
Recommendations and Reports / Vol. 65 / No. 3 July 29, 2016
U.S. Medical Eligibility Criteria
for Contraceptive Use, 2016
U.S. Department of Health and Human Services
Centers for Disease Control and Prevention
Morbidity and Mortality Weekly Report
Please note: An update has been published for this report. To view the update, please click here

Recommendations and Reports
Disclosure of Relationship
CDC, our planners, and our content experts wish to disclose
they have no financial interest or other relationships with
the manufacturers of commercial products, suppliers of
commercial services, or commercial supporters. Planners have
reviewed content to ensure there is no bias. This document will
not include any discussion of the unlabeled use of a product
or a product under investigational use, with the exception
that some of the recommendations in this document might
be inconsistent with package labeling.
The MMWR series of publications is published by the Center for Surveillance, Epidemiology, and Laboratory Services, Centers for Disease Control and Prevention (CDC),
U.S. Department of Health and Human Services, Atlanta, GA 30329-4027.
Suggested citation: [Author names; first three, then et al., if more than six.] [Title]. MMWR Recomm Rep 2016;65(No. RR-#):[inclusive page numbers].
Centers for Disease Control and Prevention
Thomas R. Frieden, MD, MPH, Director
Harold W. Jaffe, MD, MA, Associate Director for Science
Joanne Cono, MD, ScM, Director, Office of Science Quality
Chesley L. Richards, MD, MPH, Deputy Director for Public Health Scientific Services
Michael F. Iademarco, MD, MPH, Director, Center for Surveillance, Epidemiology, and Laboratory Services
MMWR Editorial and Production Staff (Serials)
Sonja A. Rasmussen, MD, MS, Editor-in-Chief
Charlotte K. Kent, PhD, MPH, Executive Editor
Christine G. Casey, MD, Editor
Teresa F. Rutledge, Managing Editor
David C. Johnson, Lead Technical Writer-Editor
Catherine B. Lansdowne, MS, Project Editor
Martha F. Boyd, Lead Visual Information Specialist
Maureen A. Leahy, Julia C. Martinroe,
Stephen R. Spriggs, Moua Yang, Tong Yang,
Visual Information Specialists
Quang M. Doan, MBA, Phyllis H. King, Terraye M. Starr,
Information Technology Specialists
MMWR Editorial Board
Timothy F. Jones, MD, Chairman
Matthew L. Boulton, MD, MPH
Virginia A. Caine, MD
Katherine Lyon Daniel, PhD
Jonathan E. Fielding, MD, MPH, MBA
David W. Fleming, MD
William E. Halperin, MD, DrPH, MPH
King K. Holmes, MD, PhD
Robin Ikeda, MD, MPH
Rima F. Khabbaz, MD
Phyllis Meadows, PhD, MSN, RN
Jewel Mullen, MD, MPH, MPA
Jeff Niederdeppe, PhD
Patricia Quinlisk, MD, MPH
Patrick L. Remington, MD, MPH
Carlos Roig, MS, MA
William L. Roper, MD, MPH
William Schaffner, MD
CONTENTS
Introduction ............................................................................................................1
Methods
....................................................................................................................2
How to Use This Document
...............................................................................3
Keeping Guidance Up to Date
.......................................................................... 5
References
................................................................................................................8
Abbreviations and Acronyms
............................................................................9
Appendix A: Summary of Changes from U.S. Medical Eligibility Criteria
for Contraceptive Use, 2010
...........................................................................10
Appendix B: Classifications for Intrauterine Devices
............................. 18
Appendix C: Classifications for Progestin-Only Contraceptives
........ 35
Appendix D: Classifications for Combined Hormonal Contraceptives
.... 55
Appendix E: Classifications for Barrier Methods
..................................... 81
Appendix F: Classifications for Fertility Awareness–Based Methods
..... 88
Appendix G: Lactational Amenorrhea Method
....................................... 90
Appendix H: Coitus Interruptus (Withdrawal)
......................................... 91
Appendix I: Female and Male Sterilization
................................................ 92
Appendix J: Classifications for Emergency Contraception
.................. 93
Appendix K: Summary of Classifications for Hormonal Contraceptive
Methods and Intrauterine Devices
............................................................ 96

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 1
US Department of Health and Human Services/Centers for Disease Control and Prevention
Introduction
Approximately 45% of all pregnancies that occur in the
United States are unintended (1), with associated increased
risks for adverse maternal and infant health outcomes (2) and
increased health care costs (3). Women, men, and couples
have increasing numbers of safe and effective choices for
contraceptive methods, including long-acting reversible
contraception methods such as intrauterine devices (IUDs)
and implants, to reduce the risk for an unintended pregnancy.
However, with these expanded options comes the need for
evidence-based guidance to help health care providers offer
quality family planning care to their patients, including
choosing the most appropriate contraceptive method for
individual circumstances and using that method correctly,
consistently, and continuously to maximize effectiveness.
In 2010, CDC published the first U.S. Medical Eligibility
Criteria for Contraceptive Use (U.S. MEC), which provided
recommendations on safe use of contraceptive methods
for women with various medical conditions and other
characteristics (and was adapted from global guidance
developed by the World Health Organization [WHO MEC])
(4,5). U.S. MEC is a companion document to the U.S. Selected
Practice Recommendations for Contraceptive Use (U.S. SPR),
which provides guidance on how to use contraceptive methods
safely and effectively once they are deemed to be medically
appropriate (6). WHO intended for the global guidance to
be used by local or national policy makers, family planning
program managers, and the scientific community as a reference
when they develop family planning guidance at the country
or program level. During 2008–2010, CDC participated in a
formal process to adapt the global guidance for appropriateness
Corresponding author: Kathryn M. Curtis, PhD, Division of
Reproductive Health, National Center for Chronic Disease Prevention
and Health Promotion, CDC. Telephone: 770-488-5200; E-mail:
U.S. Medical Eligibility Criteria for Contraceptive Use, 2016
Kathryn M. Curtis, PhD
1
Naomi K. Tepper, MD
1
Tara C. Jatlaoui, MD
1
Erin Berry-Bibee, MD
1,2
Leah G. Horton, MSPH
1
Lauren B. Zapata, PhD
1
Katharine B. Simmons, MD
1,2
H. Pamela Pagano, MPH
1
Denise J. Jamieson, MD
1
Maura K. Whiteman, PhD
1
1
Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC, Atlanta, Georgia
2
Department of Obstetrics and Gynecology, University of North Carolina School of Medicine, Chapel Hill, North Carolina
Summary
The 2016 U.S. Medical Eligibility Criteria for Contraceptive Use (U.S. MEC) comprises recommendations for the use of
specific contraceptive methods by women and men who have certain characteristics or medical conditions. These recommendations
for health care providers were updated by CDC after review of the scientific evidence and consultation with national experts who
met in Atlanta, Georgia, during August 26–28, 2015. The information in this report updates the 2010 U.S. MEC (CDC. U.S.
medical eligibility criteria for contraceptive use, 2010. MMWR 2010:59 [No. RR-4]). Notable updates include the addition
of recommendations for women with cystic fibrosis, women with multiple sclerosis, and women receiving certain psychotropic drugs
or St. John’s wort; revisions to the recommendations for emergency contraception, including the addition of ulipristal acetate; and
revisions to the recommendations for postpartum women; women who are breastfeeding; women with known dyslipidemias, migraine
headaches, superficial venous disease, gestational trophoblastic disease, sexually transmitted diseases, and human immunodeficiency
virus; and women who are receiving antiretroviral therapy. The recommendations in this report are intended to assist health care
providers when they counsel women, men, and couples about contraceptive method choice. Although these recommendations are
meant to serve as a source of clinical guidance, health care providers should always consider the individual clinical circumstances
of each person seeking family planning services. This report is not intended to be a substitute for professional medical advice for
individual patients. Persons should seek advice from their health care providers when considering family planning options.
Recommendations and Reports
2 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
for use in the United States, which included rigorous
identification and critical appraisal of the scientific evidence
through systematic reviews, and input from national experts
on how to translate that evidence into recommendations for
U.S. health care providers (5). At that time, CDC committed
to keeping this guidance up to date and based on the best
available evidence, with full review every few years (5).
This document updates CDC’s U.S. MEC 2010 (5), based
on new evidence and input from experts. A summary of
changes from U.S. MEC 2010 is provided (Appendix A).
Notable updates include the following:
• addition of recommendations for women with cystic
fibrosis, women with multiple sclerosis, and women
receiving certain psychotropic drugs or St. John’s wort
• revisions to the recommendations for emergency
contraception, including the addition of ulipristal acetate
• revisions to the recommendations for postpartum women;
women who are breastfeeding; women with known
dyslipidemias, migraine headaches, superficial venous
disease, gestational trophoblastic disease, sexually transmitted
diseases (STDs), and human immunodeficiency virus
(HIV); and women who are receiving antiretroviral therapy
The goal of these recommendations is to remove unnecessary
medical barriers to accessing and using contraception, thereby
decreasing the number of unintended pregnancies. These
recommendations are meant to serve as a source of clinical
guidance for health care providers; health care providers should
always consider the individual clinical circumstances of each
person seeking family planning services. This report is not
intended to be a substitute for professional medical advice for
individual patients, who should seek advice from their health
care providers when considering family planning options.
Methods
Since publication of U.S. MEC 2010, CDC has monitored
the literature for new evidence relevant to the recommendations
through the WHO/CDC continuous identification of research
evidence (CIRE) system. This system identifies new evidence
as it is published and allows WHO and CDC to update
systematic reviews and facilitate updates to recommendations
as new evidence warrants. Automated searches are run in
PubMed weekly, and the results are reviewed. Abstracts that
meet specific criteria are added to the web-based CIRE system,
which facilitates coordination and peer review of systematic
reviews for both WHO and CDC (7). In 2014, CDC reviewed
all of the existing recommendations in U.S. MEC 2010 for
new evidence identified by CIRE that had the potential to
lead to a changed recommendation. During August 27–28,
2014, CDC held a meeting in Atlanta, Georgia, of 11
family planning experts and representatives from partner
organizations to solicit their input on the scope of and process
for updating both U.S. MEC 2010 and U.S. SPR 2013. The
participants were experts in family planning and represented
various types of health care providers, as well as health care
provider organizations. A list of participants is provided
at the end of this report. Meeting participants discussed
topics to be addressed in the update of U.S. MEC based on
new evidence published since 2010 (identified through the
CIRE system), topics addressed at a 2014 WHO meeting to
update global guidance, and suggestions CDC received from
health care providers for the addition of recommendations
for women with medical conditions not yet included in
U.S. MEC (e.g., from provider feedback through e-mail,
public inquiry, and questions received at conferences). CDC
identified several topics to consider when updating the
guidance, including revision of existing recommendations for
certain medical conditions or characteristics (breastfeeding,
postpartum, HIV, receiving antiretroviral therapy, obesity,
dyslipidemia, increased risk for STDs, superficial venous
thrombosis, gestational trophoblastic disease, and migraine
headaches), addition of recommendations for new medical
conditions (cystic fibrosis, multiple sclerosis, use of certain
psychotropic drugs, and St. John’s wort), and addition of
recommendations for new contraceptive methods (ulipristal
acetate for emergency contraception). CDC determined that
all other recommendations in U.S. MEC 2010 were up to
date and consistent with the existing body of evidence for
that recommendation.
In preparation for a subsequent expert meeting held during
August 26–28, 2015, to review the scientific evidence for
potential recommendations, CDC staff members and other
invited authors listed at the end of this report conducted
independent systematic reviews for each of the topics being
considered. The purpose of these systematic reviews was to
identify direct evidence about the safety of contraceptive
method use by women with selected conditions (e.g., risk for
disease progression or other adverse health effects in women with
multiple sclerosis who use combined hormonal contraceptives
[CHCs]). Preferred Reporting Items for Systematic Reviews
and Meta-Analyses (PRISMA) guidelines were followed for
reporting systematic reviews (8,9), and strength and quality
of the evidence were assigned using the system of the U.S.
Preventive Services Task Force (10). When direct evidence
was limited or not available, indirect evidence (e.g., evidence
on surrogate outcomes or among healthy women) and
theoretical issues were considered and either added to direct
evidence within a systematic review or separately compiled for
presentation to the meeting participants. Completed systematic

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
reviews were peer reviewed by two or three experts and then
provided to participants before the expert meeting. Reviews
are referenced and cited throughout this document; the full
reviews appear in the published literature and contain the
details of each review, including the systematic review question,
literature search protocol, inclusion and exclusion criteria,
evidence tables, and quality assessments. CDC staff continued
to monitor new evidence identified through the CIRE system
during the preparation for the August 2015 meeting.
During August 26–28, 2015, in Atlanta, Georgia, CDC
held a meeting with 44 participants who were invited to
provide their individual perspectives on the scientific evidence
presented and potential recommendations. Twenty-nine of the
participants represented a wide range of expertise in family
planning provision and research, and included obstetricians/
gynecologists, pediatricians, family physicians, nurse
practitioners, epidemiologists, and others with research and
clinical practice expertise in contraceptive safety, effectiveness,
and management; these individuals participated in the entire
meeting. Fifteen participants with expertise relevant to
specific topics on the meeting agenda provided information
and participated in the discussion (e.g., an expert in cystic
fibrosis was asked to provide general information about the
condition and to assist in interpreting the evidence and any
theoretical concerns on the use of contraceptive methods in
women with the condition); these participants provided input
only during the session for which their topics were discussed.
Lists of participants and any potential conflicts of interest
are provided at the end of this report. During the meeting,
the evidence from the systematic review for each topic was
presented, including direct evidence and any indirect evidence
or theoretical concerns. Participants provided their perspectives
on using the evidence to develop recommendations that would
meet the needs of U.S. health care providers. After the meeting,
CDC determined the recommendations in this report, taking
into consideration the perspectives provided by the meeting
participants. Feedback also was received from three external
reviewers, composed of health care providers and researchers
who had not participated in the update meetings. These
reviewers were asked to provide comments on the accuracy,
feasibility, and clarity of the recommendations. Areas of
research that need additional investigation also were considered
during the meeting (11).
How to Use This Document
These recommendations are intended to help health care
providers determine the safe use of contraceptive methods
among women and men with various characteristics and
medical conditions. Providers also can use the information in
these recommendations when consulting with women, men,
and couples about their selection of contraceptive methods. The
tables in this document include recommendations for the use
of contraceptive methods by women and men with particular
characteristics or medical conditions. Each condition is defined
as representing either an individual’s characteristics (e.g., age
or history of pregnancy) or a known preexisting medical or
pathologic condition (e.g., diabetes or hypertension). The
recommendations refer to contraceptive methods being used
for contraceptive purposes; the recommendations do not
consider the use of contraceptive methods for treatment of
medical conditions because the eligibility criteria in these
situations might differ. The conditions affecting eligibility for
the use of each contraceptive method are classified into one of
four categories (Box 1).
Using the Categories in Practice
Health care providers can use the eligibility categories when
assessing the safety of contraceptive method use for women
and men with specific medical conditions or characteristics.
Category 1 comprises conditions for which no restrictions
exist for use of the contraceptive method. Classification
of a method/condition as category 2 indicates the method
generally can be used, although careful follow-up might be
required. For a method/condition classified as category 3,
use of that method usually is not recommended unless other
more appropriate methods are not available or acceptable. The
severity of the condition and the availability, practicality, and
acceptability of alternative methods should be considered,
and careful follow-up is required. Hence, provision of a
contraceptive method to a woman with a condition classified
as category 3 requires careful clinical judgement and access to
clinical services. Category 4 comprises conditions that represent
an unacceptable health risk if the method is used. For example,
a smoker aged <35 years generally can use combined oral
contraceptives (COCs) (category 2). However, for a woman
BOX 1. Categories of medical eligibility criteria for contraceptive use
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven
risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.
Recommendations and Reports
4 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
aged ≥35 years who smokes <15 cigarettes per day, the use
of COCs usually is not recommended unless other methods
are not available or acceptable to her (category 3). A woman
aged ≥35 years who smokes ≥15 cigarettes per day should not
use COCs because of unacceptable health risks, primarily the
risk for myocardial infarction and stroke (category 4). The
programmatic implications of these categories might depend
on the circumstances of particular professional or service
organizations. For example, in some settings, a category 3
might mean that a special consultation is warranted.
The recommendations address medical eligibility criteria for
the initiation and continued use of all methods evaluated. The
issue of continuation criteria is clinically relevant whenever
a medical condition develops or worsens during use of a
contraceptive method. When the categories differ for initiation
and continuation, these differences are noted in the Initiation
and Continuation columns. When initiation and continuation
are not indicated, the category is the same for initiation and
continuation of use.
On the basis of this classification system, the eligibility criteria
for initiating and continuing use of a specific contraceptive
method are presented in tables (Appendices A–K). In these
tables, the first column indicates the condition. Several
conditions are divided into subconditions to differentiate
between varying types or severity of the condition. The second
column classifies the condition for initiation or continuation
(or both) into category 1, 2, 3, or 4. For certain conditions,
the numeric classification does not adequately capture the
recommendation; in these cases, the third column clarifies the
numeric category. These clarifications were determined during
the discussions of the scientific evidence and are considered a
necessary element of the recommendation. The third column
also summarizes the evidence for the recommendation if
evidence exists. The recommendations for which no evidence
is cited are based on expert opinion from either the WHO or
U.S. expert meeting in which these recommendations were
developed, and might be based on evidence from sources
other than systematic reviews. For certain recommendations,
additional comments appear in the third column and generally
come from the WHO meeting or the U.S. meeting.
Recommendations for Use of
Contraceptive Methods
The classifications for whether women with certain medical
conditions or characteristics can use specific contraceptive
methods are provided for intrauterine contraception, including
the copper-containing IUD and levonorgestrel-releasing IUDs
(Appendix B); progestin-only contraceptives (POCs), including
etonogestrel implants, depot medroxyprogesterone acetate
injections, and progestin-only pills (Appendix C); CHCs,
including low-dose (containing ≤35 µg ethinyl estradiol)
COCs, combined hormonal patch, and combined vaginal
ring (Appendix D); barrier contraceptive methods, including
male and female condoms, spermicides, diaphragm with
spermicide, and cervical cap (Appendix E); fertility awareness–
based methods (Appendix F); lactational amenorrhea method
(Appendix G); coitus interruptus (Appendix H); female and
male sterilization (Appendix I); and emergency contraception,
including emergency use of the copper-containing IUD and
emergency contraceptive pills (Appendix J). A table at the end
of this report summarizes the classifications for the hormonal
and intrauterine methods (Appendix K).
Contraceptive Method Choice
Many elements need to be considered by women, men, or
couples at any given point in their lifetimes when choosing
the most appropriate contraceptive method. These elements
include safety, effectiveness, availability (including accessibility
and affordability), and acceptability. The guidance in this
report focuses primarily on the safety of a given contraceptive
method for a person with a particular characteristic or medical
condition. Therefore, the classification of category 1 means
that the method can be used in that circumstance with no
restrictions with regard to safety but does not necessarily imply
that the method is the best choice for that person; other factors,
such as effectiveness, availability, and acceptability, might
play an important role in determining the most appropriate
choice. Voluntary informed choice of contraceptive methods
is an essential guiding principle, and contraceptive counseling,
when applicable, might be an important contributor to the
successful use of contraceptive methods.
In choosing a method of contraception, dual protection from
the simultaneous risk for HIV and other STDs also should be
considered. Although hormonal contraceptives and IUDs are
highly effective at preventing pregnancy, they do not protect
against STDs, including HIV. Consistent and correct use of the
male latex condom reduces the risk for HIV infection and other
STDs, including chlamydial infection, gonococcal infection,
and trichomoniasis (12). Although evidence is limited, use
of female condoms can provide protection from acquisition
and transmission of STDs (12). All patients, regardless of
contraceptive choice, should be counseled about the use of
condoms and the risk for STDs, including HIV infection (12).
Additional information about prevention and treatment of
STDs is available from the CDC Sexually Transmitted Diseases
Treatment Guidelines (http://www.cdc.gov/std/treatment) (12).

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 5
US Department of Health and Human Services/Centers for Disease Control and Prevention
Contraceptive Method Effectiveness
Contraceptive method effectiveness is critical for minimizing
the risk for an unintended pregnancy, particularly among women
for whom an unintended pregnancy would pose additional
health risks. The effectiveness of contraceptive methods depends
both on the inherent effectiveness of the method itself and on
how consistently and correctly it is used (Figure). Methods
that depend on consistent and correct use have a wide range of
effectiveness. IUDs and implants are considered long-acting,
reversible contraception (LARC); these methods are highly
effective because they do not depend on regular compliance
from the user. LARC methods are appropriate for most women,
including adolescents and nulliparous women. All women
should be counseled about the full range and effectiveness of
contraceptive options for which they are medically eligible so
that they can identify the optimal method.
Unintended Pregnancy and Increased
Health Risk
For women with conditions that might make pregnancy
an unacceptable health risk, long-acting, highly effective
contraceptive methods might be the best choice to avoid
unintended pregnancy (Figure). Women with these conditions
should be advised that sole use of barrier methods for
contraception and behavior-based methods of contraception
might not be the most appropriate choice because of their
relatively higher typical-use rates of failure (Figure). Conditions
included in U.S. MEC that are associated with increased
risk for adverse health events as a result of pregnancy are
identified throughout the document (Box 2). Some of the
medical conditions included in U.S. MEC recommendations
are treated with teratogenic drugs. While the woman’s
medical condition may not affect her eligibility to use certain
contraceptive methods, women using teratogenic drugs are
at increased risk for poor pregnancy outcomes; long-acting,
highly effective contraceptive methods might be the best
option to avoid unintended pregnancy or delay pregnancy
until teratogenic drugs are no longer needed.
Keeping Guidance Up to Date
Updating the evidence-based recommendations as new
scientific evidence becomes available is a challenge. CDC
will continue to work with WHO to identify and assess new
relevant evidence as it becomes available and to determine
whether changes in the recommendations are warranted (7).
In most cases, U.S. MEC follows the WHO guidance updates,
which typically occur every 5 years (or sooner if warranted
by new data). However, CDC will review all WHO updates
for their application in the United States. CDC also will
identify and assess any new literature for the recommendations
and medical conditions that are not included in the WHO
guidance. CDC will completely review U.S. MEC every 5 years
as well. Updates to the guidance will appear on the CDC
U.S. MEC website (http://www.cdc.gov/reproductivehealth/
UnintendedPregnancy/USMEC.htm).
Acknowledgments
This report is based, in part, on the work of the Promoting Family
Planning Team, Department of Reproductive Health and Research,
World Health Organization, and its development of Medical
Eligibility Criteria for Contraceptive Use, 5th edition.
BOX 2. Conditions associated with increased risk for adverse health
events as a result of pregnancy*
Breast cancer
Complicated valvular heart disease
Cystic fibrosis
Diabetes: insulin dependent; with nephropathy,
retinopathy, or neuropathy or other vascular disease;
or of >20 years’ duration
Endometrial or ovarian cancer
Epilepsy
Hypertension (systolic ≥160 mm Hg or diastolic
≥100 mm Hg)
History of bariatric surgery within the past 2 years
HIV: not clinically well or not receiving antiretroviral therapy
Ischemic heart disease
Gestational trophoblastic disease
Hepatocellular adenoma and malignant liver
tumors (hepatoma)
Peripartum cardiomyopathy
Schistosomiasis with fibrosis of the liver
Severe (decompensated) cirrhosis
Sickle cell disease
Solid organ transplantation within the past 2 years
Stroke
Systemic lupus erythematosus
Thrombogenic mutations
Tuberculosis
* Long-acting, highly effective contraceptive methods might be the best
choice for women with conditions that are associated with increased risk
for adverse health events as a result of pregnancy. These women should
be advised that sole use of barrier methods for contraception and behavior-
based methods of contraception might not be the most appropriate choice
because of their relatively higher typical-use rates of failure.

Recommendations and Reports
6 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
FIGURE. Effectiveness of family planning methods*
SUN MON TUES WED THUR FRI SAT
1
2
3
4
1
2 3
4 5 6 7
8
9 10
11
12 13
14
15
16 17
18
19 20
21
22
23
24
29
30
31
25 26
27
28
1
2 3
4
JANUARY
Spermicide
Reversible Permanent
Male Sterilization Female Sterilization
Implant
Intrauterine Device
Injectable
Pill Patch Ring
Diaphragm
Male Condom Female Condom Withdrawal
Sponge
Fertility-Awareness
Based Methods
Spermicide
How to make your method
most eective
Vasectomy and
hysteroscopic sterilization:
After procedure, little or
nothing to do or remember.
Use another method for
rst 3 months.
Injectable: Get repeat
injections on time.
Pills: Take a pill each day.
Patch, Ring: Keep in place,
change on time.
Diaphragm: Use correctly
every time you have sex.
Condoms, sponge,
withdrawal, spermicides:
Use correctly every time
you have sex.
Fertility awareness-based
methods: Abstain or
use condoms on fertile
days. Newest methods
(Standard Days Method
and TwoDay Method)
may be the easiest to use
and consequently more
eective.
0.05 % LNG - 0.2 % Copper T - 0.8 % 0.15 % 0.5 %
(IUD)
(Vasectomy) (Abdominal, Laparoscopic, Hysteroscopic)
6 %
9 %
9 %
9 %
12 %
18 % 21 % 22 %
24 % 28 %
24 % parous women
12 % nulliparous women
Least
Eective
Most
Eective
Less than 1 pregnancy
6-12 pregnancies per
100 women in a year
per 100 women in a year
18 or more pregnancies
per 100 women in a year
CONDOMS SHOULD ALWAYS BE USED TO REDUCE THE RISK OF SEXUALLY TRANSMITTED INFECTIONS.
Other Methods of Contraception
Lactational Amenorrhea Method: LAM is a highly eective, temporary method of contraception.
Emergency Contraception: Emergency contraceptive pills or a copper IUD after unprotected intercourse substantially reduces risk of pregnancy.
[
[
]
Sources: Adapted from World Health Organization (WHO) Department of Reproductive Health and Research, Johns Hopkins Bloomberg School of Public Health/
Center for Communication Programs (CCP). Knowledge for health project. Family planning: a global handbook for providers (2011 update). Baltimore, MD; Geneva,
Switzerland: CCP and WHO; 2011; and Trussell J. Contraceptive failure in the United States. Contraception 2011;83:397–404.
* The percentages indicate the number out of every 100 women who experienced an unintended pregnancy within the first year of typical use of each contraceptive method.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 7
US Department of Health and Human Services/Centers for Disease Control and Prevention
U.S. Medical Eligibility Criteria for
Contraceptive Use Participants
CDC Guideline Development Group for U.S. Medical Eligibility
Criteria for Contraceptive Use and U.S. Selected Practice
Recommendations for Contraceptive Use
Kathryn M. Curtis, PhD (Chair), Erin Berry-Bibee, MD,
Suzanne G. Folger, PhD, Leah G. Horton, MSPH, Denise J.
Jamieson, MD, Tara C. Jatlaoui, MD, Polly A. Marchbanks, PhD, H.
Pamela Pagano, MPH, Halley E.M. Riley, MPH, Mirelys Rodriguez,
Katharine B. Simmons, MD, Naomi K. Tepper, MD, Maura K.
Whiteman, PhD, Lauren B. Zapata, PhD, CDC, Atlanta, Georgia.
Invited Meeting Participants, August 27–28, 2014, Atlanta, Georgia
Herbert Peterson, MD, University of North Carolina, Chapel
Hill, North Carolina (Chair); Gale Burstein, MD, Erie County
Department of Health, Buffalo, New York; Alison Edelman, MD,
Oregon Health and Science University, Portland, Oregon; Eve Espey,
MD, University of New Mexico, Albuquerque, New Mexico; Emily
Godfrey, MD, University of Washington, Seattle, Washington;
Andrew Kaunitz, MD, University of Florida, Jacksonville, Florida;
Susan Moskosky, MS, U.S. Department of Health and Human
Services, Rockville, Maryland; Kavita Nanda, MD, FHI360 and
American College of Obstetricians and Gynecologists, Durham,
North Carolina; Deborah Nucatola, MD, Planned Parenthood
Federation of America, New York, New York; Michael Policar, MD,
University of California, San Francisco, California; Carolyn Westhoff,
MD, Columbia University, New York, New York.
Systematic Review Presenters and Authors, Meeting, August 26–28,
2015, Atlanta, Georgia
Erin Berry-Bibee, MD, Kathryn M. Curtis, PhD, Leah G. Horton,
MSPH, Denise J. Jamieson, MD, Tara C. Jatlaoui, MD, Polly A.
Marchbanks PhD, Titilope Oduyebo, MD, Pamela Pagano, MPH,
Halley E.M. Riley, MPH, Katharine B. Simmons, MD, Naomi K.
Tepper, MD, Maura K. Whiteman, PhD, Lauren B. Zapata, PhD,
CDC, Atlanta, Georgia; Monica Dragoman, MD, Mary E. Gaffield,
PhD, Sharon J. Phillips, MD, Marleen Temmerman, MD, World Health
Organization, Geneva, Switzerland; Andra James, MD, Duke University
Medical Center, Durham, North Carolina; Nathalie Kapp, MD, HRA
Pharma, Paris, France; Kavita Nanda, MD, FHI360, Durham, North
Carolina; Seth Walker, MD, Emory University, Atlanta, Georgia.
Invited Meeting Participants, August 26–28, 2015, Atlanta, Georgia
Herbert Peterson, MD, University of North Carolina, Chapel
Hill, North Carolina (Chair); Rebecca Allen, MD, American Society
for Reproductive Medicine and Women and Infants Hospital,
Providence, Rhode Island; Jean Anderson, MD, Johns Hopkins
University, Baltimore, Maryland; Abbey Berenson, MD, University
of Texas Medical Branch, Galveston, Texas; Amanda Black, MD,
University of Ottawa, Ontario, Canada; Cora Collette Breuner, MD,
American Academy of Pediatrics and Seattle Children’s Hospital,
Seattle, Washington; Gale Burstein MD, Erie County Department
of Health, Buffalo, New York; Anne Calhoun, MD, University of
North Carolina, Chapel Hill, North Carolina; Nahida Chakhtoura,
MD, National Institutes of Health, Rockville, Maryland; Alicia
Christy, MD, National Institutes of Health, Rockville, Maryland;
Mitchell D. Creinin, MD, University of California, Davis, California;
Linda Dominguez, Southwest Women’s Health, Albuquerque,
New Mexico; Alison Edelman, MD, Oregon Health and Science
University, Portland, Oregon; Eve Espey, MD, University of
New Mexico, Albuquerque, New Mexico; Emily Godfrey, MD,
University of Washington, Seattle, Washington; Marji Gold, MD,
Albert Einstein College of Medicine, Bronx, New York; Donald
Goldstein, MD, Harvard Medical School, Boston, Massachusetts;
Robert Hatcher, MD, Emory University, Atlanta, Georgia; Mark
Hathaway, MD, JHPIEGO and Unity Healthcare, Washington,
DC; Stephen Heartwell, MD, Susan Thompson Buffett Foundation,
Omaha, Nebraska; Paula Hillard, MD, Stanford University, Palo
Alto, California; Maria Houtchens, MD, Harvard Medical School,
Boston, Massachusetts; Andra James, MD, Duke University Medical
Center, Durham, North Carolina; Andrew Kaunitz, MD, University
of Florida, Jacksonville, Florida; Myong-Jin Kim, Pharm-D, Food
and Drug Administration, Rockville, Maryland; Barbara Konkle,
MD, Bloodworks Northwest, Seattle, Washington; Tobias Kurth,
MD, INSERM, Bordeaux, France; Miriam Labbok, MD, Academy
of Breastfeeding Medicine and University of North Carolina, Chapel
Hill, North Carolina; Reagan McDonald-Mosley, MD, Planned
Parenthood Federation of America, New York, New York; Joan
Meek, MD, American Academy of Pediatrics and Florida State
University College of Medicine, Orlando, Florida; Mark Mirochnick,
MD, Boston University, Boston, Massachusetts; Susan Moskosky,
MS, U.S. Department of Health and Human Services, Rockville,
Maryland; Kavita Nanda, MD, FHI360, Durham, North Carolina;
Jeffrey Peipert, MD, Washington University, St. Louis, Missouri;
Michael Policar, MD, University of California, San Francisco,
California; Sarah Prager, MD, University of Washington, Seattle
Washington; David Soper, MD, Medical University of South
Carolina, Charleston, South Carolina; Lisa Soule, MD, Food and
Drug Administration, Rockville, Maryland; Alison Stuebe, MD,
American College of Obstetricians and Gynecologist and University
of North Carolina, Chapel Hill, North Carolina; James Trussell,
PhD, Princeton University, Princeton, New Jersey; Seth Walker, MD,
Emory University, Atlanta, Georgia; Nanette Wenger, MD, Emory
University, Atlanta, Georgia; Carolyn Westhoff, MD, Columbia
University, New York, New York; Christopher Zahn, MD, American
College of Obstetricians and Gynecologists, Washington, DC.
CDC Attendees
Wanda D. Barfield, MD, Peter Briss, MD, W. Craig Hooper, PhD,
Jill Huppert, MD, Caroline King, PhD, Michele Mandel, Titilope
Oduyebo, MD, Cria Perrine, MD, Sam Posner, PhD.
External Reviewers
Abigail R.A. Aiken, PhD, Princeton University, Princeton, New
Jersey; Linda Burdette, PA-C, Premier Women’s Health of Yakima,
Yakima, Washington; Mimi Zieman, MD, Planned Parenthood
Southeast, Atlanta, Georgia.
Recommendations and Reports
8 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Conflicts of Interest for Invited Meeting Participants,
August 26–28, 2015, Atlanta, Georgia
Rebecca Allen, Nexplanon trainer for Merck and Liletta trainer for
Actavis, consultant, advisory board and education grant from Bayer;
Mitchell D. Creinin, Nexplanon trainer for Merck, litigation consultant
for Bayer, advisory board for Merck and Teva Pharmaceutical Industries,
Ltd., consultant for Lemonaid – PolkaDoc app, research support
to University of California, Davis from Medicines360, Contramed,
Merck, Eunice Kennedy Shriver National Institute of Child Health
and Human Development, and Society of Family Planning; Linda
Dominguez, speaker for Bayer, Merck, and Actavis; Alison Edelman,
royalties from Up to Date, Inc., consultant for Genzyme, grant support
from the National Institutes of Health and the Gates Foundation,
travel funds from the World Health Organization, grant support and
honorarium from Society of Family Planning, honorarium and travel
funds from Contemporary Forum, trainer for Merck, consultant
for Gynuity Health Projects, honorarium from CDC, Projects In
Knowledge, and American Congress of Obstetricians and Gynecologists,
advisory board for Agile Therapeutics; Eve Espey, travel funds from
the American Congress of Obstetricians and Gynecologists, Society
for Family Planning, and U.S. Food and Drug Administration,
Reproductive and Drug Advisory Committee for U.S. Food and Drug
Administration, travel funds and honoraria from Wayne State University,
Telluride Conference, New Mexico Department of Health Clinician
Conference, Planned Parenthood National Medical Conference and
Society of Family Planning, British Columbia Contraception Access
Research Team Conference, and American Congress of Obstetricians
and Gynecologists annual meeting; Emily Godfrey, research funding
from Bayer Women’s Health, Prima-Temp, and Teva Pharmaceutical
Industries, Ltd., trainer for Merck and Upstream USA, grant reviewer
for Fellowship of Family Planning and Society of Family Planning
Research Fund; Mark Hathaway, Liletta trainer and speaker for Actavis
and Medicines360, Nexplanon trainer for Merck, advisory board for
Contramed and Afaxys Pharmaceuticals; Paula Hillard, consultant for
American Civil Liberties Union, Advanced Health Media, CMEology,
National Sleep Foundation, and Planned Parenthood Federation of
America, honoraria from National Sleep Foundation, Dignity Health,
CMEology, Advance Health Media, and Medscape, editorial board for
Advanstar–Contemporary OB/GYN, board examiner for the American
Board of Obstetrics and Gynecology, contract reviewer for the U.S.
Department of Health and Human Services, editorial board for EBSCO–
PEMSoft, Nexplanon trainer for Merck, scientific advisor to Proctor and
Gamble, publication royalties from Wiley Blackwell Publishing; Andrew
Kaunitz, advisory board participant of Allergan, Bayer, Merck, and Pfizer,
clinical trial funding to University of Florida from Agile Therapeutics,
Bayer, Merck; Mark Mirochnick, data and safety monitoring board for
Merck and ViiV Healthcare, advisory board for Merck; Jeffrey Peipert,
research funding from Bayer and Teva Pharmaceutical Industries, Ltd.,
advisory board for Perrigo; Michael Policar, litigation consultant for
Bayer; James Trussell, advisory board for Merck and Teva Pharmaceutical
Industries, Ltd., consultant for Bayer; Nanette Wenger, research grants
from Alnylam Pharmaceuticals, Gilead Sciences, National Heart, Lung,
and Blood Institute, Pfizer, and Society for Women’s Health Research,
consultant for Amgen, AstraZeneca, Gilead Sciences and Merck;
Carolyn Westhoff, data and safety monitoring board for Merck and
Bayer, advisory board for Agile Therapeutics, MicroChips Biotech, and
Actavis, research support to Columbia University from Medicines360,
León Farma, and ContraMed.
Handling Conflicts of Interest
To promote transparency, all participants were asked to disclose any
potential conflicts of interest to CDC prior to the expert meeting and
to report any potential conflicts of interest during the introductory
portion of the expert meeting. All potential conflicts of interest are
listed above. No participants were excluded from discussion based
on potential conflicts of interest. CDC staff who ultimately decided
and developed these recommendations have no financial interests or
other relationships with the manufacturers of commercial products,
suppliers of commercial services, or commercial supporters relevant
to these recommendations.
References
1. Finer LB, Zolna MR. Declines in unintended pregnancy in the United
States, 2008–2011. N Engl J Med 2016;374:843–52.http://dx.doi.
org/10.1056/NEJMsa1506575
2. Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy
on infant, child, and parental health: a review of the literature. Stud Fam Plann
2008;39:18–38. http://dx.doi.org/10.1111/j.1728-4465.2008.00148.x
3. Sonfield A, Kost K. Public costs from unintended pregnancies and the role
of public insurance programs in paying for pregnancy-related care: national
and state estimates for 2010. New York: Guttmacher Institute; 2015.
4. World Health Organization. Medical eligibility criteria for contraceptive
use. 4th ed. Geneva, Switzerland: World Health Organization; 2009.
5. CDC. U.S. medical eligibility criteria for contraceptive use, 2010.
MMWR Recomm Rep 2010;59(No. RR-4).
6. Curtis KM, Jatlaoui TC, Tepper NK, et al. U.S. selected practice
recommendations for contraceptive use, 2016. MMWR Recomm Rep
2016;65(No. RR-4).
7. Mohllajee AP, Curtis KM, Flanagan RG, Rinehart W, Gaffield ML,
Peterson HB. Keeping up with evidence a new system for WHO’s
evidence-based family planning guidance. Am J Prev Med 2005;28:483–
90.http://dx.doi.org/10.1016/j.amepre.2005.02.008
8. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for
reporting systematic reviews and meta-analyses of studies that evaluate
health care interventions: explanation and elaboration. J Clin Epidemiol
2009;62:e1–34. http://dx.doi.org/10.1016/j.jclinepi.2009.06.006
9. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred
reporting items for systematic reviews and meta-analyses: the PRISMA
statement. Int J Surg 2010;8:336–41. http://dx.doi.org/10.1016/j.
ijsu.2010.02.007
10. Harris RP, Helfand M, Woolf SH, et al; Methods Work Group, Third US
Preventive Services Task Force. Current methods of the US Preventive Services
Task Force: a review of the process. Am J Prev Med 2001;20(Suppl):21–35.
http://dx.doi.org/10.1016/S0749-3797(01)00261-6
11. Horton L, Folger SG, Berry-Bibee E, Jatlaoui TC, Tepper NK, Curtis KM.
Research gaps from evidence-based contraception guidance: the U.S. Medical
Eligibility Criteria for Contraceptive Use, 2016, and the U.S. Selected Practice
Recommendations for Contraceptive Use, 2016. Contraception. In press 2016.
12. Workowski KA, Bolan GA. Sexually transmitted diseases treatment
guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-3).
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 9
US Department of Health and Human Services/Centers for Disease Control and Prevention
Abbreviations and Acronyms
ARV = antiretroviral [therapy]
BMD = bone mineral density
BMI = body mass index
CHC = combined hormonal contraceptive
COC = combined oral contraceptive
Cu-IUD = copper-containing intrauterine device
DMPA = depot medroxyprogesterone acetate
DVT = deep venous thrombosis
ECP = emergency contraceptive pills
FAB = fertility awareness–based [methods]
hCG = human chorionic gonadotropin
HDL = high-density lipoprotein
HIV = human immunodeficiency virus
IBD = inflammatory bowel disease
IUD = intrauterine device
LARC = long-acting reversible contraception
LDL = low-density lipoprotein
LNG = levonorgestrel
LNG-IUD = levonorgestrel-releasing intrauterine device
NET-EN = norethisterone enantate
NNRTI = nonnucleoside reverse transcriptase inhibitor
NRTI = nucleoside reverse transcriptase inhibitor
PE = pulmonary embolism
PID = pelvic inflammatory disease
POC = progestin-only contraceptive
POP = progestin-only pill
SLE = systemic lupus erythematosus
SSRI = selective serotonin reuptake inhibitors
STD = sexually transmitted disease
UPA = ulipristal acetate
U.S. MEC = U.S. Medical Eligibility Criteria for Contraceptive Use
U.S. SPR = U.S. Selected Practice Recommendations for Contraceptive Use
VTE = venous thromboembolism

Recommendations and Reports
10 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix A
Summary of Changes from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010
BOX A1. Categories for classifying intrauterine devices and
hormonal contraceptives
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.
The classification additions, deletions, and modifications
from the 2010 U.S. Medical Eligibility Criteria for Contraceptive
Use (U.S. MEC) are summarized in the following tables
(Box A1) (Tables A1 and A2). For conditions for which
classifications changed for one or more contraceptive methods
or the condition description underwent a major modification,
the changes or modifications are in bold italics (Tables A1
and A2). Conditions that do not appear in this table remain
unchanged from the 2010 U.S. MEC.
TABLE A1. Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
Breastfeeding
a. <21 days postpartum — — 2 2 2 4 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
b. 21 to <30 days postpartum
i. With other risk factors for
VTE (e.g., age ≥35 years,
previous VTE, thrombophilia,
immobility, transfusion at
delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
— — 2 2 2 3 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
CHCs: For women with other risk factors for VTE, these risk
factors might increase the classication to a category 4.
ii. Without other risk factors
for VTE
— — 2 2 2 3 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
c. 30–42 days postpartum
i. With other risk factors for
VTE (e.g., age ≥35 years,
previous VTE, thrombophilia,
immobility, transfusion at
delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
— — 1 1 1 3 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
CHCs: For women with other risk factors for VTE, these risk
factors might increase the classication to a category 4.
ii. Without other risk factors
for VTE
— — 1 1 1 2 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
d. >42 days postpartum — — 1 1 1 2 Breastfeeding provides important health benets for
mother and infant. The U.S. Department of Health and
Human Services recommends increasing the proportion
of infants initially breastfed, exclusively breastfed through
6 months of life, and continuing breastfeeding through at
least 1 year of life as key public health goals (1).
See table footnotes on page 16.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 11
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
Postpartum (nonbreastfeeding
women)
a. <21 days postpartum — — 1 1 1 4 —
b. 21–42 days postpartum
i. With other risk factors for
VTE (e.g., age ≥35 years,
previous VTE, thrombophilia,
immobility, transfusion at
delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
— — 1 1 1 3 CHCs: For women with other risk factors for VTE, these risk
factors might increase the classication to a category 4.
ii. Without other risk factors
for VTE
— — 1 1 1 2 —
c. >42 days postpartum — — 1 1 1 1 —
Postpartum (including cesarean
delivery)
a. <10 minutes after delivery of
the placenta
IUDs: Insertion of IUDs among postpartum women is safe
and does not appear to increase health risks associated
with IUD use such as infection. Higher rates of expulsion
during the postpartum period should be considered as
they relate to eectiveness, along with patient access to
interval placement (i.e., not related to pregnancy) when
expulsion rates are lower.
Breastfeeding: Breastfeeding provides important health
benets for mother and infant. The U.S. Department of
Health and Human Services recommends increasing the
proportion of infants initially breastfed, exclusively
breastfed through 6 months of life, and continuing
breastfeeding through at least 1 year of life as key public
health goals (1).
i. Breastfeeding 1 2 — — — —
ii. Nonbreastfeeding 1 1 — — — —
b. 10 minutes after delivery of
the placenta to <4 weeks
(breastfeeding or
nonbreastfeeding)
2 2 — — — — IUDs: Insertion of IUDs among postpartum women is safe
and does not appear to increase health risks associated
with IUD use such as infection. Higher rates of expulsion
during the postpartum period should be considered as
they relate to eectiveness, along with patient access to
interval placement (i.e., not related to pregnancy) when
expulsion rates are lower.
Breastfeeding: Breastfeeding provides important health
benets for mother and infant. The U.S. Department of
Health and Human Services recommends increasing the
proportion of infants initially breastfed, exclusively
breastfed through 6 months of life, and continuing
breastfeeding through at least 1 year of life as key public
health goals (1).
c. ≥4 weeks (breastfeeding or
nonbreastfeeding)
1 1 — — — — IUDs: Insertion of IUDs among postpartum women is safe
and does not appear to increase health risks associated
with IUD use such as infection. Higher rates of expulsion
during the postpartum period should be considered as
they relate to eectiveness, along with patient access to
interval placement (i.e., not related to pregnancy) when
expulsion rates are lower.
Breastfeeding: Breastfeeding provides important health
benets for mother and infant. The U.S. Department of
Health and Human Services recommends increasing the
proportion of infants initially breastfed, exclusively
breastfed through 6 months of life, and continuing
breastfeeding through at least 1 year of life as key public
health goals (1).
d. Postpartum sepsis 4 4 — — — — —
See table footnotes on page 16.

Recommendations and Reports
12 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
Multiple risk factors for
atherosclerotic cardiovascular
disease (e.g., older age,
smoking, diabetes, hyperten-
sion, low HDL, high LDL, or
high triglyceride levels)
1 2 2 3 2 3/4 Implants, DMPA, POP: When multiple major risk factors
exist, risk for cardiovascular disease might increase
substantially. Certain POCs might increase the risk for
thrombosis, although this increase is substantially less
than with COCs. The eects of DMPA might persist for
some time after discontinuation.
CHCs: When a woman has multiple major risk factors, any
of which alone would substantially increase her risk for
cardiovascular disease, use of CHCs might increase her risk
to an unacceptable level. However, a simple addition of
categories for multiple risk factors is not intended; for
example, a combination of two category 2 risk factors
might not necessarily warrant a higher category.
Implants, DMPA, POP, CHCs: The recommendations
apply to known preexisting medical conditions or
characteristics. Few if any screening tests are needed
before initiation of contraception. See the U.S. Selected
Practice Recommendations for Contraceptive Use (http://
www.cdc.gov/reproductivehealth/unintendedpreg-
nancy/usspr.htm)
Supercial venous disorders
a. Varicose veins 1 1 1 1 1 1 —
b. Supercial venous
thrombosis (acute or history)
1 1 1 1 1 3 CHCs: Supercial venous thrombosis might be associated
with an increased risk for VTE. If a woman has risk factors
for concurrent DVT (e.g., known thrombophilia or cancer)
or has current or history of DVT, see recommendations
for DVT/PE. Supercial venous thrombosis associated
with a peripheral intravenous catheter is less likely to be
associated with additional thrombosis and use of CHCs
may be considered.
Headaches
a. Nonmigraine (mild or severe) 1 1 1 1 1 1 CHCs: Classication depends on accurate diagnosis of
those severe headaches that are migraines and those
headaches that are not, as well as diagnosis of ever
experiencing aura. Aura is a specic focal neurologic
symptom. For more information about headache
classication see The International Headache Classication,
3rd edition (http://www.ihs-classication.org/_downloads/
mixed/International-Headache-Classication-III-ICHD-III-
2013-Beta.pdf). Any new headaches or marked changes in
headaches should be evaluated.
b. Migraine CHCs: Classication depends on accurate diagnosis of those
severe headaches that are migraines and those headaches
that are not, as well as diagnosis of ever experiencing aura.
Aura is a specic focal neurologic symptom. For more
information about headache classication see The
International Headache Society Classication, 3rd edition
(http://www.ihs-classication.org/_downloads/mixed/
International-Headache-Classication-III-ICHD-III-2013-Beta.
pdf). Any new headaches or marked changes in headaches
should be evaluated.
CHCs: Classication is for women without any other risk
factors for stroke (e.g., age, hypertension, and smoking).
i. Without aura (This category
of migraine includes
menstrual migraine.)
1 1 1 1 1 2
ii. With aura 1 1
1 1 1 4
Multiple sclerosis
a. With prolonged immobility 1 1 1 2 1 3 —
b. Without prolonged
immobility
1 1 1 2 1 1 —
Gestational trophoblastic
disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy
(Box 2).
For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
a. Suspected gestational
trophoblastic disease
(immediate postevacuation)
For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
i. Uterine size rst trimester 1 1 1 1 1 1
ii. Uterine size second
trimester
2 2 1 1 1 1
See table footnotes on page 16.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 13
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
b. Conrmed gestational
trophoblastic disease (after
initial evacuation and during
monitoring)
Initiation Continuation Initiation Continuation
i. Undetectable/nonpregnant
β-hCG levels
1 1 1 1 1 1 1 1 For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
ii. Decreasing β-hCG levels 2 1 2 1 1 1 1 1 For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
IUD: For women at higher risk for disease progression, the
benets of eective contraception must be weighed against
the potential need for early IUD removal.
iii. Persistently elevated
β-hCG levels or malignant
disease, with no evidence or
suspicion of intrauterine
disease
2 1 2 1 1 1 1 1 For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
iv. Persistently elevated
β-hCG levels or malignant
disease, with evidence or
suspicion of intrauterine
disease
4 2 4 2 1 1 1 1 For all subconditions of gestational trophoblastic
disease, classications are based on the assumption that
women are under close medical supervision because of
the need for monitoring of β-hCG levels for appropriate
disease surveillance.
Sexually transmitted diseases Initiation Continuation Initiation Continuation
a. Current purulent cervicitis or
chlamydial infection or
gonococcal infection
4 2 4 2 1 1 1 1 IUD continuation: Treat the STD using appropriate
antibiotics. The IUD usually does not need to be removed
if the woman wants to continue using it. Continued use of
an IUD depends on the woman’s informed choice and her
current risk factors for STDs and PID.
b. Vaginitis (including
Trichomonas vaginalis and
bacterial vaginosis)
2 2 2 2 1
1 1 1 —
c. Other factors related to STDs 2 2 2 2 1 1 1 1 IUD initiation: Most women do not require additional STD
screening at the time of IUD insertion. If a woman with risk
factors for STDs has not been screened for gonorrhea and
chlamydia according to CDC STD treatment guidelines (2),
screening may be performed at the time of IUD insertion
and insertion should not be delayed.
High risk for HIV Initiation Continuation Initiation Continuation DMPA: Some studies suggest that women using
progestin-only injectable contraception might be at
increased risk for HIV acquisition; other studies do not
show this association. CDC reviewed all available
evidence and agreed that the data were not suciently
conclusive to change current guidance. However,
because of the inconclusive nature of the body of
evidence on possible increased risk for HIV acquisition,
women using progestin-only injectable contraception
should be strongly advised to also always use condoms
(male or female) and take other HIV preventive
measures. Expansion of contraceptive method mix and
further research on the relationship between hormonal
contraception and HIV infection are essential. These
recommendations will be continually reviewed in light of
new evidence.
2 2 2 2 1 1 1 1
HIV infection
For women with HIV infection
who are not clinically well or not
receiving ARV therapy, this
condition is associated with
increased risk for adverse health
events as a result of pregnancy
(Box 2).
— — — — 1 1 1 1 Implants, DMPA, POP, CHCs: Drug interactions might
exist between hormonal contraceptives and ARV drugs;
see Drug Interactions section.
a. Clinically well receiving ARV
therapy
1 1 1 1 — — — — —
b. Not clinically well or not
receiving ARV therapy
2 1 2 1 — — — — —
See table footnotes on page 16.

