..............................................................................
b. Do you think it is just ok? ......................................................................
c. Do you not like it very much?................................................................
d. Do you not like it at all?.........................................................................
e. Don’t know/refused ...............................................................................
6. What is the main message of this ad? (Do not prompt—check all that apply)
a. Everyone should have an eye exam . . . . . . . . . . . . . . . . . . . . . . . . . .
b. Everyone should have a dilated eye exam . . . . . . . . . . . . . . . . . . . . .
c. People at risk for glaucoma should have a dilated eye exam . . . . . . .
d. Eye disease is treatable if diagnosed in time . . . . . . . . . . . . . . . . . . . .
e. Other ___________________________________________________
7. Does this advertisement motivate you to do anything? If so, what does it motivate
you to do? (Do not prompt—check all that apply)
a. Get an eye exam . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
b. Get a dilated eye exam . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
c. Tell someone else to get an eye exam . . . . . . . . . . . . . . . . . . . . . . . . .
d. Tell someone else to get a dilated eye exam . . . . . . . . . . . . . . . . . . . .
e. Ask a health professional about eye disease/glaucoma . . . . . . . . . . .
f. Tell someone else to ask a health professional about eye
disease/glaucoma . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
g. Other ___________________________________________________
If not, why not? (Do not prompt—check all that apply)
a. S/he does not presently have glaucoma . . . . . . . . . . . . . . . . . . . . . . .
b. S/he does not presently know someone who has glaucoma . . . . . . . .
c. Message has good information, but respondent doesn’t feel
the need to act . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
d. Message is boring . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
e. Message is unclear . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
f. Other ___________________________________________________
8. If you saw this advertisement on television, how likely do you think you would be to get a
dilated eye exam at least every 2 years or to tell someone else to get a dilated eye exam at
least every 2 years?
a. Very likely . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
b. Somewhat likely . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
c. Not too likely . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
d. Don’t know/refused . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
190
Continued on next page...

___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
___________________________________________________________
9. How well does each of the following words/attributes describe what you just saw?
a. Is it attention-getting? very much a little not at all
b. Is it interesting? very much a little not at all
c. Is it direct/to the point? very much a little not at all
d. Is it useful information? very much a little not at all
10. Was there anything in the advertisement that you found confusing or hard to understand?
(Do not prompt—check all that apply)
a. Nothing . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
b. Confused in general . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
c. Message not clear . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
d. Words were hard to understand . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
e. Too much information presented . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
f. Message didn’t relate to me . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
g. Other ___________________________________________________
Note to interviewer: Ask the following questions after showing both advertisements.
11a. Which advertisement do you like the best?
POV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Black Out . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Why? ______________________________________________________
11b. Which advertisement do you like the least?
POV . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Black Out . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
Why? ______________________________________________________
The following questions are optional, but will help to provide background for this study.
12. Which of the following categories includes your age?
40 through 49..............................................................................................
50 through 59..............................................................................................
60 through 69..............................................................................................
70 through 79..............................................................................................
80 and older................................................................................................
APPENDIX A
Continued on next page...
191

13. Have you ever been diagnosed with glaucoma?
Yes ..............................................................................................................
No ...............................................................................................................
14. Do any of your friends or family members have glaucoma?
Yes ..............................................................................................................
No ...............................................................................................................
15. What was the last grade you completed in school? Stop me when I get to the right
category. (Interviewer read choices.)
Less than high school .................................................................................
High school diploma, GED, or technical school ..........................................
Any college or beyond.................................................................................
16. Which of the following categories contains your household’s annual income? Stop me
when I get to the right category. (Interviewer read choices.)
<20,000.......................................................................................................
20K – <35K .................................................................................................
35K – <60K .................................................................................................
60K – 75K ...................................................................................................
>75K ...........................................................................................................
Declined to answer .....................................................................................
Thank you very much for giving us your time.Your feedback has been most helpful.
192

APPENDIX A
193

Stage 3: Implementing the Program
Forms and Samples

Breast Cancer Materials User Survey
Please help us make this tool more effective by answering the following questions:
1. Did you use the assessment tool in your practice? ___YES ___NO
IF NO, please explain:
2. Who was the primary user? ___Doctor ___Nursing staff ___Office staff ___Other
IF OTHER, please specify:
3. In what setting did you use the tool? (Check all that apply)
___Office/consult room ___Reception/waiting room
___Exam room ___Resource room
___Nurse’s station/area ___Other (specify:_____________________________)
4. Was the assessment tool…
a. Easy to use? ___YES ___NO
b. Appropriate in length? ___YES ___NO
c. Useful in discussing breast cancer risk with your patients? ___YES ___NO
d. Complete? (I.e., no additional information needed?) ___YES ___NO
e. Understandable? (I.e., were patients able to understand
the assessment outcome sheet?) ___YES ___NO
5. If you responded “NO” to any part of question 4, please explain here:
APPENDIX A
6. Would you recommend this disk to others? ___YES ___NO
Continued on next page...
195

7. Other comments or suggestions:
8. Are you: ___a doctor? ___other health professional? ___office staff? ___other?
IF OTHER, please specify:
THANK YOU. PLEASE FAX THIS FORM TO (XXX) XXX-XXXX.
196

Breast Cancer Risk Assessment Tool Evaluation
Summary of Responses
Background
The Breast Cancer Risk Assessment tool is a computer program that allows physicians and
others to estimate a woman’s lifetime risk of developing invasive breast cancer. The Breast
Cancer Risk Assessment Tool was promoted and distributed via NCI’s cancerTrials Web site;
trade, consumer, and health professional media; and voluntary and advocacy organizations.
The approximately 18,000 copies of the tool (each included the survey from the previous
pages) were sent to:
Cancer patients (46 percent)
Clinicians (40 percent)
Scientists (4 percent)
Media (1 percent)
Other (9 percent)
Because the majority of the survey’s respondents were doctors and other clinicians, the
findings do not reflect the above distribution.
Findings
These findings are based upon a sample of 125 surveys returned:
• Almost all respondents (97 percent) said they would recommend the tool to others.
• Most respondents (84 percent) had used the tool in their practice. For those who had not,
it was usually because the person was not a physician or was retaining it for personal use.
• An overwhelming majority found the assessment tool easy to use (99 percent), appropriate
in length (97 percent), and understandable (99 percent). A strong majority found the tool
useful in discussing breast cancer risk with patients (94 percent).
• Almost three-quarters of respondents found the tool to be complete (68 percent).
A substantial number of respondents who did not find the tool to be complete (32 percent)
provided comments and suggestions to support their opinions. In general, respondents
suggested that the tool:
— Determine whether treatment with tamoxifen was indicated or not
—
Include risk information relative to a woman’s menopausal status
— Include risk information for patients previously diagnosed with breast cancer
Conclusions
Based upon the feedback, it appears that health care providers are using the tool and generally
find it easy to use, appropriate in length, understandable, and helpful in discussing breast
cancer risk with their patients. A substantial number of respondents (32 percent) did not find
the tool to be complete, mainly because they felt it did not provide enough information about
other risk factors that may play a role in calculating a patient’s individualized risk estimate of
invasive breast cancer.
APPENDIX A
197

Communication Research Methods
Forms and Samples

Producing Rough-Cut Video for Pretesting/Theater Testing
The three most commonly produced forms of rough messages for pretesting are:
1. Animatics—Simple line drawings are videotaped in sequence to depict your message
2. Photomatics—Photographs are videotaped in sequence to depict your message
3. Rough live action—An actual run-through of the script is videotaped using simplified
sets, live actors, easily accessible locations, or simulated backgrounds (e.g., rear
screen projection of the set)
All three of the above types of messages include an audiotaped delivery of the script.
The following table lists some advantages and disadvantages of each type of rough message.
Type of Rough Message Advantages
Disadvantages
Animatic Less expensive than others
May not approximate script
Fewer logistical arrangements
No props required
Needs artist who can render
clear line drawings
No location settings
Easiest to produce
Photomatic
More realistic than animatic
More costly than animatic
Can be inexpensive and easy
to produce if location, props,
and actors are available
More logistical arrangements
than animatic
Rough live action
More realistic than animatic
or photomatic
Can be inexpensive if
location, props, and actors
are readily available
Many logistical
arrangements and
rehearsals required
May be more difficult to
make changes
APPENDIX A
Continued on next page...
199

The closer the rough message approximates final production quality, the more likely the pretest
results will predict audience response accurately. The illustrations should be realistic, the
characters should look like those you plan to use in the final spot, facial expressions should
reflect the mood and tone of the script, and the settings should be sketched in detail. If
photographs are used, the pictures of people and places should be clear and should resemble
those to be used in the final message. Pay attention to the setting, wardrobe, props, camera
angle, and perspective. Review the processed photographs and select the clearest ones for
producing the rough message.
When producing animatics or photomatics, the illustrations or photographs must be large
enough and clear enough for videotaping. Each illustration or photograph should be at least
9
" x 12" so that the camera can capture sufficient detail. Larger sizes also permit camera
movement (e.g., moving from left to right) within the frame to create a sense of motion or
action. If you produce a photomatic, using slides projected on a screen allows you to create
whatever size scene you want.
The video portion of an animatic or a photomatic is produced by videotaping each scene,
frame by frame. Simulate motion by moving the camera in or out (zooming), left to right
(panning), or up and down. Record the audio portion of the rough message and then edit to
exactly the right length.
Finally, edit the videotape “to time” (30 or 60 seconds), using the soundtrack as a guide. The
video and audio tracks are then mixed together to produce the rough message.
If you decide to use live action instead of pictures, use nonprofessional actors (e.g., friends or
coworkers) to enact the script in a setting that closely approximates that to be used in final
production. The visuals and the sound should be recorded at the same time. To minimize the
number of times the live action must be taped, the actors should rehearse and the production
crew should be briefed ahead of time.
Minimizing Production Costs
Animatics, photomatics, and rough live action PSAs can be produced with the help of a
professional production company, your agency’s audiovisual staff, a local television station, or a
local college or university. A professional production company will be the most expensive
option; the latter three options will be less expensive. For example, a local television station
may donate its services for producing your spot, or a television production instructor may assist
you at no charge (except for the cost of the videotape) by making the production of your rough
message a student assignment.
There are several ways to help control the costs and the production quality of your rough ad:
1. Create a detailed production plan that addresses the following questions:
• What scenes will appear on the screen and in what order?
• How long will each scene be on the screen?
• What camera movements will be needed in each scene?
• How will scenes be edited together (e.g., fades, dissolves, or direct cuts)?
• What portions of the soundtrack go with each scene?
2. Send your production plan in advance to the person who will be helping you, and have extra
copies on hand at the production session.
200
Continued on next page...

3. Make sure your script and production plan for the rough message are complete and timed
in advance.
4. Prerecord the audio track before the visuals are shot.
5. Make sure your illustrations, photographs, and/or slides are in the right order when you
arrive for the production session.
6. Finally, remember that you are producing a rough message. Save perfection for
final production!
Rough message production costs may be further reduced by using amateur talent (e.g., friends
or coworkers) who can do a respectable job recording the script. These same people may be
used for photographs or in a rough live action spot. Shooting the visuals and recording the
soundtrack on the same day may also save time and money. Finally, consider contacting a local
radio station for recording the soundtrack. The station may provide its facilities free of charge or
at a lower rate than a recording studio.
Animatics may be less expensive and faster to produce than photomatics because they are
composed of artists’ renditions. While you may have to buy the artwork, you eliminate costs for
talent (actors), location setting (i.e., obtaining clearance to rent or use property), props, and
travel. However, drawings may not communicate the realities or subtleties of the visual portion
of the message as well as photographs or rough live action. These drawbacks can be
minimized by using a good illustrator and a good, clear soundtrack.
Photomatics may be more expensive than animatics, depending upon the cost of the
photography. The availability of people who can represent the characters, the accessibility of an
appropriate location, and the rate your photographer charges are the major factors that affect
costs. These costs can be kept down by working with people who are readily available and by
arranging all the details in advance. The major advantage of producing a photomatic over an
animatic is that you can produce a more realistic and believable rendition of the final message.
Compare the costs of an illustrator versus those of a photographer and factor in the logistics
involved when deciding whether you should produce an animatic or a photomatic.
A rough live action message can be the least expensive way to produce your message in
rough form if:
• You are using amateur talent who can do a respectable run-through of the script
• Your script can be produced in a readily accessible location that does not require a lot of
set-up time
• Your production crew can videotape the run-through with a minimum number of takes
We recommend that you videotape rather than film the rough message for pretesting because
editing and processing are usually less expensive. Home or studio video equipment can be
used to produce any of the three rough message forms.
201
APPENDIX A

Sample Theater-Style Pretest Questionnaire
Part I
Thank you for watching this program. One of the reasons it was shown tonight was to get your
reaction to it—to see what parts you liked and what parts you didn’t like.
1. Was there any part of the program that you especially liked?
2. Was there anything about the program that you disliked?
3. Please indicate your overall reaction to the program by circling one of the phrases below:
a. A great program, would like to see it again
b. A pretty good program
c. Just so-so, like a million others
d. Another bad program
4. Would you recommend the program to your friends? Why or why not?
Part II
For each commercial that you remember seeing, please write down what the message said
and what the message showed on the dotted lines. Write down the main idea each message
was trying to get across on the solid lines.
a. What did the message say?
b. What did the message show?
c. What was the main idea each message was trying to get across?
202
Continued on next page...

1. a.
b.
c.
2. a.
b.
c.
3. a.
b.
c.
4. a.
b.
c.
5. a.
b.
c.
Part III
1. This evening you saw an ad. Now that you have seen the ad twice, please tell us what you
think was the main message of the ad?
2. In your opinion, was there anything in particular that was worth remembering about the ad?
a.Yes
b. No
2a. If yes, what was worth remembering?
Continued on next page...
203
APPENDIX A

3. In your opinion, what type of person was this ad talking to?
a. Someone like me
b. Someone else, not me
3a. If someone else, why?
4. In your opinion, was there anything in the ad that was confusing or hard to understand?
a.Yes
b. No
4a. If yes, what was confusing?
5. We would now like you to describe the ad. From each pair of words or phrases, please circle
the one that you feel best describes the message.
a. Believable
b. Not believable
a. Well done
b. Not well done
a. Convincing
b. Not convincing
a. Made its point
b. Didn’t make its point
a. Interesting
b. Not interesting
a. Pleasant
b. Not pleasant
a. Informative
b. Not informative
204
Continued on next page...

Part IV
[Following are sample questions for each message characteristic. Feel free to adapt these
questions to your needs, or develop your own questions. Make sure your pretest questionnaire
covers all aspects of your ad.]
Use of Music
1. Please circle the one answer from each pair that best describes your feelings about the
music in the ad.
a. Appropriate to the message
b. Not appropriate to the message
a. Effective in getting the message across
b. Not effective in getting the message across
a. Could understand the words to the music
b. Could not understand the words to the music
2. Overall, how would you describe the music in the ad?
a. The music fit the message
b. The music did not fit the message
c. I don’t remember the music
Use of Famous Spokesperson
1. Which of the following best describes________________ [name of spokesperson], the
announcer in the ad?
a. Singer
b. Actor
c. Comedian
d. Athlete
e. Don’t know
2. Please circle the one answer from each pair of phrases that best describes your feelings
about the announcer, ___________________ [name of spokesperson].
a. Believable
b. Not believable
a. Appropriate to the message
b. Not appropriate to the message
a. Gets the message across
b. Does not get the message across
APPENDIX A
Continued on next page...
205

Use of Telephone Number or Address
1. The phone number (or address) was on the screen long enough for me to remember it or
write it down.
a. Agree
b. Disagree
c. Neither agree nor disagree
Request for a Particular Action
1. What did the ad ask you to do?
Instructions for Performing a Specific Health Behavior
1. Please circle one answer from each pair of phrases that best describes your feelings about
the instructions regarding________________[fill in behavior] in the ad.
a. Clear and easy to understand
b. Confusing, hard to understand
a. I would be able to perform_____________________________ [fill in behavior] after
seeing this ad.
b. I would not be able to perform_________________________ [fill in behavior] after
seeing this ad.
Presentation of Technical or Medical Information
1. The ad presented technical (or medical) information. Please select one answer from each
pair of phrases that best describes your feelings about the information.
a. The ad did a good job of presenting technical information.
b. The ad did a poor job of presenting technical information.
a. I understood all the terms in the ad.
b. I had difficulty understanding the terms in the ad.
206
Continued on next page...

Presentation of New Information
1. How much, if any, of the information in the ad was new to you?
a. All of it
b. Most of it
c. Some of it
d. None of it
2. Overall, how useful was the information in the ad to you?
a. Very useful
b. Somewhat useful
c. Not very useful
d. Not useful at all
e. Don’t know/not sure
Promotion of a Sponsoring Organization
1. From among the following choices, please indicate the organization that sponsored this ad.
[Include your organization and fill in appropriate alternatives.]
a. CARE
b. Baylor College of Medicine
c. Save the Children Foundation
d. Don’t know/Not sure
Characters Who Are Supposed to Be Typical of the Intended Audience
[The word “characters” in these questions could be substituted with “man,” “woman,”
“family,” “children,” etc.]
1. Which of the following statements best describes the characters in the ad?
a. The characters in the ad reminded me of people I know.
b. The characters in the ad did not remind me of people I know.
2. Overall, how would you describe the characters in the ad? Please select one response from
each group.
a. Realistic
b. Not realistic
a. Helped me to understand the message
b. Did not help me to understand the message
APPENDIX A
Continued on next page...
207

3. Overall, how would you describe the characters in the ad? Please select one answer from
each group.
a. Appealing
b. Not appealing
a. Get the message across
b. Do not get the message across
a. Believable
b. Not believable
a. Easy to understand
b. Not easy to understand
Use of a Voice-Over Announcer
1. Please circle the one answer from each pair of phrases that best describes your feelings
about the announcer.
a. Believable
b. Not believable
a. Appropriate to the message
b. Not appropriate to the message
a. Gets the message across
b. Does not get the message across
a. Easy to understand
b. Hard to understand
Presentation of Controversial or Unpleasant Information
1. Some people have mentioned different feelings they had during or after watching the ad.
Please circle the opinion that comes closest to yours.
a. The ad made me uncomfortable, and I had difficulty paying attention to it.
b. The ad interested me, so I paid attention to it.
c. I had no particular feeling about the ad.
2. Overall, how do you think most people would feel about this ad if they saw it on television
at home?
a. Suitable to show on television at any time
b. Suitable to show, but only at certain times
c. Not suitable to show at any time
208
Continued on next page...