Recommendations and Reports
14 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
Cystic brosis
This condition is associated with
increased risk for adverse health
events as a result of pregnancy
(Box 2).
1 1 1 2 1 1 Persons with cystic brosis are at increased risk for
diabetes, liver disease, gallbladder disease, and VTE
(particularly related to use of central venous catheters)
and are frequently prescribed antibiotics. Categories
assigned to such conditions in U.S. MEC should be the
same for women with cystic brosis who have these
conditions. For cystic brosis, classications are based on
the assumption that no other conditions are present;
these classications must be modied in the presence of
such conditions.
Implants, DMPA, POP, CHCs: Certain drugs to treat cystic
brosis (e.g., lumacaftor) might reduce eectiveness of
hormonal contraceptives, including oral, injectable,
transdermal, and implantable contraceptives.
Antiretroviral therapy Initiation Continuation Initiation Continuation IUD: No known interaction exists between ARV therapy
and IUD use. However, IUD insertion is classied as
category 2 if the woman is not clinically well or not
receiving ARV therapy. Otherwise, both insertion and
continuation are classied as category 1 (see HIV
Infection section).
a. Nucleoside reverse
transcriptase inhibitors (NRTIs)
i. Abacavir (ABC) 1/2 1 1/2 1 1 1 1 1 —
ii. Tenofovir (TDF) 1/2 1 1/2 1 1 1 1 1 —
iii. Zidovudine (AZT) 1/2 1 1/2 1 1 1 1 1 —
iv. Lamivudine (3TC) 1/2 1 1/2 1 1 1 1 1 —
v. Didanosine (DDI) 1/2 1 1/2 1 1 1 1 1 —
vi. Emtricitabine (FTC) 1/2 1 1/2 1 1 1 1 1 —
vii. Stavudine (D4T) 1/2 1 1/2 1 1 1 1 1 —
b. Nonnucleoside reverse
transcriptase inhibitors
(NNRTIs)
i. Efavirenz (EFV) 1/2 1 1/2 1 2 1
2 2 Implants, DMPA, POP, CHCs: Evidence suggests drug
interactions between efavirenz and certain hormonal
contraceptives. These interactions might reduce the
eectiveness of the hormonal contraceptive.
ii. Etravirine (ETR) 1/2 1 1/2 1 1 1 1 1 —
iii. Nevirapine (NVP) 1/2 1 1/2 1 1 1 1 1 —
iv. Rilpivirine (RPV) 1/2 1 1/2 1 1 1 1 1 —
c. Ritonavir-boosted protease
inhibitors
i. Ritonavir-boosted
atazanavir (ATV/r)
1/2 1 1/2 1 2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain ritonavir-boosted protease
inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal
contraceptive. Any potential eect on contraceptive
eectiveness is likely to be lower with DMPA than with
other POCs because of the higher dose of DMPA.
CHCs: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors
and certain hormonal contraceptives that might reduce
the eectiveness of the hormonal contraceptive.
ii. Ritonavir-boosted
darunavir (DRV/r)
1/2 1 1/2 1 2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain ritonavir-boosted protease
inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal
contraceptive. Any potential eect on contraceptive
eectiveness is likely to be lower with DMPA than with
other POCs because of the higher dose of DMPA.
CHCs: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors
and certain hormonal contraceptives that might reduce
the eectiveness of the hormonal contraceptive.
See table footnotes on page 16.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 15
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
iii. Ritonavir-boosted
fosamprenavir (FPV/r)
1/2 1 1/2 1 2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain ritonavir-boosted protease
inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal
contraceptive. Any potential eect on contraceptive
eectiveness is likely to be lower with DMPA than with
other POCs because of the higher dose of DMPA.
CHCs: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors
and certain hormonal contraceptives that might reduce
the eectiveness of the hormonal contraceptive.
iv. Ritonavir-boosted
lopinavir (LPV/r)
1/2 1 1/2 1 1 1 1 1 —
v. Ritonavir-boosted
saquinavir (SQV/r)
1/2 1 1/2 1 2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain ritonavir-boosted protease
inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal
contraceptive. Any potential eect on contraceptive
eectiveness is likely to be lower with DMPA than with
other POCs because of the higher dose of DMPA.
CHCs: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors
and certain hormonal contraceptives that might reduce
the eectiveness of the hormonal contraceptive.
vi. Ritonavir-boosted
tipranavir (TPV/r)
1/2 1 1/2 1 2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain ritonavir-boosted protease
inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal
contraceptive. Any potential eect on contraceptive
eectiveness is likely to be lower with DMPA than with
other POCs because of the higher dose of DMPA.
CHCs: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors
and certain hormonal contraceptives that might reduce
the eectiveness of the hormonal contraceptive.
d. Protease inhibitors without
ritonavir
i. Atazanavir (ATV) 1/2 1 1/2 1 1 1 1 2 CHCs: Theoretical concern exists that increased levels of
ethinyl estradiol because of interactions with ATV might
increase the risk for adverse events.
ii. Fosamprenavir (FPV) 1/2 1 1/2 1 2 2 2 3 Implants, DMPA, POP: Theoretical concern exists that
interactions between FPV and hormonal contraceptives
leading to decreased levels of FPV might diminish
eectiveness of the antiretroviral drug. The drug
interaction likely involves CYP3A4 pathways; POCs have
less eect on CYP3A4 enzymes than CHCs.
CHCs: Concern exists that interactions between FPV and
hormonal contraceptives leading to decreased levels of FPV
might diminish eectiveness of the antiretroviral drug.
iii. Indinavir (IDV) 1/2 1 1/2 1 1 1 1 1 —
iv. Nelnavir (NFV) 1/2 1 1/2 1
2 1 2 2 Implants, DMPA, POP: Theoretically, drug interactions
might occur between certain protease inhibitors and
certain hormonal contraceptives that might reduce the
eectiveness of the hormonal contraceptive. Any
potential eect on contraceptive eectiveness is likely to
be lower with DMPA than with other POCs because of the
higher dose of DMPA. Concern exists that interactions
between NFV and POCs might decrease NFV levels.
CHCs: Evidence suggests drug interactions between
certain protease inhibitors and certain hormonal
contraceptives. These interactions might reduce the
eectiveness of the hormonal contraceptive.
See table footnotes on page 16.

Recommendations and Reports
16 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE A1. (Continued) Summary of changes in classifications from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs Clarification
e. CCR5 co-receptor
antagonists
i. Maraviroc (MVC) 1/2 1 1/2 1 1 1 1 1 —
f. HIV integrase strand transfer
inhibitors
i. Raltegravir (RAL) 1/2 1 1/2 1 1 1 1 1 —
ii. Dolutegravir (DTG) 1/2 1 1/2 1 1 1 1 1 —
iii. Elvitegravir (EVG) 1/2 1 1/2 1 1 1 1 1 —
g. Fusion inhibitors
i. Enfuvirtide 1/2 1 1/2 1 1 1 1 1 —
Psychotropic medications
a. SSRIs 1 1 1 1 1 1 —
St. John’s wort 1 1 2 1 2 2 —
Abbreviations: ARV=antiretroviral; BMI=body mass index; CHC=combined hormonal contraceptive; COC=combined oral contraceptive; Cu-IUD=copper-containing intrauterine device;
DMPA=depot medroxyprogesterone acetate; DVT=deep venous thrombosis; hCG=human chorionic gonadotropin; HDL=high-density lipoprotein; HIV = human immunodeficiency
virus; LDL=low-density lipoprotein; LNG-IUD=levonorgestrel-releasing intrauterine device; PE=pulmonary embolism; PID=pelvic inflammatory disease; POC = progestin-only contraceptive;
POP=progestin-only pill; SSRI = selective serotonin uptake inhibitor; STD=sexually transmitted disease; VTE=venous thromboembolism.
* For conditions for which classification changed for one or more contraceptive methods or the condition description underwent a major modification, the changes or modifications are in
bold italics.
TABLE A2. Summary of changes for emergency contraception from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition
Category
ClarificationCu-IUD UPA LNG COC
Pregnancy 4
NA NA NA
IUD: The IUD is not indicated during pregnancy and should not be used
because of the risk for serious pelvic infection and septic spontaneous
abortion.
ECPs: Although this method is not indicated for a woman with a known or
suspected pregnancy, no harm to the woman, the course of her pregnancy, or
the fetus if ECPs are inadvertently used is known to exist.
Breastfeeding 1
1 1 1
UPA: Breastfeeding is not recommended for 24 hours after taking UPA
because it is excreted in breast milk with highest concentrations in the first
24 hours, and maximum maternal serum levels are reached 1-3 hours after
administration. Mean UPA concentrations in breast milk decrease markedly
from 0 to 24–48 hours and then slowly decrease over 5 days (3). Breast milk
should be expressed and discarded for 24 hours after taking UPA.
Past ectopic pregnancy 1
1 1 1
—
History of bariatric surgery
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease storage capacity of
the stomach (vertical banded gastroplasty, laparoscopic
adjustable gastric band, or laparoscopic sleeve gastrectomy)
1
1 1 1
—
b. Malabsorptive procedures: decrease absorption of nutrients
and calories by shortening the functional length of the
small intestine (Roux-en-Y gastric bypass or biliopancreatic
diversion)
1
1 1 1
—
History of severe cardiovascular disease (ischemic heart disease,
cerebrovascular attack, or other thromboembolic conditions)
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1
2 2 2
—
Rheumatoid arthritis
a. Receiving immunosuppressive therapy 2
1 1 1
—
b. Not receiving immunosuppressive therapy 1
1 1 1
—
Migraine 1
1 1 2
—
Inflammatory bowel disease (ulcerative colitis or Crohn’s disease) 1
1 1 1
—
Severe liver disease (including jaundice)
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1
2 2 2
—
See table footnotes on page 17.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 17
US Department of Health and Human Services/Centers for Disease Control and Prevention
References
1. US Department of Health and Human Services. Healthy people 2020:
maternal, infant, and child health objectives. Washington, DC: US
Department of Health and Human Services; 2015. http://www.
healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-
child-health/objectives
TABLE A2. (Continued) Summary of changes for emergency contraception from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010*
Condition
Category
ClarificationCu-IUD UPA LNG COC
Solid organ transplantation
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Complicated: graft failure (acute or chronic), rejection, or
cardiac allograft vasculopathy
3
1 1 1
—
b. Uncomplicated 2
1 1 1
—
Repeated ECP use 1
1 1 1
ECPs: Recurrent ECP use is an indication that the woman requires further
counseling about other contraceptive options. Frequently repeated ECP use
might be harmful for women with conditions classified as 2, 3, or 4 for CHC or
POC use.
Sexual assault 2
1 1 1
IUD: Women who have experienced sexual assault are at increased risk
for STDs. According to CDC STD treatment guidelines, routine presumptive
treatment of chlamydia, gonorrhea, and trichomonas is recommended after
sexual assault (2). Women with current purulent cervicitis or chlamydial
infection or gonococcal infection should not undergo IUD insertion (category 4).
Obesity (BMI ≥30 kg/m
2
) 1
2 2 2
ECPs: ECPs might be less effective among women with BMI ≥30 kg/m
2
than
among women with BMI <25 kg/m
2
. Despite this, no safety concerns exist.
CYP3A4 inducers (e.g., bosentan, carbamazepine, felbamate,
griseofulvin, oxcarbazepine, phenytoin, rifampin, St. John’s
wort, topiramate, efavirenz, and lumacaftor)
1
2 2 2
ECPs: Strong CYP3A4 inducers might reduce the effectiveness of ECPs.
Abbreviations: BMI=body mass index; CHC=combined hormonal contraceptive; COC=combined oral contraceptive; Cu-IUD=copper-containing intrauterine device; ECP=emergency
contraceptive pill; IUD=intrauterine device; LNG=levonorgestrel; NA=not applicable; POC=progestin-only contraceptive; STD=sexually transmitted disease; UPA=ulipristal acetate.
* For conditions for which classification changed for one or more contraceptive methods or the condition description underwent a major modification, the changes or modifications are in bold italics.
2. Workowski KA, Bolan GA. Sexually transmitted diseases treatment
guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-03).
3. Watson Pharmaceuticals. Ella [Prescribing information]. Morristown, NJ; 2010.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022474s000lbl.pdf
Recommendations and Reports
18 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix B
Classifications for Intrauterine Devices
Classifications for intrauterine devices (IUDs) are for
the copper-containing IUD and levonorgestrel-releasing
IUD (containing a total of either 13.5 mg or 52 mg
levonorgestrel) (Box B1) (Table B1). IUDs do not protect
against sexually transmitted diseases (STDs), including human
immunodeficiency virus (HIV), and women using these
methods should be counseled that consistent and correct use of
the male latex condom reduces the risk for transmission of HIV
and other STDs. Use of female condoms can provide protection
from transmission of STDs, although data are limited.
BOX B1. Categories for classifying intrauterine devices
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 19
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-releasing
intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Personal Characteristics and Reproductive History
Pregnancy 4 4 Clarification: The IUD is not indicated during pregnancy and should not be
used because of the risk for serious pelvic infection and septic spontaneous
abortion.
Age
a. Menarche to <20 years 2 2 Comment: Concern exists both about the risk for expulsion from nulliparity
and for STDs from sexual behavior in younger age groups.
b. ≥20 years 1 1 —
Parity
a. Nulliparous 2 2 Evidence: Data conflict about whether IUD use is associated with infertility
among nulliparous women, although well-conducted studies suggest no
increased risk (1–9).
b. Parous 1 1 —
Postpartum (including cesarean
delivery)
a. <10 minutes after delivery of the
placenta
Clarification: Insertion of IUDs among postpartum women is safe and does
not appear to increase health risks associated with IUD use such as infection.
Higher rates of expulsion during the postpartum period should be considered
as they relate to effectiveness, along with patient access to interval placement
(i.e., not related to pregnancy) when expulsion rates are lower.
Clarification (breastfeeding): Breastfeeding provides important health
benefits for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially breastfed,
exclusively breastfed through 6 months of life, and continuing breastfeeding
through at least 1 year of life as key public health goals (10).
Evidence: Studies suggest that immediate postplacental (<10 minutes) and
early postpartum (10 minutes up until 72 hours) placement of Cu-IUDs and
LNG-IUDs is associated with increased risk for expulsion compared with
interval placement (i.e., not related to pregnancy). Early postpartum placement
has similar or increased risk for expulsion compared with immediate
postplacental placement. Although immediate postplacental placement at the
time of cesarean delivery might have increased risk for expulsion compared
with interval placement, risk appears lower than that for placement at the time
of vaginal delivery. Evidence for infection, perforation, and removals for pain or
bleeding are limited; however, these events are rare (11–62).
Evidence (breastfeeding): Two randomized controlled trials found
conflicting results on breastfeeding outcomes when LNG-IUDs were initiated
immediately postpartum compared with 6–8 weeks postpartum. Initiation
of LNG-IUDs immediately postpartum had no other harmful effect on infant
health, growth, or development (63,64). Breastfeeding women using IUDs do
not have an increased risk for certain IUD-related adverse events including
expulsion, infection, pain, or bleeding compared with nonbreastfeeding
women. The risk for perforation is increased independently among
breastfeeding women and among women ≤36 weeks postpartum,
compared with non-postpartum women; however, the absolute risk for
perforation remains low (11–62,65).
Comment (breastfeeding): Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding difficulties, certain
medical conditions, or certain perinatal complications and those who
deliver preterm. For these women, as for all women, discussions about
contraception for breastfeeding women should include information about
risks, benefits, and alternatives.
i. Breastfeeding 1 2
ii. Nonbreastfeeding 1 1
See table footnotes on page 30.

Recommendations and Reports
20 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
b. 10 minutes after delivery of the
placenta to <4 weeks (breastfeeding
or nonbreastfeeding)
2 2 Clarification: Insertion of IUDs among postpartum women is safe and does
not appear to increase health risks associated with IUD use such as infection.
Higher rates of expulsion during the postpartum period should be considered
as they relate to effectiveness, along with patient access to interval placement
(i.e., not related to pregnancy) when expulsion rates are lower.
Clarification (breastfeeding): Breastfeeding provides important health
benefits for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially breastfed,
exclusively breastfed through 6 months of life, and continuing breastfeeding
through at least 1 year of life as key public health goals (10).
Evidence: Studies suggest that immediate postplacental (<10 minutes) and
early postpartum (10 minutes up until 72 hours) placement of Cu-IUDs and
LNG-IUDs is associated with increased risk for expulsion compared with
interval placement (i.e., not related to pregnancy). Early postpartum placement
has similar or increased risk for expulsion compared with immediate
postplacental placement. Although immediate postplacental placement at the
time of cesarean delivery might have increased risk for expulsion compared
with interval placement, risk appears lower than that for placement at the time
of vaginal delivery. Evidence for infection, perforation, and removals for pain or
bleeding are limited; however, these events are rare (11–62).
Evidence (breastfeeding): Two randomized controlled trials found
conflicting results on breastfeeding outcomes when LNG-IUDs were initiated
immediately postpartum compared with 6–8 weeks postpartum. Initiation
of LNG-IUDs immediately postpartum had no other harmful effect on infant
health, growth, or development (63,64). Breastfeeding women using IUDs do
not have an increased risk for certain IUD-related adverse events including
expulsion, infection, pain, or bleeding compared with nonbreastfeeding
women. The risk for perforation is increased independently among
breastfeeding women and among women ≤36 weeks postpartum,
compared with non-postpartum women; however, the absolute risk for
perforation remains low (11–62,65).
Comment (breastfeeding): Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding difficulties, certain
medical conditions, or certain perinatal complications and those who
deliver preterm. For these women, as for all women, discussions about
contraception for breastfeeding women should include information about
risks, benefits, and alternatives.
c. ≥4 weeks (breastfeeding or
nonbreastfeeding)
1 1 Clarification: Insertion of IUDs among postpartum women is safe and does
not appear to increase health risks associated with IUD use such as infection.
Higher rates of expulsion during the postpartum period should be considered
as they relate to effectiveness, along with patient access to interval placement
(i.e., not related to pregnancy) when expulsion rates are lower.
Clarification (breastfeeding): Breastfeeding provides important health
benefits for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially breastfed,
exclusively breastfed through 6 months of life, and continuing breastfeeding
through at least 1 year of life as key public health goals (10).
Evidence (breastfeeding): Initiation of LNG-IUDs at 4 weeks postpartum
or later demonstrated no detrimental effect on breastfeeding outcomes
and no harmful effect on infant health, growth, or development (63,64).
Breastfeeding women using IUDs do not have an increased risk for certain
IUD-related adverse events including expulsion, infection, pain, or bleeding
compared with nonbreastfeeding women. The risk for perforation is
increased independently among breastfeeding women and among women
≤36 weeks postpartum, compared with non-postpartum women; however,
the absolute risk for perforation remains low (11–62,65).
Comment (breastfeeding): Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding difficulties, certain
medical conditions, or certain perinatal complications and those who
deliver preterm. For these women, as for all women, discussions about
contraception for breastfeeding women should include information about
risks, benefits, and alternatives.
d. Postpartum sepsis 4 4 Comment: Theoretical concern exists that postpartum insertion of an IUD
in a women with recent chorioamnionitis or current endometritis might be
associated with increased complications.
See table footnotes on page 30.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 21
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Postabortion
a. First trimester 1 1 Clarification: IUDs can be inserted immediately after spontaneous or
induced abortion.
Evidence: Risk for complications from immediate versus delayed insertion of
an IUD after abortion did not differ. Expulsion was greater when an IUD was
inserted after a second trimester abortion than when inserted after a first
trimester abortion. Safety or expulsion for postabortion insertion of an LNG-
IUD did not differ from that of a Cu-IUD (66).
b. Second trimester 2 2
c. Immediate postseptic abortion 4 4 Comment: Insertion of an IUD might substantially worsen the condition.
Past ectopic pregnancy 1 1 Comment: The absolute risk for ectopic pregnancy is extremely low because
of the high effectiveness of IUDs. However, when a woman becomes
pregnant during IUD use, the relative likelihood of ectopic pregnancy
increases substantially.
History of pelvic surgery
(see Postpartum [Including Cesarean
Delivery] section)
1 1 —
Smoking
a. Age <35 years 1 1 —
b. Age ≥35 years
i. <15 cigarettes per day 1 1 —
ii. ≥15 cigarettes per day 1 1 —
Obesity
a. BMI ≥30 kg/m
2
1 1 —
b. Menarche to <18 years and BMI
≥30 kg/m
2
1 1 —
History of bariatric surgery
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease
storage capacity of the stomach
(vertical banded gastroplasty,
laparoscopic adjustable gastric
band, or laparoscopic sleeve
gastrectomy)
1 1 —
b. Malabsorptive procedures:
decrease absorption of nutrients
and calories by shortening the
functional length of the small
intestine (Roux-en-Y gastric bypass
or biliopancreatic diversion)
1 1 —
Cardiovascular Disease
Multiple risk factors for
atherosclerotic cardiovascular
disease (e.g., older age, smoking,
diabetes, hypertension, low HDL, high
LDL, or high triglyceride levels)
1 2 —
Hypertension
Systolic blood pressure ≥160 mm Hg
or diastolic blood pressure ≥100 mm
Hg are associated with increased risk
for adverse health events as a result
of pregnancy (Box 2).
a. Adequately controlled
hypertension
1 1 Clarification: For all categories of hypertension, classifications are based
on the assumption that no other risk factors for cardiovascular disease
exist. When multiple risk factors do exist, risk for cardiovascular disease
might increase substantially. A single reading of blood pressure level is not
sufficient to classify a woman as hypertensive.
b. Elevated blood pressure levels
(properly taken measurements)
Clarification: For all categories of hypertension, classifications are based
on the assumption that no other risk factors for cardiovascular disease
exist. When multiple risk factors do exist, risk for cardiovascular disease
might increase substantially. A single reading of blood pressure level is not
sufficient to classify a woman as hypertensive.
Comment: Theoretical concern exists about the effect of LNG on lipids. Use
of Cu-IUDs has no restrictions.
i. Systolic 140–159 mm Hg or
diastolic 90–99 mm Hg
1 1
ii. Systolic ≥160 mm Hg or diastolic
≥100 mm Hg
1 2
See table footnotes on page 30.

Recommendations and Reports
22 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
c. Vascular disease 1 2 Clarification: For all categories of hypertension, classifications are based
on the assumption that no other risk factors for cardiovascular disease
exist. When multiple risk factors do exist, risk for cardiovascular disease
might increase substantially. A single reading of blood pressure level is not
sufficient to classify a woman as hypertensive.
Comment: Theoretical concern exists about the effect of LNG on lipids. Use
of Cu-IUDs has no restrictions
History of high blood pressure during
pregnancy (when current blood
pressure is measurable and normal)
1 1 —
Deep venous thrombosis/
Pulmonary embolism
a. History of DVT/PE, not receiving
anticoagulant therapy
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
1 2 —
• History of estrogen-associated
DVT/PE
• Pregnancy-associated DVT/PE
• Idiopathic DVT/PE
• Known thrombophilia,
including antiphospholipid
syndrome
• Active cancer (metastatic, receiving
therapy, or within 6 months after
clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
1 2 —
b. Acute DVT/PE 2 2 Evidence: No direct evidence exists on the use of POCs among women with
acute DVT/PE. Although findings on the risk for venous thrombosis with
the use of POCs in otherwise healthy women are inconsistent, any small
increased risk is substantially less than that with COCs (67–69).
c. DVT/PE and established
anticoagulant therapy for at least
3 months
Evidence: No direct evidence exists on the use of POCs among women with
acute DVT/PE. Although findings on the risk for venous thrombosis with
the use of POCs in otherwise healthy women are inconsistent, any small
increased risk is substantially less than that with COCs (67–69).
Evidence: Limited evidence indicates that insertion of the LNG-IUD does not
pose major bleeding risks in women receiving chronic anticoagulant therapy
(70–73).
Comment: The LNG-IUD might be a useful treatment for menorrhagia in
women receiving long-term anticoagulation therapy.
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
2 2 —
• Known thrombophilia,
including antiphospholipid
syndrome
• Active cancer (metastatic, receiving
therapy, or within 6 months after
clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
2 2 —
d. Family history (first-degree
relatives)
1 1 —
e. Major surgery
i. With prolonged immobilization 1 2 —
ii. Without prolonged
immobilization
1 1 —
f. Minor surgery without
immobilization
1 1
See table footnotes on page 30.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 23
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Known thrombogenic mutations
(e.g., factor V Leiden; prothrombin
mutation; and protein S, protein C, and
antithrombin deficiencies)
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 2 Clarification: Routine screening is not appropriate because of the rarity of
the conditions and the high cost of screening.
Superficial venous disorders
a. Varicose veins 1 1 —
b. Superficial venous thrombosis
(acute or history)
1 1 —
Current and history of ischemic
heart disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 Initiation Continuation Comment: Theoretical concern exists about the effect of LNG on lipids. Use
of Cu-IUDs has no restrictions.
2 3
Stroke (history of cerebrovascular
accident)
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 2 Comment: Theoretical concern exists about the effect of LNG on lipids. Use
of Cu-IUDs has no restrictions.
Valvular heart disease
Complicated valvular heart disease is
a condition associated with increased
risk for adverse health events as a
result of pregnancy (Box 2).
Comment: According to the American Heart Association, administration of
prophylactic antibiotics solely to prevent endocarditis is not recommended
for patients who undergo genitourinary tract procedures, including insertion
or removal of IUDs (74).
a. Uncomplicated 1 1
b. Complicated (pulmonary
hypertension, risk for atrial
fibrillation, or history of subacute
bacterial endocarditis)
1 1
Peripartum cardiomyopathy
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Evidence: No direct evidence exists on the safety of IUDs among women
with peripartum cardiomyopathy. Limited indirect evidence from
noncomparative studies did not demonstrate any cases of arrhythmia or
infective endocarditis in women with cardiac disease who used IUDs (75).
Comment: IUD insertion might induce cardiac arrhythmias in healthy
women; women with peripartum cardiomyopathy have a high incidence of
cardiac arrhythmias.
a. Normal or mildly impaired
cardiac function (New York Heart
Association Functional Class I or
II: patients with no limitation of
activities or patients with slight,
mild limitation of activity) (76)
i. <6 months 2 2
ii. ≥6 months 2 2
b. Moderately or severely impaired
cardiac function (New York Heart
Association Functional Class III or IV:
patients with marked limitation of
activity or patients who should be at
complete rest) (76)
2 2
Rheumatic Diseases
Systemic lupus erythematosus
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation
a. Positive (or unknown)
antiphospholipid antibodies
1
1 3 Clarification: Persons with SLE are at increased risk for ischemic heart
disease, stroke, and VTE. Categories assigned to such conditions in U.S. MEC
should be the same for women with SLE who have these conditions. For all
subconditions of SLE, classifications are based on the assumption that no
other risk factors for cardiovascular disease are present; these classifications
must be modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive methods,
including hormonal contraceptives (73,77–94).
Evidence: Antiphospholipid antibodies are associated with a higher risk for
both arterial and venous thrombosis (95,96)
See table footnotes on page 30.

Recommendations and Reports
24 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
b. Severe thrombocytopenia 3 2 2 Clarification: Persons with SLE are at increased risk for ischemic heart
disease, stroke, and VTE. Categories assigned to such conditions in U.S. MEC
should be the same for women with SLE who have these conditions. For all
subconditions of SLE, classifications are based on the assumption that no
other risk factors for cardiovascular disease are present; these classifications
must be modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive methods,
including hormonal contraceptives (73,77–94).
Clarification: Severe thrombocytopenia increases the risk for bleeding. The
category should be assessed according to the severity of thrombocytopenia
and its clinical manifestations. In women with very severe thrombocytopenia
who are at risk for spontaneous bleeding, consultation with a specialist and
certain pretreatments might be warranted.
Evidence: The LNG-IUD might be a useful treatment for menorrhagia in
women with severe thrombocytopenia (73).
c. Immunosuppressive therapy 2 1 2 Clarification: Persons with SLE are at increased risk for ischemic heart
disease, stroke, and VTE. Categories assigned to such conditions in U.S. MEC
should be the same for women with SLE who have these conditions. For all
subconditions of SLE, classifications are based on the assumption that no
other risk factors for cardiovascular disease are present; these classifications
must be modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive methods,
including hormonal contraceptives (73,77–94).
d. None of the above 1 1 2 Clarification: Persons with SLE are at increased risk for ischemic heart
disease, stroke, and VTE. Categories assigned to such conditions in U.S. MEC
should be the same for women with SLE who have these conditions. For all
subconditions of SLE, classifications are based on the assumption that no
other risk factors for cardiovascular disease are present; these classifications
must be modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive methods,
including hormonal contraceptives (73,77–94).
Rheumatoid arthritis Initiation Continuation Initiation Continuation
a. Receiving immunosuppressive
therapy
2 1 2 1 —
b. Not receiving immunosuppressive
therapy
1 1 —
Neurologic Conditions
Headaches
a. Nonmigraine (mild or severe) 1 1 —
b. Migraine
i. Without aura (This category
of migraine includes menstrual
migraine.)
1 1 Evidence: No studies directly examined the risk for stroke among women
with migraine using LNG-IUDs (97). Limited evidence demonstrated that
women using LNG-IUDs do not have an increased risk for ischemic stroke
compared with women not using hormonal contraceptives (98).
Comment: Menstrual migraine is a subtype of migraine without aura. For
more information see The International Headache Society Classification, 3rd
edition (http://www.ihs-classification.org/_downloads/mixed/International-
Headache-Classification-III-ICHD-III-2013-Beta.pdf ).
ii. With aura 1 1
Epilepsy
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1
1 —
Multiple sclerosis
a. With prolonged immobility 1 1 —
b. Without prolonged immobility 1 1 —
Depressive Disorders
Depressive disorders 1 1 Clarification: If a woman is receiving psychotropic medications or St. John’s
wort, see Drug Interactions section.
Evidence: The frequency of psychiatric hospitalizations for women with
bipolar disorder or depression did not significantly differ among women
using DMPA, LNG-IUD, Cu-IUD, or sterilization (99).
See table footnotes on page 30.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 25
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Reproductive Tract Infections and Disorders
Vaginal bleeding patterns Initiation Continuation
a. Irregular pattern without heavy
bleeding
1 1 1 —
b. Heavy or prolonged bleeding
(includes regular and irregular
patterns)
2 1 2 Clarification: Unusually heavy bleeding should raise suspicion of a serious
underlying condition.
Evidence: Evidence from studies examining the treatment effects of the
LNG-IUD among women with heavy or prolonged bleeding reported no
increase in adverse effects and found the LNG-IUD to be beneficial in treating
menorrhagia (100–107).
Unexplained vaginal bleeding
(suspicious for serious condition)
before evaluation
Initiation
4
Continuation
2
Initiation
4
Continuation
2
Clarification: If pregnancy or an underlying pathological condition (e.g., pelvic
malignancy) is suspected, it must be evaluated and the category adjusted after
evaluation. The IUD does not need to be removed before evaluation.
Endometriosis 2 1 Evidence: LNG-IUD use among women with endometriosis decreased
dysmenorrhea, pelvic pain, and dyspareunia (108–112).
Benign ovarian tumors (including cysts) 1 1 —
Severe dysmenorrhea 2 1 Comment: Dysmenorrhea might intensify with Cu-IUD use. LNG-IUD use has
been associated with reduction of dysmenorrhea.
Gestational trophoblastic disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Suspected gestational
trophoblastic disease (immediate
postevacuation)
Clarification: For all subconditions of gestational trophoblastic disease,
classifications are based on the assumption that women are under close
medical supervision because of the need for monitoring of β-hCG levels for
appropriate disease surveillance.
Evidence: Limited evidence suggests that women using an IUD after uterine
evacuation for a molar pregnancy are not at greater risk for postmolar
trophoblastic disease than are women using other methods of contraception (113).
Comment: The risk for expulsion immediately postevacuation for gestational
trophoblastic disease is unknown. Expulsion is greater after IUD insertion
immediately postevacuation for a spontaneous or induced abortion in the
second trimester compared with IUD insertion after a first trimester abortion.
i. Uterine size first trimester 1 1
ii. Uterine size second trimester 2 2
b. Confirmed gestational
trophoblastic disease (after initial
evacuation and during monitoring)
Initiation Continuation Initiation Continuation
i. Undetectable/nonpregnant
β-hCG levels
1 1 1 1 Clarification: For all subconditions of gestational trophoblastic disease,
classifications are based on the assumption that women are under close
medical supervision because of the need for monitoring of β-hCG levels for
appropriate disease surveillance.
Evidence: Limited evidence suggests that women using an IUD after uterine
evacuation for a molar pregnancy are not at greater risk for postmolar
trophoblastic disease than are women using other methods of contraception (113).
Comment: Once β-hCG levels have decreased to nonpregnant levels, the risk
for disease progression is likely to be very low.
ii. Decreasing β-hCG levels 2 1 2 1 Clarification: For all subconditions of gestational trophoblastic disease,
classifications are based on the assumption that women are under close
medical supervision because of the need for monitoring of β-hCG levels for
appropriate disease surveillance.
Clarification: For women at higher risk for disease progression, the benefits
of effective contraception must be weighed against the potential need for
early IUD removal.
Evidence: Limited evidence suggests that women using an IUD after uterine
evacuation for a molar pregnancy are not at greater risk for postmolar
trophoblastic disease than are women using other methods of contraception (113).
See table footnotes on page 30.

Recommendations and Reports
26 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
iii. Persistently elevated β-hCG
levels or malignant disease,
with no evidence or suspicion of
intrauterine disease
2 1 2 1 Clarification: For all subconditions of gestational trophoblastic disease,
classifications are based on the assumption that women are under close
medical supervision because of the need for monitoring of β-hCG levels for
appropriate disease surveillance.
Evidence: Limited evidence suggests that women using an IUD after uterine
evacuation for a molar pregnancy are not at greater risk for postmolar
trophoblastic disease than are women using other methods of contraception (113).
iv. Persistently elevated β-hCG
levels or malignant disease,
with evidence or suspicion of
intrauterine disease
4 2 4 2 Clarification: For all subconditions of gestational trophoblastic disease,
classifications are based on the assumption that women are under close
medical supervision because of the need for monitoring of β-hCG levels for
appropriate disease surveillance.
Evidence: Limited evidence suggests that women using an IUD after uterine
evacuation for a molar pregnancy are not at greater risk for postmolar
trophoblastic disease than are women using other methods of contraception
(113).
Comment: For women with suspected or confirmed intrauterine disease,
an IUD should not be inserted because of theoretical risk for perforation,
infection, and hemorrhage. For women who already have an IUD in place,
individual circumstance along with the benefits of effective contraception
must be weighed against theoretical risks of either removal or continuation
of the IUD.
Cervical ectropion 1 1 —
Cervical intraepithelial neoplasia 1 2 Comment: Theoretical concern exists that LNG-IUDs might enhance
progression of cervical intraepithelial neoplasia.
Cervical cancer (awaiting treatment) Initiation Continuation Initiation Continuation Comment: Concern exists about the increased risk for infection and bleeding
at insertion. The IUD most likely will need to be removed at the time of
treatment but until then, the woman is at risk for pregnancy.
4 2 4 2
Breast disease
Breast cancer is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Undiagnosed mass 1 2 —
b. Benign breast disease 1 1 —
c. Family history of cancer 1 1 —
d. Breast cancer Comment: Breast cancer is a hormonally sensitive tumor. Concerns about
progression of the disease might be less with LNG-IUDs than with COCs or
higher-dose POCs.
i. Current 1 4
ii. Past and no evidence of current
disease for 5 years
1 3
Endometrial hyperplasia 1 1 Evidence: Among women with endometrial hyperplasia, no adverse health
events occurred with LNG-IUD use; most women experienced disease
regression (114).
Endometrial cancer
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation
Continuation Initiation Continuation Comment: Concern exists about the increased risk for infection, perforation,
and bleeding at insertion. The IUD most likely will need to be removed at the
time of treatment, but until then, the woman is at risk for pregnancy.
4 2 4 2
Ovarian cancer
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 Comment: Women with ovarian cancer who undergo fertility-sparing
treatment and need contraception may use an IUD.
Uterine fibroids 2 2 Evidence: Among women with uterine fibroids using an LNG-IUD, most
experienced improvements in serum levels of hemoglobin, hematocrit,
and ferritin and in menstrual blood loss (115). Rates of LNG-IUD expulsion
were higher in women with uterine fibroids (11%) than in women without
fibroids (0%–3%); these findings were either not statistically significant or
significance testing was not conducted (115). Rates of expulsion found in
noncomparative studies ranged from 0%–20% (115).
Comment: Women with heavy or prolonged bleeding should be assigned
the category for that condition.
See table footnotes on page 30.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 27
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Anatomical abnormalities
a. Distorted uterine cavity (any
congenital or acquired uterine
abnormality distorting the
uterine cavity in a manner that is
incompatible with IUD insertion)
4 4 Comment: An anatomical abnormality that distorts the uterine cavity might
preclude proper IUD placement.
b. Other abnormalities (including
cervical stenosis or cervical
lacerations) not distorting the
uterine cavity or interfering with
IUD insertion
2 2 —
Pelvic inflammatory disease Initiation Continuation Initiation Continuation
a. Past PID Comment: IUDs do not protect against STDs, including HIV, or PID. In women
at low risk for STDs, IUD insertion poses little risk for PID.
i. With subsequent pregnancy 1 1 1 1
ii. Without subsequent pregnancy 2 2 2 2
b. Current PID 4 2 4 2 Clarification (continuation): Treat the PID using appropriate antibiotics. The
IUD usually does not need to be removed if the woman wants to continue
using it. Continued use of an IUD depends on the woman’s informed choice
and her current risk factors for STDs and PID.
Evidence: Among IUD users treated for PID, clinical course did not differ
regardless of whether the IUD was removed or left in place (116).
Sexually transmitted diseases Initiation Continuation Initiation Continuation
a. Current purulent cervicitis or
chlamydial infection or gonococcal
infection
4 2 4 2 Clarification (continuation): Treat the STD using appropriate antibiotics. The
IUD usually does not need to be removed if the woman wants to continue
using it. Continued use of an IUD depends on the woman’s informed choice
and her current risk factors for STDs and PID.
Evidence: Among women who had an IUD inserted, the absolute risk for
subsequent PID was low among women with STD at the time of insertion but
greater than among women with no STD at the time of IUD insertion (117–123).
b. Vaginitis (including Trichomonas
vaginalis and bacterial vaginosis)
2 2 2 2 —
c. Other factors related to STDs 2 2 2 2 Clarification (initiation): Most women do not require additional STD
screening at the time of IUD insertion. If a woman with risk factors for STDs
has not been screened for gonorrhea and chlamydia according to CDC STD
treatment guidelines (124), screening may be performed at the time of IUD
insertion and insertion should not be delayed.
Evidence: Women who undergo same-day STD screening and IUD insertion
have low incidence rates of PID. Algorithms for predicting PID among
women with risk factors for STDs have poor predictive value. Risk for PID
among women with risk factors for STDs is low (125).
HIV
High risk for HIV Initiation Continuation Initiation Continuation Evidence: Among women at risk for HIV, Cu-IUD use did not increase risk for
HIV acquisition (126–136).
2 2 2 2
HIV infection
For women with HIV infection
who are not clinically well or not
receiving ARV therapy, this condition
is associated with increased risk for
adverse health events as a result of
pregnancy (Box 2).
Evidence: Among IUD users, limited evidence shows a low risk for PID among
HIV-infected women using IUDs and no higher risk for pelvic infectious
complications in HIV-infected than in HIV-noninfected women or among
women with varying degrees of HIV severity. IUD use did not adversely affect
progression of HIV during 6–45 months of follow-up or when compared with
hormonal contraceptive use among HIV-infected women. Furthermore, IUD
use among HIV-infected women was not associated with increased risk for
transmission to sex partners or with increased genital viral shedding (137).
a. Clinically well receiving ARV
therapy
1 1 1 1
b. Not clinically well or not receiving
ARV therapy
2 1 2 1
See table footnotes on page 30.

Recommendations and Reports
28 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Other Infections
Schistosomiasis
Schistosomiasis with fibrosis of the
liver is associated with increased risk
for adverse health events as a result
of pregnancy (Box 2).
a. Uncomplicated 1 1 —
b. Fibrosis of the liver (if severe, see
Cirrhosis section)
1 1 —
Tuberculosis
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
a. Nonpelvic 1 1 1 1 —
b. Pelvic 4 3 4 3 Comment: Insertion of an IUD might substantially worsen the condition.
Malaria 1 1 —
Endocrine Conditions
Diabetes
Insulin-dependent diabetes; diabetes
with nephropathy, retinopathy, or
neuropathy; diabetes with other
vascular disease; or diabetes of
>20 years’ duration are associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. History of gestational disease 1 1 —
b. Nonvascular disease Evidence: Limited evidence on the use of the LNG-IUD among women with
insulin-dependent or non–insulin-dependent diabetes suggests that these
methods have little effect on short-term or long-term diabetes control (e.g.,
glycosylated hemoglobin levels), hemostatic markers, or lipid profile (138,139).
i. Non-insulin dependent 1 2
ii. Insulin dependent 1 2
c. Nephropathy, retinopathy, or
neuropathy
1 2 —
d. Other vascular disease or diabetes
of >20 years’ duration
1 2 —
Thyroid disorders
a. Simple goiter 1 1 —
b. Hyperthyroid 1 1 —
c. Hypothyroid 1 1 —
Gastrointestinal Conditions
Inflammatory bowel disease
(ulcerative colitis or Crohn’s disease)
1 1 Evidence: Although two case reports described three women with IBD
who experienced exacerbation of disease 5 days–25 months after LNG-IUD
insertion, no comparative studies have examined the safety of IUD use
among women with IBD (140).
Gallbladder disease
a. Symptomatic
i. Treated by cholecystectomy 1 2 —
ii. Medically treated 1 2
—
iii. Current 1 2 —
b. Asymptomatic 1 2 —
History of cholestasis
a. Pregnancy related 1 1 —
b. Past COC related 1 2 Comment: Concern exists that history of COC related cholestasis might
predict subsequent cholestasis with LNG use. Whether risk exists with use of
LNG-IUD is unclear.
Viral hepatitis
a. Acute or flare 1 1 —
b. Carrier 1 1 —
c. Chronic 1 1 —
Cirrhosis
Severe cirrhosis is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Mild (compensated) 1 1 —
b. Severe (decompensated) 1 3 —
See table footnotes on page 30.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 29
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
Liver tumors
Hepatocellular adenoma and
malignant liver tumors are associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Benign
i. Focal nodular hyperplasia 1 2 —
ii. Hepatocellular adenoma 1 3 Comment: No evidence is available about hormonal contraceptive use
in women with hepatocellular adenoma. COC use in healthy women is
associated with development and growth of hepatocellular adenoma;
whether other hormonal contraceptives have similar effects is not known.
b. Malignant (hepatoma) 1 3 —
Respiratory Conditions
Cystic fibrosis
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 Clarification: Persons with cystic fibrosis are at increased risk for diabetes,
liver disease, gallbladder disease, and VTE (particularly related to use of
central venous catheters) and are frequently prescribed antibiotics. Categories
assigned to such conditions in U.S. MEC should be the same for women with
cystic fibrosis who have these conditions. For cystic fibrosis, classifications
are based on the assumption that no other conditions are present; these
classifications must be modified in the presence of such conditions.
Anemias
Thalassemia 2 1 Comment: Concern exists about an increased risk for blood loss with Cu-IUDs.
Sickle cell disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
2 1 Comment: Concern exists about an increased risk for blood loss with Cu-IUDs.
Iron deficiency anemia 2 1 Comment: Concern exists about an increased risk for blood loss with Cu-IUDs.
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation Evidence: No comparative studies have examined IUD use among transplant
patients. Four case reports of transplant patients using IUDs provided
inconsistent results, including beneficial effects and contraceptive failures (141).
a. Complicated: graft failure (acute
or chronic), rejection, or cardiac
allograft vasculopathy
3 2 3 2
b. Uncomplicated 2 2 2 2
Drug Interactions
Antiretroviral therapy Initiation Continuation Initiation Continuation Clarification: No known interaction exists between ARV therapy and IUD
use. However, IUD insertion is classified as category 2 if the woman is not
clinically well or not receiving ARV therapy. Otherwise, both insertion and
continuation are classified as category 1 (see HIV Infection section).
a. Nucleoside reverse transcriptase
inhibitors (NRTIs)
i. Abacavir (ABC) 1/2 1 1/2 1 —
ii. Tenofovir (TDF) 1/2 1 1/2 1 —
iii. Zidovudine (AZT) 1/2 1 1/2 1 —
iv. Lamivudine (3TC) 1/2 1 1/2
1 —
v. Didanosine (DDI) 1/2 1 1/2 1 —
vi. Emtricitabine (FTC) 1/2 1 1/2 1 —
vii. Stavudine (D4T) 1/2 1 1/2 1 —
b. Nonnucleoside reverse
transcriptase inhibitors (NNRTIs)
i. Efavirenz (EFV) 1/2 1 1/2 1 —
ii. Etravirine (ETR) 1/2 1 1/2 1 —
iii. Nevirapine (NVP) 1/2 1 1/2 1 —
iv. Rilpivirine (RPV) 1/2 1 1/2 1 —
c. Ritonavir-boosted protease
inhibitors
i. Ritonavir-boosted atazanavir (ATV/r) 1/2 1 1/2 1 —
ii. Ritonavir-boosted darunavir (DRV/r) 1/2 1 1/2 1 —
See table footnotes on page 30.