Part V
[Listed below are sample questions to be used for identifying the characteristics of your
pretest participants. Some of these questions also may be used as screening questions to
recruit participants from a specific group.]
Demographic Information
1. What is your sex?
a. Male
b. Female
2. What is your age?
a. Under 18
b. 18–24
c. 25–34
d. 35–44
e. 45–49
f. 50–54
g. 55–60
h. Over 60
3. How far did you go in school?
a. Eighth grade or less
b. Some high school
c. High school graduate
d. Some college
e. College graduate
4. Do you have children?
a.Yes (go to question 4a)
b. No (go to question 5)
4a. Please circle the age categories in which your children belong. Circle as many as apply.
a. 1–5 years old
b. 6–10 years old
c. 11–15 years old
d. 16–20 years old
e. 21 or over
5. Which of the following statements best describes you?
a. I currently smoke.
b. I used to smoke, but have now stopped.
c. I have never smoked.
APPENDIX A
Continued on next page...
209

6. Have you ever been told by a doctor or a nurse that you have . . .
a. Heart disease
b. High blood pressure
c. Cancer
d. Emphysema
e. Other
7. To the best of your knowledge, have you ever been exposed to . . .
a. Asbestos
b. Other toxic chemicals
c. Etc.
8. Which of the following best describes your race or ethnic background?
a. American Indian or Alaskan native
b. Asian
c. Black or African American
d. Hispanic or Latino
e. Native Hawaiian or Other Pacific Islander
f. White
210

Sample Script for Hosting a Theater-Style Test
Introduction
Good evening. I’m ____________________________________, and I’d like to thank you all for
coming today (tonight). I think we’re all going to have a good time. Just a few more words of
introduction and we’ll get started. We’ve asked you here because we feel that it’s very
important to get your ideas about new television program material. So consider this your
chance to give the TV program producers your opinions . . .
Keep in mind that what we’re interested in is your own personal views. We don’t want you to tell
us what you think we want to hear or what your spouse thinks or anyone else—we need your
own opinions.
There are no right answers and no wrong answers. So, please don’t discuss the program or
your answers with the people around you.
Also, please make sure that you write your answers clearly in the space provided on the
questionnaire we’ve given you, and be sure that you don’t move to a new section of the
questionnaire until I ask you to.
Do you have any questions about this procedure? I’ll answer any other questions you have at
the end of the test session. Okay? Now enjoy the show.
[Play the pretesting program videotape]
Reactions to the Program
All right. Now we’d like to find out about your reactions to the program—what parts you liked
and what parts you didn’t like. I’d like you to turn to the first page of the questionnaire and
answer the questions. Please don’t go on to the next page until I ask you to.
Reactions to the Ads
All right. Now we’d like to find out about your reactions to the advertisements you saw—what
you liked and what you didn’t like. I’d like you to turn to the second section of the questionnaire
and answer the questions. Please don’t go on to the next section until I ask you to.
Reactions to Your Ad
All right. Now we’d like to find out about your reactions to one specific ad. I will play it again and
then ask you to complete a few more questions. [Play your ad again] Now I’d like you to turn to
the next section of the questionnaire and answer the questions.
211
APPENDIX A

Tabulating Responses to Closed- and Open-Ended Questions
Tabulating Responses to Closed-Ended Questions
Closed-ended questions force participants to select a response from several alternatives.
A quick method for tabulating or counting responses to each question is to use a
blank questionnaire:
1. Take the first questionnaire and record the answers to each closed-ended question by
making a check mark in the right-hand column next to the appropriate response.
2. Repeat this procedure for every questionnaire.
3. Tally the total number of check marks and then calculate the percentage of participants
who gave each response.
Tabulating Responses to Open-Ended Questions
Tabulating or counting responses to open-ended questions is more time consuming. Open-
ended questions allow participants to express themselves in their own words. For example:
• What did the message say?
• What did the message show?
• What was the main idea the message was trying to get across?
The easiest way to analyze these questions is to write each question at the top of a separate
blank page (the coding sheet). Because participants are answering in their own words, the first
step is to group the responses into categories (e.g., correct, partially correct, and incorrect).
When categorizing the audience recall and main idea responses, use the ad script and your
own statement of the message’s main points to guide the analysis. For some open-ended
questions (e.g., “What, if anything, did you like about the message?” or “What, if anything, did
you dislike?”), you may wish to classify the responses as favorable or unfavorable.
Use the following procedure to tally the responses:
1. Take the first questionnaire and record the answers to each open-ended question by
making a check mark in the appropriate column (e.g., favorable or unfavorable).
2. Repeat this procedure for every questionnaire.
3. Tally the total number of check marks in each column and then calculate the percentage
of participants who gave each type of response.
Once you have tabulated the responses to each question, your interpretation should be guided
by the objectives you set forth in the planning stage.
212

Average Ratings for Commercial Ads to Help Interpret
Standard Pretesting Questions
1
Variable/Descriptor Females 18–65 Males 18–65
% Who Completely Agree
2
% Who Completely Agree
2
:30 Rough :30 Finished :30 Rough :30 Finished
Com’l Norm Com’l Norm Com’l Norm Com’l Norm
Effective main idea (% of 40 40 40 40
respondents who agree
on a single main idea)
Appropriate 49 53 48 54
Attention-getting 35 47 34 44
Believable 38 40 37 40
Confusing 4 5 5 6
Convincing 31 33 28 31
Effective 36 43 --- ---
Informative 36 36 37 37
Interesting 23 30 23 35
Meaningful 23 28 --- ---
Relevant 28 29 25 29
Something you could relate to 36 37 37 34
Told you something important 23 25 28 28
Told you something new 30 28 26 27
Worth remembering 22 33 19 ---
1
This table, based on the Ipsos-ASI, Inc., Market Research Database of Diagnostic Norms, includes national
averages for standard copy test questions used in testing commercial ads. Please note that these norms are
derived from national telephone interviews (rather than mall intercepts or theater testing) and include findings
from stand-alone viewing.
2
Responses are on a 3-point scale: completely agree, somewhat agree, do not agree at all.
APPENDIX A
Continued on next page...
213
This table can be helpful in comparing your ad pretest to previous pretest results. This
comparison should not be the sole basis of your analysis. Rather, the ranges should serve as
guidelines. They are designed to help you extract meaning from the percentages you compute
for your test ad. Before drawing any conclusions or making recommendations, you should
analyze the results for every question.
This book cannot provide ranges or guidelines for the questions that relate specifically to your
test ad. Therefore, you will have to interpret the percentages on your own. Ask yourself how
critical it is for the majority of participants to respond in a certain manner to each question. For
example, if the test ad communicates the main idea through music, it is essential that a large
majority report being able to understand the words to the music. On the other hand, if the
music in the ad serves only as background sound, then it is not as critical for the lyrics to be
understood.
It is important to examine how many responses to open-ended questions fall into each
category (correct, partially correct, or incorrect; favorable or unfavorable). Ideally, the majority
of responses will fall into the correct category. This pattern tends to confirm that the test ad is
meeting its objectives. On the other hand, if the majority of responses are categorized as
partially correct or incorrect, the ad may not be meeting your communication objectives.
Statistical Techniques
You can use statistical techniques to analyze subgroup information (e.g., males vs. females, or
younger participants vs. older ones) only if you boost the sample size to at least 50 participants
in each subgroup. If you recruit only 50 participants in total, the sample will be too small to be
reviewed by subgroup. Comparing findings between subgroups that are too small can be
misleading and may result in faulty conclusions.
Do not try to make generalizations from the results of this pretest to ad messages in general.
Each ad pretest you conduct will provide direction for making changes that might be necessary
before final production and for improving the potential effectiveness of each particular
message. The sample size and the methodology used do not allow for formulating definitive
conclusions about what your message’s impact will be after it is distributed.
214

APPENDIX A
215

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
APPENDIX B
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Selected Planning Frameworks,
Social Science Theories, and
Models of Change
*
APPENDIX B
* From Theory at a Glance: A Guide for Health Promotion Practice (NIH Publication No.
97-3896), by the National Cancer Institute, 1995. Bethesda, MD. In the public domain.