Recommendations and Reports
30 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE B1. (Continued) Classifications for intrauterine devices, including the copper-containing intrauterine device and levonorgestrel-
releasing intrauterine device
Condition
Category
Clarifications/Evidence/CommentsCu-IUD LNG-IUD
iii. Ritonavir-boosted
fosamprenavir (FPV/r)
1/2 1 1/2 1 —
iv. Ritonavir-boosted lopinavir (LPV/r) 1/2 1 1/2 1 —
v. Ritonavir-boosted saquinavir (SQV/r) 1/2 1 1/2 1 —
vi. Ritonavir-boosted tipranavir (TPV/r) 1/2 1 1/2 1 —
d. Protease inhibitors without
ritonavir
i. Atazanavir (ATV) 1/2 1 1/2 1 —
ii. Fosamprenavir (FPV) 1/2 1 1/2 1 —
iii. Indinavir (IDV) 1/2 1 1/2 1 —
iv. Nelfinavir (NFV) 1/2 1 1/2 1 —
e. CCR5 co-receptor antagonists
i. Maraviroc (MVC) 1/2 1 1/2 1 —
f. HIV integrase strand transfer
inhibitors
i. Raltegravir (RAL) 1/2 1 1/2 1 —
ii. Dolutegravir (DTG) 1/2 1 1/2 1 —
iii. Elvitegravir (EVG) 1/2 1 1/2 1 —
g. Fusion inhibitors
i. Enfuvirtide 1/2 1 1/2 1 —
Anticonvulsant therapy
a. Certain anticonvulsants
(phenytoin, carbamazepine,
barbiturates, primidone, topiramate,
and oxcarbazepine)
1 1 Evidence: Limited evidence suggests use of certain anticonvulsants does not
interfere with the contraceptive effectiveness of the LNG-IUD (142).
b. Lamotrigine 1 1 Evidence: No drug interactions have been reported among women with epilepsy
who are receiving lamotrigine and using the LNG-IUD (143).
Antimicrobial therapy
a. Broad-spectrum antibiotics 1 1 —
b. Antifungals 1 1 —
c. Antiparasitics 1 1 —
d. Rifampin or rifabutin therapy 1 1 Evidence: One cross-sectional survey found that rifabutin had no impact on
the effectiveness of the LNG-IUD (142
).
Psychotropic medications Comment: For many common psychotropic agents, limited or no theoretical
concern exists for clinically significant drug interactions when co-administered
with hormonal contraceptives. However, either no or very limited data exist
examining potential interactions for these classes of medications.
a. SSRIs 1 1 —
St. John’s wort 1 1 —
Abbreviations: ARV=antiretroviral; BMI=body mass index; COC=combined oral contraceptive; Cu-IUD=copper-containing IUD; DVT=deep venous thrombosis; hCG=human chorionic
gonadotropin; HDL= high-density lipoprotein; HIV =human immunodeficiency virus; IBD= inflammatory bowel disease; IUD =intrauterine device; LDL =low-density lipoprotein;
LNG=levonorgestrel; LNG-IUD=levonorgestrel-releasing IUD; PE=pulmonary embolism; PID=pelvic inflammatory disease; POC=progestin-only contraceptive; SLE=systemic lupus
erythematosus; SSRI = selective serotonin reuptake inhibitor; STD=sexually transmitted disease; VTE = venous thromboembolism.
References
1. Cramer DW, Schiff I, Schoenbaum SC, et al. Tubal infertility and the
intrauterine device. N Engl J Med 1985;312:941–7. http://dx.doi.
org/10.1056/NEJM198504113121502
2. Daling JR, Weiss NS, Metch BJ, et al. Primary tubal infertility in relation
to the use of an intrauterine device. N Engl J Med 1985;312:937–41.
http://dx.doi.org/10.1056/NEJM198504113121501
3. Daling JR, Weiss NS, Voigt LF, McKnight B, Moore DE. The intrauterine
device and primary tubal infertility. N Engl J Med 1992;326:203–4.
http://dx.doi.org/10.1056/NEJM199201163260314
4. Delbarge W, Bátár I, Bafort M, et al. Return to fertility in nulliparous
and parous women after removal of the GyneFix intrauterine contraceptive
system. Eur J Contracept Reprod Health Care 2002;7:24–30. http://
dx.doi.org/10.1080/ejc.7.1.24.30
5. Doll H, Vessey M, Painter R. Return of fertility in nulliparous women
after discontinuation of the intrauterine device: comparison with women
discontinuing other methods of contraception. BJOG 2001;108:304–14.
http://dx.doi.org/10.1111/j.1471-0528.2001.00075.x
6. Hubacher D, Lara-Ricalde R, Taylor DJ, Guerra-Infante F, Guzmán-
Rodríguez R. Use of copper intrauterine devices and the risk of tubal
infertility among nulligravid women. N Engl J Med 2001;345:561–7.
http://dx.doi.org/10.1056/NEJMoa010438
7. Skjeldestad FE, Bratt H. Return of fertility after use of IUDs (Nova-T,
MLCu250 and MLCu375). Adv Contracept 1987;3:139–45. http://
dx.doi.org/10.1007/BF01890702
8. Urbach DR, Marrett LD, Kung R, Cohen MM. Association of
perforation of the appendix with female tubal infertility. Am J Epidemiol
2001;153:566–71. http://dx.doi.org/10.1093/aje/153.6.566
9. Wilson JC. A prospective New Zealand study of fertility after removal
of copper intrauterine contraceptive devices for conception and because
of complications: a four-year study. Am J Obstet Gynecol 1989;160:391–
6. http://dx.doi.org/10.1016/0002-9378(89)90455-9
10. US Department of Health and Human Services. Healthy people 2020:
Maternal, infant, and child health objectives. Washington, DC: US
Department of Health and Human Services; 2015. http://www.
healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-
child-health/objectives
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 31
US Department of Health and Human Services/Centers for Disease Control and Prevention
28. Eroğlu K, Akkuzu G, Vural G, et al. Comparison of efficacy and
complications of IUD insertion in immediate postplacental/early
postpartum period with interval period: 1 year follow-up. Contraception
2006;74:376–81.http://dx.doi.org/10.1016/j.contraception.2006.07.003
29. Gueye M, Gaye YF, Diouf AA, et al. Trancesarean intra-uterine device.
Pilot study performed at Dakar teaching hospital. [French]. J Gynecol
Obstet Biol Reprod (Paris) 2013;42:585–90.http://dx.doi.org/10.1016/j.
jgyn.2013.06.003
30. Gupta S, Malik S, Sinha R, Shyamsunder S, Mittal MK. Association of
the Position of the Copper T 380A as Determined by the Ultrasonography
Following its Insertion in the Immediate Postpartum Period with the
Subsequent Complications: An Observational Study. J Obstet Gynaecol
India 2014;64:349–53.http://dx.doi.org/10.1007/s13224-014-0532-5
31. Hagbard L, Ingemanson CA, Sorbe B. Early postpartum insertion
of copper IUD. Contraception 1978;17:355–63.http://dx.doi.
org/10.1016/0010-7824(78)90081-1
32. Hayes JL, Cwiak C, Goedken P, Zieman M. A pilot clinical trial of
ultrasound-guided postplacental insertion of a levonorgestrel intrauterine
device. Contraception 2007;76:292–6.http://dx.doi.org/10.1016/j.
contraception.2007.06.003
33. Jatlaoui TC, Marcus M, Jamieson DJ, Goedken P, Cwiak C. Postplacental
intrauterine device insertion at a teaching hospital. Contraception
2014;89:528–33.http://dx.doi.org/10.1016/j.contraception.2013.10.008
34. Kumar S, Sethi R, Balasubramaniam S, et al. Women’s experience with
postpartum intrauterine contraceptive device use in India. Reprod Health
2014;11:32.http://dx.doi.org/10.1186/1742-4755-11-32
35. Laes E, Lehtovirta P, Weintraub D, Pyörälä T, Luukkainen T. Early
puerperal insertions of copper-T-200. Contraception 1975;11:289–95.
http://dx.doi.org/10.1016/0010-7824(75)90037-2
36. Lara Ricalde R, Menocal Tobías G, Ramos Pérez C, Velázquez Ramírez
N. [Random comparative study between intrauterine device Multiload
Cu375 and TCu 380a inserted in the postpartum period]. Ginecol
Obstet Mex 2006;74:306–11.
37. Lavin P, Bravo C, Waszak C. Comparison of T Cu 200 and Progestasert
IUDs. Contracept Deliv Syst 1983;4:143–7.
38. Lavin P, Waszak C, Bravo C. Preliminary report on a postpartum CuT
200 study, Santiago, Chile. Int J Gynaecol Obstet 1983;21:71–5.http://
dx.doi.org/10.1016/0020-7292(83)90073-5
39. Lester F, Kakaire O, Byamugisha J, et al. Intracesarean insertion of the Copper
T380A versus 6 weeks postcesarean: a randomized clinical trial. Contraception
2015;91:198–203.http://dx.doi.org/10.1016/j.contraception.2014.12.002
40. Letti Müller AL, Lopes Ramos JG, Martins-Costa SH, et al. Transvaginal
ultrasonographic assessment of the expulsion rate of intrauterine devices
inserted in the immediate postpartum period: a pilot study. Contraception
2005;72:192–5.http://dx.doi.org/10.1016/j.contraception.2005.03.014
41. Levi E, Cantillo E, Ades V, Banks E, Murthy A. Immediate postplacental
IUD insertion at cesarean delivery: a prospective cohort study. Contraception
2012;86:102–5.http://dx.doi.org/10.1016/j.contraception.2011.11.019
42. Levi EE, Stuart GS, Zerden ML, Garrett JM, Bryant AG. Intrauterine
device placement during cesarean delivery and continued use 6 months
postpartum: a randomized controlled trial. Obstet Gynecol 2015;126:5–
11.http://dx.doi.org/10.1097/AOG.0000000000000882
43. Mishra S. Evaluation of Safety, Efficacy, and Expulsion of Post-Placental
and Intra-Cesarean Insertion of Intrauterine Contraceptive Devices
(PPIUCD). J Obstet Gynaecol India 2014;64:337–43.http://dx.doi.
org/10.1007/s13224-014-0550-3
44. Morrison C, Waszak C, Katz K, Diabaté F, Mate EM. Clinical outcomes
of two early postpartum IUD insertion programs in Africa. Contraception
1996;53:17–21.http://dx.doi.org/10.1016/0010-7824(95)00254-5
45. Nelson AL, Chen S, Eden R. Intraoperative placement of the Copper
T-380 intrauterine devices in women undergoing elective cesarean
delivery: a pilot study. Contraception 2009;80:81–3.http://dx.doi.
org/10.1016/j.contraception.2009.01.014
11. Annus J, Brat T, Diethelm MP, et al.; World Health Organization Special.
Comparative multicentre trial of three IUDs inserted immediately
following delivery of the placenta. Contraception 1980;22:9–18.http://
dx.doi.org/10.1016/0010-7824(80)90112-2
12. Apelo RA, Waszak CS. Postpartum IUD insertions in Manila,
Philippines. Adv Contracept 1985;1:319–28.
13. Baldwin MK, Edelman AB, Lim JY, Nichols MD, Bednarek PH, Jensen
JT. Intrauterine device placement at 3 versus 6weeks postpartum: a
randomized trial. Contraception 2016;93:356–63.http://dx.doi.
org/10.1016/j.contraception.2015.12.006
14. Bonilla Rosales F, Aguilar Zamudio ME, Cázares Montero ML,
Hernández Ortiz ME, Luna Ruiz MA. [Factors for expulsion of
intrauterine device Tcu380A applied immediately postpartum and after
a delayed period]. Rev Med Inst Mex Seguro Soc 2005;43:5–10.
15. Braniff K, Gomez E, Muller R. A randomised clinical trial to assess
satisfaction with the levonorgestrel- releasing intrauterine system inserted
at caesarean section compared to postpartum placement. Aust N Z J
Obstet Gynaecol 2015;55:279–83.http://dx.doi.org/10.1111/ajo.12335
16. Bryant AG, Kamanga G, Stuart GS, Haddad LB, Meguid T, Mhango C.
Immediate postpartum versus 6-week postpartum intrauterine device
insertion: a feasibility study of a randomized controlled trial. Afr J Reprod
Health 2013;17:72–9.
17. Caliskan E, Ozturk N, Dilbaz BO, Dilbaz S. Analysis of risk factors
associated with uterine perforation by intrauterine devices. Eur J Contracep
Reprod 2003;8:150–5.
18. Çelen S, Möröy P, Sucak A, Aktulay A, Danişman N. Clinical outcomes of early
postplacental insertion of intrauterine contraceptive devices. Contraception
2004;69:279–82.http://dx.doi.org/10.1016/j.contraception.2003.12.004
19. Çelen Ş, Sucak A, Yıldız Y, Danışman N. Immediate postplacental insertion
of an intrauterine contraceptive device during cesarean section. Contraception
2011;84:240–3.http://dx.doi.org/10.1016/j.contraception.2011.01.006
20. Chen BA, Reeves MF, Hayes JL, Hohmann HL, Perriera LK, Creinin
MD. Postplacental or delayed insertion of the levonorgestrel intrauterine
device after vaginal delivery: a randomized controlled trial. Obstet Gynecol
2010;116:1079–87.http://dx.doi.org/10.1097/AOG.0b013e3181f73fac
21. Chen JH, Wu SC, Shao WQ, et al. The comparative trial of TCu 380A IUD
and progesterone-releasing vaginal ring used by lactating women. Contraception
1998;57:371–9.http://dx.doi.org/10.1016/S0010-7824(98)00043-2
22. Cohen R, Sheeder J, Arango N, Teal SB, Tocce K. Twelve-month
contraceptive continuation and repeat pregnancy among young mothers
choosing postdelivery contraceptive implants or postplacental
intrauterine devices. Contraception 2016;93:178–83.http://dx.doi.
org/10.1016/j.contraception.2015.10.001
23. Dahlke JD, Terpstra ER, Ramseyer AM, Busch JM, Rieg T, Magann EF.
Postpartum insertion of levonorgestrel—intrauterine system at three
time periods: a prospective randomized pilot study. Contraception
2011;84:244–8.http://dx.doi.org/10.1016/j.contraception.2011.01.007
24. Dias T, Abeykoon S, Kumarasiri S, Gunawardena C, Padeniya T,
D’Antonio F. Use of ultrasound in predicting success of intrauterine
contraceptive device insertion immediately after delivery. Ultrasound
Obstet Gynecol 2015;46:104–8.
25. Elsedeek MS. Puerperal and menstrual bleeding patterns with different
types of contraceptive device fitted during elective cesarean delivery. Int
J Gynaecol Obstet 2012;116:31–4.http://dx.doi.org/10.1016/j.
ijgo.2011.07.036
26. Elsedeek MS. Five-year follow-up of two types of contraceptive device
fitted during elective cesarean delivery. Int J Gynaecol Obstet
2015;130:179–82.http://dx.doi.org/10.1016/j.ijgo.2015.02.031
27. El-Shafei MM, Mashali A, Hassan EO, El-Boghdad L, El-Lakkany N.
Postpartum and postabortion intrauterine device insertion unmet needs
of safe reproductive health: three years experience of Mansoura University
Hospital. J Egypt Soc Obstet Gynecol 2000;26:253–62.
Recommendations and Reports
32 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
46. Newton J, Harper M, Chan KK. Immediate post-placental insertion of
intrauterine contraceptive devices. Lancet 1977;310:272–4.http://
dx.doi.org/10.1016/S0140-6736(77)90955-2
47. Prema K, Gayathri TL, Philips FS. Comparative study of early
postpartum, postabortal and interval insertion of Cu T 200 mm2 device.
J Obstet Gynaecol India 1978;28:946–8.
48. Puzey M. Mirena at caesarean section. Eur J Contracep Reprod
2005;10:164–7.
49. Ragab A, Hamed HO, Alsammani MA, et al. Expulsion of Nova-T380,
Multiload 375, and Copper-T380A contraceptive devices inserted during
cesarean delivery. Int J Gynaecol Obstet 2015;130:174–8.http://dx.doi.
org/10.1016/j.ijgo.2015.03.025
50. Shukla M, Qureshi S; Chandrawati. Post-placental intrauterine device
insertion—a five year experience at a tertiary care centre in north India.
Indian J Med Res 2012;136:432–5.
51. Singal S, Bharti R, Dewan R, et al. Clinical Outcome of Postplacental
Copper T 380A Insertion in Women Delivering by Caesarean Section.
J Clin Diagn Res 2014;8:OC01–04.
52. Stuart GS, Bryant AG, O’Neill E, Doherty IA. Feasibility of postpartum
placement of the levonorgestrel intrauterine system more than 6 h after
vaginal birth. Contraception 2012;85:359–62.http://dx.doi.
org/10.1016/j.contraception.2011.08.005
53. Stuart GS, Lesko CR, Stuebe AM, Bryant AG, Levi EE, Danvers AI. A
randomized trial of levonorgestrel intrauterine system insertion 6 to 48 h
compared to 6 weeks after vaginal delivery; lessons learned. Contraception
2015;91:284–8.http://dx.doi.org/10.1016/j.contraception.2014.12.009
54. Thiery M, Van Kets H, Van der Pas H. Immediate post-placental IUD
insertion: the expulsion problem. Contraception 1985;31:331–49.http://
dx.doi.org/10.1016/0010-7824(85)90002-2
55. Van Der Pas MT, Delbeke L, Van Dets H. Comparative performance of
two copper-wired IUDs (ML Cu 250 and T Cu 200: immediate postpartum
and interval insertion. Contracept Deliv Syst 1980;1:27–35.
56. Welkovic S, Costa LO, Faúndes A, de Alencar Ximenes R, Costa CF. Post-partum
bleeding and infection after post-placental IUD insertion. Contraception
2001;63:155–8.http://dx.doi.org/10.1016/S0010-7824(01)00180-9
57. Whitaker AK, Endres LK, Mistretta SQ, Gilliam ML. Postplacental
insertion of the levonorgestrel intrauterine device after cesarean delivery
vs. delayed insertion: a randomized controlled trial. Contraception
2014;89:534–9.http://dx.doi.org/10.1016/j.contraception.2013.12.007
58. Woo CJ, Alamgir H, Potter JE. Women’s experiences after Planned Parenthood’s
exclusion from a family planning program in Texas. Contraception 2016;93:298–
302.http://dx.doi.org/10.1016/j.contraception.2015.12.004
59. Wu SC; Research Group on Failure Causes and Prevention Measures of
Intrauterine Device. [Efficacy of intrauterine device TCu380A when inserted
in four different periods]. Zhonghua Fu Chan Ke Za Zhi 2009;44:431–5.
60. Xu J, Yang X, Gu X, et al. Comparison between two techniques used in
immediate postplacental insertion of TCu 380A intrauterine device:
36-month follow-up. Reprod Contracept 1999;10:156–62.
61. Xu J, Zhuang L, Yu G. [Comparison of two techniques used in immediate
postplacental insertion of TCu 380A intrauterine device: 12 month follow-
up of 910 cases]. Zhonghua Fu Chan Ke Za Zhi 1997;32:354–7.
62. Xu JX, Rivera R, Dunson TR, et al. A comparative study of two techniques
used in immediate postplacental insertion (IPPI) of the Copper T-380A
IUD in Shanghai, People’s Republic of China. Contraception 1996;54:33–
8.http://dx.doi.org/10.1016/0010-7824(96)00117-5
63. Braniff K, Gomez E, Muller R. A randomised clinical trial to assess
satisfaction with the levonorgestrel- releasing intrauterine system inserted
at caesarean section compared to postpartum placement. Aust N Z J
Obstet Gynaecol 2015;55:279–83. http://dx.doi.org/10.1111/ajo.12335
64. Phillips SJ, Tepper NK, Kapp N, Nanda K, Temmerman M, Curtis KM.
Progestogen-only contraceptive use among breastfeeding women: a
systematic review. Contraception 2015;S0010-7824(15)00585-5.
65. Berry-Bibee E, Tepper N, Jatlaoui T, Whiteman M, Jamieson D,
Curtis K. The safety of intrauterine devices in breastfeeding women: a
systematic review. Contraception. In press 2016.
66. Steenland MW, Tepper NK, Curtis KM, Kapp N. Intrauterine
contraceptive insertion postabortion: a systematic review. Contraception
2011;84:447–64. http://dx.doi.org/10.1016/j.contraception.2011.03.007
67. World Health Organization Collaborative Study of Cardiovascular
Disease and Steroid Hormone Contraception. Cardiovascular disease
and use of oral and injectable progestogen-only contraceptives and
combined injectable contraceptives. Results of an international,
multicenter, case-control study. Contraception 1998;57:315–24. http://
dx.doi.org/10.1016/S0010-7824(98)00041-9.
68. Heinemann LA, Assmann A, DoMinh T, Garbe E. Oral progestogen-
only contraceptives and cardiovascular risk: results from the Transnational
Study on Oral Contraceptives and the Health of Young Women. Eur J
Contracept Reprod Health Care 1999;4:67–73. http://dx.doi.
org/10.3109/13625189909064007
69. Vasilakis C, Jick H, del Mar Melero-Montes M. Risk of idiopathic venous
thromboembolism in users of progestagens alone. Lancet 1999;354:1610–
1. http://dx.doi.org/10.1016/S0140-6736(99)04394-9
70. Kingman CE, Kadir RA, Lee CA, Economides DL. The use of
levonorgestrel-releasing intrauterine system for treatment of menorrhagia
in women with inherited bleeding disorders. BJOG 2004;111:1425–8.
http://dx.doi.org/10.1111/j.1471-0528.2004.00305.x
71. Lukes AS, Reardon B, Arepally G. Use of the levonorgestrel-releasing
intrauterine system in women with hemostatic disorders. Fertil Steril
2008;90:673–7. http://dx.doi.org/10.1016/j.fertnstert.2007.07.1315
72. Pisoni CN, Cuadrado MJ, Khamashta MA, Hunt BJ. Treatment of
menorrhagia associated with oral anticoagulation: efficacy and safety of
the levonorgestrel releasing intrauterine device (Mirena coil). Lupus
2006;15:877–80. http://dx.doi.org/10.1177/0961203306071706
73. Schaedel ZE, Dolan G, Powell MC. The use of the levonorgestrel-
releasing intrauterine system in the management of menorrhagia in
women with hemostatic disorders. Am J Obstet Gynecol 2005;193:1361–
3. http://dx.doi.org/10.1016/j.ajog.2005.05.002
74. Wilson W, Taubert KA, Gewitz M, et al; American Heart Association
Rheumatic Fever, Endocarditis, and Kawasaki Disease Committee;
American Heart Association Council on Cardiovascular Disease in the
Young; American Heart Association Council on Clinical Cardiology;
American Heart Association Council on Cardiovascular Surgery and
Anesthesia; Quality of Care and Outcomes Research Interdisciplinary
Working Group. Prevention of infective endocarditis: guidelines from
the American Heart Association: a guideline from the American Heart
Association Rheumatic Fever, Endocarditis, and Kawasaki Disease
Committee, Council on Cardiovascular Disease in the Young, and the
Council on Clinical Cardiology, Council on Cardiovascular Surgery and
Anesthesia, and the Quality of Care and Outcomes Research
Interdisciplinary Working Group. Circulation 2007;116:1736–54.
http://dx.doi.org/10.1161/CIRCULATIONAHA.106.183095
75. Tepper NK, Paulen ME, Marchbanks PA, Curtis KM. Safety of
contraceptive use among women with peripartum cardiomyopathy: a
systematic review. Contraception 2010;82:95–101. http://dx.doi.
org/10.1016/j.contraception.2010.02.004
76. The Criteria Committee of the New York Heart Association.
Nomenclature and criteria for diagnosis of diseases of the heart and great
vessels. 9th ed. Boston, MA: Little, Brown and Co; 1994.
77. Bernatsky S, Clarke A, Ramsey-Goldman R, et al. Hormonal exposures
and breast cancer in a sample of women with systemic lupus
erythematosus. Rheumatology (Oxford) 2004;43:1178–81. http://
dx.doi.org/10.1093/rheumatology/keh282
78. Bernatsky S, Ramsey-Goldman R, Gordon C, et al. Factors associated
with abnormal Pap results in systemic lupus erythematosus.
Rheumatology (Oxford) 2004;43:1386–9. http://dx.doi.org/10.1093/
rheumatology/keh331
79. Chopra N, Koren S, Greer WL, et al. Factor V Leiden, prothrombin
gene mutation, and thrombosis risk in patients with antiphospholipid
antibodies. J Rheumatol 2002;29:1683–8.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 33
US Department of Health and Human Services/Centers for Disease Control and Prevention
80. Esdaile JM, Abrahamowicz M, Grodzicky T, et al. Traditional Framingham
risk factors fail to fully account for accelerated atherosclerosis in systemic
lupus erythematosus. Arthritis Rheum 2001;44:2331–7. http://dx.doi.
org/10.1002/1529-0131(200110)44:10<2331::AID-ART395≥3.0.CO;2-I
81. Julkunen HA, Kaaja R, Friman C. Contraceptive practice in women
with systemic lupus erythematosus. Br J Rheumatol 1993;32:227–30.
http://dx.doi.org/10.1093/rheumatology/32.3.227
82. Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of
myocardial infarction and angina in women with systemic lupus
erythematosus: comparison with the Framingham Study. Am J Epidemiol
1997;145:408–15. http://dx.doi.org/10.1093/oxfordjournals.aje.
a009122
83. McAlindon T, Giannotta L, Taub N, D’Cruz D, Hughes G. Environmental
factors predicting nephritis in systemic lupus erythematosus. Ann Rheum
Dis 1993;52:720–4. http://dx.doi.org/10.1136/ard.52.10.720
84. McDonald J, Stewart J, Urowitz MB, Gladman DD. Peripheral vascular
disease in patients with systemic lupus erythematosus. Ann Rheum Dis
1992;51:56–60. http://dx.doi.org/10.1136/ard.51.1.56
85. Mintz G, Gutiérrez G, Delezé M, Rodríguez E. Contraception with
progestagens in systemic lupus erythematosus. Contraception
1984;30:29–38. http://dx.doi.org/10.1016/0010-7824(84)90076-3
86. Petri M. Musculoskeletal complications of systemic lupus erythematosus
in the Hopkins Lupus Cohort: an update. Arthritis Care Res
1995;8:137–45. http://dx.doi.org/10.1002/art.1790080305
87. Petri M. Lupus in Baltimore: evidence-based ‘clinical pearls’ from the
Hopkins Lupus Cohort. Lupus 2005;14:970–3. http://dx.doi.
org/10.1191/0961203305lu2230xx
88. Sánchez-Guerrero J, Uribe AG, Jiménez-Santana L, et al. A trial of
contraceptive methods in women with systemic lupus erythematosus. N
Engl J Med 2005;353:2539–49. http://dx.doi.org/10.1056/NEJMoa050817
89. Sarabi ZS, Chang E, Bobba R, et al. Incidence rates of arterial and venous
thrombosis after diagnosis of systemic lupus erythematosus. Arthritis
Rheum 2005;53:609–12. http://dx.doi.org/10.1002/art.21314
90. Somers E, Magder LS, Petri M. Antiphospholipid antibodies and
incidence of venous thrombosis in a cohort of patients with systemic
lupus erythematosus. J Rheumatol 2002;29:2531–6.
91. Urowitz MB, Bookman AA, Koehler BE, Gordon DA, Smythe HA, Ogryzlo
MA. The bimodal mortality pattern of systemic lupus erythematosus. Am J
Med 1976;60:221–5. http://dx.doi.org/10.1016/0002-9343(76)90431-9
92. Julkunen HA. Oral contraceptives in systemic lupus erythematosus:
side-effects and influence on the activity of SLE. Scand J Rheumatol
1991;20:427–33. http://dx.doi.org/10.3109/03009749109096822
93. Jungers P, Dougados M, Pélissier C, et al. Influence of oral contraceptive
therapy on the activity of systemic lupus erythematosus. Arthritis Rheum
1982;25:618–23. http://dx.doi.org/10.1002/art.1780250603
94. Petri M, Kim MY, Kalunian KC, et al; OC-SELENA Trial. Combined
oral contraceptives in women with systemic lupus erythematosus. N Engl
J Med 2005;353:2550–8. http://dx.doi.org/10.1056/NEJMoa051135
95. Choojitarom K, Verasertniyom O, Totemchokchyakarn K, Nantiruj K,
Sumethkul V, Janwityanujit S. Lupus nephritis and Raynaud’s
phenomenon are significant risk factors for vascular thrombosis in SLE
patients with positive antiphospholipid antibodies. Clin Rheumatol
2008;27:345–51. http://dx.doi.org/10.1007/s10067-007-0721-z
96. Wahl DG, Guillemin F, de Maistre E, Perret C, Lecompte T, Thibaut G.
Risk for venous thrombosis related to antiphospholipid antibodies in
systemic lupus erythematosus—a meta-analysis. Lupus 1997;6:467–73.
http://dx.doi.org/10.1177/096120339700600510
97. Tepper NK, Whiteman MK, Zapata LB, Marchbanks PA, Curtis KM. Safety
of hormonal contraceptives among women with migraine: a systematic review.
Contraception 2016. Epub May 3, 2016. http:// dx.doi.org/10.1016/j.
contraception.2016.04.016
98. Tepper NK, Whiteman MK, Marchbanks PA, James AH, Curtis KM.
Progestin-only contraception and thromboembolism: a systematic review.
Contraception 2016. Epub May 3, 2016. http://dx.doi.org/10.1016/j.
contraception.2016.04.014
99. Pagano HP, Zapata LB, Berry-Bibee EN, Nanda K, Curtis KM. Safety of
hormonal contraception and intrauterine devices among women with
depressive and bipolar disorders: a systematic review. Contraception 2016.
Epub June 27, 2016. http://dx.doi.org/10.1016/j.contraception.2016.06.012
100. Barrington JW, Arunkalaivanan AS, Abdel-Fattah M. Comparison between
the levonorgestrel intrauterine system (LNG-IUS) and thermal balloon
ablation in the treatment of menorrhagia. Eur J Obstet Gynecol Reprod Biol
2003;108:72–4. http://dx.doi.org/10.1016/S0301-2115(02)00408-6
101. Gupta B, Mittal S, Misra R, Deka D, Dadhwal V. Levonorgestrel-
releasing intrauterine system vs. transcervical endometrial resection for
dysfunctional uterine bleeding. Int J Gynaecol Obstet 2006;95:261–6.
http://dx.doi.org/10.1016/j.ijgo.2006.07.004
102. Hurskainen R, Teperi J, Rissanen P, et al. Quality of life and cost-
effectiveness of levonorgestrel-releasing intrauterine system versus
hysterectomy for treatment of menorrhagia: a randomised trial.[see
comment]. Lancet 2001;357:273–7. http://dx.doi.org/10.1016/
S0140-6736(00)03615-1
103. Istre O, Trolle B. Treatment of menorrhagia with the levonorgestrel
intrauterine system versus endometrial resection. Fertil Steril
2001;76:304–9. http://dx.doi.org/10.1016/S0015-0282(01)01909-4
104. Koh SC, Singh K. The effect of levonorgestrel-releasing intrauterine
system use on menstrual blood loss and the hemostatic, fibrinolytic/
inhibitor systems in women with menorrhagia. J Thromb Haemost
2007;5:133–8. http://dx.doi.org/10.1111/j.1538-7836.2006.02243.x
105. Lethaby AE, Cooke I, Rees M. Progesterone/progestogen releasing
intrauterine systems versus either placebo or any other medication for heavy
menstrual bleeding. Cochrane Database Syst Rev 2000;(2):CD002126.
106. Magalhães J, Aldrighi JM, de Lima GR. Uterine volume and menstrual
patterns in users of the levonorgestrel-releasing intrauterine system with
idiopathic menorrhagia or menorrhagia due to leiomyomas. Contraception
2007;75:193–8. http://dx.doi.org/10.1016/j.contraception.2006.11.004
107. Stewart A, Cummins C, Gold L, Jordan R, Phillips W. The
effectiveness of the levonorgestrel-releasing intrauterine system in
menorrhagia: a systematic review. BJOG 2001;108:74–86. http://
dx.doi.org/10.1111/j.1471-0528.2001.00020.x
108. Fedele L, Bianchi S, Zanconato G, Portuese A, Raffaelli R. Use of a
levonorgestrel-releasing intrauterine device in the treatment of
rectovaginal endometriosis. Fertil Steril 2001;75:485–8. http://dx.doi.
org/10.1016/S0015-0282(00)01759-3
109. Lockhat FBE, Emembolu J, Konje JC. The effect of a levonorgestrel intrauterine
system (LNG-IUS) on symptomatic endometriosis. Fertil Steril 2002;77(Suppl
1):S24. http://dx.doi.org/10.1016/S0015-0282(01)03086-2
110. Petta CA, Ferriani RA, Abrao MS, et al. Randomized clinical trial of a
levonorgestrel-releasing intrauterine system and a depot GnRH analogue for
the treatment of chronic pelvic pain in women with endometriosis. Hum
Reprod 2005;20:1993–8. http://dx.doi.org/10.1093/humrep/deh869
111. Vercellini P, Aimi G, Panazza S, De Giorgi O, Pesole A, Crosignani PG.
A levonorgestrel-releasing intrauterine system for the treatment of
dysmenorrhea associated with endometriosis: a pilot study. Fertil Steril
1999;72:505–8. http://dx.doi.org/10.1016/S0015-0282(99)00291-5
112. Vercellini P, Frontino G, De Giorgi O, Aimi G, Zaina B, Crosignani
PG. Comparison of a levonorgestrel-releasing intrauterine device versus
expectant management after conservative surgery for symptomatic
endometriosis: a pilot study. Fertil Steril 2003;80:305–9. http://dx.doi.
org/10.1016/S0015-0282(03)00608-3
113. Gaffield ME, Kapp N, Curtis KM. Combined oral contraceptive and
intrauterine device use among women with gestational trophoblastic
disease. Contraception 2009;80:363–71. http://dx.doi.org/10.1016/j.
contraception.2009.03.022
Recommendations and Reports
34 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
114. Whiteman MK, Zapata LB, Tepper NK, Marchbanks PA, Curtis KM.
Use of contraceptive methods among women with endometrial
hyperplasia: a systematic review. Contraception 2010;82:56–63. http://
dx.doi.org/10.1016/j.contraception.2010.02.005
115. Zapata LB, Whiteman MK, Tepper NK, Jamieson DJ, Marchbanks
PA, Curtis KM. Intrauterine device use among women with uterine
fibroids: a systematic review. Contraception 2010;82:41–55. http://
dx.doi.org/10.1016/j.contraception.2010.02.011
116. Tepper NK, Steenland MW, Gaffield ME, Marchbanks PA, Curtis
KM. Retention of intrauterine devices in women who acquire pelvic
inflammatory disease: a systematic review. Contraception 2013;87:655–
60. http://dx.doi.org/10.1016/j.contraception.2012.08.011
117. Faúndes A, Telles E, Cristofoletti ML, Faúndes D, Castro S, Hardy E.
The risk of inadvertent intrauterine device insertion in women carriers
of endocervical Chlamydia trachomatis. Contraception 1998;58:105–
9. http://dx.doi.org/10.1016/S0010-7824(98)00064-X
118. Ferraz do Lago R, Simões JA, Bahamondes L, Camargo RP, Perrotti M,
Monteiro I. Follow-up of users of intrauterine device with and without
bacterial vaginosis and other cervicovaginal infections. Contraception
2003;68:105–9. http://dx.doi.org/10.1016/S0010-7824(03)00109-4
119. Morrison CS, Sekadde-Kigondu C, Miller WC, Weiner DH, Sinei SK.
Use of sexually transmitted disease risk assessment algorithms for
selection of intrauterine device candidates. Contraception 1999;59:97–
106. http://dx.doi.org/10.1016/S0010-7824(99)00006-2
120. Pap-Akeson M, Solheim F, Thorbert G, Akerlund M. Genital tract infections
associated with the intrauterine contraceptive device can be reduced by
inserting the threads into the uterine cavity. Br J Obstet Gynaecol
1992;99:676–9. http://dx.doi.org/10.1111/j.1471-0528.1992.tb13854.x
121. Sinei SK, Schulz KFLP, Lamptey PR, et al. Preventing IUCD-related pelvic
infection: the efficacy of prophylactic doxycycline at insertion. Br J Obstet
Gynaecol 1990;97:412–9. http://dx.doi.org/10.1111/j.1471-0528.1990.
tb01828.x
122. Skjeldestad FE, Halvorsen LE, Kahn H, Nordbø SA, Saake K. IUD users
in Norway are at low risk for genital C. trachomatis infection. Contraception
1996;54:209–12. http://dx.doi.org/10.1016/S0010-7824(96)00190-4
123. Walsh TL, Bernstein GS, Grimes DA, Frezieres R, Bernstein L, Coulson AH;
IUD Study Group. Effect of prophylactic antibiotics on morbidity associated
with IUD insertion: results of a pilot randomized controlled trial. Contraception
1994;50:319–27. http://dx.doi.org/10.1016/0010-7824(94)90019-1
124. Workowski KA, Bolan GA. Sexually transmitted diseases treatment
guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-03).
125. Jatlaoui TC, Simmons KB, Curtis KM. The safety of intrauterine
contraception initiation among women with current asymptomatic cervical
infections or at increased risk of sexually transmitted infections.
Contraception 2016. Epub June 1, 2016. http://dx.doi.org/10.1016/j.
contraception.2016.05.013
126. Carael M, Van de Perre PH, Lepage PH, et al. Human immunodeficiency
virus transmission among heterosexual couples in Central Africa. AIDS
1988;2:201–5.
127. European Study Group on Heterosexual Transmission of HIV.
Comparison of female to male and male to female transmission of HIV
in 563 stable couples. BMJ 1992;304:809–13. http://dx.doi.
org/10.1136/bmj.304.6830.809
128. Kapiga SH, Lyamuya EF, Lwihula GK, Hunter DJ. The incidence of
HIV infection among women using family planning methods in Dar
es Salaam, Tanzania. AIDS 1998;12:75–84. http://dx.doi.
org/10.1097/00002030-199801000-00009.
129. Kapiga SH, Shao JF, Lwihula GK, Hunter DJ. Risk factors for HIV
infection among women in Dar-es-Salaam, Tanzania. J Acquir Immune
Defic Syndr 1994;7:301–9.
130. Mann JM, Nzilambi N, Piot P, et al. HIV infection and associated risk
factors in female prostitutes in Kinshasa, Zaire. AIDS 1988;2:249–54.
http://dx.doi.org/10.1097/00002030-198808000-00002
131. Martin HL Jr, Nyange PM, Richardson BA, et al. Hormonal
contraception, sexually transmitted diseases, and risk of heterosexual
transmission of human immunodeficiency virus type 1. J Infect Dis
1998;178:1053–9. http://dx.doi.org/10.1086/515654
132. Mali JK, Hunter DJ, Maggwa BN, Tukei PM. Contraceptive use and
the risk of HIV infection in Nairobi, Kenya. Int J Gynaecol Obstet
1995;48:61–7. http://dx.doi.org/10.1016/0020-7292(94)02214-3
133. Nicolosi A, Corrêa Leite ML, Musicco M, Arici C, Gavazzeni G,
Lazzarin A; Italian Study Group on HIV Heterosexual Transmission.
The efficiency of male-to-female and female-to-male sexual transmission
of the human immunodeficiency virus: a study of 730 stable couples.
[comment]. Epidemiology 1994;5:570–5. http://dx.doi.
org/10.1097/00001648-199411000-00003
134. Plourde PJ, Plummer FA, Pepin J, et al. Human immunodeficiency
virus type 1 infection in women attending a sexually transmitted
diseases clinic in Kenya.[comment]. J Infect Dis 1992;166:86–92.
http://dx.doi.org/10.1093/infdis/166.1.86
135. Sinei SK, Fortney JA, Kigondu CS, et al. Contraceptive use and HIV
infection in Kenyan family planning clinic attenders. Int J STD AIDS
1996;7:65–70. http://dx.doi.org/10.1258/0956462961917104
136. Spence MR, Robbins SM, Polansky M, Schable CA. Seroprevalence
of human immunodeficiency virus type I (HIV-1) antibodies in a
family-planning population. Sex Transm Dis 1991;18:143–5. http://
dx.doi.org/10.1097/00007435-199107000-00003
137. Tepper NK, Curtis KM, Nanda K, Jamieson DJ. Safety of intrauterine devices
among women with HIV: a systematic review. Contraception 2016. Epub
June 22, 2016. http://dx.doi.org/0.1016/j.contraception.2016.06.011
138. Grigoryan OR, Grodnitskaya EE, Andreeva EN, Shestakova MV,
Melnichenko GA, Dedov II. Contraception in perimenopausal women
with diabetes mellitus. Gynecol Endocrinol 2006;22:198–206. http://
dx.doi.org/10.1080/09513590600624317
139. Rogovskaya S, Rivera R, Grimes DA, et al. Effect of a levonorgestrel
intrauterine system on women with type 1 diabetes: a randomized trial.
Obstet Gynecol 2005;105:811–5. http://dx.doi.org/10.1097/01.
AOG.0000156301.11939.56
140. Zapata LB, Paulen ME, Cansino C, Marchbanks PA, Curtis KM.
Contraceptive use among women with inflammatory bowel disease: a
systematic review. Contraception 2010;82:72–85. http://dx.doi.
org/10.1016/j.contraception.2010.02.012
141. Paulen ME, Folger SG, Curtis KM, Jamieson DJ. Contraceptive use
among solid organ transplant patients: a systematic review.
Contraception 2010;82:102–12. http://dx.doi.org/10.1016/j.
contraception.2010.02.007
142. Bounds W, Guillebaud J. Observational series on women using the
contraceptive Mirena concurrently with anti-epileptic and other
enzyme-inducing drugs. J Fam Plann Reprod Health Care 2002;28:78–
80. http://dx.doi.org/10.1783/147118902101195992
143. Reimers A, Helde G, Brodtkorb E. Ethinyl estradiol, not progestogens,
reduces lamotrigine serum concentrations. Epilepsia 2005;46:1414–7.
http://dx.doi.org/10.1111/j.1528-1167.2005.10105.x

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 35
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix C
Classifications for Progestin-Only Contraceptives
Classifications for progestin-only contraceptives
(POCs) include those for progestin-only implants, depot
medroxyprogesterone acetate (DMPA; 150 mg intramuscularly
or 104 mg subcutaneously), and progestin-only pills (POPs) (Box
C1) (Table C1). POCs do not protect against sexually transmitted
diseases (STDs), including human immunodeficiency virus
(HIV), and women using these methods should be counseled
that consistent and correct use of the male latex condom reduces
the risk for transmission of HIV and other STDs. Use of female
condoms can provide protection from transmission of STDs,
although data are limited.
BOX C1. Categories for classifying progestin-only contraceptives
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.
TABLE C1. Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Personal Characteristics and Reproductive History
Pregnancy NA NA NA Clarification: Use of POCs is not required. No known harm to the
woman, the course of her pregnancy, or the fetus occurs if POCs
are inadvertently used during pregnancy. However, the relation
between DMPA use during pregnancy and its effects on the fetus
remains unclear.
Age Evidence: Most studies have found that women lose BMD
during DMPA use but recover BMD after discontinuation.
Limited evidence shows a weak association with fracture.
However, one large study suggests that women who choose
DMPA might be at higher risk for fracture before initiation
(1). It is unclear whether adult women with long durations of
DMPA use can regain BMD to baseline levels before entering
menopause and whether adolescents can reach peak bone
mass after discontinuation of DMPA. The relationship between
these changes in BMD during the reproductive years and future
fracture risk is unknown. Studies generally find no effect of
POCs other than DMPA on BMD (1–48).
a. Menarche to <18 years 1 2 1
b. 18–45 years 1 1 1
c. >45 years 1 2 1
Parity
a. Nulliparous 1 1 1 —
b. Parous 1 1 1 —
Breastfeeding
a. <21 days postpartum 2 2 2 Clarification: Breastfeeding provides important health benefits
for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially
breastfed, exclusively breastfed through 6 months of life, and
continuing breastfeeding through at least 1 year of life as key public
health goals (49).
Evidence: Two small, randomized controlled trials found no
adverse impact on breastfeeding with initiation of etonogestrel
implants within 48 hours postpartum. Other studies found
that initiation of POPs, injectables, and implants at ≤6
weeks postpartum compared with nonhormonal use had
no detrimental effect on breastfeeding outcomes or infant
health, growth, and development in the first year postpartum.
In general, these studies are of poor quality, lack standard
definitions of breastfeeding or outcome measures, and have not
included premature or ill infants (50,51).
Comment: Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding
difficulties, certain medical conditions, and certain perinatal
complications and those who deliver preterm. For these
women, as for all women, discussions about contraception for
breastfeeding women should include information about risks,
benefits, and alternatives.
See table footnotes on page 49.

Recommendations and Reports
36 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
b. 21 to <30 days postpartum Clarification: Breastfeeding provides important health benefits
for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially
breastfed, exclusively breastfed through 6 months of life, and
continuing breastfeeding through at least 1 year of life as key public
health goals (49).
Evidence: Two small, randomized controlled trials found no
adverse impact on breastfeeding with initiation of etonogestrel
implants within 48 hours postpartum. Other studies found
that initiation of POPs, injectables, and implants at ≤6
weeks postpartum compared with nonhormonal use had
no detrimental effect on breastfeeding outcomes or infant
health, growth, and development in the first year postpartum.
In general, these studies are of poor quality, lack standard
definitions of breastfeeding or outcome measures, and have not
included premature or ill infants (50,51).
Comment: Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding
difficulties, certain medical conditions, and certain perinatal
complications and those who deliver preterm. For these
women, as for all women, discussions about contraception for
breastfeeding women should include information about risks,
benefits, and alternatives.
i. With other risk factors for VTE
(e.g., age ≥35 years, previous
VTE, thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
2 2 2
ii. Without other risk factors for VTE 2 2 2
c. 30–42 days postpartum Clarification: Breastfeeding provides important health benefits
for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially
breastfed, exclusively breastfed through 6 months of life, and
continuing breastfeeding through at least 1 year of life as key public
health goals (49).
Evidence: Two small, randomized controlled trials found no
adverse impact on breastfeeding with initiation of etonogestrel
implants within 48 hours postpartum. Other studies found
that initiation of POPs, injectables, and implants at ≤6
weeks postpartum compared with nonhormonal use had
no detrimental effect on breastfeeding outcomes or infant
health, growth, and development in the first year postpartum.
In general, these studies are of poor quality, lack standard
definitions of breastfeeding or outcome measures, and have not
included premature or ill infants (50,51).
Comment: Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding
difficulties, certain medical conditions, and certain perinatal
complications and those who deliver preterm. For these
women, as for all women, discussions about contraception for
breastfeeding women should include information about risks,
benefits, and alternatives.
i. With other risk factors for VTE
(e.g., age ≥35 years, previous
VTE, thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
1 1 1
ii. Without other risk factors for VTE 1 1 1
d. >42 days postpartum 1 1 1 Clarification: Breastfeeding provides important health benefits
for mother and infant. The U.S. Department of Health and Human
Services recommends increasing the proportion of infants initially
breastfed, exclusively breastfed through 6 months of life, and
continuing breastfeeding through at least 1 year of life as key public
health goals (49).
Evidence: Overall, studies found that initiation of POPs,
injectables, and implants at >6 weeks postpartum compared
with nonhormonal use had no detrimental effect on
breastfeeding outcomes or infant health, growth, and
development in the first year postpartum. In general, these
studies are of poor quality, lack standard definitions of
breastfeeding or outcome measures, and have not included
premature or ill infants (51).
Comment: Certain women might be at risk for breastfeeding
difficulties, such as women with previous breastfeeding
difficulties, certain medical conditions, and certain perinatal
complications and those who deliver preterm. For these
women, as for all women, discussions about contraception for
breastfeeding women should include information about risks,
benefits, and alternatives.
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 37
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Postpartum (nonbreastfeeding
women)
a. <21 days postpartum 1 1 1 —
b. 21–42 days postpartum
i. With other risk factors for VTE
(e.g., age ≥35 years, previous
VTE, thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/
m
2
, postpartum hemorrhage,
postcesarean delivery,
preeclampsia, or smoking)
1 1 1 —
ii. Without other risk factors for VTE 1 1 1 —
c. >42 days postpartum 1 1 1 —
Postabortion
a. First trimester 1 1 1 Clarification: POCs may be started immediately postabortion.
Evidence: Limited evidence suggests that no adverse side effects
occur when implants (Norplant) or progestin-only injectables
(NET-EN) are initiated after first trimester abortion (52–55).
b. Second trimester 1 1 1 Clarification: POCs may be started immediately postabortion.
c. Immediate postseptic abortion 1 1 1 Clarification: POCs may be started immediately postabortion.
Past ectopic pregnancy 1 1 2 Comment: POP users have a higher absolute rate of ectopic
pregnancy than do users of other POCs but still lower than
women using no method.
History of pelvic surgery 1 1 1 —
Smoking
a. Age <35 years 1 1 1 —
b. Age ≥35 years
i. <15 cigarettes per day 1 1 1 —
ii. ≥15 cigarettes per day 1 1 1 —
Obesity —
a. BMI ≥30 kg/m
2
1 1 1 —
b. Menarche to <18 years and BMI
≥30 kg/m
2
1 2 1 Evidence: Among adult women, generally no association has
been found between baseline weight and weight gain among
DMPA users compared with nonusers. Evidence is mixed for
adolescent DMPA users, with some studies observing greater
weight gain among obese compared with normal weight
users but other studies showing no association; methodologic
differences across studies might account for the differences
in findings. Data on other POC methods and other adverse
outcomes including weight gain are limited (56–73).
History of bariatric surgery
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease
storage capacity of the stomach
(vertical banded gastroplasty,
laparoscopic adjustable gastric band,
or laparoscopic sleeve gastrectomy)
1 1 1 Evidence: Limited evidence demonstrated no substantial
decrease in effectiveness of oral contraceptives among women
who underwent laparoscopic placement of an adjustable
gastric band (74).
b. Malabsorptive procedures:
decrease absorption of nutrients
and calories by shortening the
functional length of the small
intestine (Roux-en-Y gastric bypass
or biliopancreatic diversion)
1 1 3 Evidence: Limited evidence demonstrated no substantial
decrease in effectiveness of oral contraceptives among women
who underwent a biliopancreatic diversion; however, evidence
from pharmacokinetic studies suggested conflicting results
regarding oral contraceptive effectiveness among women who
underwent a jejunoileal bypass (74).
Comment: Bariatric surgical procedures involving a
malabsorptive component have the potential to decrease
oral contraceptive effectiveness, perhaps further decreased
by postoperative complications such as long-term diarrhea,
vomiting, or both.
See table footnotes on page 49.

Recommendations and Reports
38 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Cardiovascular Disease
Multiple risk factors for
atherosclerotic cardiovascular
disease (e.g., older age, smoking,
diabetes, hypertension, low HDL, high
LDL, or high triglyceride levels)
2 3 2 Clarification: When multiple major risk factors exist, risk for
cardiovascular disease might increase substantially. Certain POCs
might increase the risk for thrombosis, although this increase
is substantially less than with COCs. The effects of DMPA might
persist for some time after discontinuation.
Clarification: The recommendations apply to known preexisting
medical conditions or characteristics. Few if any screening tests
are needed before initiation of contraception. See the U.S. Selected
Practice Recommendations for Contraceptive Use (http://www.cdc.
gov/reproductivehealth/unintendedpregnancy/usspr.htm).
Hypertension
Systolic blood pressure ≥160 mm Hg
or diastolic blood pressure ≥100 mm
Hg are associated with increased risk
for adverse health events as a result of
pregnancy (Box 2).
a. Adequately controlled
hypertension
1 2 1 Clarification: For all categories of hypertension, classifications
are based on the assumption that no other risk factors exist for
cardiovascular disease. When multiple risk factors do exist, risk
for cardiovascular disease might increase substantially. A single
reading of blood pressure level is not sufficient to classify a
woman as hypertensive.
Clarification: Women adequately treated for hypertension are
at lower risk for acute myocardial infarction and stroke than
are untreated women. Although no data exist, POC users with
adequately controlled and monitored hypertension should be
at lower risk for acute myocardial infarction and stroke than are
untreated hypertensive POC users.
b. Elevated blood pressure levels
(properly taken measurements)
Clarification: For all categories of hypertension, classifications
are based on the assumption that no other risk factors exist for
cardiovascular disease. When multiple risk factors do exist, risk
for cardiovascular disease might increase substantially. A single
reading of blood pressure level is not sufficient to classify a
woman as hypertensive.
Evidence: Limited evidence suggests that among women
with hypertension, those who used POPs or progestin-only
injectables had a small increased risk for cardiovascular events
compared with women who did not use these methods (75).
i. Systolic 140–159 mm Hg or
diastolic 90–99 mm Hg
1 2 1
ii. Systolic ≥160 mm Hg or diastolic
≥100 mm Hg
2 3 2
c. Vascular disease 2 3 2 Clarification: For all categories of hypertension, classifications
are based on the assumption that no other risk factors exist for
cardiovascular disease. When multiple risk factors do exist, risk
for cardiovascular disease might increase substantially. A single
reading of blood pressure level is not sufficient to classify a
woman as hypertensive.
Comment: Concern exists about hypoestrogenic effects
and reduced HDL levels, particularly among users of DMPA.
However, little concern exists about these effects with regard
to POPs. The effects of DMPA might persist for some time
after discontinuation.
History of high blood pressure
during pregnancy (when current
blood pressure is measurable
and normal)
1 1 1 —
Deep venous thrombosis/Pulmonary
embolism
a. History of DVT/PE, not receiving
anticoagulant therapy
See table footnotes on page 49.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 39
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
2 2 2 —
• History of estrogen-associated
DVT/PE
• Pregnancy-associated DVT/PE
• Idiopathic DVT/PE
• Known thrombophilia, including
antiphospholipid syndrome
• Active cancer (metastatic, receiving
therapy, or within 6 months after
clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
2 2 2 —
b. Acute DVT/PE 2 2 2 Evidence: No direct evidence exists on use of POCs among
women with acute DVT/PE. Although findings on the risk for
venous thrombosis with use of POCs in otherwise healthy
women is inconsistent, any small increased risk is substantially
less than that with COCs (75–77).
c. DVT/PE and established
anticoagulant therapy for at
least 3 months
Evidence: No direct evidence exists on use of POCs among
women with DVT/PE receiving anticoagulant therapy. Although
findings on the risk for venous thrombosis with use of POCs is
inconsistent in otherwise healthy women, any small increased
risk is substantially less than that with COCs (75–77).
Limited evidence indicates that intramuscular injections of
DMPA in women receiving chronic anticoagulation therapy does
not pose a significant risk for hematoma at the injection site or
increase the risk for heavy or irregular vaginal bleeding (78).
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
2 2 2
• Known thrombophilia, including
antiphospholipid syndrome
• Active cancer (metastatic, receiving
therapy, or within 6 months after
clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
2 2 2
d. Family history (first-degree
relatives)
1 1 1 —
e. Major surgery
i. With prolonged immobilization 2 2 2 —
ii. Without prolonged
immobilization
1 1 1 —
f. Minor surgery without
immobilization
1 1 1 —
Known thrombogenic mutations
(e.g., factor V Leiden; prothrombin
mutation; and protein S, protein C,
and antithrombin deficiencies)
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
2 2 2 Clarification: Routine screening is not appropriate because of
the rarity of the conditions and the high cost of screening.
Superficial venous disorders
a. Varicose veins 1 1 1 —
b. Superficial venous thrombosis
(acute or history)
1 1 1 —
Current and history of ischemic
heart disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation Comment: Concern exists about hypoestrogenic effects
and reduced HDL levels, particularly among users of DMPA.
However, little concern exists about these effects with regard
to POPs. The effects of DMPA might persist for some time
after discontinuation.
2 3 3 2 3
Stroke (history of cerebrovascular
accident)
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation Comment: Concern exists about hypoestrogenic effects
and reduced HDL levels, particularly among users of DMPA.
However, little concern exists about these effects with regard
to POPs. The effects of DMPA might persist for some time
after discontinuation.
2 3 3 2 3
Valvular heart disease
Complicated valvular heart disease
is associated with increased risk for
adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 —
See table footnotes on page 49.

Recommendations and Reports
40 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
b. Complicated (pulmonary
hypertension, risk for atrial
fibrillation, or history of subacute
bacterial endocarditis)
1 1 1 —
Peripartum cardiomyopathy
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Evidence: No direct evidence exists on the safety of POCs
among women with peripartum cardiomyopathy. Limited
indirect evidence from noncomparative studies of women
with cardiac disease demonstrated few cases of hypertension,
thromboembolism, and heart failure in women with cardiac
disease using POPs and DMPA (79).
Comment: Progestin-only implants might induce cardiac
arrhythmias in healthy women; women with peripartum
cardiomyopathy have a high incidence of cardiac arrhythmias.
a. Normal or mildly impaired cardiac
function (New York Heart Association
Functional Class I or II: patients
with no limitation of activities or
patients with slight, mild limitation
of activity) (80)
i. <6 months 1 1 1
ii. ≥6 months 1 1 1
b. Moderately or severely impaired
cardiac function (New York Heart
Association Functional Class III or IV:
patients with marked limitation of
activity or patients who should be at
complete rest) (80)
2 2 2
Rheumatic Diseases
Systemic lupus erythematosus
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Initiation Continuation
a. Positive (or unknown)
antiphospholipid antibodies
3 3 3 3 Clarification: Persons with SLE are at increased risk for ischemic
heart disease, stroke, and VTE. Categories assigned to such
conditions in U.S. MEC should be the same for women with SLE who
have these conditions. For all subconditions of SLE, classifications
are based on the assumption that no other risk factors for
cardiovascular disease are present; these classifications must be
modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive
methods, including hormonal contraceptives (81–99).
Evidence: Antiphospholipid antibodies are associated with a
higher risk for both arterial and venous thrombosis (100,101).
b. Severe thrombocytopenia 2 3 2 2 Clarification: Persons with SLE are at increased risk for ischemic
heart disease, stroke, and VTE. Categories assigned to such
conditions in U.S. MEC should be the same for women with SLE who
have these conditions. For all subconditions of SLE, classifications
are based on the assumption that no other risk factors for
cardiovascular disease are present; these classifications must be
modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive
methods, including hormonal contraceptives (81–99).
Comment: Severe thrombocytopenia increases the risk for
bleeding. POCs might be useful in treating menorrhagia
in women with severe thrombocytopenia. However, given
the increased or erratic bleeding that might be seen on
initiation of DMPA and its irreversibility for 11–13 weeks after
administration, initiation of this method in women with severe
thrombocytopenia should be done with caution.
c. Immunosuppressive therapy 2 2 2 2 Clarification: Persons with SLE are at increased risk for ischemic
heart disease, stroke, and VTE. Categories assigned to such
conditions in U.S. MEC should be the same for women with SLE who
have these conditions. For all subconditions of SLE, classifications
are based on the assumption that no other risk factors for
cardiovascular disease are present; these classifications must be
modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive
methods, including hormonal contraceptives (81–99).
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 41
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
. Initiation Continuation
d. None of the above 2 2 2 2 Clarification: Persons with SLE are at increased risk for ischemic
heart disease, stroke, and VTE. Categories assigned to such
conditions in U.S. MEC should be the same for women with SLE who
have these conditions. For all subconditions of SLE, classifications
are based on the assumption that no other risk factors for
cardiovascular disease are present; these classifications must be
modified in the presence of such risk factors. Many women with
SLE can be considered good candidates for most contraceptive
methods, including hormonal contraceptives (81–99).
Rheumatoid arthritis
a. Receiving immunosuppressive
therapy
1 2/3 1 Clarification (DMPA): DMPA use among women receiving long-
term corticosteroid therapy with a history of, or with risk factors for,
nontraumatic fractures is classified as category 3. Otherwise, DMPA
use for women with rheumatoid arthritis is classified as category 2.
Evidence: Limited evidence shows no consistent pattern of
improvement or worsening of rheumatoid arthritis with use of
oral contraceptives, progesterone, or estrogen (102).
b. Not receiving immunosuppressive
therapy
1 2 1 Evidence: Limited evidence shows no consistent pattern of
improvement or worsening of rheumatoid arthritis with use of
oral contraceptives, progesterone, or estrogen (102).
Neurologic Conditions
Headaches
a. Nonmigraine (mild or severe) 1 1 1 —
b. Migraine Evidence: No studies directly examined the risk for stroke
among women with migraine using POCs (103). Limited
evidence demonstrated that women using POPs, DMPA, or
implants do not have an increased risk for ischemic stroke
compared with nonusers (104).
Comment: Menstrual migraine is a subtype of migraine without
aura. For more information, see The International Headache
Society Classification, 3rd edition (http://www.ihs-classification.
org/_downloads/mixed/International-Headache-Classification-
III-ICHD-III-2013-Beta.pdf ).
i. Without aura (This category
of migraine includes
menstrual migraine.)
1 1 1
ii. With aura 1 1 1
Epilepsy
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 1 Clarification: If a woman is taking anticonvulsants, see
Drug Interactions section. Certain anticonvulsants lower
POC effectiveness.
Multiple sclerosis Evidence: Limited evidence suggests that use of COCs or oral
contraceptives (type not specified) among women with multiple
sclerosis does not worsen the clinical course of disease (105).
Comment: Women with multiple sclerosis might have
compromised bone health from disease-related disability,
immobility, and use of corticosteroids. Use of DMPA, which
has been associated with small changes in BMD, might
be of concern.
a. With prolonged immobility 1 2 1
b. Without prolonged immobility 1 2 1
Depressive Disorders
Depressive disorders 1 1 1 Clarification: If a woman is taking psychotropic medications or
St. John’s wort, see Drug Interactions section.
Evidence: The frequency of psychiatric hospitalizations for
women with bipolar disorder or depression did not significantly
differ among women using DMPA, LNG-IUD, Cu-IUD, or
sterilization (106).
Reproductive Tract Infections and Disorders
Vaginal bleeding patterns
a. Irregular pattern without
heavy bleeding
2 2 2 Comment: Irregular menstrual bleeding patterns are common
among healthy women. POC use frequently induces an irregular
bleeding pattern. Implant use might induce irregular bleeding
patterns, especially during the first 3–6 months, although these
patterns might persist longer.
b. Heavy or prolonged bleeding
(includes regular and irregular
patterns)
2 2 2 Clarification: Unusually heavy bleeding should raise the
suspicion of a serious underlying condition.
See table footnotes on page 49.

Recommendations and Reports
42 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Unexplained vaginal bleeding
(suspicious for serious condition)
before evaluation
3 3 2 Clarification: If pregnancy or an underlying pathological
condition (e.g., pelvic malignancy) is suspected, it must be
evaluated and the category adjusted after evaluation.
Comment: POCs might cause irregular bleeding patterns,
which might mask symptoms of underlying pathologic
conditions. The effects of DMPA might persist for some time
after discontinuation.
Endometriosis 1 1 1 —
Benign ovarian tumors
(including cysts)
1 1 1 —
Severe dysmenorrhea 1 1 1 —
Gestational trophoblastic disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Clarification: For all subconditions of gestational trophoblastic
disease, classifications are based on the assumption that women
are under close medical supervision because of the need for
monitoring of β-hCG levels for appropriate disease surveillance.
a. Suspected gestational
trophoblastic disease (immediate
postevacuation)
i. Uterine size first trimester 1 1 1
ii. Uterine size second trimester 1 1 1
b. Confirmed gestational
trophoblastic disease (after initial
evacuation and during monitoring)
i. Undetectable/nonpregnant β–
hCG levels
1 1 1
ii. Decreasing β–hCG levels 1 1 1
iii. Persistently elevated β-hCG
levels or malignant disease,
with no evidence or suspicion of
intrauterine disease
1 1 1
iv. Persistently elevated β-hCG
levels or malignant disease,
with evidence or suspicion of
intrauterine disease
1 1 1
Cervical ectropion 1 1 1 —
Cervical intraepithelial neoplasia 2 2 1 Evidence: Among women with persistent human papillomavirus
infection, long-term DMPA use (≥5 years) might increase the risk
for carcinoma in situ and invasive carcinoma (107).
Cervical cancer
(awaiting treatment)
2 2 1 Comment: Theoretical concern exists that POC use might affect
prognosis of the existing disease. While awaiting treatment,
women may use POCs. In general, treatment of this condition
can render a woman sterile.
Breast disease
Breast cancer is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Undiagnosed mass 2 2
2 Clarification: Evaluation should be pursued as early as possible.
b. Benign breast disease 1 1 1 —
c. Family history of cancer 1 1 1 —
d. Breast cancer Comment: Breast cancer is a hormonally sensitive tumor, and
the prognosis for women with current or recent breast cancer
might worsen with POC use.
i. Current 4 4 4
ii. Past and no evidence of current
disease for 5 years
3 3 3
Endometrial hyperplasia 1 1 1 —
Endometrial cancer
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 1 Comment: While awaiting treatment, women may use POCs. In
general, treatment of this condition renders a woman sterile.
Ovarian cancer
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 1 Comment: While awaiting treatment, women may use POCs. In
general, treatment of this condition can render a woman sterile.
Uterine fibroids 1 1 1 Comment: POCs do not appear to cause growth of uterine fibroids.
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 43
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Pelvic inflammatory disease Comment: Whether POCs, like COCs, reduce the risk for PID
among women with STDs is unknown; however, they do not
protect against HIV or lower genital tract STDs.
a. Past PID
i. With subsequent pregnancy 1 1 1
ii. Without subsequent pregnancy 1 1 1
b. Current PID 1 1 1
Sexually transmitted diseases
a. Current purulent cervicitis or
chlamydial infection or gonococcal
infection
1 1 1 —
b. Vaginitis (including Trichomonas
vaginalis and bacterial vaginosis)
1 1 1 —
c. Other factors related to STDs 1 1 1 —
HIV
High risk for HIV 1 1 1 Clarification (DMPA): Some studies suggest that women
using progestin-only injectable contraception might be at
increased risk for HIV acquisition; other studies do not show this
association. CDC reviewed all available evidence and agreed
that the data were not sufficiently conclusive to change current
guidance. However, because of the inconclusive nature of the
body of evidence on possible increased risk for HIV acquisition,
women using progestin-only injectable contraception should
be strongly advised to also always use condoms (male or
female) and take other HIV preventive measures. Expansion
of contraceptive method mix and further research on the
relationship between hormonal contraception and HIV infection
are essential. These recommendations will be continually
reviewed in light of new evidence.
Evidence: Overall, evidence does not support an association
between oral contraceptives and risk for HIV acquisition,
evidence is inconsistent regarding an association between
DMPA and increased risk for HIV acquisition, and no studies have
suggested an increased risk for HIV acquisition with etonogestrel
implants although data are limited (108).
HIV infection
For women with HIV infection who
are not clinically well or not using ARV
therapy, this condition is associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 1 Clarification: Drug interactions might exist between hormonal
contraceptives and ARV drugs; see Drug Interactions section.
Evidence: Overall, evidence does not support an association
between POC use and progression of HIV. Limited direct
evidence on an association between POC use and transmission
of HIV to noninfected partners, as well as studies measuring
genital viral shedding as a proxy for infectivity, have had mixed
results. Studies measuring whether hormonal contraceptive
methods affect plasma HIV viral load generally have found no
effect (109–111).
Other Infections
Schistosomiasis
Schistosomiasis with fibrosis of the
liver is associated with increased risk
for adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 Evidence: Among women with uncomplicated schistosomiasis,
limited evidence showed that DMPA use had no adverse effects
on liver function (112).
b. Fibrosis of the liver (if severe, see
Cirrhosis section)
1 1 1 —
Tuberculosis
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
Clarification: If a woman is taking rifampin, see Drug
Interactions section. Rifampin is likely to decrease the
effectiveness of some POCs.
a. Nonpelvic 1 1 1
b. Pelvic 1 1 1
Malaria 1 1 1 —
See table footnotes on page 49.