Planning Systems/Frameworks
Once health communications planners identify a health problem, they can use a planning
framework such as the two described below: social marketing and PRECEDE-PROCEED.
These planning systems can help identify the social science theories most appropriate for
understanding the problem or situation. Thus, planners use the theories and models described
below within the construct of a planning framework.
Using planning systems like social marketing and PRECEDE-PROCEED increases the odds of
program success by examining health and behavior at multiple levels. Planning system
perspectives emphasize changing people, their environment, or both.
Social Marketing
Social marketing has been defined as “the application of commercial marketing technologies to
the analysis, planning, execution, and evaluation of programs designed to influence the
voluntary behavior of target audiences in order to improve their personal welfare and that of
their society” (Andreason, 1995). This definition encompasses several key aspects of the social
marketing approach; it is seen as:
1. A key benefit to individuals and society; not focused on profit and organizational benefits as
commercial marketing practices are
2. A focus on behavior, not awareness or attitude change
3. An approach centered on the target audience’s having a primary role in the process
Social marketing practices are based on commercial marketing practices that make the
consumer the central focus for planning and conducting a program. The program's
components address:
• Price—what the consumer must give up in order to receive the program’s benefits (these
costs may be intangible [e.g., changes in beliefs or habits] or tangible [e.g., money, time,
or travel])
• Product—what the program is trying to change within the intended audience and what the
audience stands to gain
• Promotion—how the exchange is communicated (e.g., appeals used)
• Place—what channels the program uses to reach the intended audience (e.g., mass media,
community, or interpersonal)
The formulation of price, product, promotion, and place evolves from research with the
consumers to determine what benefits and costs they would consider acceptable and how
they might be reached. Lessons learned from social marketing stress the importance of
understanding the intended audiences and designing strategies based on their wants and
needs rather than what good health practice directs that they should do.
For Further Reading
Andreason, A. (1995). Marketing social change: Changing behavior to promote health, social
development, and the environment. San Francisco: Jossey-Bass.
218
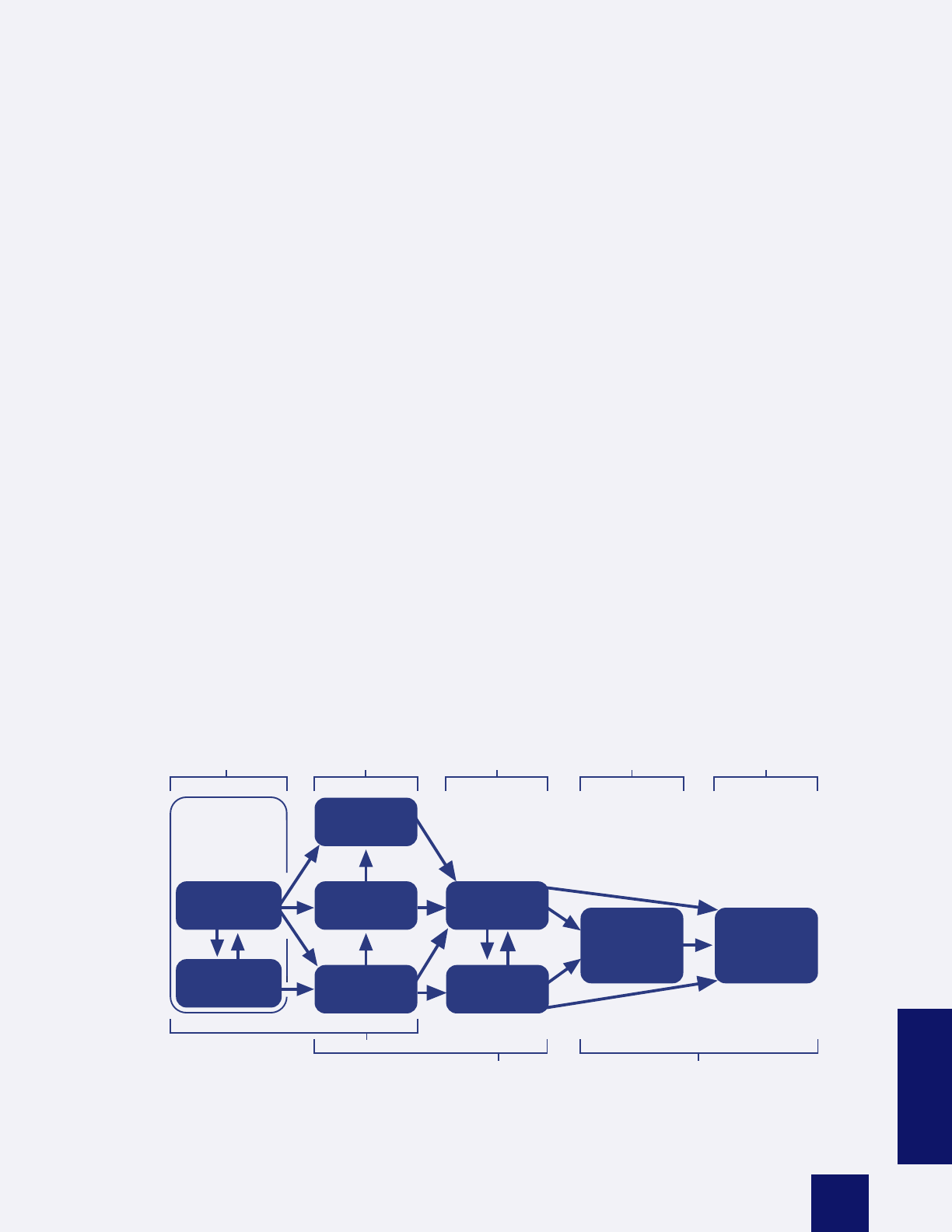
Kotler, P., & Roberto, E. L. (1989). Social marketing: Strategies for changing public behavior.
New York: Free Press.
Lefebvre, R. C., & Rochlin, L. (1997). Social marketing. In K. Glanz, F. M. Lewis, & B. K. Rimer
(Eds.), Health behavior and health education: Theory, research, and practice (2nd ed.).
San Francisco: Jossey-Bass.
PRECEDE-PROCEED
The PRECEDE-PROCEED framework is an approach to planning that examines the factors
contributing to behavior change. These include:
• Predisposing factors—the individual’s knowledge, attitudes, behavior, beliefs, and values
before intervention that affect willingness to change
• Enabling factors—factors in the environment or community of an individual that facilitate or
present obstacles to change
• Reinforcing factors—the positive or negative effects of adopting the behavior (including
social support) that influence continuing the behavior
These factors require that individuals be considered in the context of their community
and social structures, and not in isolation, when planning communication or health
education strategies.
PRECEDE-PROCEED Framework
PRECEDE
PHASE 5
PHASE 4
PHASE 3
PHASE 2
PHASE 1
Administration
Educational and
Behavioral and
Epidemiological
Social
and Policy
Organizational
Environmental
Diagnosis
Diagnosis
Diagnosis
Diagnosis
Diagnosis
Health
Promotion
Health
education
Policy regulation
organization
Predisposing
factors
Reinforcing
factors
Enabling
factors
Behavior and
lifestyle
Environment
Health
Quality
of life
PHASE 6 PHASE 7
PHASE 8 PHASE 9
Implementation Process
Impact
Outcome
Evaluation
Evaluation
Evaluation
PROCEED
219
APPENDIX B
For Further Reading
Green, L. W., & Kreuter, M. W. (1999). Health promotion planning: An educational and
ecological approach (3rd ed.). Mountain View, CA: Mayfield.
Green, L. W., & Ottoson, J. M. (1999). Community and population health (8th ed.). New York:
McGraw-Hill.
Selected Social Science Theories, Models, and Constructs
Individual Level
Behavioral Intentions
Studies of behavioral intentions suggest that the likelihood of intended audiences’ adopting a
desired behavior can be predicted by assessing (and subsequently trying to change or
influence) their attitudes toward and perceptions of benefits of the behavior, along with how
they think that their peers will view their behavior. Research by Fishbein and Ajzen supports
the idea that individuals’ and society’s (perceived) attitudes are an important predecessor to
action. Therefore, an important step toward influencing behavior is a preliminary assessment
of intended audience attitudes, and subsequent tracking is necessary to identify any
attitudinal changes.
For Further Reading
Fishbein, M., & Ajzen, I. (1975). Belief, attitude, intention and behavior: An introduction to
theory and research. Reading, MA: Addison-Wesley.
Communications for Persuasion
William McGuire has described the steps an individual must be persuaded to pass through to
assimilate a desired behavior. These steps are:
• Exposure to the message
• Attention to the message
• Interest in or personal relevance of the message
• Understanding of the message
• Personalizing the behavior to fit one’s life
• Accepting the change
• Remembering the message and continuing to agree with it
• Being able to think of it
• Making decisions based on bringing the message to mind
• Behaving as decided
• Receiving positive reinforcement for behavior
• Accepting the behavior into one’s life
220

To communicate the message successfully, five communication components all must work:
1. Credibility of the message source
2. Message design
3. Delivery channel
4. Intended Audience
5. Intended behavior
Paying attention to McGuire’s steps helps ensure that a communication program plan
addresses all the factors that determine whether a message is received and absorbed, that the
program is staged over time to address intended audience needs as they differ over time, and
that progress is being made toward behavior change.
For Further Reading
McGuire, W. J. (1984). Public communication as a strategy for inducing health-promoting
behavioral change. Preventive Medicine, 13(3), 299–313.
Stages of Change
The basic premise of the stages-of-change construct, the central construct of the
transtheoretical model, is that behavior change is a process and not an event and that
individuals are at varying levels of motivation, or readiness, to change. People at different
points in the process of change can benefit from different interventions, matched to their stage
at that time.
By knowing an individual’s current stage, you can help set realistic program goals.You can also
tailor messages, strategies, and programs to the appropriate stage.
Five distinct stages are identified in the stages-of-change construct:
1. Precontemplation
2. Contemplation
3. Decision/determination
4. Action
5. Maintenance
It is important to note that this is a circular, not a linear, model. People don’t go through the
stages and “graduate”; they can enter and exit at any point, and often recycle.
For Further Reading
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change.
American Journal of Health Promotion, 12(1), 38–48.
APPENDIX B
221

Health Belief Model
The health belief model (HBM) was originally designed to explain why people did not
participate in programs to prevent or detect diseases. The core components of HBM include:
• Perceived susceptibility—the subjective perception of risk of developing a particular
health condition
• Perceived severity—feelings about the seriousness of the consequences of developing
a specific health problem
• Perceived benefits—beliefs about the effectiveness of various actions that might reduce
susceptibility and severity (taken together, perceived susceptibility and severity are
labeled “threat”)
• Perceived barriers—potential negative aspects of taking specific actions
• Cues to action—bodily or environmental events that trigger action
More recently, HBM has been amended to include the notion of self-efficacy as another
predictor of health behaviors—especially more complex ones in which lifestyle changes must
be maintained over time. A wide variety of demographic, social, psychological, and structural
variables may also impact people’s perceptions and, indirectly, their health-related behaviors.
Some of the more important variables include educational attainment, age, gender,
socioeconomic status, and prior knowledge.
For Further Reading
Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health Education
Quarterly, 11, 1–47.
Strecher, V. J., & Rosenstock, I. M. (1997). The health belief model. In K. Glanz, F. M. Lewis,
& B. K. Rimer (Eds.), Health behavior and health education: Theory, research, and practice
(2nd ed.). San Francisco: Jossey-Bass.
Consumer Information Processing Model
The consumer information processing (CIP) model was not developed specifically to study
health-related behavior, nor to be applied in health promotion programs, but it has many useful
applications in the health arena. Information is a common tool for health education and is often
an essential foundation for health decisions.
Information can increase or decrease people’s anxiety, depending on their information
preferences and how much and what kind of information they are given. Also, illness and its
treatments can interfere with information processing. By understanding the key concepts and
processes of CIP, health educators can examine why people use or fail to use health
information and design informational strategies to better chances for success. CIP theory
reflects a combination of rational and motivational ideas. The use of information is an
intellectual process; however, motivation drives the search for information and how much
attention people pay to it. The central assumptions of CIP are that 1) individuals are limited in
how much information they can process, and 2) to increase the usability of information, they
222

combine bits of information into “chunks” and create decision rules, known as heuristics, to
make choices faster and more easily. According to basic CIP concepts, before people will use
health information, it must be 1) available, 2) seen as useful and new, and 3) processable, or
format-friendly.
For Further Reading
Bettman, J. R. (1979). An information processing theory of consumer choice. Reading, MA:
Addison-Wesley.
Interpersonal Level
Social Cognitive Theory
Social cognitive theory (SCT) explains behavior in terms of triadic reciprocality (“reciprocal
determinism”) in which behavior, cognitive and other interpersonal factors, and environmental
events all operate as interacting determinants of one another. SCT describes behavior as
dynamically determined and fluid, influenced by both personal factors and the environment.
Changes in any of these three factors are hypothesized to render changes in the others.
One of the key concepts in SCT is the environmental variable: observational learning. In
contrast to earlier behavioral theories, SCT views the environment as not just a variable that
reinforces or punishes behaviors, but one that also provides a milieu where an individual can
watch the actions of others and learn the consequences of those behaviors. Processes
governing observational learning include:
• Attention—gaining and maintaining attention
• Retention—being remembered
• Reproduction—reproducing the observed behavior
• Motivation—being stimulated to produce the behavior
Other core components of SCT include:
• Self-efficacy—judgment of one’s capability to accomplish a certain level of performance
• Outcome expectation—judgment of the likely consequence such behavior will produce
• Outcome expectancies—the value placed on the consequences of the behavior
• Emotional coping responses—strategies used to deal with emotional stimuli, including
psychological defenses (denial, repression), cognitive techniques such as problem
restructuring, and stress management
• Enactive learning—learning from the consequences of one’s actions (versus
observational learning)
• Rule learning—generating and regulating behavioral patterns, most often achieved through
vicarious processes and capabilities (versus direct experience)
• Self-regulatory capability—much of behavior is motivated and regulated by internal
standards and people’s self-evaluative reactions to their own actions
APPENDIX B
223

For Further Reading
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory.
Englewood Cliffs, NJ: Prentice-Hall.
Lefebvre, R. C. (2000). Theories and models in social marketing. In P. N. Bloom & G. T.
Gundlach (Eds.), Handbook of marketing and society. Thousand Oaks, CA: Sage.
Organization/Community/Societal Level
Organizational Change Theory
Organizations are complex and layered social systems, composed of resources, members,
roles, exchanges, and unique cultures. Thus, organizational change can best be promoted by
working at multiple levels within the organization. Understanding organizational change is
important in promoting health to help establish policies and environments that support healthy
practices and create the capacity to solve new problems. While there are many theories of
organization behavior, two are especially promising in public health interventions: stage theory
and organizational development (OD) theory.
Stage theory is based on the idea that organizations pass through a series of steps or stages
as they change. By recognizing those stages, strategies to promote change can be matched
to various points in the process of change. An abbreviated version of stage theory involves
four stages:
1. Problem definition (awareness)
2. Initiation of action (adoption)
3. Implementation
4. Institutionalization
OD theory grew out of the recognition that organizational structures and processes influence
worker behavior and motivation. OD theory concerns the identification of problems that impede
an organization’s functioning, rather than the introduction of a specific type of change. Human
relations and quality of work-life factors are often the targets of OD problem diagnosis, action
planning, interventions, and evaluation. A typical OD strategy involves process consultation,
in which an outside specialist helps identify problems and facilitates the planning of
change strategies.
Stage theory and OD theory have the greatest potential to produce health-enhancing change
in organizations when they are combined. That is, OD strategies can be used at various stages
as they are warranted. Simultaneously, the stages signal the need to involve organization
members and decision-makers at various points in the process.
224

For Further Reading
Beyer, J. M., & Trice, H. M. (1978). Implementing change: Alcoholism policies in work
organizations. New York: Free Press.
Porras, J. I., & Roberston, P. J. (1987). Organization development theory: A typology and
evaluation. In R. W. Woodman & W. A. Pasmore (Eds.), Research in organizational change and
development (Vol. 1). Greenwich, CT: JAI Press.
Community Organization Theory
Community organization theory has its roots in theories of social networks and support. It
emphasizes active participation and developing communities that can better evaluate and solve
health and social problems. Community organization is the process by which community
groups are helped to identify common problems or goals, mobilize resources, and develop and
implement strategies for reaching their goals. It has roots in several theoretical perspectives:
the ecological perspective, social systems perspective, social networks, and social support.
It is also consistent with social learning theory (SLT) and can be successfully used along
with SLT-based strategies. Community organization is composed of several alternative
change models:
• Locality development (also called community development) uses a broad cross-section of
people in the community to identify and solve its own problems. It stresses consensus
development, capacity building, and a strong task orientation; outside practitioners help to
coordinate and enable the community to successfully address its concerns.
• Social planning uses tasks and goals, and addresses substantive problem solving, with
expert practitioners providing technical assistance to benefit community consumers.
• Social action aims to increase the problem-solving ability of the community and to achieve
concrete changes to redress social injustice that is identified by a disadvantaged or
oppressed group.
Although community organization does not use a single unified model, several key concepts
are central to the various approaches. The process of empowerment is intended to stimulate
problem solving and activate community members. Community competence is an approximate
community-level equivalent of self-efficacy plus behavioral capability, which are the confidence
and skills to solve problems effectively. Participation and relevance go together: They involve
citizen activation and a collective sense of readiness for change. Issue selection concerns
identifying “winnable battles” as a focus for action, and critical consciousness stresses the
active search for root causes of problems.
Social action approaches to community organizing go beyond the traditional notion of
geographic and political boundaries. Communities of people who share common health
problems have coalesced to attract attention to and to obtain power to address their needs—
including health services, antidiscrimination policies, and more research funding. Foremost
among these groups presently are AIDS activists. Women’s health advocates have also used
social action to pressure powerful institutions to address their problems; breast cancer is now
a focus for action and advocacy among breast cancer survivors and their relatives. They have
used media advocacy as a powerful tool in their efforts.
APPENDIX B
225

Media advocacy is the strategic use of mass media as a resource for advancing a social or
public policy initiative. It is an important, and often essential, part of social action and advocacy
campaigns because the media focus public concern and spur public action. The core
components of media advocacy are developing an understanding of how an issue relates to
prevailing public opinions and values and designing messages that frame the issues so as to
maximize their impact and attract powerful and broad public support.
For Further Reading
Rothman, J., & Tropman, J. E. (1987). Models of community organization and macro practice:
Their mixing and phasing. In F. M. Cox, J. L. Ehrlich, J. Rothman, & J. E. Tropman (Eds.),
Strategies of community organization (4th ed.). Itasca, IL: Peacock.
Diffusion of Innovations Theory
Diffusion of innovations theory addresses how new ideas, products, and social practices
spread within a society or from one society to another. The challenge of diffusion requires
approaches that differ from those focused solely on individuals or small groups. It involves
paying attention to the innovation (a new idea, product, practice, or technology) as well as to
communication channels and social systems (networks with members, norms, and
social structures).
A focus on the characteristics of innovations can improve the chances that they will be adopted
and hence diffused. It also has implications for how an innovation is positioned to maximize its
appeal. Some of the most important characteristics of innovations are their:
• Relative advantage—is it better than what was there before?
• Compatibility—fit with intended audience
• Complexity—ease of use
• Trialability—can it be tried out first?
• Observability—visibility of results
Communication channels are another important component of diffusion of innovations theory.
Diffusion theories view communication as a two-way process rather than one of merely
“persuading” an intended audience to take action. The two-step flow of communication—in
which opinion leaders mediate the impact of mass media—emphasizes the value of social
networks (or interpersonal channels) over and above mass media for adoption decisions.
For Further Reading
Green, L. W., Gottlieb, N. H., & Parcel, G. S. (1987). Diffusion theory extended and applied. In
W. B. Ward (Ed.), Advances in health education and promotion. Greenwich, CT: JAI Press.
Rogers, E. M. (1983). Diffusion of innovations (3rd ed.). New York: Free Press.
226

APPENDIX B
227

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
APPENDIX C
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Information Sources
APPENDIX C

National Sources of Health-Related Information
Agency for Healthcare Research and Quality (AHRQ)
Publication Clearinghouse
P.O. Box 8547
Silver Spring, MD 20907-8547
1-800-358-9295
www.ahrq.gov
American Cancer Society (ACS)
1599 Clifton Road, NE
Atlanta, GA 30329
1-800-ACS-2345
www.cancer.org
Cancer Information Service
National Cancer Institute
6116 Executive Boulevard, SMC 8322
Room 3036A
Bethesda, MD 20892
1-800-4-CANCER (1-800-422-6237)
Center for Substance Abuse Prevention
National Clearinghouse for Alcohol and Drug Information
P.O. Box 2345
Rockville, MD 20847-2345
1-800-729-6686
Centers for Disease Control and Prevention (CDC)
www.cdc.gov
Centers for Medicare and Medicaid Services
7500 Security Boulevard
Baltimore, MD 21244-1850
1-800-638-6833 (Medicare)
202-690-6145 (Press Office)
www.cms.gov
Health Promotion Online—Canada
Partnerships and Marketing Division
Health Promotion and Programs Branch
Health Canada
55 St. Clair Avenue East, 4th Floor
Toronto, Ontario
M4T 1M2
www.hc-sc.gc.ca/hppb/hpo
230

National Center for Chronic Disease Prevention and Health Promotion
Division of Cancer Prevention and Control
4770 Buford Highway, NE
Atlanta, GA 30341-3724
770-488-4880
770-488-4727 (fax)
www.cdc.gov/nccdphp
National Center for Health Statistics
6525 Belcrest Road
Hyattsville, MD 20782-2003
301-458-4636
www.cdc.gov/nchs
Roper Center for Public Opinion Research
341 Mansfield Road
Unit 1164
University of Connecticut
Storrs, CT 06269-1164
860-486-4440
www.ropercenter.uconn.edu
U.S. Department of Health and Human Services
200 Independence Avenue, SW
Washington, DC 20201
202-619-0257
1-877-696-6775
www.os.dhhs.gov
Internet Resources
Combined Health Information Database
http://chid.nih.gov
Community Toolbox
http://ctb.lsi.ukans.edu
Health Education Professional Resources
www.nyu.edu/education/hepr/index.html
Healthfinder
(To locate Federal Clearinghouse and other Federal information sources)
www.healthfinder.gov
APPENDIX C
231