Recommendations and Reports
44 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Endocrine Conditions
Diabetes
Insulin-dependent diabetes; diabetes
with nephropathy, retinopathy, or
neuropathy; diabetes with other
vascular disease; or diabetes of
>20 years’ duration are associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. History of gestational disease 1 1 1 Evidence: POCs had no adverse effects on serum lipid levels
in women with a history of gestational diabetes in two small
studies (113,114). Limited evidence is inconsistent about the
development of noninsulin-dependent diabetes among users of
POCs with a history of gestational diabetes (115–118).
b. Nonvascular disease Evidence: Among women with insulin-dependent or non–
insulin-dependent diabetes, limited evidence on use of POCs
(POPs, DMPA, and LNG implant) suggests that these methods
have little effect on short-term or long-term diabetes control
(e.g., glycosylated hemoglobin levels), hemostatic markers, or
lipid profile (119–122).
i. Non-insulin dependent 2 2 2
ii. Insulin dependent 2 2 2
c. Nephropathy, retinopathy, or
neuropathy
2 3 2 Comment: Concern exists about hypoestrogenic effects and
reduced HDL levels, particularly among users of DMPA. The
effects of DMPA might persist for some time after discontinuation.
Some POCs might increase the risk for thrombosis, although this
increase is substantially less than with COCs.
d. Other vascular disease or diabetes
of >20 years’ duration
2 3 2 Comment: Concern exists about hypoestrogenic effects and
reduced HDL levels, particularly among users of DMPA. The
effects of DMPA might persist for some time after discontinuation.
Some POCs might increase the risk for thrombosis, although this
increase is substantially less than with COCs.
Thyroid disorders
a. Simple goiter 1 1 1 —
b. Hyperthyroid 1 1 1 —
c. Hypothyroid 1 1 1 —
Gastrointestinal Conditions
Inflammatory bowel disease
(ulcerative colitis or Crohn’s disease)
1 2 2 Evidence: Risk for disease relapse among women with IBD using
oral contraceptives (most studies did not specify formulation)
did not increase significantly from that for nonusers (123).
Comment: Absorption of POPs among women with IBD might be
reduced if the woman has substantial malabsorption caused by
severe disease or small bowel surgery.
Women with IBD have a higher prevalence of osteoporosis and
osteopenia than the general population. Use of DMPA, which has
been associated with small changes in BMD, might be of concern.
Gallbladder disease
a. Symptomatic
i. Treated by cholecystectomy 2 2 2 —
ii. Medically treated 2 2 2 —
iii. Current 2 2 2 —
b. Asymptomatic 2 2 2 —
History of cholestasis
a. Pregnancy related 1 1 1 —
b. Past COC related 2 2 2 Comment: Theoretical concern exists that a history of COC-
related cholestasis might predict subsequent cholestasis with
POC use. However, this has not been documented.
Viral hepatitis
a. Acute or flare 1 1 1 —
b. Carrier 1 1 1 —
c. Chronic 1 1 1 —
Cirrhosis
Severe cirrhosis is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Mild (compensated) 1 1 1 —
b. Severe (decompensated) 3 3 3 —
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 45
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Liver tumors
Hepatocellular adenoma and
malignant liver tumors are associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Benign
i. Focal nodular hyperplasia 2 2 2 Evidence: Limited direct evidence suggests that hormonal
contraceptive use does not influence either progression or
regression of liver lesions among women with focal nodular
hyperplasia (124).
ii. Hepatocellular adenoma 3 3 3 Comment: No evidence is available about hormonal
contraceptive use among women with hepatocellular adenoma.
COC use in healthy women is associated with development and
growth of hepatocellular adenoma; whether other hormonal
contraceptives have similar effects is not known.
b. Malignant (hepatoma) 3 3 3 —
Respiratory Conditions
Cystic fibrosis
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 2 1 Clarification: Persons with cystic fibrosis are at increased risk for
diabetes, liver disease, gallbladder disease, and VTE (particularly
related to use of central venous catheters) and are frequently
prescribed antibiotics. Categories assigned to such conditions
in U.S. MEC should be the same for women with cystic fibrosis
who have these conditions. For cystic fibrosis, classifications are
based on the assumption that no other conditions are present;
these classifications must be modified in the presence of such
conditions.
Clarification: Certain drugs to treat cystic fibrosis (e.g.,
lumacaftor) might reduce effectiveness of hormonal
contraceptives, including oral, injectable, transdermal, and
implantable contraceptives.
Evidence: Limited evidence suggests that use of COCs or oral
contraceptives (type not specified) among women with cystic
fibrosis is not associated with worsening of disease severity. Very
limited evidence suggests that cystic fibrosis does not impair the
effectiveness of hormonal contraception (125).
Comment: Women with cystic fibrosis have a higher prevalence
of osteopenia, osteoporosis, and fragility fractures than the
general population. Use of DMPA, which has been associated
with small changes in BMD, might be of concern.
Anemias
Thalassemia 1 1 1 —
Sickle cell disease
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
1 1 1 Evidence: Among women with sickle cell disease, POC use did
not have adverse effects on hematologic parameters and, in some
studies, was beneficial with respect to clinical symptoms (126–133).
Iron deficiency anemia 1 1 1 Comment: Changes in the menstrual pattern associated with
POC use have little effect on hemoglobin levels.
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with
increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Complicated: graft failure (acute
or chronic), rejection, or cardiac
allograft vasculopathy
2 2 2 —
b. Uncomplicated 2 2 2 —
See table footnotes on page 49.

Recommendations and Reports
46 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Drug Interactions
Antiretroviral therapy Comment: These recommendations generally are for ARV agents
used alone. However, most women receiving ARV therapy
are using multiple drugs in combination. In general, whether
interactions between ARVs and hormonal contraceptives differ
when ARVs are given alone or in combination is unknown.
a. Nucleoside reverse transcriptase
inhibitors (NRTIs)
i. Abacavir (ABC) 1 1 1 Evidence: NRTIs do not appear to have significant risk for
interactions with hormonal contraceptive methods (134–139).
ii. Tenofovir (TDF) 1 1 1
iii. Zidovudine (AZT) 1 1 1
iv. Lamivudine (3TC) 1 1 1
v. Didanosine (DDI) 1 1 1
vi. Emtricitabine (FTC) 1 1 1
vii. Stavudine (D4T) 1 1 1
b. Nonnucleoside reverse
transcriptase inhibitors (NNRTIs)
i. Efavirenz (EFV) 2 1 2 Clarification: Evidence suggests drug interactions between EFV
and certain hormonal contraceptives. These interactions might
reduce the effectiveness of the hormonal contraceptive.
Evidence: One study found that women using etonogestrel
implants with EFV had a higher pregnancy rate than women
not using ARVs, although confidence intervals overlapped
and absolute pregnancy rates were still lower than for other
hormonal methods; another study found that etonogestrel
levels were decreased and 5% of women had presumptive
ovulation while using etonogestrel implants with EFV (140,141).
Three studies of women using LNG implants showed increased
pregnancy rates for women using EFV-containing ARV therapy
compared with no ARV use, although absolute pregnancy
rates were still lower than for other hormonal methods in one
study (141–143); another study of LNG implant users found
no difference in pregnancy rates with EFV compared with
no EFV (144).No significant effects were found on pregnancy
rates, DMPA levels, EFV levels, or HIV disease progression in
women using DMPA and EFV compared with DMPA alone
(141,144–148). No significant effects were found on HIV disease
progression in women using LNG implants and EFV compared
with no ARVs (143). No data have assessed effectiveness
of contraceptive implants during later years of use when
progestin concentrations are lower and risk for failure from drug
interactions might be greater.
ii. Etravirine (ETR) 1 1 1 —
iii. Nevirapine (NVP) 1 1 1 Evidence: Five studies found no significant increase in
pregnancy rates among women using implants and NVP
compared with implants alone (141–144,149). Four studies
found no significant increase in pregnancy rates among
women using DMPA or other contraceptive injectables and NVP
compared with DMPA or other contraceptive injectables alone
(141,144,147
,150). One study found no ovulations or changes
in DMPA concentrations (145). No effect was found on HIV
disease progression with use of NVP and DMPA or LNG implants
(143,145,147–149,151). No data have assessed effectiveness
of contraceptive implants during later years of use when
progestin concentrations are lower and risk for failure from drug
interactions might be greater.
iv. Rilpivirine (RPV) 1 1 1 —
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 47
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
c. Ritonavir-boosted protease
inhibitors
i. Ritonavir-boosted atazanavir
(ATV/r)
2 1 2 Clarification: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors and
certain hormonal contraceptives that might reduce the
effectiveness of the hormonal contraceptive. Any potential effect
on contraceptive effectiveness is likely to be lower with DMPA
than with other POCs because of the higher dose of DMPA.
Evidence: One pharmacokinetic study demonstrated increased
progestin concentrations with use of POPs and ATV/r compared
with POPs alone (152).
ii. Ritonavir-boosted darunavir
(DRV/r)
2 1 2 Clarification: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors and
certain hormonal contraceptives that might reduce the
effectiveness of the hormonal contraceptive. Any potential effect
on contraceptive effectiveness is likely to be lower with DMPA
than with other POCs because of the higher dose of DMPA.
iii. Ritonavir-boosted fosamprenavir
(FPV/r)
2 1 2 Clarification: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors and
certain hormonal contraceptives that might reduce the
effectiveness of the hormonal contraceptive. Any potential effect
on contraceptive effectiveness is likely to be lower with DMPA
than with other POCs because of the higher dose of DMPA.
iv. Ritonavir-boosted lopinavir
(LPV/r)
1 1 1 Evidence: One study demonstrated no pregnancies, no
ovulations, no change in LPV/r level, and no change in HIV
disease progression in women using DMPA (153); another study
found a small increase in pregnancy rate in women using DMPA
with LPV/r compared with no ARV therapy, however confidence
intervals overlapped (141). Two studies found no increased risk for
pregnancy in women using implants (141,142). Two studies found
contraceptive hormones increased in women using LPV/r with
DMPA or etonogestrel implants (140,153).
v. Ritonavir-boosted saquinavir
(SQV/r)
2 1 2 Clarification: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors and
certain hormonal contraceptives that might reduce the
effectiveness of the hormonal contraceptive. Any potential effect
on contraceptive effectiveness is likely to be lower with DMPA
than with other POCs because of the higher dose of DMPA.
vi. Ritonavir-boosted tipranavir
(TPV/r)
2 1 2 Clarification: Theoretically, drug interactions might occur
between certain ritonavir-boosted protease inhibitors and
certain hormonal contraceptives that might reduce the
effectiveness of the hormonal contraceptive. Any potential effect
on contraceptive effectiveness is likely to be lower with DMPA
than with other POCs because of the higher dose of DMPA.
d. Protease inhibitors without
ritonavir
i. Atazanavir (ATV) 1 1 1 Comment: When ATV is administered with Cobicistat,
theoretical concern exists for a drug interaction with hormonal
contraceptives. Cobicistat is an inhibitor of CYP3A and CYP2D6
and could theoretically increase contraceptive hormone levels.
However, its effects on CYP enzymes and drug levels might vary
when combined with other ARVs.
ii. Fosamprenavir (FPV) 2 2 2 Clarification: Theoretical concern exists that interactions
between FPV and hormonal contraceptives leading to decreased
levels of FPV might diminish effectiveness of the ARV drug. The
drug interaction likely involves CYP3A4 pathways; POCs have
less effect on CYP3A4 enzymes than CHCs.
iii. Indinavir (IDV) 1 1 1 —
See table footnotes on page 49.

Recommendations and Reports
48 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
iv. Nelfinavir (NFV) 2 1 2 Clarification: Theoretically, drug interactions might occur
between certain protease inhibitors and certain hormonal
contraceptives that might reduce the effectiveness of the
hormonal contraceptive. Any potential effect on contraceptive
effectiveness is likely to be lower with DMPA than with other
POCs because of the higher dose of DMPA. Concern exists that
interactions between NFV and POCs might decrease NFV levels.
Evidence: One study found no pregnancies, no ovulations, no
change in DMPA concentrations and no change in HIV disease
progression with use of DMPA and NFV compared with DMPA
alone; NFV concentrations were decreased with concomitant
DMPA use (145,147).
e. CCR5 co-receptor antagonists
i. Maraviroc (MVC) 1 1 1
f. HIV integrase strand transfer
inhibitors
i. Raltegravir (RAL) 1 1 1 —
ii. Dolutegravir (DTG) 1 1 1 —
iii. Elvitegravir (EVG) 1 1 1 Comment: When EVG is administered with Cobicistat,
theoretical concern exists for a drug interaction with hormonal
contraceptives. Cobicistat is an inhibitor of CYP3A and CYP2D6
and could theoretically increase contraceptive hormone levels.
However, its effects on CYP enzymes and drug levels may vary
when combined with other ARVs.
g. Fusion inhibitors
i. Enfuvirtide 1 1 1 —
Anticonvulsant therapy —
a. Certain anticonvulsants
(phenytoin, carbamazepine,
barbiturates, primidone, topiramate,
and oxcarbazepine)
2 1 3 Clarification: Although the interaction of certain anticonvulsants
with POPs and etonogestrel implants is not harmful to women, it is
likely to reduce the effectiveness of POPs and etonogestrel implants.
Whether increasing the hormone dose of POPs alleviates this concern
remains unclear. Use of other contraceptives should be encouraged
for women who are long-term users of any of these drugs. Use of
DMPA is a category 1 because its effectiveness is not decreased by
use of certain anticonvulsants.
Evidence: Use of certain anticonvulsants might decrease the
effectiveness of POCs (154–156).
b. Lamotrigine 1 1 1 Evidence: No drug interactions have been reported among
women with epilepsy receiving lamotrigine and POCs (157).
Antimicrobial therapy
a. Broad-spectrum antibiotics 1 1 1 —
b. Antifungals 1 1 1 —
c. Antiparasitics 1 1 1 —
d. Rifampin or rifabutin therapy 2 1 3 Clarification: Although the interaction of rifampin or rifabutin
with POPs and etonogestrel implants is not harmful to women,
it is likely to reduce the effectiveness of POPs and etonogestrel
implants. Use of other contraceptives should be encouraged for
women who are long-term users of any of these drugs. Use of
DMPA is a category 1 because its effectiveness is not decreased
by use of rifampin or rifabutin. Whether increasing the hormone
dose of POPs alleviates this concern remains unclear.
See table footnotes on page 49.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 49
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE C1. (Continued) Classifications for progestin-only contraceptives, including implants, depot medroxyprogesterone acetate, and progestin-
only pills
Condition
Category
Clarifications/Evidence/CommentsImplants DMPA POPs
Psychotropic medications Comment: For many common psychotropic agents, limited
or no theoretical concern exits for clinically significant drug
interactions when co-administered with hormonal contraceptives.
However, either no or very limited data exist examining potential
interactions for these classes of medications.
a. SSRIs 1 1 1 Evidence: No evidence specifically examined the use of POCs
with SSRIs. Limited clinical and pharmacokinetic data do not
demonstrate concern for SSRIs decreasing the effectiveness
of oral contraceptives. Limited evidence suggests that for
women taking SSRIs, the use of hormonal contraceptives was
not associated with differences in effectiveness of the SSRI for
treatment or in adverse events when compared with women not
taking hormonal contraceptives (158).
Comment: Drugs that are inhibitors of CYP3A4 or CYP2C9
theoretically have the potential to increase levels of
contraceptive steroid, which might increase adverse events.
Fluvoxamine is an SSRI known to be a moderate inhibitor of both
3A4 and 2C9; however, no clinical or pharmacokinetic studies
were identified to explore potential drug-drug interactions.
St. John’s wort 2 1 2 Evidence: No evidence specifically examined the use of POCs
with St John’s wort. Although clinical data are limited, studies with
pharmacokinetic and pharmacodynamics outcomes raise concern
that St. John’s wort might decrease effectiveness of hormonal
contraceptives, including increased risk for breakthrough bleeding
and ovulation and increased metabolism of estrogen and
progestin. Any interactions might be dependent on the dose of
St John’s wort, and the concentration of active ingredients across
types of St. John’s wort preparations may vary (159).
Comment: Any potential effect on contraceptive effectiveness
is likely to be lower with DMPA than with other POCs because of
the higher dose of DMPA.
Abbreviations: ARV=antiretroviral; BMD=bone mineral density; BMI=body mass index; COC=combined oral contraceptive; DMPA=depot medroxyprogesterone acetate; DVT=deep
venous thrombosis; hCG=human chorionic gonadotropin; HDL=high-density lipoprotein; HIV=human immunodeficiency virus; IBD=inflammatory bowel disease; LDL=low-density
lipoprotein; LNG = levonorgestrel; NA = not applicable; NET-EN=norethisterone enantate; PE=pulmonary embolism; PID=pelvic inflammatory disease; POC=progestin-only contraceptive;
POP=progestin-only pill; SSRI = selective serotonin reuptake inhibitor; STD=sexually transmitted disease; VTE=venous thromboembolism.
References
1. Lanza LL, McQuay LJ, Rothman KJ, et al. Use of depot medroxyprogesterone
acetate contraception and incidence of bone fracture. Obstet Gynecol
2013;121:593–600. http://dx.doi.org/10.1097/AOG.0b013e318283d1a1
2. Harel Z, Riggs S, Vaz R, Flanagan P, Harel D, Machan JT. Bone accretion
in adolescents using the combined estrogen and progestin transdermal
contraceptive method Ortho Evra: a pilot study. J Pediatr Adolesc Gynecol
2010;23:23–31. http://dx.doi.org/10.1016/j.jpag.2009.04.008
3. Kaunitz AM, Miller PD, Rice VM, Ross D, McClung MR. Bone mineral
density in women aged 25–35 years receiving depot medroxyprogesterone
acetate: recovery following discontinuation. Contraception 2006;74:90–9.
http://dx.doi.org/10.1016/j.contraception.2006.03.010
4. Kaunitz AM, Arias R, McClung M. Bone density recovery after depot
medroxyprogesterone acetate injectable contraception use. Contraception
2008;77:67–76. http://dx.doi.org/10.1016/j.contraception.2007.10.005
5. Kaunitz AM, Darney PD, Ross D, Wolter KD, Speroff L. Subcutaneous
DMPA vs. intramuscular DMPA: a 2-year randomized study of
contraceptive efficacy and bone mineral density. Contraception
2009;80:7–17. http://dx.doi.org/10.1016/j.contraception.2009.02.005
6. Lappe JM, Stegman MR, Recker RR. The impact of lifestyle factors on
stress fractures in female Army recruits. Osteoporos Int 2001;12:35–42.
http://dx.doi.org/10.1007/s001980170155
7. Lara-Torre E, Edwards CP, Perlman S, Hertweck SP. Bone mineral density in
adolescent females using depot medroxyprogesterone acetate. J Pediatr Adolesc
Gynecol 2004;17:17–21. http://dx.doi.org/10.1016/j.jpag.2003.11.017
8. Lopez LM, Chen M, Mullins S, Curtis KM, Helmerhorst FM. Steroidal
contraceptives and bone fractures in women: evidence from observational
studies. Cochrane Database Syst Rev 2012;8:CD009849.
9. Lopez LM, Grimes DA, Schulz KF, Curtis KM. Steroidal contraceptives: effect
on bone fractures in women. Cochrane Database Syst Rev 2011;(7):CD006033.
10. Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot
medroxyprogesterone acetate and fracture risk. J Clin Endocrinol Metab
2010;95:4909–16. http://dx.doi.org/10.1210/jc.2010-0032
11. Merki-Feld GS, Neff M, Keller PJ. A 2-year prospective study on the
effects of depot medroxyprogesterone acetate on bone mass-response to
estrogen and calcium therapy in individual users. Contraception
2003;67:79–86. http://dx.doi.org/10.1016/S0010-7824(02)00460-2
12. Monteiro-Dantas C, Espejo-Arce X, Lui-Filho JF, Fernandes AM, Monteiro I,
Bahamondes L. A three-year longitudinal evaluation of the forearm bone density
of users of etonogestrel- and levonorgestrel-releasing contraceptive implants.
Reprod Health 2007;4:11. http://dx.doi.org/10.1186/1742-4755-4-11
13. Naessen T, Olsson SE, Gudmundson J. Differential effects on
bone density of progestogen-only methods for contraception in
premenopausal women. Contraception 1995;52:35–9. http://dx.doi.
org/10.1016/0010-7824(95)00121-P
14. Sanches L, Marchi NM, Castro S, Juliato CT, Villarroel M, Bahamondes L.
Forearm bone mineral density in postmenopausal former users of depot
medroxyprogesterone acetate. Contraception 2008;78:365–9. http://
dx.doi.org/10.1016/j.contraception.2008.07.013
15. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Injectable hormone
contraception and bone density: results from a prospective study. Epidemiology
2002;13:581–7. http://dx.doi.org/10.1097/00001648-200209000-00015
Recommendations and Reports
50 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
32. Berenson AB, Rahman M, Breitkopf CR, Bi LX. Effects of depot
medroxyprogesterone acetate and 20-microgram oral contraceptives on
bone mineral density. Obstet Gynecol 2008;112:788–99. http://dx.doi.
org/10.1097/AOG.0b013e3181875b78
33. Busen NH, Britt RB, Rianon N. Bone mineral density in a cohort of
adolescent women using depot medroxyprogesterone acetate for one to
two years. J Adolesc Health 2003;32:257–9. http://dx.doi.org/10.1016/
S1054-139X(02)00567-0
34. Caird LE, Reid-Thomas V, Hannan WJ, Gow S, Glasier AF. Oral
progestogen-only contraception may protect against loss of bone mass
in breast-feeding women. Clin Endocrinol (Oxf) 1994;41:739–45.
http://dx.doi.org/10.1111/j.1365-2265.1994.tb02788.x
35. Clark MK, Sowers M, Levy B, Nichols S. Bone mineral density loss and
recovery during 48 months in first-time users of depot medroxyprogesterone
acetate. Fertil Steril 2006;86:1466–74. http://dx.doi.org/10.1016/j.
fertnstert.2006.05.024
36. Cromer BA, Lazebnik R, Rome E, et al. Double-blinded randomized
controlled trial of estrogen supplementation in adolescent girls who receive
depot medroxyprogesterone acetate for contraception. Am J Obstet
Gynecol 2005;192:42–7. http://dx.doi.org/10.1016/j.ajog.2004.07.041
37. Cromer BA, Blair JM, Mahan JD, Zibners L, Naumovski Z. A
prospective comparison of bone density in adolescent girls receiving
depot medroxyprogesterone acetate (Depo-Provera), levonorgestrel
(Norplant), or oral contraceptives. J Pediatr 1996;129:671–6. http://
dx.doi.org/10.1016/S0022-3476(96)70148-8
38. Cromer BA, Bonny AE, Stager M, et al. Bone mineral density in
adolescent females using injectable or oral contraceptives: a 24-month
prospective study. Fertil Steril 2008;90:2060–7. http://dx.doi.
org/10.1016/j.fertnstert.2007.10.070
39. Cromer BA, Stager M, Bonny A, et al. Depot medroxyprogesterone acetate,
oral contraceptives and bone mineral density in a cohort of adolescent girls. J
Adolesc Health 2004;35:434–41. http://dx.doi.org/10.1016/j.
jadohealth.2004.07.005
40. Cundy T, Ames R, Horne A, et al. A randomized controlled trial of estrogen
replacement therapy in long-term users of depot medroxyprogesterone
acetate. J Clin Endocrinol Metab 2003;88:78–81. http://dx.doi.
org/10.1210/jc.2002-020874
41. Cundy T, Cornish J, Evans MC, Roberts H, Reid IR. Recovery of bone
density in women who stop using medroxyprogesterone acetate. BMJ
1994;308:247–8. http://dx.doi.org/10.1136/bmj.308.6923.247
42. Cundy T, Cornish J, Roberts H, Reid IR. Menopausal bone loss in
long-term users of depot medroxyprogesterone acetate contraception.
Am J Obstet Gynecol 2002;186:978–83. http://dx.doi.org/10.1067/
mob.2002.122420
43. Di X, Li Y, Zhang C, Jiang J, Gu S. Effects of levonorgestrel-releasing subdermal
contraceptive implants on bone density and bone metabolism. Contraception
1999;60:161–6. http://dx.doi.org/10.1016/S0010-7824(99)00080-3
44. Díaz S, Reyes MV, Zepeda A, et al. Norplant® implants and progesterone
vaginal rings do not affect maternal bone turnover and density during
lactation and after weaning. Hum Reprod 1999;14:2499–505. http://
dx.doi.org/10.1093/humrep/14.10.2499
45. Gai L, Zhang J, Zhang H, Gai P, Zhou L, Liu Y. The effect of depot
medroxyprogesterone acetate (DMPA) on bone mineral density (BMD)
and evaluating changes in BMD after discontinuation of DMPA in
Chinese women of reproductive age. Contraception 2011;83:218–22.
http://dx.doi.org/10.1016/j.contraception.2010.07.027
46. Bahamondes L, Espejo-Arce X, Hidalgo MM, Hidalgo-Regina C, Teatin-
Juliato C, Petta CA. A cross-sectional study of the forearm bone density
of long-term users of levonorgestrel-releasing intrauterine system. Hum
Reprod 2006;21:1316–9. http://dx.doi.org/10.1093/humrep/dei457
47. Bahamondes L, Monteiro-Dantas C, Espejo-Arce X, et al. A prospective
study of the forearm bone density of users of etonorgestrel- and
levonorgestrel-releasing contraceptive implants. Hum Reprod
2006;21:466–70. http://dx.doi.org/10.1093/humrep/dei358
16. Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM. Change in
bone mineral density among adolescent women using and discontinuing
depot medroxyprogesterone acetate contraception. Arch Pediatr Adolesc
Med 2005;159:139–44. http://dx.doi.org/10.1001/archpedi.159.2.139
17. Segall-Gutierrez P, Agarwal R, Ge M, Lopez C, Hernandez G, Stanczyk
FZ. A pilot study examining short-term changes in bone mineral density
among class 3 obese users of depot-medroxyprogesterone acetate. Eur J
Contracept Reprod Health Care 2013;18:199–205. http://dx.doi.org/
10.3109/13625187.2013.774358
18. Tang OS, Tang G, Yip PS, Li B. Further evaluation on long-term depot-
medroxyprogesterone acetate use and bone mineral density: a longitudinal
cohort study. Contraception 2000;62:161–4. http://dx.doi.org/10.1016/
S0010-7824(00)00168-2
19. Vestergaard P, Rejnmark L, Mosekilde L. The effects of depot
medroxyprogesterone acetate and intrauterine device use on fracture risk
in Danish women. Contraception 2008;78:459–64. http://dx.doi.
org/10.1016/j.contraception.2008.07.014
20. Viola AS, Castro S, Marchi NM, Bahamondes MV, Viola CF, Bahamondes
L. Long-term assessment of forearm bone mineral density in postmenopausal
former users of depot medroxyprogesterone acetate. Contraception
2011;84:122–7. http://dx.doi.org/10.1016/j.contraception.2010.11.007
21. Walsh JS, Eastell R, Peel NF. Depot medroxyprogesterone acetate use
after peak bone mass is associated with increased bone turnover but no
decrease in bone mineral density. Fertil Steril 2010;93:697–701. http://
dx.doi.org/10.1016/j.fertnstert.2008.10.004
22. Wetmore CM, Ichikawa L, LaCroix AZ, Ott SM, Scholes D. Association
between caffeine intake and bone mass among young women: potential
effect modification by depot medroxyprogesterone acetate use.
Osteoporos Int 2008;19:519–27. http://dx.doi.org/10.1007/
s00198-007-0473-2
23. Wong AY, Tang LC, Chin RK. Levonorgestrel-releasing intrauterine system
(Mirena) and depot medroxyprogesterone acetate (Depoprovera) as long-term
maintenance therapy for patients with moderate and severe endometriosis: a
randomised controlled trial. Aust N Z J Obstet Gynaecol 2010;50:273–9.
http://dx.doi.org/10.1111/j.1479-828X.2010.01152.x
24. Yang KY, Kim YS, Ji YI, Jung MH. Changes in bone mineral density of
users of the levonorgestrel-releasing intrauterine system. J Nippon Med
Sch 2012;79:190–4. http://dx.doi.org/10.1272/jnms.79.190
25. Zhang MH, Zhang W, Zhang AD, Yang Y, Gai L. Effect of depot
medroxyprogesterone acetate on bone mineral density in adolescent
women. Chin Med J (Engl) 2013;126:4043–7.
26. Bahamondes MV, Monteiro I, Castro S, Espejo-Arce X, Bahamondes
L. Prospective study of the forearm bone mineral density of long-term
users of the levonorgestrel-releasing intrauterine system. Hum Reprod
2010;25:1158–64. http://dx.doi.org/10.1093/humrep/deq043
27. Banks E, Berrington A, Casabonne D. Overview of the relationship between
use of progestogen-only contraceptives and bone mineral density. BJOG
2001;108:1214–21. http://dx.doi.org/10.1111/j.1471-0528.2001.00296.x
28. Beerthuizen R, van Beek A, Massai R, Mäkäräinen L, Hout J, Bennink HC.
Bone mineral density during long-term use of the progestagen contraceptive
implant Implanon compared to a non-hormonal method of contraception.
Hum Reprod 2000;15:118–22. http://dx.doi.org/10.1093/humrep/15.1.118
29. Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral density
in adolescents using norethisterone enanthate, depot-medroxyprogesterone
acetate or combined oral contraceptives for contraception. Contraception
2007;75:438–43. http://dx.doi.org/10.1016/j.contraception.2007.02.001
30. Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral
density in a cohort of adolescents during use of norethisterone enanthate,
depot-medroxyprogesterone acetate or combined oral contraceptives
and after discontinuation of norethisterone enanthate. Contraception
2009;79:345–9. http://dx.doi.org/10.1016/j.contraception.2008.11.009
31. Berenson AB, Breitkopf CR, Grady JJ, Rickert VI, Thomas A. Effects
of hormonal contraception on bone mineral density after 24 months of
use. Obstet Gynecol 2004;103:899–906. http://dx.doi.org/10.1097/01.
AOG.0000117082.49490.d5
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 51
US Department of Health and Human Services/Centers for Disease Control and Prevention
48. Pitts SA, Feldman HA, Dorale A, Gordon CM. Bone mineral density,
fracture, and vitamin D in adolescents and young women using depot
medroxyprogesterone acetate. J Pediatr Adolesc Gynecol 2012;25:23–6.
http://dx.doi.org/10.1016/j.jpag.2011.07.014
49. US Department of Health and Human Services. Healthy people 2020:
maternal, infant, and child health objectives. Washington, DC: US
Department of Health and Human Services; 2015. http://www.
healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-
child-health/objectives
50. Braga GC, Ferriolli E, Quintana SM, Ferriani RA, Pfrimer K, Vieira CS.
Immediate postpartum initiation of etonogestrel-releasing implant: a
randomized controlled trial on breastfeeding impact. Contraception
2015;92:536–42. http://dx.doi.org/10.1016/j.contraception.2015.07.009
51. Phillips SJ, Tepper NK, Kapp N, Nanda K, Temmerman M, Curtis KM.
Progestogen-only contraceptive use among breastfeeding women: a
systematic review. Contraception 2015;S0010-7824(15)00585-5.
52. Kurunmäki H. Contraception with levonorgestrel-releasing subdermal
capsules, Norplant, after pregnancy termination. Contraception
1983;27:473–82. http://dx.doi.org/10.1016/0010-7824(83)90044-6
53. Kurunmäki H, Toivonen J, Lähteenmäki PL, Luukkainen T. Immediate
postabortal contraception with Norplant: levonorgestrel, gonadotropin,
estradiol, and progesterone levels over two postabortal months and return
of fertility after removal of Norplant capsules. Contraception
1984;30:431–42. http://dx.doi.org/10.1016/0010-7824(84)90035-0.
54. Lähteenmäki P, Toivonen J, Lähteenmäki PL. Postabortal contraception
with norethisterone enanthate injections. Contraception 1983;27:553–
62 http://dx.doi.org/10.1016/0010-7824(83)90020-3
55. Ortayli N, Bulut A, Sahin T, Sivin I. Immediate postabortal contraception
with the levonorgestrel intrauterine device, Norplant, and traditional
methods. Contraception 2001;63:309–14. http://dx.doi.org/10.1016/
S0010-7824(01)00212-8
56. Beksinska ME, Smit JA, Kleinschmidt I, Milford C, Farley TM. Prospective
study of weight change in new adolescent users of DMPA, NET-EN, COCs,
nonusers and discontinuers of hormonal contraception. Contraception
2010;81:30–4. http://dx.doi.org/10.1016/j.contraception.2009.07.007
57. Bender NM, Segall-Gutierrez P, Najera SO, Stanczyk FZ, Montoro M,
Mishell DR Jr. Effects of progestin-only long-acting contraception on
metabolic markers in obese women. Contraception 2013;88:418–25.
http://dx.doi.org/10.1016/j.contraception.2012.12.007
58. Berenson AB, Rahman M. Changes in weight, total fat, percent body
fat, and central-to-peripheral fat ratio associated with injectable and oral
contraceptive use. Am J Obstet Gynecol 2009;200:329.e1–8. http://
dx.doi.org/10.1016/j.ajog.2008.12.052
59. Bonny AE, Secic M, Cromer B. Early weight gain related to later weight
gain in adolescents on depot medroxyprogesterone acetate. Obstet Gynecol
2011;117:793–7. http://dx.doi.org/10.1097/AOG.0b013e31820f387c.
60. Bonny AE, Ziegler J, Harvey R, Debanne SM, Secic M, Cromer BA.
Weight gain in obese and nonobese adolescent girls initiating depot
medroxyprogesterone, oral contraceptive pills, or no hormonal
contraceptive method. Arch Pediatr Adolesc Med 2006;160:40–5 http://
dx.doi.org/10.1001/archpedi.160.1.40
61. Clark MK, Dillon JS, Sowers M, Nichols S. Weight, fat mass, and central
distribution of fat increase when women use depot-medroxyprogesterone
acetate for contraception. Int J Obes 2005;29:1252–8. http://dx.doi.
org/10.1038/sj.ijo.0803023
62. Gerlach LS, Saldaña SN, Wang Y, Nick TG, Spigarelli MG. Retrospective
review of the relationship between weight change and demographic factors
following initial depot medroxyprogesterone acetate injection in adolescents.
Clin Ther 2011;33:182–7. http://dx.doi.org/10.1016/j.clinthera.2011.02.008
63. Jain J, Jakimiuk AJ, Bode FR, Ross D, Kaunitz AM. Contraceptive
efficacy and safety of DMPA-SC. Contraception 2004;70:269–75.
http://dx.doi.org/10.1016/j.contraception.2004.06.011
64. Kozlowski KJ, Rickert VI, Hendon A, Davis P. Adolescents and Norplant:
preliminary findings of side effects. J Adolesc Health 1995;16:373–8.
http://dx.doi.org/10.1016/S1054-139X(94)00029-E
65. Le YC, Rahman M, Berenson AB. Early weight gain predicting later weight
gain among depot medroxyprogesterone acetate users. Obstet Gynecol
2009;114:279–84. http://dx.doi.org/10.1097/AOG.0b013e3181af68b2
66. Leiman G. Depo-medroxyprogesterone acetate as a contraceptive agent:
its effect on weight and blood pressure. Am J Obstet Gynecol
1972;114:97–102. http://dx.doi.org/10.1016/0002-9378(72)90296-7.
67. Lopez LM, Grimes DA, Chen M, et al. Hormonal contraceptives for
contraception in overweight or obese women. Cochrane Database Syst
Rev 2013;4:CD008452.
68. Mangan SA, Larsen PG, Hudson S. Overweight teens at increased risk
for weight gain while using depot medroxyprogesterone acetate. J Pediatr
Adolesc Gynecol 2002;15:79–82. http://dx.doi.org/10.1016/
S1083-3188(01)00147-4
69. Nyirati CM, Habash DL, Shaffer LE. Weight and body fat changes in
postpartum depot-medroxyprogesterone acetate users. Contraception
2013;88:169–76. http://dx.doi.org/10.1016/j.contraception.2012.10.016
70. Pantoja M, Medeiros T, Baccarin MC, Morais SS, Bahamondes L,
Fernandes AM. Variations in body mass index of users of depot-
medroxyprogesterone acetate as a contraceptive. Contraception
2010;81:107–11. http://dx.doi.org/10.1016/j.contraception.2009.07.008
71. Risser WL, Gefter LR, Barratt MS, Risser JM. Weight change in
adolescents who used hormonal contraception. J Adolesc Health
1999;24:433–6. http://dx.doi.org/10.1016/S1054-139X(98)00151-7
72. Segall-Gutierrez P, Xiang AH, Watanabe RM, et al. Deterioration in
cardiometabolic risk markers in obese women during depot
medroxyprogesterone acetate use. Contraception 2012;85:36–41. http://
dx.doi.org/10.1016/j.contraception.2011.04.016
73. Westhoff C, Jain JK, Milsom I, Ray A. Changes in weight with depot
medroxyprogesterone acetate subcutaneous injection 104 mg/0.65 mL.
Contraception 2007;75:261–7. http://dx.doi.org/10.1016/j.
contraception.2006.12.009
74. Paulen ME, Zapata LB, Cansino C, Curtis KM, Jamieson DJ. Contraceptive
use among women with a history of bariatric surgery: a systematic review.
Contraception 2010;82:86–94. http://dx.doi.org/10.1016/j.
contraception.2010.02.008
75. World Health Organization Collaborative Study of Cardiovascular
Disease and Steroid Hormone Contraception. Cardiovascular disease
and use of oral and injectable progestogen-only contraceptives and
combined injectable contraceptives. Results of an international,
multicenter, case-control study. Contraception 1998;57:315–24 http://
dx.doi.org/10.1016/S0010-7824(98)00041-9
76. Heinemann LA, Assmann A, DoMinh T, Garbe E. Oral progestogen-
only contraceptives and cardiovascular risk: results from the Transnational
Study on Oral Contraceptives and the Health of Young Women. Eur J
Contracept Reprod Health Care 1999;4:67–73. http://dx.doi.
org/10.3109/13625189909064007
77. Vasilakis C, Jick H, del Mar Melero-Montes M. Risk of idiopathic venous
thromboembolism in users of progestagens alone. Lancet 1999;354:1610–1.
http://dx.doi.org/10.1016/S0140-6736(99)04394-9
78. Sönmezer M, Atabekoğlu C, Cengiz B, Dökmeci F, Cengiz SD. Depot-
medroxyprogesterone acetate in anticoagulated patients with previous
hemorrhagic corpus luteum. Eur J Contracept Reprod Health Care
2005;10:9–14. http://dx.doi.org/10.1080/13625180400020952
79. Tepper NK, Paulen ME, Marchbanks PA, Curtis KM. Safety of
contraceptive use among women with peripartum cardiomyopathy: a
systematic review. Contraception 2010;82:95–101. http://dx.doi.
org/10.1016/j.contraception.2010.02.004
80. The Criteria Committee of the New York Heart Association.
Nomenclature and criteria for diagnosis of diseases of the heart and great
vessels. 9th ed. Boston, MA: Little, Brown and Co; 1994.
81. Bernatsky S, Clarke A, Ramsey-Goldman R, et al. Hormonal exposures
and breast cancer in a sample of women with systemic lupus erythematosus.
Rheumatology (Oxford) 2004;43:1178–81. http://dx.doi.org/10.1093/
rheumatology/keh282
Recommendations and Reports
52 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
82. Bernatsky S, Ramsey-Goldman R, Gordon C, et al. Factors associated
with abnormal Pap results in systemic lupus erythematosus.
Rheumatology (Oxford) 2004;43:1386–9. http://dx.doi.org/10.1093/
rheumatology/keh331
83. Chopra N, Koren S, Greer WL, et al. Factor V Leiden, prothrombin
gene mutation, and thrombosis risk in patients with antiphospholipid
antibodies. J Rheumatol 2002;29:1683–8.
84. Esdaile JM, Abrahamowicz M, Grodzicky T, et al. Traditional Framingham
risk factors fail to fully account for accelerated atherosclerosis in systemic
lupus erythematosus. Arthritis Rheum 2001;44:2331–7. http://dx.doi.
org/10.1002/1529-0131(200110)44:10<2331::AID-ART395≥3.0.CO;2-I
85. Julkunen HA. Oral contraceptives in systemic lupus erythematosus:
side-effects and influence on the activity of SLE. Scand J Rheumatol
1991;20:427–33. http://dx.doi.org/10.3109/03009749109096822
86. Julkunen HA, Kaaja R, Friman C. Contraceptive practice in women
with systemic lupus erythematosus. Br J Rheumatol 1993;32:227–30.
http://dx.doi.org/10.1093/rheumatology/32.3.227
87. Jungers P, Dougados M, Pélissier C, et al. Influence of oral contraceptive
therapy on the activity of systemic lupus erythematosus. Arthritis Rheum
1982;25:618–23. http://dx.doi.org/10.1002/art.1780250603
88. Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of
myocardial infarction and angina in women with systemic lupus
erythematosus: comparison with the Framingham Study. Am J Epidemiol
1997;145:408–15. http://dx.doi.org/10.1093/oxfordjournals.aje.a009122
89. McAlindon T, Giannotta L, Taub N, D’Cruz D, Hughes G. Environmental
factors predicting nephritis in systemic lupus erythematosus. Ann Rheum
Dis 1993;52:720–4. http://dx.doi.org/10.1136/ard.52.10.720
90. McDonald J, Stewart J, Urowitz MB, Gladman DD. Peripheral vascular
disease in patients with systemic lupus erythematosus. Ann Rheum Dis
1992;51:56–60. http://dx.doi.org/10.1136/ard.51.1.56
91. Mintz G, Gutiérrez G, Delezé M, Rodríguez E. Contraception with
progestagens in systemic lupus erythematosus. Contraception
1984;30:29–38. http://dx.doi.org/10.1016/0010-7824(84)90076-3
92. Petri M. Musculoskeletal complications of systemic lupus erythematosus
in the Hopkins Lupus Cohort: an update. Arthritis Care Res
1995;8:137–45. http://dx.doi.org/10.1002/art.1790080305
93. Petri M. Lupus in Baltimore: evidence-based ‘clinical pearls’ from the
Hopkins Lupus Cohort. Lupus 2005;14:970–3. http://dx.doi.
org/10.1191/0961203305lu2230xx
94. Petri M, Kim MY, Kalunian KC, et al; OC-SELENA Trial. Combined
oral contraceptives in women with systemic lupus erythematosus. N Engl
J Med 2005;353:2550–8. http://dx.doi.org/10.1056/NEJMoa051135
95. Sánchez-Guerrero J, Uribe AG, Jiménez-Santana L, et al. A trial of
contraceptive methods in women with systemic lupus erythematosus. N
Engl J Med 2005;353:2539–49. http://dx.doi.org/10.1056/NEJMoa050817
96. Sarabi ZS, Chang E, Bobba R, et al. Incidence rates of arterial and venous
thrombosis after diagnosis of systemic lupus erythematosus. Arthritis
Rheum 2005;53:609–12. http://dx.doi.org/10.1002/art.21314
97. Schaedel ZE, Dolan G, Powell MC. The use of the levonorgestrel-releasing
intrauterine system in the management of menorrhagia in women with
hemostatic disorders. Am J Obstet Gynecol 2005;193:1361–3. http://dx.doi.
org/10.1016/j.ajog.2005.05.002
98. Somers E, Magder LS, Petri M. Antiphospholipid antibodies and
incidence of venous thrombosis in a cohort of patients with systemic
lupus erythematosus. J Rheumatol 2002;29:2531–6.
99. Urowitz MB, Bookman AA, Koehler BE, Gordon DA, Smythe HA, Ogryzlo
MA. The bimodal mortality pattern of systemic lupus erythematosus. Am J
Med 1976;60:221–5. http://dx.doi.org/10.1016/0002-9343(76)90431-9
100. Choojitarom K, Verasertniyom O, Totemchokchyakarn K, Nantiruj K,
Sumethkul V, Janwityanujit S. Lupus nephritis and Raynaud’s phenomenon
are significant risk factors for vascular thrombosis in SLE patients with
positive antiphospholipid antibodies. Clin Rheumatol 2008;27:345–51.
http://dx.doi.org/10.1007/s10067-007-0721-z
101. Wahl DG, Guillemin F, de Maistre E, Perret C, Lecompte T, Thibaut
G. Risk for venous thrombosis related to antiphospholipid antibodies
in systemic lupus erythematosus—a meta-analysis. Lupus 1997;6:467–
73. http://dx.doi.org/10.1177/096120339700600510
102. Farr SL, Folger SG, Paulen ME, Curtis KM. Safety of contraceptive methods
for women with rheumatoid arthritis: a systematic review. Contraception
2010;82:64–71. http://dx.doi.org/10.1016/j.contraception.2010.02.003
103. Tepper NK, Whiteman MK, Zapata LB, Marchbanks PA, Curtis KM.
Safety of hormonal contraceptives among women with migraine: a
systematic review. Contraception 2016. Epub May 3, 2016. http://
dx.doi.org/10.1016/j.contraception.2016.04.016
104. Tepper NK, Whiteman MK, Marchbanks PA, James AH, Curtis KM.
Progestin-only contraception and thromboembolism: a systematic
review. Contraception 2016. Epub May 3, 2016. http://dx.doi.
org/10.1016/j.contraception.2016.04.014
105. Zapata LB, Oduyebo T, Whiteman MK, Marchbanks PA, Curtis KM.
Contraceptive use among women with multiple sclerosis: a systematic
review. Contraception. In press 2016.
106. Pagano HP, Zapata LB, Berry-Bibee EN, Nanda K, Curtis KM. Safety of
hormonal contraception and intrauterine devices among women with
depressive and bipolar disorders: a systematic review. Contraception 2016.
Epub June 27, 2016. http://dx.doi.org/10.1016/j.contraception.2016.06.012
107. Smith JS, Green J, Berrington de Gonzalez A, et al. Cervical cancer and
use of hormonal contraceptives: a systematic review. Lancet 2003;361:1159–
67. http://dx.doi.org/10.1016/S0140-6736(03)12949-2.
108. Polis CB, Phillips SJ, Curtis KM, et al. Hormonal contraceptive
methods and risk of HIV acquisition in women: a systematic review
of epidemiological evidence. Contraception 2014;90:360–90 http://
dx.doi.org/10.1016/j.contraception.2014.07.009
109. Phillips SJ, Curtis KM, Polis CB. Effect of hormonal contraceptive
methods on HIV disease progression: a systematic review. AIDS
2013;27:787–94. http://dx.doi.org/10.1097/QAD.0b013e32835bb672
110. Polis CB, Phillips SJ, Curtis KM. Hormonal contraceptive use and
female-to-male HIV transmission: a systematic review of the
epidemiologic evidence. AIDS 2013;27:493–505. http://dx.doi.
org/10.1097/QAD.0b013e32835ad539
111. Phillips SJ, Polis CB, Curtis KM. The safety of hormonal contraceptives
for women living with HIV and their sexual partners. Contraception
2016;93:11–6 http://dx.doi.org/10.1016/j.contraception.2015.10.002.
112. Tagy AH, Saker ME, Moussa AA, Kolgah A. The effect of low-dose
combined oral contraceptive pills versus injectable contraceptive (Depot
Provera) on liver function tests of women with compensated bilharzial
liver fibrosis. Contraception 2001;64:173–6. http://dx.doi.org/10.1016/
S0010-7824(01)00248-7
113. Pyörälä T, Vähäpassi J, Huhtala M. The effect of lynestrenol and
norethindrone on the carbohydrate and lipid metabolism in subjects
with gestational diabetes. Ann Chir Gynaecol 1979;68:69–74.
114. Rådberg T, Gustafson A, Skryten A, Karlsson K. Metabolic studies in
gestational diabetic women during contraceptive treatment: effects on
glucose tolerance and fatty acid composition of serum lipids. Gynecol
Obstet Invest 1982;13:17–29. http://dx.doi.org/10.1159/000299480
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 53
US Department of Health and Human Services/Centers for Disease Control and Prevention
115. Kjos SL, Peters RK, Xiang A, Thomas D, Schaefer U, Buchanan TA.
Contraception and the risk of type 2 diabetes mellitus in Latina women
with prior gestational diabetes mellitus. JAMA 1998;280:533–8. http://
dx.doi.org/10.1001/jama.280.6.533
116. Nelson AL, Le MH, Musherraf Z, Vanberckelaer A. Intermediate-term
glucose tolerance in women with a history of gestational diabetes:
natural history and potential associations with breastfeeding and
contraception. Am J Obstet Gynecol 2008;198:699.e1–8.
117. Xiang AH, Kawakubo M, Buchanan TA, Kjos SL. A longitudinal study
of lipids and blood pressure in relation to method of contraception in
Latino women with prior gestational diabetes mellitus. Diabetes Care
2007;30:1952–8. http://dx.doi.org/10.2337/dc07-0180
118. Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable
progestin contraception and risk of type 2 diabetes in Latino women
with prior gestational diabetes mellitus. Diabetes Care 2006;29:613–7.
http://dx.doi.org/10.2337/diacare.29.03.06.dc05-1940
119. Diab KM, Zaki MM. Contraception in diabetic women: comparative
metabolic study of Norplant, depot medroxyprogesterone acetate, low dose
oral contraceptive pill and CuT380A. J Obstet Gynaecol Res 2000;26:17–
26. http://dx.doi.org/10.1111/j.1447-0756.2000.tb01195.x
120. Lunt H, Brown LJ. Self-reported changes in capillary glucose
and insulin requirements during the menstrual cycle. Diabet
Med 1996;13:525–30. http://dx.doi.org/10.1002/
(SICI)1096-9136(199606)13:6<525::AID-DIA123≥3.0.CO;2-D
121. Rådberg T, Gustafson A, Skryten A, Karlsson K. Oral contraception
in diabetic women. A cross-over study on serum and high density
lipoprotein (HDL) lipids and diabetes control during progestogen and
combined estrogen/progestogen contraception. Horm Metab Res
1982;14:61–5.
122. Skouby SO, Mølsted-Pedersen L, Kühl C, Bennet P. Oral contraceptives
in diabetic women: metabolic effects of four compounds with different
estrogen/progestogen profiles. Fertil Steril 1986;46:858–64 http://
dx.doi.org/10.1016/S0015-0282(16)49825-0.
123. Zapata LB, Paulen ME, Cansino C, Marchbanks PA, Curtis KM.
Contraceptive use among women with inflammatory bowel disease: a
systematic review. Contraception 2010;82:72–85. http://dx.doi.
org/10.1016/j.contraception.2010.02.012
124. Kapp N, Curtis KM. Hormonal contraceptive use among women with
liver tumors: a systematic review. Contraception 2009;80:387–90.
http://dx.doi.org/10.1016/j.contraception.2009.01.021
125. Whiteman MK, Oduyebo T, Zapata LB, Walker S, Curtis KM.
Contraceptive safety among women with cystic fibrosis: a systematic
review. Contraception 2016. Epub June 7, 2016. http://dx.doi.
org/10.1016/j.contraception.2016.05.016
1 26. Adadevoh BK, Isaacs WA. The effect of megestrol acetate on sickling. Am J Med Sci
1973;265:367–70. http://dx.doi.org/10.1097/00000441-197305000-00002
127. Barbosa IC, Ladipo OA, Nascimento ML, et al. Carbohydrate
metabolism in sickle cell patients using a subdermal implant containing
nomegestrol acetate (Uniplant). Contraception 2001;63:263–5. http://
dx.doi.org/10.1016/S0010-7824(01)00202-5
128. de Abood M, de Castillo Z, Guerrero F, Espino M, Austin KL. Effect
of Depo-Provera or Microgynon on the painful crises of sickle cell
anemia patients. Contraception 1997;56:313–6. http://dx.doi.
org/10.1016/S0010-7824(97)00156-X
129. De Ceulaer K, Hayes R, Gruber C, Serjeant GR. Medroxyprogesterone
acetate and homozygous sickle-cell disease. Lancet 1982;320:229–31.
http://dx.doi.org/10.1016/S0140-6736(82)90320-8
130. Howard RJ, Lillis C, Tuck SM. Contraceptives, counselling, and
pregnancy in women with sickle cell disease. BMJ 1993;306:1735–7.
http://dx.doi.org/10.1136/bmj.306.6894.1735
131. Ladipo OA, Falusi AG, Feldblum PJ, Osotimehin BO, Otolorin EO,
Ojengbede OA. Norplant use by women with sickle cell disease. Int J Gynaecol
Obstet 1993;41:85–7. http://dx.doi.org/10.1016/0020-7292(93)90159-T
132. Nascimento ML, Ladipo OA, Coutinho EM. Nomegestrol acetate
contraceptive implant use by women with sickle cell disease. Clin
Pharmacol Ther 1998;64:433–8. http://dx.doi.org/10.1016/
S0009-9236(98)90074-1
133. Yoong WC, Tuck SM, Yardumian A. Red cell deformability in oral
contraceptive pill users with sickle cell anaemia. Br J Haematol 1999;104:868–
70. http://dx.doi.org/10.1046/j.1365-2141.1999.01255.x
134. Aweeka FT, Rosenkranz SL, Segal Y, et al; NIAID AIDS Clinical Trials
Group. The impact of sex and contraceptive therapy on the plasma
and intracellular pharmacokinetics of zidovudine. AIDS 2006;20:1833–
41. http://dx.doi.org/10.1097/01.aids.0000244202.18629.36
135. Kearney BP, Mathias A. Lack of effect of tenofovir disoproxil fumarate
on pharmacokinetics of hormonal contraceptives. Pharmacotherapy
2009;29:924–9. http://dx.doi.org/10.1592/phco.29.8.924
136. Todd CS, Deese J, Wang M, et al; FEM-PrEP Study Group. Sino-implant
(II)® continuation and effect of concomitant tenofovir disoproxil
fumarate-emtricitabine use on plasma levonorgestrel concentrations
among women in Bondo, Kenya. Contraception 2015;91:248–52.
http://dx.doi.org/10.1016/j.contraception.2014.10.008
137. Murnane PM, Heffron R, Ronald A, et al; Partners PrEP Study Team.
Pre-exposure prophylaxis for HIV-1 prevention does not diminish the
pregnancy prevention effectiveness of hormonal contraception. AIDS
2014;28:1825–30. http://dx.doi.org/10.1097/QAD.0000000000000290
138. Kasonde M, Niska RW, Rose C, et al. Bone mineral density changes among
HIV-uninfected young adults in a randomised trial of pre-exposure
prophylaxis with tenofovir-emtricitabine or placebo in Botswana. PLoS
One 2014;9:e90111. http://dx.doi.org/10.1371/journal.pone.0090111
139. Callahan R, Nanda K, Kapiga S, et al; FEM-PrEP Study Group.
Pregnancy and contraceptive use among women participating in the
FEM-PrEP trial. J Acquir Immune Defic Syndr 2015;68:196–203.
http://dx.doi.org/10.1097/QAI.0000000000000413
140. Vieira CS, Bahamondes MV, de Souza RM, et al. Effect of antiretroviral
therapy including lopinavir/ritonavir or efavirenz on etonogestrel-
releasing implant pharmacokinetics in HIV-positive women. J Acquir
Immune Defic Syndr 2014;66:378–85. http://dx.doi.org/10.1097/
QAI.0000000000000189
141. Patel RC, Onono M, Gandhi M, et al. Pregnancy rates in HIV-positive
women using contraceptives and efavirenz-based or nevirapine-based
antiretroviral therapy in Kenya: a retrospective cohort study. Lancet HIV
2015;2:e474–82. http://dx.doi.org/10.1016/S2352-3018(15)00184-8
142. Perry SH, Swamy P, Preidis GA, Mwanyumba A, Motsa N, Sarero HN.
Implementing the Jadelle implant for women living with HIV in a
resource-limited setting: concerns for drug interactions leading to
unintended pregnancies. AIDS 2014;28:791–3. http://dx.doi.
org/10.1097/QAD.0000000000000177
143. Scarsi KK, Darin KM, Nakalema S, et al. Unintended pregnancies
observed with combined use of the levonorgestrel contraceptive implant
and efavirenz-based antiretroviral therapy: a three-arm pharmacokinetic
evaluation over 48 weeks. Clin Infect Dis 2015;62:675–82. http://
dx.doi.org/10.1093/cid/civ1001
Recommendations and Reports
54 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
144. Pyra M, Heffron R, Mugo NR, et al; Partners in Prevention HSVHIV
Transmission Study and Partners PrEP Study Teams. Effectiveness of
hormonal contraception in HIV-infected women using antiretroviral
therapy. AIDS 2015;29:2353–9. http://dx.doi.org/10.1097/
QAD.0000000000000827
145. Cohn SE, Park JG, Watts DH, et al; ACTG A5093 Protocol Team. Depo-
medroxyprogesterone in women on antiretroviral therapy: effective
contraception and lack of clinically significant interactions. Clin Pharmacol
Ther 2007;81:222–7. http://dx.doi.org/10.1038/sj.clpt.6100040
146. Nanda K, Amaral E, Hays M, Viscola MA, Mehta N, Bahamondes L.
Pharmacokinetic interactions between depot medroxyprogesterone
acetate and combination antiretroviral therapy. Fertil Steril
2008;90:965–71. http://dx.doi.org/10.1016/j.fertnstert.2007.07.1348
147. Watts DH, Park JG, Cohn SE, et al. Safety and tolerability of depot
medroxyprogesterone acetate among HIV-infected women on
antiretroviral therapy: ACTG A5093. Contraception 2008;77:84–90.
http://dx.doi.org/10.1016/j.contraception.2007.10.002
148. Polis CB, Nakigozi G, Ssempijja V, et al. Effect of injectable
contraceptive use on response to antiretroviral therapy among women
in Rakai, Uganda. Contraception 2012;86:725–30. http://dx.doi.
org/10.1016/j.contraception.2012.05.001
149. Hubacher D, Liku J, Kiarie J, et al. Effect of concurrent use of anti-
retroviral therapy and levonorgestrel sub-dermal implant for contraception
on CD4 counts: a prospective cohort study in Kenya. J Int AIDS Soc
2013;16:18448. http://dx.doi.org/10.7448/IAS.16.1.18448
150. Myer L, Carter RJ, Katyal M, Toro P, El-Sadr WM, Abrams EJ. Impact
of antiretroviral therapy on incidence of pregnancy among HIV-infected
women in Sub-Saharan Africa: a cohort study. PLoS Med
2010;7:e1000229. http://dx.doi.org/10.1371/journal.pmed.1000229
151. Day S, Graham SM, Masese LN, et al. A prospective cohort study of
the effect of depot medroxyprogesterone acetate on detection of plasma
and cervical HIV-1 in women initiating and continuing antiretroviral
therapy. J Acquir Immune Defic Syndr 2014;66:452–6. http://dx.doi.
org/10.1097/QAI.0000000000000187
152. DuBois BN, Atrio J, Stanczyk FZ, Cherala G. Increased exposure of
norethindrone in HIV+ women treated with ritonavir-boosted
atazanavir therapy. Contraception 2015;91:71–5. http://dx.doi.
org/10.1016/j.contraception.2014.08.009
153. Luque AE, Cohn SE, Park JG, et al. Depot medroxyprogesterone acetate
in combination with a twice-daily lopinavir-ritonavir-based regimen
in HIV-infected women showed effective contraception and a lack of
clinically significant interactions, with good safety and tolerability:
results of the ACTG 5283 study. Antimicrob Agents Chemother
2015;59:2094–101. http://dx.doi.org/10.1128/AAC.04701-14
154. Odlind V, Olsson SE. Enhanced metabolism of levonorgestrel during
phenytoin treatment in a woman with Norplant implants. Contraception
1986;33:257–61. http://dx.doi.org/10.1016/0010-7824(86)90018-1
155. Schindlbeck C, Janni W, Friese K. Failure of Implanon contraception
in a patient taking carbamazepin for epilepsia. Arch Gynecol Obstet
2006;273:255–6. http://dx.doi.org/10.1007/s00404-005-0064-4
156. Shane-McWhorter L, Cerveny JD, MacFarlane LL, Osborn C.
Enhanced metabolism of levonorgestrel during phenobarbital treatment
and resultant pregnancy. Pharmacotherapy 1998;18:1360–4.
157. Reimers A, Helde G, Brodtkorb E. Ethinyl estradiol, not progestogens,
reduces lamotrigine serum concentrations. Epilepsia 2005;46:1414–7.
http://dx.doi.org/10.1111/j.1528-1167.2005.10105.x
158. Berry-Bibee E, Kim MJ, Simmons K, Pagano P, Curtis K. Drug
interactions between hormonal contraceptives and psychotropic drugs:
a systematic review. Contraception. In press 2016.
159. Berry-Bibee E, Kim MJ, Tepper N, Riley H, Curtis K. The safety of
St. John’s wort and hormonal contraceptives: a systematic review.
Contraception. In press 2016.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 55
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix D
Classifications for Combined Hormonal Contraceptives
Combined hormonal contraceptives (CHCs) include low-
dose (containing ≤35
µg ethinyl estradiol) combined oral
contraceptives (COCs), the combined hormonal patch, and
the combined vaginal ring (Box D1) (Table D1). Limited
information is available about the safety of the combined
hormonal patch and combined vaginal ring among women
with specific medical conditions. Evidence indicates that the
combined hormonal patch and the combined vaginal ring
provide comparable safety and pharmacokinetic profiles to
COCs with similar hormone formulations (1–33). Pending
further studies, the evidence available for recommendations
about COCs applies to the recommendations for the combined
hormonal patch and vaginal ring. Therefore, the patch and
ring should have the same categories as COCs, except where
noted. Therefore, the assigned categories should be considered
a preliminary best judgement, which will be reevaluated as new
data become available.
BOX D1. Categories for classifying combined hormonal contraceptives
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.
COCs, the patch, and the ring do not protect against
sexually transmitted diseases (STDs), including human
immunodeficiency virus (HIV), and women using these methods
should be counseled that consistent and correct use of the male
latex condom reduces the risk for transmission of HIV and other
STDs. Use of female condoms can provide protection from
transmission of STDs, although data are limited