Journals
American Journal for Health Promotion
1660 Cass Lake Road
Suite 104
Keego Harbor, MI 48320
248-682-0707
248-682-1212 (fax)
www.healthpromotionjournal.com/index.htm
American Journal of Health Behavior
American Academy of Health Behavior
P.O. Box 4593
Star City, WV 26504-4593
http://131.230.221.136/ajhb
American Journal of Public Health
American Public Health Association
800 I Street, NW
Washington, DC 20001
202-777-APHA
202-777-2534 (fax)
www.apha.org/journal/AJPH2.htm
Health Education and Behavior
Society for Public Health Education
1015 15th Street, NW
Suite 410
Washington, DC 20005
202-408-9804
202-408-9815 (fax)
inf[email protected] (e-mail)
www.sph.umich.edu/hbhe/heb
Health Education Research
Oxford University Press
2001 Evans Road
Cary, NC 27513
www.oup.co.uk/healed
232

Journal of Health Communication
Department of International Public Health
School of Public Health and Health Services
The George Washington University
2175 K Street, NW
Suite 820
Washington, DC 20037
www.aed.org/jhealthcom
Journal of the American Medical Association
515 North State Street
Chicago, IL 60610
312-464-5000
http://jama.ama-assn.org
Morbidity and Mortality Weekly Report (MMWR)
Centers for Disease Control and Prevention
1600 Clifton Road
Atlanta, GA 30333
www.cdc.gov/mmwr
The New England Journal of Medicine
10 Shattuck Street
Boston, MA 02115-6094
617-734-9800
617-734-4457 (fax)
www.nejm.org
Social Marketing Quarterly
Best Start Social Marketing
4809 East Busch Boulevard
Suite 104
Tampa, FL 33617
813-971-2119
813-971-2280 (fax)
APPENDIX C
233

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
APPENDIX D
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Selected Readings
and Resources
APPENDIX D

Academy for Educational Development. (1995). A tool box for building health communication
capacity. Washington, DC.
Adler, E. (1993). Everyone’s guide to successful publications: How to produce powerful
brochures, newsletters, flyers, and business communications, start to finish. Berkeley, CA:
PeachPit.
Agency for International Development, Academy for Educational Development. (1992).
Results and realities: A decade of experience in communication for child survival.
Washington, DC.
Agency for Toxic Substances and Disease Registry. (1994). Guidelines for planning and
evaluating environmental health education programs. Atlanta.
American Cancer Society. (2001). Cancer facts and figures. Atlanta.
American Marketing Association, New York Chapter. (2001). The focus group directory.
New York.
American Marketing Association, New York Chapter. (2001/2002). Green Book: International
directory of marketing research companies and services. New York.
American Public Health Association. (2000). APHA media advocacy manual 2000.
Washington, DC.
Andreasen, A. (1988). Cheap but good marketing research. Homewood, IL: Dow Jones-Irvin.
Andreasen, A. (1995). Marketing social change: Changing behavior to promote health, social
development, and the environment. San Francisco: Jossey-Bass.
Arkin, E. B., Romano, R. M., Van Nevel, J. P., & McKenna, W. (1993). Effect of the mass media
in promoting calls to the Cancer Information Service. In The Cancer Information Service: A 15-
year history of service and research (Monograph of the Journal of the National Cancer
Institute, No. 14).
Backer, T. E., Rogers, E. M., & Sopory, P. (1992). Designing health communication campaigns:
What works. Thousand Oaks, CA: Sage.
Bandura, A. (1986). Social foundations of thought and action: A social cognitive theory.
Englewood Cliffs, NJ: Prentice-Hall.
Bettman, J. R. (1979). An information processing theory of consumer choice. Reading, MA:
Addison-Wesley.
Calvert, P. (Ed.). (1996). The communicator’s handbook: Tools, techniques, and technology
(3rd ed.). Gainesville, FL: Maupin House.
236

Campbell, M. K., DeVellis, B. M., Strecher, V. J., Ammerman, A. S., DeVellis, R. F., & Sandler,
R. S. (1994). The impact of message tailoring on dietary behavior change for disease
prevention in primary care settings. American Journal of Public Health, 84, 783–787.
Center for Substance Abuse Prevention. (1994). Careful concept development paves the way
to effective prevention materials [Technical Assistance Bulletin]. Washington, DC: U.S.
Government Printing Office.
Center for Substance Abuse Prevention. (1994). Conducting focus groups with young children
requires special considerations and techniques [Technical Assistance Bulletin].
Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1994). Following specific guidelines will help you
assess cultural competence in program design, application, and management [Technical
Assistance Bulletin]. Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1994). A key step in developing prevention materials
is to obtain expert and gatekeeper reviews [Technical Assistance Bulletin]. Washington, DC:
U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1994). Pretesting is essential: You can choose from
various methods [Technical Assistance Bulletin]. Washington, DC: U.S. Government Printing
Office.
Center for Substance Abuse Prevention. (1994). You can increase your media coverage
[Technical Assistance Bulletin]. Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1994). You can manage focus groups effectively
for maximum impact [Technical Assistance Bulletin]. Washington, DC: U.S. Government
Printing Office.
Center for Substance Abuse Prevention. (1994). You can prepare easy-to-read materials
[Technical Assistance Bulletin]. Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1994). You can use communications principles to
create culturally sensitive and effective prevention materials [Technical Assistance Bulletin].
Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention. (1998). Evaluating the results of communication
programs [Technical Assistance Bulletin]. Washington, DC: U.S. Government Printing Office.
Center for Substance Abuse Prevention Communications Cooperative Agreements. (1996).
Bridging the gap for people with disabilities. Rockville, MD: U.S. Department of Health and
Human Services.
APPENDIX D
237

Centers for Disease Control and Prevention. (1994). Listening to your audience: Using focus
groups to plan breast and cervical cancer public education programs (CDC Publication No.
PDF-245K). Denver: AMC Cancer Research Center.
Centers for Disease Control and Prevention. (1994). The prevention marketing initiative
community kit: It’s your move, prevent AIDS (CDC Publication No. D738). Atlanta.
Centers for Disease Control and Prevention. (1996). The prevention marketing initiative:
Applying prevention marketing (CDC Publication No. D905). Atlanta.
Centers for Disease Control and Prevention. (2000). Beyond the brochure (CDC Publication
No. PDF-821K). Atlanta.
Centers for Disease Control and Prevention. (2001). CDCynergy 2001 [CD-ROM].
Atlanta.
Coyle, S. L., Boruch, R. F., & Turner, C. F. (Eds.). (1991). Evaluating AIDS prevention programs:
Expanded edition. Washington, DC: National Academy Press.
Davis, J. (Ed.). (2001). Health and medicine on the Internet: An annual guide to the World
Wide Web for health care professionals. Los Angeles: Practice Management
Information Corporation.
Debus, M. (1988). Methodological review: A handbook for excellence in focus group research.
Washington, DC: Academy for Educational Development.
The Dialog Corporation. (2001). Packaged facts. Available:
http://library.dialog.com/sourcebook/researchline/pf.html.
Dignan, M. B., & Carr, P. A. (1992). Program planning for health education and health
promotion (2nd ed.). Philadelphia: Lea & Febiger.
Eng, T. R., & Gustafson, D. H. (Eds.). (1999). Wired for health and well-being: The emergence
of interactive health communication. Washington, DC: U.S. Department of Health and Human
Services, U.S. Government Printing Office.
Fishbein, M., & Ajzen, I. (1975). Belief, attitude, intention and behavior: An introduction to
theory and research. Reading, MA: Addison-Wesley.
Flay, B. R., & Cook, T. D. (1989). Three models for evaluating prevention campaigns with a
mass media component. In R. E. Rice & C. K. Atkin (Eds.), Public communication campaigns
(2nd ed.). Thousand Oaks, CA: Sage.
Flay, B. R., Kessler, R. C., & Utts, J. M. (1991). Evaluating media campaigns. In S. L. Coyle,
R. F. Boruch, & C. F. Turner (Eds.), Evaluating AIDS prevention programs. Washington, DC:
National Academy Press.
238

Glanz, K., Lewis, F. M., & Rimer, B. K. (Eds.). (1997). Health behavior and health education:
Theory, research, and practice (2nd ed.). San Francisco: Jossey-Bass.
Glanz, K., & Rimer, B. K. (1995). Theory at a glance: A guide for health promotion practice
(NIH Publication No. 97-3896). Bethesda, MD: National Cancer Institute.
Glassman, B. & Rimer, B. K. (1999). Is there a use for tailored print communications in cancer
risk communications? (Monograph of the Journal of the National Cancer Institute, No. 25).
Goldberg, M. E., Fishbein, M. F., & Middlestadt, S. E. (Eds.). (1997). Social marketing:
Theoretical and practical perspectives. Mahwah, NJ: Erlbaum.
Green, L. W., Gottlieb, N. H., & Parcel, G. S. (1987). Diffusion theory extended and applied. In
W. B. Ward (Ed.), Advances in health education and promotion. Greenwich, CT: JAI Press.
Green, L. W., & Kreuter, M. W. (1999). Health promotion planning: An educational and
ecological approach (3rd ed.). Mountain View, CA: Mayfield.
Green, L. W., & Ottoson, J. M. (1999). Community and population health (8th ed.). New York:
McGraw-Hill.
Ipsos-ASI, Inc. Market research database of diagnostic norms. Norwalk, CT. Information:
www.ipsos-asi.com.
Janz, N. K., & Becker, M. H. (1984). The health belief model: A decade later. Health Education
Quarterly, 11, 1–47.
Jernigan, D. H., & Wright, P. A. (1996). Media advocacy: Lessons from community experiences.
Journal of Public Health Policy, 17, 306–330.
Jones, J. P. (Ed.). (1998). How advertising works: The role of research. Thousand Oaks,
CA: Sage.
Kotler, P., & Roberto, E. L. (1989). Social marketing: Strategies for changing public behavior.
New York: Free Press.
Lefebvre, R. C. (2000). Theories and models in social marketing. In P. N. Bloom & G. T.
Gundlach (Eds.), Handbook of marketing and society. Thousand Oaks, CA: Sage.
Lefebvre, R. C., & Rochlin, L. (1997). Social marketing. In K. Glanz, F. M. Lewis, & B. K. Rimer
(Eds.), Health behavior and health education: Theory, research, and practice (2nd ed.). San
Francisco: Jossey-Bass.
Lipkus, I. M., Lyna, P. R., & Rimer, B. K. (1999). Using tailored interventions to enhance
smoking cessation among African Americans at the community health center. Nicotine and
Tobacco Research, 1(1), 77–85.
APPENDIX D
239