Recommendations and Reports
56 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Personal Characteristics and Reproductive History
Pregnancy NA Clarication: Use of CHCs is not required. No known harm to the woman, the course of
her pregnancy, or the fetus occurs if CHCs are inadvertently used during pregnancy.
Age Evidence: Evidence is inconsistent about whether CHC use aects fracture risk
(34–45), although three recent studies show no eect (34,35,45). CHC use might
decrease BMD in adolescents, especially in those choosing very low-dose
formulations (COCs containing <30 µg ethinyl estradiol) (46–59). CHC use has little to
no eect on BMD in premenopausal women (60–74) and might preserve bone mass
in those who are perimenopausal (75–83). BMD is a surrogate marker for fracture risk
that might not be valid for premenopausal women and therefore might not
accurately predict current or future (postmenopausal) fracture risk (84–86).
Comment: The risk for cardiovascular disease increases with age and might
increase with CHC use. In the absence of other adverse clinical conditions, CHCs
can be used until menopause.
a. Menarche to <40 years 1
b. ≥40 years 2
Parity
a. Nulliparous 1 —
b. Parous 1 —
Breastfeeding
a. <21 days postpartum 4 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
b. 21 to <30 days postpartum
i. With other risk factors for VTE (e.g., age ≥35 years, previous VTE,
thrombophilia, immobility, transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
, postpartum hemorrhage,
postcesarean delivery, preeclampsia, or smoking)
3 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Clarication: For women with other risk factors for VTE, these risk factors might
increase the classication to a category 4.
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Evidence:
One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 57
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
ii. Without other risk factors for VTE 3 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
c. 30–42 days postpartum
i. With other risk factors for VTE (e.g., age ≥35 years, previous VTE,
thrombophilia, immobility, transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
, postpartum hemorrhage,
postcesarean delivery, preeclampsia, or smoking)
3 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Clarication: For women with other risk factors for VTE, these risk factors might
increase the classication to a category 4.
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
See table footnotes on page 69.

Recommendations and Reports
58 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
ii. Without other risk factors for VTE 2 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
d. >42 days postpartum 2 Clarication: Breastfeeding provides important health benets for mother and
infant. The U.S. Department of Health and Human Services recommends increasing
the proportion of infants initially breastfed, exclusively breastfed through 6 months
of life, and continuing breastfeeding through at least 1 year of life as key public
health goals (87).
Evidence: Clinical studies demonstrate conicting results regarding eects on
breastfeeding continuation or exclusivity in women exposed to COCs during
lactation. No consistent eects on infant growth or illness have been reported.
Adverse health outcomes or manifestations of exogenous estrogen in infants
exposed to CHCs through breast milk have not been demonstrated; however,
studies have been inadequately designed to determine whether a risk for either
serious or subtle long-term eects exists (88).
Comment: Certain women might be at risk for breastfeeding diculties, such as
women with previous breastfeeding diculties, certain medical conditions, or
certain perinatal complications, and those who deliver preterm. For these women,
as for all women, discussions about contraception for breastfeeding women should
include information about risks, benets, and alternatives.
Postpartum (nonbreastfeeding women)
a. <21 days postpartum 4 Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94). Risk for pregnancy during the
rst 21 days postpartum is very low but increases after that point; ovulation before
rst menses is common (95).
b. 21–42 days postpartum
i. With other risk factors for VTE (e.g., age ≥35 years, previous VTE,
thrombophilia, immobility, transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
postpartum hemorrhage,
postcesarean delivery, preeclampsia, or smoking)
3 Clarication: For women with other risk factors for VTE, these risk factors might
increase the classication to a category 4.
Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
ii. Without other risk factors for VTE 2 Evidence: One study examined use of CHCs during the postpartum period and
found that VTE rates were higher for CHC users compared with nonusers at all time
points postpartum (89). Rates were signicantly dierent only after 13 weeks
postpartum; however, the numbers needed to harm were lowest in the rst 6
weeks postpartum. VTE risk is increased during pregnancy and the postpartum
period; this risk is most pronounced in the rst 3 weeks after delivery, decreasing to
near baseline levels by 42 days postpartum (90–94).
c. >42 days postpartum 1 —
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 59
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Postabortion Clarication: CHCs may be started immediately postabortion.
Evidence: Women who started taking COCs immediately after rst trimester
medical or surgical abortion did not experience more side eects or adverse
vaginal bleeding outcomes or clinically signicant changes in coagulation
parameters than did women who used a placebo, an IUD, a nonhormonal
contraceptive method, or delayed COC initiation (96–102). Limited evidence on
women using the ring immediately after rst trimester medical or surgical abortion
found no serious adverse events and no infection related to use of the combined
vaginal ring during 3 cycles of follow-up postabortion (103).
a. First trimester 1
b. Second trimester 1
c. Immediate postseptic abortion 1
Past ectopic pregnancy 1 Comment: The risk for future ectopic pregnancy is increased among women who
have had an ectopic pregnancy in the past. CHCs protect against pregnancy in
general, including ectopic gestation.
History of pelvic surgery 1 —
Smoking Evidence: COC users who smoked were at increased risk for cardiovascular
diseases, especially myocardial infarction, compared with those who did not
smoke. Studies also showed an increased risk for myocardial infarction with
increasing number of cigarettes smoked per day (104–116).
a. Age <35 years 2
b. Age ≥35 years
i. <15 cigarettes per day 3
ii. ≥15 cigarettes per day 4
Obesity Evidence: Obese women who use COCs are more likely than obese women who do
not use COCs to experience VTE. Research examining the interaction between
COCs and BMI on VTE risk is limited, particularly for women in the highest BMI
categories (BMI ≥35 kg/m
2
). Although the absolute risk for VTE in otherwise
healthy women of reproductive age is small, obese women are at 2–3 times higher
risk for VTE than normal weight women regardless of COC use. Limited evidence
suggests that obese women who use COCs do not have a higher risk for acute
myocardial infarction or stroke than do obese nonusers (117). Limited evidence
suggests that eectiveness of some COC formulations might decrease with
increasing BMI, however the observed reductions in eectiveness are minimal and
evidence is conicting (118–125). Eectiveness of the patch might be reduced in
women >90 kg (126). Limited evidence suggests obese women are no more likely
to gain weight during COC or vaginal ring use than normal weight or overweight
women (117,127).
a. BMI ≥30 kg/m
2
2
b. Menarche to <18 years and BMI ≥30 kg/m
2
2
History of bariatric surgery
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease storage capacity of the stomach
(vertical banded gastroplasty, laparoscopic adjustable gastric band, or
laparoscopic sleeve gastrectomy)
1 Evidence: Limited evidence demonstrated no substantial decrease in eectiveness
of oral contraceptives among women who underwent laparoscopic placement of
an adjustable gastric band (128).
b. Malabsorptive procedures: decrease absorption of nutrients and
calories by shortening the functional length of the small intestine
(Roux-en-Y gastric bypass or biliopancreatic diversion)
COCs: 3
Patch and ring: 1
Evidence: Limited evidence demonstrated no substantial decrease in eectiveness
of oral contraceptives among women who underwent a biliopancreatic diversion;
however, evidence from pharmacokinetic studies reported conicting results of
oral contraceptive eectiveness among women who underwent a jejunoileal
bypass (128).
Comment: Bariatric surgical procedures involving a malabsorptive component
have the potential to decrease oral contraceptive eectiveness, perhaps further
decreased by postoperative complications, such as long-term diarrhea or vomiting.
Cardiovascular Disease
Multiple risk factors for atherosclerotic cardiovascular disease (e.g.,
older age, smoking, diabetes, hypertension, low HDL, high LDL, or high
triglyceride levels)
3/4 Clarication: When a woman has multiple major risk factors, any of which alone
would substantially increase her risk for cardiovascular disease, use of CHCs might
increase her risk to an unacceptable level. However, a simple addition of categories
for multiple risk factors is not intended; for example, a combination of two
category 2 risk factors might not necessarily warrant a higher category.
Clarication: The recommendations apply to known preexisting medical
conditions or characteristics. Few if any screening tests are needed before initiation
of contraception. See the U.S. Selected Practice Recommendations for Contraceptive
Use (http://www.cdc.gov/reproductivehealth/unintendedpregnancy/usspr.htm).
See table footnotes on page 69.

Recommendations and Reports
60 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Hypertension
Systolic blood pressure ≥160 mm Hg or diastolic blood pressure ≥100
mm Hg are associated with increased risk for adverse health events as a
result of pregnancy (Box 2).
a. Adequately controlled hypertension 3 Clarication: For all categories of hypertension, classications are based on the
assumption that no other risk factors exist for cardiovascular disease. When
multiple risk factors do exist, risk for cardiovascular disease might increase
substantially. A single reading of blood pressure level is not sucient to classify a
woman as hypertensive.
Clarication: Women adequately treated for hypertension are at reduced risk for
acute myocardial infarction and stroke compared with untreated women.
Although no data exist, CHC users with adequately controlled and monitored
hypertension should be at reduced risk for acute myocardial infarction and stroke
compared with untreated hypertensive CHC users.
Evidence: Among women with hypertension, COC users were at higher risk than
nonusers for stroke, acute myocardial infarction, and peripheral arterial disease
(104,106,113–116,129–143). Discontinuation of COCs in women with hypertension
might improve blood pressure control (144).
b. Elevated blood pressure levels
(properly taken measurements)
Clarication: For all categories of hypertension, classications are based on the
assumption that no other risk factors exist for cardiovascular disease. When
multiple risk factors do exist, risk for cardiovascular disease might increase
substantially. A single reading of blood pressure level is not sucient to classify a
woman as hypertensive.
Evidence: Among women with hypertension, COC users were at higher risk than
nonusers for stroke, acute myocardial infarction, and peripheral arterial disease
(104,106,113–116,129–143). Discontinuation of COCs in women with hypertension
might improve blood pressure control (144).
i. Systolic 140–159 mm Hg or diastolic 90–99 mm Hg 3
ii. Systolic ≥160 mm Hg or diastolic ≥100 mm Hg 4
c. Vascular disease 4
History of high blood pressure during pregnancy (when current blood
pressure is measurable and normal)
2 Evidence: Women with a history of high blood pressure in pregnancy who also
used COCs had a higher risk for myocardial infarction and VTE than did COC users
who did not have a history of high blood pressure during pregnancy. The absolute
risks for acute myocardial infarction and VTE in this population remained small
(115,130,142,143,145–151).
Deep venous thrombosis/Pulmonary embolism
a. History of DVT/PE, not receiving anticoagulant therapy
i. Higher risk for recurrent DVT/PE (one or more risk factors) 4 —
• History of estrogen-associated DVT/PE
• Pregnancy-associated DVT/PE
• Idiopathic DVT/PE
• Known thrombophilia, including antiphospholipid syndrome
• Active cancer (metastatic, receiving therapy, or within 6 months
after clinical remission), excluding nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE (no risk factors) 3 —
b. Acute DVT/PE 4 —
c. DVT/PE and established anticoagulant therapy for at least 3 months Clarication: Women using anticoagulant therapy are at risk for gynecologic
complications of therapy, such as hemorrhagic ovarian cysts and severe
menorrhagia. Hormonal contraceptive methods can be of benet in preventing or
treating these complications. When a contraceptive method is used as a therapy,
rather than solely to prevent pregnancy, the risk/benet ratio might dier and
should be considered on a case-by-case basis.
i. Higher risk for recurrent DVT/PE (one or more risk factors) 4
• Known thrombophilia, including antiphospholipid syndrome
• Active cancer (metastatic, receiving therapy, or within 6 months
after clinical remission), excluding nonmelanoma skin cancer
• History of recurrent DTV/PE
ii. Lower risk for recurrent DVT/PE (no risk factors) 3
d. Family history (rst-degree relatives) 2 Comment: Some conditions that increase the risk for DTV/PE are heritable.
e. Major surgery
i. With prolonged immobilization 4 —
ii. Without prolonged immobilization 2 —
f. Minor surgery without immobilization 1 —
Known thrombogenic mutations (e.g., factor V Leiden; prothrombin
mutation; and protein S, protein C, and antithrombin deciencies)
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
4 Clarication: Routine screening is not appropriate because of the rarity of the
conditions and the high cost of screening.
Evidence: Among women with thrombogenic mutations, COC users had a twofold
to twentyfold higher risk for thrombosis than did nonusers (152–175).
Supercial venous disorders
a. Varicose veins 1 Evidence: One study suggested that among women with varicose veins, the rate of
VTE and supercial venous thrombosis was higher in oral contraceptive users
compared with nonusers; however, statistical signicance was not reported and
the number of events was small (176).
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 61
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
b. Supercial venous thrombosis (acute or history) 3 Clarication: Supercial venous thrombosis might be associated with an increased risk
for VTE. If a woman has risk factors for concurrent DVT (e.g., known thrombophilia or
cancer) or has current or history of DVT, see recommendations for DVT/PE. Supercial
venous thrombosis associated with a peripheral intravenous catheter is less likely to be
associated with additional thrombosis and use of CHCs may be considered.
Evidence: One study demonstrated that among women with supercial venous
thrombosis, the risk for VTE was higher in oral contraceptive users compared with
nonusers (176).
Current and history of ischemic heart disease
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
4 —
Stroke (history of cerebrovascular accident)
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
4 —
Valvular heart disease
Complicated valvular heart disease is associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
a. Uncomplicated 2 —
b. Complicated (pulmonary hypertension, risk for atrial brillation, or
history of subacute bacterial endocarditis)
4 Comment: Among women with valvular heart disease, CHC use may further
increase the risk for arterial thrombosis; women with complicated valvular heart
disease are at greatest risk.
Peripartum cardiomyopathy
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
Evidence: No direct evidence exists about the safety of CHCs among women with
peripartum cardiomyopathy. Limited indirect evidence from noncomparative
studies of women with cardiac disease demonstrated few cases of hypertension
and transient ischemic attack in women with cardiac disease using COCs. No cases
of heart failure were reported (177).
Comment: COCs might increase uid retention in healthy women; uid retention
may worsen heart failure in women with peripartum cardiomyopathy. COCs might
induce cardiac arrhythmias in healthy women; women with peripartum
cardiomyopathy have a high incidence of cardiac arrhythmias.
a. Normal or mildly impaired cardiac function (New York Heart
Association Functional Class I or II: patients with no limitation of
activities or patients with slight, mild limitation of activity) (178)
i. <6 months 4
ii. ≥6 months 3
b. Moderately or severely impaired cardiac function (New York Heart
Association Functional Class III or IV: patients with marked limitation of
activity or patients who should be at complete rest) (178)
4
Rheumatic Diseases
Systemic lupus erythematosus
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Positive (or unknown) antiphospholipid antibodies 4 Clarication: Persons with SLE are at increased risk for ischemic heart disease, stroke,
and VTE. Categories assigned to such conditions in U.S. MEC should be the same for
women with SLE who have these conditions. For all subconditions of SLE,
classications are based on the assumption that no other risk factors for cardiovascu-
lar disease are present; these classications must be modied in the presence of such
risk factors. Many women with SLE can be considered good candidates for most
contraceptive methods, including hormonal contraceptives (179–197).
Evidence: Antiphospholipid antibodies are associated with a higher risk for both
arterial and venous thrombosis (198,199).
b. Severe thrombocytopenia 2 Clarication: Persons with SLE are at increased risk for ischemic heart disease, stroke,
and VTE. Categories assigned to such conditions in U.S. MEC should be the same for
women with SLE who have these conditions. For all subconditions of SLE,
classications are based on the assumption that no other risk factors for cardiovascu-
lar disease are present; these classications must be modied in the presence of such
risk factors. Many women with SLE can be considered good candidates for most
contraceptive methods, including hormonal contraceptives (179–197).
c. Immunosuppressive therapy 2 Clarication: Persons with SLE are at increased risk for ischemic heart disease, stroke,
and VTE. Categories assigned to such conditions in U.S. MEC should be the same for
women with SLE who have these conditions. For all subconditions of SLE,
classications are based on the assumption that no other risk factors for cardiovascu-
lar disease are present; these classications must be modied in the presence of such
risk factors. Many women with SLE can be considered good candidates for most
contraceptive methods, including hormonal contraceptives (179–
197).
d. None of the above 2 Clarication: Persons with SLE are at increased risk for ischemic heart disease, stroke,
and VTE. Categories assigned to such conditions in U.S. MEC should be the same for
women with SLE who have these conditions. For all subconditions of SLE,
classications are based on the assumption that no other risk factors for cardiovascu-
lar disease are present; these classications must be modied in the presence of such
risk factors. Many women with SLE can be considered good candidates for most
contraceptive methods, including hormonal contraceptives (179–197).
See table footnotes on page 69.

Recommendations and Reports
62 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Rheumatoid arthritis Evidence: Limited evidence shows no consistent pattern of improvement or
worsening of rheumatoid arthritis with use of oral contraceptives, progesterone, or
estrogen (200).
a. Receiving immunosuppressive therapy 2
b. Not receiving immunosuppressive therapy 2
Neurologic Conditions
Headaches
a. Nonmigraine (mild or severe) 1 Clarication: Classication depends on accurate diagnosis of those severe
headaches that are migraines and those headaches that are not, as well as
diagnosis of ever experiencing aura. Aura is a specic focal neurologic symptom.
For more information about headache classication see The International Headache
Society Classication, 3rd edition (http://www.ihs-classication.org/_downloads/
mixed/International-Headache-Classication-III-ICHD-III-2013-Beta.pdf). Any new
headaches or marked changes in headaches should be evaluated.
b. Migraine Clarication: Classication depends on accurate diagnosis of those severe
headaches that are migraines and those headaches that are not, as well as
diagnosis of ever experiencing aura. Aura is a specic focal neurologic symptom.
For more information about headache classication see The International Headache
Society Classication, 3rd edition (http://www.ihs-classication.org/_downloads/
mixed/International-Headache-Classication-III-ICHD-III-2013-Beta.pdf). Any new
headaches or marked changes in headaches should be evaluated.
Clarication: Classication is for women without any other risk factors for stroke
(e.g., age, hypertension, and smoking).
Evidence: Among women with migraine, oral contraceptive use is associated with
about a threefold increased risk for ischemic stroke compared with nonuse,
although most studies did not specify migraine type or oral contraceptive
formulation. The only study to examine migraine type found that the risk for
ischemic stroke among women with migraine with aura was increased to a similar
level among both oral contraceptive users and nonusers, compared with women
without migraine (201). The risk for ischemic stroke is increased among women
using COCs, compared with women not using COCs (104,202). The risk for ischemic
stroke is also increased among women with migraine with aura, compared with
women without migraine (203–205). One older meta-analysis found that migraine
without aura was associated with an increased risk for ischemic stroke, while two
more recent meta-analyses did not nd such an association (203–205).
Comment: Menstrual migraine is a subtype of migraine without aura. For more
information, see The International Headache Society Classication, 3rd edition (http://
www.ihs-classication.org/_downloads/mixed/International-Headache-
Classication-III-ICHD-III-2013-Beta.pdf).
i. Without aura (This category of migraine includes
menstrual migraine.)
2
ii. With aura 4
Epilepsy
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
1 Clarication: If a woman is taking anticonvulsants, see Drug Interactions section.
Certain anticonvulsants lower COC eectiveness. The extent to which patch or ring
use is similar to COC use in this regard remains unclear.
Multiple sclerosis Evidence: Limited evidence suggests that use of COCs or oral contraceptives (type
not specied) among women with multiple sclerosis does not worsen the clinical
course of disease (206).
Comment: No data exist that evaluate the increased risk for VTE among women
with multiple sclerosis using CHCs. However, women with multiple sclerosis are at
higher risk than unaected women for VTE.
a. With prolonged immobility 3
b. Without prolonged immobility 1
Depressive Disorders
Depressive disorders 1 Clarication: If a woman is receiving psychotropic medications or St. John’s wort,
see Drug Interactions section.
Evidence: COC use was not associated with increased depressive symptoms in
women with depression or scoring above threshold levels on a validated
depression screening instrument compared with baseline or with nonusers with
depression. One small study of women with bipolar disorder found that oral
contraceptives did not signicantly change mood across the menstrual cycle (207).
Reproductive Tract Infections and Disorders
Vaginal bleeding patterns
a. Irregular pattern without heavy bleeding 1 Comment: Irregular menstrual bleeding patterns are common among healthy women.
b. Heavy or prolonged bleeding (includes regular and
irregular patterns)
1 Clarication: Unusually heavy bleeding should raise the suspicion of a serious
underlying condition.
Evidence: A Cochrane Collaboration Review identied one randomized controlled
trial evaluating the eectiveness of COC use compared with naproxen and danazol
in treating menorrhagia. Women with menorrhagia did not report worsening of
the condition or any adverse events related to COC use (208).
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 63
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Unexplained vaginal bleeding
(suspicious for serious condition) before evaluation
2 Clarication: If pregnancy or an underlying pathological condition (e.g., pelvic
malignancy) is suspected, it must be evaluated and the category adjusted
after evaluation.
Comment: No conditions that cause vaginal bleeding will be worsened in the
short-term by use of CHCs.
Endometriosis 1 Evidence: A Cochrane Collaboration Review identied one randomized controlled
trial evaluating the eectiveness of COC use compared with a gonadotropin-
releasing hormone analog in treating the symptoms of endometriosis. Women
with endometriosis did not report worsening of the condition or any adverse
events related to COC use (209).
Benign ovarian tumors (including cysts) 1
Severe dysmenorrhea 1 Evidence: Risk for side eects with COC use was not higher among women with
dysmenorrhea than among women not using COCs. Some COC users had a
reduction in pain and bleeding (210,211).
Gestational trophoblastic disease
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
Clarication: For all subconditions of gestational trophoblastic disease,
classications are based on the assumption that women are under close medical
supervision because of the need for monitoring of β-hCG levels for appropriate
disease surveillance.
Evidence: After molar pregnancy evacuation, the balance of evidence found COC use
did not increase the risk for postmolar trophoblastic disease, and β–hCG levels
regressed more rapidly in some COC users than in nonusers (212). Limited evidence
suggests that use of COCs during chemotherapy does not signicantly aect the
regression or treatment of postmolar trophoblastic disease compared with women
who used a nonhormonal contraceptive method or DMPA during chemotherapy (212).
a. Suspected gestational trophoblastic disease (immediate
postevacuation)
i. Uterine size rst trimester 1
ii. Uterine size second trimester 1
b. Conrmed gestational trophoblastic disease (after initial evacuation
and during monitoring)
i. Undetectable/nonpregnant β-hCG levels 1
ii. Decreasing β-hCG levels 1
iii. Persistently elevated β-hCG levels or malignant disease, with no
evidence or suspicion of intrauterine disease
1
iv. Persistently elevated β-hCG levels or malignant disease, with
evidence or suspicion of intrauterine disease
1
Cervical ectropion 1 Comment: Cervical ectropion is not a risk factor for cervical cancer, and restriction
of CHC use is unnecessary.
Cervical intraepithelial neoplasia 2 Evidence: Among women with persistent human papillomavirus infection,
long-term COC use (≥5 years) might increase the risk for carcinoma in situ and
invasive carcinoma (213). Limited evidence on women with low-grade squamous
intraepithelial lesions found use of the vaginal ring did not worsen the condition (9).
Cervical cancer (awaiting treatment) 2 Comment: Theoretical concern exists that CHC use might aect prognosis of the
existing disease. While awaiting treatment, women may use CHCs. In general,
treatment of this condition can render a woman sterile.
Breast disease
Breast cancer is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Undiagnosed mass 2 Clarication: The woman should be evaluated as early as possible.
b. Benign breast disease 1 —
c. Family history of cancer 1 Evidence: Women with breast cancer susceptibility genes (e.g., BRCA1 and BRCA2)
have a higher baseline risk for breast cancer than women without these genes. The
baseline risk for breast cancer is also higher among women with a family history of
breast cancer than among those who do not have such a history. However,
evidence does not suggest that the increased risk for breast cancer among women
with either a family history of breast cancer or breast cancer susceptibility genes is
modied by the use of COCs (214–231).
d. Breast cancer Comment: Breast cancer is a hormonally sensitive tumor, and the prognosis for
women with current or recent breast cancer might worsen with CHC use.
i. Current 4
ii. Past and no evidence of current disease for 5 years 3
Endometrial hyperplasia 1 —
Endometrial cancer
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
1 Comment: COC use reduces the risk for endometrial cancer; whether patch or ring
use reduces the risk for endometrial cancer is not known. While awaiting
treatment, women may use CHCs. In general, treatment of this condition renders a
woman sterile.
Ovarian cancer
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
1 Comment: COC use reduces the risk for ovarian cancer; whether patch or ring use
reduces the risk for ovarian cancer is not known. While awaiting treatment, women
may use CHCs. In general, treatment of this condition can render a woman sterile.
Uterine broids 1 Comment: COCs do not appear to cause growth of uterine broids, and patch and
ring also are not expected to cause growth.
See table footnotes on page 69.

Recommendations and Reports
64 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Pelvic inammatory disease Comment: COCs might reduce the risk for PID among women with STDs but do
not protect against HIV or lower genital tract STDs. Whether use of patch or ring
reduces the risk for PID among women with STDs is unknown; however, they do
not protect against HIV or lower genital tract STDs.
a. Past PID
i. With subsequent pregnancy 1
ii. Without subsequent pregnancy 1
b. Current PID 1
Sexually transmitted diseases
a. Current purulent cervicitis or chlamydial infection or gonococcal
infection
1 —
b. Vaginitis (including Trichomonas vaginalis and bacterial vaginosis) 1 —
c. Other factors related to STDs 1 —
HIV
High risk for HIV 1 Evidence: Overall, evidence does not support an association between oral
contraceptives and risk for HIV acquisition (232).
HIV infection
For women with HIV infection who are not clinically well or not receiving
ARV therapy, this condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 Clarication: Drug interactions might exist between hormonal contraceptives and
ARV drugs; see Drug Interactions section.
Evidence: Overall, evidence does not support an association between COC use and
progression of HIV. Limited direct evidence does not support an association
between COC use and transmission of HIV to noninfected partners; studies
measuring genital viral shedding as a proxy for infectivity have had mixed results.
Studies measuring whether hormonal contraceptive methods aect plasma HIV
viral load generally have found no eect (233–235).
Other Infections
Schistosomiasis
Schistosomiasis with brosis of the liver is associated with increased risk
for adverse health events as a result of pregnancy (Box 2).
a. Uncomplicated 1 Evidence: Among women with uncomplicated schistosomiasis, COC use had no
adverse eects on liver function (236–242).
b. Fibrosis of the liver (if severe, see Cirrhosis section) 1 —
Tuberculosis
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
Clarication: If a woman is taking rifampin, see Drug Interactions section. Rifampin
is likely to decrease COC eectiveness. The extent to which patch or ring use is
similar to COC use in this regard remains unclear.
a. Nonpelvic 1
b. Pelvic 1
Malaria 1 —
Endocrine Conditions
Diabetes
Insulin-dependent diabetes; diabetes with nephropathy, retinopathy, or
neuropathy; diabetes with other vascular disease; or diabetes of
>20 years’ duration are associated with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. History of gestational disease 1 Evidence: The development of non–insulin-dependent diabetes in women with a
history of gestational diabetes is not increased by use of COCs (243–250). Likewise,
lipid levels appear to be unaected by COC use (251–253).
b. Nonvascular disease Evidence: Among women with insulin-dependent or non–insulin-dependent
diabetes, COC use had limited eect on daily insulin requirements and no eect on
long-term diabetes control (e.g., glycosylated hemoglobin levels) or progression to
retinopathy. Changes in lipid prole and hemostatic markers were limited, and
most changes remained within normal values (254–263).
i. Non-insulin dependent 2
ii. Insulin dependent 2
c. Nephropathy, retinopathy, or neuropathy 3/4
Clarication: The category should be assessed according to the severity of the condition.
d. Other vascular disease or diabetes of >20 years’ duration 3/4 Clarication: The category should be assessed according to the severity of the condition.
Thyroid disorders
a. Simple goiter 1 —
b. Hyperthyroid 1 —
c. Hypothyroid 1 —
Gastrointestinal Conditions
Inammatory bowel disease (ulcerative colitis or Crohn’s disease) 2/3 Clarication: For women with mild IBD and with no other risk factor for VTE, the
benets of CHC use generally outweigh the risks (category 2). However, for women
with IBD who are at increased risk for VTE (e.g., those with active or extensive
disease, surgery, immobilization, corticosteroid use, vitamin deciencies, or uid
depletion), the risks of CHC use generally outweigh the benets (category 3).
Evidence: Risk for disease relapse was not signicantly higher among women with
IBD using oral contraceptives (most studies did not specify type) than among
nonusers (264). Absorption of COCs among women with mild ulcerative colitis and
no or small ileal resections was similar to the absorption among healthy women
(264). Findings might not apply to women with Crohn’s disease or more extensive
bowel resections. No data exist that evaluate the increased risk for VTE among
women with IBD using CHCs. However, women with IBD are at higher risk than
unaected women for VTE (264).
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 65
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
Gallbladder disease Comment: CHCs might cause a small increased risk for gallbladder disease. CHCs
might worsen existing gallbladder disease.
a. Symptomatic
i. Treated by cholecystectomy 2
ii. Medically treated 3
iii. Current 3
b. Asymptomatic 2
History of cholestasis
a. Pregnancy related 2 Comment: History of pregnancy-related cholestasis might predict an increased risk
for COC-related cholestasis.
b. Past COC related 3 Comment: History of COC-related cholestasis predicts an increased risk with
subsequent COC use.
Viral hepatitis Initiation Continuation
a. Acute or are 3/4 2 Clarication (initiation): The category should be assessed according to the severity
of the condition.
Evidence: Data suggest that in women with chronic hepatitis, COC use does not
increase the rate or severity of cirrhotic brosis, nor does it increase the risk for
hepatocellular carcinoma. For women who are carriers, COC use does not appear
to trigger liver failure or severe dysfunction. Evidence is limited for COC use during
active hepatitis (265).
b. Carrier 1 1 Evidence: Data suggest that in women with chronic hepatitis, COC use does not
increase the rate or severity of cirrhotic brosis, nor does it increase the risk for
hepatocellular carcinoma. For women who are carriers, COC use does not appear
to trigger liver failure or severe dysfunction. Evidence is limited for COC use during
active hepatitis (265).
c. Chronic 1 1 Evidence: Data suggest that in women with chronic hepatitis, COC use does not
increase the rate or severity of cirrhotic brosis, nor does it increase the risk for
hepatocellular carcinoma. For women who are carriers, COC use does not appear
to trigger liver failure or severe dysfunction. Evidence is limited for COC use during
active hepatitis (265).
Cirrhosis
Severe cirrhosis is associated with increased risk for adverse health
events as a result of pregnancy (Box 2).
a. Mild (compensated) 1 —
b. Severe (decompensated) 4 —
Liver tumors
Hepatocellular adenoma and malignant liver tumors are associated with
increased risk for adverse health events as a result of pregnancy (Box 2).
a. Benign
i. Focal nodular hyperplasia 2 Evidence: Limited direct evidence suggests that hormonal contraceptive use does
not inuence either progression or regression of liver lesions among women with
focal nodular hyperplasia (266).
ii. Hepatocellular adenoma 4 —
b. Malignant (hepatoma) 4 —
Respiratory Conditions
Cystic brosis
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
1 Clarication: Persons with cystic brosis are at increased risk for diabetes, liver
disease, gallbladder disease, and VTE (particularly related to use of central venous
catheters) and are frequently prescribed antibiotics. Categories assigned to such
conditions in U.S. MEC should be the same for women with cystic brosis who have
these conditions. For cystic brosis, classications are based on the assumption
that no other conditions are present; these classications must be modied in the
presence of such conditions.
Clarication: Certain drugs to treat cystic brosis (e.g., lumacaftor) might reduce
eectiveness of hormonal contraceptives, including oral, injectable, transdermal,
and implantable contraceptives.
Evidence: Limited evidence suggests that use of COCs or oral contraceptives (type
not specied) among women with cystic brosis is not associated with worsening
of disease severity. Very limited evidence suggests that cystic brosis does not
impair the eectiveness of hormonal contraception (267).
Anemias
Thalassemia 1 Comment: Anecdotal evidence from countries where thalassemia is prevalent
indicates that COC use does not worsen the condition.
Sickle cell disease
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
2 —
Iron deciency anemia 1 Comment: CHC use might decrease menstrual blood loss.
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with increased risk for adverse health events
as a result of pregnancy (Box 2).
See table footnotes on page 69.

Recommendations and Reports
66 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
a. Complicated: graft failure (acute or chronic), rejection, cardiac
allograft vasculopathy
4 Evidence: Limited evidence of COC and patch users indicated no overall changes in
biochemical measures. However, one study reported discontinuations of COC use in
two (8%) of 26 women as a result of serious medical complications, and in one case
report, a woman developed cholestasis associated with high-dose COC use (268).
b. Uncomplicated 2 Clarication: Women with Budd-Chiari syndrome should not use CHCs because of
the increased risk for thrombosis.
Evidence: Limited evidence of COC and patch users indicated no overall changes in
biochemical measures. However, one study reported discontinuations of COC use in
two (8%) of 26 women as a result of serious medical complications, and in one case
report, a woman developed cholestasis associated with high-dose COC use (268).
Drug Interactions
Antiretroviral therapy Comment: These recommendations generally are for ARV agents used alone.
However, most women receiving ARV therapy are using multiple drugs in
combination. In general, whether interactions between ARVs and hormonal
contraceptives dier when ARVs are given alone or in combination is unknown.
a. Nucleoside reverse transcriptase inhibitors (NRTIs)
i. Abacavir (ABC) 1 Evidence: NRTIs do not appear to have signicant risk for interactions with
hormonal contraceptive methods (269–274).
ii. Tenofovir (TDF) 1
iii. Zidovudine (AZT) 1
iv. Lamivudine (3TC) 1
v. Didanosine (DDI) 1
vi. Emtricitabine (FTC) 1
vii. Stavudine (D4T) 1
b. Nonnucleoside reverse transcriptase inhibitors (NNRTIs)
i. Efavirenz (EFV) 2 Clarication: Evidence suggests drug interactions between EFV and certain
hormonal contraceptives. These interactions might reduce the eectiveness of the
hormonal contraceptive.
Evidence: Two studies suggested that pregnancy rates might be higher among
women using COCs and EFV compared with COCs alone, although one study found
no dierence in pregnancy rates (275–277) Two studies found conicting results on
ovulations in women receiving COCs and EFV compared with EFV alone (278,279).
Two pharmacokinetic studies demonstrated decreases in ethinyl estradiol and
progestin concentrations in women receiving COCs and EFV compared with COCs
alone (279,280). Pharmacokinetic studies demonstrated generally no changes in
EFV concentrations with concomitant COC use (279,280).
ii. Etravirine (ETR) 1 Evidence: One study demonstrated no clinically relevant pharmacokinetic or
pharmacodynamic changes in women using COCs and ETR compared with COCs
alone (281).
iii. Nevirapine (NVP) 1 Evidence: Five studies found no signicant dierences in pregnancy rates among
women using COCs and NVP compared with women using COCs alone (275–
277,282,283). Three studies reported no ovulations among women receiving COCs
and NVP (278,283,284). Two pharmacokinetic studies demonstrated decreased
concentrations of ethinyl estradiol and progestin among women using COCs and
NVP compared with COCs alone, and one study found no change in contraceptive
hormone concentrations (278,284,285). Pharmacokinetic studies demonstrated
generally no changes in NVP concentrations with concomitant COC use
(278,285,286).
iv. Rilpivirine (RPV) 1 Evidence: One study demonstrated no clinical signicant pharmacokinetic
changes or adverse events in women using COCs and RPV compared with COCs
alone (287).
c. Ritonavir-boosted protease inhibitors
i. Ritonavir-boosted atazanavir (ATV/r) 2 Clarication: Theoretically, drug interactions might occur between certain
ritonavir-boosted protease inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal contraceptive.
Evidence: One pharmacokinetic study demonstrated decreased estrogen but
increased progestin concentrations in women using COCs and ATV/r compared
with COCs alone (288).
ii. Ritonavir-boosted darunavir (DRV/r) 2 Clarication: Theoretically, drug interactions might occur between certain
ritonavir-boosted protease inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal contraceptive.
Evidence: One pharmacokinetic study demonstrated no change in follicle-stimu-
lating hormone or luteinizing hormone but decreases in ethinyl estradiol and
norethindrone in women using COCs with DRV/r compared with COCs alone (289).
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 67
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
iii. Ritonavir-boosted fosamprenavir (FPV/r) 2 Clarication: Theoretically, drug interactions might occur between certain
ritonavir-boosted protease inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal contraceptive.
Evidence: Information from the package label states that both ethinyl estradiol
and norethindrone concentrations decreased with concurrent administration of
COCs and FPV/r (290).
iv. Ritonavir-boosted lopinavir (LPV/r) 1 Evidence: One study demonstrated a non-signicant increase in pregnancy rates
among women using COCs and LPV/r compared with COCs alone (275). One study
demonstrated no ovulations in women using the combined hormonal patch and
LPV/r compared with combined hormonal patch alone; ethinyl estradiol
concentrations for COC and patch users decreased but norelgestromin concentra-
tions increased with use of the patch (291).
v. Ritonavir-boosted saquinavir (SQV/r) 2 Clarication: Theoretically, drug interactions might occur between certain
ritonavir-boosted protease inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal contraceptive.
Evidence: One pharmacokinetic study demonstrated no change in SQV
concentrations in women using COC and SQV compared with COCs alone (292).
iv. Ritonavir-boosted tipranavir (TPV/r) 2 Clarication: Theoretically, drug interactions might occur between certain
ritonavir-boosted protease inhibitors and certain hormonal contraceptives that
might reduce the eectiveness of the hormonal contraceptive.
Evidence: Information from the package label states that ethinyl estradiol
concentrations decrease but norethindrone concentrations increased with
concurrent administration of COCs and TPV/r (293).
d. Protease inhibitors without ritonavir
i. Atazanavir (ATV) 2 Clarication: Theoretical concern exists that increased levels of ethinyl estradiol
because of interactions with ATV might increase the risk for adverse events.
Evidence: Information from the package label states that there are inconsistent
changes in ethinyl estradiol concentrations and increases in progestin concentra-
tions with concurrent administration of two dierent COCs and ATV (294).
Comment: When ATV is administered with Cobicistat, theoretical concern exists for
a drug interaction with hormonal contraceptives. Cobicistat is an inhibitor of
CYP3A and CYP2D6 and could theoretically increase contraceptive hormone levels.
However, its eects on CYP enzymes and drug levels may vary when combined
with other ARVs.
ii. Fosamprenavir (FPV) 3 Clarication: Concern exists that interactions between FPV and hormonal
contraceptives leading to decreased levels of FPV might diminish eectiveness of
the ARV drug.
Evidence: Information from the package label states that amprenavir concentra-
tions decreased with concurrent administration of COCs and amprenavir.
Norethindrone concentrations increased and ethinyl estradiol concentrations did
not change (290).
iii. Indinavir (IDV) 1 Evidence: One small study found no pregnancies in women using COCs and IDV (277).
iv. Nelnavir (NFV) 2 Clarication: Evidence suggests drug interactions between certain protease
inhibitors and certain hormonal contraceptives. These interactions might reduce
the eectiveness of the hormonal contraceptive.
Evidence: One small study suggested that women using COCs and NFV may have
had higher pregnancy rates than those using COCs alone (277).
e. CCR5 co-receptor antagonists
i. Maraviroc (MVC) 1 Evidence: COC concentrations were not altered by co-administration with MVC (295).
f. HIV integrase strand transfer inhibitors
i. Raltegravir (RAL) 1 Evidence: One pharmacokinetic study demonstrated increased concentrations of
norgestimate and no change in ethinyl estradiol among women using COCs and
RAL compared with COCs alone (296).
ii. Dolutegravir (DTG) 1 Evidence: One study demonstrated no clinically relevant pharmacokinetic or
pharmacodynamic changes in women using COCs and DTG compared with COCs
alone (297).
See table footnotes on page 69.

Recommendations and Reports
68 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
iii. Elvitegravir (EVG) 1 Evidence: Information from the package label states that ethinyl estradiol
concentrations decreased and norgestimate concentrations increased with
concurrent administration of COCs and EVG (298).
Comment: When ATV is administered with Cobicistat, theoretical concern exists for
a drug interaction with hormonal contraceptives. Cobicistat is an inhibitor of
CYP3A and CYP2D6 and could theoretically increase contraceptive hormone levels.
However, its eects on CYP enzymes and drug levels may vary when combined
with other ARVs.
g. Fusion inhibitors
i. Enfuvirtide 1 —
Anticonvulsant therapy
a. Certain anticonvulsants (phenytoin, carbamazepine, barbiturates,
primidone, topiramate, oxcarbazepine)
3 Clarication: Although the interaction of certain anticonvulsants with CHCs is not
harmful to women, it is likely to reduce the eectiveness of CHCs. Use of other
contraceptives should be encouraged for women who are long-term users of any
of these drugs. When a COC is chosen, a preparation containing a minimum of 30
µg ethinyl estradiol should be used.
Evidence: Use of certain anticonvulsants might decrease the eectiveness of COCs
(299–302).
b. Lamotrigine 3 Clarication: The recommendation for lamotrigine applies only for situations
where lamotrigine monotherapy is taken concurrently with COCs. Anticonvulsant
treatment regimens that combine lamotrigine and non–enzyme-inducing
antiepileptic drugs (e.g., sodium valproate) do not interact with COCs.
Evidence: Pharmacokinetic studies show levels of lamotrigine decrease
signicantly during COC use (303–307). Some women who used both COCs and
lamotrigine experienced increased seizure activity in one trial (303).
Antimicrobial therapy
a. Broad-spectrum antibiotics 1 Evidence: Most broad-spectrum antibiotics do not aect the contraceptive
eectiveness of COCs (308–344), patch (345), or ring (346).
b. Antifungals 1 Evidence: Studies of antifungal agents have shown no clinically signicant
pharmacokinetic interactions with COCs (347–356), or ring (357).
c. Antiparasitics 1 Evidence: Studies of antiparasitic agents have shown no clinically signicant
pharmacokinetic interactions with COCs (236,358–362).
d. Rifampin or rifabutin therapy 3 Clarication: Although the interaction of rifampin or rifabutin therapy with CHCs is
not harmful to women, it is likely to reduce the eectiveness of CHCs. Use of other
contraceptives should be encouraged for women who are long-term users of
either of these drugs. When a COC is chosen, a preparation containing a minimum
of 30 µg ethinyl estradiol should be used.
Evidence: The balance of the evidence suggests that rifampin reduces the
eectiveness of COCs (363–378). Data on rifabutin are limited, but eects on
metabolism of COCs are less than with rifampin, and small studies have not shown
evidence of ovulation (365,372).
Psychotropic medications Comment: For many common psychotropic agents, limited or no theoretical
concern exists for clinically signicant drug interactions when co-administered
with hormonal contraceptives. However, either no or very limited data exist
examining potential interactions for these classes of medications. For psychotropic
agents that are CYP1A2 substrates, such as duloxetine, mirtazapine, ziprasidone,
olanzapine, clomipramine, imipramine, and amitriptyline, co-administration with
CHCs could theoretically yield increased concentrations of the psychotropic drug.
For agents with narrow therapeutic windows, such as tricyclic antidepressants,
increased drug concentrations might pose safety concerns that could necessitate
closer monitoring.
a. SSRIs 1 Evidence:
Limited clinical and pharmacokinetic data do not demonstrate concern
for SSRIs decreasing the eectiveness of oral contraceptives. Limited evidence
suggests that for women taking SSRIs, the use of hormonal contraceptives was not
associated with dierences in eectiveness of the SSRI for treatment or in adverse
events when compared with women not taking hormonal contraceptives (379).
Comment: Drugs that are inhibitors of CYP3A4 or CYP2C9 theoretically have the
potential to increase levels of contraceptive steroids which might increase adverse
events. Fluvoxamine is an SSRI known to be a moderate inhibitor of both CYP3A4
and CYP2C9; however, no clinical or pharmacokinetic studies were identied to
explore potential drug-drug interactions.
See table footnotes on page 69.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 69
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE D1. (Continued) Classifications for combined hormonal contraceptives, including pill, patch, and ring
Condition Category CHCs Clarifications/Evidence/Comments
St. John’s wort 2 Evidence: Although clinical data are limited, studies with pharmacokinetic and
pharmacodynamics outcomes raise concern that St. John’s wort might decrease
eectiveness of hormonal contraceptives, including increased risk for break-
through bleeding and ovulation and increased metabolism of estrogen and
progestins. Any interactions might be dependent on the dose of St John’s wort,
and the concentration of active ingredients across types of St. John’s wort
preparations may vary (380).
Abbreviations: ARV=antiretroviral; BMD=bone mineral density; BMI=body mass index; CHC=combined hormonal contraceptive; COC=combined oral contraceptive; DVT=deep venous
thrombosis; hCG=human chorionic gonadotropin; HDL=high-density lipoprotein; HIV=human immunodeficiency virus; IBD=inflammatory bowel disease; LDL=low-density lipoprotein;
PE=pulmonary embolism; PID=pelvic inflammatory disease; SLE = systemic lupus erythematosus; SSRI = selective serotonin reuptake inhibitor; STD=sexually transmitted infection;
VTE=venous thromboembolism.
References
1. Abrams LS, Skee DM, Natarajan J, Wong FA, Lasseter KC. Multiple-
dose pharmacokinetics of a contraceptive patch in healthy women
participants. Contraception 2001;64:287–94. http://dx.doi.
org/10.1016/S0010-7824(01)00273-6
2. Ahrendt HJ, Nisand I, Bastianelli C, et al. Efficacy, acceptability and
tolerability of the combined contraceptive ring, NuvaRing, compared
with an oral contraceptive containing 30 microg of ethinyl estradiol and
3 mg of drospirenone. Contraception 2006;74:451–7. http://dx.doi.
org/10.1016/j.contraception.2006.07.004
3. Audet M-C, Moreau M, Koltun WD, et al; ORTHO EVRA/EVRA
004 Study Group. Evaluation of contraceptive efficacy and cycle control
of a transdermal contraceptive patch vs an oral contraceptive: a
randomized controlled trial. JAMA 2001;285:2347–54. http://dx.doi.
org/10.1001/jama.285.18.2347
4. Bjarnadóttir RI, Tuppurainen M, Killick SR. Comparison of cycle control
with a combined contraceptive vaginal ring and oral levonorgestrel/
ethinyl estradiol. Am J Obstet Gynecol 2002;186:389–95. http://dx.doi.
org/10.1067/mob.2002.121103
5. Boonyarangkul A, Taneepanichskul S. Comparison of cycle control and side
effects between transdermal contraceptive patch and an oral contraceptive
in women older than 35 years. J Med Assoc Thai 2007;90:1715–9.
6. Burkman RT. The transdermal contraceptive patch: a new approach to
hormonal contraception. Int J Fertil Womens Med 2002;47:69–76.
7. Cole JA, Norman H, Doherty M, Walker AM. Venous thromboembolism,
myocardial infarction, and stroke among transdermal contraceptive
system users. Obstet Gynecol 2007;109:339–46. http://dx.doi.
org/10.1097/01.AOG.0000250968.82370.04
8. Devineni D, Skee D, Vaccaro N, et al. Pharmacokinetics and
pharmacodynamics of a transdermal contraceptive patch and an oral
contraceptive. J Clin Pharmacol 2007;47:497–509. http://dx.doi.
org/10.1177/0091270006297919.
9. Dieben TO, Roumen FJ, Apter D. Efficacy, cycle control, and user
acceptability of a novel combined contraceptive vaginal ring. Obstet
Gynecol 2002;100:585–93.
10. Dittrich R, Parker L, Rosen JB, Shangold G, Creasy GW, Fisher AC;
Ortho Evra/Evra 001 Study Group. Transdermal contraception:
evaluation of three transdermal norelgestromin/ethinyl estradiol doses
in a randomized, multicenter, dose-response study. Am J Obstet Gynecol
2002;186:15–20. http://dx.doi.org/10.1067/mob.2002.118844
11. Duijkers I, Killick S, Bigrigg A, Dieben TO. A comparative study on
the effects of a contraceptive vaginal ring NuvaRing and an oral
contraceptive on carbohydrate metabolism and adrenal and thyroid
function. Eur J Contracept Reprod Health Care 2004;9:131–40. http://
dx.doi.org/10.1080/13625180400007199
12. Duijkers IJ, Klipping C, Verhoeven CH, Dieben TO. Ovarian function with
the contraceptive vaginal ring or an oral contraceptive: a randomized study.
Hum Reprod 2004;19:2668–73. http://dx.doi.org/10.1093/humrep/deh493
13. Elkind-Hirsch KE, Darensbourg C, Ogden B, Ogden LF, Hindelang P.
Contraceptive vaginal ring use for women has less adverse metabolic
effects than an oral contraceptive. Contraception 2007;76:348–56.
http://dx.doi.org/10.1016/j.contraception.2007.08.001
14. Hedon B, Helmerhorst FM, Cronje HS, Shangold GA, Fisher AC,
Creasy GW. Comparison of efficacy, cycle control, compliance, and
safety in users of a contraceptive patch versus an oral contraceptive. Int
J Gynaecol Obstet 2000;70(Suppl 2):B78. http://dx.doi.org/10.1016/
S0020-7292(00)85161-9
15. Jick S, Kaye JA, Li L, Jick H. Further results on the risk of nonfatal
venous thromboembolism in users of the contraceptive transdermal
patch compared to users of oral contraceptives containing norgestimate
and 35 microg of ethinyl estradiol. Contraception 2007;76:4–7. http://
dx.doi.org/10.1016/j.contraception.2007.03.003
16. Jick SS, Jick H. Cerebral venous sinus thrombosis in users of four
hormonal contraceptives: levonorgestrel-containing oral contraceptives,
norgestimate-containing oral contraceptives, desogestrel-containing oral
contraceptives and the contraceptive patch. Contraception 2006;74:290–
2. http://dx.doi.org/10.1016/j.contraception.2006.05.071
17. Jick SS, Jick H. The contraceptive patch in relation to ischemic stroke
and acute myocardial infarction. Pharmacotherapy 2007;27:218–20.
http://dx.doi.org/10.1592/phco.27.2.218
18. Jick SS, Kaye JA, Russmann S, Jick H. Risk of nonfatal venous
thromboembolism in women using a contraceptive transdermal patch
and oral contraceptives containing norgestimate and 35 microg of ethinyl
estradiol. Contraception 2006;73:223–8. http://dx.doi.org/10.1016/j.
contraception.2006.01.001
19. Magnusdóttir EM, Bjarnadóttir RI, Onundarson PT, et al. The contraceptive
vaginal ring (NuvaRing) and hemostasis: a comparative study. Contraception
2004;69:461–7. http://dx.doi.org/10.1016/j.contraception.2003.12.010
20. Massai R, Mäkäräinen L, Kuukankorpi A, Klipping C, Duijkers I, Dieben
T. The combined contraceptive vaginal ring and bone mineral density in
healthy pre-menopausal women. Hum Reprod 2005;20:2764–8. http://
dx.doi.org/10.1093/humrep/dei117
21. Milsom I, Lete I, Bjertnaes A, et al. Effects on cycle control and bodyweight
of the combined contraceptive ring, NuvaRing, versus an oral contraceptive
containing 30 µg ethinyl estradiol and 3 mg drospirenone. Hum Reprod
2006;21:2304–11. http://dx.doi.org/10.1093/humrep/del162
22. Oddsson K, Leifels-Fischer B, de Melo NR, et al. Efficacy and safety of
a contraceptive vaginal ring (NuvaRing) compared with a combined oral
contraceptive: a 1-year randomized trial. Contraception 2005;71:176–
82. http://dx.doi.org/10.1016/j.contraception.2004.09.001
23. Pierson RA, Archer DF, Moreau M, Shangold GA, Fisher AC, Creasy GW.
Ortho Evra/Evra versus oral contraceptives: follicular development and
ovulation in normal cycles and after an intentional dosing error. Fertil Steril
2003;80:34–42. http://dx.doi.org/10.1016/S0015-0282(03)00556-9
24. Radowicki S, Skórzewska K, Szlendak K. Safety evaluation of a
transdermal contraceptive system with an oral contraceptive [Polish].
Ginekol Pol 2005;76:884–9.
Recommendations and Reports
70 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
44. Cooper C, Hannaford P, Croft P, Kay CR. Oral contraceptive pill use
and fractures in women: a prospective study. Bone 1993;14:41–5. http://
dx.doi.org/10.1016/8756-3282(93)90254-8
45. Meier C, Brauchli YB, Jick SS, Kraenzlin ME, Meier CR. Use of depot
medroxyprogesterone acetate and fracture risk. J Clin Endocrinol Metab
2010;95:4909–16. http://dx.doi.org/10.1210/jc.2010-0032
46. Cibula D, Skrenkova J, Hill M, Stepan JJ. Low-dose estrogen combined
oral contraceptives may negatively influence physiological bone mineral
density acquisition during adolescence. Eur J Endocrinol 2012;166:1003–
11. http://dx.doi.org/10.1530/EJE-11-1047
47. Gai L, Jia Y, Zhang M, et al. Effect of two kinds of different combined oral
contraceptives use on bone mineral density in adolescent women. Contraception
2012;86:332–6. http://dx.doi.org/10.1016/j.contraception.2012.01.009
48. Scholes D, Hubbard RA, Ichikawa LE, et al. Oral contraceptive use and
bone density change in adolescent and young adult women: a prospective
study of age, hormone dose, and discontinuation. J Clin Endocrinol
Metab 2011;96:E1380–7. http://dx.doi.org/10.1210/jc.2010-3027
49. Lattakova M, Borovsky M, Payer J, Killinger Z. Oral contraception
usage in relation to bone mineral density and bone turnover in adolescent
girls. Eur J Contracept Reprod Health Care 2009;14:207–14. http://
dx.doi.org/10.1080/13625180902838828
50. Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral
density in a cohort of adolescents during use of norethisterone enanthate,
depot-medroxyprogesterone acetate or combined oral contraceptives
and after discontinuation of norethisterone enanthate. Contraception
2009;79:345–9. http://dx.doi.org/10.1016/j.contraception.2008.11.009
51. Pikkarainen E, Lehtonen-Veromaa M, Möttönen T, Kautiainen H, Viikari
J. Estrogen-progestin contraceptive use during adolescence prevents bone
mass acquisition: a 4-year follow-up study. Contraception 2008;78:226–
31. http://dx.doi.org/10.1016/j.contraception.2008.05.002
52. Cromer BA, Bonny AE, Stager M, et al. Bone mineral density in adolescent
females using injectable or oral contraceptives: a 24-month prospective study.
Fertil Steril 2008;90:2060–7. http://dx.doi.org/10.1016/j.fertnstert.2007.10.070
53. Berenson AB, Rahman M, Breitkopf CR, Bi LX. Effects of depot
medroxyprogesterone acetate and 20-µg oral contraceptives on bone
mineral density. Obstet Gynecol 2008;112:788–99. http://dx.doi.
org/10.1097/AOG.0b013e3181875b78
54. Harel Z, Riggs S, Vaz R, Flanagan P, Harel D, Machan JT. Bone accretion
in adolescents using the combined estrogen and progestin transdermal
contraceptive method Ortho Evra: a pilot study. J Pediatr Adolesc
Gynecol 2010;23:23–31. http://dx.doi.org/10.1016/j.jpag.2009.04.008
55. Cobb KL, Bachrach LK, Sowers M, et al. The effect of oral contraceptives
on bone mass and stress fractures in female runners. Med Sci Sports Exerc
2007;39:1464–73. http://dx.doi.org/10.1249/mss.0b013e318074e532
56. Beksinska ME, Kleinschmidt I, Smit JA, Farley TM. Bone mineral density
in adolescents using norethisterone enanthate, depot-medroxyprogesterone
acetate or combined oral contraceptives for contraception. Contraception
2007;75:438–43. http://dx.doi.org/10.1016/j.contraception.2007.02.001
57. Lara-Torre E, Edwards CP, Perlman S, Hertweck SP. Bone mineral density in
adolescent females using depot medroxyprogesterone acetate. J Pediatr Adolesc
Gynecol 2004;17:17–21. http://dx.doi.org/10.1016/j.jpag.2003.11.017
58. Cromer BA, Blair JM, Mahan JD, Zibners L, Naumovski Z. A
prospective comparison of bone density in adolescent girls receiving
depot medroxyprogesterone acetate (Depo-Provera), levonorgestrel
(Norplant), or oral contraceptives. J Pediatr 1996;129:671–6. http://
dx.doi.org/10.1016/S0022-3476(96)70148-8
59. Polatti F, Perotti F, Filippa N, Gallina D, Nappi RE. Bone mass and long-term
monophasic oral contraceptive treatment in young women. Contraception
1995;51:221–4. http://dx.doi.org/10.1016/0010-7824(95)00036-A
60. Sørdal T, Grob P, Verhoeven C. Effects on bone mineral density of a monophasic
combined oral contraceptive containing nomegestrol acetate/17ß-estradiol in
comparison to levonorgestrel/ethinylestradiol. Acta Obstet Gynecol Scand
2012;91:1279–85. http://dx.doi.org/10.1111/j.1600-0412.2012.01498.x
25. Sabatini R, Cagiano R. Comparison profiles of cycle control, side effects
and sexual satisfaction of three hormonal contraceptives. Contraception
2006;74:220–3. http://dx.doi.org/10.1016/j.contraception.2006.03.022
26. Smallwood GH, Meador ML, Lenihan JP, Shangold GA, Fisher AC, Creasy
GW; ORTHO EVRA/EVRA 002 Study Group. Efficacy and safety of a
transdermal contraceptive system. Obstet Gynecol 2001;98:799–805.
27. Timmer CJ, Mulders TM. Pharmacokinetics of etonogestrel and ethinylestradiol
released from a combined contraceptive vaginal ring. Clin Pharmacokinet
2000;39:233–42. http://dx.doi.org/10.2165/00003088-200039030-00005
28. Tuppurainen M, Klimscheffskij R, Venhola M, Dieben TO. The
combined contraceptive vaginal ring (NuvaRing) and lipid metabolism:
a comparative study. Contraception 2004;69:389–94. http://dx.doi.
org/10.1016/j.contraception.2004.01.004
29. Urdl W, Apter D, Alperstein A, et al; ORTHO EVRA/EVRA 003 Study
Group. Contraceptive efficacy, compliance and beyond: factors related
to satisfaction with once-weekly transdermal compared with oral
contraception. Eur J Obstet Gynecol Reprod Biol 2005;121:202–10.
http://dx.doi.org/10.1016/j.ejogrb.2005.01.021
30. van den Heuvel MW, van Bragt AJM, Alnabawy AKM, Kaptein MCJ.
Comparison of ethinylestradiol pharmacokinetics in three hormonal
contraceptive formulations: the vaginal ring, the transdermal patch and
an oral contraceptive. Contraception 2005;72:168–74. http://dx.doi.
org/10.1016/j.contraception.2005.03.005
31. Veres S, Miller L, Burington B. A comparison between the vaginal ring
and oral contraceptives. Obstet Gynecol 2004;104:555–63. http://
dx.doi.org/10.1097/01.AOG.0000136082.59644.13
32. White T, Ozel B, Jain JK, Stanczyk FZ. Effects of transdermal and oral
contraceptives on estrogen-sensitive hepatic proteins. Contraception
2006;74:293–6. http://dx.doi.org/10.1016/j.contraception.2006.04.005
33. Zieman M, Guillebaud J, Weisberg E, Shangold GA, Fisher AC, Creasy GW.
Contraceptive efficacy and cycle control with the Ortho Evra/Evra transdermal
system: the analysis of pooled data. Fertil Steril 2002;77(Suppl 2):S13–8.
http://dx.doi.org/10.1016/S0015-0282(01)03275-7
34. Memon S, Iversen L, Hannaford PC. Is the oral contraceptive pill
associated with fracture in later life? New evidence from the Royal College
of General Practitioners Oral Contraception Study. Contraception
2011;84:40–7. http://dx.doi.org/10.1016/j.contraception.2010.11.019
35. Vestergaard P, Rejnmark L, Mosekilde L. Fracture risk in very young
women using combined oral contraceptives. Contraception 2008;78:358–
64. http://dx.doi.org/10.1016/j.contraception.2008.06.010
36. Vestergaard P, Rejnmark L, Mosekilde L. Oral contraceptive use and risk
of fractures. Contraception 2006;73:571–6. http://dx.doi.org/10.1016/j.
contraception.2006.01.006
37. Barad D, Kooperberg C, Wactawski-Wende J, Liu J, Hendrix SL, Watts
NB. Prior oral contraception and postmenopausal fracture: a Women’s
Health Initiative observational cohort study. Fertil Steril 2005;84:374–
83. http://dx.doi.org/10.1016/j.fertnstert.2005.01.132
38. Michaëlsson K, Baron JA, Farahmand BY, Ljunghall S. Influence of
parity and lactation on hip fracture risk. Am J Epidemiol 2001;153:1166–
72. http://dx.doi.org/10.1093/aje/153.12.1166
39. Michaëlsson K, Baron JA, Farahmand BY, Persson I, Ljunghall S. Oral-
contraceptive use and risk of hip fracture: a case-control study. Lancet
1999;353:1481–4. http://dx.doi.org/10.1016/S0140-6736(98)09044-8
40. La Vecchia C, Tavani A, Gallus S. Oral contraceptives and risk of
hip fractures. Lancet 1999;354:335–6. http://dx.doi.org/10.1016/
S0140-6736(05)75239-9
41. Vessey M, Mant J, Painter R. Oral contraception and other factors in relation
to hospital referral for fracture. Findings in a large cohort study. Contraception
1998;57:231–5. http://dx.doi.org/10.1016/S0010-7824(98)00026-2
42. O’Neill TW, Marsden D, Adams JE, Silman AJ. Risk factors, falls, and
fracture of the distal forearm in Manchester, UK. J Epidemiol Community
Health 1996;50:288–92. http://dx.doi.org/10.1136/jech.50.3.288
43. Mallmin H, Ljunghall S, Persson I, Bergström R. Risk factors for fractures
of the distal forearm: a population-based case-control study. Osteoporos
Int 1994;4:298–304. http://dx.doi.org/10.1007/BF01622186
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 71
US Department of Health and Human Services/Centers for Disease Control and Prevention
61. Gargano V, Massaro M, Morra I, Formisano C, Di Carlo C, Nappi C.
Effects of two low-dose combined oral contraceptives containing
drospirenone on bone turnover and bone mineral density in young fertile
women: a prospective controlled randomized study. Contraception
2008;78:10–5. http://dx.doi.org/10.1016/j.contraception.2008.01.016
62. Nappi C, Di Spiezio Sardo A, Greco E, Tommaselli GA, Giordano E,
Guida M. Effects of an oral contraceptive containing drospirenone on
bone turnover and bone mineral density. Obstet Gynecol 2005;105:53–
60. http://dx.doi.org/10.1097/01.AOG.0000148344.26475.fc
63. Berenson AB, Radecki CM, Grady JJ, Rickert VI, Thomas A. A
prospective, controlled study of the effects of hormonal contraception
on bone mineral density. Obstet Gynecol 2001;98:576–82.
64. Berenson AB, Breitkopf CR, Grady JJ, Rickert VI, Thomas A. Effects
of hormonal contraception on bone mineral density after 24 months of
use. Obstet Gynecol 2004;103:899–906. http://dx.doi.org/10.1097/01.
AOG.0000117082.49490.d5
65. Elgán C, Samsioe G, Dykes AK. Influence of smoking and oral
contraceptives on bone mineral density and bone remodeling in young
women: a 2-year study. Contraception 2003;67:439–47. http://dx.doi.
org/10.1016/S0010-7824(03)00048-9
66. Elgán C, Dykes AK, Samsioe G. Bone mineral density changes in young
women: a two year study. Gynecol Endocrinol 2004;19:169–77. http://
dx.doi.org/10.1080/09513590400012119
67. Endrikat J, Mih E, Düsterberg B, et al. A 3-year double-blind, randomized,
controlled study on the influence of two oral contraceptives containing either
20 µg or 30 µg ethinylestradiol in combination with levonorgestrel on bone
mineral density. Contraception 2004;69:179–87. http://dx.doi.org/10.1016/j.
contraception.2003.10.002
68. Paoletti AM, Orrù M, Lello S, et al. Short-term variations in bone
remodeling markers of an oral contraception formulation containing
3 mg of drospirenone plus 30 microg of ethinyl estradiol: observational
study in young postadolescent women. Contraception 2004;70:293–8.
http://dx.doi.org/10.1016/j.contraception.2004.04.004
69. Nappi C, Di Spiezio Sardo A, Acunzo G, et al. Effects of a low-dose and
ultra-low-dose combined oral contraceptive use on bone turnover and
bone mineral density in young fertile women: a prospective controlled
randomized study. Contraception 2003;67:355–9. http://dx.doi.
org/10.1016/S0010-7824(03)00025-8
70. Reed SD, Scholes D, LaCroix AZ, Ichikawa LE, Barlow WE, Ott SM.
Longitudinal changes in bone density in relation to oral contraceptive
use. Contraception 2003;68:177–82. http://dx.doi.org/10.1016/
S0010-7824(03)00147-1
71. Cobb KL, Kelsey JL, Sidney S, Ettinger B, Lewis CE. Oral contraceptives
and bone mineral density in white and black women in CARDIA.
Coronary Risk Development in Young Adults. Osteoporos Int
2002;13:893–900. http://dx.doi.org/10.1007/s001980200123
72. Burr DB, Yoshikawa T, Teegarden D, et al. Exercise and oral contraceptive
use suppress the normal age-related increase in bone mass and strength
of the femoral neck in women 18–31 years of age. Bone 2000;27:855–63.
http://dx.doi.org/10.1016/S8756-3282(00)00403-8
73. Recker RR, Davies KM, Hinders SM, Heaney RP, Stegman MR, Kimmel
DB. Bone gain in young adult women. JAMA 1992;268:2403–8. http://
dx.doi.org/10.1001/jama.1992.03490170075028
74. Mazess RB, Barden HS. Bone density in premenopausal women: effects
of age, dietary intake, physical activity, smoking, and birth-control pills.
Am J Clin Nutr 1991;53:132–42.
75. Gambacciani M, Cappagli B, Lazzarini V, Ciaponi M, Fruzzetti F,
Genazzani AR. Longitudinal evaluation of perimenopausal bone loss:
effects of different low dose oral contraceptive preparations on bone
mineral density. Maturitas 2006;54:176–80. http://dx.doi.org/10.1016/j.
maturitas.2005.10.007
76. Gambacciani M, Spinetti A, Taponeco F, Cappagli B, Piaggesi L,
Fioretti P. Longitudinal evaluation of perimenopausal vertebral bone
loss: effects of a low-dose oral contraceptive preparation on bone mineral
density and metabolism. Obstet Gynecol 1994;83:392–6.
77. Gambacciani M, Spinetti A, Cappagli B, et al. Hormone replacement
therapy in perimenopausal women with a low dose oral contraceptive
preparation: effects on bone mineral density and metabolism. Maturitas
1994;19:125–31. http://dx.doi.org/10.1016/0378-5122(94)90062-0
78. Gambacciani M, Cappagli B, Ciaponi M, Benussi C, Genazzani AR. Hormone
replacement therapy in perimenopause: effect of a low dose oral contraceptive
preparation on bone quantitative ultrasound characteristics. Menopause
1999;6:43–8. http://dx.doi.org/10.1097/00042192-199906010-00009
79. Volpe A, Malmusi S, Zanni AL, Landi S, Cagnacci A. Oral contraceptives
and bone metabolism. Eur J Contracept Reprod Health Care
1997;2:225–8. http://dx.doi.org/10.3109/13625189709165298
80. Hansen MA, Overgaard K, Riis BJ, Christiansen C. Potential risk factors
for development of postmenopausal osteoporosis—examined over a
12-year period. Osteoporos Int 1991;1:95–102. http://dx.doi.
org/10.1007/BF01880450
81. Shargil AA. Hormone replacement therapy in perimenopausal women
with a triphasic contraceptive compound: a three-year prospective study.
Int J Fertil 1985;30:15, 18–28.
82. Taechakraichana N, Limpaphayom K, Ninlagarn T, Panyakhamlerd K,
Chaikittisilpa S, Dusitsin N. A randomized trial of oral contraceptive
and hormone replacement therapy on bone mineral density and coronary
heart disease risk factors in postmenopausal women. Obstet Gynecol
2000;95:87–94.
83. Taechakraichana N, Jaisamrarn U, Panyakhamlerd K, Chaikittisilpa S,
Limpaphayom K. Difference in bone acquisition among hormonally
treated postmenopausal women with normal and low bone mass. J Med
Assoc Thai 2001;84(Suppl 2):S586–92.
84. Grimes DA, Schulz KF. Surrogate end points in clinical research:
hazardous to your health. Obstet Gynecol 2005;105:1114–8. http://
dx.doi.org/10.1097/01.AOG.0000157445.67309.19
85. Schönau E. The peak bone mass concept: is it still relevant? Pediatr Nephrol
2004;19:825–31. http://dx.doi.org/10.1007/s00467-004-1465-5
86. Cohen A, Shane E. Treatment of premenopausal women with low bone
mineral density. Curr Osteoporos Rep 2008;6:39–46. http://dx.doi.
org/10.1007/s11914-008-0007-7
87. US Department of Health and Human Services. Healthy people 2020:
maternal, infant, and child health objectives. Washington, DC: US
Department of Health and Human Services; 2015. http://www.
healthypeople.gov/2020/topics-objectives/topic/maternal-infant-and-
child-health/objectives.
88. Tepper NK, Phillips SJ, Kapp N, Gaffield ME, Curtis KM. Combined
hormonal contraceptive use among breastfeeding women: an updated
systematic review. Contraception 2015;S0010-7824(15)00218-8.
89. Petersen JF, Bergholt T, Nielsen AK, Paidas MJ, Løkkegaard EC.
Combined hormonal contraception and risk of venous thromboembolism
within the first year following pregnancy. Danish nationwide historical
cohort 1995–2009. Thromb Haemost 2014;112:73–8. http://dx.doi.
org/10.1160/TH13-09-0797
90. Jackson E, Curtis KM, Gaffield ME. Risk of venous thromboembolism
during the postpartum period: a systematic review. Obstet Gynecol
2011;117:691–703. http://dx.doi.org/10.1097/AOG.0b013e31820ce2db
91. Kamel H, Navi BB, Sriram N, Hovsepian DA, Devereux RB, Elkind MS.
Risk of a thrombotic event after the 6-week postpartum period. N Engl J
Med 2014;370:1307–15. http://dx.doi.org/10.1056/NEJMoa1311485
92. Sultan AA, Tata LJ, West J, et al. Risk factors for first venous
thromboembolism around pregnancy: a population-based cohort study
from the United Kingdom. Blood 2013;121:3953–61. http://dx.doi.
org/10.1182/blood-2012-11-469551
93. Sultan AA, West J, Tata LJ, Fleming KM, Nelson-Piercy C, Grainge MJ.
Risk of first venous thromboembolism in and around pregnancy: a
population-based cohort study. Br J Haematol 2012;156:366–73. http://
dx.doi.org/10.1111/j.1365-2141.2011.08956.x
Recommendations and Reports
72 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
94. Tepper NK, Boulet SL, Whiteman MK, et al. Postpartum venous
thromboembolism: incidence and risk factors. Obstet Gynecol
2014;123:987–96. http://dx.doi.org/10.1097/AOG.0000000000000230
95. Jackson E, Glasier A. Return of ovulation and menses in postpartum
nonlactating women: a systematic review. Obstet Gynecol 2011;117:657–
62. http://dx.doi.org/10.1097/AOG.0b013e31820ce18c
96. Lähteenmäki P. Influence of oral contraceptives on immediate
postabortal pituitary-ovarian function. Acta Obstet Gynecol Scand
Suppl 1978;76:1–43.
97. Lähteenmäki P, Rasi V, Luukkainen T, Myllyä G. Coagulation factors
in women using oral contraceptives or intrauterine contraceptive devices
immediately after abortion. Am J Obstet Gynecol 1981;141:175–9.
98. Martin CW, Brown AH, Baird DT. A pilot study of the effect of methotrexate
or combined oral contraceptive on bleeding patterns after induction of
abortion with mifepristone and a prostaglandin pessary. Contraception
1998;58:99–103. http://dx.doi.org/10.1016/S0010-7824(98)00072-9
99. Niswonger JW, London GD, Anderson GV, Wolfe L. Oral
contraceptives during immediate postabortal period. Obstet Gynecol
1968;32:325–7.
100. Peterson WF. Contraceptive therapy following therapeutic abortion:
an analysis. Obstet Gynecol 1974;44:853–7.
101. Tang OS, Gao PP, Cheng L, Lee SW, Ho PC. A randomized double-blind
placebo-controlled study to assess the effect of oral contraceptive pills on
the outcome of medical abortion with mifepristone and misoprostol. Hum
Reprod 1999;14:722–5. http://dx.doi.org/10.1093/humrep/14.3.722
102. Tang OS, Xu J, Cheng L, Lee SW, Ho PC. The effect of contraceptive pills
on the measured blood loss in medical termination of pregnancy by
mifepristone and misoprostol: a randomized placebo controlled trial. Hum
Reprod 2002;17:99–102. http://dx.doi.org/10.1093/humrep/17.1.99
103. Fine PM, Tryggestad J, Meyers NJ, Sangi-Haghpeykar H. Safety and
acceptability with the use of a contraceptive vaginal ring after surgical
or medical abortion. Contraception 2007;75:367–71. http://dx.doi.
org/10.1016/j.contraception.2007.01.009
104. Gillum LA, Mamidipudi SK, Johnston SC. Ischemic stroke risk with
oral contraceptives: a meta-analysis. JAMA 2000;284:72–8. http://
dx.doi.org/10.1001/jama.284.1.72
105. Jick SS, Walker AM, Stergachis A, Jick H. Oral contraceptives and
breast cancer. Br J Cancer 1989;59:618–21. http://dx.doi.org/10.1038/
bjc.1989.125
106. Khader YS, Rice J, John L, Abueita O. Oral contraceptives use and the
risk of myocardial infarction: a meta-analysis. Contraception
2003;68:11–7. http://dx.doi.org/10.1016/S0010-7824(03)00073-8
107. Lawson DH, Davidson JF, Jick H. Oral contraceptive use and venous
thromboembolism: absence of an effect of smoking. BMJ 1977;2:729–
30. http://dx.doi.org/10.1136/bmj.2.6089.729
108. Lidegaard O, Edström B, Kreiner S. Oral contraceptives and venous
thromboembolism. A case-control study. Contraception 1998;57:291–
301. http://dx.doi.org/10.1016/S0010-7824(98)00033-X
109. Nightingale AL, Lawrenson RA, Simpson EL, Williams TJ, MacRae
KD, Farmer RD. The effects of age, body mass index, smoking and
general health on the risk of venous thromboembolism in users of
combined oral contraceptives. Eur J Contracept Reprod Health Care
2000;5:265–74. http://dx.doi.org/10.1080/13625180008500402
110. Petitti DB, Wingerd J, Pellegrin F, Ramcharan S. Risk of vascular disease
in women. Smoking, oral contraceptives, noncontraceptive estrogens,
and other factors. JAMA 1979;242:1150–4. http://dx.doi.org/10.1001/
jama.1979.03300110022020
111. Rosenberg L, Palmer JR, Rao RS, Shapiro S. Low-dose oral contraceptive
use and the risk of myocardial infarction. Arch Intern Med
2001;161:1065–70. http://dx.doi.org/10.1001/archinte.161.8.1065
112. Straneva P, Hinderliter A, Wells E, Lenahan H, Girdler S. Smoking,
oral contraceptives, and cardiovascular reactivity to stress. Obstet
Gynecol 2000;95:78–83.
113. Tanis BC, van den Bosch MA, Kemmeren JM, et al. Oral contraceptives
and the risk of myocardial infarction. N Engl J Med 2001;345:1787–
93. http://dx.doi.org/10.1056/NEJMoa003216
114. Van den Bosch MA, Kemmeren JM, Tanis BC, et al. The RATIO study:
oral contraceptives and the risk of peripheral arterial disease in young
women. J Thromb Hemost 2003;1:439–44.
115. World Health Organization Collaborative Study of Cardiovascular
Disease and Steroid Hormone Contraception. Venous thromboembolic
disease and combined oral contraceptives: results of international
multicentre case-control study. Lancet 1995;346:1575–82. http://
dx.doi.org/10.1016/S0140-6736(95)91926-0
116. Collaborative Group for the Study of Stroke in Young Women. Oral
contraceptives and stroke in young women. Associated risk factors. JAMA
1975;231:718–22. http://dx.doi.org/10.1001/jama.1975.03240190022010
117. Horton LG, Simmons KB, Curtis KM. Combined hormonal
contraceptive use among obese women and risk for cardiovascular events:
a systematic review. Contraception 2016. Epub June 1, 2016. http://
dx.doi.org/10.1016/j.contraception.2016.05.014
118. Brunner Huber LR, Hogue CJ, Stein AD, Drews C, Zieman M. Body
mass index and risk for oral contraceptive failure: a case-cohort study
in South Carolina. Ann Epidemiol 2006;16:637–43. http://dx.doi.
org/10.1016/j.annepidem.2006.01.001
119. Brunner Huber LR, Toth JL. Obesity and oral contraceptive failure:
findings from the 2002 National Survey of Family Growth. Am J
Epidemiol 2007;166:1306–11. http://dx.doi.org/10.1093/aje/kwm221
120. Brunner LR, Hogue CJ. The role of body weight in oral contraceptive failure:
results from the 1995 national survey of family growth. Ann Epidemiol
2005;15:492–9. http://dx.doi.org/10.1016/j.annepidem.2004.10.009
121. Holt VL, Cushing-Haugen KL, Daling JR. Body weight and risk of
oral contraceptive failure. Obstet Gynecol 2002;99:820–7.
122. Holt VL, Scholes D, Wicklund KG, Cushing-Haugen KL, Daling JR. Body
mass index, weight, and oral contraceptive failure risk. Obstet Gynecol
2005;105:46–52. http://dx.doi.org/10.1097/01.AOG.0000149155.11912.52
123. Trussell J, Schwarz EB, Guthrie K. Obesity and oral contraceptive pill
failure. Contraception 2009;79:334–8. http://dx.doi.org/10.1016/j.
contraception.2008.11.017
124. Vessey M. Oral contraceptive failures and body weight: findings in a
large cohort study. J Fam Plann Reprod Health Care 2001;27:90–1.
http://dx.doi.org/10.1783/147118901101195092
125. Yamazaki M, Dwyer K, Sobhan M, et al. Effect of obesity on the
effectiveness of hormonal contraceptives: an individual participant data
meta-analysis. Contraception 2015;92:445–52. http://dx.doi.
org/10.1016/j.contraception.2015.07.016
126. Zieman M, Guillebaud J, Weisberg E, Shangold GA, Fisher AC, Creasy
GW. Contraceptive efficacy and cycle control with the Ortho Evra/Evra
transdermal system: the analysis of pooled data. Fertil Steril 2002;77(Suppl
2):S13–8. http://dx.doi.org/10.1016/S0015-0282(01)03275-7
127. O’Connell KJ, Osborne LM, Westhoff C. Measured and reported
weight change for women using a vaginal contraceptive ring vs. a low-
dose oral contraceptive. Contraception 2005;72:323–7. http://dx.doi.
org/10.1016/j.contraception.2005.05.008
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 73
US Department of Health and Human Services/Centers for Disease Control and Prevention
128. Paulen ME, Zapata LB, Cansino C, Curtis KM, Jamieson DJ.
Contraceptive use among women with a history of bariatric surgery: a
systematic review. Contraception 2010;82:86–94. http://dx.doi.
org/10.1016/j.contraception.2010.02.008
129. Lidegaard Ø, Edström B, Kreiner S. Oral contraceptives and venous
thromboembolism: a five-year national case-control study. Contraception
2002;65:187–96. http://dx.doi.org/10.1016/S0010-7824(01)00307-9
130. Croft P, Hannaford PC. Risk factors for acute myocardial infarction
in women: evidence from the Royal College of General Practitioners’
oral contraception study. BMJ 1989;298:165–8. http://dx.doi.
org/10.1136/bmj.298.6667.165
131. D’Avanzo B, La Vecchia C, Negri E, Parazzini F, Franceschi S. Oral
contraceptive use and risk of myocardial infarction: an Italian case-
control study. J Epidemiol Community Health 1994;48:324–5. http://
dx.doi.org/10.1136/jech.48.3.324
132. Dunn NR, Faragher B, Thorogood M, et al. Risk of myocardial
infarction in young female smokers. Heart 1999;82:581–3. http://
dx.doi.org/10.1136/hrt.82.5.581
133. Hannaford PC, Croft PR, Kay CR. Oral contraception and stroke.
Evidence from the Royal College of General Practitioners’ Oral
Contraception Study. Stroke 1994;25:935–42. http://dx.doi.
org/10.1161/01.STR.25.5.935
134. Heinemann LA, Lewis MA, Spitzer WO, Thorogood M, Guggenmoos-
Holzmann I, Bruppacher R; Transnational Research Group on Oral
Contraceptives and the Health of Young Women. Thromboembolic
stroke in young women. A European case-control study on oral
contraceptives. Contraception 1998;57:29–37. http://dx.doi.
org/10.1016/S0010-7824(97)00204-7
135. Kemmeren JM, Tanis BC, van den Bosch MA, et al. Risk of Arterial
Thrombosis in Relation to Oral Contraceptives (RATIO) study: oral
contraceptives and the risk of ischemic stroke. Stroke 2002;33:1202–8.
http://dx.doi.org/10.1161/01.STR.0000015345.61324.3F
136. Lewis MA, Heinemann LA, Spitzer WO, MacRae KD, Bruppacher R.
The use of oral contraceptives and the occurrence of acute myocardial
infarction in young women. Results from the Transnational Study on
Oral Contraceptives and the Health of Young Women. Contraception
1997;56:129–40. http://dx.doi.org/10.1016/S0010-7824(97)00118-2
137. Lidegaard O. Oral contraception and risk of a cerebral thromboembolic
attack: results of a case-control study. BMJ 1993;306:956–63. http://
dx.doi.org/10.1136/bmj.306.6883.956
138. Lidegaard O. Oral contraceptives, pregnancy and the risk of cerebral
thromboembolism: the influence of diabetes, hypertension, migraine
and previous thrombotic disease. Br J Obstet Gynaecol 1995;102:153–
9. http://dx.doi.org/10.1111/j.1471-0528.1995.tb09070.x
139. Lubianca JN, Faccin CS, Fuchs FD. Oral contraceptives: a risk factor for
uncontrolled blood pressure among hypertensive women. Contraception
2003;67:19–24. http://dx.doi.org/10.1016/S0010-7824(02)00429-8
140. Narkiewicz K, Graniero GR, D’Este D, Mattarei M, Zonzin P, Palatini P.
Ambulatory blood pressure in mild hypertensive women taking oral
contraceptives. A case-control study. Am J Hypertens 1995;8:249–53.
http://dx.doi.org/10.1016/0895-7061(95)96212-3
141. Siritho S, Thrift AG, McNeil JJ, You RX, Davis SM, Donnan GA;
Melbourne Risk Factor Study (MERFS) Group. Risk of ischemic stroke
among users of the oral contraceptive pill: The Melbourne Risk Factor
Study (MERFS) Group. Stroke 2003;34:1575–80. http://dx.doi.
org/10.1161/01.STR.0000077925.16041.6B
142. WHO Collaborative Study of Cardiovascular Disease and Steroid
Hormone Contraception. Ischaemic stroke and combined oral
contraceptives: results of an international, multicentre, case-control
study. Lancet 1996;348:498–505. http://dx.doi.org/10.1016/
S0140-6736(95)12393-8
143. WHO Collaborative Study of Cardiovascular Disease and Steroid
Hormone Contraception. Acute myocardial infarction and combined
oral contraceptives: results of an international multicentre case-control
study. Lancet 1997;349:1202–9. http://dx.doi.org/10.1016/
S0140-6736(97)02358-1
144. Lubianca JN, Moreira LB, Gus M, Fuchs FD. Stopping oral
contraceptives: an effective blood pressure-lowering intervention in
women with hypertension. J Hum Hypertens 2005;19:451–5. http://
dx.doi.org/10.1038/sj.jhh.1001841
145. Aberg H, Karlsson L, Melander S. Studies on toxaemia of pregnancy with
special reference to blood pressure. II. Results after 6–11 years’ follow-up. Ups
J Med Sci 1978;83:97–102. http://dx.doi.org/10.3109/03009737809179119
146. Carmichael SM, Taylor MM, Ayers CR. Oral contraceptives,
hypertension, and toxemia. Obstet Gynecol 1970;35:371–6.
147. Meinel H, Ihle R, Laschinski M. [Effect of hormonal contraceptives
on blood pressure following pregnancy-induced hypertension].
Zentralbl Gynakol 1987;109:527–31.
148. Pritchard JA, Pritchard SA. Blood pressure response to estrogen-progestin oral
contraceptive after pregnancy-induced hypertension. Am J Obstet Gynecol
1977;129:733–9 http://dx.doi.org/10.1016/0002-9378(77)90390-8.
149. Sibai BM, Taslimi MM, el-Nazer A, Amon E, Mabie BC, Ryan GM.
Maternal-perinatal outcome associated with the syndrome of hemolysis,
elevated liver enzymes, and low platelets in severe preeclampsia-
eclampsia. Am J Obstet Gynecol 1986;155:501–7. http://dx.doi.
org/10.1016/0002-9378(86)90266-8
150. Sibai BM, Ramadan MK, Chari RS, Friedman SA. Pregnancies
complicated by HELLP syndrome (hemolysis, elevated liver enzymes,
and low platelets): subsequent pregnancy outcome and long-term
prognosis. Am J Obstet Gynecol 1995;172:125–9. http://dx.doi.
org/10.1016/0002-9378(95)90099-3
151. WHO Collaborative Study of Cardiovascular Disease and Steroid
Hormone Contraception. Haemorrhagic stroke, overall stroke risk,
and combined oral contraceptives: results of an international,
multicentre, case-control study. Lancet 1996;348:505–10. http://
dx.doi.org/10.1016/S0140-6736(95)12394-6
152. Sidney S, Petitti DB, Soff GA, Cundiff DL, Tolan KK, Quesenberry
CP Jr. Venous thromboembolic disease in users of low-estrogen
combined estrogen-progestin oral contraceptives. Contraception
2004;70:3–10. http://dx.doi.org/10.1016/j.contraception.2004.02.010
153. Andersen BS, Olsen J, Nielsen GL, et al. Third generation oral
contraceptives and heritable thrombophilia as risk factors of non-fatal
venous thromboembolism. Thromb Haemost 1998;79:28–31.
154. Aznar J, Mira Y, Vayá A, et al. Factor V Leiden and prothrombin
G20210A mutations in young adults with cryptogenic ischemic stroke.
Thromb Haemost 2004;91:1031–4.
155. Bennet L, Odeberg H. Resistance to activated protein C, highly
prevalent amongst users of oral contraceptives with venous
thromboembolism. J Intern Med 1998;243:27–32. http://dx.doi.
org/10.1046/j.1365-2796.1998.00310.x
156. Bloemenkamp KW, Rosendaal FR, Helmerhorst FM, Vandenbroucke
JP. Higher risk of venous thrombosis during early use of oral contraceptives
in women with inherited clotting defects.[comment]. Arch Intern Med
2000;160:49–52. http://dx.doi.org/10.1001/archinte.160.1.49
Recommendations and Reports
74 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
157. Bloemenkamp KW, Helmerhorst FM, Rosendaal FR, Vandenbroucke
JP, Büller HR. Enhancement by factor V Leiden mutation of risk of
deep-vein thrombosis associated with oral contraceptives containing a
third-generation progestagen. Lancet 1995;346:1593–6. http://dx.doi.
org/10.1016/S0140-6736(95)91929-5
158. de Bruijn SF, Stam J, Koopman MM, Vandenbroucke JP; The Cerebral
Venous Sinus Thrombosis Study Group. Case-control study of risk of
cerebral sinus thrombosis in oral contraceptive users and in [correction
of who are] carriers of hereditary prothrombotic conditions. BMJ
1998;316:589–92. http://dx.doi.org/10.1136/bmj.316.7131.589
159. Emmerich J, Rosendaal FR, Cattaneo M, et al; Study Group for Pooled-
Analysis in Venous Thromboembolism. Combined effect of factor V
Leiden and prothrombin 20210A on the risk of venous
thromboembolism—pooled analysis of 8 case-control studies including
2310 cases and 3204 controls. Thromb Haemost 2001;86:809–16.
160. Gadelha T, André C, Jucá AA, Nucci M. Prothrombin 20210A and
oral contraceptive use as risk factors for cerebral venous thrombosis.
Cerebrovasc Dis 2005;19:49–52. http://dx.doi.org/10.1159/000081911
161. Legnani C, Palareti G, Guazzaloca G, et al. Venous thromboembolism
in young women; role of thrombophilic mutations and oral
contraceptive use. Eur Heart J 2002;23:984–90. http://dx.doi.
org/10.1053/euhj.2001.3082
162. Martinelli I, Battaglioli T, Bucciarelli P, Passamonti SM, Mannucci
PM. Risk factors and recurrence rate of primary deep vein thrombosis
of the upper extremities. Circulation 2004;110:566–70. http://dx.doi.
org/10.1161/01.CIR.0000137123.55051.9B
163. Martinelli I, Sacchi E, Landi G, Taioli E, Duca F, Mannucci PM. High
risk of cerebral-vein thrombosis in carriers of a prothrombin-gene
mutation and in users of oral contraceptives.[comment]. N Engl J Med
1998;338:1793–7. http://dx.doi.org/10.1056/NEJM199806183382502
164. Martinelli I, Taioli E, Bucciarelli P, Akhavan S, Mannucci PM.
Interaction between the G20210A mutation of the prothrombin gene
and oral contraceptive use in deep vein thrombosis. Arterioscler Thromb
Vasc Biol 1999;19:700–3. http://dx.doi.org/10.1161/01.ATV.19.3.700
165. Middeldorp S, Meinardi JR, Koopman MM, et al. A prospective
study of asymptomatic carriers of the factor V Leiden mutation
to determine the incidence of venous thromboembolism.
[comment]. Ann Intern Med 2001;135:322–7. http://dx.doi.
org/10.7326/0003-4819-135-5-200109040-00008
166. Pabinger I, Schneider B; The GTH Study Group on Natural Inhibitors.
Thrombotic risk of women with hereditary antithrombin III-, protein C- and
protein S-deficiency taking oral contraceptive medication. Thromb Haemost
1994;71:548–52.
167. Pezzini A, Grassi M, Iacoviello L, et al. Inherited thrombophilia and stratification
of ischaemic stroke risk among users of oral contraceptives. J Neurol Neurosurg
Psychiatry 2007;78:271–6. http://dx.doi.org/10.1136/jnnp.2006.101675
168. Santamaría A, Mateo J, Oliver A, et al. Risk of thrombosis associated
with oral contraceptives of women from 97 families with inherited
thrombophilia: high risk of thrombosis in carriers of the G20210A
mutation of the prothrombin gene. Haematologica 2001;86:965–71.
169. Slooter AJ, Rosendaal FR, Tanis BC, Kemmeren JM, van der Graaf Y,
Algra A. Prothrombotic conditions, oral contraceptives, and the risk
of ischemic stroke. J Thromb Haemost 2005;3:1213–7. http://dx.doi.
org/10.1111/j.1538-7836.2005.01442.x
170. Spannagl M, Heinemann LA, Schramm W. Are factor V Leiden carriers
who use oral contraceptives at extreme risk for venous thromboembolism?
Eur J Contracept Reprod Health Care 2000;5:105–12. http://dx.doi.
org/10.1080/13625180008500383
171. van Boven HH, Vandenbroucke JP, Briët E, Rosendaal FR. Gene-gene
and gene-environment interactions determine risk of thrombosis in families
with inherited antithrombin deficiency. Blood 1999;94:2590–4.
172. van Vlijmen EF, Brouwer JL, Veeger NJ, Eskes TK, de Graeff PA, van
der Meer J. Oral contraceptives and the absolute risk of venous
thromboembolism in women with single or multiple thrombophilic
defects: results from a retrospective family cohort study. Arch Intern
Med 2007;167:282–9. http://dx.doi.org/10.1001/archinte.167.3.282
173. Vandenbroucke JP, Koster T, Rosendaal FR, Briët E, Reitsma PH, Bertina RM.
Increased risk of venous thrombosis in oral-contraceptive users who are carriers
of factor V Leiden mutation.[comment]. Lancet 1994;344:1453–7. http://
dx.doi.org/10.1016/S0140-6736(94)90286-0
174. Vayá A, Mira Y, Mateo J, et al. Prothrombin G20210A mutation and
oral contraceptive use increase upper-extremity deep vein thrombotic
risk. Thromb Haemost 2003;89:452–7.
175. Martinelli I, Battaglioli T, Burgo I, Di Domenico S, Mannucci PM.
Oral contraceptive use, thrombophilia and their interaction in young
women with ischemic stroke. Haematologica 2006;91:844–7.
176. Tepper NK, Marchbanks PA, Curtis KM. Superficial venous disease
and combined hormonal contraceptives: a systematic review.
Contraception 2015;S0010-7824(15)00128-6.
177. Tepper NK, Paulen ME, Marchbanks PA, Curtis KM. Safety of
contraceptive use among women with peripartum cardiomyopathy: a
systematic review. Contraception 2010;82:95–101. http://dx.doi.
org/10.1016/j.contraception.2010.02.004
178. The Criteria Committee of the New York Heart Association.
Nomenclature and criteria for diagnosis of diseases of the heart and
great vessels. 9th ed. Boston, MA: Little, Brown and Co; 1994.
179. Bernatsky S, Clarke A, Ramsey-Goldman R, et al. Hormonal exposures
and breast cancer in a sample of women with systemic lupus
erythematosus. Rheumatology (Oxford) 2004;43:1178–81. http://
dx.doi.org/10.1093/rheumatology/keh282
180. Bernatsky S, Ramsey-Goldman R, Gordon C, et al. Factors associated
with abnormal Pap results in systemic lupus erythematosus.
Rheumatology (Oxford) 2004;43:1386–9. http://dx.doi.org/10.1093/
rheumatology/keh331
181. Chopra N, Koren S, Greer WL, et al. Factor V Leiden, prothrombin
gene mutation, and thrombosis risk in patients with antiphospholipid
antibodies. J Rheumatol 2002;29:1683–8.
182. Esdaile JM, Abrahamowicz M, Grodzicky T, et al. Traditional Framingham
risk factors fail to fully account for accelerated atherosclerosis in systemic
lupus erythematosus. Arthritis Rheum 2001;44:2331–7. http://dx.doi.
org/10.1002/1529-0131(200110)44:10<2331::AID-ART395≥3.0.CO;2-I
183. Julkunen HA. Oral contraceptives in systemic lupus erythematosus:
side-effects and influence on the activity of SLE. Scand J Rheumatol
1991;20:427–33. http://dx.doi.org/10.3109/03009749109096822
184. Julkunen HA, Kaaja R, Friman C. Contraceptive practice in women
with systemic lupus erythematosus. Br J Rheumatol 1993;32:227–30.
http://dx.doi.org/10.1093/rheumatology/32.3.227
185. Jungers P, Dougados M, Pélissier C, et al. Influence of oral contraceptive
therapy on the activity of systemic lupus erythematosus. Arthritis
Rheum 1982;25:618–23. http://dx.doi.org/10.1002/art.1780250603
186. Manzi S, Meilahn EN, Rairie JE, et al. Age-specific incidence rates of
myocardial infarction and angina in women with systemic lupus
erythematosus: comparison with the Framingham Study. Am J Epidemiol
1997;145:408–15. http://dx.doi.org/10.1093/oxfordjournals.aje.a009122
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 75
US Department of Health and Human Services/Centers for Disease Control and Prevention
187. McAlindon T, Giannotta L, Taub N, D’Cruz D, Hughes G.
Environmental factors predicting nephritis in systemic lupus
erythematosus. Ann Rheum Dis 1993;52:720–4. http://dx.doi.
org/10.1136/ard.52.10.720
188. McDonald J, Stewart J, Urowitz MB, Gladman DD. Peripheral vascular
disease in patients with systemic lupus erythematosus. Ann Rheum
Dis 1992;51:56–60. http://dx.doi.org/10.1136/ard.51.1.56
189. Mintz G, Gutiérrez G, Delezé M, Rodríguez E. Contraception with
progestagens in systemic lupus erythematosus. Contraception
1984;30:29–38. http://dx.doi.org/10.1016/0010-7824(84)90076-3
190. Petri M. Musculoskeletal complications of systemic lupus erythematosus
in the Hopkins Lupus Cohort: an update. Arthritis Care Res
1995;8:137–45. http://dx.doi.org/10.1002/art.1790080305
191. Petri M. Lupus in Baltimore: evidence-based ‘clinical pearls’ from the
Hopkins Lupus Cohort. Lupus 2005;14:970–3. http://dx.doi.
org/10.1191/0961203305lu2230xx
192. Petri M, Kim MY, Kalunian KC, et al; OC-SELENA Trial. Combined
oral contraceptives in women with systemic lupus erythematosus. N Engl
J Med 2005;353:2550–8. http://dx.doi.org/10.1056/NEJMoa051135
193. Sánchez-Guerrero J, Uribe AG, Jiménez-Santana L, et al. A trial of
contraceptive methods in women with systemic lupus erythematosus. N
Engl J Med 2005;353:2539–49. http://dx.doi.org/10.1056/NEJMoa050817
194. Sarabi ZS, Chang E, Bobba R, et al. Incidence rates of arterial and venous
thrombosis after diagnosis of systemic lupus erythematosus. Arthritis
Rheum 2005;53:609–12. http://dx.doi.org/10.1002/art.21314
195. Schaedel ZE, Dolan G, Powell MC. The use of the levonorgestrel-
releasing intrauterine system in the management of menorrhagia in
women with hemostatic disorders. Am J Obstet Gynecol
2005;193:1361–3. http://dx.doi.org/10.1016/j.ajog.2005.05.002
196. Somers E, Magder LS, Petri M. Antiphospholipid antibodies and
incidence of venous thrombosis in a cohort of patients with systemic
lupus erythematosus. J Rheumatol 2002;29:2531–6.
197. Urowitz MB, Bookman AA, Koehler BE, Gordon DA, Smythe HA, Ogryzlo
MA. The bimodal mortality pattern of systemic lupus erythematosus. Am J
Med 1976;60:221–5. http://dx.doi.org/10.1016/0002-9343(76)90431-9
198. Choojitarom K, Verasertniyom O, Totemchokchyakarn K, Nantiruj
K, Sumethkul V, Janwityanujit S. Lupus nephritis and Raynaud’s
phenomenon are significant risk factors for vascular thrombosis in SLE
patients with positive antiphospholipid antibodies. Clin Rheumatol
2008;27:345–51. http://dx.doi.org/10.1007/s10067-007-0721-z
199. Wahl DG, Guillemin F, de Maistre E, Perret C, Lecompte T, Thibaut
G. Risk for venous thrombosis related to antiphospholipid antibodies
in systemic lupus erythematosus—a meta-analysis. Lupus 1997;6:467–
73. http://dx.doi.org/10.1177/096120339700600510
200. Farr SL, Folger SG, Paulen ME, Curtis KM. Safety of contraceptive methods
for women with rheumatoid arthritis: a systematic review. Contraception
2010;82:64–71. http://dx.doi.org/10.1016/j.contraception.2010.02.003
201. Tepper NK, Whiteman MK, Zapata LB, Marchbanks PA, Curtis KM. Safety
of hormonal contraceptives among women with migraine: a systematic review.
Contraception 2016. Epub May 3, 2016. http:// dx.doi.org/10.1016/j.
contraception.2016.04.016
202. Xu Z, Li Y, Tang S, Huang X, Chen T. Current use of oral contraceptives
and the risk of first-ever ischemic stroke: A meta-analysis of
observational studies. Thromb Res 2015;136:52–60. http://dx.doi.
org/10.1016/j.thromres.2015.04.021
203. Etminan M, Takkouche B, Isorna FC, Samii A. Risk of ischaemic stroke
in people with migraine: systematic review and meta-analysis of
observational studies. BMJ 2005;330:63. http://dx.doi.org/10.1136/
bmj.38302.504063.8F
204. Schürks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T.
Migraine and cardiovascular disease: systematic review and meta-
analysis. BMJ 2009;339:b3914. http://dx.doi.org/10.1136/bmj.b3914
205. Spector JT, Kahn SR, Jones MR, Jayakumar M, Dalal D, Nazarian S.
Migraine headache and ischemic stroke risk: an updated meta-analysis. Am
J Med 2010;123:612–24. http://dx.doi.org/10.1016/j.amjmed.2009.12.021
206. Zapata LB, Oduyebo T, Whiteman MK, Marchbanks PA, Curtis KM.
Contraceptive use among women with multiple sclerosis: a systematic
review. Contraception. In press 2016.
207. Pagano HP, Zapata LB, Berry-Bibee EN, Nanda K, Curtis KM. Safety of
hormonal contraception and intrauterine devices among women with
depressive and bipolar disorders: a systematic review. Contraception 2016.
Epub June 27, 2016. http://dx.doi.org/10.1016/j.contraception.2016.06.012
208. Iyer V, Farquhar C, Jepson R. Oral contraceptive pills for heavy
menstrual bleeding. Cochrane Database Syst Rev 2000;(2):CD000154.
209. Davis L, Kennedy SS, Moore J, Prentice A. Oral contraceptives for
pain associated with endometriosis. Cochrane Database Syst Rev
2007;(3):CD001019.
210. Hendrix SL, Alexander NJ. Primary dysmenorrhea treatment with a
desogestrel-containing low-dose oral contraceptive. Contraception
2002;66:393–9. http://dx.doi.org/10.1016/S0010-7824(02)00414-6
211. Proctor ML, Roberts H, Farquhar CM. Combined oral contraceptive
pill (OCP) as treatment for primary dysmenorrhoea. Cochrane
Database Syst Rev 2001;(4):CD002120.
212. Gaffield ME, Kapp N, Curtis KM. Combined oral contraceptive and
intrauterine device use among women with gestational trophoblastic
disease. Contraception 2009;80:363–71. http://dx.doi.org/10.1016/j.
contraception.2009.03.022
213. Smith JS, Green J, Berrington de Gonzalez A, et al. Cervical cancer and
use of hormonal contraceptives: a systematic review. Lancet 2003;361:1159–
67. http://dx.doi.org/10.1016/S0140-6736(03)12949-2
214. Black MM, Barclay THC, Polednak A, Kwon CS, Leis HP Jr,
Pilnik S. Family history, oral contraceptive usage, and breast cancer.
Cancer 1983;51:2147–51. http://dx.doi.org/10.1002/1097-
0142(19830601)51:11<2147::AID-CNCR2820511133≥3.0.CO;2-X
215. Brinton LA, Hoover R, Szklo M, Fraumeni JF Jr. Oral contraceptives
and breast cancer. Int J Epidemiol 1982;11:316–22. http://dx.doi.
org/10.1093/ije/11.4.316
216. Brohet RM, Goldgar DE, Easton DF, et al. Oral contraceptives and
breast cancer risk in the international BRCA1/2 carrier cohort study:
a report from EMBRACE, GENEPSO, GEO-HEBON, and the
IBCCS Collaborating Group. J Clin Oncol 2007;25:3831–6. http://
dx.doi.org/10.1200/JCO.2007.11.1179
217. Claus EB, Stowe M, Carter D. Oral contraceptives and the risk of
ductal breast carcinoma in situ. Breast Cancer Res Treat 2003;81:129–
36. http://dx.doi.org/10.1023/A:1025728524310
218. Collaborative Group on Hormonal Factors in Breast Cancer. Familial
breast cancer: collaborative reanalysis of individual data from 52
epidemiological studies including 58,209 women with breast cancer
and 101,986 women without the disease. Lancet 2001;358:1389–99.
http://dx.doi.org/10.1016/S0140-6736(01)06524-2
219. Grabrick DM, Hartmann LC, Cerhan JR, et al. Risk of breast cancer with oral
contraceptive use in women with a family history of breast cancer.[comment].
JAMA 2000;284:1791–8. http://dx.doi.org/10.1001/jama.284.14.1791
220. Gronwald J, Byrski T, Huzarski T, et al. Influence of selected lifestyle
factors on breast and ovarian cancer risk in BRCA1 mutation carriers
from Poland. Breast Cancer Res Treat 2006;95:105–9. http://dx.doi.
org/10.1007/s10549-005-9051-5
Recommendations and Reports
76 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
221. Haile RW, Thomas DC, McGuire V, et al; kConFab Investigators;
Ontario Cancer Genetics Network Investigators. BRCA1 and BRCA2
mutation carriers, oral contraceptive use, and breast cancer before
age 50. Cancer Epidemiol Biomarkers Prev 2006;15:1863–70. http://
dx.doi.org/10.1158/1055-9965.EPI-06-0258
222. Harris NV, Weiss NS, Francis AM, Polissar L. Breast cancer in relation to
patterns of oral contraceptive use. Am J Epidemiol 1982;116:643–51.
223. Hennekens CH, Speizer FE, Lipnick RJ, et al. A case-control study of
oral contraceptive use and breast cancer. J Natl Cancer Inst
1984;72:39–42.
224. Jernström H, Loman N, Johannsson OT, Borg A, Olsson H. Impact of
teenage oral contraceptive use in a population-based series of early-onset
breast cancer cases who have undergone BRCA mutation testing. Eur J
Cancer 2005;41:2312–20. http://dx.doi.org/10.1016/j.ejca.2005.03.035
225. Marchbanks PA, McDonald JA, Wilson HG, et al. Oral contraceptives
and the risk of breast cancer. N Engl J Med 2002;346:2025–32. http://
dx.doi.org/10.1056/NEJMoa013202
226. Milne RL, Knight JA, John EM, et al. Oral contraceptive use and risk
of early-onset breast cancer in carriers and noncarriers of BRCA1 and
BRCA2 mutations. Cancer Epidemiol Biomarkers Prev 2005;14:350–6.
http://dx.doi.org/10.1158/1055-9965.EPI-04-0376
227. Narod SA, Dubé MP, Klijn J, et al. Oral contraceptives and the risk of
breast cancer in BRCA1 and BRCA2 mutation carriers. J Natl Cancer
Inst 2002;94:1773–9. http://dx.doi.org/10.1093/jnci/94.23.1773
228. Rosenberg L, Palmer JR, Rao RS, et al. Case-control study of oral
contraceptive use and risk of breast cancer. Am J Epidemiol 1996;143:25–
37. http://dx.doi.org/10.1093/oxfordjournals.aje.a008654
229. Silvera SA, Miller AB, Rohan TE. Oral contraceptive use and risk of
breast cancer among women with a family history of breast cancer: a
prospective cohort study. Cancer Causes Control 2005;16:1059–63.
http://dx.doi.org/10.1007/s10552-005-0343-1
230. Ursin G, Henderson BE, Haile RW, et al. Does oral contraceptive use
increase the risk of breast cancer in women with BRCA1/BRCA2
mutations more than in other women? Cancer Res 1997;57:3678–81.
231. Ursin G, Ross RK, Sullivan-Halley J, Hanisch R, Henderson B,
Bernstein L. Use of oral contraceptives and risk of breast cancer in
young women. Breast Cancer Res Treat 1998;50:175–84. http://dx.doi.
org/10.1023/A:1006037823178
232. Polis CB, Phillips SJ, Curtis KM, et al. Hormonal contraceptive
methods and risk of HIV acquisition in women: a systematic review
of epidemiological evidence. Contraception 2014;90:360–90. http://
dx.doi.org/10.1016/j.contraception.2014.07.009
233. Polis CB, Phillips SJ, Curtis KM. Hormonal contraceptive use and
female-to-male HIV transmission: a systematic review of the
epidemiologic evidence. AIDS 2013;27:493–505. http://dx.doi.
org/10.1097/QAD.0b013e32835ad539
234. Phillips SJ, Polis CB, Curtis KM. The safety of hormonal contraceptives
for women living with HIV and their sexual partners. Contraception
2016;93:11–6 http://dx.doi.org/10.1016/j.contraception.2015.10.002.
235. Phillips SJ, Curtis KM, Polis CB. Effect of hormonal contraceptive
methods on HIV disease progression: a systematic review. AIDS
2013;27:787–94. http://dx.doi.org/10.1097/QAD.0b013e32835bb672
236. el-Raghy I, Back DJ, Osman F, Orme ML, Fathalla M. Contraceptive
steroid concentrations in women with early active schistosomiasis: lack
of effect of antischistosomal drugs. Contraception 1986;33:373–7.
http://dx.doi.org/10.1016/0010-7824(86)90099-5
237. Gad-el-Mawla N, Abdallah A. Liver function in bilharzial females
receiving contraceptive pills. Acta Hepatosplenol 1969;16:308–10.
238. Gad-el-Mawla N, el-Roubi O, Sabet S, Abdallah A. Plasma lipids and
lipoproteins in bilharzial females during oral contraceptive therapy. J Egypt
Med Assoc 1972;55:137–47.
239. Shaaban MM, Hammad WA, Falthalla MF, et al. Effects of oral
contraception on liver function tests and serum proteins in women
with active schistosomiasis. Contraception 1982;26:75–82. http://
dx.doi.org/10.1016/0010-7824(82)90174-3
240. Shaaban MM, Ghaneimah SA, Mohamed MA, Abdel-Chani S, Mostafa
SA. Effect of oral contraception on serum bile acid. Int J Gynaecol Obstet
1984;22:111–5. http://dx.doi.org/10.1016/0020-7292(84)90023-7
241. Sy FS, Osteria TS, Opiniano V, Gler S. Effect of oral contraceptive on liver
function tests of women with schistosomiasis in the Philippines. Contraception
1986;34:283–94. http://dx.doi.org/10.1016/0010-7824(86)90009-0
242. Tagy AH, Saker ME, Moussa AA, Kolgah A. The effect of low-dose
combined oral contraceptive pills versus injectable contraceptive (Depot
Provera) on liver function tests of women with compensated bilharzial
liver fibrosis. Contraception 2001;64:173–6. http://dx.doi.org/10.1016/
S0010-7824(01)00248-7
243. Beck P, Wells SA. Comparison of the mechanisms underlying
carbohydrate intolerance in subclinical diabetic women during
pregnancy and during post-partum oral contraceptive steroid treatment.
J Clin Endocrinol Metab 1969;29:807–18. http://dx.doi.org/10.1210/
jcem-29-6-807
244. Kjos SL, Peters RK, Xiang A, Thomas D, Schaefer U, Buchanan TA.
Contraception and the risk of type 2 diabetes mellitus in Latina women
with prior gestational diabetes mellitus. JAMA 1998;280:533–8. http://
dx.doi.org/10.1001/jama.280.6.533
245. Kung AW, Ma JT, Wong VC, et al. Glucose and lipid metabolism with triphasic
oral contraceptives in women with history of gestational diabetes. Contraception
1987;35:257–69. http://dx.doi.org/10.1016/0010-7824(87)90027-8
246. Rådberg T, Gustafson A, Skryten A, Karlsson K. Metabolic studies in
gestational diabetic women during contraceptive treatment: effects on
glucose tolerance and fatty acid composition of serum lipids. Gynecol
Obstet Invest 1982;13:17–29. http://dx.doi.org/10.1159/000299480
247. Skouby SO, Andersen O, Kühl C. Oral contraceptives and insulin
receptor binding in normal women and those with previous gestational
diabetes. Am J Obstet Gynecol 1986;155:802–7. http://dx.doi.
org/10.1016/S0002-9378(86)80024-2
248. Skouby SO, Andersen O, Saurbrey N, Kühl C. Oral contraception and
insulin sensitivity: in vivo assessment in normal women and women
with previous gestational diabetes. J Clin Endocrinol Metab
1987;64:519–23. http://dx.doi.org/10.1210/jcem-64-3-519
249. Skouby SO, Mølsted-Pedersen L, Kühl C. Low dosage oral
contraception in women with previous gestational diabetes. Obstet
Gynecol 1982;59:325–8.
250. Xiang AH, Kawakubo M, Kjos SL, Buchanan TA. Long-acting injectable
progestin contraception and risk of type 2 diabetes in Latino women
with prior gestational diabetes mellitus. Diabetes Care 2006;29:613–7.
http://dx.doi.org/10.2337/diacare.29.03.06.dc05-1940
251. Kjos SL, Shoupe D, Douyan S, et al. Effect of low-dose oral contraceptives on
carbohydrate and lipid metabolism in women with recent gestational diabetes:
results of a controlled, randomized, prospective study. Am J Obstet Gynecol
1990;163:1822–7. http://dx.doi.org/10.1016/0002-9378(90)90757-X
252. Rådberg T, Gustafson A, Skryten A, Karlsson K. Metabolic studies in
women with previous gestational diabetes during contraceptive
treatment: effects on serum lipids and high density lipoproteins. Acta
Endocrinol (Copenh) 1982;101:134–9.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 77
US Department of Health and Human Services/Centers for Disease Control and Prevention
253. Skouby SO, Kühl C, Mølsted-Pedersen L, Petersen K, Christensen MS.
Triphasic oral contraception: metabolic effects in normal women and those
with previous gestational diabetes. Am J Obstet Gynecol 1985;153:495–
500. http://dx.doi.org/10.1016/0002-9378(85)90460-0
254. Beck P, Arnett DM, Alsever RN, Eaton RP. Effect of contraceptive steroids on
arginine- stimulated glucagon and insulin secretion in women. II. Carbohydrate
and lipid physiology in insulin-dependent diabetics. Metabolism 1976;25:23–
31 http://dx.doi.org/10.1016/0026-0495(76)90156-6.
255. Diab KM, Zaki MM. Contraception in diabetic women: comparative
metabolic study of Norplant, depot medroxyprogesterone acetate, low dose
oral contraceptive pill and CuT380A. J Obstet Gynaecol Res 2000;26:17–
26. http://dx.doi.org/10.1111/j.1447-0756.2000.tb01195.x
256. Garg SK, Chase HP, Marshall G, Hoops SL, Holmes DL, Jackson WE.
Oral contraceptives and renal and retinal complications in young women
with insulin-dependent diabetes mellitus. JAMA 1994;271:1099–102.
http://dx.doi.org/10.1001/jama.1994.03510380055037
257. Grigoryan OR, Grodnitskaya EE, Andreeva EN, Shestakova MV,
Melnichenko GA, Dedov II. Contraception in perimenopausal women
with diabetes mellitus. Gynecol Endocrinol 2006;22:198–206. http://
dx.doi.org/10.1080/09513590600624317
258. Margolis KL, Adami H-O, Luo J, Ye W, Weiderpass E. A prospective study of
oral contraceptive use and risk of myocardial infarction among Swedish women.
Fertil Steril 2007;88:310–6. http://dx.doi.org/10.1016/j.fertnstert.2006.11.206
259. Petersen KR, Skouby SO, Jespersen J. Balance of coagulation activity
with fibrinolysis during use of oral contraceptives in women with
insulin-dependent diabetes mellitus. Int J Fertil Menopausal Stud
1995;40(Suppl 2):105–11.
260. Petersen KR, Skouby SO, Sidelmann J, Jespersen J. Assessment of
endothelial function during oral contraception in women with insulin-
dependent diabetes mellitus. Metabolism 1994;43:1379–83. http://
dx.doi.org/10.1016/0026-0495(94)90031-0
261. Rådberg T, Gustafson A, Skryten A, Karlsson K. Oral contraception in
diabetic women. A cross-over study on serum and high density lipoprotein
(HDL) lipids and diabetes control during progestogen and combined
estrogen/progestogen contraception. Horm Metab Res 1982;14:61–5.
262. Skouby SO, Jensen BM, Kühl C, Mølsted-Pedersen L, Svenstrup B,
Nielsen J. Hormonal contraception in diabetic women: acceptability
and influence on diabetes control and ovarian function of a nonalkylated
estrogen/progestogen compound. Contraception 1985;32:23–31.
http://dx.doi.org/10.1016/0010-7824(85)90113-1
263. Skouby SO, Mølsted-Pedersen L, Kühl C, Bennet P. Oral contraceptives
in diabetic women: metabolic effects of four compounds with different
estrogen/progestogen profiles. Fertil Steril 1986;46:858–64 http://
dx.doi.org/10.1016/S0015-0282(16)49825-0.
264. Zapata LB, Paulen ME, Cansino C, Marchbanks PA, Curtis KM.
Contraceptive use among women with inflammatory bowel disease: A
systematic review. Contraception 2010;82:72–85. http://dx.doi.
org/10.1016/j.contraception.2010.02.012
265. Kapp N, Tilley IB, Curtis KM. The effects of hormonal contraceptive
use among women with viral hepatitis or cirrhosis of the liver: a
systematic review. Contraception 2009;80:381–6. http://dx.doi.
org/10.1016/j.contraception.2009.04.007
266. Kapp N, Curtis KM. Hormonal contraceptive use among women with
liver tumors: a systematic review. Contraception 2009;80:387–90.
http://dx.doi.org/10.1016/j.contraception.2009.01.021
267. Whiteman MK, Oduyebo T, Zapata LB, Walker S, Curtis KM.
Contraceptive safety among women with cystic fibrosis: a systematic review.
Contraception 2016. Epub June 7, 2016. http://dx.doi.org/10.1016/j.
contraception.2016.05.016
268. Paulen ME, Folger SG, Curtis KM, Jamieson DJ. Contraceptive use among
solid organ transplant patients: a systematic review. Contraception
2010;82:102–12. http://dx.doi.org/10.1016/j.contraception.2010.02.007
269. Aweeka FT, Rosenkranz SL, Segal Y, et al; NIAID AIDS Clinical Trials
Group. The impact of sex and contraceptive therapy on the plasma
and intracellular pharmacokinetics of zidovudine. AIDS 2006;20:1833–
41. http://dx.doi.org/10.1097/01.aids.0000244202.18629.36
270. Kearney BP, Mathias A. Lack of effect of tenofovir disoproxil fumarate
on pharmacokinetics of hormonal contraceptives. Pharmacotherapy
2009;29:924–9. http://dx.doi.org/10.1592/phco.29.8.924
271. Todd CS, Deese J, Wang M, et al; FEM-PrEP Study Group. Sino-implant
(II)® continuation and effect of concomitant tenofovir disoproxil
fumarate-emtricitabine use on plasma levonorgestrel concentrations
among women in Bondo, Kenya. Contraception 2015;91:248–52.
http://dx.doi.org/10.1016/j.contraception.2014.10.008
272. Murnane PM, Heffron R, Ronald A, et al; Partners PrEP Study Team.
Pre-exposure prophylaxis for HIV-1 prevention does not diminish the
pregnancy prevention effectiveness of hormonal contraception. AIDS
2014;28:1825–30. http://dx.doi.org/10.1097/QAD.0000000000000290
273. Kasonde M, Niska RW, Rose C, et al. Bone mineral density changes
among HIV-uninfected young adults in a randomised trial of pre-
exposure prophylaxis with tenofovir-emtricitabine or placebo in
Botswana. PLoS One 2014;9:e90111. http://dx.doi.org/10.1371/
journal.pone.0090111
274. Callahan R, Nanda K, Kapiga S, et al; FEM-PrEP Study Group.
Pregnancy and contraceptive use among women participating in the
FEM-PrEP trial. J Acquir Immune Defic Syndr 2015;68:196–203.
http://dx.doi.org/10.1097/QAI.0000000000000413
275. Patel RC, Onono M, Gandhi M, et al. Pregnancy rates in HIV-positive
women using contraceptives and efavirenz-based or nevirapine-based
antiretroviral therapy in Kenya: a retrospective cohort study. Lancet HIV
2015;2:e474–82. http://dx.doi.org/10.1016/S2352-3018(15)00184-8
276. Pyra M, Heffron R, Mugo NR, et al; Partners in Prevention HSV/HIV
Transmission Study and Partners PrEP Study Teams. Effectiveness of hormonal
contraception in HIV-infected women using antiretroviral therapy. AIDS
2015;29:2353–9. http://dx.doi.org/10.1097/QAD.0000000000000827
277. Clark RA, Theall K. Population-based study evaluating association
between selected antiretroviral therapies and potential oral contraceptive
failure. J Acquir Immune Defic Syndr 2004;37:1219–20. http://dx.doi.
org/10.1097/01.qai.0000136724.15758.ae
278. Landolt NK, Phanuphak N, Ubolyam S, et al. Efavirenz, in contrast
to nevirapine, is associated with unfavorable progesterone and
antiretroviral levels when coadministered with combined oral
contraceptives. J Acquir Immune Defic Syndr 2013;62:534–9. http://
dx.doi.org/10.1097/QAI.0b013e31827e8f98
279. Sevinsky H, Eley T, Persson A, et al. The effect of efavirenz on the
pharmacokinetics of an oral contraceptive containing ethinyl estradiol
and norgestimate in healthy HIV-negative women. Antivir Ther
2011;16:149–56. http://dx.doi.org/10.3851/IMP1725
280. Landolt NK, Phanuphak N, Ubolyam S, et al. Significant decrease of
ethinylestradiol with nevirapine, and of etonogestrel with efavirenz in
HIV-positive women. J Acquir Immune Defic Syndr 2014;66:e50–2.
281. Schöller-Gyüre M, Kakuda TN, Woodfall B, et al. Effect of steady-state
etravirine on the pharmacokinetics and pharmacodynamics of
ethinylestradiol and norethindrone. Contraception 2009;80:44–52.
http://dx.doi.org/10.1016/j.contraception.2009.01.009
Recommendations and Reports
78 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
282. Myer L, Carter RJ, Katyal M, Toro P, El-Sadr WM, Abrams EJ. Impact
of antiretroviral therapy on incidence of pregnancy among HIV-infected
women in Sub-Saharan Africa: a cohort study. PLoS Med 2010;7:e1000229.
http://dx.doi.org/10.1371/journal.pmed.1000229
283. Nanda K, Delany-Moretlwe S, Dubé K, et al. Nevirapine-based
antiretroviral therapy does not reduce oral contraceptive effectiveness.
AIDS 2013;27(Suppl 1):S17–25. http://dx.doi.org/10.1097/
QAD.0000000000000050
284. Stuart GS, Moses A, Corbett A, et al. Combined oral contraceptives and
antiretroviral PK/PD in Malawian women: pharmacokinetics and
pharmacodynamics of a combined oral contraceptive and a generic
combined formulation antiretroviral in Malawi. J Acquir Immune Defic
Syndr 2011;58:e40–3. http://dx.doi.org/10.1097/QAI.0b013e31822b8bf8
285. Mildvan D, Yarrish R, Marshak A, et al. Pharmacokinetic interaction between
nevirapine and ethinyl estradiol/norethindrone when administered concurrently
to HIV-infected women. J Acquir Immune Defic Syndr 2002;29:471–7.
http://dx.doi.org/10.1097/00042560-200204150-00007
286. Muro E, Droste JA, Hofstede HT, Bosch M, Dolmans W, Burger DM.
Nevirapine plasma concentrations are still detectable after more than 2 weeks
in the majority of women receiving single-dose nevirapine: implications for
intervention studies. J Acquir Immune Defic Syndr 2005;39:419–2. http://
dx.doi.org/10.1097/01.qai.0000167154.37357.f9
287. Crauwels HM, van Heeswijk RP, Buelens A, Stevens M, Hoetelmans RM.
Lack of an effect of rilpivirine on the pharmacokinetics of ethinylestradiol
and norethindrone in healthy volunteers. Int J Clin Pharmacol Ther
2014;52:118–28. http://dx.doi.org/10.5414/CP201943
288. Zhang J, Chung E, Yones C, et al. The effect of atazanavir/ritonavir
on the pharmacokinetics of an oral contraceptive containing ethinyl
estradiol and norgestimate in healthy women. Antivir Ther
2011;16:157–64. http://dx.doi.org/10.3851/IMP1724
289. Sekar VJ, Lefebvre E, Guzman SS, et al. Pharmacokinetic interaction
between ethinyl estradiol, norethindrone and darunavir with low-dose
ritonavir in healthy women. Antivir Ther 2008;13:563–9.
290. Glaxo Smith Kline. Lexiva (fosamprenavir calcium) [Package insert].
Research Triangle Park, NC: Glaxo Smith Kline; 2015.
291. Vogler MA, Patterson K, Kamemoto L, et al. Contraceptive efficacy of
oral and transdermal hormones when co-administered with protease
inhibitors in HIV-1-infected women: pharmacokinetic results of ACTG
trial A5188. J Acquir Immune Defic Syndr 2010;55:473–82. http://
dx.doi.org/10.1097/QAI.0b013e3181eb5ff5
292. Fröhlich M, Burhenne J, Martin-Facklam M, et al. Oral
contraception does not alter single dose saquinavir pharmacokinetics
in women. Br J Clin Pharmacol 2004;57:244–52 http://dx.doi.
org/10.1111/j.1365-2125.2003.01983.x.
293. Boehringer Ingelheim Pharmaceuticals. Aptivus (tipranavir) [Package
insert]. Ridgefield, CT; 2005.
294. Bristol-Myers Squibb. Reyataz (atazanavir sulfate) [Package insert].
Princeton, NJ; 2003.
295. Abel S, Russell D, Whitlock LA, Ridgway CE, Muirhead GJ. Effect of
maraviroc on the pharmacokinetics of midazolam, lamivudine/
zidovudine, and ethinyloestradiol/levonorgestrel in healthy volunteers.
Br J Clin Pharmacol 2008;65(Suppl 1):19–26. http://dx.doi.
org/10.1111/j.1365-2125.2008.03132.x
296. Anderson MS, Hanley WD, Moreau AR, et al. Effect of raltegravir on
estradiol and norgestimate plasma pharmacokinetics following oral
contraceptive administration in healthy women. Br J Clin Pharmacol
2011;71:616–20. http://dx.doi.org/10.1111/j.1365-2125.2010.03885.x
297. Song IH, Borland J, Chen S, Wajima T, Peppercorn AF, Piscitelli SC.
Dolutegravir has no effect on the pharmacokinetics of oral contraceptives
with norgestimate and ethinyl estradiol. Ann Pharmacother 2015;49:784–
9. http://dx.doi.org/10.1177/1060028015580637
298. Gilead Sciences. Vitekta (elvitegravir) [Package insert]. Foster City, CA; 2012.
299. Back DJ, Bates M, Bowden A, et al. The interaction of phenobarbital and
other anticonvulsants with oral contraceptive steroid therapy. Contraception
1980;22:495–503. http://dx.doi.org/10.1016/0010-7824(80)90102-X
300. Doose DR, Wang SS, Padmanabhan M, Schwabe S, Jacobs D, Bialer
M. Effect of topiramate or carbamazepine on the pharmacokinetics of
an oral contraceptive containing norethindrone and ethinyl estradiol
in healthy obese and nonobese female subjects. Epilepsia 2003;44:540–
9. http://dx.doi.org/10.1046/j.1528-1157.2003.55602.x
301. Fattore C, Cipolla G, Gatti G, et al. Induction of ethinylestradiol and
levonorgestrel metabolism by oxcarbazepine in healthy women. Epilepsia
1999;40:783–7. http://dx.doi.org/10.1111/j.1528-1157.1999.tb00779.x
302. Rosenfeld WE, Doose DR, Walker SA, Nayak RK. Effect of topiramate
on the pharmacokinetics of an oral contraceptive containing norethindrone
and ethinyl estradiol in patients with epilepsy. Epilepsia 1997;38:317–23.
http://dx.doi.org/10.1111/j.1528-1157.1997.tb01123.x
303. Christensen J, Petrenaite V, Atterman J, et al. Oral contraceptives
induce lamotrigine metabolism: evidence from a double-blind,
placebo-controlled trial. Epilepsia 2007;48:484–9. http://dx.doi.
org/10.1111/j.1528-1167.2007.00997.x
304. Contin M, Albani F, Ambrosetto G, et al. Variation in lamotrigine
plasma concentrations with hormonal contraceptive monthly cycles in
patients with epilepsy. Epilepsia 2006;47:1573–5. http://dx.doi.
org/10.1111/j.1528-1167.2006.00558.x
305. Reimers A, Helde G, Brodtkorb E. Ethinyl estradiol, not progestogens,
reduces lamotrigine serum concentrations. Epilepsia 2005;46:1414–7.
http://dx.doi.org/10.1111/j.1528-1167.2005.10105.x
306. Sabers A, Buchholt JM, Uldall P, Hansen EL. Lamotrigine plasma levels
reduced by oral contraceptives. Epilepsy Res 2001;47:151–4. http://
dx.doi.org/10.1016/S0920-1211(01)00305-9
307. Sabers A, Ohman I, Christensen J, Tomson T. Oral contraceptives
reduce lamotrigine plasma levels. Neurology 2003;61:570–1. http://
dx.doi.org/10.1212/01.WNL.0000076485.09353.7A
308. Back DJ, Breckenridge AM, MacIver M, et al. The effects of ampicillin
on oral contraceptive steroids in women. Br J Clin Pharmacol
1982;14:43–8. http://dx.doi.org/10.1111/j.1365-2125.1982.tb04932.x
309. Back DJ, Grimmer SF, Orme ML, Proudlove C, Mann RD,
Breckenridge AM. Evaluation of Committee on Safety of Medicines
yellow card reports on oral contraceptive-drug interactions with
anticonvulsants and antibiotics. Br J Clin Pharmacol 1988;25:527–32.
http://dx.doi.org/10.1111/j.1365-2125.1988.tb03341.x
310. Back DJ, Tjia J, Martin C, et al. The lack of interaction between
temafloxacin and combined oral contraceptive steroids. Contraception
1991;43:317–23. http://dx.doi.org/10.1016/0010-7824(91)90070-V
311. Bacon JF, Shenfield GM. Pregnancy attributable to interaction between
tetracycline and oral contraceptives. BMJ 1980;280:293. http://dx.doi.
org/10.1136/bmj.280.6210.293
312. Bainton R. Interaction between antibiotic therapy and contraceptive
medication. Oral Surg Oral Med Oral Pathol 1986;61:453–5. http://
dx.doi.org/10.1016/0030-4220(86)90385-3
313. Bollen M. Use of antibiotics when taking the oral contraceptive pill.
[comment]. Aust Fam Physician 1995;24:928–9.
314. Bromham DR, Cartmill RS. Knowledge and use of secondary
contraception among patients requesting termination of pregnancy.
BMJ 1993;306:556–7. http://dx.doi.org/10.1136/bmj.306.6877.556
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 79
US Department of Health and Human Services/Centers for Disease Control and Prevention
315. Côté J. Interaction of griseofulvin and oral contraceptives.[comment].
J Am Acad Dermatol 1990;22:124–5. http://dx.doi.org/10.1016/
S0190-9622(08)80010-2
316. Csemiczky G, Alvendal C, Landgren BM. Risk for ovulation in women
taking a low-dose oral contraceptive (Microgynon) when receiving
antibacterial treatment with a fluoroquinolone (ofloxacin). Adv
Contracept 1996;12:101–9. http://dx.doi.org/10.1007/BF01849631
317. de Groot AC, Eshuis H, Stricker BH. Inefficacy of oral contraception
during use of minocycline [Dutch]. Ned Tijdschr Geneeskd
1990;134:1227–9.
318. DeSano EA Jr, Hurley SC. Possible interactions of antihistamines and
antibiotics with oral contraceptive effectiveness. Fertil Steril
1982;37:853–4 http://dx.doi.org/10.1016/S0015-0282(16)46350-8.
319. Donley TG, Smith RF, Roy B. Reduced oral contraceptive effectiveness
with concurrent antibiotic use: a protocol for prescribing antibiotics
to women of childbearing age. Compendium 1990;11:392–6.
320. Friedman CI, Huneke AL, Kim MH, Powell J. The effect of ampicillin
on oral contraceptive effectiveness. Obstet Gynecol 1980;55:33–7.
321. Grimmer SF, Allen WL, Back DJ, Breckenridge AM, Orme M, Tjia J. The
effect of cotrimoxazole on oral contraceptive steroids in women. Contraception
1983;28:53–9. http://dx.doi.org/10.1016/S0010-7824(83)80005-5
322. Helms SE, Bredle DL, Zajic J, Jatjoura D, Brodell RT, Krishnarao I.
Oral contraceptive failure rates and oral antibiotics. J Am Acad Dermatol
1997;36:705–10. http://dx.doi.org/10.1016/S0190-9622(97)80322-2
323. Hempel E, Böhm W, Carol W, Klinger G. [Enzyme induction by drugs
and hormonal contraception]. Zentralbl Gynakol 1973;95:1451–7.
324. Hempel E, Zorn C, Graf K. [Effect of chemotherapy agents and
antibiotics on hormonal contraception]. Z Arztl Fortbild (Jena)
1978;72:924–6.
325. Hetényi G. Possible interactions between antibiotics and oral
contraceptives. Ther Hung 1989;37:86–9.
326. Hughes BR, Cunliffe WJ. Interactions between the oral contraceptive
pill and antibiotics.[comment]. Br J Dermatol 1990;122:717–8. http://
dx.doi.org/10.1111/j.1365-2133.1990.tb07299.x
327. Joshi JV, Joshi UM, Sankholi GM, et al. A study of interaction
of low-dose combination oral contraceptive with Ampicillin and
Metronidazole. Contraception 1980;22:643–52. http://dx.doi.
org/10.1016/0010-7824(80)90089-X
328. Kakouris H, Kovacs GT. Pill failure and nonuse of secondary
precautions. Br J Fam Plann 1992;18:41–4.
329. Kakouris H, Kovacs GT. How common are predisposing factors to pill
failure among pill users? Br J Fam Plann 1994;20:33–5.
330. Kovacs GT, Riddoch G, Duncombe P, et al. Inadvertent pregnancies
in oral contraceptive users. Med J Aust 1989;150:549–51.
331. Lequeux A. [Pregnancy under oral contraceptives after treatment with
tetracycline]. Louv Med 1980;99:413–4.
332. London BM, Lookingbill DP. Frequency of pregnancy in acne patients taking
oral antibiotics and oral contraceptives. Arch Dermatol 1994;130:392–3.
http://dx.doi.org/10.1001/archderm.1994.01690030128027
333. Maggiolo F, Puricelli G, Dottorini M, Caprioli S, Bianchi W, Suter F.
The effect of ciprofloxacin on oral contraceptive steroid treatments.
Drugs Exp Clin Res 1991;17:451–4.
334. Murphy AA, Zacur HA, Charache P, Burkman RT. The effect of
tetracycline on levels of oral contraceptives. Am J Obstet Gynecol
1991;164:28–33. http://dx.doi.org/10.1016/0002-9378(91)90617-Z
335. Neely JL, Abate M, Swinker M, D’Angio R. The effect of doxycycline
on serum levels of ethinyl estradiol, norethindrone, and endogenous
progesterone. Obstet Gynecol 1991;77:416–20.
336. Pillans PI, Sparrow MJ. Pregnancy associated with a combined oral
contraceptive and itraconazole.[comment]. N Z Med J 1993;106:436.
337. Scholten PC, Droppert RM, Zwinkels MG, Moesker HL, Nauta JJ,
Hoepelman IM. No interaction between ciprofloxacin and an oral
contraceptive. Antimicrob Agents Chemother 1998;42:3266–8.
338. Silber TJ. Apparent oral contraceptive failure associated with antibiotic
administration. J Adolesc Health Care 1983;4:287–9. http://dx.doi.
org/10.1016/S0197-0070(83)80014-X
339. Sparrow MJ. Pill method failures. N Z Med J 1987;100:102–5.
340. Sparrow MJ. Pregnancies in reliable pill takers. N Z Med J
1989;102:575–7.
341. Sparrow MJ. Pill method failures in women seeking abortion: fourteen
years experience. N Z Med J 1998;111:386–8.
342. van Dijke CP, Weber JC. Interaction between oral contraceptives and
griseofulvin. Br Med J (Clin Res Ed) 1984;288:1125–6. http://dx.doi.
org/10.1136/bmj.288.6424.1125-a
343. Wermeling DP, Chandler MH, Sides GD, Collins D, Muse KN.
Dirithromycin increases ethinyl estradiol clearance without allowing
ovulation. Obstet Gynecol 1995;86:78–84. http://dx.doi.
org/10.1016/0029-7844(95)00075-3
344. Young LK, Farquhar CM, McCowan LM, Roberts HE, Taylor J. The
contraceptive practices of women seeking termination of pregnancy in
an Auckland clinic. N Z Med J 1994;107:189–92.
345. Abrams LS, Skee D, Natarajan J, Wong FA. Pharmacokinetic overview
of Ortho Evra/Evra. Fertil Steril 2002;77(Suppl 2):S3–12. http://
dx.doi.org/10.1016/S0015-0282(01)03261-7
346. Dogterom P, van den Heuvel MW, Thomsen T. Absence of
pharmacokinetic interactions of the combined contraceptive vaginal
ring NuvaRing with oral amoxicillin or doxycycline in two randomised
trials. Clin Pharmacokinet 2005;44:429–38. http://dx.doi.
org/10.2165/00003088-200544040-00007
347. Devenport MH, Crook D, Wynn V, Lees LJ. Metabolic effects of low-
dose fluconazole in healthy female users and non-users of oral
contraceptives. Br J Clin Pharmacol 1989;27:851–9. http://dx.doi.
org/10.1111/j.1365-2125.1989.tb03449.x
348. Hilbert J, Messig M, Kuye O, Friedman H. Evaluation of interaction
between fluconazole and an oral contraceptive in healthy women.
Obstet Gynecol 2001;98:218–23.
349. Kovács I, Somos P, Hámori M. Examination of the potential interaction
between ketoconazole (Nizoral) and oral contraceptives with special
regard to products of low hormone content (Rigevidon, anteovin).
Ther Hung 1986;34:167–70.
350. Lunell NO, Pschera H, Zador G, Carlström K. Evaluation of the
possible interaction of the antifungal triazole SCH 39304 with oral
contraceptives in normal healthy women. Gynecol Obstet Invest
1991;32:91–7. http://dx.doi.org/10.1159/000293003
351. McDaniel PA, Caldroney RD. Oral contraceptives and griseofulvin
interactions. Drug Intell Clin Pharm 1986;20:384.
352. Meyboom RH, van Puijenbroek EP, Vinks MH, Lastdrager CJ.
Disturbance of withdrawal bleeding during concomitant use of
itraconazole and oral contraceptives. N Z Med J 1997;110:300.
353. Rieth H, Sauerbrey N. [Interaction studies with fluconazole, a new
triazole antifungal drug]. Wien Med Wochenschr 1989;139:370–4.
354. Sinofsky FE, Pasquale SA. The effect of fluconazole on circulating
ethinyl estradiol levels in women taking oral contraceptives. Am J
Obstet Gynecol 1998;178:300–4. http://dx.doi.org/10.1016/
S0002-9378(98)80016-1
Recommendations and Reports
80 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
355. van Puijenbroek EP, Feenstra J, Meyboom RH. [Pill cycle disturbance
in simultaneous use of itraconazole and oral contraceptives]. Ned
Tijdschr Geneeskd 1998;142:146–9.
356. Van Puijenbroek EP, Egberts AC, Meyboom RH, Leufkens HG.
Signalling possible drug-drug interactions in a spontaneous reporting
system: delay of withdrawal bleeding during concomitant use of oral
contraceptives and itraconazole. Br J Clin Pharmacol 1999;47:689–93.
http://dx.doi.org/10.1046/j.1365-2125.1999.00957.x
357. Verhoeven CH, van den Heuvel MW, Mulders TM, Dieben TO. The
contraceptive vaginal ring, NuvaRing, and antimycotic co-medication.
Contraception 2004;69:129–32. http://dx.doi.org/10.1016/j.
contraception.2003.10.001
358. Back DJ, Breckenridge AM, Grimmer SF, Orme ML, Purba HS.
Pharmacokinetics of oral contraceptive steroids following the administration
of the antimalarial drugs primaquine and chloroquine. Contraception
1984;30:289–95. http://dx.doi.org/10.1016/0010-7824(84)90092-1
359. Croft AM, Herxheimer A. Adverse effects of the antimalaria drug, mefloquine:
due to primary liver damage with secondary thyroid involvement? BMC Public
Health 2002;2:6. http://dx.doi.org/10.1186/1471-2458-2-6
360. Karbwang J, Looareesuwan S, Back DJ, Migasana S, Bunnag D,
Breckenridge AM. Effect of oral contraceptive steroids on the clinical
course of malaria infection and on the pharmacokinetics of mefloquine
in Thai women. Bull World Health Organ 1988;66:763–7.
361. McGready R, Stepniewska K, Seaton E, et al. Pregnancy and use of
oral contraceptives reduces the biotransformation of proguanil to
cycloguanil. Eur J Clin Pharmacol 2003;59:553–7. http://dx.doi.
org/10.1007/s00228-003-0651-x
362. Wanwimolruk S, Kaewvichit S, Tanthayaphinant O, Suwannarach C,
Oranratnachai A. Lack of effect of oral contraceptive use on the
pharmacokinetics of quinine. Br J Clin Pharmacol 1991;31:179–81.
http://dx.doi.org/10.1111/j.1365-2125.1991.tb05509.x
363. Back DJ, Breckenridge AM, Crawford F, et al. The effect of rifampicin
on norethisterone pharmacokinetics. Eur J Clin Pharmacol
1979;15:193–7. http://dx.doi.org/10.1007/BF00563105
364. Back DJ, Breckenridge AM, Crawford FE, et al. The effect of rifampicin
on the pharmacokinetics of ethynylestradiol in women. Contraception
1980;21:135–43. http://dx.doi.org/10.1016/0010-7824(80)90125-0
365. Barditch-Crovo P, Trapnell CB, Ette E, et al. The effects of rifampin
and rifabutin on the pharmacokinetics and pharmacodynamics of a
combination oral contraceptive. Clin Pharmacol Ther 1999;65:428–38.
http://dx.doi.org/10.1016/S0009-9236(99)70138-4
366. Bolt HM, Bolt M, Kappus H. Interaction of rifampicin treatment with
pharmacokinetics and metabolism of ethinyloestradiol in man. Acta
Endocrinol (Copenh) 1977;85:189–97.
367. Gupta KC, Ali MY. Failure of oral contraceptive with rifampicin. Med
J Zambia 1980;15:23.
368. Hirsch A. [Letter: Sleeping pills]. Nouv Presse Med 1973;2:2957.
369. Hirsch A, Tillement JP, Chretien J. Effets contrariants de la rifampicine
sur les contraceptifs oraux: a propos de trois grossesses non desiree chez
trois malades. Rev Fr Mal Respir 1975;2:174–82.
370. Joshi JV, Joshi UM, Sankolli GM, et al. A study of interaction of a low-dose
combination oral contraceptive with anti-tubercular drugs. Contraception
1980;21:617–29. http://dx.doi.org/10.1016/0010-7824(80)90034-7
371. Kropp R. [Rifampicin and oral contraceptives (author’s transl)]. Prax
Pneumol 1974;28:270–2.
372. LeBel M, Masson E, Guilbert E, et al. Effects of rifabutin and rifampicin on
the pharmacokinetics of ethinylestradiol and norethindrone. J Clin Pharmacol
1998;38:1042–50. http://dx.doi.org/10.1177/009127009803801109
373. Meyer B, Müller F, Wessels P, Maree J. A model to detect interactions
between roxithromycin and oral contraceptives. Clin Pharmacol Ther
1990;47:671–4. http://dx.doi.org/10.1038/clpt.1990.92
374. Nocke-Finck L, Breuer H, Reimers D. Dtsch Med Wochenschr
1973;98:1521–3. http://dx.doi.org/10.1055/s-0028-1107071
375. Piguet B, Muglioni JF, Chaline G. [Letter: Oral contraception and
rifampicin]. Nouv Presse Med 1975;04:115–6.
376. Reimers D, Jezek A. [The simultaneous use of rifampicin and other
antitubercular agents with oral contraceptives]. Prax Pneumol
1971;25:255–62.
377. Skolnick JL, Stoler BS, Katz DB, Anderson WH. Rifampin, oral
contraceptives, and pregnancy. JAMA 1976;236:1382. http://dx.doi.
org/10.1001/jama.1976.03270130044027
378. Szoka PR, Edgren RA. Drug interactions with oral contraceptives:
compilation and analysis of an adverse experience report database. Fertil
Steril 1988;49(Suppl 2):31S–8S.
379. Berry-Bibee E, Kim MJ, Simmons K, Pagano P, Curtis K. Drug
interactions between hormonal contraceptives and psychotropic drugs:
a systematic review. Contraception. In press 2016.
380. Berry-Bibee E, Kim MJ, Tepper N, Riley H, Curtis K. The safety of
St John’s wort and hormonal contraceptives: a systematic review.
Contraception. In press 2016.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 81
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix E
Classifications for Barrier Methods
BOX E1. Categories for classifying barrier methods
1=A condition for which there is no restriction for the
use of the contraceptive method.
2=A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3=A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4=A condition that represents an unacceptable health
risk if the contraceptive method is used.
TABLE E1. Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
Personal Characteristics and Reproductive History
Pregnancy NA NA NA Clarication: None of these methods are relevant for
contraception during known pregnancy. However, for
women who remain at risk for STDs/HIV during
pregnancy, the correct and consistent use of condoms is
recommended.
Age
a. Menarche to <40 years 1 1 1 —
b. ≥40 years 1 1 1 —
Parity
a. Nulliparous 1 1 1 —
b. Parous 1 1 2 Clarication: Risk for cervical cap failure is higher in
parous women than in nulliparous women.
Postpartum (breastfeeding and nonbreastfeeding)
a. <6 weeks postpartum 1 1 NA Clarication: Diaphragm and cap are unsuitable until
uterine involution is complete.
b. ≥6 weeks postpartum 1 1 1 —
Postabortion
a. First trimester 1 1 1 —
b. Second trimester 1 1 1 Clarication: Diaphragm and cap are unsuitable until 6
weeks after second trimester abortion.
c. Immediate postseptic abortion 1 1 1 —
Past ectopic pregnancy 1 1 1 —
History of pelvic surgery 1 1 1 —
Smoking
a. Age <35 years 1 1 1 —
b. Age ≥35 years
i. <15 cigarettes per day 1 1 1 —
ii. ≥15 cigarettes per day 1 1 1 —
Obesity Comment: Severe obesity might make diaphragm and
cap placement dicult.
a. BMI ≥30 kg/m
2
1 1 1
b. Menarche to <18 years and BMI ≥30 kg/m
2
1 1 1
See table footnotes on page 87.
Classifications for barrier contraceptive methods include
those for condoms, which include male latex condoms, male
polyurethane condoms, and female condoms; spermicides; and
diaphragm with spermicide or cervical cap (Box E1) (Table E1).
Women with conditions that make pregnancy an unacceptable
risk should be advised that barrier methods for pregnancy
prevention might not be appropriate for those who cannot
use them consistently and correctly because of the relatively
higher typical-use failure rates of these methods. Women
should be counseled that consistent and correct use of the
male latex condom reduces the risk for transmission of human
immunodeficiency virus (HIV) and other sexually transmitted
diseases (STDs). Use of female condoms can provide protection
from transmission of STDs, although data are limited.