Maibach, E., Maxfield, A., Ladin, K., & Slater, M. (1996). Translating health psychology into
effective health communication. Journal of Health Psychology, 1, 261–277.
Maibach, E., & Parrott, R. L. (Eds.). (1995). Designing health messages: Approaches from
communication theory and public health practice. Thousand Oaks, CA: Sage.
Marketing Research Association. (2001). Blue book 2001. Available:
www.bluebook.org/scripts/bluebook/index.efm.
Matiella, A. C. (Ed.). (1990). Getting the word out: A practical guide to AIDS materials
development. Santa Cruz, CA: Network Publications.
McGuire, W. J. (1984). Public communication as a strategy for inducing health-promoting
behavioral change. Preventive Medicine, 13(3), 299–313.
Merton, R. K. (1987). Focused interviews and focus groups: Continuities and discontinuities.
Public Opinion Quarterly, 51, 550–556.
Merton, R. K., Riske, M., & Kendall, P. L. (1996). The focused interview (2nd ed.). New York:
Free Press.
Miller, J., & Pifer, L. K. (1993). Public understanding of biomedical science in the United
States, 1993: A report to the National Institutes of Health. Chicago: Chicago Academy
of Science.
Morgan, D. L., & Krueger, R. A. (1998). The focus group kit. Thousand Oaks, CA: Sage.
Morra, M. E. (Ed.). (1998). The impact and value of the Cancer Information Service: A model for
health communication. Journal of Health Communication, 3(3) Suppl.
Muraskin, L. D. (1993). Understanding evaluation: The way to better prevention programs.
Washington, DC: U.S. Department of Education.
National Cancer Institute. (1993). A picture of health (NIH Publication No. 94-3604). Rockville,
MD: U.S. Department of Health and Human Services.
National Cancer Institute. (1994). Clear and simple: Developing effective print materials for
low-literate readers (NIH Publication No. 95-3594). Rockville, MD: U.S. Department of Health
and Human Services.
National Cancer Institute. (1996). Cancer rates and risks (4th ed.; NIH Publication No. 96-691).
Bethesda, MD: Surveillance, Epidemiology, and End Results (SEER) Program.
National Cancer Institute. (1998) How the public perceives, processes, and interprets risk
information: Findings from focus group research with the general public. Rockville, MD: U.S.
Department of Health and Human Services.
240

National Cancer Institute. (1998). Media strategies for smoking control guidelines.
Bethesda, MD: U.S. Department of Health and Human Services.
National Cancer Institute. (2000). Multi-ethnic focus groups to test motivational messages on
mammography and breast cancer. Bethesda, MD.
Palmgreen, P., et al. (1995). Reaching at-risk populations in a mass media drug abuse
prevention campaign: Sensation seeking as a targeting variable. Drugs and Society, 8(3),
29–45.
Porras, J. I., & Roberston, P. J. (1987). Organization development theory: A typology and
evaluation. In R. W. Woodman & W. A. Pasmore (Eds.), Research in organizational change and
development (Vol. 1). Greenwich, CT: JAI Press.
Prochaska, J. O., & Velicer, W. F. (1997). The transtheoretical model of health behavior change.
American Journal of Health Promotion, 12(1), 38–48.
Rice, M., & Valdivia, L. (1991). A simple guide for design, use, and evaluation for education
materials. Health Education Quarterly, 18(1), 79–85.
Rice, R. E., & Atkin, C. K. (2000). Public communication campaigns (3rd ed.). Thousand Oaks,
CA: Sage.
Rimer, B. K. (1995). Audiences and messages for breast and cervical cancer screenings.
Wellness Perspectives: Research, Theory, and Practice, 11(2), 13–39.
Rimer, B. K., & Glassman, B. (1998). Tailoring communications for primary care settings.
Methods of Information in Medicine, 37(3), 171–177.
Rogers, E. M. (1983). Diffusion of innovations (3rd ed.). New York: Free Press.
Rossi, P. H., Freeman, H. E., & Lipsey, M. W. (1998). Evaluation: A systematic approach
(6th ed.). Thousand Oaks, CA: Sage.
Rothman, J., & Tropman, J. E. (1987). Models of community organization and macro practice:
Their mixing and phasing. In F. M. Cox, J. L. Ehrlich, J. Rothman, & J. E. Tropman (Eds.),
Strategies of community organization (4th ed.). Itasca, IL: Peacock.
Schooler, C., Chaffee, S. H., Flora, J. A., & Roser, C. (1998). Health campaign channels:
Tradeoffs among reach, specificity, and impact. Human Communication Research, 24,
410–432.
Selden, C. R., Zorn, M., Ratzan, S., & Parker, R. M. (2000). Health literacy, January 1990
through October 1999. Bethesda, MD: National Library of Medicine.
APPENDIX D
241
Siegel, M., & Doner, L. (1998). Marketing public health: Strategies to promote social change.
Gaithersburg, MD: Aspen.
Slater, M. D. (1996). Theory and method in health audience segmentation. Journal of Health
Communication, 1, 267–283.
Strecher, V. J., Kreuter, M. W., DenBoer, C. H., Kobrin, S. C., Hospers, H. J., & Skinner, C. S.
(1994). The effects of computer-tailored smoking cessation messages in family practice
settings. Journal of Family Practice, 39, 262–270.
Strecher, V. J., & Rosenstock, I. M. (1997). The health belief model. In K. Glanz, F. M. Lewis, &
B. K. Rimer (Eds.), Health behavior and health education: Theory, research, and practice (2nd
ed.). San Francisco: Jossey-Bass.
U.S. Department of Health and Human Services. (2000). Healthy people 2010 (2nd ed.; in two
volumes: Understanding and improving health and Objectives for improving health.).
Washington, DC: U.S. Government Printing Office.
University of Kansas. (2002). Community Toolbox, Community Workstation. Available at
http://ctb.lsi.ukans.edu/tools/CWS/socialmarketing/outline.htm.
University of Toronto. (1999). Overview of health communication campaigns. Toronto, Canada:
Health Communication Unit, Centre for Health Promotion, University of Toronto.
Wallach, L., & Dorfman, L. (1996). Media advocacy: A strategy for advancing policy and
promoting health. Health Education Quarterly, 23(3), 293–317.
Wallach, L., Dorfman, L., Jernigan, D., & Themba, M. (1993). Media advocacy and public
health: Power of prevention. Thousand Oaks, CA: Sage.
Wallach, L., Woodruff, K., Dorfman, L., & Diaz, I. (1999). News for a change: An advocate’s
guide to working with the media. Thousand Oaks, CA: Sage.
Weitzman, E. A., & Miles, M. B. (1995). Computer programs for qualitative data analysis: A
software sourcebook. Thousand Oaks, CA: Sage.
Wells, W. D. (Ed.). (1997). Measuring advertising effectiveness. Mahwah, NJ: Erlbaum.
Windsor, R. W., Baranowski, T. B., Clark, N. C., & Cutter, G. C. (1994). Evaluation of health
promotion, health education and disease prevention programs (2nd ed.). Mountain View,
CA: Mayfield.
242

APPENDIX D
243

GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
APPENDIX E
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide
GuideAPlanner’sGuideAPlanner’sGuideAPlanner’sGuide

Glossary
APPENDIX E

Attention. A pretesting measure used to describe a message’s ability to attract listener or
viewer attention; this is often measured as “recall” of a message or image.
Attitudes. An individual’s predispositions toward an issue, person, or group, which influence
his or her response to be positive or negative, favorable or unfavorable.
Baseline study. The collection and analysis of data regarding an intended audience or
situation prior to intervention.
Bounceback card. A short questionnaire, often on a business-reply postcard, that is
distributed with materials to collect process evaluation data.
Central-location intercept interviews. A method used for pretesting messages and
materials. It involves “intercepting” potential intended audience members at a highly trafficked
location (such as a shopping mall), asking them a few questions to see if they fit the intended
audience’s characteristics, showing them the messages or materials, and then administering a
questionnaire of predominantly closed-ended questions. Because respondents form a
convenience sample, the results cannot be projected to the population. Also called mall
intercept interviews.
Channel. The route of message delivery (e.g., mass media channels include television, radio,
newspapers, magazines; interpersonal channels include health professional to patient;
community channels include community events, such as health fairs or sporting events).
Closed-ended questions. Questions that provide respondents with a list of possible answers
from which to choose; also called multiple choice, forced-choice, or fixed-choice questions.
Communication concepts. See message concepts.
Communication objectives. The specific outcomes you expect exposure to your
communications will produce in support of the program’s overall goal.
Communication strategy. A statement that describes:
• The intended audience members
• The settings, channels, and activities that should be used to reach them
• The image that program communications should convey
• The action intended audience members should take as a result of exposure to
your communication
• A compelling benefit they will receive by taking the action
• Support that convinces them they will experience the benefit
Communication strategy statement. A written document containing the communication
strategy, which may be supplemented with additional information such as background on the
health problem, the goals the communication program is designed to help attain, or more
thorough intended audience profiles. This document provides the direction and consistency for
all program messages and materials.
246