Recommendations and Reports
82 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
History of bariatric surgery
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease storage capacity of the
stomach (vertical banded gastroplasty, laparoscopic
adjustable gastric band, or laparoscopic sleeve
gastrectomy)
1 1 1 —
b. Malabsorptive procedures: decrease absorption of
nutrients and calories by shortening the functional length
of the small intestine (Roux-en-Y gastric bypass or
biliopancreatic diversion)
1 1 1 —
Cardiovascular Disease
Multiple risk factors for atherosclerotic cardiovascular
disease (e.g., older age, smoking, diabetes, hypertension,
low HDL, high LDL, or high triglyceride levels)
1 1 1 —
Hypertension
Systolic blood pressure ≥160 mm Hg or diastolic blood
pressure ≥100 mm Hg are associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
a. Adequately controlled hypertension 1 1 1 —
b. Elevated blood pressure levels
(properly taken measurements)
i. Systolic 140–159 mm Hg or diastolic 90–99 mm Hg 1 1 1 —
ii. Systolic ≥160 mm Hg or diastolic ≥100 mm Hg 1 1 1 —
c. Vascular disease 1 1 1 —
History of high blood pressure during pregnancy (when
current blood pressure is measurable and normal)
1 1 1 —
Deep venous thrombosis/Pulmonary embolism
a. History of DVT/PE, not receiving anticoagulant therapy
i. Higher risk for recurrent DVT/PE (one or more risk
factors)
1 1 1 —
• History of estrogen-associated DVT/PE
• Pregnancy-associated DVT/PE
• Idiopathic DVT/PE
• Known thrombophilia, including antiphospholipid
syndrome
• Active cancer (metastatic, receiving therapy, or within
6 months after clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE (no risk factors) 1 1 1 —
b. Acute DVT/PE 1 1 1 —
c. DVT/PE and established anticoagulant therapy for at
least 3 months
i. Higher risk for recurrent DVT/PE (one or more risk
factors)
1 1 1
• Known thrombophilia, including antiphospholipid
syndrome
• Active cancer (metastatic, receiving therapy, or within
6 months after clinical remission), excluding
nonmelanoma skin cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE (no risk factors) 1 1 1 —
d. Family history (rst-degree relatives) 1 1 1 —
e. Major surgery
i. With prolonged immobilization 1 1 1 —
ii. Without prolonged immobilization 1 1 1 —
f. Minor surgery without immobilization 1 1 1 —
See table footnotes on page 87.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 83
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
Known thrombogenic mutations (e.g., factor V Leiden;
prothrombin mutation; or protein S, protein C, and
antithrombin deciencies)
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 Clarication: Routine screening is not appropriate
because of the rarity of the conditions and the high cost
of screening.
Supercial venous disorders
a. Varicose veins 1 1 1 —
b. Supercial venous thrombosis (acute or history) 1 1 1 —
Current and history of ischemic heart disease
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Stroke (history of cerebrovascular accident)
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Valvular heart disease
Complicated valvular heart disease is associated with
increased risk for adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 —
b. Complicated (pulmonary hypertension, risk for atrial
brillation, or history of subacute bacterial endocarditis)
1 1 2 —
Peripartum cardiomyopathy
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Normal or mildly impaired cardiac function (New York
Heart Association Functional Class I or II: patients with no
limitation of activities or patients with slight, mild
limitation of activity) (1)
i. <6 months 1 1 1 —
ii. ≥6 months 1 1 1 —
b. Moderately or severely impaired cardiac function (New
York Heart Association Functional Class III or IV: patients
with marked limitation of activity or patients who should
be at complete rest) (1)
1 1 1 —
Rheumatic Diseases
Systemic lupus erythematosus
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Positive (or unknown) antiphospholipid antibodies 1 1 1 —
b. Severe thrombocytopenia 1 1 1 —
c. Immunosuppressive therapy 1 1 1 —
d. None of the above 1 1 1
—
Rheumatoid arthritis
a. Receiving immunosuppressive therapy 1 1 1 —
b. Not receiving immunosuppressive therapy 1 1 1 —
Neurologic Conditions
Headaches —
a. Nonmigraine (mild or severe) 1 1 1 —
b. Migraine
i. Without aura (This category of migraine includes
menstrual migraine.)
1 1 1 Comment: Menstrual migraine is a subtype of migraine
without aura. For more information see The International
Headache Society Classication, 3rd edition (http://www.
ihs-classication.org/_downloads/mixed/International-
Headache-Classication-III-ICHD-III-2013-Beta.pdf).
ii. With aura 1 1 1 —
Epilepsy
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Multiple sclerosis
a. With prolonged immobility 1 1 1 —
b. Without prolonged immobility 1 1 1 —
Depressive Disorders
Depressive disorders 1 1 1 —
Reproductive Tract Infections and Disorders
Unexplained vaginal bleeding
(suspicious for serious condition) before evaluation
1 1 1 Clarication: If pregnancy or an underlying pathological
condition (e.g., pelvic malignancy) is suspected, it must
be evaluated and the category adjusted after evaluation.
See table footnotes on page 87.

Recommendations and Reports
84 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
Endometriosis 1 1 1 —
Benign ovarian tumors (including cysts) 1 1 1 —
Severe dysmenorrhea 1 1 1 —
Gestational trophoblastic disease
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Suspected gestational trophoblastic disease
(immediate postevacuation)
i. Uterine size rst trimester 1 1 1 —
ii. Uterine size second trimester 1 1 1 —
b. Conrmed gestational trophoblastic disease
(after initial evacuation and during monitoring)
i. Undetectable/nonpregnant β–hCG levels 1 1 1 —
ii. Decreasing β–hCG levels 1 1 1 —
iii. Persistently elevated β-hCG levels or malignant
disease, with no evidence or suspicion of intrauterine
disease
1 1 1 —
iv. Persistently elevated β-hCG levels or malignant
disease, with evidence or suspicion of intrauterine
disease
1 1 1 —
Cervical ectropion 1 1 1 —
Cervical intraepithelial neoplasia 1 1 1 Clarication: The cap should not be used. Diaphragm use
has no restrictions.
Cervical cancer (awaiting treatment) 1 2 1 Clarication: The cap should not be used. Diaphragm use
has no restrictions.
Comment: Repeated and high-dose use of the spermicide
nonoxynol-9 can cause vaginal and cervical irritation or
abrasions.
Breast disease
Breast cancer is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Undiagnosed mass 1 1 1 —
b. Benign breast disease 1 1 1 —
c. Family history of cancer 1 1 1 —
d. Breast cancer
i. Current 1 1 1 —
ii. Past and no evidence of current disease for 5 years
1 1 1 —
Endometrial hyperplasia 1 1 1 —
Endometrial cancer
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Ovarian cancer
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Uterine broids 1 1 1 —
Anatomical abnormalities 1 1 NA Clarication: The diaphragm cannot be used in certain
cases of prolapse. Cap use is not appropriate for a woman
with markedly distorted cervical anatomy.
Pelvic inammatory disease
a. Past PID
i. With subsequent pregnancy 1 1 1 —
ii. Without subsequent pregnancy 1 1 1 —
b. Current PID 1 1 1 —
Sexually transmitted diseases
a. Current purulent cervicitis or chlamydial infection or
gonococcal infection
1 1 1 —
b. Vaginitis (including Trichomonas vaginalis and bacterial
vaginosis)
1 1 1 —
c. Other factors related to STDs 1 1 1 —
HIV
High risk for HIV 1 4 4 Evidence: Repeated and high-dose use of the spermicide
nonoxynol-9 was associated with increased risk for
genital lesions, which might increase the risk for HIV
infection (2).
Comment: Diaphragm use is assigned category 4 because
of concerns about the spermicide, not the diaphragm.
See table footnotes on page 87.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 85
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
HIV infection
For women with HIV infection who are not clinically well or
not receiving ARV therapy, this condition is associated with
increased risk for adverse health events as a result of
pregnancy (Box 2).
1 3 3 Comment: Use of spermicides or diaphragms (with
spermicide) can disrupt the cervical mucosa, which might
increase viral shedding and HIV transmission to
noninfected sex partners.
Other Infections
Schistosomiasis
Schistosomiasis with brosis of the liver is associated with
increased risk for adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 —
b. Fibrosis of the liver 1 1 1 —
Tuberculosis
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Nonpelvic 1 1 1 —
b. Pelvic 1 1 1 —
Malaria 1 1 1 —
History of toxic shock syndrome 1 1 3 Comment: Toxic shock syndrome has been reported in
association with contraceptive sponge and diaphragm use.
Urinary tract infection 1 1 2 Comment: Use of diaphragms and spermicides might
increase risk for urinary tract infection.
Endocrine Conditions
Diabetes
Insulin-dependent diabetes; diabetes with nephropathy,
retinopathy, or neuropathy; diabetes with other vascular
disease; or diabetes of >20 years’ duration are associated
with increased risk for adverse health events as a result of
pregnancy (Box 2).
a. History of gestational disease 1 1 1 —
b. Nonvascular disease
i. Non-insulin dependent 1 1 1 —
ii. Insulin dependent 1 1 1 —
c. Nephropathy, retinopathy, or neuropathy 1 1 1 —
d. Other vascular disease or diabetes of >20 years’
duration
1 1 1 —
Thyroid disorders
a. Simple goiter 1 1 1 —
b. Hyperthyroid 1 1 1 —
c. Hypothyroid 1 1 1 —
Gastrointestinal Conditions
Inammatory bowel disease
(ulcerative colitis or Crohn’s disease)
1 1 1 —
Gallbladder disease
a. Symptomatic
i. Treated by cholecystectomy 1 1 1 —
ii. Medically treated 1 1 1 —
iii. Current 1 1 1 —
b. Asymptomatic 1 1 1 —
History of cholestasis
a. Pregnancy related 1 1 1 —
b. Past COC related 1 1 1 —
Viral hepatitis
a. Acute or are 1 1 1 —
b. Carrier 1 1 1 —
c. Chronic 1 1 1 —
Cirrhosis
Severe cirrhosis is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Mild (compensated) 1 1 1 —
b. Severe (decompensated) 1 1 1 —
See table footnotes on page 87.

Recommendations and Reports
86 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
Liver tumors
Hepatocellular adenoma and malignant liver tumors are
associated with increased risk for adverse health events as a
result of pregnancy (Box 2).
a. Benign
i. Focal nodular hyperplasia 1 1 1 —
ii. Hepatocellular adenoma 1 1 1 —
b. Malignant (hepatoma) 1 1 1 —
Respiratory Conditions
Cystic brosis
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Anemias
Thalassemia 1 1 1 —
Sickle cell disease
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
1 1 1 —
Iron deciency anemia 1 1 1 —
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with increased risk for adverse
health events as a result of pregnancy (Box 2).
a. Complicated: graft failure (acute or chronic), rejection,
or cardiac allograft vasculopathy
1 1 1 —
b. Uncomplicated 1 1 1 —
Drug Interactions
Antiretroviral therapy Clarication: No drug interaction between ARV therapy
and barrier method use is known. However, HIV infection
is classied as category 3 for spermicides and diaphragms
(see HIV section).
a. Nucleoside reverse transcriptase inhibitors (NRTIs)
i. Abacavir (ABC) 1 3 3
ii. Tenofovir (TDF) 1 3 3
iii. Zidovudine (AZT) 1 3 3
iv. Lamivudine (3TC) 1 3 3
v. Didanosine (DDI) 1 3 3
vi. Emtricitabine (FTC) 1 3 3
vii. Stavudine (D4T) 1 3 3
b. Nonnucleoside reverse transcriptase inhibitors (NNRTIs)
i. Efavirenz (EFV) 1 3 3
ii. Etravirine (ETR) 1 3 3
iii. Nevirapine (NVP) 1 3 3
iv. Rilpivirine (RPV) 1 3 3
c. Ritonavir-boosted protease inhibitors
i. Ritonavir-boosted atazanavir (ATV/r) 1
3 3
ii. Ritonavir-boosted darunavir (DRV/r) 1 3 3
iii. Ritonavir-boosted fosamprenavir (FPV/r) 1 3 3
iv. Ritonavir-boosted lopinavir (LPV/r) 1 3 3
v. Ritonavir-boosted saquinavir (SQV/r) 1 3 3
vi. Ritonavir-boosted tipranavir (TPV/r) 1 3 3
d. Protease inhibitors without ritonavir
i. Atazanavir (ATV) 1 3 3
ii. Fosamprenavir (FPV) 1 3 3
iii. Indinavir (IDV) 1 3 3
iv. Nelnavir (NFV) 1 3 3
e. CCR5 co-receptor antagonists
i. Maraviroc (MVC) 1 3 3
f. HIV integrase strand transfer inhibitors
i. Raltegravir (RAL) 1 3 3
ii. Dolutegravir (DTG) 1 3 3
iii. Elvitegravir (EVG) 1 3 3
g. Fusion inhibitors
i. Enfuvirtide 1 3 3
Anticonvulsant therapy
a. Certain anticonvulsants (phenytoin, carbamazepine,
barbiturates, primidone, topiramate, or oxcarbazepine)
1 1 1 —
b. Lamotrigine 1 1 1 —
See table footnotes on page 87.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 87
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE E1. (Continued) Classifications for barrier methods, including condoms, spermicides, diaphragms (with spermicide), and cap
Condition
Category
Clarifications/Evidence/CommentsCondom Spermicide
Diaphragm (with
spermicide)/Cap
Antimicrobial therapy
a. Broad-spectrum antibiotics 1 1 1 —
b. Antifungals 1 1 1 —
c. Antiparasitics 1 1 1 —
d. Rifampin or rifabutin therapy 1 1 1 —
Psychotropic medications
a. SSRIs 1 1 1 —
St. John’s wort 1 1 1 —
Allergy to latex 3 1 3 Clarication: The condition of allergy to latex does not
apply to plastic condoms/diaphragms.
Abbreviations: ARV=antiretroviral; BMI=body mass index; COC=combined oral contraceptive; DVT=deep venous thrombosis; hCG=human chorionic gonadotropin; HDL=high-density
lipoprotein; HIV=human immunodeficiency virus; LDL=low-density lipoprotein; NA=not applicable; PE=pulmonary embolism; PID=pelvic inflammatory disease; SSRI = selective serotonin
reuptake inhibitor; STD=sexually transmitted disease.
References
1. The Criteria Committee of the New York Heart Association. Nomenclature
and criteria for diagnosis of diseases of the heart and great vessels. 9th ed.
Boston, MA: Little, Brown and Co; 1994.
2. Wilkinson D, Ramjee G, Tholandi M, Rutherford G. Nonoxynol-9 for
preventing vaginal acquisition of HIV infection by women from men.
Cochrane Database Syst Rev 2002;4(CD003936):CD003936.

Recommendations and Reports
88 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix F
Classifications for Fertility Awareness–Based Methods
Fertility awareness–based (FAB) methods of family planning
involve identifying the fertile days of the menstrual cycle,
whether by observing fertility signs such as cervical secretions
and basal body temperature or by monitoring cycle days
(Box F1) (Table F1). FAB methods can be used in combination
with abstinence or barrier methods during the fertile time. If
barrier methods are used, see the Classifications for Barrier
Methods (Appendix E).
No medical conditions worsen because of FAB methods.
In general, FAB methods can be used without concern for
health effects in persons who choose them. However, several
conditions make their use more complex. The existence of
these conditions suggests that 1) use of these methods should
be delayed until the condition is corrected or resolved, or
2) persons using FAB methods need special counseling, and
a provider with particular training in use of these methods is
generally necessary to ensure correct use.
Women with conditions that make pregnancy an unacceptable
risk should be advised that FAB methods might not be
appropriate for them because of the relatively higher typical-use
failure rates of these methods. Symptoms-based and calendar-
based methods do not protect against sexually transmitted
diseases (STDs), including human immunodeficiency virus
(HIV), and women using these methods should be counseled
that consistent and correct use of the male latex condom reduces
the risk for transmission of HIV and other STDs. Use of female
condoms can provide protection from transmission of STDs,
although data are limited.
BOX F1. Definitions for terms associated with fertility awareness–
based methods
• Symptoms-based methods: FAB methods based on
observation of fertility signs (e.g., cervical secretions or basal
body temperature) such as the cervical mucus method, the
symptothermal method, and the TwoDay method.
• Calendar-based methods: FAB methods based on
calendar calculations such as the calendar rhythm
method and the standard days method.
• Accept: No medical reason exists to deny the particular
FAB method to a woman in this circumstance.
• Caution: The method normally is provided in a routine
setting but with extra preparation and precautions. For
FAB methods, this usually means that special counseling
might be needed to ensure correct use of the method by
a woman in this circumstance.
• Delay: Use of this method should be delayed until the
condition is evaluated or corrected. Alternative
temporary methods of contraception should be offered.
Abbreviation: FAB = fertility awareness–based.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 89
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE F1. Fertility awareness–based methods, including symptoms-based and calendar-based methods
Condition
Category
Clarifications/Evidence/Comments
Symptoms-based
method
Calendar-based
method
Personal Characteristics and Reproductive History
Pregnancy NA NA Clarication: FAB methods are not relevant during pregnancy.
Life stage Comment: Menstrual irregularities are common in postmenarche and perimenopause
and might complicate the use of FAB methods.
a. Postmenarche Caution Caution
b. Perimenopause Caution Caution
Breastfeeding Comment: Use of FAB methods when breastfeeding might be less eective than when
not breastfeeding.
a. <6 weeks postpartum Delay Delay Comment: Women who are primarily breastfeeding and are amenorrheic are unlikely to
have sucient ovarian function to produce detectable fertility signs and hormonal changes
during the rst 6 months postpartum. However, the likelihood of resumption of fertility
increases with time postpartum and with substitution of breast milk by other foods.
b. ≥6 weeks Caution Delay
c. After menses begin Caution Caution Clarication: When the woman notices fertility signs, particularly cervical secretions, she
can use a symptoms-based method. First postpartum menstrual cycles in breastfeeding
women vary signicantly in length. Return to regularity takes several cycles. When she has
had at least three postpartum menses and her cycles are regular again, she can use a
calendar-based method. When she has had at least four postpartum menses and her most
recent cycle lasted 26–32 days, she can use the standard days method. Before that time, a
barrier method should be oered if the woman plans to use a FAB method later.
Postpartum (nonbreastfeeding women)
a. <4 weeks Delay Delay Clarication: Nonbreastfeeding women are not likely to have detectable fertility signs
or hormonal changes before 4 weeks postpartum. Although the risk for pregnancy is
low, ovulation before rst menses is common; therefore, a method appropriate for the
postpartum period should be oered.
b. ≥4 weeks Accept Delay Clarication: Nonbreastfeeding women are likely to have sucient ovarian function to
produce detectable fertility signs, hormonal changes, or both at this time; likelihood
increases rapidly with time postpartum. Women can use calendar-based methods as
soon as they have completed three postpartum menses. Methods appropriate for the
postpartum period should be oered before that time.
Postabortion Caution Delay Clarication: After abortion, women are likely to have sucient ovarian function to
produce detectable fertility signs, hormonal changes, or both; likelihood increases with
time postabortion. Women can start using calendar-based methods after they have had
at least one postabortion menses (e.g., women who before this pregnancy primarily had
cycles of 26–32 days can then use the standard days method). Methods appropriate for
the postabortion period should be oered before that time.
Reproductive Tract Infections and Disorders
Irregular vaginal bleeding Delay Delay Clarication: Presence of this condition makes FAB methods unreliable. Therefore,
barrier methods should be recommended until the bleeding pattern is compatible with
proper method use. The condition should be evaluated and treated as necessary.
Vaginal discharge Delay Accept Clarication: Because vaginal discharge makes recognition of cervical secretions
dicult, the condition should be evaluated and treated if needed before providing
methods based on cervical secretions.
Other
Use of drugs that aect cycle regularity,
hormones, or fertility signs
Caution /Delay Caution/Delay Clarication: Use of certain mood-altering drugs such as lithium, tricyclic antidepres-
sants, and antianxiety therapies, as well as certain antibiotics and anti-inammatory
drugs, might alter cycle regularity or aect fertility signs. The condition should be
carefully evaluated and a barrier method oered until the degree of eect has been
determined or the drug is no longer being used.
Diseases that elevate body temperature
a. Chronic diseases Caution Accept Clarication: Elevated temperatures might make basal body temperature dicult to interpret
but have no eect on cervical secretions. Thus, use of a method that relies on temperature
should be delayed until the acute febrile disease abates. Temperature-based methods are not
appropriate for women with chronically elevated temperatures. In addition, some chronic
diseases interfere with cycle regularity, making calendar-based methods dicult to interpret.
b. Acute diseases Delay Accept
Abbreviations: FAB=fertility awareness–based; NA = not applicable.
Recommendations and Reports
90 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix G
Lactational Amenorrhea Method
The Bellagio Consensus provided the scientific basis for
defining the conditions under which breastfeeding can be used
safely and effectively for birth-spacing purposes; programmatic
guidelines were developed at a meeting of family planning
experts for its use as a method of family planning, and the
method was then given the name the lactational amenorrhea
method (1,2). These guidelines include the following three
criteria, all of which must be met to ensure adequate protection
from an unplanned pregnancy: 1) amenorrhea; 2) fully or
nearly fully breastfeeding (no interval of >4–6 hours between
breastfeeds); and 3) <6 months postpartum.
All major medical organizations recommend exclusive
breastfeeding for the first 6 months of life, with continuing
breastfeeding through the first year and beyond for as long as
mutually desired (3). No medical conditions exist for which
use of the lactational amenorrhea method for contraception is
restricted. However, breastfeeding might not be recommended
for women or infants with certain conditions.
Women with conditions that make pregnancy an unacceptable
risk should be advised that the lactational amenorrhea method
might not be appropriate for them because of its relatively higher
typical-use failure rates. The lactational amenorrhea method does
not protect against sexually transmitted diseases (STDs), including
human immunodeficiency virus (HIV), and women using this
method should be counseled that consistent and correct use of
the male latex condom reduces the risk for transmission of HIV
and other STDs. Use of female condoms can provide protection
from transmission of STDs, although data are limited.
HIV Infection
HIV can be transmitted from mother to infant through
breastfeeding. Therefore, in the United States, where
replacement feeding is affordable, feasible, acceptable,
sustainable, and safe, breastfeeding for women with HIV is
not recommended (3,4).
Other Medical Conditions
The American Academy of Pediatrics (AAP) also recommends
against breastfeeding for women with active untreated
tuberculosis disease, untreated brucellosis, varicella, H1N1
influenza, or positivity for human T-cell lymphotropic virus
types I or II or for those who have herpes simplex lesions on
a breast. In addition, infants with classic galactosemia should
not breastfeed (3).
Medication Used During Breastfeeding
AAP recommends that the benefits of breastfeeding outweigh
the risk of exposure to most therapeutic agents via human
milk. More information about specific drugs and radioactive
compounds is provided by AAP (5) and LactMed (http://
toxnet.nlm.nih.gov).
References
1. Kennedy KI, Rivera R, McNeilly AS. Consensus statement on the use of
breastfeeding as a family planning method. Contraception 1989;39:477–
96. http://dx.doi.org/10.1016/0010-7824(89)90103-0
2. Labbok M, Cooney K, Coly S. Guidelines: breastfeeding, family planning,
and the Lactational Amenorrhea Method-LAM. Washington, DC: Institute
for Reproductive Health; 1994.
3. American Academy of Pediatrics Section on Breastfeeding. Breastfeeding
and the use of human milk [Policy statement]. Pediatrics 2012;129:e827–
41. http://dx.doi.org/10.1542/peds.2011-3552
4. Perinatal HIV Guidelines Working Group. Public Service Task Force
recommendations for use of antiretroviral drugs in pregnant HIV-infected women
for maternal health and interventions to reduce perinatal HIV transmission in
the United States. Rockville, MD: Public Health Service Task Force; 2009.
5. Sachs HC; Committee On Drugs. The transfer of drugs and therapeutics
into human breast milk: an update on selected topics. Pediatrics
2013;132:e796–809. http://dx.doi.org/10.1542/peds.2013-1985
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 91
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix H
Coitus Interruptus (Withdrawal)
Coitus interruptus, also known as withdrawal, is a traditional
family planning method in which the man completely removes
his penis from the vagina and away from the external genitalia
of the female partner before he ejaculates. Coitus interruptus
prevents sperm from entering the woman’s vagina, thereby
preventing contact between spermatozoa and the ovum.
is method might be appropriate for couples
• who are highly motivated and able to use this method
effectively;
• with religious or philosophical reasons for not using other
methods of contraception;
• who need contraception immediately and have entered
into a sexual act without alternative methods available;
• who need a temporary method while awaiting the start of
another method; or
• who have intercourse infrequently.
Some benefits of coitus interruptus are that the method, if used
correctly, does not affect breastfeeding and is always available
for primary use or use as a back-up method. In addition, coitus
interruptus involves no economic cost or use of chemicals and
has no directly associated health risks. Coitus interruptus does not
protect against sexually transmitted diseases (STDs), including
human immunodeficiency virus (HIV), and women using this
method should be counseled that consistent and correct use of the
male latex condom reduces the risk for transmission of HIV and
other STDs. Use of female condoms can provide protection from
transmission of STDs, although data are limited.
Coitus interruptus is unforgiving of incorrect use, and its
effectiveness depends on the willingness and ability of the couple
to use withdrawal with every act of intercourse. Women with
conditions that make pregnancy an unacceptable risk should be
advised that coitus interruptus might not be appropriate for them
because of its relatively higher typical-use failure rates.
Recommendations and Reports
92 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
Appendix I
Female and Male Sterilization
Tubal sterilization for women and vasectomy for men are
permanent, safe, and highly effective methods of contraception.
In general, no medical conditions absolutely restrict a person’s
eligibility for sterilization (with the exception of known
allergy or hypersensitivity to any materials used to complete
the sterilization method). However, certain conditions
place a woman at high surgical risk; in these cases, careful
consideration should be given to the risks and benefits of
other acceptable alternatives, including long-acting, highly
effective, reversible methods and vasectomy. Female and male
sterilization do not protect against sexually transmitted diseases
(STDs), including human immunodeficiency virus (HIV),
and women using these methods should be counseled that
consistent and correct use of the male latex condom reduces
the risk for transmission of HIV and other STDs. Use of female
condoms can provide protection from transmission of STDs,
although data are limited.
Because these methods are intended to be irreversible,
persons who choose sterilization should be certain that they
want to prevent pregnancy permanently. Most persons who
choose sterilization remain satisfied with their decision.
However, a small proportion of women regret this decision
(1%–26% from different studies, with higher rates of regret
reported by women who were younger at sterilization) (1,2).
Regret among men about vasectomy has been reported to be
approximately 5% (3), similar to the proportion of women
who report regretting their husbands’ vasectomy (6%) (4).
Therefore, all persons should be appropriately counseled about
the permanency of sterilization and the availability of highly
effective, reversible methods of contraception.
References
1. Hillis SD, Marchbanks PA, Tylor LR, Peterson HB. Poststerilization
regret: findings from the United States Collaborative Review of
Sterilization. Obstet Gynecol 1999;93:889–95.
2. Peterson HB. Sterilization. Obstet Gynecol 2008;111:189–203. http://
dx.doi.org/10.1097/01.AOG.0000298621.98372.62
3. Ehn BE, Liljestrand J. A long-term follow-up of 108 vasectomized men.
Good counselling routines are important. Scand J Urol Nephrol
1995;29:477–81. http://dx.doi.org/10.3109/00365599509180030
4. Jamieson DJ, Kaufman SC, Costello C, Hillis SD, Marchbanks PA,
Peterson HB; US Collaborative Review of Sterilization Working Group.
A comparison of women’s regret after vasectomy versus tubal sterilization.
Obstet Gynecol 2002;99:1073–9.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 93
US Department of Health and Human Services/Centers for Disease Control and Prevention
BOX J1. Categories for classifying emergency contraception
1 = A condition for which there is no restriction for the
use of the contraceptive method.
2 = A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3 = A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4 = A condition that represents an unacceptable health
risk if the contraceptive method is used.
TABLE J1. Classifications for emergency contraception, including the copper-containing intrauterine device, ulipristal acetate, levonorgestrel,
and combined oral contraceptives*
Condition
Category
Clarifications/Evidence/CommentsCu-IUD UPA LNG COC
Personal Characteristics and Reproductive History
Pregnancy 4 NA NA NA Clarication (IUD): The IUD is not indicated during pregnancy and should
not be used because of the risk for serious pelvic infection and septic
spontaneous abortion.
Clarication (ECPs): Although this method is not indicated for a woman with
a known or suspected pregnancy, no harm to the woman, the course of her
pregnancy, or the fetus if ECPs are inadvertently used is known to exist.
Evidence: Evidence suggests that poor pregnancy outcomes are rare
among pregnant women who used ECPs during conception cycle or early in
pregnancy (1).
Breastfeeding 1 1 1 1 Clarication (UPA): Breastfeeding is not recommended for 24 hours after
taking UPA because it is excreted in breast milk, with highest concentra-
tions in the rst 24 hours, and maximum maternal serum levels are reached
1–3 hours after administration. Mean UPA concentrations in breast milk
decrease markedly from 0 to 24–48 hours and then slowly decrease over 5
days (2). Breast milk should be expressed and discarded for 24 hours after
taking UPA.
Evidence: Breastfeeding outcomes do not seem to dier between women
exposed to LNG and those who are not exposed. One pharmacokinetic
study demonstrated that LNG passes to breast milk but in minimal
quantities (1).
Past ectopic pregnancy 1 1 1 1 —
History of bariatric surgery
This condition is associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease storage capacity
of the stomach (vertical banded gastroplasty,
laparoscopic adjustable gastric band, or laparoscopic
sleeve gastrectomy)
1 1 1 1 —
b. Malabsorptive procedures: decrease absorption of
nutrients and calories by shortening the functional
length of the small intestine (Roux-en-Y gastric
bypass or biliopancreatic diversion)
1 1 1 1 Comment: Bariatric surgical procedures involving a malabsorptive
component have the potential to decrease oral contraceptive eectiveness,
perhaps further decreased by postoperative complications such as
long-term diarrhea, vomiting, or both. Because of these malabsorptive
concerns, an emergency IUD might be more appropriate than ECPs.
See table footnotes on page 94.
Appendix J
Classifications for Emergency Contraception
A copper-containing intrauterine device (Cu-IUD) can be
used within 5 days of unprotected intercourse as an emergency
contraceptive. However, when the time of ovulation can be
estimated, the Cu-IUD can be inserted beyond 5 days after
intercourse, if necessary, as long as the insertion does not occur
>5 days after ovulation. The eligibility criteria for interval
Cu-IUD insertion also apply for the insertion of Cu-IUDs as
emergency contraception (Box J1) (Table J1).
Classifications for emergency contraceptive pills (ECPs) are
given for ulipristal acetate (UPA), levonorgestrel (LNG), and
combined oral contraceptives (COCs). Cu-IUDs, UPA, LNG,
and COCs do not protect against sexually transmitted diseases
(STDs), including human immunodeficiency virus (HIV),
and women using these methods should be counseled that
consistent and correct use of the male latex condom reduces
the risk for transmission of HIV and other STDs. Use of female
condoms can provide protection from transmission of STDs,
although data are limited.

Recommendations and Reports
94 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE J1. (Continued) Classifications for emergency contraception, including the copper-containing intrauterine device, ulipristal acetate,
levonorgestrel, and combined oral contraceptives*
Condition
Category
Clarifications/Evidence/CommentsCu-IUD UPA LNG COC
Cardiovascular Disease
History of severe cardiovascular disease (ischemic
heart disease, cerebrovascular attack, or other
thromboembolic conditions)
This condition is associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
1 2 2 2 Comment: The duration of ECP use is less than that of regular use of COCs
or POPs and thus would be expected to have less clinical impact.
Rheumatic Diseases
Rheumatoid arthritis
a. Receiving immunosuppressive therapy 2 1 1 1 —
b. Not receiving immunosuppressive therapy 1 1 1 1 —
Neurologic Conditions
Migraine 1 1 1 2 Comment: The duration of ECP use is less than that of regular use of COCs
and thus would be expected to have less clinical impact.
Gastrointestinal Conditions
Inammatory bowel disease (ulcerative colitis or
Crohn’s disease)
1 1 1 1 —
Severe liver disease (including jaundice)
This condition is associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
1 2 2 2 Comment: The duration of ECP use is less than that of regular use of COCs
or POPs and thus would be expected to have less clinical impact.
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with increased risk for
adverse health events as a result of pregnancy (Box 2).
a. Complicated: graft failure (acute or chronic),
rejection, or cardiac allograft vasculopathy
3 1 1 1 —
b. Uncomplicated 2 1 1 1 —
Other
Repeated ECP use 1 1 1 1 Clarication: Recurrent ECP use is an indication that the woman requires
further counseling about other contraceptive options. Frequently repeated
ECP use might be harmful for women with conditions classied as 2, 3, or 4
for CHC or POC use.
Evidence: In one case-control study, risk for ectopic pregnancy compared
with intrauterine pregnancy did not increase after repeated use of LNG
ECPs compared with nonuse (1).
Sexual assault 2 1 1 1 Clarication (IUD): Women who have experienced sexual assault are at
increased risk for STDs. According to CDC STD treatment guidelines, routine
presumptive treatment of chlamydia, gonorrhea, and trichomonas is
recommended after sexual assault (3). Women with current purulent
cervicitis or chlamydial infection or gonococcal infection should not
undergo IUD insertion (category 4).
Obesity (BMI ≥30 kg/m
2
) 1 2 2 2 Clarication (ECPs): ECPs might be less eective among women with BMI
≥30 kg/m
2
than among women with BMI <25 kg/m
2
. Despite this, no safety
concerns exist.
Evidence: Limited evidence from secondary data analyses suggests that
women with BMI ≥30 kg/m
2
experience an increased risk for pregnancy
after use of LNG compared with women with BMI <25 kg/m
2
. Two analyses
suggest obese women might also experience an increased risk for
pregnancy after use of UPA compared with nonobese women, although
this increase was not signicant in one study (4).
CYP3A4 inducers (e.g., bosentan, carbamazepine,
felbamate, griseofulvin, oxcarbazepine, phenytoin,
rifampin, St. John’s wort, topiramate, efavirenz, and
lumacaftor)
1 2 2 2 Clarication (ECPs): Strong CYP3A4 inducers might reduce the eective-
ness of ECPs.
Evidence: According to labelling information, rifampin markedly decreases
UPA levels by ≥90%, which might decrease its ecacy (2). Therefore,
theoretical concerns extend to use of other CYP3A4 inducers as well as to
COC and LNG ECPs, which have metabolic pathways similar to those of UPA.
A small pharmacokinetic study found that concomitant efavirenz use
decreased LNG levels in women taking LNG ECPs (0.75 mg) by 56%
compared with LNG ECPs alone (5).
Abbreviations: BMI = body mass index; CHC = combined hormonal contraceptive; COC = combined hormonal contraceptive; Cu-IUD = copper-containing intrauterine device; ECP = emergency
contraceptive pill; HIV = human immunodeficiency virus; IUD = intrauterine device; LNG = levonorgestrel; NA = not applicable; POC = progestin-only contraceptive; POP = progestin-only
pill; STD = sexually transmitted disease; UPA = ulipristal acetate.
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 95
US Department of Health and Human Services/Centers for Disease Control and Prevention
References
1. Jatlaoui TC, Riley H, Curtis KM. Safety data for levonorgestrel, ulipristal
acetate and Yuzpe regimens for emergency contraception. Contraception
2016;93:93–112. http://dx.doi.org/10.1016/j.contraception.2015.11.001
2. Watson Pharmaceuticals. Ella [Prescribing information]. Morristown, NJ; 2010.
https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022474s000lbl.pdf
3. Workowski KA, Bolan GA. Sexually transmitted diseases treatment
guidelines, 2015. MMWR Recomm Rep 2015;64(No. RR-03).
4. Jatlaoui TC, Curtis KM. Safety and effectiveness data for emergency
contraceptive pills among women with obesity: a systematic review.
Contraception 2016. Epub May 24, 2016. http://dx.doi.org/10.1016/j.
contraception.2016.05.002
5. Carten ML, Kiser JJ, Kwara A, Mawhinney S, Cu-Uvin S. Pharmacokinetic
interactions between the hormonal emergency contraception,
levonorgestrel (Plan B), and efavirenz. Infect Dis Obstet Gynecol
2012;2012:137192.

Recommendations and Reports
96 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Personal Characteristics And Reproductive History
Pregnancy 4* 4* NA* NA* NA* NA*
Age Menarche to
<20 years: 2
Menarche to
<20 years: 2
Menarche to
<18 years: 1
Menarche to
<18 years: 2
Menarche to
<18 years: 1
Menarche to
<40 years: 1
≥20 years: 1 ≥20 years: 1 18–45 years: 1 18–45 years: 1 18–45 years: 1 ≥40 years: 2
>45 years: 1 >45 years: 2 >45 years: 1
Parity
a. Nulliparous 2 2 1 1 1 1
b. Parous 1 1 1 1 1 1
Breastfeeding
a. <21 days postpartum — — 2* 2* 2* 4*
b. 21 to <30 days postpartum
i. With other risk factors for VTE (e.g.,
age ≥35 years, previous VTE,
thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
,
postpartum hemorrhage,
postcesarean delivery, preeclampsia,
or smoking)
— — 2* 2* 2* 3*
ii. Without other risk factors for VTE — — 2* 2* 2* 3*
c. 30–42 days postpartum
i. With other risk factors for VTE (e.g.,
age ≥35 years, previous VTE,
thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
,
postpartum hemorrhage,
postcesarean delivery, preeclampsia,
or smoking)
— — 1* 1* 1* 3*
ii. Without other risk factors for VTE — — 1* 1* 1* 2*
d. >42 days postpartum — — 1* 1* 1* 2*
See table footnotes on page 103.
Appendix K
Summary of Classifications for Hormonal Contraceptive Methods and Intrauterine Devices
Health-care providers can use the summary table as a quick
reference guide to the classifications for hormonal contraceptive
methods and intrauterine contraception to compare classifications
across these methods (Box K1) (Table K1). See the respective
appendix for each method for clarifications to the numeric
categories, as well as for summaries of the evidence and additional
comments. Hormonal contraceptives and intrauterine devices
do not protect against sexually transmitted diseases (STDs),
including human immunodeficiency virus (HIV), and women
using these methods should be counseled that consistent and
correct use of the male latex condom reduces the risk for
transmission of HIV and other STDs. Use of female condoms
can provide protection from transmission of STDs, although
data are limited.
BOX K1. Categories for classifying hormonal contraceptives and
intrauterine devices
1 = A condition for which there is no restriction for the
use of the contraceptive method.
2 = A condition for which the advantages of using the
method generally outweigh the theoretical or proven risks.
3 = A condition for which the theoretical or proven risks
usually outweigh the advantages of using the method.
4 = A condition that represents an unacceptable health
risk if the contraceptive method is used.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 97
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Postpartum (nonbreastfeeding
women)
a. <21 days postpartum — — 1 1 1 4
b. 21–42 days postpartum
i. With other risk factors for VTE (e.g.,
age ≥35 years, previous VTE,
thrombophilia, immobility,
transfusion at delivery, peripartum
cardiomyopathy, BMI ≥30 kg/m
2
,
postpartum hemorrhage,
postcesarean delivery, preeclampsia,
or smoking)
— — 1 1 1 3*
ii. Without other risk factors for VTE — — 1 1 1 2
c. >42 days postpartum — — 1 1 1 1
Postpartum (including cesarean
delivery)
a. <10 minutes after delivery of the
placenta
i. Breastfeeding 1* 2* — — — —
ii. Nonbreastfeeding 1* 1* — — — —
b. 10 minutes after delivery of the
placenta to <4 weeks (breastfeeding
or nonbreastfeeding)
2* 2* — — — —
c. ≥4 weeks (breastfeeding or
nonbreastfeeding)
1* 1* — — — —
d. Postpartum sepsis 4 4 — — — —
Postabortion
a. First trimester 1* 1* 1* 1* 1* 1*
b. Second trimester 2* 2* 1* 1* 1* 1*
c. Immediate postseptic abortion 4 4 1* 1* 1* 1*
Past ectopic pregnancy 1 1 1 1 2 1
History of pelvic surgery (see
Postpartum [Including Cesarean
Delivery] section)
1 1 1 1 1 1
Smoking
a. Age <35 years 1 1 1 1 1 2
b. Age ≥35 years
i. <15 cigarettes per day 1 1 1 1 1 3
ii. ≥15 cigarettes per day 1 1 1 1 1 4
Obesity
a. BMI ≥30 kg/m
2
1 1 1 1 1 2
b. Menarche to <18 years and BMI
≥30 kg/m
2
1 1 1 2 1 2
History of bariatric surgery
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Restrictive procedures: decrease
storage capacity of the stomach
(vertical banded gastroplasty,
laparoscopic adjustable gastric band,
or laparoscopic sleeve gastrectomy)
1 1 1 1 1 1
b. Malabsorptive procedures:
decrease absorption of nutrients and
calories by shortening the functional
length of the small intestine
(Roux-en-Y gastric bypass or
biliopancreatic diversion)
1 1 1 1 3 COCs: 3
Patch and ring: 1
Cardiovascular Disease
Multiple risk factors for atherosclerotic
cardiovascular disease (e.g., older age,
smoking, diabetes, hypertension, low
HDL, high LDL, or high triglyceride levels)
1 2 2* 3* 2* 3/4*
Hypertension
Systolic blood pressure ≥160 mm Hg or
diastolic blood pressure ≥100 mm Hg
are associated with increased risk for
adverse health events as a result of
pregnancy (Box 2).
a. Adequately controlled
hypertension
1* 1* 1* 2* 1* 3*
See table footnotes on page 103.

Recommendations and Reports
98 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
b. Elevated blood pressure levels
(properly taken measurements)
i. Systolic 140–159 mm Hg or
diastolic 90–99 mm Hg
1* 1* 1* 2* 1* 3*
ii. Systolic ≥160 mm Hg or diastolic
≥100 mm Hg
1* 2* 2* 3* 2* 4*
c. Vascular disease 1* 2* 2* 3* 2* 4*
History of high blood pressure during
pregnancy (when current blood
pressure is measurable and normal)
1 1 1 1 1 2
Deep venous thrombosis/
Pulmonary embolism
a. History of DVT/PE, not receiving
anticoagulant therapy
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
1 2 2 2 2 4
• History of estrogen-associated
DVT/PE
• Pregnancy-associated DVT/PE
• Idiopathic DVT/PE
• Known thrombophilia, including
antiphospholipid syndrome
• Active cancer (metastatic,
receiving therapy, or within
6 months after clinical remission),
excluding nonmelanoma skin
cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
1 2 2 2 2 3
b. Acute DVT/PE 2 2 2 2 2 4
c. DVT/PE and established anticoagu-
lant therapy for at least 3 months
i. Higher risk for recurrent DVT/PE
(one or more risk factors)
2 2 2 2 2 4*
• Known thrombophilia, including
antiphospholipid syndrome
• Active cancer (metastatic,
receiving therapy, or within
6 months after clinical remission),
excluding nonmelanoma skin
cancer
• History of recurrent DVT/PE
ii. Lower risk for recurrent DVT/PE
(no risk factors)
2 2 2 2 2 3*
d. Family history (rst-degree
relatives)
1 1 1 1 1 2
e. Major surgery
i. With prolonged immobilization 1 2 2 2
2 4
ii. Without prolonged
immobilization
1 1 1 1 1 2
f. Minor surgery without
immobilization
1 1 1 1 1 1
Known thrombogenic mutations (e.g.,
factor V Leiden; prothrombin mutation;
and protein S, protein C, and
antithrombin deciencies)
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
1* 2* 2* 2* 2* 4*
Supercial venous disorders
a. Varicose veins 1 1 1 1 1 1
b. Supercial venous thrombosis
(acute or history)
1 1 1 1 1 3*
Current and history of ischemic
heart disease
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation Initiation Continuation
1 2 3 2 3 3 2 3 4
See table footnotes on page 103.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 99
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Stroke (history of cerebrovascular
accident)
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
1 2 2 3 3 2 3 4
Valvular heart disease
Complicated valvular heart disease is
associated with increased risk for
adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 1 1 2
b. Complicated (pulmonary
hypertension, risk for atrial brillation,
or history of subacute bacterial
endocarditis)
1 1 1 1 1 4
Peripartum cardiomyopathy
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Normal or mildly impaired cardiac
function (New York Heart Association
Functional Class I or II: patients with no
limitation of activities or patients with
slight, mild limitation of activity) (1)
i. <6 months 2 2 1 1 1 4
ii. ≥6 months 2 2 1 1 1 3
b. Moderately or severely impaired
cardiac function (New York Heart
Association Functional Class III or IV:
patients with marked limitation of
activity or patients who should be at
complete rest) (1).
2 2 2 2 2 4
Rheumatic Diseases
Systemic lupus erythematosus
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
a. Positive (or unknown) antiphospho-
lipid antibodies
1* 1* 3* 3* 3* 3* 3* 4*
b. Severe thrombocytopenia 3* 2* 2* 2* 3* 2* 2* 2*
c. Immunosuppressive therapy 2* 1* 2* 2* 2* 2*
2* 2*
d. None of the above 1* 1* 2* 2* 2* 2* 2* 2*
Rheumatoid arthritis Initiation Continuation Initiation Continuation
a. Receiving immunosuppressive
therapy
2 1 2 1 1 2/3* 1 2
b. Not receiving immunosuppressive
therapy
1 1 1 2 1 2
Neurologic Conditions
Headaches
a. Nonmigraine (mild or severe) 1 1 1 1 1 1*
b. Migraine
i. Without aura (This category of
migraine includes menstrual
migraine.)
1 1 1 1 1 2*
ii. With aura 1 1 1 1 1 4*
Epilepsy
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
1 1 1* 1* 1* 1*
Multiple sclerosis
a. With prolonged immobility 1 1 1 2 1 3
b. Without prolonged immobility 1 1 1 2 1 1
Depressive Disorders
Depressive disorders 1* 1* 1* 1* 1* 1*
Reproductive Tract Infections and Disorders
Vaginal bleeding patterns Initiation Continuation
a. Irregular pattern without heavy
bleeding
1 1 1 2 2 2 1
b. Heavy or prolonged bleeding
(includes regular and irregular
patterns)
2* 1* 2* 2* 2* 2* 1*
See table footnotes on page 103.

Recommendations and Reports
100 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Unexplained vaginal bleeding
(suspicious for serious condition)
before evaluation
Initiation Continuation Initiation Continuation
4* 2* 4* 2* 3* 3* 2* 2*
Endometriosis 2 1 1 1 1 1
Benign ovarian tumors (including
cysts)
1 1 1 1 1 1
Severe dysmenorrhea 2 1 1 1 1 1
Gestational trophoblastic disease
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Suspected gestational trophoblastic
disease (immediate postevacuation)
i. Uterine size rst trimester 1* 1* 1* 1* 1* 1*
ii. Uterine size second trimester 2* 2* 1* 1* 1* 1*
b. Conrmed gestational trophoblas-
tic disease (after initial evacuation and
during monitoring)
Initiation Continuation Initiation Continuation
i. Undetectable/nonpregnant β-hCG
levels
1* 1* 1* 1* 1* 1* 1* 1*
ii. Decreasing β-hCG levels 2* 1* 2* 1* 1* 1* 1* 1*
iii. Persistently elevated β-hCG levels
or malignant disease, with no
evidence or suspicion of intrauterine
disease
2* 1* 2* 1* 1* 1* 1* 1*
iv. Persistently elevated β-hCG levels
or malignant disease, with evidence
or suspicion of intrauterine disease
4* 2* 4* 2* 1* 1* 1* 1*
Cervical ectropion 1 1 1 1 1
1
Cervical intraepithelial neoplasia 1 2 2 2 1 2
Cervical cancer (awaiting treatment) Initiation Continuation Initiation Continuation
4 2 4 2 2 2 1 2
Breast disease
Breast cancer is associated with
increased risk of adverse health events
as a result of pregnancy (Box 2).
a. Undiagnosed mass 1 2 2* 2* 2* 2*
b. Benign breast disease 1 1 1 1 1 1
c. Family history of cancer 1 1 1 1 1 1
d. Breast cancer
i. Current 1 4 4 4 4 4
ii. Past and no evidence of current
disease for 5 years
1 3 3 3 3 3
Endometrial hyperplasia 1 1 1 1 1 1
Endometrial cancer
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
4 2 4 2 1 1 1 1
Ovarian cancer
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
1 1 1 1 1 1
Uterine broids 2 2 1 1 1 1
Anatomical abnormalities
a. Distorted uterine cavity (any
congenital or acquired uterine
abnormality distorting the uterine
cavity in a manner that is incompat-
ible with IUD insertion)
4 4 — — — —
b. Other abnormalities (including
cervical stenosis or cervical
lacerations) not distorting the uterine
cavity or interfering with IUD insertion
2 2 — —
— —
Pelvic inammatory disease
a. Past PID Initiation Continuation Initiation Continuation
i. With subsequent pregnancy 1 1 1 1 1 1 1 1
ii. Without subsequent pregnancy 2 2 2 2 1 1 1 1
b. Current PID 4 2* 4 2* 1 1 1 1
See table footnotes on page 103.

Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 101
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Sexually transmitted diseases Initiation Continuation Initiation Continuation
a. Current purulent cervicitis or
chlamydial infection or gonococcal
infection
4 2* 4 2* 1 1 1 1
b. Vaginitis (including Trichomonas
vaginalis and bacterial vaginosis)
2 2 2 2 1 1 1 1
c. Other factors related to STDs 2* 2 2* 2 1 1 1 1
HIV
Initiation Continuation Initiation Continuation
High risk for HIV 2 2 2 2 1 1* 1 1
HIV infection
For women with HIV infection who are
not clinically well or not receiving ARV
therapy, this condition is associated
with increased risk for adverse health
events as a result of pregnancy (Box 2).
— — — — 1* 1* 1* 1*
a. Clinically well receiving ARV
therapy
1 1 1 1 — — — —
b. Not clinically well or not receiving
ARV therapy
2 1 2 1 — — — —
Other Infections
Schistosomiasis
Schistosomiasis with brosis of the liver
is associated with increased risk for
adverse health events as a result of
pregnancy (Box 2).
a. Uncomplicated 1 1 1 1 1 1
b. Fibrosis of the liver (if severe, see
Cirrhosis)
1 1 1 1 1 1
Tuberculosis
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
a. Nonpelvic 1 1 1 1 1* 1* 1* 1*
b. Pelvic 4 3 4 3 1* 1* 1* 1*
Malaria 1 1 1 1 1 1
Endocrine Conditions
Diabetes
Insulin-dependent diabetes; diabetes
with nephropathy, retinopathy, or
neuropathy; diabetes with other
vascular disease; or diabetes of
>20 years’ duration are associated with
increased risk of adverse health events
as a result of pregnancy (Box 2).
a. History of gestational disease 1 1 1 1 1 1
b. Nonvascular disease
i. Non-insulin dependent 1 2 2 2 2 2
ii. Insulin dependent 1 2 2 2 2 2
c. Nephropathy, retinopathy, or
neuropathy
1 2 2 3 2 3/4*
d. Other vascular disease or diabetes
of >20 years’ duration
1 2 2 3 2 3/4*
Thyroid disorders
a. Simple goiter 1 1 1 1 1 1
b. Hyperthyroid 1 1 1 1 1 1
c. Hypothyroid 1 1 1 1 1 1
Gastrointestinal Conditions
Inammatory bowel disease
(ulcerative colitis or Crohn’s disease)
1 1 1 2 2 2/3*
Gallbladder disease
a. Symptomatic
i. Treated by cholecystectomy 1 2 2 2 2 2
ii. Medically treated 1 2 2 2 2 3
iii. Current 1 2 2 2 2
3
b. Asymptomatic 1 2 2 2 2 2
History of cholestasis
a. Pregnancy related 1 1 1 1 1 2
b. Past COC related 1 2 2 2 2 3
See table footnotes on page 103.

Recommendations and Reports
102 MMWR / July 29, 2016 / Vol. 65 / No. 3
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
Viral hepatitis Initiation Continuation
a. Acute or are 1 1 1 1 1 3/4* 2
b. Carrier 1 1 1 1 1 1 1
c. Chronic 1 1 1 1 1 1 1
Cirrhosis
Severe cirrhosis is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Mild (compensated) 1 1 1 1 1 1
b. Severe (decompensated) 1 3 3 3 3 4
Liver tumors
Hepatocellular adenoma and malignant
liver tumors are associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
a. Benign
i. Focal nodular hyperplasia 1 2 2 2 2 2
ii. Hepatocellular adenoma 1 3 3 3 3 4
b. Malignant (hepatoma) 1 3 3 3 3 4
Respiratory Conditions
Cystic brosis
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
1* 1* 1* 2* 1* 1*
Anemias
Thalassemia 2 1 1 1 1 1
Sickle cell disease
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
2 1 1 1 1 2
Iron-deciency anemia 2 1 1 1 1 1
Solid Organ Transplantation
Solid organ transplantation
This condition is associated with
increased risk for adverse health events
as a result of pregnancy (Box 2).
Initiation Continuation Initiation Continuation
a. Complicated: graft failure (acute or
chronic), rejection, or cardiac allograft
vasculopathy
3 2 3 2 2 2 2 4
b. Uncomplicated 2 2 2 2 2 2 2 2*
Drug Interactions
Antiretroviral therapy Initiation Continuation Initiation Continuation
a. Nucleoside reverse transcriptase
inhibitors (NRTIs)
i. Abacavir (ABC) 1/2* 1* 1/2* 1* 1 1 1 1
ii. Tenofovir (TDF) 1/2* 1* 1/2* 1* 1 1 1 1
iii. Zidovudine (AZT) 1/2* 1* 1/2* 1* 1 1 1 1
iv. Lamivudine (3TC) 1/2* 1* 1/2* 1* 1 1 1 1
v. Didanosine (DDI) 1/2* 1* 1/2* 1* 1 1 1 1
vi. Emtricitabine (FTC) 1/2* 1* 1/2* 1* 1 1 1 1
vii. Stavudine (D4T) 1/2* 1* 1/2* 1* 1 1 1 1
b. Nonnucleoside reverse transcrip-
tase inhibitors (NNRTIs)
i. Efavirenz (EFV) 1/2* 1* 1/2* 1* 2* 1* 2* 2*
ii. Etravirine (ETR) 1/2* 1* 1/2* 1* 1 1 1 1
iii. Nevirapine (NVP) 1/2* 1* 1/2* 1* 1 1 1 1
iv. Rilpivirine (RPV) 1/2* 1*
1/2* 1* 1 1 1 1
c. Ritonavir-boosted protease
inhibitors
i. Ritonavir-boosted atazanavir
(ATV/r)
1/2* 1* 1/2* 1* 2* 1* 2* 2*
ii. Ritonavir-boosted darunavir
(DRV/r)
1/2* 1* 1/2* 1* 2* 1* 2* 2*
iii. Ritonavir-boosted fosamprenavir
(FPV/r)
1/2* 1* 1/2* 1* 2* 1* 2* 2*
iv. Ritonavir-boosted lopinavir
(LPV/r)
1/2* 1* 1/2* 1* 1 1 1 1
v. Ritonavir-boosted saquinavir
(SQV/r)
1/2* 1* 1/2* 1* 2* 1* 2* 2*
vi. Ritonavir-boosted tipranavir
(TPV/r)
1/2* 1* 1/2* 1* 2* 1* 2* 2*
See table footnotes on page 103.
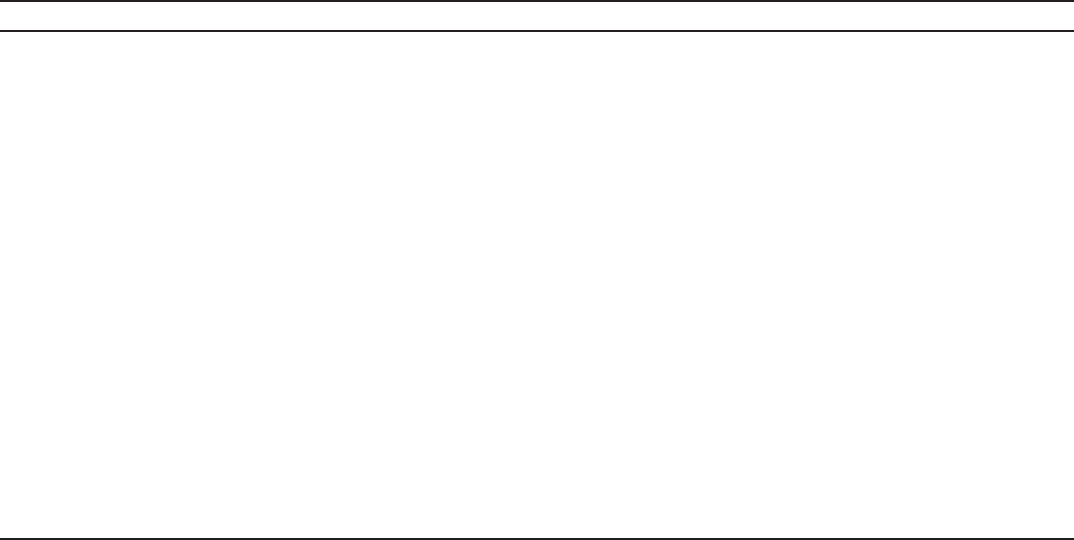
Recommendations and Reports
MMWR / July 29, 2016 / Vol. 65 / No. 3 103
US Department of Health and Human Services/Centers for Disease Control and Prevention
TABLE K1. (Continued) Summary of classifications for hormonal contraceptive methods and intrauterine devices
Condition Cu-IUD LNG-IUD Implants DMPA POP CHCs
d. Protease inhibitors without
ritonavir
i. Atazanavir (ATV) 1/2* 1* 1/2* 1* 1 1 1 2*
ii. Fosamprenavir (FPV) 1/2* 1* 1/2* 1* 2* 2* 2* 3*
iii. Indinavir (IDV) 1/2* 1* 1/2* 1* 1 1 1 1
iv. Nelnavir (NFV) 1/2* 1* 1/2* 1* 2* 1* 2* 2*
e. CCR5 co-receptor antagonists
i. Maraviroc (MVC) 1/2* 1* 1/2* 1* 1 1 1 1
f. HIV integrase strand transfer
inhibitors
i. Raltegravir (RAL) 1/2* 1* 1/2* 1* 1 1 1 1
ii. Dolutegravir (DTG) 1/2* 1* 1/2* 1* 1 1 1 1
iii. Elvitegravir (EVG) 1/2* 1* 1/2* 1* 1 1 1 1
g. Fusion inhibitors
i. Enfuvirtide 1/2* 1* 1/2* 1* 1 1 1 1
Anticonvulsant therapy
a. Certain anticonvulsants (phenytoin,
carbamazepine, barbiturates,
primidone, topiramate, and
oxcarbazepine)
1 1 2* 1* 3* 3*
b. Lamotrigine 1 1 1 1 1 3*
Antimicrobial therapy
a. Broad-spectrum antibiotics 1 1 1 1 1 1
b. Antifungals 1 1 1 1 1 1
c. Antiparasitics 1 1 1
1 1 1
d. Rifampin or rifabutin therapy 1 1 2* 1* 3* 3*
Psychotropic medications
a. SSRIs 1 1 1 1 1 1
St. John’s wort 1 1 2 1 2 2
Abbreviations: BMI = body mass index; COC = combined oral contraceptive; Cu-IUD = copper-containing IUD; DMPA = depot medroxyprogesterone acetate;
DVT = deep venous thrombosis; hCG = human chorionic gonadotropin; HDL = high-density lipoprotein; HIV = human immunodeficiency virus.; IUD = intrauterine
device; LDL = low-density lipoprotein; LNG-IUD = levonorgestrel-releasing IUD; NA = not applicable; PE = pulmonary embolism; PID = pelvic inflammatory disease;
POP = progestin-only pill; SSRI = selective serotonin reuptake inhibitor; STD = sexually transmitted disease.
* Consult the appendix for this contraceptive method for a clarification to this classification.
References
1. The Criteria Committee of the New York Heart Association. Nomenclature
and criteria for diagnosis of diseases of the heart and great vessels. 9th ed.
Boston, MA: Little, Brown & Co; 1994.

ISSN: 1057-5987 (Print)
The Morbidity and Mortality Weekly Report (MMWR) Series is prepared by the Centers for Disease Control and Prevention (CDC) and is available free of
charge in electronic format. To receive an electronic copy each week, visit MMWR’s free subscription page at http://www.cdc.gov/mmwr/mmwrsubscribe.html.
Paper copy subscriptions are available through the Superintendent of Documents, U.S. Government Printing Office, Washington, DC 20402; telephone
202-512-1800.
Readers who have difficulty accessing this PDF file may access the HTML file at http://www.cdc.gov/mmwr/volumes/65/rr/rr6503a1.htm?s_cid=rr6503a1_w.
Address all inquiries about the MMWR Series, including material to be considered for publication, to Executive Editor, MMWR Series, Mailstop E-90,
CDC, 1600 Clifton Rd., N.E., Atlanta, GA 30329-4027 or to [email protected].
All material in the MMWR Series is in the public domain and may be used and reprinted without permission; citation as to source, however, is appreciated.
Use of trade names and commercial sources is for identification only and does not imply endorsement by the U.S. Department of Health and Human Services.
References to non-CDC sites on the Internet are provided as a service to MMWR readers and do not constitute or imply endorsement of these organizations
or their programs by CDC or the U.S. Department of Health and Human Services. CDC is not responsible for the content of these sites. URL addresses
listed in MMWR were current as of the date of publication.