Comprehension. A pretesting measure used to determine whether messages are
clearly understood.
Consumer panel. A research study in which the buying behavior and other characteristics
of a group of consumers are studied over time. Data can be collected through periodic
questionnaires, consumer diaries, UPC scanners, or a combination of techniques. Because
information is collected at multiple times, changes in behavior over time can be examined
and panel members can be recontacted and asked additional questions that are specific to
a particular health problem or communication effort. Consumer panel data are subject to the
same limitations of any panel study (e.g., sample possibly being misrepresentative due to
selection bias, difficulty in ensuring participation over time, and inability to control the
drop-out rate).
Convenience samples. Samples that consist of respondents who are typical of the intended
audience and who are easily accessible; results cannot be projected to the entire population
being studied.
Creative brief. A short (one- to two-page) version of the communication strategy statement,
used to guide development of materials and activities. The short creative brief is sometimes
used in place of the longer communication strategy statement, especially if the program is not
very complex.
Diagnostic information. The results of pretesting research that indicate the strengths and
weaknesses in messages and materials.
Education entertainment. A form of health communication in which educational content and
information is intentionally incorporated into an entertainment format (e.g., songs, comics,
nonnews television or radio programming, movies).
Environmental factors. Factors that are external to an individual but can influence the
individual’s behavior (e.g., policies, access to services, geography, physical features such as
sidewalks and parks).
Focus group. A qualitative research technique in which an experienced moderator guides
about 8 to 10 participants through a discussion of a selected topic, allowing them to talk freely
and spontaneously. Focus groups are often used to identify previously unknown issues or
concerns or to explore reactions to potential actions, benefits, or concepts during the planning
and development stages.
Formative evaluation. Evaluative research conducted during program development. May
include state-of-the art reviews, pretesting messages and materials, and pilot testing a
program on a small scale before full implementation.
Frequency. The average number of times an audience is exposed to a specific
media message.
Gatekeeper. An organization or individual you must work with before you can reach an
intended audience (e.g., an organization, a schoolteacher, a television public service director).
APPENDIX E
247

Geodemographic databases. Customized computer programs that combine many
variables—such as demographic, lifestyle, behavior, and geographic information—from
different surveys into one analysis.
Goal. The overall health improvement an organization or agency strives to create.
Health belief model. A conceptual framework of health behavior stating that health behavior is
a function of both knowledge and motivation. Specifically, the model emphasizes the role of
perceived vulnerability to a condition, perceived severity of the condition, perceived benefits of
the recommended action, perceived barriers to the advised action, cues to action, and self-
efficacy in terms of one’s ability to take action.
Impact evaluation. A type of research designed to identify whether and to what extent
a program contributed to accomplishing its stated goals (here, more global than
outcome evaluation).
In-depth interviews. A type of qualitative research in which a trained interviewer guides an
individual through a discussion of a selected topic, allowing the person to talk freely and
spontaneously. This technique is often used to identify previously unknown issues or concerns,
or to explore reactions to potential actions, benefits, or concepts during the planning and
development stages.
Intended audience. The audience selected for program messages and materials (see
segmentation). The primary intended audience consists of those individuals the program
is designed to affect. The secondary intended audience is the group (or groups) that can
help reach or influence the primary audience. (intended audience is also referred to as
“target audience.”)
Intended population. A broad definition of the audience for a program. The intended
population is defined by the epidemiology of the problem and factors contributing to it (e.g.,
women ages 40 and over for a mammography screening program).
Internet. A global network connecting millions of computers all over the world, allowing for the
exchange of information.
Low literacy. A limited ability to use printed and written information to function in society, to
achieve one’s goals, and to develop one’s knowledge and potential.
Media advocacy. The strategic use of mass media to reframe issues, shape public discussion,
or build support for a policy, point of view, or environmental change.
Media literacy. Having the skills to deconstruct media messages to identify the sponsor’s
motives and to construct or compose media messages representing the intended audience’s
point of view. This is often taught to youth so they can evaluate the media messages directed
toward them.
248

Message concepts. Brief statements, sometimes accompanied by visuals, that present key
aspects of the communication strategy (e.g., action to be taken, benefit promised in exchange,
support for the benefit) to the intended audience. Message concepts often differ in terms of the
type of appeal used; one may be factual, one may be emotional, and one may demonstrate the
action to be taken.
Objectives. See communication objectives.
Omnibus survey. A national survey conducted by a research organization that includes
questions on varied topics for various sponsoring organizations. This method of survey
research allows multiple organizations to add questions to construct one questionnaire,
reducing survey costs to participating organizations.
Open-ended questions. Questions that allow an individual to respond freely in his or her own
words, in contrast to closed-ended or fixed-choice questions.
Outcome evaluation. Research designed to assess the extent to which a program achieved
its objectives.
Over-recruiting. Recruiting more respondents than required to compensate for expected
“no-shows.”
Polysyllabic words. Words that contain three or more syllables.
Pretesting. A type of formative evaluation that involves systematically gathering intended
audience reactions to messages and materials before the messages and materials are
produced in final form.
Primary intended audience. See intended audience.
Probe. A technique used primarily in qualitative research (e.g., focus groups, in-depth
interviews) to solicit additional information about a question or issue. Probes should be neutral
(e.g., “What else can you tell me about _____?”), not directive (“Do you think the pamphlet was
suggesting that you take a particular step, such as changing your diet?”).
Process evaluation. Research conducted to document and study the functioning of different
components of program implementation; includes assessments of whether materials are being
distributed to the right people and in what quantities, whether and to what extent program
activities are occurring, and other measures of how and how well the program is working.
Program objectives. The specific outcomes that you expect your entire program to achieve.
These will be broader than communication objectives, but must also specify outcomes.
PSA. A public service announcement; an advertisement that a mass media outlet (e.g.,
magazine, newspaper, radio station, television station, Web site, outdoor venue) prints or
broadcasts without charging the sponsoring organization.
APPENDIX E
249

Public relations. Marketing activities designed to raise the public’s awareness about a
product, service, individual, or issue; management of an organization’s public image that helps
the public understand the organization and its products.
Qualitative research. Subjective research that involves obtaining reactions and impressions
from small numbers of people by engaging them in discussions. The information gathered
should not be described in numerical terms, and generalizations about the intended audience
cannot be made. Qualitative research is useful for exploring reactions and uncovering
additional ideas, issues, or concerns.
Quantitative research. Research designed to gather objective information by asking a large
number of people identical (and predominantly closed-ended) questions. Results are
expressed in numerical terms (e.g., 35 percent are aware of X and 65 percent are not), and,
if the respondents are a representative random sample, quantitative data can be used to
draw conclusions about the intended audience as a whole. Quantitative research is useful
for measuring the extent to which knowledge, attitudes, or behaviors are prevalent in an
intended audience.
Random sample. A sample of respondents selected from an intended population in which
every member of the population had an equal chance of being included.
Reach. The number of people or households exposed to a specific media message during a
specific period of time.
Readability testing. Using a formula to predict the approximate reading level (usually
expressed in grades) a person must have achieved in order to understand written material.
Recall. In pretesting, a measure that describes the extent to which respondents remember
seeing or hearing a message that was shown in a competitive media environment—usually
centers on recall of the main idea, not the verbatim message.
Search engine. A mechanism for finding Web sites or documents contained on Web sites.
To make sure others can find your site, you can register it with popular search engines (e.g.,
Yahoo!) by providing a description of your site and a few keywords.
Secondary intended audience. See intended audience.
Segmentation. Subdividing an overall population into homogeneous subsets in order to better
describe and understand a group, predict behavior, and tailor messages and programs to
match specific interests, needs, or other group characteristics. Segments may be demographic
(e.g., age, sex, education, life cycle), geographic (e.g., Southeastern U.S., rural, north side of
town), or psychographic (e.g., personality, lifestyle, usage patterns, risk factors, benefits
sought), or they may be based on a combination of these factors.
Self-administered questionnaires. Questionnaires that are filled out by respondents
themselves (rather than by an interviewer).
Settings. Times, places, and states of mind during which an intended audience is attentive
and open to a message and finds it credible.
250

Social cognitive theory. A theory of human behavior that stresses the dynamic
interrelationships among people, their behavior, and their environment. While the environment
shapes, maintains, and constrains behavior, people are not passive in the process; they can
create and change their environments. A basic premise of the theory is that people learn not
only through their own experiences but also by observing the actions of others and the results
of those actions. Social learning theory was the precursor to social cognitive theory.
Social marketing. The application and adaptation of commercial marketing concepts to the
planning, development, implementation, and evaluation of programs that are designed to bring
about behavior change to improve the welfare of individuals or their society. Social marketing
emphasizes thorough market research to identify and understand the intended audience and
what is preventing them from adopting a certain health behavior, and to then develop, monitor,
and constantly adjust a program to stimulate appropriate behavior change. Social marketing
programs can address any or all of the traditional marketing mix variables—product, price,
place, or promotion.
Stages-of-change model. A theoretical framework that explains behavior change as a
process rather than as an event. The model identifies individuals at various stages of readiness
to attempt, to make, and to sustain a behavior change. The stages are precontemplation,
contemplation, decision/determination, action, and maintenance.
Strategy. The overall approaches a program takes.
Tailored communication. Messages crafted for and delivered to each individual based on
individual needs, interests, and circumstances.
Target audience. See intended audience.
Web site. A location on the World Wide Web containing documents or files. Each site is owned
and managed by an individual, company, or organization.
World Wide Web. A part of the Internet designed to facilitate navigation of the network through
graphic user interfaces and hypertext links.
251
APPENDIX E
